Abstract
Non-invasive methods for assessing fracture healing are crucial for biomedical engineers. An approach based on mechanical vibrations was tried out in the 1990s, but was soon abandoned due to insufficiently advanced technologies. The same approach is re-proposed in the present study in order to monitor the healing process of a lengthened femur with an external fixator. The pins screwed into the bone were exploited for the impact testing (IT) to excite the bone and capture its response. Transmission through the soft tissues was thus prevented, and the quality of the signals was improved. Impact tests were performed every three to four weeks for five months. Unfortunately, after seven weeks, some pins were removed due to infection, and thus, the system was modified. Two different configurations were considered: before and after pin removal. An additional configuration was examined in the last two sessions, when the fixator body was removed, while four pins were left in the femur. The evolution of the frequency response function and of the resonant frequencies of the system were analysed for the duration of the monitoring period. The IT results were compared to the indications provided by X-ray images. During the evolution of the callus from the soft phase to the woven bone, the resonant frequencies of the system were found to increase by approximately 2–3% per week. The largest increase (approx. 22%) was observed for the first resonant frequency. After formation of the woven bone, the vibratory response remained almost the same, suggesting that the healing assessment could be related to the relative variation in the resonant frequencies. The results presented support the application of the IT approach for fracture healing assessment.
Keywords: biomechanics, vibration analysis, fracture healing, non-invasive monitoring, external fixation, bone lengthening
1. Introduction
Bone fracture healing is currently assessed using radiographic images and manipulation. It is dependent on the operator's experience and exposes the patient to unhealthy radiation doses that cannot be repeated as often as would be desirable. Alternative diagnostic tools to accurately and safely monitor the status of the fracture are strongly needed. In the 1990s, the impact testing (IT) approach was proposed as a non-invasive and quantitative method to assess bone healing. The idea behind this approach is that, as the bone heals, it gets stiffer and stiffer, and its resonant frequencies increase. The first in vivo applications of the IT approach can be found in [1–3]. Despite the promising results, the method was soon abandoned and never transferred into clinical practice, probably because of technical limitations and difficulties related to the damping caused by soft tissues.
Technological progress along with the development of novel and fast algorithms for vibrational data processing has renewed the interest in this approach. The present authors applied the IT method for assessing fracture healing in [4–6], focusing on cases treated with external fixators. These cases were chosen for two reasons: first, when external fixators are used, healing monitoring is crucial in order to identify a safe time for dynamizing and removing the device. Secondly, the presence of pins screwed into the bone overcomes the problem of tissue damping, both for bone excitation and vibratory response measurements.
A wide campaign of in vitro tests on a tibia phantom with an external fixator was initially carried out to outline the IT procedure and to prove the feasibility of the method [4,5]. More recently, the proposed procedure was used to monitor the healing of a patient treated with an external fixator [6]. The patient had a four-part right leg fracture caused by a motorcycle crash, with an exposed tibia. After several surgical interventions and other complications, such as osteomyelitis, the fracture was stabilized with an Xcaliber Meta-Diaphyseal External Fixator (Orhofix®). The healing process was monitored for three months through a series of five impact tests. In fact, an increase in the first resonant frequencies was observed, of up to 4% per week.
The aim of the present study was to evaluate the IT approach further as a future option for non-invasive healing monitoring. The IT procedure was used to monitor the healing of a fracture aimed at lengthening a femur and treated with an external fixator. Impact tests were performed throughout the consolidation phase of the limb lengthening: from the end of the distraction procedure to the bone remodelling phase, after the removal of the fixator.
2. Material and methods
2.1. Case study
The case study was a 19-year-old female, who had undergone a paediatric femoral fracture, on the right side. The fracture healed with a malunion that left the shaft with 25° of varus deformity and 25° of procurvatum. Overall, the right limb appeared to be 40 mm shorter than the left leg. Consequently, a correction of the bone deformity was performed using a biplanar closed wedge osteotomy, followed by the application of a carbon monoaxial external fixator (LRS Orthofix®). Ten days after the intervention, the patient started the lengthening procedure, 1 mm d−1 for 24 days. Initially, the fixator was assembled using six pins (OsteoTite Bone Screws, Orthofix®), although two of them were removed after about two months because of infection and halisteresis. The fixator body was removed after four months, while the pins were left for an additional month in case of reoperation.
