Abstract
We described the utility of computed tomography (CT) angiography in detection of bleeding vessels for a rapid percutaneous arterial embolization of the spontaneous rectus sheath hematoma. A 70-year-old woman comes to our attention with acute abdominal pain and a low hemoglobin level. An unenhanced CT was performed demonstrating a large rectus sheath hematoma. A conservative management was initially established. Despite this therapy, the abdominal pain increased together with a further decrease of hemoglobin values. A CT angiography was then performed, demonstrating an active bleeding within the hematoma and addressing the patient to a rapid percutaneous arterial embolization.
Keywords: Rectus sheath hematoma, Acute abdomen, Arterial embolization, CT angiography, Active bleeding
Introduction
Rectus sheath hematoma (RSH) is a rare clinical condition caused by bleeding into the rectus abdominis muscles due to the rupture of superior or inferior epigastric artery or caused by direct muscular tear [1]. The frequency of this occurrence is increasing with the use of anticoagulant therapy [2], and it can generate a misdiagnosis as it may mimic many acute abdominal conditions [3], [4]. The most common presenting features are acute abdominal pain, palpable abdominal wall mass and decrease in hemoglobin levels [1], [3]. Appropriate and early diagnosis is important to exclude a false acute abdomen and to avoid unnecessary exploratory surgery. Computed tomography (CT) is the main diagnostic modality; in particular, CT angiography can demonstrate the existence of the active bleeding within the hematoma [5], [6]. In most cases, the RSH management is conservative [3]. However, an invasive intervention should be always considered when clinical severity criteria are present, such as a neurologic deficit and hemodynamic instability or persistent abdominal pain [7].
We described a case of a 70-year-old woman with a large RSH, in which the CT angiography examination proved to be decisive for urgent embolization.
Case report
A 70-year-old woman, subjected to an anticoagulant therapy after a recent aortic valve repair, came to our observation manifesting an acute abdomen, anemia, palpable abdominal mass, and abdominal pain localized in the right subcostal region. Initially, the patient underwent a liver sonography on suspicion of an acute cholecystitis, but the examination did not confirm this clinical suspicion. In addition, the patient denied any recent traumatic event. Because of the hemoglobin level reduction at 9.5 g/dL together with the presence of an apparent peritoneal irritation, an urgent unenhanced CT was done. The CT examination revealed a 12 × 9 × 4-cm right RSH with a mixed pattern, with fluid-fluid levels due to hemorrhagic sedimentation (hematocrit effect) (Fig. 1). The choice for an unenhanced CT examination was considered because of the high serum creatinine level and the condition of solitary kidney for prior nephrectomy. Then a conservative management with analgesia, intravenous hydration, stopping of anticoagulants, and transfusion has been established. Despite this therapy, in the subsequent 2 days, the abdominal pain worsened and the hemoglobin level continued to decrease (8 g/dL). The clinical worsening justified the appeal to an urgent CT angiography, demonstrating an active arterial extravasation (small jet) within the hematoma (Fig. 2), originating from a media branch of right superior epigastric artery (Fig. 3).
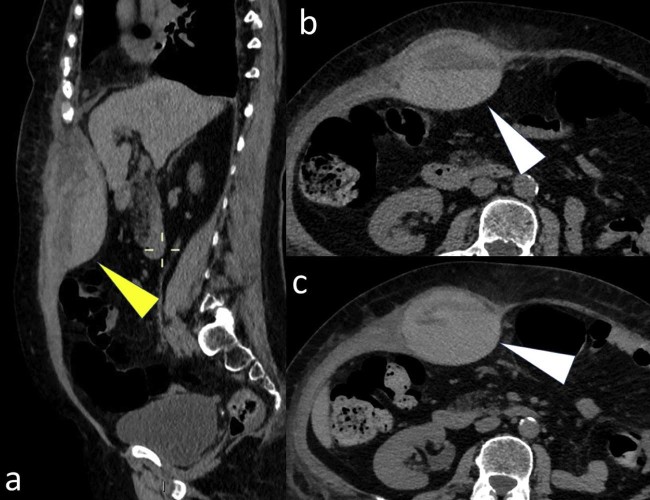
Fig. 1.
