Highlights
-
•
Ectopic parathyroid glands should be suspected when positive sestaMIBI uptake is seen in the mediastinum.
-
•
Other types of imaging (e.g. contrast enhanced CT scan or PET-CT) may confirm the finding of an ectopic parathyroid adenoma.
-
•
A multidisciplinary effort is necessary to address an intrathoracic adenoma.
Keywords: Primary hyperparathyroidism, Ectopic adenomas, Parathyroidectomy, Preoperative imaging, Case report
Abstract
Introduction
Primary hyperparathyroidism (PHPT) is a common endocrine disorder caused by pathologic growth of one or more of the parathyroid glands. Parathyroidectomies (PTX) in patients with PHPT are procedures with low morbidity, few complications, and a high cure rate. However, the parathyroid glands may be found at various anatomical locations and occasionally they are intrathoracic.
Case presentation
We present a 57-year-old patient with PHPT. Before the first and second operation, the preoperative imaging indicated pathologic parathyroid tissue in the neck. Due to postoperative persistent hypercalcemia we performed a 11C-methionine positron emission tomography (11C-MET-PET/CT). The scan showed a focus with increased activity in the mediastinum. Due to persistent disease, an ectopic parathyroid gland in the mediastinum was suspected. At a third operation, the parathyroid adenoma was resected through an anterolateral thoracotomy. Biochemical values normalized and bone mineral density improved postoperatively. Hence, an ectopic localization of a parathyroid gland should be considered during the preoperative planning of a PTX, especially in the re-operative setting. A multidisciplinary effort is necessary to address an intrathoracic adenoma.
Conclusion
Ectopic parathyroid glands should be suspected when positive sestaMIBI uptake is seen in the mediastinum and other types of imaging (e.g. contrast enhanced CT scan or PET-CT) may confirm the finding of an ectopic parathyroid adenoma. From the present case and previous studies we found 11C-MET-PET/CT valuable in difficult PHPT cases.
1. Introduction
Primary hyperparathyroidism (PHPT) is a common endocrine disorder caused by pathologic growth of one or more of the parathyroid glands. The pathologic tissue is a single adenoma in approximately 85–90% of the cases whereas 10–15% have multiple adenomas or hyperplasia [1]. PHPT is diagnosed by elevated plasma calcium levels with concomitant elevated or inappropriately high-normal PTH levels, after excluding other causes of hyperparathyroid hypercalcemia.
The only curative treatment for PHPT is parathyroidectomy (PTX), with a cure rate of approximately 93%–98% [[1], [2]]. There are a few different causes of persistent disease. First, it can be impossible to find all the glands in the neck due to an ectopic pathologic gland or a very small missed gland in the neck. Secondly, in the case of 4 hyperplastic glands it may be advisable to keep one of them to avoid hypoparathyroidism. Due to increasing diagnosis of new PHPT patients, a low rate of surgical complications, and overall good surgical results, the number of patients undergoing PTX is increasing.
The work has been reported in line with the SCARE criteria [11].
2. Case presentation
A 57 year old woman was referred to our Department of Endocrinology and Internal Medicine due to hyperparathyroid hypercalcemia. The biochemical abnormalities were accidentally found during hospitalization for a urinary tract infection.
Laboratory findings revealed elevated plasma ionized calcium (Ca2+) of 1.56 mmol/L (reference interval 1.18–1.32 mmol/L) and plasma parathyroid hormone (PTH) of 10.6 pmol/L (1.6–6.9 pmol/L). She had no clinical symptoms of hypercalcemia, but was diagnosed with osteoporosis by dual energy X-ray absorptiometry (DXA) in the lumbar spine and forearm with T-scores of −2.7 and −2.8, respectively. The T-score was −1.8 at the total hip. There were no kidney stones on a computed tomography scan (CT-scan) and a 24-h urine sample was with normal calcium creatinine clearance ratio (>0.02). In summary, the indication for surgery was based on moderate hypercalcemia and presence of osteoporosis.
