Abstract
Background
The number of deaths per year attributed to non-communicable diseases is increasing in low- and middle-income countries, including Thailand. To facilitate the development of evidence-based public health programs and policies in Thailand, research on physical activity (PA) and sedentary behaviour (SB) is needed. The aims of this scoping review were to: (i) map all available evidence on PA and SB in Thailand; (ii) identify research gaps; and (iii) suggest directions for future research.
Methods
A systematic literature search was conducted through 10 bibliographic databases. Additional articles were identified through secondary searches of reference lists, websites of relevant Thai health organisations, Google, and Google Scholar. Studies written in Thai or English were screened independently by two authors and included if they presented quantitative or qualitative data relevant to public health research on PA and/or SB.
Results
Out of 25,007 screened articles, a total of 564 studies were included in the review. Most studies included PA only (80%), 6.7% included SB only, and 13.3% included both PA and SB. The most common research focus was correlates (58.9%), followed by outcomes of PA/SB (22.2%), prevalence of PA/SB (12.4%), and instrument validation (3.2%). Most PA/SB research was cross-sectional (69.3%), while interventions (19.7%) and longitudinal studies (2.8%) were less represented. Most studies (94%) used self-reports of PA/SB, and few (2.5%) used device-based measures. Both sexes were examined in most studies (82.5%). Adults were the main target population group (51.1%), followed by older adults (26.9%), adolescents (15.7%), and children (6.3%). Clinical populations were investigated in the context of PA/SB in a relatively large number of studies (15.3%), most frequently those with cardiovascular disease, diabetes, and hypertension (22%, 21%, and 21% respectively).
Conclusions
The number of Thai papers on PA published per year has been increasing, indicating a growing interest in this research area. More studies using population-representative samples are needed, particularly among children and adolescents, and investigating SB as a health risk factor. To provide stronger evidence on determinants and outcomes of PA/SB, longitudinal studies using standardised measures of PA and SB are required.
Electronic supplementary material
The online version of this article (10.1186/s12889-018-5643-y) contains supplementary material, which is available to authorized users.
Keywords: Physical activity, Sedentary behaviour, Scoping review, Thailand
Background
Deaths caused by non-communicable diseases (NCDs), such as cardiovascular disease and cancer, are common worldwide. Global rates of deaths attributed to NCDs increased from 60% in 2000 to 70% in 2015 [1]. Importantly, the rates of mortality caused by NCDs are increasing faster in low- and middle-income countries than in high-income countries [1]. In Thailand, NCD mortality rates increased from 64% in 2000 to 71% in 2015 [1]. Strong evidence has shown positive impacts of physical activity (PA) on the prevention of NCDs [2–5]. Some evidence also suggests that excessive sedentary behaviour (SB) (e.g. sitting) may increase the risk of several common NCDs, independently of PA [6]. It should be noted, however, that recent methodological papers questioned the independence of PA and SB, based on the argument that these behaviours are co-dependent parts of a time-use composition [7–9]. Nevertheless, the prevalence of physical inactivity, defined as not meeting the recommended level of moderate-to-vigorous physical activity (MVPA) and excessive SB, defined as sitting or reclining with low energy expenditure for more than 7 hours/day, is still high across the world, particularly in middle- and high-income countries [10–12]. In 2012, it was estimated that nearly three-quarters of all physical inactivity-related deaths occurred in low- and middle-income countries [13]. In Thailand, it was estimated that 6.3% of total mortality cases could be attributable to physical inactivity in 2013 [14]. Although, no country-specific estimates are available for Thailand, global estimates suggest that excessive SB is responsible for 3.4% of all-cause mortality [12].
Thailand has been affected by urbanisation, where, in search of better socioeconomic opportunities, many young working people move to urban areas or cities, especially to the capital, Bangkok. According to the Department of Economic and Social Affairs, United Nations, half of the Thai population (51.1%) is urban [13]. This increased rapidly from 1955 when only 18% of the Thai population lived in urban areas [13]. Many issues have arisen as a consequence of the increasing number of people living in the urban setting. An emerging concern related to urbanisation is the increasing time spent in SB in Thai population and its negative health outcomes [14]. In Thailand, there has been increasing focus on strategies to improve engagement in PA and reduce SB. Thailand has experienced significant economic development over the past four decades, moving from a low-income to upper-middle income economy [15]. Since 2002, Thailand has established a “Universal Health Coverage” scheme, to provide healthcare and financial protection to all Thai nationals [16].