Unenhanced computed tomography (CT) at the level of the upper right abdomen (A) shows, in sagittal plane, a large rectus sheath hematoma (yellow arrowhead) with hematocrit effect (white arrowhead in axial images B and C).
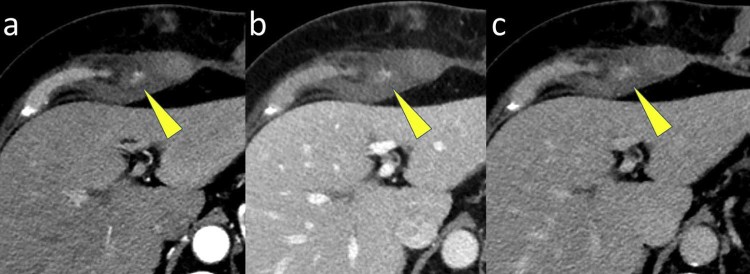
Fig. 2.
Axial images of computed tomography (CT) angiography obtained in the arterial (A), venous (B), and late (C) phases show active bleeding (yellow arrowhead) in superior region of hematoma.
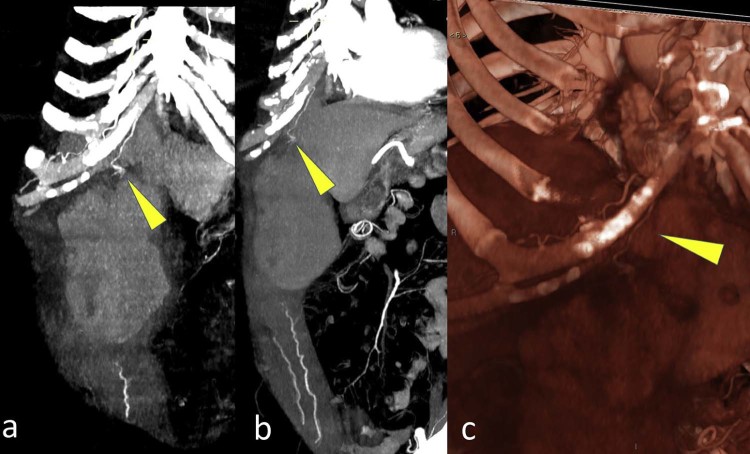
Fig. 3.
Computed tomography (CT) angiography clearly shows arterial jet extravasation (yellow arrowhead) in superior region of hematoma (A and B) originating from a media branch of right superior epigastric artery (volume rendering image in C: yellow arrowhead).
The patient underwent an urgent digital subtraction angiography that confirmed the jet of active bleeding from distal, medial collateral of right superior epigastric artery (Fig. 4); then, the collateral branch was embolized using the axium detachable coil system (Helix ev3). The final digital subtraction angiography control confirmed the complete embolization.
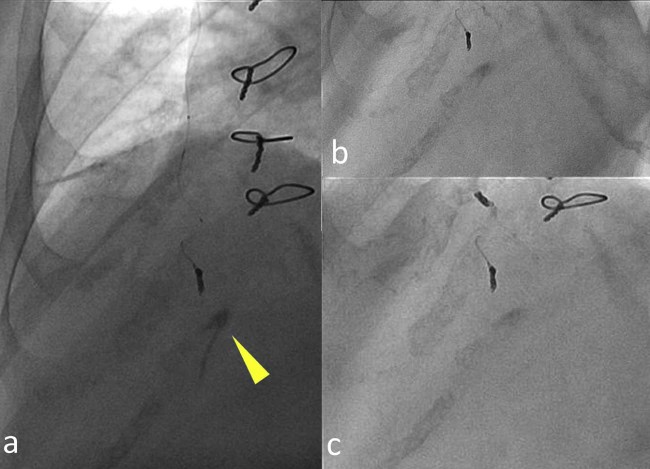
Fig. 4.