The patient gave informed consent to this research.
2.2. Test set-up and procedure
The experimental set-up and procedure described in our previous papers [4–6] were adopted in this study. Some basic concepts regarding the IT approach are reported in the appendix, while for a deeper understanding see the notes by Avitabile [7].
Impact excitation was performed using an instrumented microhammer (5800SL, Dytran®), while vibrations were measured through three accelerometers, two of which were uniaxial (4507, Brüel & Kjær®) and one triaxial (3133A1, Dytran®). It should be noted that the impact level was less than 0.1 N, and thus, the procedure was not harmful for the patient. Data were acquired and processed using LMS® hardware (LMS Scadas mobile 01) and software (LMS Test.Lab). Signals were acquired in the bandwidth 0–4096 Hz, with a frequency resolution of 2 Hz, and each measurement was obtained by averaging 10 trials. The resonant frequencies (frequency analysis) were identified using the PolyMAX Plus algorithm available in the Modal Analysis package of Test.Lab. Based on previous results, only the frequencies within the bandwidth 0–1000 Hz were estimated.
2.3. Test plan
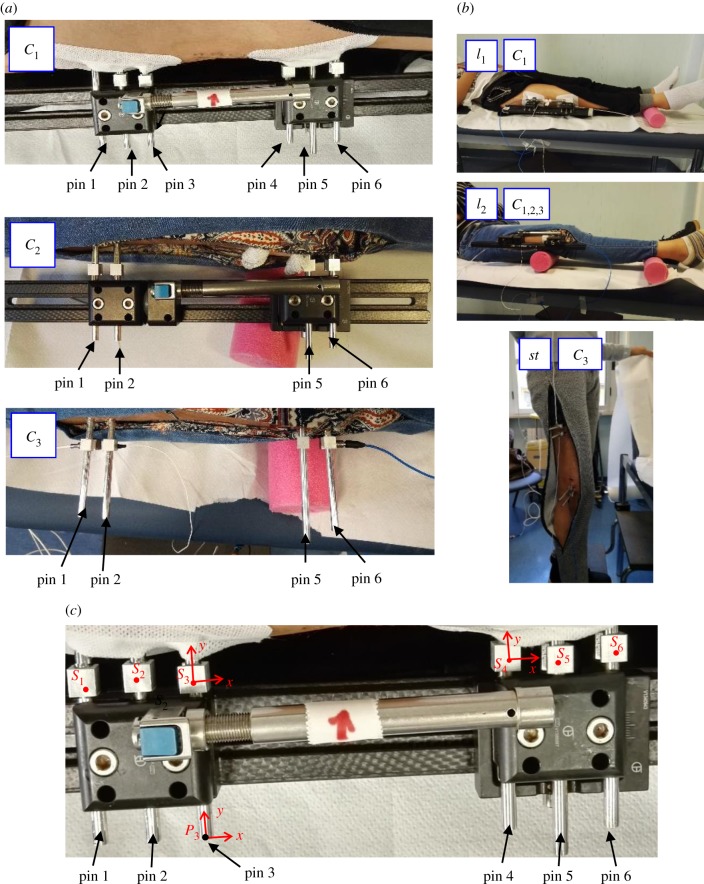
Fracture healing was monitored every three to four weeks from the end of the distraction phase, considering the time-zero, to the fixator and pin removal (after approx. five months), for a total of six sessions (table 1). During the monitoring period, some changes were made to the fixation system, and thus, three different configurations were studied (figure 1a):
— C1, with fixator and six pins, used in the first three sessions, at weeks 0, 4 and 7;
— C2, with fixator and four pins, used in sessions 4 and 5, at weeks 13 and 16;
— C3, with pins only, used in sessions 5 and 6, at weeks 16 and 20.
Table 1.