As part of the national health promotion strategies, the Thai Government has aimed to promote engagement in PA since 1997 and has recently included targets to reduce SB as ways to reduce the burden of NCDs [17]. Moreover, a number of national actions have been taken to help achieve the World Health Organization’s (WHO) 15-year global target, set in 2010, of 10% reduction in the prevalence of physical inactivity, defined as less than 60 minutes of MVPA daily for adolescents and 150 minutes of MVPA weekly for persons aged 18 and over [17, 18]. WHO has commended Thailand as the regional leader in developing national health policies to promote better health through increasing PA [19]. Many PA promoting initiatives and public campaigns were introduced in Thailand, such as the development of new cycle paths, marathons organised all over the country, and a weekly program of aerobic exercise at workplace launched and led by the Prime Minister of Thailand [17, 19, 20]. Further, the national strategies and guidelines for increasing PA and reducing SB were developed [21]. Despite initiatives to increase the Thai population’s engagement in PA, population-based studies suggest that the prevalence of physical inactivity has increased from 18.5% in 2008 [22] to 19.2% in 2014 [23]. This suggests that the development and implementation of effective public health programs and policies to promote PA and decrease SB is needed.
In PA and SB epidemiology, a number of literature reviews have been conducted. For example, reviews have examined worldwide patterns of PA and SB, and show a shift from physically active to sedentary lifestyles [24–26]. Other reviews have examined factors associated with PA and SB, and the efficacy of interventions to influence the behaviours, especially in high-income countries [27–33]. However, most previous literature reviews are restricted to English language studies only and, therefore, studies from many low- and middle-income countries, including Thailand, have typically not been included. Furthermore, many previous reviews on PA and SB are restricted to specific, narrow topics (e.g. environmental determinants of PA) [27]. A comprehensive assessment of epidemiological evidence on PA and SB in the Thai context is lacking. To provide directions for future studies informing public health policies and actions targeted to increase PA and reduce SB, it is important to map the available evidence on epidemiology of PA and SB in Thailand. Scoping reviews have shown to be a useful method for a systematic assessment of the current body of evidence in a broad subject area [34]. In this study, we conducted a systematic scoping review to assess previous Thai PA and SB research, to identify research gaps and provide evidence-based directions for future research on PA and SB in Thailand to guide the development of strategies and policies.
Methods
Search strategy
This scoping review was conducted according to the Guidance for Conducting Systematic Scoping Reviews [35]. It included primary and secondary database searches. The primary literature search was conducted from database inception to September 2016 through the following bibliographic databases: Academic Search Premier; CINAHL; Health Source: Nursing/Academic Edition; MasterFILE Premier; PsycINFO; PubMed/MEDLINE; Scopus; SPORTDiscus; Web of Science (including Science Citation Index Expanded, Social Sciences Citation Index, Arts & Humanities Citation Index, Conference Proceedings Citation Index- Science, and Conference Proceedings Citation Index- Social Science & Humanities); and the Networked Digital Library of Theses and Dissertations (NDLTD). PubMed/MEDLINE, Scopus and Web of Science databases were searched using their own search engines, whilst other databases were searched through EBSCOhost. The search was conducted through titles, abstracts, and keywords of the indexed publications. The detailed search strategies, including the full search syntaxes, used for each database can be found in Additional file 1.
Additional articles and grey literature documents were identified via secondary literature searching through: (i) the reference lists of all articles selected in the primary search; (ii) websites of ten relevant Thai public health institutions and organizations, including the Division of Physical Activity, Ministry of Public Health; Thai Health Promotion Foundation; Physical Activity Research Centre; Health Systems Research Institute; Thai NCD Network; Thai National Research Repository; Thai Thesis Database; and three university sources including Institute for Population and Social Research, Mahidol University; Chulalongkorn University Intellectual Repository; and Kasetsart University Research and (iii) Google and Google Scholar.
Study selection and inclusion criteria
All references from the primary database search were imported in EndNote X7 software (Thompson Reuters, San Francisco, CA, USA). After removing duplicates, the references were screened independently by two authors (NL and KS). The discrepancies between the study selections were resolved in discussion and consensus with a third author (ZP).
