Abstract
We report a case of a 50-year-old man with a history of liver cirrhosis and colon cancer post end colostomy presenting to the emergency department with stomal bleeding and passage of clots into the colostomy bag. The patient was treated with transjugular intrahepatic portosystemic shunt (TIPS) and concomitant embolization of the stomal varices via the TIPS shunt using N-butyl cyanoacrylate mixed with ethiodol. Although stomal variceal bleeding is uncommon, this entity can have up to 40% mortality upon initial presentation, given the challenges in diagnosis and management. Currently, there are no established standard treatments for stomal variceal bleeding. In addition, to the best of our knowledge, there are no cases in the current literature in which treatment of this entity is performed with a combination of TIPS shunt placement and N-butyl cyanoacrylate variceal embolization.
Keywords: Stomal varices, TIPS, Cirrhosis, Colon cancer, Embolization, NBCA
Case report
The patient is a 50-year-old man who presented to the emergency department (ED) with abdominal pain in April 2015. The patient's history was significant for alcohol abuse, hepatitis C, and liver cirrhosis diagnosed 4 years previously. An abdominal computed tomography (CT) scan subsequently demonstrated liver cirrhosis (Fig. 1A and B) and an eccentric mass-like focal thickening of the sigmoid colon measuring 3.9 × 3.2 cm (Fig. 2A and B). The patient was then referred to the colorectal surgery for further workup. The patient underwent a colonoscopy, and a colonic mass biopsy revealed carcinoma in situ. The plan was to undergo repeat colonoscopy for tattooing of the lesion. However, the patient then presented to the ED with abdominal pain and hematuria. A small-bowel follow-through demonstrated multifocal moderate small-bowel dilation and delayed transit time consistent with small-bowel obstruction (Fig. 3). A repeat CT of the abdomen and pelvis showed a 12 × 11.8 × 11.5 cm mixed soft tissue low-density lesion (Fig. 4A-C) at the superior right lateral aspect of the bladder without a clear fat plane demonstrated between the lesion and the bladder.
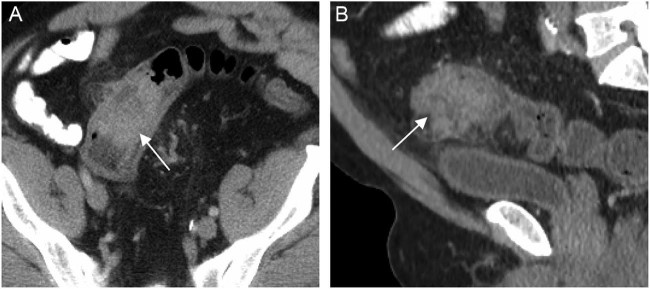
Fig. 1.
Computed tomography (A) and ultrasound (B) demonstrating irregular, nodular hepatic contours (arrows) compatible with cirrhosis.
Fig. 2.
Coronal (A) and sagittal (B) computed tomographies demonstrating an eccentric mass-like focal thickening (arrows) of the sigmoid colon measuring 3.9 × 3.2 cm, which proved to be colon adenocarcinoma.
Fig. 3.

A small-bowel follow-through demonstrates multifocal moderate small-bowel dilation (arrows) and delayed transit time consistent with small-bowel obstruction.
Fig. 4.
Axial (A), coronal (B), and sagittal (C) computed tomographies show a 12.0 × 11.8 × 11.5 cm mixed soft tissue hypodense lesions (arrows) abutting the superior right lateral aspect of the bladder without a fat plane seen between the lesion and the bladder. This proved to be an abscess.
The patient then underwent a laparoscopic sigmoid colectomy with end colostomy and closure of the distal rectal stump in June 2015. Intraoperatively, the mass thought to be arising from the bladder was found to be an intraperitoneal abscess likely from a perforated appendix, so appendectomy and abscess drainage were also performed during the surgery. The patient was then diagnosed with stage IIA colon adenocarcinoma. In July 2015, the patient underwent laparoscopic lysis of adhesions for release of small-bowel obstruction and drainage of a new peritoneal abscess.
The patient was not a surgical candidate for ostomy reversal and parastomal hernia repair secondary to portal hypertension and engorged intra-abdominal veins. The patient then presented to the ED in April 2017 for diffuse abdominal pain and bleeding and passage of large clots through his stoma. The patient underwent esophagogastroduodenoscopy (EGD) and there was no evidence of varices or portal hypertensive gastropathy. CT angiogram performed on admission showed prominent venous collaterals to the stoma (Figs. 5A-C and 6). The patient then underwent TIPS procedure for portal venous decompression and selective inferior mesenteric vein varix embolization using N-butyl cyanoacrylate (NBCA) mixed with ethiodol in April 2017 (Fig. 7, Fig. 8, Fig. 9, Fig. 10). The inferior mesenteric vein varices were confined only to the sigmoid colon, which was the external portion of the ostomy. The patient was discharged from the hospital in stable condition a few days later.
