Abstract
The purpose of this systematic review was to assess the state of adherence to HIV care such as HIV medication and appointment adherence among Black women in the United States. After a systematic search of CINAHL, PUBMED, EMBASE, and clinicialtrials.gov, 26 studies and 2 ongoing trials met inclusion criteria. Psychosocial factors such as intersectional stigmas and depression were among the salient factors associated with adherence to care behaviors in women living with HIV (WLWH). In addition, interpersonal factors such as social support and the patient-provider relationship were frequently associated with adherence to care behaviors. No culturally relevant interventions for Black WLWH were found in the literature, but one ongoing trial that was developed specifically for Black WLWH seemed promising. Considering the dearth of tailored interventions, more gender-specific and culturally relevant interventions are urgently needed to improve adherence to care behaviors and optimize health outcomes for Black WLWH.
Keywords: adherence, African American, female, HIV, retention in care, systematic review
Advances in the management of HIV infection have demonstrated efficacy in controlling the progression of the disease and extending the life expectancy of people living with HIV (PLWH), thereby, transforming HIV from an acute, life-threatening illness to a manageable, chronic condition (Panel on Antiretroviral Guidelines for Adults and Adolescents, 2016; Rodger et al., 2013). Living well with chronic HIV disease requires that PLWH develop adherence to care behaviors, including attending regular HIV clinic appointments (retention in care) and adhering to antiretroviral therapy (ART).
Retention in care is conceptualized as HIV health care utilization and it is operationalized in several ways: (a) missed visits, (b) appointment adherence, (c) visit consistency, (d) gaps in care, or (e) a combination of these measures. Retention in care is not to be confused with the term engagement in care, which represents the spectrum from initial linkage, subsequent retention, and re-engagement for those who dropped out of care. Retention in HIV care is essential for ART initiation, on-going receipt of ART, and ART adherence, which, in turn, are determinants of clinical outcomes (e.g., mortality rates and viral suppression; Mugavero, Davila, Nevin, & Giordano, 2010). Yet, only about half of PLWH are retained in HIV care and even fewer achieve viral suppression (aCenters for Disease Control and Prevention [CDC], 2016a). Therefore, adherence to HIV care represents critical modifiable behavior associated with viral suppression and optimal health outcomes such as improved quality of life and reduced mortality and HIV transmission (Mugavero, Lin, Willig, et al., 2009).
Despite advances in HIV treatment, gender and racial disparities exist for retention in HIV care and ART adherence (Ike, Hernandez, An, Huang, & Hall, 2015; Mugavero, Lin, Allison, et al., 2009). Black women continue to be disproportionately burdened by the HIV epidemic including higher incidence and prevalence rates and increased mortality rates (CDC, 2015). More specifically within the United States, 1 in 48 Black women as compared to 1 in 880 White women will be diagnosed with HIV in their respective lifetimes (CDC, 2016b). In 2014, the mortality rate (per 100,000 population) for Black women (13.8) was more than 17 times higher than the mortality rates for White women (0.8; CDC, 2015). A 2010 analysis of CDC data, suggested that retention rates were suboptimal for Black women with approximately 50% of women being retained in HIV care (Ike et al., 2015). Similarly, rates of viral suppression were worse for Black women living with HIV (WLWH) than their White counterparts (47% versus 42%, p <.05; Ike et al., 2015).
The multifaceted cognitive, social, and behavioral challenges faced by Black WLWH have the potential to influence suboptimal adherence to HIV care, retention in HIV care, and ART adherence (Konkle-Parker, Erlen, & Dubbert, 2008; Konkle-Parker, Erlen, Dubbert, & May, 2012; Moneyham et al., 1997). Yet few multilevel interventions exist to address the multiple dimensions of these modifiable antecedents (Tufts et al., 2015). Undoubtedly, there is a critical need to enhance retention in care and ART adherence in Black WLWH by first gaining a better understanding of determinants of retention in care and ART adherence in these women, which is critical to reducing disparities. The information in this review provides information to help program developers and health care professionals develop culturally appropriate interventions and provide culturally competent care to improve these pivotal adherence behaviors in Black WLWH. Therefore, the aim of our systematic review was to assess the state of the science for adherence to HIV care in Black WLWH by a) assessing determinants associated with retention in HIV care and ART adherence in Black WLWH; and b) reviewing the current literature for evidence-based retention in HIV care and ART adherence interventions developed and tailored for Black WLWH.
Theoretical Framework
The socioecological model of health promotion was used to guide the organization of data extraction for this review (McLeroy, Bibeau, Steckler, & Glanz, 1988). We chose the socioecological model because factors related to retention in care and ART adherence map to the multiple levels of the framework, ranging from the individual level to health care system and policy-level factors. The model has been used to explain and to develop interventions to influence behaviors from physical activity to intimate partner violence and smoking cessation to diabetes self-management (Glanz, Rimer, & Viswanath, 2008). The model has been used to help understand and explain multiple level factors related to retention in care in PLWH (Messer et al., 2013; Mugavero, Amico, Horn, & Thompson, 2013).
The socioecological model consists of factors at multiple levels that interact to influence behavior (McLeroy et al., 1988). The levels often consist of intrapersonal, interpersonal, community, and systems factors. The model posits that behaviors are influenced by the interplay between and among multiple level factors (Glanz et al., 2008; McLeroy et al., 1988). In order to maximally change behaviors, interventions must address factors across multiple levels.
The intrapersonal (individual) level consists of biologic, psychologic, and other individual factors that influence specific health outcomes. For Black WLWH, this may include non-modifiable factors such as age and race, and modifiable factors such as education, income, and psychosocial factors such as internalized stigma, resiliency, coping, and mental illness. The interpersonal or relationship level explains an individual’s closest social networks such as family, friends, and intimate partners, as well as health care providers, community health workers, and others. The community level consists of social settings in which individuals have interpersonal relationships such as neighborhoods, schools, and churches. The community also identifies characteristics of the social setting such as income, education, access to resources (i.e., transportation and health care facilities), stigma, and social norms (often referred to as social determinants of health). The societal level is the broadest level and consists of policies, funding, workforce, and social norms (Glanz et al., 2008; Mugavero et al., 2013). Understanding the complex interplay between levels of adherence behaviors (retention in care and mediation adherence) is critical to developing tailored multilevel interventions to improve health outcomes for Black WLWH.
Methods
Eligibility Criteria
Our review was conducted using the Preferred Reporting Items for Systematic Review (PRISMA). PRISMA is well-known in health care as an outline for reporting systematic reviews, with the purpose of informing practice and research (Liberati et al., 2009). We set eligibility criteria according to the purpose of our study, which was to assess determinants associated with adherence to care behaviors (retention in care and ART adherence) and review evidence-based adherence to care interventions tailored to Black WLWH. Studies were included if they met the following eligibility criteria: (a) written in English; (b) targeted only WLWH, with majority being Black; (c) focused on retention in HIV primary care and/or antiretroviral adherence; and (d) were published in a peer-reviewed journal after January 2000. The review was limited to articles published after 2000 because literature regarding ART, WLWH, and behavioral research were not widely available until 2000.