Studies were included in the present review, if they: (i) targeted any population group living in Thailand; (ii) conducted research on PA, physical inactivity, and/or SB; (iii) presented any quantitative or qualitative data relevant to public health, including but not limited to the levels, prevalence, correlates, determinants, or outcomes of engagement in PA and/or SB; or described the development or performed an evaluation of a PA and/or SB measurement tool or intervention; (iv) used any type of PA and/or SB measure, such as self-reports or device-based measures; (v) were written in Thai or English; and (vi) published as a journal article, conference paper, conference abstract, Master’s thesis, Doctoral thesis, or report. Studies were excluded, if they: targeted non-Thai populations; had the primary outcome(s) focusing on sports/exercise performance, or physical therapy; and were published as literature reviews, commentaries, and editorials.
Data extraction
The following data were extracted from the included studies: (i) general bibliographical information, including author names, publication year, title, publication type, full text availability, language of full text, abstract availability, and language of abstract; (ii) description of research methods, including study design, survey method, sample size, and sampling method; (iii) information about the study population, including sex, age, municipality (rural/urban), region, and other specific characteristics of participants; (iv) description of measures, including the type of PA/SB measure, device model or questionnaire name, domains included (such as work, transport, and leisure-time), information about whether the measure has been validated or not (if applicable), and intervention type (if applicable); and (v) information about the study objectives. The detailed data extraction table for studies used in the review is available in Additional file 2.
Results
Search results
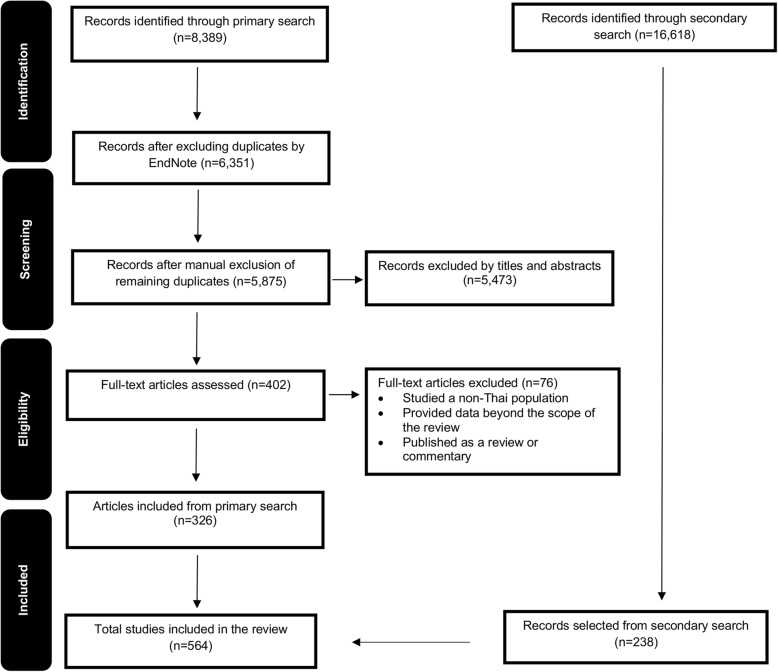
The flow diagram depicting the search and study selection processes can be found in Fig. 1. A total of 25,007 records were screened for inclusion. Of these, 8,389 studies were identified through primary searches, where, after removing duplicates, the titles and abstracts of 5,875 and full texts of 402 articles were screened. The secondary search yielded 16,618 results, of which 238 articles were selected. Overall, a total of 564 studies were included for review [36–598].
Fig. 1.
Flow diagram of study selection process
Bibliographic characteristics of included studies
All papers included in this review were published between 1987 and 2016. The number of papers published per year has increased over time (Fig. 2). English was the primary language used in the majority of Thai PA/SB papers full texts (67.4%), whilst nearly all papers (n = 546) had at least an English abstract (Fig. 3). Furthermore, 17% of full-text articles and 10.1% of abstracts were not available online, and, therefore, other means were used to access the publications (e.g. authors’ contacts and request through university libraries). Most studies were peer-reviewed journal articles (68.3%), followed by theses (19.9%), conference papers (6.6%), and reports (5.3%).
Fig. 2.