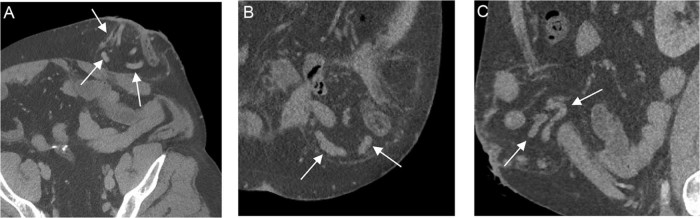
Fig. 5.
Axial (A), coronal (B), and sagittal (C) computed tomography angiograms demonstrate stomal varices (arrows).
Fig. 6.

Computed tomography venogram 3-dimensional reconstruction showing stomal varices arising from the inferior mesenteric vein. The circle is part of the 3D reconstruction. It is piece of the external ostomy bag.
Fig. 7.
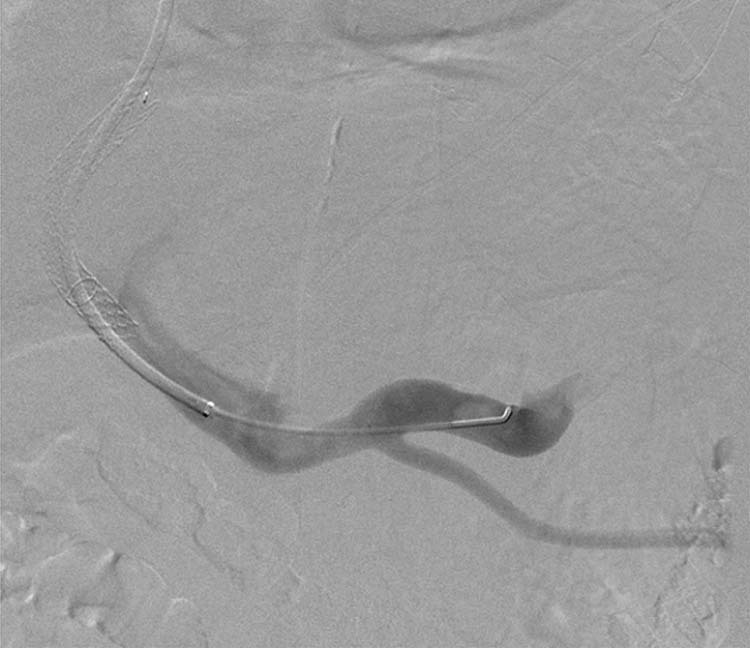
Digital subtraction venography via the transjugular intrahepatic portosystemic shunt (TIPS) shunt demonstrating the confluence of the inferior mesenteric vein into the splenic vein.
Fig. 8.

Digital subtraction venography showing stomal varices arising from the inferior mesenteric vein sigmoid colon tributaries.
Fig. 9.
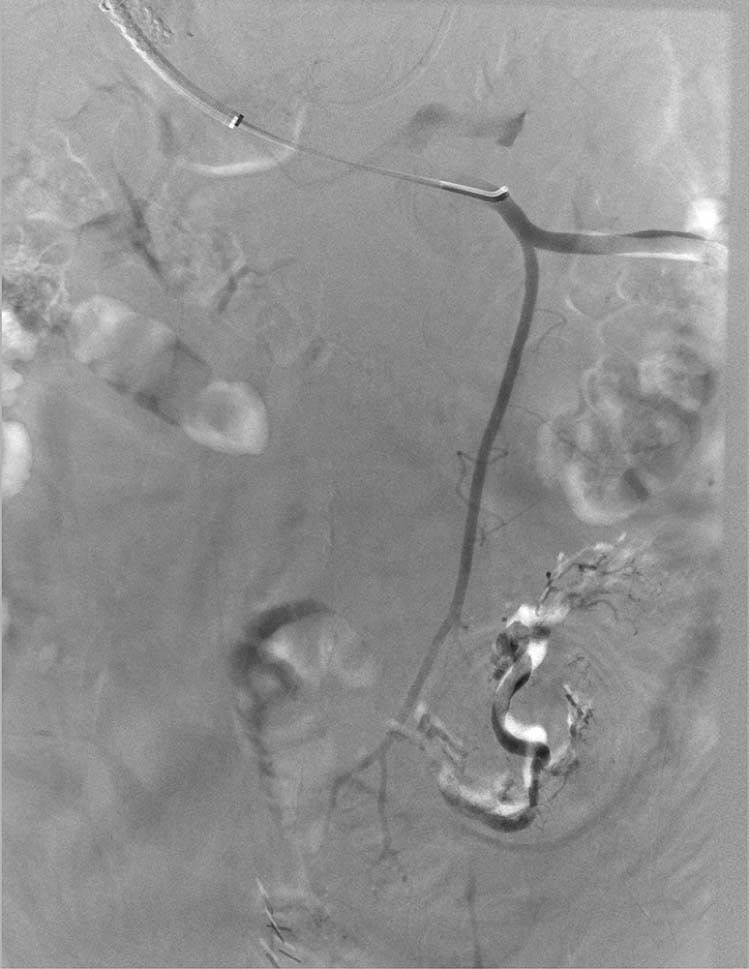
Digital subtraction venography demonstrating stasis of the sigmoidal stomal varices with normal opacification of the superior rectal vein.