Information Sources
We searched the following databases and trial registry: CINAHL (Cumulative Index to Nursing and Allied Health Literature), PUBMED, and EMBASE. Studies were identified by searching the electronic databases, reviewing the reference lists of articles, and scanning the related articles. In addition, an expert in retention in care contributed articles for review. We also searched clinicaltrials.gov, which provided information about ongoing studies. The final search was performed on January 9, 2016.
Search Strategy
To identify articles, the following key terms were used to guide the search of all databases and trials registry: (Adherence OR retention in care) AND (antiretroviral adherence OR medication adherence) AND (HIV infection OR AIDS) AND (Black OR African American) AND female, or we used similar terms that were appropriate for specific databases (e.g., preferred terms in EMBASE).
Study Selection
Databases were searched using the key terms followed by a review of the titles and abstracts of articles that met the eligibility criteria. From the selected articles, the full-text documents were examined. The articles that: (a) were conducted in the United States; and (b) included participants 18 years of age and older were reviewed in more detail and all duplicated articles across databases were excluded.
Eligibility assessment was independently conducted by two reviewers. Disagreements were resolved by discussion between the two reviewers, if consensus could not be reached, a third reviewer was used to resolve disagreements. Each reviewer independently extracted and compiled each study’s characteristics into a table describing sample size, study purpose, study design, and identifying key findings as barriers or facilitators. Disagreements were resolved by discussion between members of the research team. The same process was followed to review ongoing trials registered at clinicaltrials.gov. Clinical trial studies that met our inclusion criteria were included.
Results
Our goal was to search the literature (i.e., published and grey literature) to assess antecedents associated with retention in HIV care and/or ART adherence in Black WLWH, and to assess evidence-based retention in HIV care and ART adherence interventions developed and tailored for Black WLWH. The initial literature search, using various combinations of our search terms such as adherence, retention in care, antiretroviral adherence, medication adherence, HIV, and AIDS, generated 415 published articles and 90 trials registered at clinicaltrials.gov. Figure 1 describes the process of article review and selection. After excluding articles not meeting the inclusion criteria, information was extracted from 21 articles for the primary aim, and 6 articles provided data from five interventions for the secondary aim. Note that 26 articles were reviewed, and one article was used for the primary and secondary aims. For registered trials at clinicaltrials.gov, information was extracted from 2 ongoing trials.
Figure 1.
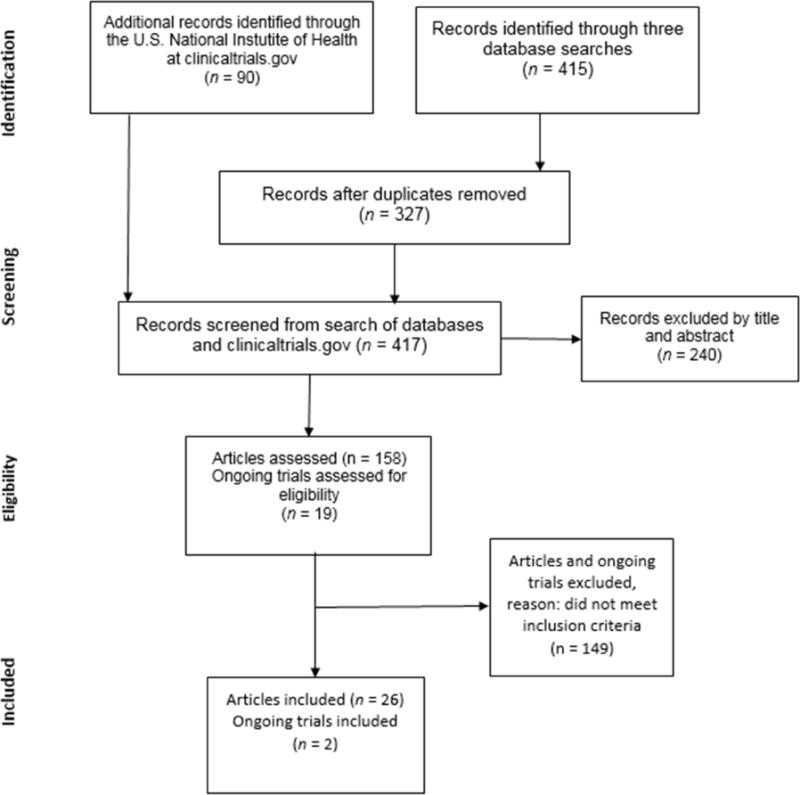
Flow diagram of literature search and review process.
Adapted from: Liberati et al. (2009).
The results for Aim I were guided by the socio-ecologic model. Figure 2 provides a visual of the findings detailed in an adapted socioecological framework (Mugavero et al., 2013). The results for Aim II will be presented in an aggregated format instead of separating the findings by levels because most of the interventions focused on the individual level.
Figure 2.
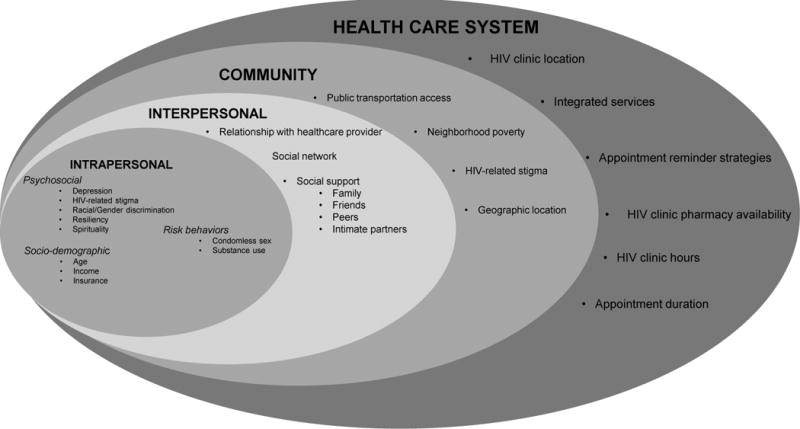
An adapted socioecological framework depicting the complex layers and interplay of intrapersonal (individual), interpersonal (relationship), community, and health care system factors that influence adherence to care among Black women living with HIV.
Note. Adapted from Mugavero et al., The state of engagement in HIV care in the United States: From cascade to continuum to control, Clinical Infectious Diseases, 2013, 57, 8, 1164–1171; reprinted by permission of the Infectious Diseases Society of America.
Determinants Associated with Adherence to Care - Individual
Individual level determinants were categorized into psychosocial, demographic, and risk behavior factors. Twelve articles examined ART adherence or retention in HIV care in Black WLWH. Retention in HIV care was less frequently examined.