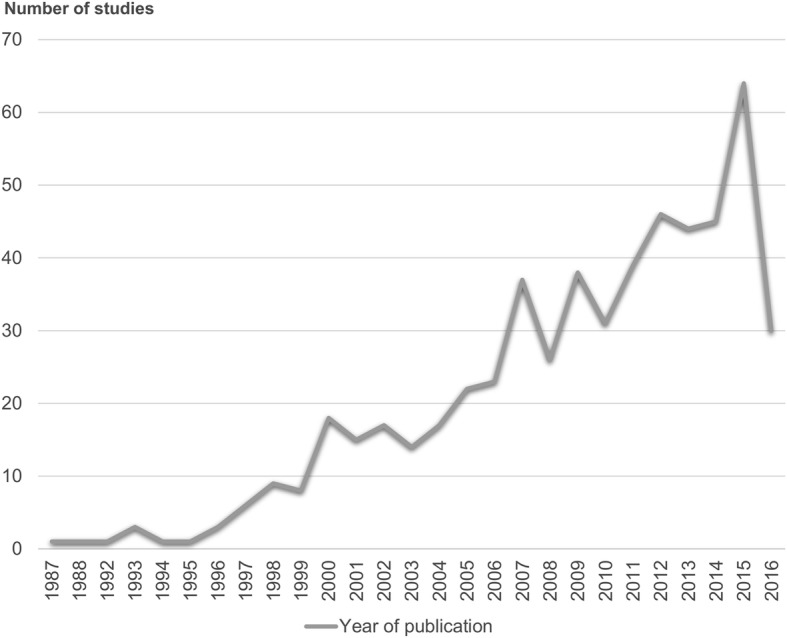
The number of Thai studies on physical activity and sedentary behaviour published per year
Fig. 3.
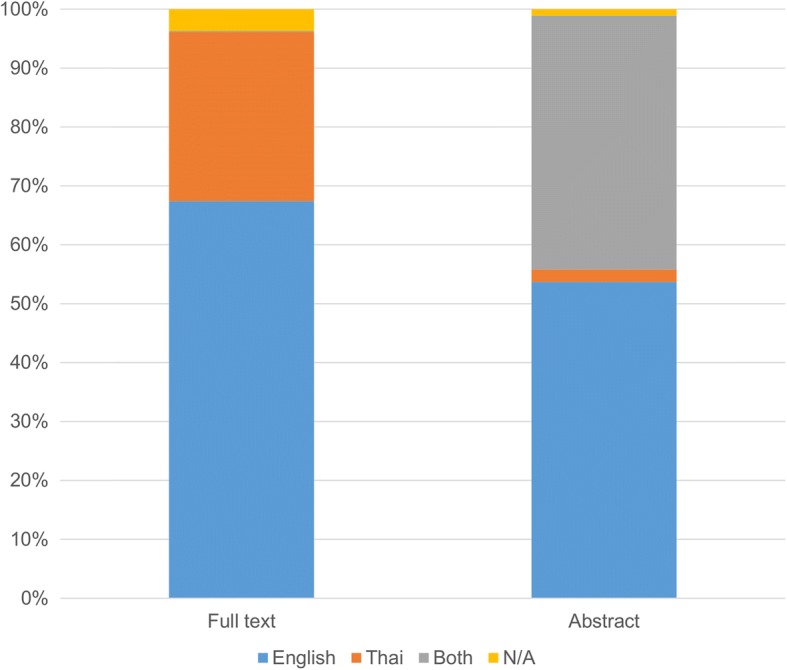
Languages used in full-texts and abstracts of Thai physical activity and sedentary behaviour publications
Study characteristics
In 363 of 564 included studies (64.4%), PA and/or SB were the primary focus of the research (e.g. a study on correlates of PA), whilst the remaining studies were not strictly focused on PA and/or SB but were analysed among multiple other variables as key explanatory or outcome variables together with PA and/or SB (e.g. other lifestyle characteristics such as smoking). Eighty percent of the studies included PA only, 6.7% included SB only, and 13.3% included both PA and SB. Most studies focused on correlates of PA/SB (58.9%), followed by outcomes of PA/SB (22.2%), prevalence of PA/SB (12.4%), and instrument validation (3.2%). 69.3% of studies used cross-sectional designs. Less represented were intervention trials (19.7%), case-control studies (3.7%), longitudinal studies (2.8%), and measurement studies (2.3%). The majority of studies used quantitative methods (87.9%), with only 4.6% and 7.5% utilising qualitative methods or mixed-methods, respectively. In most studies, the data was collected using self-administered surveys (56.7%) or face-to-face interviews (31.4%) (Fig. 4). The sample sizes of the studies ranged from 6 to 113,882 and 7.8% of the studies were conducted using nationally representative samples. Among the studies in nationally representative samples, 29.5% were secondary data analyses of the following national surveys: National Health Examination Survey; National Elderly Survey; Thailand Global School-Based Student Health Survey; 2007 National Physical Activity and Obesity Survey; and 2010 Evaluation of Health Promotion and Sports in Regions. There were seven government reports on PA and/or SB levels presenting results from population-based studies, such as the Health and Welfare Survey 2015 conducted by the National Statistical Office and National Health Examination Survey conducted by the National Health Examination Survey Office.
