Highlights
-
•
Rapunzel syndrome is a rare condition in which gastric trichobezoar extends beyond the pylorus and into small intestine.
-
•
Diagnosis is by ultrasound, upper gastrointestinal series, CT scan and upper gastrointestinal endoscopy.
-
•
The trichobezoar mass can be removed via laparotomy(gastrotomy and enterotomy) or endoscopic approach.
-
•
long-term follow-up with surgical and psychiatric consultation is recommended to prevent recurrences.
Keywords: Rapunzel syndrome, Trichobezoar, Trichophagia, Recurrence
Abstract
Introduction
Rapunzel syndrome is a rare condition predominantly found in trichophagic females that occurs when gastric trichobezoar extends beyond the pylorus and into duodenum, jejunum, ileum or even to colon. There are only five cases reported in literature. This case report has been reported in line with the SCARE criteria.
Presentation of case
A 19 year old female, with a history of trichotillomania with trichophagia, who presented with epigastric pain and vomiting for 12 months. She underwent laparotomy ten years back to extract a trichobezoar, which was diagnosed to be Rapunzel syndrome and lack of follow-up resulted in recurrence. Further examination and imaging showed a large trichobezoar extending into small intestine. She underwent gastrotomy and entrerotomy and extraction of hairball.
Discussion
In a trichophagic female with abdominal pain, nausea and vomiting, and abdominal mass, diagnosis is done by ultrasound, CT scan and upper gastrointestinal endoscopy. Small trichobezoars can be removed endoscopically. Large (>20 cms)acutely symptomatic trichobezoars, especially when accompanied by Rapunzel syndrome, must be removed surgically by gastrotomy and enterotomy is required if impacted extension is present. Long-term surgical and psychiatric follow-up with psychotherapy and cognitive behavioural therapy along with selective serotonin reuptake inhibitors are critical to prevent recurrences.
Conclusion
Although Rapunzel syndrome is an extremely rare disease, it should be considered when diagnosing young women, especially those with a history of trichophagia or trichotillomania. After the surgical removal of trichobezoars by laparotomy, long-term follow-up combined with psychiatric consultation is recommended to prevent recurrences.
1. Introduction
Bezoars are concretions of foreign and intrinsic material in the gastrointestinal tract. The term Bezoars is thought to be derived from the Arabic word “Badzehr” or the Persian word “Padzhar,” which mean “antidote” [2]. Trichobezoars are hairballs or hair-like fibers formed by chewing and swallowing hair or any other indigestible materials. Trichobezoars usually form in the gastric body and are thus prepyloric The first report of Rapunzel syndrome dates back to 1968, when Vaughan described a patient with this disease [1] and this was named after a fairy tale written in 1812 by Brothers Grimm’s about the German princess Rapunzel who let her long golden hair down from her prison tower to permit her young prince to climb up to her window and rescue her [3]. Recurrence of this condition is extremely rare and only around five cases have been reported. We report another case which presented to our institution. This case report has been reported in line with the SCARE criteria [15].
2. Presentation of case
A 19-year-old girl of normal intelligence presented with 12 months of dull aching upper abdominal pain with non-bilious vomiting and loss of appetite. Patient had undergone laparotomy for trichobezoar 10 years back in 2008. It was diagnosed as Rapunzel syndrome as trichobezoar was extending into small intestine (Fig. 1a and b. Patient was on psychiatric followup, but they missed follow-ups for last two years. Personal history revealed trichophagia.
Fig. 1.
(a) Trichobezoar being extracted at first laparotomy. (b) Trichobezoar extracted by first laparotomy.
The girl was 155 cm tall and weighed only 43 kg. On examination she looked pale and a little depressed. She had no patchy alopecia or halitosis. Vital signs were Stable. Physical examination revealed a firm, non-tender, solid palpable mass over the epigastric region; however, there were no signs of peritonitis or obstruction.
Complete blood workup revealed normocytic hypochromic anemia, with a hemoglobin content of 9.1 gm/dL. Blood sugar, Renal Function Tests, Liver function tests, serum electrolytes, urine analysis and serum amylase results were normal. Chest radiograph, X-ray Abdomen, ECG and 2D ECHO were normal.
Barium meal study revealed a large filling defect in the stomach that was suggestive of bezoars (Fig. 2). Ultrasonography of abdomen revealed a large intraluminal mass in stomach.
Fig. 2.
Barium meal image showing filling defect.