Psychosocial
Psychosocial factors, including depression, perceived HIV-related stigma, and perceived racial discrimination, were significantly linked to retention in care and ART adherence in WLWH. Several studies reported that psychosocial factors were directly and indirectly associated with retention in HIV care and ART adherence (Kempf et al., 2010; McFall et al., 2013; Turan et al., 2016; Tyer-Viola et al., 2014; Walcott, Kempf, Merlin, & Turan, 2016). Internalized stigma was associated with suboptimal ART adherence in a subsample of predominately Black women from the Women’s Interagency HIV study (Turan et al., 2016). Internalized stigma is the acceptance of negative assumptions and feelings held by an individual living with HIV about the self because of personal HIV infection (Turan et al., 2016).
Depression was another frequently cited factor associated with suboptimal ART adherence (McFall et al., 2013; Tyer-Viola et al., 2014). In a 2014 cross-sectional study of WLWH in North America, depression was prevalent among Black WLWH and was a predictor of ART adherence (Tyer-Viola et al., 2014). In fact, more depressive symptoms mediated the relationship between stigma and ART adherence, suggesting that internalized stigma predicted depression, which predicted suboptimal medication adherence (Turan et al., 2016).
Perceived racial and gender discrimination were indirectly associated with viral suppression, which is the biological correlate of ART adherence. Black WLWH who reported higher perceived gender and racial discrimination were more likely to achieve viral suppression if they were more aware of racial and gender inequalities (Kelso et al., 2014). Nevertheless, women who were more aware of racial and gender inequalities were also more educated than women who were not as aware of inequalities. Thus, heightened awareness was potentially an indirect measure of education attainment.
In addition, resiliency is a coping mechanism directly linked to ART adherence. In a majority sample of Black women, higher resiliency scores were associated with optimal medication adherence (> 95%) and viral suppression (Dale et al., 2014).
Another coping mechanism frequently reported by Black WLWH was spirituality. Women attending an academic medical center in North Carolina reported that God was a priority in maintaining their health, retention in care, and ART adherence (Messer et al., 2013).
Socio-demographics
Age and low socioeconomic status (SES) played a role in ART adherence and retention in care in WLWH. Low SES defined by low income (< $24,000 USD) was associated with suboptimal adherence in Black WLWH (McFall et al., 2013). Findings also suggested that being under-insured or uninsured negatively impacted ART adherence and retention in care (Moneyham et al., 2010; Walcott et al., 2016).
Many resources are available to WLWH including medication assistance programs and subsidized health care. Yet many women are not aware of available services, do not have access to the services, or are unable to navigate the system to access the services, which has the potential to prevent women from being in care or taking their medications (Walcott et al., 2016).
Furthermore, age was a potential barrier to ART adherence. Younger age potentially increased a woman’s risk for deleterious health outcomes. In a few studies of women, older age was also associated with low viral load (Holstad, Diiorio, & McCarty, 2011; McCoy, Higgins, Zuniga, & Holstad, 2015).
Risk behavior
Engaging in risky sexual behaviors such as condomless sex and substance use in WLWH has been associated with suboptimal ART adherence. As indicated in the aforementioned study of 193 predominately Black WLWH (93%), engaging in risky behaviors – substance use and condomless sex – was linked with suboptimal ART adherence (Holstad, Diiorio, & McCarty, 2011). Substance use has been linked to suboptimal retention in HIV care, suboptimal ART adherence, and, ultimately, death in another study of WLWH (Anastos et al., 2005). Only one study linked risky sexual behavior to retention in HIV care (Blackstock, Blank, Fletcher, Verdecias, & Cunningham, 2015).
Determinants Associated with Adherence to Care - Interpersonal
Social networks and relationships can be enabling or motivating factors influencing health care outcomes such as retention in care and ART adherence in WLWH. The patient-provider relationship is often a salient factor positively associated with retention in care and ART adherence (DeMoss et al., 2014; Kempf et al., 2010; Messer et al., 2013; Tufts, Wessell, & Kearney, 2010; Webel & Higgins, 2012). In-depth interviews with 14 Black WLWH revealed that relationships with their providers positively influenced ART adherence (DeMoss et al., 2014). In addition to a positive patient-provider relationship in facilitating rapport, women in the rural Deep South reported wanting their providers to be caring and to inquire about their overall well-being (Boehme et al., 2012).
A positive patient-provider relationship with open communication, however, is not always a prominent determinant of retention in care. For example, in a study conducted by Wyatt, Carmona, Loeb, and Williams (2005), Black women did not report the patient-provider relationship as a barrier to retention in care. In addition to the patient-provider relationship, positive social support (disease-specific or general) has been frequently cited as influencing retention in care (Messer et al., 2013; Toth, Messer, & Quinlivan, 2013; Tufts et al., 2010). Many women spoke of social support as a facilitator and they reported actively seeking social support via friends, family, or treatment-specific peer groups, which boosted self-esteem and self-worth (Tufts et al., 2010). Women often suggested that social support buffered barriers; therefore, social support should be offered in the clinical setting (Toth et al., 2013). Motherhood or being a mother or a grandmother was another significant relationship factor. The role of caring for children or grandchildren motivated women to attend regularly scheduled primary HIV care appointments and take their ART as directed (Webel & Higgins, 2012).
Determinants Associated with Adherence to Care – Community
Community level factors such as a poverty, stigma, and lack of resources have been cited as barriers to retention in care and ART adherence. In a majority Black sample of women living in the Deep South, women reported not having the basic needs such as food and shelter, which have commonly been required for medication consumption and storage (Walcott et al., 2016). Women also reported distance from the clinic and limited access to public transportation, including limited services, distance to a bus stop, and infrequent routes as barriers to retention in care (Kempf et al., 2010; Moneyham et al., 2010; Walcott et al., 2016). However, this was not the case for all women. Blackstock et al. (2015) reported that women in a multisite study aimed at enhancing retention in care for women of color denied that transportation was a barrier to care. An estimated 70% of those women lived in an urban area where public transportation might have been easier to access, which was one potential explanation for contradictory findings. Indeed, these findings suggested that geographic and regional differences existed for Black WLWH for community level social determinants of health. In addition, organizations providing gas vouchers and transportation services were possible facilitators to retention in care (Kempf et al., 2010), but a cohort of women from rural Mississippi reported fear of disclosure and stigma when using transportation services provided by community organizations or insurance carriers (e.g., vans or taxis; Evans & Williams, 2013). Community level stigma is a salient factor associated with poor retention in HIV care. Women in the Deep South expressed apprehension with using HIV services for fear of being seen in the HIV Clinic, resulting in possible involuntary disclosure and HIV-related discrimination (Walcott et al., 2016). In addition to perceiving stigma, some women experienced stigma first-hand because of their HIV status. In an analysis of WLWH living in Georgia and Alabama, the women who reported higher levels of HIV discrimination were less likely to be retained in HIV care (Wingood et al., 2007).