Fig. 4.
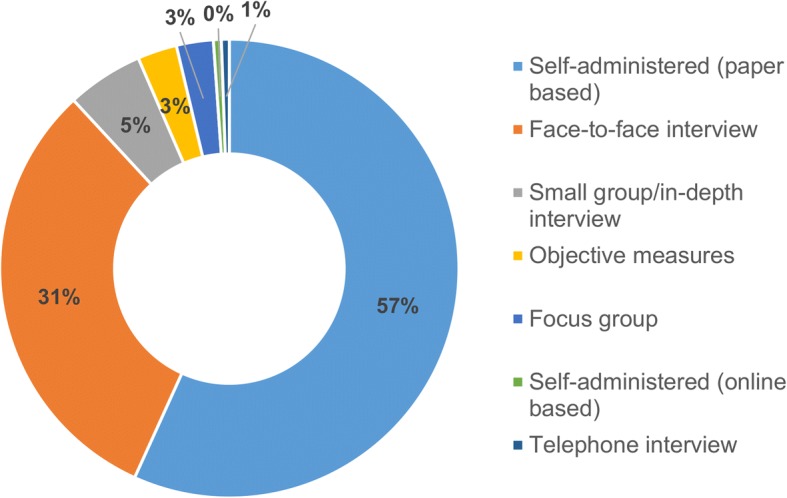
Measures of physical activity and sedentary behaviour used in Thai studies
Characteristics of study samples
Participants of both sexes were included in 82.5% of studies. Studies of females only (15.4%) were more common than studies of males only (2.1%). Adults (18-59 years) were the most frequently investigated age group (51.1%), followed by older adults (60+ years; 26.9%), adolescents (10 to 17 years; 15.7%), children (4 to 9 years; 5.4%), and infants/toddlers (0 to 3 years; 0.9%). A large majority of studies were conducted in non-clinical populations (84.7%). Of these, 28.5% were conducted among primary-school, secondary-school, high-school, and university students. Employees in health-related professions, including nurses, physicians, and health-care students such as medical residents were participants in 9.8% of studies. Other specific occupations were represented in 6.5% of studies; most common among them were farmers, military personnel, university staff, and office workers. Some studies (2.1%) were conducted among employees in specific organizations, such as the Electricity Generating Authority of Thailand, Metropolitan Waterworks, and the Teachers Council. Other specific non-clinical populations included in the studies were, for instance, people with low or high level of PA or SB regularity (5.6%), obese/overweight people (3.8%), women before or in menopause (2.9%), pregnant women (1.3%), and tobacco smokers (0.4%). Clinical populations were also examined in the context of PA/SB (17.7%). Patients with cardiovascular disease, diabetes, and hypertension were among the most frequently observed groups (22%, 21%, and 21%, respectively). Hip/knee problems (13%) and cancers (6%) were also clinical conditions of interest (Table 1). By geographical distribution, Bangkok the capital was the most studied area (28.8%) and the Southern region was the least studied area (15.2%).
Table 1.