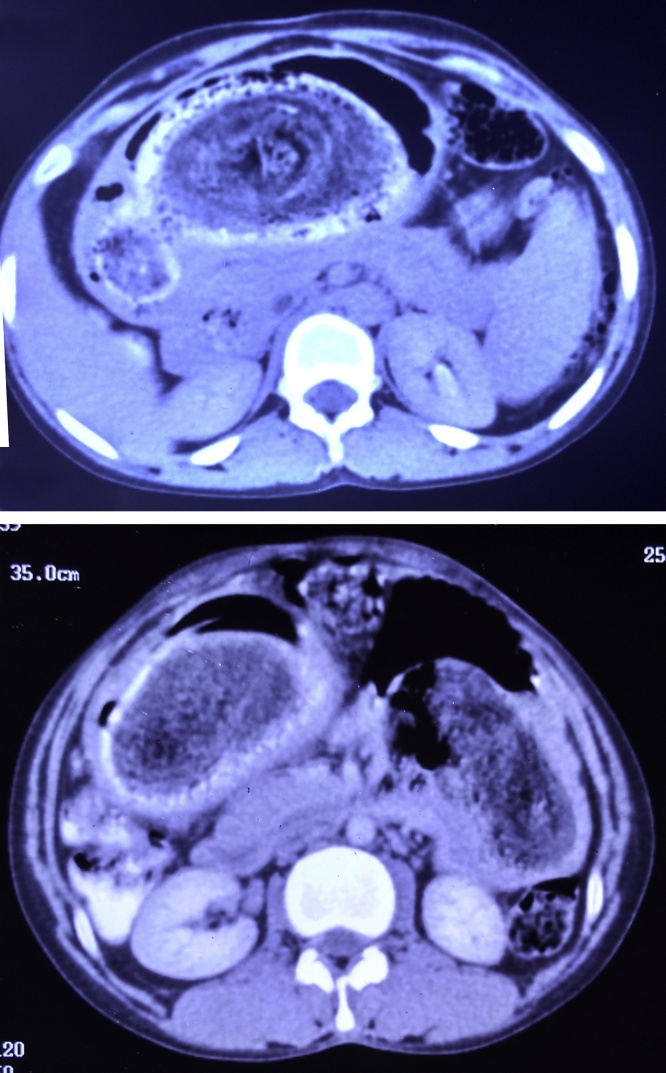
A computed tomography (CT) scan demonstrated well defined heterogeneous, iso to hypodense cast-like mass with peripheral contrast opacification, mainly in body and pyloric region also extending to the duodenum and also in jejunum with focal dilatation of jejunal loops in left lumbar region. (Fig. 3). An upper gastrointestinal endoscopy revealed a giant gastric trichobezoar. Gastric mucosa appeared normal without evidence of ulceration.
Fig. 3.
CT scan of the abdomen demonstrated a trichobezoar in the stomach that extended into the duodenum and jejunum.
Due to the bulky size of the trichobezoar, the patient underwent exploratory laparotomy. The stomach was completely filled by the large trichobezoar, and a long tail extended through pylorus and duodenum into upper parts of jejunum. Thus, the diagnosis of Rapunzel syndrome was confirmed. The trichobezoar mass was removed via anterior gastrotomy and enterotomy incisions (Fig. 4a and b). There was no evidence of gastric necrosis or intraperitoneal infection. The total length of the trichobezoar was approximately 40 cm* 22 cm* 10 cm, with a weight of 1300 g (Fig. 5) and was a perfect cast of stomach, pylorus, duodenum and proximal jejunum. Abdominal cavity was closed after two layerd closure of gastrotomy and enterotomy.
Fig. 4.
(a) The trichobezoar being extracted by gastrotomy. (b) The trichobezoar being extracted by enterotomy.
Fig. 5.
Stomach shaped trichobezoar with tapering tail extending into duodenum and jejunum specimen extracted by second laparotomy.
The postoperative course was uneventful. Oral dietary intake was started after 48 h of surgery and sutures were removed on Day 10. Patient was referred to psychiatrist and started on Table Fluoxetine and behavioural therapy which was cornerstone to prevent recurrence. The patient was discharged on day 12 after surgery. Patient is being followed up by surgical and psychiatric team and patient is doing fine.
3. Discussion
There are six types of bezoars described according to their composition: trichobezoars, phytobezoars, lactobezoars, lithobezoars, pharmacobezoars and plasticobezoars.
