Highlights
-
•
A rare case of laparoscopic Roux-en-Y gastric bypass on a patient with situs inversus totalis (SIT).
-
•
SIT is a rare congenital condition, but surgeons in general do encounter those patients throughout their career.
-
•
SIT should not solely be an indication for an open approach as minimally invasive surgery is safe and should still be considered the standard of care.
-
•
Gastric bypass can be safely performed in SIT without the need for major adjustment to the surgeon’s position, trocar placement or instruments used.
Keywords: Situs inversus totalis, SIT, Laparoscopic Roux-en Y gastric bypass, LRYGB, Bariatric surgery, Obesity, Case report
Abstract
Introduction
Laparoscopic Roux-en-Y gastric bypass (LRYGB) has proven over the years to be one of the most effective bariatric procedures. It is highly technical, and therefore is mostly performed by bariatric and metabolic surgeons. Although Situs Inversus Totalis (SIT) is a very rare congenital condition, surgeons do occasionally have to operate intra-abdominally on those patients, consequently facing some challenges related to the unusual anatomy.
Case presentation
We describe a rare case of LRYGB for chronic morbid obesity on a 43 year old patient with pre-operative diagnosis of situs inversus totalis without Kartagener’s syndrome, using slight modification from the usual technique based on anatomical correlation without the need to change the surgeon’s position or switching trocar placements as described in previous papers. This could help surgeons in general reduce the potential challenges faced when performing such procedure.
Conclusion
Situs Inversus Totalis is a rare congenital condition, but surgeons in general do encounter those patients throughout their career. This rare condition should not solely be an indication for an open approach as minimally invasive surgery, whether laparoscopic or robotic, is safe and should still be considered the standard of care approach. Bariatric surgery is one of the most technical intra-abdominal procedures mainly due to the patients’ body habitus, different instrumentations used, and the different anastomoses created. Gastric bypass and bariatric surgery in general can be safely performed on patients with SIT without the need for major adjustment to the surgeon’s position, trocar placement or instruments used.
1. Introduction
Situs inversus totalis (SIT) is a rare autosomal recessive condition that is found in about 0.005%–0.02% of the population. It involves complete transposition of intra-abdominal organs (mirror image formation) with the heart located in the right chest cavity (dextrocardia). The majority of SIT patients have no symptoms or complications because the relationship between the organs is not changed. Laparoscopic Roux-en-y gastric bypass (LRYGB) for morbid obesity is one of the most effective bariatric procedures done in the United States and is currently considered the gold standard in bariatric surgery. We report a rare case of LRYGB that was done successfully on a patient with SIT without major changes in the usual operative technique or length of procedure.
2. Case presentation
Our patient is a 43 year old female with known pre-operative diagnosis of situs inversus without Kartagener’s syndrome that was demonstrated on a prior CT of the abdomen and pelvis (Fig. 1). Her dextrocardia was discovered in the past on a chest x-ray (CXR) obtained during a work up for atrial fibrillation (Fig. 2). Pre-operative BMI was 50 kg/m2 and comorbidities included hypertension, Insulin dependent diabetes mellitus, obstructive sleep apnea, dyslipidemia, severe gastro-esophageal reflux disease (GERD) on daily proton pump inhibitor (PPI) therapy and atrial fibrillation on daily Clopidogrel. Patient failed throughout the years to achieve or maintain any significant weight loss despite multiple dietary and exercise attempts. After proper pre-operative workup she was found to be a good candidate for LRYGB. Surgery was performed successfully without significant changes in the usual surgeon and trocar positions or in the operative time and technique.
Fig. 1.
CT scan of the abdomen in our situs inversus totalis (SIT) patient showing the spleen (S) located on the right side, the liver and gallbladder (GB) on the left side.