Population groups studied in Thai physical activity and sedentary behaviour research
| Population groups | No. of studies |
|---|---|
| Non-clinical populations | |
| Students | 136 |
| General (no specific characteristics) | 135 |
| Occupation-specific populations | 31 |
| Groups based on PA/SB participation | 27 |
| Health-care students | 27 |
| Health-care professionals | 20 |
| Obese/overweight | 18 |
| Pre/post-menopausal women | 14 |
| Employees of a specific organization | 10 |
| Multiple populations groups | 10 |
| Pregnant and postpartum women | 6 |
| Ageing population | 5 |
| Religious groups | 4 |
| Smokers/non-smokers/ex-smokers | 2 |
| Others | 19 |
| Total | 464 |
| Clinical populations (general characteristic) | |
| Cardiovascular disease | 22 |
| Diabetes | 21 |
| Hypertension | 21 |
| Hip/knee injury/condition | 13 |
| Cancer | 6 |
| Respiratory disease/condition | 4 |
| Parkinson’s disease | 3 |
| Diabetes and hypertension | 2 |
| Epilepsy | 2 |
| Dementia | 1 |
| Total | 100 |
Measures of physical activity and sedentary behaviour
Out of 526 studies that investigated PA, most relied on self-reports only (73.4%) and 2.1% used both self-report and device-based measures. In nearly all of these studies (97.2%) PA was assessed using self-reported or proxy-reported questionnaires, and in most cases it was not specified which questionnaire or questionnaire item(s) were used for this purpose. The Global Physical Activity Questionnaire (GPAQ) and the International Physical Activity Questionnaire (IPAQ) were used in 25 (6.5%) and 23 studies (6%), respectively. Other self-reports were PA diary and logbook used in 14 studies (3.5%). Device-based measurement was used in 23 studies (4.4%), with accelerometer (n = 10) and pedometer (n = 9) being the most common devices. A large proportion of PA studies focused on exercise only (49.6%) or on total PA (32.5%). Domain-specific PA levels, including leisure-time, household, work-related, and transport PA, were examined in isolation in 2.5% of all PA studies. The most commonly studied domain of PA was leisure time (n = 16). Walking, as a type-specific PA, was investigated independently in 5 studies. In total, 5.9% of studies assessed a combination of domain- and type-specific PA levels, including exercise, sport and walking.
A total of 113 studies examined SB. Questionnaires were the most common measure of SB (91.2%), followed by activity diaries (4.4%), and device-based tools (3.5%). Most studies (65.5%) did not specify which questionnaires they used. GPAQ, IPAQ, and accelerometers were used in eight, four, and two studies, respectively. Screen time - including TV viewing, computer use, videogames, and internet/social networking - was the most commonly investigated type-specific SB (59.3%). Total sedentary or sitting time was assessed in 37 studies (32.7%), while SB in work and leisure-time domains was assessed in seven and five studies respectively.
Study topics
Correlates of PA and/or SB were the most common topic and were investigated in 58.9% of studies. We identified 11 groups of PA/SB correlates. The most common were: socio-demographic correlates, such as, age, gender, and education level (24%); psychological correlates, such as mental health and well-being, self-efficacy, social behaviours, and cognitive tasks (20.9%); physical health and functioning correlates including physiological and biological functions, diseases, and health problems (19.8%); and social and cultural correlates, such as social support, beliefs, and social practices (11.4%). Other reported correlates included: health behaviours and lifestyles; physical environment; general health; physical skills, abilities, and fitness; academic performance; knowledge; and policy (Table 2).
Table 2.
Number of studies investigating correlates and outcomes of physical activity and sedentary behaviour in Thai populations
| Categories | Correlates | Outcomes | ||
|---|---|---|---|---|
| No. of studies | % | No. of studies | % | |
| Socio-demographic | 162 | 24 | - | - |
| General health | 37 | 5.5 | 9 | 4.2 |
| Physical health and functioning | 134 | 19.8 | 73 | 33.8 |
| Physical skills, abilities, and fitness | 10 | 1.5 | 42 | 19.4 |
| Psychological | 141 | 20.9 | 47 | 21.8 |
| Health behaviours and lifestyle | 35 | 5.2 | 32 | 14.8 |
| Social and culture | 77 | 11.4 | 2 | 0.9 |
| Physical environment | 38 | 5.6 | 1 | 0.5 |
| Academic/school performance | 8 | 1.2 | - | - |
| Mortality | - | - | 2 | 0.9 |
| Knowledge | 27 | 4.0 | 8 | 3.7 |
| Policy | 6 | 0.9 | - | - |
| Total* | 675 | 100 | 216 | 100 |
Note: *Multiple correlates and/or outcomes were investigated in some studies; hence the sum of the totals is greater than the total number of included studies
In total, 125 (22.2%) of the selected studies examined outcomes of PA and/or SB. Most of these studies examined physical health and functioning (33.8%), psychological outcomes (21.8%), physical skills, abilities, and fitness (19.4%), and health behaviours and lifestyles (14.8%). Other reported outcomes included general health; mortality; social characteristics; environmental characteristics; and knowledge (Table 2).