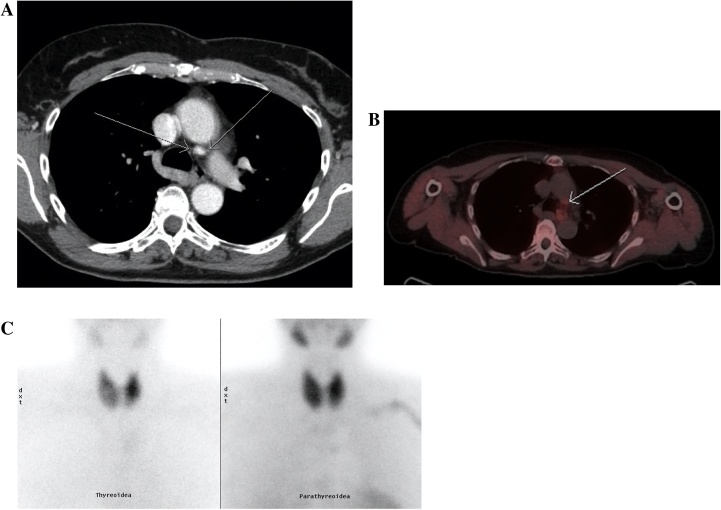
Preoperatively, a 99mTc-methoxy-isobutyl-isonitrile (MIBI) scintigraphy showed possible parathyroid adenoma near the lower left part of the thyroid gland. In addition, there was a focus with increased uptake near the ascending aorta, but this was in first instance interpreted as an inflammatory lymph node. Further, ultrasonography of the neck showed a multinodular goiter and was without visible parathyroid glands.
A bilateral neck exploration was performed, and three parathyroid glands were identified and two and a half parathyroid glands were removed. The fourth parathyroid gland at the inferior position on the right side was not identified. Intraoperative PTH levels decreased insufficiently by only 44% (from 18.6 pmol/L to 10.4 pmol/L) after resection of 2.5 glands. Due to postoperative persistent hypercalcemia we performed a 11C-methionine positron emission tomography (11C-MET-PET/CT). The scan showed a focus with increased activity inside the right thyroid lobe, correspondent to the same area where no parathyroid gland was identified during the first operation. In addition the previous focus with increased activity in the mediastinum was also present on the 11C-MET-PET/CT scan, and interpreted as an inflammatory lymph node.
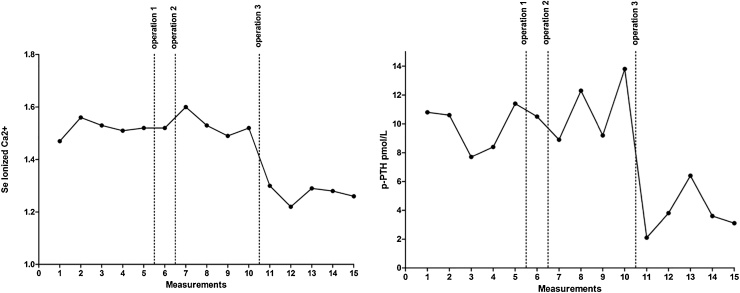
Consequently, it was decided to perform a right-sided hemithyroidectomy. Again the intraoperative PTH levels did not decrease significantly (Fig. 1) and hypercalcemia persisted with Ca2+ levels of 1.50 mmol/L after the second operation. Histopathological examination showed no parathyroid tissue in the specimen removed.
Fig. 1.
Measures of ionized Ca2+ and PTH at the preoperative work-up (1–5), between the first and second operation (6), between the second and third operation (7–10), and after the third operation (11–15).
After the second operation, the patient went through a wide endocrine examination to exclude rare causes of hypercalcemia. We performed genetic tests to exclude Multiple Endocrine Neoplasia, mutations in the gene encoding the Calcium-sensing Receptor, and Cell Division Cycle 73 gene. A control DXA scan revealed a sustained low T-score of −3.0 at the lumbar spine and −3.1 at the forearm.
Due to persistent hypercalcemia, an ectopic localized parathyroid gland in the mediastinum was considered. The interdisciplinary team advised to perform a third operation to explore the upper mediastinum. Prior to the operation, a contrast enhanced CT scan was performed, to identify the precise localization of the process (Fig. 2). The gland was located directly behind the ascending aorta, in the aorta-pulmonary window. An anterolateral thoracotomy was performed and a parathyroid adenoma was resected.
Fig. 2.