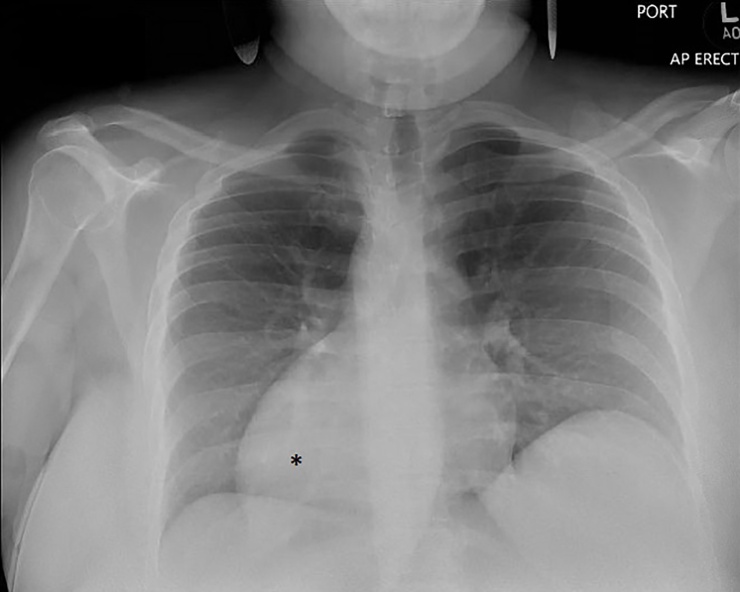
Fig. 2.
CXR in our SIT patient demonstrating dextrocardia *.
In standard setup for LRYGB with normal anatomy we usually place the patient in supine position with arms abducted and the operating surgeon performing the entire procedure standing on the right side of the patient using the dominant right hand when utilizing energy, stapling and free hand suturing.
Having in mind that performing this procedure on SIT patients standing entirely on the left side of the patient, using the non-dominant left hand for most of the technical aspects of the procedure, can be very confusing and challenging we opted to maintain our standard setting and continue to operate from the right side of the patient for the most part of the procedure to minimize any confusion and maintain efficiency. The total number and location of trocars used in our case were similar to that in standard cases with normal anatomy, except that we had to make one of the left sided trocars a 12 mm instead of 5 mm so we can use the stapling device from the left side when creating the gastric pouch. A supra-umbilical (Optiview) trocar was used for entry to the abdominal cavity. Two trocars were placed in the left upper quadrant and left mid-abdomen, and two other trocars in the right upper quadrant and right mid-abdomen. We also used the Nathanson liver retractor via an epigastric incision. The operating surgeon and camera holder were both on the right side of the patient, while the assistant was on the left side. The only part that required the operating surgeon to be on the left side of the patient was during the gastric pouch creation. Upon entering the abdominal cavity, general inspection confirmed the totally reversed anatomy (Fig. 3) with the gallbladder located on the left side of the abdominal cavity, the spleen, angle of His and the greater curvature of the stomach on the right side. After splitting the omentum and retracting the transverse mesocolon cephalad, the ligament of Treitz (LT) was identified. We expected, due to her reversed anatomy that the LT would be located to the right of the midline/falciform ligament, but it was found to be located just to the left of the falciform ligament. In the normal anatomy scenario the LT is located to the left of the midline, and the bilio-pancreatic (BP) limb and jejuno-jejunal (JJ) anastomosis are also located to the left of the falciform ligament alongside the LT while the Roux limb is located opposite to and to the right of the LT, BP limb and the JJ anastomosis. This proper orientation and placement of the Roux limb relative to the LT, BP limb and JJ anastomosis prevents twisting/kinking of the small bowel mesentery of the Roux limb, and facilitates proper closure of Peterson’s defect hence reducing the potential development of an internal hernia. The operating surgeon was able, in our patient, to perform a side to side stapled JJ anastomosis standing on the patient’s right side to minimize technical confusion and maintain a higher level of efficiency. The BP and Roux limb lengths were 50 cm and 150 cm respectively. To ascertain that no twisting of the small bowel mesentery was created, the LT, BP limb and JJ anastomosis were placed on one side; which in this case was just at or slightly to the left of the falciform ligament, and the Roux limb was positioned opposite to these structures and to the right of the falciform ligament (Fig. 4). Next the gastric pouch was created with the operating surgeon on the left side of the patient. We found that using a pediatric colonoscope was very helpful in creating the pouch to make sure it maintained a longitudinal configuration, and to prevent any narrowing near the gastro-esophageal junction (GEJ). Then the gastro-jejunal anastomosis (GJ) anastomosis was created using a 25 mm circular stapler using the trans-oral anvil. This step was performed in the usual manner with the surgeon standing at the patient’s right side. The total operative time was around 180 min. A brief video presentation describing the main parts of the surgery is provided through the link (Video).