A number of measures were tested for validity and reliability in the Thai context (6.7%). These were mostly questionnaires (92.1%) such as GPAQ, IPAQ (short version), Godin-Shephard Leisure-Time Physical Activity Questionnaire (GSLTPAQ), Modifiable Activity Questionnaire for Adolescents (MAQA), and Perceived Benefits to Physical Activity Scale (PBEPAS). Two studies evaluated measurement properties of device-based measures of PA (pedometer and heart rate monitors). In one study [159] the Compendium of Physical Activities [599] was translated and validated.
Discussion
This study is the first systematic scoping review that summarises current evidence of Thai PA and SB research to support national directions in promoting healthy lifestyle through PA. We identified a large number of PA and SB studies conducted in Thailand, covering a broad range of topics, and using a variety of study designs. There was an increase in the number of Thai PA and SB studies published per year, from one study in 1987 to 64 studies in 2015 (the search was conducted up to September 2016), indicating a growing interest in this research area.
The first Thai publication focusing on PA that we identified was a doctoral thesis from 1987 [289], however the vast majority of PA studies were published in the last two decades. Importantly, the number of Thai papers on PA published per year has been increasing (Fig. 2), indicating that this area of research is developing. It is important to note that half of the studies on PA focused on exercise only, overlooking other types of PA (such as occupational PA, household PA, transport-related PA, and leisure-time PA other than exercise). Historically, the terms ‘physical activity’ and ‘exercise’ have been used interchangeably, and exercise has been one of the most commonly studied types of PA [600]. However, exercise is only one out of several various specific types of PA that may be important for health. From the public health perspective, it is important to study not only exercise but also other types of PA. In Thailand, the term “exercise” had been more widely used until the “physical activity” term was formally promoted in 2002, when the national focal point was changed from the Exercise Unit to the Division of Physical Activity and Health [17].
This finding for Thai studies is consistent with global trends in PA research over the last few decades. The proportion of studies using total MVPA (and not just exercise) as a measure of PA has increased in the last decade [49, 67, 230, 231, 432]. To align with Thai national recommendations on total MVPA, this trend in gathering evidence should be continued in future studies. Importantly, we did not locate any Thai population-based study that considered participation in muscle-strengthening activities, which is similar to the situation in most other countries [601, 602]. Given that Thai national PA guidelines for adults include a separate recommendation on participation in muscle-strengthening activities [603], this suggests more studies on this specific type of PA are needed.
Up until the present, studies on SB in Thailand were less represented than those on PA. SB research is a more recent field of inquiry, compared with PA epidemiology. It has only been in the past two decades that SB has been recognised as a risk factor independent of PA level [604–607]. It was therefore expected that in Thailand SB research would be less developed than PA research. Of the 113 studies addressing SB, 40 looked at specific types of SB, such as TV viewing, computer/internet use, and playing video games. The earliest Thai study we identified that examined type-specific SB, was conducted in 1994, as part of a doctoral thesis focusing on TV viewing and academic achievement [99]. The first study assessing total SB was conducted in 2000, again as part of a doctoral thesis [434]. Since then, there has been a steady increase in the number of Thai papers on SB published per year, indicating an increasing recognition of the importance of this area of research. Given the prevalence of SB and its potential negative health outcomes [6, 12], it is important that future studies continue to focus on SB in Thai populations.
Recent methodological developments have led to the establishment of a new discipline, called time-use epidemiology, where periods of time spent in PA, SB and sleep are no longer considered as independent risk factors, but instead are treated as mutually exclusive and exhaustive parts of the 24-hour day [7–9]. The new approach allows for drawing conclusions about how different reallocations of time between PA, SB and sleep affect health, and for finding the optimal balance of these components of time-use for good health [9, 608]. In line with the new developments and with the public health guidelines adopted in other countries [609–611], the most recent Thai guidelines on movement/non-movement behaviours included recommendations on PA, SB, and sleep [603]. However, the current review found no Thai studies aligned with this new approach, suggesting that this might be an area worth exploring in future epidemiological studies in Thailand.