Determinants Associated with Adherence to Care - System
Health care system level factors such as appointment reminder strategies, clinic hours and location, appointment duration, services offered, and pharmacy availability and hours, have the potential to negatively or positively impact retention in care and ART adherence (Kempf et al., 2010; Messer et al., 2013; Moneyham et al., 2010; Walcott et al., 2016). Appointment reminders, such as phone calls by clinic staff, positively influenced retention in care by encouraging women to attend upcoming appointments (Kempf et al., 2010). In a few studies, women complained about wait times during clinic visits, which they contributed to the staff being unorganized and scheduling too many patients (Kempf et al., 2010; Messer et al., 2013; Moneyham et al., 2010). Other women preferred to receive comprehensive care, allowing them to reduce health care visits, despite long wait times (Kempf et al., 2010). Receiving comprehensive care also reduced the need to seek health services outside the HIV clinic (Walcott, 2016). Furthermore, distance from the clinic was a potential barrier to retention in care despite geographic location. Black WLWH in the Western United States reported that distances from the clinic and difficulty contacting the clinic to schedule an appointment, were barriers to retention in care (Wyatt et al., 2005). Similarly, women living with HIV in the Deep South reported the ease of accessing conveniently located HIV services as a facilitator to retention in HIV care (Messer et al., 2013). A list of common factors (barriers and facilitators) to ART adherence and/or retention in care is depicted in Table 1. Two articles did not fit into a category and were not included in Table 1.
Table 1.
Barriers and Facilitators of Adherence to Care in Women Living With HIV
| Study | Methods/Study | Purpose | Stigma/ discrimination |
Depression | Transportation | Finance/ Housing |
Alcohol/drug/ Risky behavior |
Work schedule, employer |
Care-giver | Clinic/ Appointment system |
Health insurance |
Living Healthy | Provider relationship |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Turan et al., 2016 | Cohort study, 1,168 women, 67.5% Black | Test whether social isolation and depressive symptoms mediate a relationship between internalized stigma and HIV medication non-adherence in a large sample | B | B | |||||||||
| Blackstock et al., 2015 | Cross sectional, survey 748 WOC, 65.6% Black | Examine differences between women engaged to care and not engaged, and examine different targets of tailored intervention | B | B | B | B | B | B | |||||
| Walcott et al., 2016 | Qualitative Study, 14 stakeholders and 46 women, 89% Black | Understand poverty and community factors contributing to suboptimal engagement in deep south | B | B | B | B | B | ||||||
| DeMoss et al., 2014 | Qualitative Study 14 Black women | Explore influencing factors of ART adherence among Black women in deep south | B | F | F | ||||||||
| Kelso et al., 2014 | Cross Sectional, survey, 67 Black WLWH | Evaluate critical consciousness as a moderator of perceived gender and racial discrimination on HIV viral load | B | ||||||||||
| Tyer-Viola et al., 2014 | Convenience descriptive survey, 450 women, 50% Black | Understand SAT domains of contextual, environmental, and regulatory factors in relation to ART adherence | B | B | F | ||||||||
| McFall et al., 2013 | Cohort study, 887 women, 54% Black | Describe pattern of virologic failure by race/ethnicity, and relation of ART adherence to socioeconomic and psychological aspects | B | B | |||||||||
| Evans & Williams, 2013 | Qualitative study, single focus group, small pilot study 8 Black women | Find extent of transportation barriers to access clinic appointments | B | ||||||||||
| Messer et al., 2013 | Qualitative study, focus group 30 WOC, 91% Black | Assess barriers/facilitators for WOC in 3 stages of HIV continuum: testing, engaging in care, and retaining in care. | B | B | B | B | B | B | F | F | |||
| Toth et al., 2013 | Qualitative study 164 women, 85% Black | Find the extent of care barriers for WOC, and their relation to social demographic, mental/physical co-morbidities, and self-determination | B | B | B | B | |||||||
| Boehme et al., 2012 | Qualitative study, focus groups, 39 women, 92% Black | Explore the patient/provider relationship of rural WLWH | B/F | ||||||||||
| Webel & Higgins, 2012 | Qualitative Study, focus group 48 women, 69% Black | Examine social roles and their relation to self-management for WLWH | B | B | F | ||||||||
| Holstad, Diiorio, & McCarty, 2011 | RBT & MI, 207 women, 93% Black | Determine connection between ART adherence and risk reduction behaviors | B | ||||||||||
| Kempf et al., 2010 | Qualitative Study, focus group 40 women, 92% Black | Explore WLWH experiences with care retention, care barriers, and facilitators | B | B | B | B | B | B/F | F | F | |||
| Moneyham et al., 2010 | Qualitative study, focus group 44 Black women | Identify barriers to HIV care among WLWH in deep south | B | B | B | B | B | B | |||||
| Tufts et al., 2010 | Qualitative Study 21 Black women | Discuss barriers and facilitators to self-care | B | B | F | ||||||||
| Wingood et al., 2007 | Cross Sectional 366 women, 84.2% Black | Investigate correlation of self-reported HIV discrimination and health outcomes for Black women | B | ||||||||||
| Anastos et al., 2005 | Cohort study, 961 women, 59.6% Black | Investigate ART responses, understanding data limitations of race/ethnicity | B | ||||||||||
| Wyatt, et al. 2005 | Cohort study, 70 Black women | Describe substance abuse patterns among Black WLWH, and possible barriers to health | B | B | B |
Note. ART = antiretroviral therapy; WLWH = women living with HIV infection; RBT = randomized behavioral trial; MI = motivational interviewing; SAT = Social Action Theory; WOC = women of color; B = barriers; F = facilitators.
Tailored Evidence-Based Adherence to Care Interventions
All extracted articles (n = 6; 5 interventions) included interventions tailored for WLWH. However, no documented studies were culturally tailored for Black WLWH. Our outcome variables were ART adherence and retention in HIV care, but the outcomes variable for the six articles (4 interventions) reviewed were only ART adherence. The literature lacks interventions aimed at improving retention in care among women in general and tailored for Black women specifically. We excluded one of the six articles because it provided information about an ongoing research project and results were not presented (Holstad, DiIorio, & Magowe, 2006). Findings from the five remaining interventions are presented in Table 2.
Table 2.
Characteristics of Intervention Studies for WLWH
| Authors | Sample | Purpose | Design/Method | Pertinent Findings |
|---|---|---|---|---|
| Holstad, Diiorio, Kelley et al., 2011 | n = 203; 93% Black | Determine the efficacy of a group intervention based in MI in promoting ART adherence and risk reduction | RBT Survey MEMs cap | High MI attendees had higher ART adherence when compared to control at immediate and 3-month follow-up |
| Webel, 2010 | n = 89; 76% Black | Determine impact of a peer-led symptom management intervention on ART adherence, symptom management, and quality of life | RBT Survey | No difference between groups across time for ART adherence |
| Bova et al., 2008 | n = 187; 18% Black | Evaluate the Positive Life Skills Workshop | Mixed methods Focus groups | Significant improvement detected in ART adherence post-workshop Women felt a sense of accomplishment. They enjoyed the experience and wanted longer sessions |
| Jones et al., 2007 | n = 237; % Black not reported | Assess effects of a group cognitive behavioral stress management intervention plus a health education intervention on ART adherence | 2×2 factorial Survey | Significant group effect on ART adherence when compared to individual intervention. |
| Visnegarwala et al., 2006 | n = 54; 83% Black | Evaluate effects of weekly ART delivery on ART adherence for 6 months | Program evaluation Survey | No significant finding related to ART adherence. The weekly ART delivery group had a higher proportion of participants achieving viral suppression than those in the standard of care group. |
Note. WLWH = women living with HIV infection; RBT – Randomized behavioral trial; MI = motivational interviewing; ART = antiretroviral therapy.