Test plan: time from the end of the lengthening phase (t), system configuration (config.), boundary conditions (BCs) and input–output points and directions. Sdi and Pdi identify Support and Pin pints, with i = 1–6 corresponding to the pin number and d = x, y, z to the direction. Other symbols are explained in (figure 1).
| session | t (weeks) | config. | BCs | input | output |
|---|---|---|---|---|---|
| 1 | 0 | C1 | l1, l2 |  |
 |
| 2 | 4 | l2 |  |
||
| 3 | 7 | l2 |  |
||
| 4 | 13 | C2 | l2 |  |
 |
| 5 | 16 | l2 |  |
||
| C3 | l2 |  |
|||
| st |  |
||||
| 6 | 20 | l2 |  |
||
| st |  |
Figure 1.
Test configurations C1–3 (a) and boundary conditions l1,2 and st (b). Points and directions used to excite and measure vibrations (c). (Online version in colour.)
Since each configuration corresponded to a different mechanical system with its own vibratory response and resonant frequencies, only results obtained for each specific configuration were compared.
Three different boundary conditions (BCs) for the leg were used during the tests, as shown in figure 1b:
l1 patient lying down with a rubber cylinder under her ankle, used for C1 and C2;
l2 patient lying down with a second rubber cylinder positioned under the knee, used for all configurations;
st patient standing on her healthy leg with the fractured leg freely hanging, used only for C3.
In each test session, several combinations of input/output (IO) points and directions were used, as detailed in figure 1c. Accelerometers were mounted on cubic supports, while the excitation was given both on supports and on pin extremities. Local frames were defined to specify directions, with x almost parallel to the femur axis, y corresponding to the pin axis and z normal to the support face. Support and pin points were labelled, respectively, as  and
and  , with i = 1–6 corresponding to the pin number and d = x, y, z to the direction.
, with i = 1–6 corresponding to the pin number and d = x, y, z to the direction.
3. Results and discussion
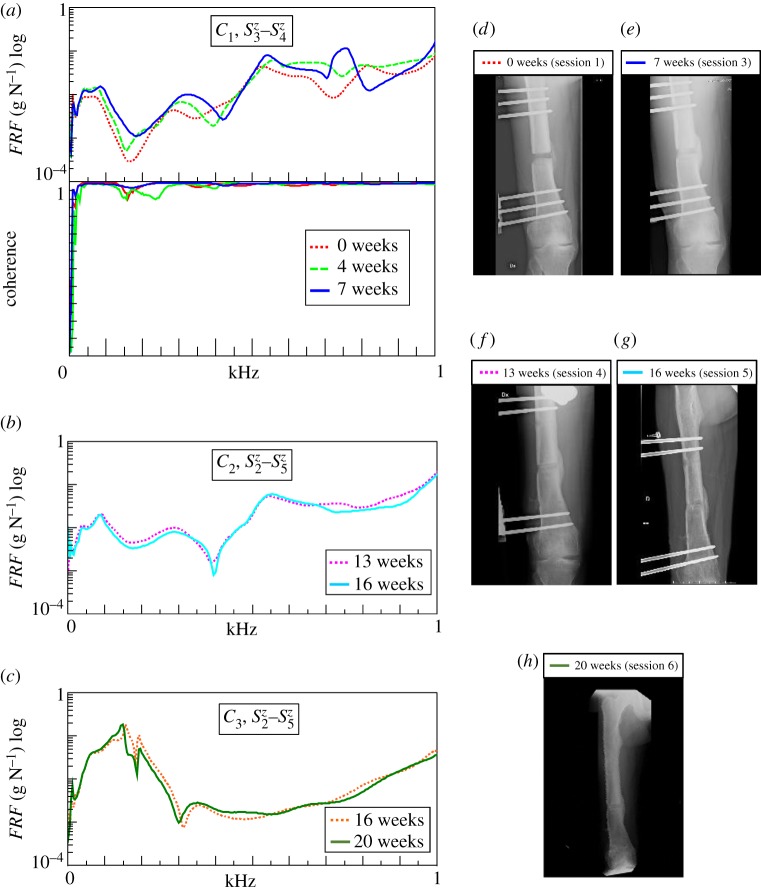
The main results of this study are presented in two ways: the graphical evolution of the frequency response function (FRF) and the numerical estimation of the resonant frequencies, reported in figure 2 and table 2, respectively.