Selective angiography before embolization (A) shows the active bleeding (yellow arrowhead) and complete cessation of extravasation after embolization (B and C).
The postoperative course was characterized by the rapid resolution of pain with increased hemoglobin level (10.5 g/dL). Early follow-up showed the absence of clinical complications and the reduction of the hematoma.
Discussion
RSH is a rare condition caused by bleeding into the rectus abdominis muscles; it represents the cause of acute abdominal pain in less than 2% of the cases [1]. RSH development is due to the rupture of the epigastric arteries or caused by direct abdominal trauma or excessively forceful contraction of the rectus abdominis [1].
Several risk factors have been described in the literature: trauma, surgery, anticoagulation, coughing, intense rectus muscle contractions, pregnancy, and various medical conditions (vasculitis or hematologic disorders) [1].
The most common presenting signs or symptoms are abdominal pain, palpable abdominal wall mass, decrease in hemoglobin level, abdominal wall ecchymosis, and peritoneal irritation; less frequently, nausea or vomiting, tachycardia, constipation, dizziness, urinary retention, and abdominal distension have been reported [1], [3].
These various signs or symptoms may result in a wide range of misdiagnoses, such as acute appendicitis, cholecystitis and biliary colic, diverticulitis, strangulated hernia, intestinal obstruction, ovarian torsion, and abdominal aneurysm [1], [4].
An appropriate and early diagnosis has the potential to avoid unnecessary exploratory surgery.
CT is the diagnostic modality of choice for patients with RSH, and it is more accurate than ultrasonography, providing not only more accurate information such as location, size, origin, and extension of the rectus hematoma, but also exclusion of other acute abdominal conditions [1], [3], [4], [5]. In addition, CT angiography is extremely important because it can demonstrate the existence of the active bleeding within the hematoma [6].
Anyway, an evident active bleeding at CT examination is not necessarily related to a clinical severity, and, therefore, should be not considered a stand-alone criterion for invasive treatment. Other clinical severity criteria, such as neurologic deficit, hemodynamic instability, and persistent abdominal pain, must be simultaneously present to proceed with invasive intervention [7].
The more typical unenhanced CT findings are a hyperdense muscular mass (measuring between 60 and 80 Hounsfield units [HU]), a mixed pattern with fluid-fluid levels due to the hematocrit effect, an isodense mass with hypodense areas [4], [8], and a contrast material extravasation on CT angiography [7]. The active arterial bleeding (contrast extravasation) is seen as a focal area of higher density within the hematoma, presenting similar values of the abdominal aorta or major adjacent arteries [8], [9]. Willmann et al. [10], however, reported HU mean values for the active bleeding equal to 115 HU (range: 91-274 HU), significantly lower than those measured over splanchnic arteries (range: 126-315 HU; mean 199 HU), but significantly higher than typical unenhanced, hyperdense, muscular hematomas (range: 28-82 HU; mean 54 HU).
In most rectus hematomas, the management is conservative and typically self-limited as the bleeding tamponades itself [3]. It includes analgesia, intravenous hydration, stopping, and antagonizing of anticoagulants and transfusion [11]. Indications for invasive treatment (surgery or catheter embolization) are persistent bleeding, hemodynamic instability, and neurological deficit [7].
In the past, the most used treatment was surgery with evacuation of hematoma and ligation of bleeding vessels. Presently, the gold standard is the endovascular percutaneous treatment, considered a less invasive alternative [8], [12], [13].
Our case emphasized the need to always perform a CT angiography after an unenhanced CT scan, when a large rectus abdominis muscle hematoma is present in an anticoagulated patient.
In conclusion, the CT angiography examination must be considered necessary for a correct therapeutic pathway in patients with rectus sheath hematoma presenting also severe clinical criteria.
Compliance with Ethical Standards: This study received no funding.
Ethical Approval: All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent: Written informed consent was obtained from the patient for the publication of this report and any accompanying images.
Acknowledgment
We want to dedicate this paper to the memory of our beloved Carmine Laviola, who inspired everyone for his love for science.