Fig. 3.
The gallbladder (GB) is located in the left upper quadrant, and the pylorus (P) in the midline at the level of the falciform ligament.
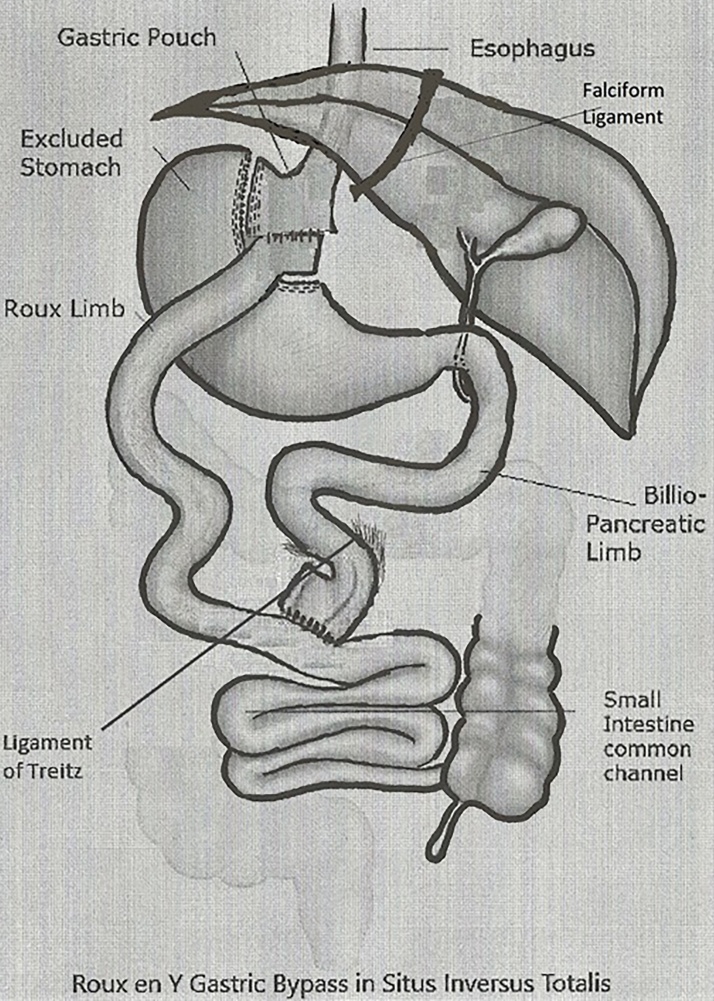
Fig. 4.
Represent the actual anatomy in our patient and the relationship of ligament of Treitz (LT) relative to the falciform ligament (both in midline position), and the corresponding orientation of the Roux limb, the bilio-pancreatic limb and the jejuno-jejunal anastomosis.
Patient did very well postoperatively, and was discharged home on post-operative day two. She is now one year out from surgery; she is completely off of diabetic, anti-hypertensive and cholesterol medications. She is no longer using her CPAP after a sleep study showed resolution of obstructive sleep apnea. Her last HbA1C was below 5% and her BMI is down to 25 kg/m2. She is also off of Clopidogrel, and is only on 81 mg of daily Aspirin.
3. Literature review
3.1. Methods
PubMed, ResearchGate, and Google Scholar search revealed a total of 22 cases of bariatric surgeries performed on patients with Situs Inversus between 1998 and 2017. Data collected from each case included: gender, age, BMI, technique, length of operation, technical difficulties, postoperative course, length of stay and complications. Results listed in (Table 1).
Table 1.
