Highlights
-
•
Foreign body ingestion is a common clinical presentation with less than 1% of the cases requiring surgical intervention.
-
•
Laparoscopic appendicectomy is recommended for the removal of appendiceal foreign bodies.
-
•
Small, sharp objects can cause acute appendicitis or perforation whereas large, round objects may cause appendicitis later in life.
Keywords: Appendicitis, Laparoscopy, Appendicectomy, Foreign body ingestion, Razor blades, Case report
Abstract
Introduction
Foreign body ingestion is a common clinical presentation with less than 1% of the cases requiring surgical intervention. In this report, we present a rare case of razor blades lodged in the appendix as a result of intentional ingestion.
Presentation of case
A 25 year old male prisoner presented to our hospital with persistent right iliac fossa pain after razor blade ingestion. After 5 days of conservative management, there was no sign of transition on serial X-Rays. Laparoscopy with intraoperative image intensification confirmed the presence of the razor blades in the appendix and appendicectomy was subsequently performed without complications.
Discussion
Most ingested objected with diameter less than 2.5 cm and length less than 6 cm can pass through the gastrointestinal tract spontaneously in less than one week. The entry of foreign objects into the appendix is thought to be due to relative low motility of the caecum, the dependent position of the appendix and the size of the appendiceal orifice. Radiographic localisation to the appendiceal lumen was complicated by metallic artefact, but was consistent with failure to transit. Appendicectomy was felt to be the safest mode of retrieval.
Conclusion
Ingested foreign body lodged in the appendix is a rare event. Once the exact location is confirmed, a simple laparoscopic appendicectomy can be performed to facilitate the removal.
1. Introduction
This case report is in line with the SCARE criteria [1].
Foreign body ingestion is a common clinical presentation and intentional ingestion is well recognised amongst the prison population [2]. Fortunately, around 80% of the ingested foreign bodies are able to transit through the gastrointestinal tract uneventfully, 20% lead to endoscopic extraction and surgical intervention accounts is required in less than 1% of presentations [3].
Foreign body in the appendix is rare and there have been no documented reports of razor blades being responsible. Given the unusual presentation and the difficulty in defining the blades’ precise location on imaging, we present a case of non-accidental ingestion of razor blades lodged in the appendix.
2. Case report
A 25 year old male prisoner initially presented to hospital with generalised abdominal pain which gradually localised to his right iliac fossa after intentional razor blade ingestion 12 h prior. His background is significant for depression with a history of multiple intentional ingestions. There were no associated symptoms and the patient remained haemodynamically stable with minimal tenderness. His biochemistry was unremarkable and initial plain films demonstrated two radiopaque fragments in the right lower quadrant, presumed to be within distal small bowel or proximal large bowel with no evidence of pneumoperitoneum.
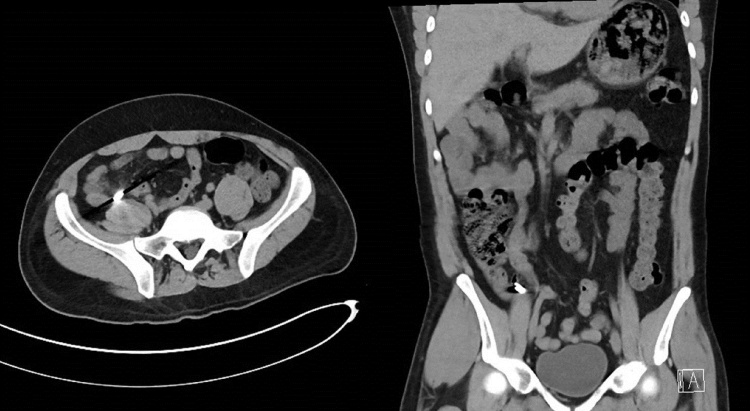
Conservative management was initially attempted but the patient was persistently tender over the right iliac fossa, and the foreign bodies remained static in position on serial plain films Fig. 1. CT Scan performed on day four of admission again noted the two foreign bodies in the right lower quadrant, but precise anatomical localisation was limited by streak artefact. There were no features to suggest perforation Fig. 2.
Fig. 1.