The KHARMA project was a randomized controlled behavioral clinical trial consisting of 2-arms: motivational interviewing (MI) group and control group delivery over 8 weekly sessions. The study was conducted at five HIV clinical sites in a large southeastern metropolitan city and participants were randomized within sites to one of the two arms using a computer generated randomized program. The aim of the study was to evaluate the effects of MI in a group setting on ART adherence and risk reduction behaviors (Holstad, DiIorio, Kelley, Resnicow, & Sharma, 2011). The majority (93%) of the participants identified as Black. Although medication adherence was suboptimal (< 75%) across groups, women who attended more sessions (≥ 7) reported better ART adherence in the MI group, but the effect was only statistically significant at 3 months. Jones et al. (2007) reported similar group effects on ART adherence despite group intervention delivery in the SMART/EST Women’s Project II Trial. The trial consisted of 2 arms: a group intervention format and an individual education/information format, delivered in 150-minute biweekly sessions for 12 weeks. Participants were recruited from three metropolitan cities in the Southeastern and Northeastern United States. The aim of the study was to evaluate whether a group cognitive behavioral stress management (CBSM) intervention plus a health education intervention would improve HIV-relevant health behaviors such as ART adherence. Participating in the group intervention resulted in increased adherence (self-reported) when compared to women in the individual condition.
Knowing the impact of group interventions, Bova, Burwick, and Quinones (2008) developed a multi-session life skills workshop to improve ART adherence in WLWH in the Northeast region of the United States. The multi-session workshop improved ART adherence and the women reported that they enjoyed the information offered, skills presented, and environment created for socialization (Bova et al., 2008). Women also provided feedback to improve future workshops: including more time during sessions to socialize, longer timeframes for group sessions, and continued, long-term access to sessions (Bova et al., 2008). Despite existing evidence in support of group-based interventions, Webel (2010) found no significant differences in ART adherence between the control and intervention groups. The purpose of the randomized clinical trial was to test the effect of participation in a peer-led multi-session intervention for symptom management for WLWH. The participants were randomized to 2 arms, the experimental condition and the control group. The experimental group attended seven, peer-led sessions for 7 weeks, while the control group received a copy of an HIV symptom management strategies manual. The authors found no significant difference in medication adherence between the experimental and control groups. One rationale was that the study was not powered to detect significant group differences. The intervention was also short (7 weeks) as compared to other adherence-related interventions, which continued for at least 12 weeks.
The final study was a feasibility study to examine the influence of weekly ART delivery by a community outreach worker on ART adherence compared to standard of care and cognitive-behavioral health care team approaches. Participants were recruited using convenience sampling from an ambulatory HIV clinic in the Southern United States at different times from 1999 to 2003. The study lacked power, including only 54 participants across three groups, and did not yield significant findings related to ART adherence (Visnegarwala et al., 2006). However, findings suggested that sustained viral suppression during the 6-month study period was significantly better for women receiving weekly ART delivery when compared to standard of care (Visnegarwala et al., 2006). Therefore, the study had potential if adequately powered and rigorous research methods were implemented such as randomization. Unfortunately, lifelong weekly delivery of ART may not be cost effective and could possibly lead to untoward effects, such as community-level stigma and discrimination, all of which could be evaluated in an adequately powered and rigorously designed study.
Using our key terms, 90 trials were identified from clinicaltrials.gov matching our inclusion criteria. Nineteen trials remained after selecting only ongoing trials and we further excluded trials that were conducted outside of the United States and/or the primary aims were not ART adherence or retention in care, leaving two trials (see Table 3). Of the remaining two trials, only one trial was developed for Black women, but results were not available because the trial was ongoing.
Table 3.
Retention in Care and ART Adherence Randomized Controlled Trials for Women Living with HIV Registered at clinictrials.gov
| Principal Investigator | Clinical Trial Registration Number | Study Title | Design | Data Collection Method | Region | Tailored for Black WLWH | Estimated Enrollment |
|---|---|---|---|---|---|---|---|
| Dale | NCT02764853 | Striving Toward EmPowerment and Medication Adherence (STEP-UP) | RCT 2-arm Parallel assignment Single Blind |
Self-report Medical chart |
Northeast | Yes | 60 |
| Morse | NCT02964845 | Women’s Initiative Supporting Health Increasing Healthcare Access | RCT 2-arm Parallel assignment |
Self-report Serology |
Northeast | No | 100 |
Note. RCT = Randomized Control Trial; WLWH = women living with HIV infection.
Discussion
The purpose of our systematic review was to: (a) assess determinants associated with adherence to care behaviors (retention in care and ART adherence) and (b) review evidence-based adherence to care interventions tailored for Black WLWH. The socioecological framework was used to identify and categorize factors associated with retention in care and ART adherence in WLWH, in general, and Black women living with HIV, specifically.
Most of the published literature we reviewed was aimed at understanding individual-level determinants of ART adherence and retention in care. Several studies were cross-sectional or employed qualitative methods and none of the existing interventions were tailored for Black women, but one on-going clinical trial was promising. Notably, no interventions to improve retention in care and ART adherence and tailored for Black women were found. Furthermore, in many of the intervention studies, both conditions (control and experimental) where delivered in a group setting, allowing participants to receive similar time and attention, which could serve as an intervention. Clinical trials without usual care arms are limited and often cannot claim efficacy (Thompson & Schoenfeld, 2007).
Across articles, common modifiable and non-modifiable factors were associated with suboptimal ART adherence and/or retention in care. Non-modifiable individual-level factors associated with suboptimal ART adherence and retention in care included younger age, Black race, uninsured, and poverty. The literature supported findings that ART adherence improved with age. This suggests that younger women potentially have more barriers to care; therefore, future studies should focus on younger WLWH, and the unique challenges they face. Commonly cited modifiable and psychosocial factors such as intersecting stigmas and depression were associated with retention in care and ART adherence. The relationship between stigma and ART adherence was both direct and indirect. Turan et al. (2016) reported a significant relationship between internalized stigma and ART adherence. Stigma, a commonly reported factor impacting ART adherence, was found to be an antecedent to factors such as depression and inadequate social support resources. Using a serial mediation model, the findings of Turan et al. (2016) suggested that internalized stigma predicted less social support, which predicted higher depression, and higher depressive symptoms predicted suboptimal ART adherence. The link between stigma, discrimination, and adherence to care suggests that we need to find ways to help Black WLWH develop active coping skills to buffer the negative effects of HIV-related stigma and discrimination. These results have the potential to inform future research by providing targeted areas of focus for intervention development.