Figure 2.
(a–c) Evolution of FRFs of the fractured femur during healing, both with fixator (a,b) and with only pins (c) (in l2). An example of the coherence functions is also provided at the bottom of (a). (d–h) X-ray images of the fractured femur from the end of bone lengthening (0 week) to the beginning of bone remodelling (20 weeks). (Online version in colour.)
Table 2.
Average values and standard deviations of resonant frequencies of the fractured thigh during healing, evaluated considering all input–output points and directions for each test session. Each column identifies the same vibrational mode for a given configuration.
| t (weeks) | config. | f1 (Hz) | f2 (Hz) | f3 (Hz) | f4 (Hz) | f5 (Hz) | f6 (Hz) |
|---|---|---|---|---|---|---|---|
| 0 | C1 | 75 (2) | 277 (4) | 523 (4) | 689 (4) | 761 (3) | 812 (1) |
| 4 | 80 (2) | 316 (4) | 559 (3) | 726 (4) | 775 (3) | 845 (0) | |
| 7 | 91 (2) | 315 (2) | 538 (1) | 764 (2) | 863 (3) | 954 (3) | |
| 13 | C2 | 89 (1) | 302 (3) | 497 (1) | 538 (2) | 580 (3) | 943 (4) |
| 16 | 89 (1) | 298 (5) | 495 (2) | 545 (2) | 587 (5) | 937 (2) | |
| 16 | C3 | 128 (2) | 155 (1) | 189 (0) | 317 (1) | ||
| 20 | 129 (3) | 151 (1) | 191 (1) | 322 (3) |
The quality of measurements was assessed by verifying the system reciprocity, i.e. the same FRFs by exchanging IO points and directions, and by the goodness of the coherence function, close to unit. For example, the coherence functions obtained for the measurements in configurations C1 are plotted in the bottom of figure 2a.
The effect of the boundary conditions was investigated both with and without the fixator, by comparing results obtained for l1 and l2 and for l2 and st, respectively. The number of rubber cylinders did not affect the results, though l2 BC was more repeatable and comfortable for the patient. On the other hand, the FRFs and the resonant frequencies estimated in the standing and lying-down conditions were slightly different. This was probably due to the muscle contraction required to maintain the standing position. The following results were obtained in l2 BC.
Regarding the choice of IO points and directions, all combinations tested were able to excite most of the vibrational modes of interest. However, a higher number of resonant frequencies was generally achieved when IO points were taken on the pins closest to the fracture. Excitations/responses in the x or y directions did not provide additional information on the healing process with respect to the z direction. The FRFs were thus compared only for IO points on the pins closest to the fracture and with an excitation/response in the z direction, as depicted in figure 2a–c. On the other hand, the resonant frequencies were estimated from all the measurements (i.e. all IO points and directions). Table 2 describes the average values and the standard deviation of the resonant frequencies obtained for each configuration. The columns correspond to the vibrational modes. The standard deviation values ranged in the interval 0–5 Hz, with an average value of 2 Hz, which corresponds to the measurement acquisition resolution, thus confirming the quality of data.
4. Healing monitoring with a complete fixator
Figure 2a shows the FRFs of the complete fixator for configuration C1, obtained from measurements at weeks 0, 4 and 7. The curves are characterized by very similar trends, although they clearly appear to shift towards higher values as the healing process advanced. Only at week 7, did the FRF show a marked large peak at approximately 750 Hz, which was not visible in the previous sessions. This change in the FRF might be due to the combined effect of callus stiffening and mass reduction, as well as to a change in the muscular tone. The frequency analysis identified six frequencies between 0 and 1000 Hz (table 2).