Results of weight loss surgery in patients with SIT. LRYGB: laparoscopic roux en y gastric bypass. LBRYGB: laparoscopic banded roux en y gastric bypass. LAGB: laparoscopic adjustable gastric banding. LSG: laparoscopic sleeve gastrectomy. SILSG: single incision laparoscopic sleeve gastrectomy. DS: duodenal switch. SIPS: stomach intestine pylorus sparing surgery. RRYGB: robotic assisted roux en y gastric bypass. MGB: mini gastric bypass (single anastomosis gastric bypass, or Omega loop gastric bypass).
| Author | Year | BMI | Surgery | Gender | Age | Complications |
|---|---|---|---|---|---|---|
| Wittgrove [1] | 1998 | 47.8 | LRYGB | F | 38 | N/A |
| Ersoy [2] | 2005 | 35 | LAGB | F | 33 | N/A |
| Catheline [3] | 2006 | 76 | LSG | M | 19 | N/A |
| Ahmad [4] | 2006 | 58.1 | LRYGB | F | 47 | N/A |
| Samaan [5] | 2008 | 56 | LAGB | M | 29 | Band erosion |
| Matar [6] | 2008 | 51 | LAGB | M | 28 | N/A |
| Pauli [7] | 2008 | 60 | LAGB | F | 47 | N/A |
| Taskin [8] | 2009 | 54.8 | LAGB | F | 20 | N/A |
| De Barros [9] | 2010 | 40 | LBRYGB | M | 24 | N/A |
| Deutsh [10] | 2012 | 42 | LSG | F | 39 | Staple-line leak |
| Wall [11] | 2013 | 43.4 | RRYGB | M | 58 | N/A |
| Stier [12] | 2014 | 44 | LSG | F | 51 | N/A |
| Stier [12] | 2014 | 44 | LRYGB | M | 39 | N/A |
| Tsepelidis [13] | 2015 | 43 | LRYGB | F | 51 | N/A |
| Nelson [14] | 2015 | 45.3 | LRYGB | F | 43 | N/A |
| Genser [15] | 2015 | 49 | SILSG | F | 52 | N/A |
| Yazar [16] | 2016 | 41.8 | LSG | F | 21 | N/A |
| Watanabe [17] | 2016 | 40.3 | DS | F | 46 | N/A |
| Surve [18] | 2016 | 52.5 | SIPS | F | 31 | N/A |
| Aziret [19] | 2016 | 48 | LSG | F | 54 | N/A |
| Kassir [20] | 2017 | N/A | MGB | N/A | N/A | N/A |
| Salerno [21] | 2017 | 46.4 | LSG | M | 41 | N/A |
4. Results
Fourteen out of twenty one patients (66.6%) were females. The youngest patient was 19 years old [3] and the oldest was 58 years old [11] with median age of 39 years. BMI ranged between 40 and 76 kg/m2 with median BMI of 48 kg/m2. In one case the authors did not provide any demographic data about their patient [20]. Laparoscopic Roux-en-Y gastric bypass (LRYGB) was performed in 5 patients (22.7%) [[1], [4], [12], [13], [14]]; Laparoscopic banded Roux-en-Y gastric bypass (LBRYGB) in one patient [9]; Robotic assisted RYGB (RRYGB) in one patient [11]; and laparoscopic adjustable gastric banding (LAGB) in 5 patients [[2], [5], [6], [7], [8]]. Laparoscopic sleeve gastrectomy (LSG) was performed in 7 patients [[3], [10], [12], [15], [16], [19], [21]]; modified duodenal switch (LSG + duodeno-jejunal bypass, and stomach-intestine pylorus sparing; SIPS) in two cases [[17], [18]], and there was a single case of Omega loop gastric bypass or mini gastric bypass that was published with a Supplementary video [20].
Complications were documented in 2 cases [[5], [10]]. One case was a staple-line leak after LSG [10], and the second was band erosion through gastric wall after LAGB where the band had to be removed [5].