In addition to focusing on intersecting stigmas and depression as a pathway to improving ART adherence, we cannot ignore the importance of reducing engagement in risk behaviors to improve ART adherence as well as HIV transmission. Holstad, Diiorio, and McCarty (2011) found that women who engaged in risk behaviors (e.g., condomless transactional sex and substance use) were more likely to have suboptimal ART adherence. Several explanations have been offered for the link between sexual risk behavior and ART adherence such as having a risk taker personality, depression, fear of stigma, and gender-related factors. A person who is a risk taker may be more likely to skip doses, despite risk of virologic failure, or use condoms less frequently due to factors such as lack of impulse control, less education, denial of HIV, or other reasons (Holstad, Diiorio, & McCarty, 2011; Wilson et al., 2002). Depression, which is common in WLWH, may also play a role in suboptimal ART adherence (Turan et al., 2016; Wilson et al. 2002). Unintentional disclosure and fear of anticipated HIV stigma related to ART prescriptions or medication bottles may have negative implications for ART adherence (Holstad, Diiorio, & McCarty, 2011). In addition, some women depend on men for financial support and lack the power to negotiate condom use (Gakumo, Enah, & Azuero, 2011). Therefore, risk reduction strategies, as a method to improve ART adherence, are critical to future intervention development.
Inadequate social support and poor patient-provider relationships were consistently cited as interpersonal factors associated with or predictors of retention in care and/or ART adherence (DeMoss et al., 2014; Kempf et al., 2010; Messer et al., 2013; Toth, Messer, & Quinlivan, 2013; Tufts, Wessell, & Kearney, 2010; Webel & Higgins, 2012). Social support in the form of family, friends, or peers were seen as valuable resources that improved ART adherence and retention in care. Providing access to treatment-centric social support will be essential to facilitate ART adherence and retention in care.
The patient-provider relationship is also essential to improving ART adherence and retention in care. Patients may perceive a poor quality or weak relationship when providers fail to listen and communicate critical information about the plan of care. Patients may also perceive a poor-quality or weak relationship when providers fail to care about the patient by providing disease-focused care instead of holistic care (Boehme et al., 2012). In many cases, the patient-provider relationship encompasses more than patient satisfaction and communication; patients want to be actively included in the decision-making related to their health, health outcome, and the influence on their quality of life. Shared decision-making has been shown to improve health care outcomes such as adherence and should be evaluated in WLWH (Woods et al., 2006). In some cases, the patient-provider relationship may not be mendable, at which time a new provider should be assigned to prevent disengagement.
Very little research has focused on community and health care system level factors, but associations between transportation, discrimination, stigma, ART adherence, and retention in care have been established. Transportation is a salient community-level factor associated with retention in care and ART adherence (Kempf et al., 2010; Moneyham et al., 2010; Walcott et al., 2016). Indeed, our review revealed that even when transportation services were made available in the rural Deep South, stigma and discrimination may have mitigated the benefits offered by these resources (Blackstock et al., 2015). Evidence has suggested that the adverse effects of discrimination have a greater impact on health outcomes for Black WLWH by increasing individual-level factors such as psychological stress and depressive symptoms resulting in suboptimal ART adherence (Wingood et al., 2007), but few studies have focused on methods for reducing or coping with racial discrimination in Black WLWH as a way to improve ART adherence. Again, providing resources to give women the tools to cope with stressors such as racial and even gender discrimination has the potential to reduce depressive symptoms and improve retention in care and ART adherence. In terms of community, study findings suggested that place matters, such that factors will have variable importance and impact depending on a woman’s geographic location. Hence, future research should evaluate tools to train women to cope positively with and overcome discrimination and stigma.
The number of ongoing trials tailored for women and registered at clinicaltrials.gov was promising, but the dearth of trials tailored to Black WLWH was unfortunate, leaving an important area open for research. Our search yielded two trials that met inclusion criteria. Both trials focused on empowering women with the goal of improving medication adherence and/or retention in care (Dale NCT02764853; Morse NCT02964845) by using motivational interviewing or resiliency coping strategies. Both trials address trauma, such as physical or sexual abuse, and use multi-session approaches for intervention delivery, but only one trial (Dale NCT02764853) proposed to deliver an intervention tailored for Black WLWH. While the NCT02764853 (Morse) trial did not limit recruitment to only WLWH, the results may have important implications for women living with or at risk for HIV infection. Although limited, these studies, once completed, could provide a foundation for future research with the potential to improve health outcomes for women in general and Black women specifically.
Ultimately, to reduce health disparities in ART adherence and retention in care for Black WLWH, researchers must develop gender-specific and culturally appropriate interventions. In order to tailor interventions, we need to engage patients and other stakeholders early in the intervention development process by establishing equitable partnerships with shared discussion and decision-making (Carman et al., 2013; CDC, 2011).
The majority of the literature reviewed for WLWH focused on ART adherence. The literature regarding retention in care in WLWH was limited. The majority of studies used qualitative methods to elucidate barriers to retention in HIV care. Although the qualitative data provided a breadth of data about specific phenomena, having knowledge of the frequency, magnitude, direction, cause of the relationship, and generalizability would better inform intervention development. Therefore, additional mixed method or quantitative gender-specific research is needed with Black WLWH to advance the retention in care literature.
Our systematic review was not without limitations. While the search of existing literature was thorough and conducted by a team, relevant literature may have been unintentionally omitted. Nonetheless, the factors associated with adherence to care presented here were consistent across studies, which can assist researchers in developing targeted interventions. In addition, the search was limited by the availability of experimental research and the data available at clinicaltrials.gov.
Conclusion
Our review revealed a gap in the HIV literature. Despite Black women being disproportionately burdened by the HIV epidemic, few gender-specific and culturally appropriate interventions existed for Black WLWH, specifically those in the South where the epidemic has carried a greater burden. Several multilevel factors such as depression, stigma, discrimination, social support, and clinical level factors are known to directly and indirectly influence ART adherence and retention in HIV care. Few studies have examined predictors of retention in care and its relationship to ART adherence among Black WLWH. Therefore, future research should explore the aforementioned relationship in the targeted population. In addition, future intervention development should include stakeholders in the process, create social support resources, and focus on skill building as a method to teach coping strategies. This area of research is promising and ready for advances, including rigorous studies such as randomized controlled trials.
Key Considerations.
Black women continue to be disproportionately burdened by the HIV epidemic, but there is a paucity of documented gender-specific and/or culturally appropriate interventions aimed at addressing this burden.
A multilevel socioecological framework can be used not only to identify and organize data, but to develop gender-specific and culturally-appropriate strategies that focus on ART adherence and HIV appointment adherence interventions.
Psychosocial factors such as depression, stigma, and discrimination, as well as relationship factors such as relationship with providers, friends, family, and peers are essential factors to address for Black women living with HIV.
More research is needed to focus on developing or adapting existing interventions to make them culturally appropriate, gender-specific, and translatable to the practice setting.