For the diagnosis of Rapunzel syndrome, a history of eating hair is essential. Only 1% patients with trichophagia presents with a trichobezoar. These disorders are often the result of psychological problems, family discord, childhood neglect or abuse or mental retardation [4]. Hairstrands are retained in gastric mucosa, peristalsis causes these to become enmeshed until a ball is formed that is too large to leave the stomach causing gastric atony. In this case, the parents of the patient indicated that the patient had exhibited a habit of playing with hair since childhood, and she would sometimes pick up hair and chew, which likely lead to swallowing.This condition occurs most commonly in females under the age of 30, youngest being a six month old infant. Our patient was nine years old at initial detection and 19years old when recurrent Rapunzel syndrome was confirmed.
Patients with Rapunzel syndrome presents with abdominal pain (37%), nausea and vomiting (33.3%), abdominal mass, diarrhoea or constipation, weight loss (7.4%), anorexia, anemia and jaundice. Complications include gastrointestinal obstruction (25.9%), peritonitis and perforation (18.3%), gastrointestinal bleeding(10%) intussusceptions (7.4%), pancreaticobiliary obstruction, pancreatitis and malabsorption complications like protein-losing enteropathy and iron deficiency and megaloblastic anemia [5]. In our case, the patient presented with trichophagia since the age of 8 years, while the main symptoms leading to the patient’s hospitalization were abdominal pain and intermittent vomiting. As the proteins of follicles denature by acid contents of stomach, they discolour, turning black or brown, and an unpleasant odour seems to be emitted due to decomposition and fermentation of fats [6]. If bezoars are left without treatment, the mortality rate can reach 30%.
Abdominal imaging examinations include plain film, ultrasound, upper gastrointestinal series, and CT scan, while the final diagnosis should be made via upper gastrointestinal endoscopy [7]. Ultrasound may demonstrate a band of increased echogenicity caused by the intermixed hair, air, and food in the trichobezoar is diagnostic. Detection rate of trichobezoars by USG has been reported to be around 88% [8].
An upper gastrointestinal series can demonstrate a filling defect in the stomach, while CT scan demonstrates heterogeneous masses containing trapped air bubbles or homogenous mottled appearance in the region of stomach or intestines [8]. Upper gastrointestinal endoscopy is considered to be the gold standard for the diagnosis of trichobezoar, but it may not prove the presence of a co-existing Rapunzel syndrome [9]. However, if Rapunzel syndrome is considered a possibility, a barium meal is not recommended because it may lead to obstruction or perforation. We made the current diagnosis based on the patient’s history, clinical examination, upper gastro-intestinal endoscopy and radiological imaging studies.
Treatment depends on the size of the trichobezoars and their location. Small trichobezoars can be removed endoscopically [10]. However, a recent study by Gorter et al. showed that endoscopic removal of trichobezoars was successful in only approximately 5% of patients [11]. Laparoscopic approach is advocated only for appropriate patients(small to moderate sized bezoars) due to increased operating time, the added risk of intra-abdominal spillage of the trichobezoar contents, and the necessity of extended incisions. Thus, large (>20cms) symptomatic trichobezoars, especially when accompanied by Rapunzel syndrome, must be removed surgically by laparotomy. Enzymatic dissolution(by papain syrup, pancreatic lipase, and cellulose), Nd-YaG laser and extracorporeal shock wave fragmentation are novel approaches that have to be evaluated [12].
Although the recurrence of Rapunzel syndrome is extremely rare, there is no doubt that the prevention of recurrence is critical. The most common reason for recurrence is patients lost in follow-up. Long-term surgical follow-up with upper GI endoscopy or USG abdomen [13] and psychiatric follow-up with psychotherapy and cognitive behavioural therapy along with selective serotonin reuptake inhibitors are critical after the surgical removal of trichobezoars to prevent recurrences [14].
4. Conclusion
Although recurrencr of Rapunzel syndrome is extremely rare, it should be considered when diagnosing young women, especially those with a history of trichophagia or trichotillomania. After diagnosing with endoscopy and imaging studies, surgical removal of trichobezoars by laparotomy and long-term follow-up combined with psychiatric consultation is recommended to prevent recurrences.
Conflicts of interest
None. There are no financial or personal relationship with other people or organisations for any of the authors who had contributed for the study.
Sources of funding
None. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Ethical approval
Ethical committee approval has been exempted by our institution as this is a case report.
Consent
Available upon request. Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request
Author contribution
Antony Nettikadan – Author, assisted the surgery and in management of the patient, Data collection and interpretation, wrote the manuscript, corresponding author.