Images from contrast enhanced computed tomography (2A), 11C-MET-PET/CT (2B), and from MIBI scintigraphy with thyroid scintigraphy with Tc-99m-Pertechnetate to the left and Tc-99m-sestamibi scintigraphy to the right (2C). Arrows point to the parathyroid gland behind the ascending aorta.
Postoperatively PTH decreased to 1.4 pmol/L (Fig. 1) and ionized calcium normalized at 1.30 mmol/L. There were no postoperative complications, especially no palsy of the recurrent laryngeal nerve. One year after operation the T-score increased by 7.8% in the lumbar spine to −2.5, whereas T-scores in the hip and forearm were unchanged.
3. Discussion
Hyper functioning adenomas are found in an ectopic location in 6% to 16% [3]. These ectopic glands can be found in numerous places, including high cervical positions, the carotid bifurcation, within the thyroid tissue, para-aortic, retro- and para-esophageal and within the thymus [3]. Due to these frequent and various locations there are many ways to identify the precise location of the pathologic gland in the preoperative phase. Further, the preoperative scans are used to evaluate whether the patient is likely to have single- or multigland disease. In the case of negative imaging, the indication for surgery is rarely affected since the operative indication is based on age, symptoms, severity of disease, and presence of organ manifestations to PHPT [[4], [5]]. Hence, the experience of the parathyroid surgeon is crucial when there is no evidence of the number of affected glands or where to find the pathologic gland(s). In the case of negative preoperative imaging, there is a higher risk of persistent postoperative PHPT and the use of intraoperative PTH analysis is crucial [6]. Further, if there is hyperplasia in all four glands, there is a risk of both persistent PHPT after removal of 3 glands but also a higher risk of postoperative hypoparathyroidism.
Within recent years, improvements in the field of imaging have allowed a more targeted surgical approach. Commonly used imaging techniques are ultrasonography (US) and MIBI scintigraphy, usually performed as SPECT with low-dose CT. US is non-invasive, inexpensive and a relatively simple method of imaging. MIBI scintigraphy can be formed using different protocols, usually in goiter rich regions, as ours, the subtraction protocol with petechnetate or I-123 for thyroid imaging is performed together with the sestamibi scan. There is also uptake of sestamibi in thyroid nodules and lymph nodes, which can lead to false-positive scans [4]. There are various ways of performing the scintigraphy. Different isotopes can be used in different ways and with different timing [4]. Further, the CT scan with SPECT can be performed in different ways and occasionally with contrast enhancement. Alternatively, a 4D-CT scan or a CT scan with 11C-MET-PET/CT may be useful [7]. Methionine seems to accumulate more intensively and specifically in enlarged parathyroid glands, although the biochemical mechanisms are not yet fully understood. It is assumed to be related to the synthesis of pre-pro-PTH [7]. 11C-MET-PET/CT is not part of a standardized protocol in the diagnosis of PHPT and previous studies are not all in favor of 11C-MET-PET/CT [8]. In our Hospital 11C-MET-PET has so far been performed in case of persisting PHPT after PTX or in the case of negative conventional imaging studies.
After primary surgery for PHPT, 2% to 7% turn out to have persistent PHPT and some will require re-exploration [2]. Causes of surgical failure include inadequate resection of the adenoma, parathyroid hyperplasia, or an adenoma in an ectopic location. Before re-operation, other causes of elevated PTH and calcium must be carefully considered. This includes tests for familiar hypocalciuric hypercalcemia. If persistent PHPT clearly is the case, the previous imaging examinations, operative notes, biochemical markers, and pathological findings must be meticulously reviewed. In case of postoperative persistent PHPT, missed adenomas in ectopic location have been found in as high as 33% to 56% of patients [3]. Ectopic location of adenoma in the mediastinum is often a challenge both in medical and surgical terms. Increased morbidity is seen due to more extensive dissection, leading to scarring and distortion of tissue planes during surgery [9]. Common complications are in these situations palsy of the recurrent laryngeal nerve and hypoparathyroidism. These challenges have lead to an ongoing discussion of the best imaging modality before re-exploration.