5. Discussion
Morbid obesity is a serious and devastating disease that can involve nearly every organ system and interferes with basic physical functions such as breathing or walking. Undoubtedly those with morbid obesity are at a significantly greater risk for diseases such as Type II Diabetes Mellitus, Hypertension, Obstructive sleep apnea, gastroesophageal reflux disease (GERD), chronic osteoarthritis, heart diseases, and even cancer. Management of morbid obesity requires a comprehensive multimodality treatment approach that includes but not limited to: diet modification, exercise and lifestyle changes, certain medications and natural supplements, genetic testing (gene polymorphisms, etc.) and psychiatric evaluation and support. Bariatric surgery has demonstrated over the years its ability to offer significant metabolic benefit to those patients when other non-surgical options have failed to provide long-lasting metabolic and weight loss results. (LRYGB) for morbid obesity is one of the most common bariatric procedures done in the United States [14] and is still considered the gold standard in bariatric surgery. Situs inversus totalis is a rare autosomal recessive congenital condition where there is complete transposition of intra-abdominal organs (mirror image formation) with Dextrocardia [4]. On average, it occurs in about one in ten thousand people. Patient with Situs inversus may have primary ciliary dyskinesia or Kartagener’s syndrome. Applying advanced minimally invasive techniques on patients with SIT can potentially pose some technical challenges due to the inversed anatomy, and despite those challenges bariatric surgery has been accomplished successfully and safely. Literature review revealed 22 patients with situs inversus who successfully underwent bariatric surgery (Table.1).
A total of five patients underwent LRYGB [[1], [4], [12], [13], [14]], one had a banded RYGB [9], another patient had a robotic assisted surgery[11], and one patient had an Omega loop or mini gastric bypass [20]. A total of seven patients had LSG [[3], [10], [12], [15], [16], [19], [21]], one patient had a LSG with duodeno-jejunal bypass [17] and another patient had SIPS [18]. Only five patients had LAGB [[2], [5], [6], [7], [8]]. None of the gastric bypass patients developed any complications. Deutsch et al. reported a case of LSG that was complicated with staple line leak [10], while band erosion occurred in the case reported by Samaan et al. [5].
Most reported cases of gastric bypass in SIT patients were performed in a mirror image technique with the operating surgeon standing on the left side of the patient. In some of these cases, the authors mentioned the technical challenges related to changing the routine surgeon’s position and trocar placement. In our patient, her gastric bypass was successfully accomplished without any changes in trocar placement or the operating surgeon’s position except for the gastric pouch creation which required the operating surgeon to be standing on the patient’s left side. By investing the time in identifying her anatomy and the relationship of the Roux limb to the LT, BP limb and JJ anastomosis, we were able to significantly reduce the level of technical difficulty and confusion, and maintain an efficient pace that matches our standard operative time in normal anatomy patients.
Wittgrove [1] was the first author to describe LRYGB in a patient with situs inversus totalis in 1998. He described several technical challenges such as the operating surgeon’s position, using opposite hands when handling the instruments and the opposite foot to operate the foot pedal. He also mentioned that the operative time nearly doubled; 300 mins vs 159 mins. Ahmad et al. [4] described minimal difficulty in performing LRYGB standing exclusively on the patient’s left side. Changing sides did not alter the surgeon’s use of his right hand as previously reported by Wittgrove et al. All intracorporeal suturing was performed with the surgeon’s right hand and the operative time was only slightly longer than his standard time (160 mins vs 105 mins). In 2013 Wall et al. [11] described a case of robotic assisted RYGB in a patient with SIT. The author described the advantage of using the robot compared to traditional laparoscopy where the robot eliminated the need to change the surgeon’s position, trocar placement, or instrument orientation and concluded that robotic assisted Roux-en-Y gastric bypass can be successfully and safely performed in patients with situs inversus. Stier et al. [12] described a successful LRYGB in a SIT patient using the mirror image technique without significant prolongation of the operative time. The author though did not elaborate on the level of technical difficulties. In 2015 Nelson et al. [14] published a case of LRYGB in a patient with SIT. The author described some of the technical difficulties but did not describe the operating surgeon’s position or the operative time.
In May 2017 Kassir et al. [20] published a video of an Omega loop gastric bypass performed in France with the patient placed in the modified lithotomy position and the operating surgeon standing between the patient’s legs. There was no change in their standard operative time, trocar placement or the operating surgeon’s position throughout the surgery. The authors emphasized the advantage of operating in the modified lithotomy position in such cases to minimize technical confusion by enabling the operating surgeon to complete the procedure from the usual position.
Results of LRYGB in SIT are listed in (Table 2).
Table 2.