During the first four weeks, all the frequencies increased, the first ones more markedly than the others (2–4% versus less than 1% per week). From weeks 4 to 7, f1, f5 and f6 continued to increase, much more than in the previous period (4–5% per week), while f2 remained constant and f3 decreased by approximately −1% per week. Consequently, f1, f5 and f6, were the best parameters to follow this first phase of the healing. In agreement with Mattei et al. [6], the first resonant frequency was affected by the most significant variations increasing from 75 to 80 Hz and finally 91 Hz (+22%). This estimated evolution of the fracture healing was corroborated by the radiographic images as shown in figure 2d,e: the soft callus visible at week 0 developed in the stiffer woven bone at week 7. The image of week 4 is not shown because it is very similar to the image of week 0. This suggested delayed healing, which finally resulted in prolonged application of the fixator, i.e. approximately 50 days for 1 cm of increase in length instead of the 30–35 usually expected.
Tests performed in configuration C2, at weeks 13–16, produced very similar results, as proved by the FRFs compared in figure 2b corresponding to changes in the resonant frequencies that were lower than 0.3% per week (table 2). The radiographic images in figure 2f,g demonstrated that at week 13, the healing process was advanced, given the presence a mixture of woven bone which became hard callus at week 16, when the fixator was removed. Thus, the results suggest that when the resonant frequency increases reach a steady condition, the bone can be considered healed and thus stiff and strong enough to remove the fixator.
5. Healing monitoring after fixator removal
The FRF of the thigh was also evaluated after fixator body (configuration C3) had been removed at weeks 17 and 20. The completion of the fracture healing was confirmed by almost overlapping curves (figure 2c) and resonant frequencies (table 2). The patient's thigh was characterized by four resonant frequencies in the band 0–1000 Hz: 122, 150, 191 and 321 Hz, at week 7. Only f2 decreased by −3%, i.e. from 156 to 150 Hz, probably as a consequence of a different muscle tone and/or thigh mass. X-ray images at week 20 (figure 2h) showed the callus in the remodelling phase, i.e. towards the development of compact bone. The values of the resonant frequencies in this configuration represent the dynamic behaviour of the thigh, which was also characterized by a damping coefficient (for each one of the frequencies). The values determined by the PolyMAX Plus method for the damping coefficients for f1–4 were 17%, 2%, 2% and 17%, respectively. In agreement with [6], the first mode was the most damped.
6. Conclusion
The present study examined the efficacy of the IT approach as a future option for non-invasive and quantitative healing monitoring. As a case study, the consolidation phase of a femur lengthening procedure was considered. The results showed that the callus evolution from the soft phase to the woven bone affected the resonant frequencies by approximately 2–3% per week, with the largest increase for the first resonant frequency (approx. 22%). After the formation of the woven bone, the vibratory response remained almost the same, suggesting that the healing assessment could be related to the relative variation of the resonant frequencies. The impact level was very low (less than 0.1 N), and thus, the procedure was not harmful for the patient.
Our results support the application of the IT approach to fracture healing assessment. However, further tests are needed in order to prove the reliability of the IT approach in cases of complex fractures and fixator assemblies. In the case presented, the main limitation was due to the removal of the pins, which entails a change to the system and a discontinuity in the monitoring process. This drawback could be limited by performing tests more frequently. On the other hand, the method itself can be used to check the pin–bone interaction, because an anomalous response may be a warning sign of problems such as infections.
An appealing feature of this method is that it could be used through an automatic system, using wearable sensors, which is probably cheaper than other approaches such as three-dimensional tomography (QCT), DEXA or ultrasound.
Acknowledgements
The authors thank Elmira Khoubanfar for her contribution in the experimental activities.
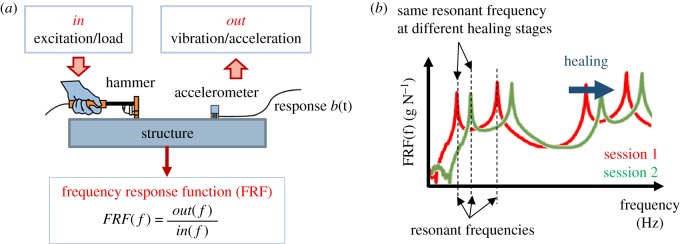
Appendix A. Brief note on experimental modal analysis
The way a structure or a body vibrates can provide important information on its mechanical properties, typically summarized as mass, stiffness and damping. For example, a simple system, composed of a mass (m) and a spring (k), freely vibrates with a frequency f proportional to  . A more complex system is usually characterized by more frequencies, and the way its points move is given by the superposition of harmonic functions at such frequencies. Experimental modal analysis investigates the vibratory response of structures or machines (i.e. bridges, cars and the human body) to determine the way they vibrate, which means frequencies and deformed shapes.