Ravi M J – Author, Managed the patient and did the surgery, helped in drafting the manuscript.
M Shivaprasad – Author, Totally supervised this case report and management of the patient.
All authors read and approved the final manuscript.
Guarantor
Antony Nettikadan and M Shivaprasad.
References
- 1.Vaughan E.D., Jr, Sawyers J.L., Scott H.W., Jr The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery. 1968;63:339–343. https://www.ncbi.nlm.nih.gov/pubmed/5638179 [PubMed] [Google Scholar]
- 2.Rabie M.E., Arishi A.R., Khan A., et al. Rapunzel syndrome: the unsuspected culprit. World J. Gastroenterol. 2008;14:1141–1143. doi: 10.3748/wjg.14.1141. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2689422/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grimm Brothers:. Rapunzel. Translated by Godwin-Jones R. Richmond, Virginia Commonwealth University Department of Foreign Languages. 1994–1999. www.oalib.com/references/14387817.
- 4.Grant J.E., Odlauq B.L. Clinical characteristics of trichotillomania with trichophagia. Compr. Psychiatry. 2008;49:579–584. doi: 10.1016/j.comppsych.2008.05.002. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2605948/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barzilai M., Peled N., Soudack M., Siplovich L. Trichobezoars. Harefuah. 1998;135:97–101. https://www.ncbi.nlm.nih.gov/pubmed/9885650 [PubMed] [Google Scholar]
- 6.Sharma V., Sahi R.P., Misra N.C. Gastro- Intestinal Bezoars. J. Indian Med. Assoc. 1991;89:338–339. https://www.ncbi.nlm.nih.gov/pubmed/1816314 [PubMed] [Google Scholar]
- 7.Coulter R., Antony M.T., Bhuta P., et al. large gastric trichobezoar in a normal healthy woman: case report and review of pertinent literature. South Med. J. 2005;98:1042–1044. doi: 10.1097/01.smj.0000182175.55032.4a. https://www.ncbi.nlm.nih.gov/pubmed/16295823 [DOI] [PubMed] [Google Scholar]
- 8.Ripolles T., Garcia-Aguayo J., Martinez M.J., Gil P. Gastrointestinal Bezoars: sonographic and CT characteristics. AJR Am. J. Roentgenol. 2001;177:65–69. doi: 10.2214/ajr.177.1.1770065. https://www.ncbi.nlm.nih.gov/pubmed/11418400 [DOI] [PubMed] [Google Scholar]
- 9.Newman B., Girdany B.R. Gastric trichobezoars – sonographic and computed tomographic appearance. Pediatr. Radiol. 1990;20:526–527. doi: 10.1007/BF02011382. https://www.ncbi.nlm.nih.gov/pubmed/2216587 [DOI] [PubMed] [Google Scholar]
- 10.Konuma H., Fu K., Morimoto T., et al. Endoscopic retrieval of a gastric trichobezoar. World J. Gastrointest. Endosc. 2011;3:20–22. doi: 10.4253/wjge.v3.i1.20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3024478/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorter R.R., Kneepkens C.M., Mattens E.C., et al. Management of trichobezoar: case report and literature review. Pediatr. Surg. Int. 2010;26:457–463. doi: 10.1007/s00383-010-2570-0. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2856853/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nirasawa Y., Mori T., Ito Y., et al. Laparoscopic removal of a large gastric trichobezoar. J. Pediatr. Surg. 1998;33:663–665. doi: 10.1016/s0022-3468(98)90342-6. https://www.ncbi.nlm.nih.gov/pubmed/9574777 [DOI] [PubMed] [Google Scholar]
- 13.Fallon S.C., Slater B.J., Larimer E.L., et al. The surgical management of Rapunzel syndrome: a case series and literature review. J. Pediatr. Surg. 2013;48:830–834. doi: 10.1016/j.jpedsurg.2012.07.046. https://www.ncbi.nlm.nih.gov/pubmed/23583142 [DOI] [PubMed] [Google Scholar]
- 14.Miltenberger R.G., Rapp J.T., Long E.S. 2001. Habit Reversal Treatment Manual for Trichotilomania; pp. 170–195. [DOI] [Google Scholar]
- 15.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. https://www.equator-network.org/reporting-guidelines/the-scare-statement-consensus-based-surgical-case-report-guidelines/ [DOI] [PubMed] [Google Scholar]