Results of LRYGB in patients with SIT.
| Author | Year | Age | Gender | Surgeon position | Operation time | Complications |
|---|---|---|---|---|---|---|
| Wittgrove [1] | 1998 | 38 | F | Left side | 300 min | N/A |
| Ahmad [4] | 2006 | 47 | F | Mirror image technique | 160 min | N/A |
| De Barros [9] | 2010 | 24 | M | Not described | 400 min | N/A |
| Wall [11] | 2013 | 58 | M | Robotic assisted | N/A | N/A |
| Stier [12] | 2014 | 39 | M | Mirror image technique | 76 min | N/A |
| Tsepelidis [13] | 2015 | 51 | F | Not described | 120 min | N/A |
| Nelson [14] | 2015 | 43 | F | Not described | N/A | N/A |
| Kassir [20]a | 2017 | N/A | N/A | French position | 90 min | N/A |
This case was a single anastomosis gastric bypass which is known as Omega loop or mini gastric bypass.
6. Conclusion
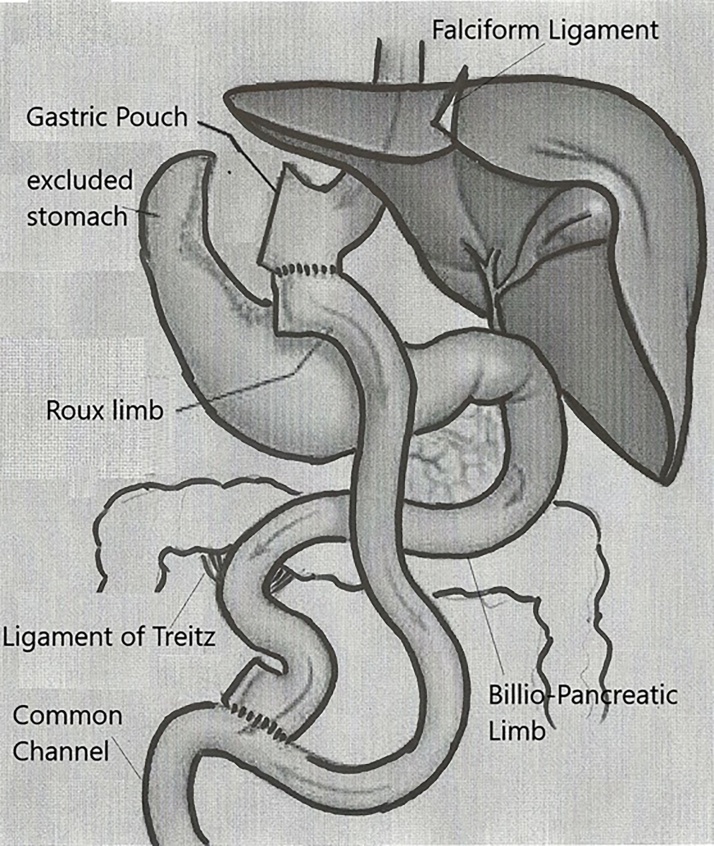
Situs Inversus Totalis is a rare congenital condition, but surgeons in general do encounter those patients throughout their career. This rare condition should not solely be an indication for an open approach as minimally invasive surgery; whether laparoscopic or robotic, is a safe alternative and should still be considered the standard of care approach. Bariatric surgery is one of the most technical intra-abdominal procedures mainly due to the patients’ body habitus, different instrumentations used, and the different anastomoses created. Gastric bypass and bariatric surgery in general can be safely performed in this population without the need for major adjustment to the surgeon’s position, trocar placement or instruments used. Performing this procedure on SIT patients standing entirely on the left side of the patient using the non-dominant left hand for most of the technical aspects of the procedure as described in the literature can be very challenging. In our case, we felt that most of the confusion could occur with the JJ anastomosis and the concern for improper orientation of the Roux limb leading to kinking or twisting of the mesentery. We opted to maintain the same standard technique by performing these steps with the surgeon standing on the right side of the patient. By examining the relationship of the falciform ligament to the LT, and making sure to place the LT, BP limb and JJ anastomosis on one side, and the Roux limb on the opposite side, we were able to easily eliminate factors that could lead to confusion and improper technique. We describe in Fig. 4, Fig. 5 the proper relationship of the Roux limb to the LT, BP limb and JJ anastomosis if the LT was at the level of the falciform ligament (Fig. 4) or to the right of the falciform ligament (Fig. 5). Our goal in this literature review and the figures included is to help reduce any potential technical difficulties or confusion that may face surgeons when planning intra-abdominal procedures that involve the Roux-en-Y configuration whether bariatric surgery related or not.