Fig. 10.
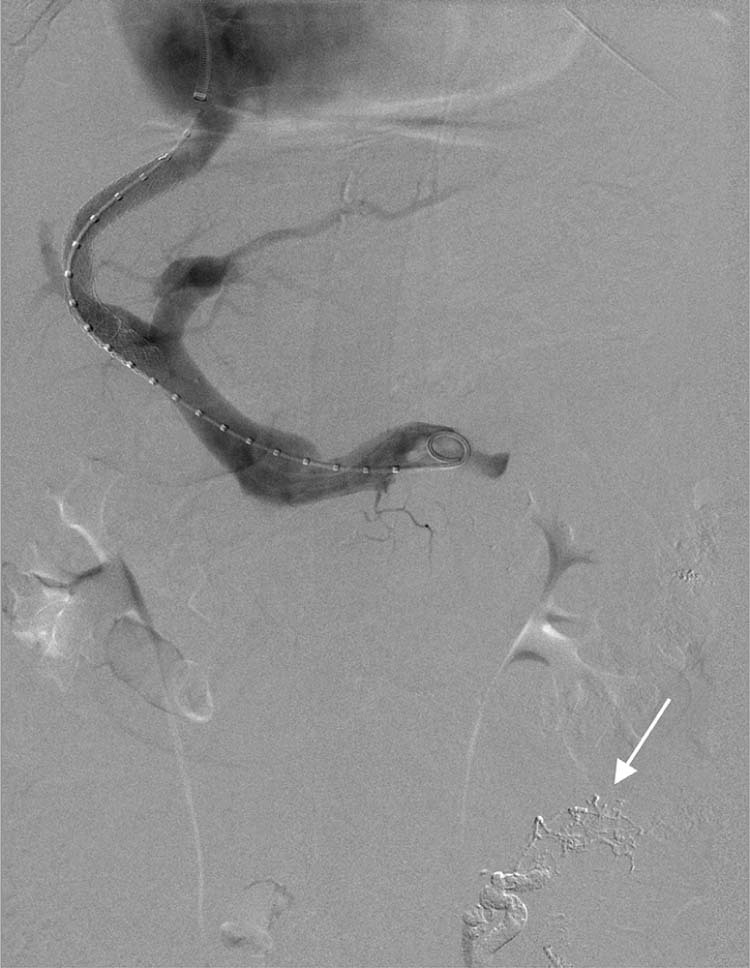
Digital subtraction venography demonstrating successful transjugular intrahepatic portosystemic shunt (TIPS) shunt placement and N-butyl cyanoacrylate cast demarcating the embolized stomal varices (arrow).
Discussion
Patients with liver cirrhosis and portal hypertension commonly develop varices that typically arise in the gastroesophageal region. Rarely, “ectopic” varices occur at other sites along the gastrointestinal tract; these varices account for only 5% of variceal bleeds [1]. The first case of stomal varices was described in 1968 during a study that used surgical colon exclusion for treatment of hepatic encephalopathy [2]. Since that time, there have only been anecdotal or small case series with short-term follow-up periods in the current literature [2].
Patients present with stomal hemorrhage from stomal varices, which can be recognized as a purplish hue in the area of the stoma [1]. Bleeding from stomal varices is an uncommon entity but carries an estimated risk of death of 3%-4% [3]. However, the mortality from initial bleeding can be quite high (40%), likely secondary to delay in diagnosis and treatment [4]. Various imaging modalities such as ultrasound and CT aid in diagnosis demonstrating cirrhosis, stigmata of chronic liver disease, and location of varices.