Acknowledgments
Dr. Chapman Lambert was supported by the National Institute of Allergy and Infectious Disease and the National Institute of Mental Health of the National Institute of Health under the following award numbers: Diversity Supplement R01AI03661 (Michael Mugavero, PI) and R25MH087217 (Barbara J. Guthrie and Jean J. Schensul, PIs).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors report no real or perceived vested interests that relate to this article that could be construed as a conflict of interest.
Contributor Information
Crystal Chapman Lambert, Assistant Professor, School of Nursing, University of Alabama at Birmingham, Birmingham, Alabama, USA.
Michael J. Mugavero, Professor, School of Medicine, University of Alabama at Birmingham, Birmingham, Alabama, USA.
Yaseen S. Najjar, International Clinical Training Program (InterACT) Fellow, School of Medicine, University of Alabama at Birmingham, USA.
Comfort Enah, Associate Professor, School of Nursing, University of Alabama at Birmingham, Birmingham, Alabama, USA.
Barbara J. Guthrie, Professor, Bouve College of Health, School of Nursing, Northwestern University, Boston, Massachusetts, USA.
References
- Anastos K, Schneider MF, Gange SJ, Minkoff H, Greenblatt RM, Feldman J, Cohen M. The association of race, sociodemographic, and behavioral characteristics with response to highly active antiretroviral therapy in women. Journal of Acquired Immune Deficiency Syndrome. 2005;39(5):537–544. [PubMed] [Google Scholar]
- Blackstock OJ, Blank AE, Fletcher JJ, Verdecias N, Cunningham CO. Considering care-seeking behaviors reveals important differences among HIV-positive women not engaged in care: Implications for intervention. AIDS Patient Care and STDS. 2015;29(Suppl. 1):S20–S26. doi: 10.1089/apc.2014.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehme AK, Moneyham L, McLeod J, Walcott MW, Wright L, Seal P, Kempf MC. HIV-infected women’s relationships with their health care providers in the rural deep south: an exploratory study. Health Care for Women International. 2012;33(4):403–419. doi: 10.1080/07399332.2011.610533. [DOI] [PubMed] [Google Scholar]
- Bova C, Burwick TN, Quinones M. Improving women’s adjustment to HIV infection: Results of the Positive Life Skills Workshop Project. Journal of the Association of Nurses AIDS Care. 2008;19(1):58–65. doi: 10.1016/j.jana.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, Sweeney J. Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Affairs. 2013;32(2):223–231. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV surveillance report: Diagnosis of HIV infection in the US and dependents areas 2014. 2015 Retrieved from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2014-vol-26.pdf.
- Centers for Disease Control and Prevention. Selected national HIV prevention and care outcomes. 2016a Retrieved from http://www.cdc.gov/hiv/pdf/library/slidesets/cdc-hiv-prevention-and-care-outcomes.pdf.
- Centers for Disease Control and Prevention. Lifetime risk of HIV diagnosis. 2016b Retrieved from https://www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html.
- Centers for Disease Control and Prevention. Principles of community engagement. 2011 Retrieved from https://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf.
- Dale S, Cohen M, Weber K, Cruise R, Kelso G, Brody L. Abuse and resilience in relation to HAART medication adherence and HIV viral load among women with HIV in the United States. AIDS Patient Care and STDS. 2014;28(3):136–143. doi: 10.1089/apc.2013.0329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMoss M, Bonney L, Grant J, Klein R, del Rio C, Barker JC. Perspectives of middle-aged African-American women in the Deep South on antiretroviral therapy adherence. AIDS Care. 2014;26(5):532–537. doi: 10.1080/09540121.2013.841835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SD, Williams BE. Transportation-related barriers to care among Black women living with HIV/AIDS: “What you getting out of the cab for?”. Online Journal of Rural and Urban Research. 2013;3(1) doi: 10.1300/J013v46n02_07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gakumo C, Enah C, Azuero A. A comparison of sexual health and sexual pressure among young Black and Caucasian women. Journal of Health Disparities Research and Practice. 2011;7(2):107–117. [Google Scholar]
- Glanz K, Rimer B, Viswanath K. Health behaviors and health education. San Francisco, CA: John Wiley & Sons, Inc; 2008. [Google Scholar]
- Holstad MM, DiIorio C, Kelley ME, Resnicow K, Sharma S. Group motivational interviewing to promote adherence to antiretroviral medications and risk reduction behaviors in HIV infected women. AIDS and Behavior. 2011;15(5):885–896. doi: 10.1007/s10461-010-9865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holstad MM, DiIorio C, Magowe MK. Motivating HIV positive women to adhere to antiretroviral therapy and risk reduction behavior: The KHARMA Project. Online Journal of Issues in Nursing. 2006;11(1):5. [PubMed] [Google Scholar]
- Holstad MM, Diiorio C, McCarty F. Adherence, sexual risk, and viral load in HIV-infected women prescribed antiretroviral therapy. AIDS Patient Care and STDs. 2011;25(7):431–438. doi: 10.1089/apc.2010.0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ike N, Hernandez AL, An Q, Huang T, Hall HI. Care and viral suppression among women, 18 US jurisdictions; Paper presented at the CROI; 2015.2015. [Google Scholar]
- Jones DL, McPherson-Baker S, Lydston D, Camille J, Brondolo E, Tobin JN, Weiss SM. Efficacy of a group medication adherence intervention among HIV positive women: The SMART/EST Women’s Project. AIDS and Behavior. 2007;11(1):79–86. doi: 10.1007/s10461-006-9165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelso GA, Cohen MH, Weber KM, Dale SK, Cruise RC, Brody LR. Critical consciousness, racial and gender discrimination, and HIV disease markers in Black women with HIV. AIDS and Behavior. 2014;18(7):1237–1246. doi: 10.1007/s10461-013-0621-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempf MC, McLeod J, Boehme AK, Walcott MW, Wright L, Seal P, Moneyham L. A qualitative study of the barriers and facilitators to retention-in-care among HIV-positive women in the rural southeastern United States: Implications for targeted interventions. AIDS Patient Care and STDS. 2010;24(8):515–520. doi: 10.1089/apc.2010.0065. [DOI] [PubMed] [Google Scholar]