Abdominal X-Ray on day 4 showing 2 radiopaque fragments in the right iliac fossa which have not changed in position compared to previous.
Fig. 2.
CT slices showing the metallic objects in the right iliac fossa, however it was difficult to assess their precise location due to streak artefacts.
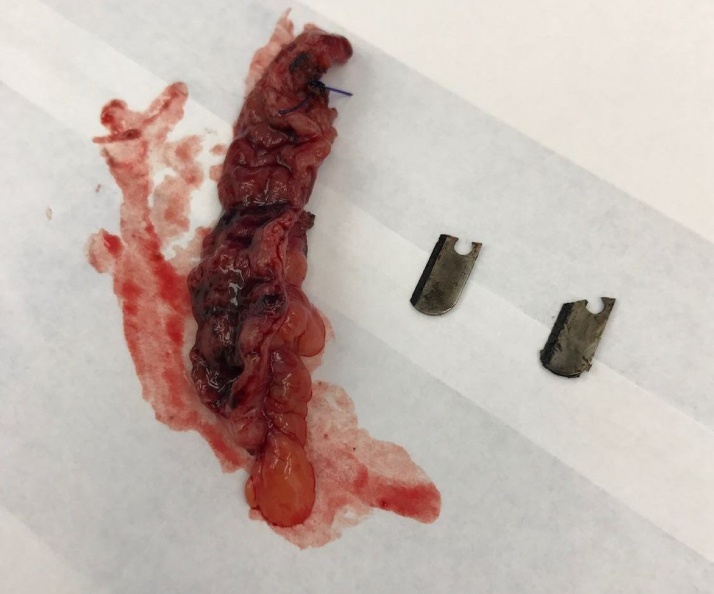
A diagnostic laparoscopy was performed to locate and remove the foreign bodies. Intraoperative image intensification located the razor blades in the appendix. There were no signs to suggest perforation and the base of the appendix was healthy. The tip of the appendix was mildly injected but there was no other macroscopic evidence of appendicitis. The appendix was skeletonised and the base divided between 2 snares (Endoloop). After removal in a pouch (10 mm EndoCatch), the two blades were confirmed to be entirely within the specimen Fig. 3. There were no complications and patient was discharged on day 1 post operation. Histological assessment showed foci of active inflammation in the lamina propria with cryptitis and neutrophils in surface of epithelium associated with haemorrhage which is consistent with early mucosal appendicitis Fig. 4.
Fig. 3.
Using image intensification, we were able to locate the razor blades in the appendiceal lumen.
Fig. 4.
Specimen showing the transected appendix with the razor blades extracted.
3. Discussion
Ingested foreign bodies can be categorised based on size, surface consistency and the material involved. Large, round objects such as coin or meat can impact the thoracic inlet or the gastro-oesophageal junction; spherical or cylindrical objects may be halted at the pylorus and elongated, sharp objects may find themselves lodged at areas of anatomical narrowing or acute angulations such as the duodenal loop, duodenojejunal junction, ileocaecal valve or appendix [4]. In the case of small objects with diameter less than 2.5 cm and length less than 6 cm which have transited to the small intestine, the majority (approximately 67–80%) will pass spontaneously, usually within a week [[2], [3]].
In this case, the swallowed razor blades showed no sign of transition despite five days of conservative management. Precise localisation on CT was limited by streak artefact. It was not clear the objects would protrude from the appendiceal orifice to allow visualisation or retrieval at colonoscopy. We therefore proceeded to a laparoscopy which, with the assistance of intraoperative imaging, confirmed the location within the appendix and allowed for safe removal, and exclusion of local complications.
In this case the foreign bodies were contained entirely in the specimen beyond the distal snare and did not complicate transection at the base. In retrospect this was perhaps fortunate, since it would be difficult to exclude on pre-operative imaging, intra-operative image intensification or instrument handling at laparoscopy. Tightening of a snare onto an intraluminal blade could cause a full thickness injury at the base. While this would hopefully be recognised at operation, a better approach might be to divide the appendix without a proximal snare, extract the remaining foreign body if required, and snare or suture the base after transection.