Fig. 5.
Demonstrates the proper orientation of the Roux limb, the bilio-pancreatic limb and the jejuno-jejunal anastomosis in SIT patients if the LT is located to the right of the falciform ligament (right of the midline).
Conflicts of interest
None.
Funding
None.
Ethical approval
Ethical approval has been exempted by institution for this case.
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent
Written informed consent was obtained from the patient for publication. A copy of the written consents is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Abdelaziz Atwez: Writing the paper, data collection and data analysis.
Zeid Keilani: Study concept and design, proofreading.
Registration of research studies
N/A.
Guarantor
Zeid Keilani.
Footnotes
This work has been reported in line with the SCARE criteria [22].
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.ijscr.2018.03.004.
Contributor Information
Abdelaziz Atwez, Email: Abdelaziz.Atwez@Palmettohealth.org.
Zeid Keilani, Email: zeid.keilani@uscmed.sc.edu.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Wittgrove A.C., Clark G.W. Laparoscopic gastric bypass for morbid obesity in a patient with situs inversus. J. Laparoendosc. Adv. Surg. Tech. A. 1998;8(February (1)):53–55. doi: 10.1089/lap.1998.8.53. [DOI] [PubMed] [Google Scholar]
- 2.Ersoy E., Koksal H., Ege B. Laparoscopic gastric banding for morbid obesity in a patient with situs inversus totalis. Obes. Surg. 2005;15(October (9)):1344–1346. doi: 10.1381/096089205774512591. [DOI] [PubMed] [Google Scholar]
- 3.Catheline J.M., Rosales C., Cohen R., Bihan H., Fournier J.L., Roussel J., Bénichou J. Laparoscopic sleeve gastrectomy for a super-super-obese patient with situs inversus totalis. Obes. Surg. 2006;16(August (8)):1092–1095. doi: 10.1381/096089206778026352. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed A.R., O'malley W. Laparoscopic Roux-en-Y gastric bypass in a patient with situs inversus. Obes. Surg. 2006;16(October (10)):1392–1394. doi: 10.1381/096089206778663670. [DOI] [PubMed] [Google Scholar]
- 5.Samaan M., Ratnasingham A., Pittathankal A., Hashemi M. Laparoscopic adjustable gastric banding for morbid obesity in a patient with situs inversus totalis. Obes. Surg. 2008;18(July (7)):898–901. doi: 10.1007/s11695-008-9445-7. [DOI] [PubMed] [Google Scholar]
- 6.Matar Z.S. Laparoscopic adjustable gastric banding in a morbidly obese patient with situs inversus totalis. Obes. Surg. 2008;18(December (12)):1632–1635. doi: 10.1007/s11695-008-9546-3. [DOI] [PubMed] [Google Scholar]
- 7.Pauli E.M., Wadiwala I.I., Rogers A.M. Laparoscopic placement of an adjustable gastric band in a super–super obese patient with situs inversus. Surg. Obes. Relat. Dis. 2008;4(November–December (6)):768–769. doi: 10.1016/j.soard.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 8.Taskin M., Zengin K., Ozben V. Concomitant laparoscopic adjustable gastric banding and laparoscopic cholecystectomy in a super-obese patient with situs inversus totalis who previously underwent intragastric balloon placement. Obes. Surg. 2009;19(December (12)):1724–1726. doi: 10.1007/s11695-008-9725-2. [DOI] [PubMed] [Google Scholar]
- 9.De Barros C.J., Rapoport A., de Andrade Sobrinho J., Dedivitis R.A., Grill E.H. The gastric bypass banding for morbid obesity in a patient with situs inversus. Rev. Col. Bras. Cir. 2010;37(April (2)):157–158. doi: 10.1590/s0100-69912010000200014. [DOI] [PubMed] [Google Scholar]