Use of 11C-MET-PET/CT is recommended in reoperations in some studies [7]. In a retrospective study [8] 11C-MET-PET/CT was inferior in detection and localization of parathyroid adenomas compared with US, MIBI scintigraphy, and morphologic imaging (CT and/or MRI) due to a markedly lower sensitivity. The study included 41 patients with primary or secondary hyperparathyroidism without prior thyroidectomy. However, ectopic adenomas and recurrent PHPT were not included and the authors did not elaborate on postsurgical diagnostic challenges. Beggs et al. investigated 11C-MET-PET/CT in PHPT patients with negative conventional imaging [10]. 51 patients were retrospectively reviewed and 11C-MET-PET/CT was found to have a sensitivity of 83%, a specificity of 100% and an accuracy of 88% in successfully location of parathyroid adenomas. 29 of the patients were recurrent/persistent PHPT. All patients had a negative or equivocal MIBI scintigraphy. Sensitivity may have been even higher as five of six false negative scans were due to adenomas in the lower mediastinum, which was not included in the scans.
4. Conclusion
From the present case and previous studies we found 11C-MET-PET/CT valuable in difficult PHPT cases. However, currently there is not sufficient evidence for use of 11C-MET-PET/CT as a routine preoperative imaging examination.
Conflicts of interest
Nothing to declare from any author.
Funding
Nothing to declare from any author.
Ethical approval
This study is exempt from ethnical approval from my institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
All authors have approved the final manuscript.
Marie Møller: main author, data interpretation.
Lars Rolighed: assisted in manuscript production, surgeon, data collection, data interpretation.
Lars Rejnmark: data collection, data interpretation.
Anne Arveschoug: data collection, data interpretation.
Anette Højsgaard: data collection, surgeon.
Guarantor
MD Marie Møller.
MD Lars Rolighed.
References
- 1.Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann. Surg. 2002;235(5):665–670. doi: 10.1097/00000658-200205000-00008. discussion 670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Witteveen J.E., Kievit J., Morreau H., Romijn J.A., Hamdy N.A. No recurrence of sporadic primary hyperparathyroidism when cure is established 6 months after parathyroidectomy. Eur. J. Endocrinol. 2010;162(2):399–406. doi: 10.1530/EJE-09-0789. [DOI] [PubMed] [Google Scholar]
- 3.Roy M., Mazeh H., Chen H., Sippel R.S. Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J. Surg. 2013;37(1):102–106. doi: 10.1007/s00268-012-1773-z. [DOI] [PubMed] [Google Scholar]
- 4.Udelsman R., Akerstrom G., Biagini C., et al. The surgical management of asymptomatic primary hyperparathyroidism: proceedings of the fourth international workshop. J. Clin. Endocrinol. Metab. 2014;99(10):3595–3606. doi: 10.1210/jc.2014-2000. [DOI] [PubMed] [Google Scholar]
- 5.Bilezikian J.P., Brandi M.L., Eastell R., et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the fourth international workshop. J. Clin. Endocrinol. Metab. 2014 doi: 10.1210/jc.2014-1413. jc20141413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bergenfelz Wallin A.O.G., Jansson S., et al. Results of surgery for sporadic primary hyperparathyroidism in patients with preoperatively negative sestamibi scintigraphy and ultrasound. Langenbecks Arch. Surg. 2011;396(1):83–90. doi: 10.1007/s00423-010-0724-0. [DOI] [PubMed] [Google Scholar]
- 7.Kluijfhout W.P., Pasternak J.D., Beninato T., et al. Diagnostic performance of computed tomography for parathyroid adenoma localization; a systematic review and meta-analysis. Eur. J. Radiol. 2017;88:117–128. doi: 10.1016/j.ejrad.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Herrmann K., Takei T., Kanegae K., et al. Clinical value and limitations of [11C]-methionine PET for detection and localization of suspected parathyroid adenomas. Mol. Imaging Biol. 2009;11(5):356–363. doi: 10.1007/s11307-009-0205-4. [DOI] [PubMed] [Google Scholar]
- 9.Phitayakorn R., McHenry C.R. Incidence and location of ectopic abnormal parathyroid glands. Am. J. Surg. 2006;191(3):418–423. doi: 10.1016/j.amjsurg.2005.10.049. [DOI] [PubMed] [Google Scholar]
- 10.Beggs A.D., Hain S.F. Localization of parathyroid adenomas using 11C-methionine positron emission tomography. Nucl. Med. Commun. 2005;26(2):133–136. doi: 10.1097/00006231-200502000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]