. A more complex system is usually characterized by more frequencies, and the way its points move is given by the superposition of harmonic functions at such frequencies. Experimental modal analysis investigates the vibratory response of structures or machines (i.e. bridges, cars and the human body) to determine the way they vibrate, which means frequencies and deformed shapes.
Figure 3a shows a representation of IT: a structure is excited by an instrumented hammer and its vibratory response is measured by an accelerometer. The input and output signals are acquired and their ratio, in the frequency domain, represents the FRF of the structure. An FRF plot, shown in figure 3b, typically presents peaks at the resonant frequencies. During the healing process, the increase in bone stiffness leads to an increase in the resonant frequencies, with a global translation of FRF towards the high frequencies. In damped structures, such as the leg, FRF peaks are less pronounced. However, the identification of resonant frequencies is usually an automated procedure, based on numerical algorithms that are implemented in most specific laboratory software applications.
Figure 3.
(a) IT procedure and FRF reconstruction. (b) Effect of the bone fracture healing on FRFs: translation of FRF towards high frequencies.
Data accessibility
Experimental data from impact test sessions are available at: https://goo.gl/WwUo4E.
Authors' contributions
F.D.P. and L.M. conceptualized the study and performed the tests. L.M. processed and interpreted the data. F.D.P. supervised the process. S.M. was responsible for the clinical aspects, including X-ray analyses and interpreted correlations between X-rays and vibratory analysis results. L.M. and F.D.P. wrote the manuscript. All the authors read and approved the final manuscript.
Competing interests
We declare we have no competing interests.
Funding
This work was supported by the University of Pisa (PRA 2017).
References
- 1.Tower SS, Beals RK, Duwelius PJ. 1993. Resonant frequency analysis of the tibia as a measure of fracture healing. J. Orthop. Trauma. 7, 552–557. ( 10.1097/00005131-199312000-00011) [DOI] [PubMed] [Google Scholar]
- 2.Cunningham JL, Kenwright J, Kershaw CJ. 1990. Biomechanical measurement of fracture healing. J. Med. Eng. Technol. 14, 92–101. ( 10.3109/03091909009015420) [DOI] [PubMed] [Google Scholar]
- 3.Benirschke SK, Mirels H, Jones D, Tencer AF. 1993. The use of resonant frequency measurements for the noninvasive assessment of mechanical stiffness of the healing tibia. J. Orthop. Trauma 7, 64–71. ( 10.1097/00005131-199302000-00012) [DOI] [PubMed] [Google Scholar]
- 4.Mattei L, Longo A, Di Puccio F, Ciulli E, Marchetti S. 2017. Vibration testing procedures for bone stiffness assessment in fractures treated with external fixation. Ann. Biomed. Eng. 45, 1111–1121. ( 10.1007/s10439-016-1769-1) [DOI] [PubMed] [Google Scholar]
- 5.Di Puccio F, Mattei L, Longo A, Marchetti S. 2017. Fracture healing assessment based on impact testing: in vitro simulation and monitoring of the healing process of a tibial fracture with external fixator. Int. J. Appl. Mech. 9, 1750098 ( 10.1142/S1758825117500983) [DOI] [Google Scholar]
- 6.Mattei L, Di Puccio F, Marchetti S. Submitted. Fracture healing monitoring by impact tests: single case study of a fractured tibia with external fixator. [DOI] [PMC free article] [PubMed]
- 7.Avitabile P.2001. Experimental modal analysis: a simple non-mathematical presentation. Sound and Vibration. See http://www.sandv.com/downloads/0101avit.pdf .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Experimental data from impact test sessions are available at: https://goo.gl/WwUo4E.