- Konkle-Parker DJ, Erlen JA, Dubbert PM. Barriers and facilitators to medication adherence in a southern minority population with HIV disease. Journal of the Association of Nurses in AIDS Care. 2008;19(2):98–104. doi: 10.1016/j.jana.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konkle-Parker DJ, Erlen JA, Dubbert PM, May W. Pilot testing of an HIV medication adherence intervention in a public clinic in the Deep South. Journal of the American Academy of Nurse Practitioners. 2012;24(8):488–498. doi: 10.1111/j.1745-7599.2012.00712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Annuals of Internal Medicine. 2009;151(4):W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- McCoy K, Higgins M, Zuniga JA, Holstad MM. Age, stigma, adherence and clinical indicators in HIV-infected women. HIV/AIDS Reseaerch and Treatment. 2015;2015(SE3):S1–S8. doi: 10.17140/HARTOJ-SE-3-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFall AM, Dowdy DW, Zelaya CE, Murphy K, Wilson TE, Young MA, Althoff KN. Understanding the disparity: Predictors of virologic failure in women using highly active antiretroviral therapy vary by race and/or ethnicity. Journal of Acquired Immune Deficiency Syndrome. 2013;64(3):289–298. doi: 10.1097/QAI.0b013e3182a095e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Messer LC, Quinlivan EB, Parnell H, Roytburd K, Adimora AA, Bowditch N, DeSousa N. Barriers and facilitators to testing, treatment entry, and engagement in care by HIV-positive women of color. AIDS Patient Care and STDs. 2013;27(7):398–407. doi: 10.1089/apc.2012.0435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moneyham L, McLeod J, Boehme A, Wright L, Mugavero M, Seal P, Kempf MC. Perceived barriers to HIV care among HIV-infected women in the Deep South. Journal of the Association of Nurses in AIDS Care. 2010;21(6):467–477. doi: 10.1016/j.jana.2010.03.003. [DOI] [PubMed] [Google Scholar]
- Moneyham L, Seals B, Sowell R, Hennessy M, Demi A, Brake S. The impact of HIV on emotional distress of infected women: Cognitive appraisal and coping as mediators. Scholarly Inquiry in Nursing Practice. 1997;11(2):125–145. discussion 147-151. [PubMed] [Google Scholar]
- Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: From cascade to continuum to control. Clinical Infectious Disease. 2013;57(8):1164–1171. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- Mugavero MJ, Davila JA, Nevin CR, Giordano TP. From access to engagement: Measuring retention in outpatient HIV clinical care. AIDS Patient Care and STDs. 2010;24(10):607–613. doi: 10.1089/apc.2010.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugavero MJ, Lin HY, Allison JJ, Giordano TP, Willig JH, Raper JL, Saag MS. Racial disparities in HIV virologic failure: Do missed visits matter? Journal of Acquired Immune Deficiency Syndrome. 2009;50(1):100–108. doi: 10.1097/QAI.0b013e31818d5c37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugavero MJ, Lin HY, Willig JH, Westfall AO, Ulett KB, Routman JS, Allison JJ. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clinical Infectious Diseases. 2009;48(2):248–256. doi: 10.1086/595705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolecents. 2016 Retrieved from https://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf.
- Rodger AJ, Lodwick R, Schechter M, Deeks S, Amin J, Gilson R, Phillips A. Mortality in well controlled HIV in the continuous antiretroviral therapy arms of the SMART and ESPRIT trials compared with the general population. AIDS. 2013;27(6):973–979. doi: 10.1097/QAD.0b013e32835cae9c. [DOI] [PubMed] [Google Scholar]
- Thompson BT, Schoenfeld D. Usual care as the control group in clinical trials of nonpharmacologic interventions. Proceedings of the American Thoracic Society. 2007;4(7):577–582. doi: 10.1513/pats.200706-072JK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth M, Messer LC, Quinlivan EB. Barriers to HIV care for women of color living in the Southeastern US are associated with physical symptoms, social environment, and self-determination. AIDS Patient Care and STDs. 2013;27(11):613–620. doi: 10.1089/apc.2013.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tufts KA, Wessell J, Kearney T. Self-care behaviors of African American women living with HIV: A qualitative perspective. Journal of the Association of Nurses in AIDS Care. 2010;21(1):36–52. doi: 10.1016/j.jana.2009.07.006. [DOI] [PubMed] [Google Scholar]
- Tufts KA, Johnson KF, Shepard JG, Lee JY, Bait MS, Mahan LB, Kims MT. Novel interventions for HIV self-management in African American women: A systematic review of mHealth interventions. Journal of the Association of Nurses in AIDS Care. 2015;26(2):139–150. doi: 10.1016/j.jana.2014.08.002. [DOI] [PubMed] [Google Scholar]
- Turan B, Smith W, Cohen MH, Wilson TE, Adimora AA, Merenstein D, Turan JM. Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: The mediating roles of social isolation and depression. Journal of Acquired Immune Deficiency Syndrome. 2016;72(2):198–205. doi: 10.1097/QAI.0000000000000948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyer-Viola LA, Corless IB, Webel A, Reid P, Sullivan KM, Nichols P. Predictors of medication adherence among HIV-positive women in North America. Journal of Obstetric Gynecololgic and Neonatal Nursing. 2014;43(2):168–178. doi: 10.1111/1552-6909.12288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visnegarwala F, Rodriguez-Barradass MC, Graviss EA, Caprio M, Nykyforchyn M, Laufman L. Community outreach with weekly delivery of anti-retroviral drugs compared to cognitive-behavioural health care team-based approach to improve adherence among indigent women newly starting HAART. AIDS Care. 2006;18(4):332–338. doi: 10.1080/09540120500162155. [DOI] [PubMed] [Google Scholar]
- Walcott M, Kempf MC, Merlin JS, Turan JM. Structural community factors and sub-optimal engagement in HIV care among low-income women in the Deep South of the USA. Culture Health and Sexuality. 2016;18(6):682–694. doi: 10.1080/13691058.2015.1110255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webel AR. Testing a peer-based symptom management intervention for women living with HIV/AIDS. AIDS Care. 2010;22(9):1029–1040. doi: 10.1080/09540120903214389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webel AR, Higgins PA. The relationship between social roles and self-management behavior in women living with HIV/AIDS. Womens Health Issues. 2012;22(1):e27–33. doi: 10.1016/j.whi.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson TE, Barron Y, Cohen M, Richardson J, Greenblatt R, Sacks HS, Young M. Adherence to antiretroviral therapy and its association with sexual behavior in a national sample of women with human immunodeficiency virus. Clinical Infectious Disease. 2002;34(4):529–534. doi: 10.1086/338397. [DOI] [PubMed] [Google Scholar]
- Wingood GM, Diclemente RJ, Mikhail I, McCree DH, Davies SL, Hardin JW, Saag M. HIV discrimination and the health of women living with HIV. Women and Health. 2007;46(2–3):99–112. doi: 10.1300/J013v46n02_07. [DOI] [PubMed] [Google Scholar]
- Woods ER, Klein JD, Wingood GM, Rose ES, Wypij D, Harris SK, Diclemente RJ. Development of a new Adolescent Patient-Provider Interaction Scale (APPIS) for youth at risk for STDs/HIV. Journal of Adolescent Health. 2006;38(6):753 e751–757. doi: 10.1016/j.jadohealth.2005.08.013. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Carmona JV, Loeb TB, Williams JK. HIV-positive Black women with histories of childhood sexual abuse: Patterns of substance use and barriers to health care. Journal of Health Care for the Poor and Underserved. 2005;16(4 Suppl B):9–23. doi: 10.1353/hpu.2005.0120. [DOI] [PubMed] [Google Scholar]