Footnotes
Competing Interest: The authors declare that they have no conflict of interest. The authors declare no association with any individual, company, or organization having a vested interest in the subject matter or products mentioned in this article.
References
- 1.Hatjipetrou A., Anyfantakis D., Kastanakis M. Rectus sheath hematoma: a review of the literature. Int J Surg. 2015;13:267–271. doi: 10.1016/j.ijsu.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 2.Fitzgerald J.E., Fitzgerald L.A., Anderson F.E., Acheson A.G. The changing nature of rectus sheath haematoma: case series and literature review. Int J Surg. 2009;7(2):150–154. doi: 10.1016/j.ijsu.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Cherry W.B., Mueller P.S. Rectus sheath hematoma: review of 126 cases at a single institution. Medicine (Baltimore) 2006;85(2):105–110. doi: 10.1097/01.md.0000216818.13067.5a. [DOI] [PubMed] [Google Scholar]
- 4.Berná J.D., Zuazu I., Madrigal M., García-Medina V., Fernández C., Guirado F. Conservative treatment of large rectus sheath hematoma in patients undergoing anticoagulant therapy. Abdom Imaging. 2000;25(3):230–234. doi: 10.1007/s002610000007. [DOI] [PubMed] [Google Scholar]
- 5.Salemis N.S., Gourgiotis S., Karalis G. Diagnostic evaluation and management of patients with rectus sheath hematoma. A retrospective study. Int J Surg. 2010;8(4):290–293. doi: 10.1016/j.ijsu.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Rimola J., Perendreu J., Falcó J., Fortuño J.R., Massuet A., Branera J. Percutaneous arterial embolization in the management of rectus sheath hematoma. AJR Am J Roentgenol. 2007;188(6):W497–W502. doi: 10.2214/AJR.06.0861. [DOI] [PubMed] [Google Scholar]
- 7.Landecy M., Paquette B., Revel L., Behr J., Badet N., Delabrousse E. Does IV contrast extravasation on CT in anticoagulant-related rectus sheath and iliopsoas hematoma predict hematoma expansion and patient outcomes? Abdom Radiol (NY) 2016;41(11):2241–2247. doi: 10.1007/s00261-016-0818-4. [DOI] [PubMed] [Google Scholar]
- 8.Zissin R., Gayer G., Kots E., Ellis M., Bartal G., Griton I. Transcatheter arterial embolisation in anticoagulant-related haematoma—a current therapeutic option: a report of four patients and review of the literature. Int J Clin Pract. 2007;61(8):1321–1327. doi: 10.1111/j.1742-1241.2006.01207.x. [DOI] [PubMed] [Google Scholar]
- 9.Jeffrey R.B., Jr, Cardoza J.D., Olcott E.W. Detection of active intraabdominal arterial hemorrhage: value of dynamic contrast-enhanced CT. AJR Am J Roentgenol. 1991;156:725–729. doi: 10.2214/ajr.156.4.2003435. [DOI] [PubMed] [Google Scholar]
- 10.Willmann J.K., Roos J.E., Platz A., Pfammatter T., Hilfiker P.R., Marincek B. Multidetector CT: detection of active hemorrhage in patients with blunt abdominal trauma. AJR Am J Roentgenol. 2002;179:437–444. doi: 10.2214/ajr.179.2.1790437. [DOI] [PubMed] [Google Scholar]
- 11.Valdez G., Smalligan R. Clinical images: spontaneous rectus sheath hematoma. CMAJ. 2010;182:E20. doi: 10.1503/cmaj.081751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torcia P., Rossi U.G., Squarza S., Cariati M. Spontaneous hematoma of the rectus sheath: urgent embolization with Squidperi liquid embolic device. Case Rep Radiol. 2017;2017 doi: 10.1155/2017/3420313. 3420313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Magill S.T., del Prado G., Chiovaro J. Embolization of hemorrhaging rectus sheath hematoma. J Gen Intern Med. 2014;29(2):408–409. doi: 10.1007/s11606-013-2579-x. [DOI] [PMC free article] [PubMed] [Google Scholar]