Although the standard of treatment for stomal variceal bleeding is not fully established, treatment currently ranges from conservative management to surgery [5].
The recommended first step in the treatment of an acute variceal bleed includes local therapy, including application of pressure, epinephrine-soaked gauze, Gelfoam, suturing, and cauterization [1], [2]. Band ligation and sclerotherapy have been described as options for management but at high risk of necrosis and perforation [2]. In a patient in need of portal decompression, TIPS is the preferred treatment as this will treat the underlying pathology by decreasing portal hypertension [6], [7]. The TIPS can be performed alone or in combination with variceal embolization. Most reports in literature describe the use of coils for embolization. In cases of TIPS failure, surgical shunting is appropriate [2]. A liver transplant is the ultimate management for patients with decompensated liver failure and recurrent stomal variceal bleeding [6].
Coil embolization has a high incidence of recurrent hemorrhage secondary to vessel recanalization and new varix formation eventually necessitating intervention [2], [5]. TIPS procedure with the use of coil embolization of stomal varices has been described, but no evidence suggests this is superior to TIPS alone [2]. There have also been reports in the literature describing rebleeding post TIPS even when the trans-sinusoidal pressure gradient is reduced to less than 12 mm Hg [2]. In most cases in the current literature, TIPS has been performed with or without coil embolization or, in 1 study, with NBCA embolization alone [8]. To the best of our knowledge, there are no reports in the current literature of management of stomal variceal hemorrhage using a combination of TIPS and NBCA variceal embolization.
Conclusions
We present an uncommon case of stomal variceal bleeding treated with TIPS and sigmoid colon variceal embolization using NBCA. Stomal varices are a rarely reported topic in the literature and there are no standard treatments currently established. Although unusual, recognizing this entity as a source for stomal bleeding is paramount for expeditious diagnosis and management.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Ethical approval: This case report does not contain any studies with human participants performed by any of the authors.
Informed consent was not obtained in this case report.
References
- 1.Norton I.D., Andrews J.C., Kamath P.S. Management of ectopic varices. Hepatology. 1998;28:1154–1158. doi: 10.1002/hep.510280434. [DOI] [PubMed] [Google Scholar]
- 2.Spier B.J., Fayyad A.A., Lucey M.R., Johnson E.A., Wojtowycz M., Rikkers L. Bleeding stomal varices: case series and systematic review of the literature. Clin Gastroenterol Hepatol. 2008;6:346–352. doi: 10.1016/j.cgh.2007.12.047. [DOI] [PubMed] [Google Scholar]
- 3.Naidu S.G., Castle E.P., Kriegshauser J.S., Huettl E.A. Direct percutaneous embolization of bleeding stomal varices. Cardiovasc Intervent Radiol. 2010;33:201–204. doi: 10.1007/s00270-009-9536-4. [DOI] [PubMed] [Google Scholar]
- 4.Lashley D.B., Saxon R.R., Fuchs E.F., Chin D.H., Lowe B.A. Bleeding ileal conduit stomal varices: diagnosis and management using transjugular transhepatic angiography and embolization. Urology. 1997;50:612–614. doi: 10.1016/S0090-4295(97)00267-7. [DOI] [PubMed] [Google Scholar]
- 5.Maciel M.J., Pereira O.I., Motta Leal Filho J.M., Ziemiecki Junior E., Cosme S.L., Souza M.A. Peristomal variceal bleeding treated by coil embolization using a percutaneous transhepatic approach. World J Clin Cases. 2016;4:25–29. doi: 10.12998/wjcc.v4.i1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alkari B., Shaath N.M., El-Dhuwaib Y., Aboutwerat A., Warnes T.W., Chalmers N. Transjugular intrahepatic porto-systemic shunt and variceal embolisation in the management of bleeding stomal varices. Int J Colorectal Dis. 2005;20:457. doi: 10.1007/s00384-004-0669-2. [DOI] [PubMed] [Google Scholar]
- 7.Morris C.S., Najarian K.E. Transjugular intrahepatic portosystemic shunt for bleeding stomal varices associated with chronic portal vein occlusion: long-term angiographic, hemodynamic, and clinical follow-up. Am J Gastroenterol. 2000;95:2966–2968. doi: 10.1111/j.1572-0241.2000.03211.x. [DOI] [PubMed] [Google Scholar]
- 8.Yao D.H., Luo X.F., Zhou B., Li X. Ileal conduit stomal variceal bleeding managed by endovascular embolization. World J Gastroenterol. 2013;19:8156–8159. doi: 10.3748/wjg.v19.i44.8156. [DOI] [PMC free article] [PubMed] [Google Scholar]