Previous articles have identified risk factors for entrance of foreign bodies into the appendix [[5], [6]]: 1. The dependent position of the caecum and its low motility; 2. Heavier, denser objects gravitating to the appendiceal orifice; 3. The relative position of the appendix and the size of the appendiceal orifice. Of note, a retrocaecal appendix is much less likely to admit foreign bodies. Once lodged, peristalsis is usually insufficient to expel an object back into the caecum. Obstructing foreign bodies may precipitate appendicitis (sometimes at a later stage) [[7], [8], [9]] and small, sharp objects may cause peri-appendiceal inflammation or perforation [10].
The management of intentional foreign body ingestion in the prison population can be complex as a significant portion of these patients have underlying psychiatric or personality disorders In the acute setting, gaining cooperation from these patients to perform clinical assessment can be difficult and obtaining a valid, informed consent can be challenging. The involvement of the psychiatric team can be beneficial especially in assessing the risks of self-harm and secondary gains. The long term objective would focus on the patients’ safety following their discharge from the hospital and to prevent representations which can potentially lead to recurring laparotomies with their associated risks and complications.
Conflicts of interest
There are no conflicts of interest, financial, personal or otherwise which could influence bias.
Sources of funding
No funding was needed for this case report, except for the amount required if published.
Ethical approval
Ethical approval was not required for this case as it is exempted by our institution.
Consent
Consent was obtained from the patient to submit this case report and the accompanying images. Identifying details have been omitted.
Author contribution
Dr Jason Cui – Corresponding author. Review of patient notes, drafted article. Critical analysis and approval of final submission.
Dr Trent Cross – Critical analysis of draft and approval of final submission.
Dr David Lockwood – Consultant surgeon involved in patient care and decision making. Critical analysis and approval of final submission.
Guarantor
Dr Jason Cui (MBBS), Dr Trent Cross (BSc, MBBS, MSc).
References
- 1.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Evans D.C., Wojda T.R., Jones C.D., Otey A.J., Stawicki S.P. Intentional ingestions of foreign objects among prisoners: a review. World J. Gastrointest Endosc. 2015;7:162–168. doi: 10.4253/wjge.v7.i3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ambe P., Weber S.A., Schauer M., Knoefel W.T. Swallowed foreign bodies in adults. Dtsch Arztebl Int. 2012;109(50):869–875. doi: 10.3238/arztebl.2012.0869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hunter T.B., Taljanovic M.S. Foreign bodies. Radiographics. 2003;23(3):731–757. doi: 10.1148/rg.233025137. [DOI] [PubMed] [Google Scholar]
- 5.Klingler P.J., Seelig M.H., DeVault K.R., Wetscher G.J., Floch N.R., Branton S.A., et al. Ingested foreign bodies within the appendix: a 100-year review of the literature. Dig. Dis. 1998;16:308–314. doi: 10.1159/000016880. [DOI] [PubMed] [Google Scholar]
- 6.Wakeley C.P. The position of the vermiform appendix as ascertained by an analysis of 10,000 cases. J. Anat. 1933;67(Pt 2):277–283. [PMC free article] [PubMed] [Google Scholar]
- 7.Hazer B., Dandin O., Karakaş D. A rare cause of acute appendicitis: an ingested foreign body. Ulus Travma Acil Cerrahi Derg. 2013;19(6):570–572. doi: 10.5505/tjtes.2013.60329. [DOI] [PubMed] [Google Scholar]
- 8.Balch C., Silver D. Foreign bodies in the appendix: report of eight cases and review of the literature. Arch. Surg. 1971;102:14–20. doi: 10.1001/archsurg.1971.01350010016004. [DOI] [PubMed] [Google Scholar]
- 9.Song Y., Covarrubias D., Nardi P. Foreign body appendicitis. AJR Am. J. Roentgenol. 2009;193:W154–155. doi: 10.2214/AJR.08.2148. [DOI] [PubMed] [Google Scholar]
- 10.Price J., Dewar G.A., Metreweli C. Airgun pellet appendicitis. Australas. Radiol. 1988;32:368–370. doi: 10.1111/j.1440-1673.1988.tb02755.x. [DOI] [PubMed] [Google Scholar]