- 10.Deutsch G.B., Gunabushanam V., Mishra N., Sathyanarayana S.A., Kamath V., Buchin D. Laparoscopic vertical sleeve gastrectomy after open gastric banding in a patient with situs inversus totalis. J. Minim. Access. Surg. 2012;8(July (3)):93–96. doi: 10.4103/0972-9941.97595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wall A., Feng Z., Melvin W. Robotic-assisted Roux-en-Y gastric bypass in a patient with situs inversus. J. Robotic Surg. 2014;8:169–171. doi: 10.1007/s11701-013-0402-7. [DOI] [PubMed] [Google Scholar]
- 12.Stier C., El-Sayes I., Theodoridou S. Are laparoscopic bariatric procedures feasible in morbidly obese patients with situs inversus? A report of 2 cases and a brief review. Surg. Obes. Relat. Dis. 2014;10(November–December (6)):e53–e56. doi: 10.1016/j.soard.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Tsepelidis D., Loi P., Katsanos G., Closset J. Gastric Bypass for Morbid Obesity in a Patient with Situs Inversus Totalis. Acta Chir. Belg. 2015;115(January (1)):81–82. [PubMed] [Google Scholar]
- 14.Nelson L., Teixeira A.F., Jawad M.A. Laparoscopic Roux-en-Y gastric bypass in a patient with situs inversus. Surg. Obes. Relat. Dis. 2016;12(March–April (3)):711–713. doi: 10.1016/j.soard.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Genser L., Tayar C., Eddine I.K. Trans-umbilical single ıncision laparoscopic sleeve gastrectomy in a patient with situs ınversus totalis and kartagener syndrome: video report. Obes. Surg. 2015;25(October (10)):1985–1986. doi: 10.1007/s11695-015-1820-6. [DOI] [PubMed] [Google Scholar]
- 16.Yazar F.M., Emre A., Akbulut S., Urfalıoğlu A., Cengiz E., Sertkaya M., Yıldız H., Bülbüloğlu E. Laparoscopic sleeve gastrectomy in situs inversus totalis: a case report and comprehensive literature review. Indian J. Surg. 2016;78(April (2)):130–135. doi: 10.1007/s12262-015-1437-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watanabe A., Seki Y., Kasama K. Laparoscopic sleeve gastrectomy with duodeno-jejunal bypass for morbid obesity in a patient with situs inversus totalis. Asian J. Endosc. Surg. 2016;9(August (3)):218–221. doi: 10.1111/ases.12285. [DOI] [PubMed] [Google Scholar]
- 18.Surve A., Zaveri H., Cottam D., Richards C., Medlin W., Cottam A. Laparoscopic stomach intestinal pylorus sparing surgery in a patient with morbid obesity and situs inversus: first video case report. Surg. Obes. Relat. Dis. 2017;13(January (1)):122–124. doi: 10.1016/j.soard.2016.08.503. [DOI] [PubMed] [Google Scholar]
- 19.Aziret M., Karaman K., Ercan M., Bostancı E.B., Akoğlu M. Laparoscopic sleeve gastrectomy on a morbidly obese patient with situs inversus totalis: a case study and systematic review of the literature. Obes. Res. Clin. Pract. 2017;11(September–October (5S1)):144–151. doi: 10.1016/j.orcp.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 20.Kassir R., Mourthadhoi F., Tiffet O., Lointier P. How do I do a laparoscopic one-anastomosis gastric bypass in a patient with situs inversus totalis. Obes. Surg. 2017;27(August (8)):2218–2219. doi: 10.1007/s11695-017-2761-z. [DOI] [PubMed] [Google Scholar]
- 21.Salerno A., Trotta M., Sarra G., D'Alessandro G., Marinari G.M. Laparoscopic sleeve gastrectomy in a patient with situs viscerum inversus totalis: is the life easy upside-down? Surg. Endosc. 2017;(August (4)) doi: 10.1007/s00464-017-5734-3. [DOI] [PubMed] [Google Scholar]
- 22.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.