Almost 70% of all included studies (PA and SB) used cross-sectional designs, whilst the evidence base on determinants and outcomes of PA/SB from longitudinal studies and intervention trials is less developed, potentially due to affordability-related reasons. However, a limitation of cross-sectional data is that they do not allow to draw conclusions about the direction of analysed relationships. To get a better insight into potential causes and consequences of PA and SB, longitudinal studies and controlled intervention trials are needed. Most studies in Thailand assessed PA and/or SB using self-reports. Despite the limitations of self-report instruments [612], these are still the predominant measure of PA and SB in population-based surveys internationally [613, 614]. The use of device-based measures of PA and SB, such as accelerometers, in large-scale epidemiological studies is becoming more affordable, especially in high-income countries [615–617]. However, device-based measurement of PA and/or SB was seldom used in the Thai context. This is likely due to issues related to the high cost and participant burden associated with device-based measurement of PA and SB [614]. Although device-based measuring has limitations in assessing domain- and type-specific PA and SB levels, it may provide some data that cannot be reliably assessed by existing questionnaires (e.g. timing of different activities during a day, detailed data on weekly distribution of PA). To better understand patterns of PA and SB in Thai populations, future research might benefit from employing device-based measures alongside self-report measures.
Although studies included in this review used a variety of sampling methods and a broad range of sample sizes, few were conducted in large-scale population-representative samples. Besides national surveys funded by the Thai government using large scale data samples, such as National Health Examination Survey, Thailand Physical Activity Children Survey, National Physical Activity and Obesity Survey, and Health and Welfare Survey, 10 other studies also utilized a large scale sample (n range: 24,743 – 87,143) from the Sukhothai Thammathirat Open University cohort. To improve the generalisability of findings from observational studies, the use of such large, nationally representative samples should be encouraged in future Thai PA and SB research.
Across age categories, young to middle aged adults (18-59 years) were the most commonly studied population group, followed by older adults (60+ years). The convenience of conducting research among adults and older adults, compared with research among children and adolescents, in terms of ethical considerations, ease of access to participants, and simplicity of measurement, may partially explain why most Thai PA and SB studies focused on these age groups. Another reason may be that adulthood and older age are more convenient stages to observe health impacts of PA and SB, as symptoms of many diseases rarely occur in younger population groups [618]. However, in addition to a number of topics in PA and SB research that are specific for children and adolescent populations (e.g. levels and patterns of school-based PA and SB, tracking of PA and SB from childhood to adolescence, association of PA and SB with educational outcomes in primary and secondary schools, effectiveness of PA and SB interventions in the school setting), findings among adults may not be generalizable to the populations of children and adolescents, which calls for more studies of these age groups in the future.
Thai PA and SB studies covered a wide range of topics, largely consistent with PA/SB research trends in middle- and high-income countries globally [5, 10, 12, 27]. However, there has been limited research on environmental correlates/determinants of PA and SB, associations between PA/SB and mortality outcomes, PA/SB policy research, and validation of device-based measures of PA/SB in different Thai population groups (e.g. across different sociodemographic groups). Around one-third of Thai PA/SB papers were published in the Thai language, while the remaining papers were published in English. Publications in English have higher visibility in the international scholarly context. Alternatively, publications in Thai may better inform local public health stakeholders, media and the general non-academic readership. Ideally, all publications would be in both languages, but in reality this is not feasible. It is, therefore, important to keep a balance between publishing in Thai and English, by always carefully considering the primary purpose of the paper and the targeted readership.
This systematic scoping review has several strengths. First, a systematic search and study selection strategy were applied to identify eligible studies. Comprehensiveness of the search was achieved by using a large number of relevant PA- and SB-related keywords, conducting primary search through 10 bibliographic databases, and supplementing this with an extensive secondary search. Second, data on 39 variables were extracted from the selected studies, which allowed for a detailed interpretation of the current situation in Thai PA and SB research. Last, a key strength was that, since both Thai and English language papers were included, we were able to review a large number of studies that might not have been captured if we only reviewed papers in one language.
This scoping review has some limitations. Although we tried to identify as many studies as possible, we may have missed some studies because they were not indexed in the selected databases. Furthermore, given the large total number of included studies, we focused on providing general recommendations, whilst an in-depth assessment of each individual study was not feasible. Future reviews are needed to summarise findings on specific topics in PA/SB epidemiology within the Thai context, particularly by different age groups (e.g. children, adolescents, adults, and older adults.
Summary recommendations for future research
Based on this systematic scoping review, it can be concluded that the greatest Thai PA/SB research gaps and limitations are: the lack of studies on SB; the use of unspecified and non-validated measures of PA and SB; a limited number of longitudinal studies; a limited number of studies conducted in population-representative samples; a limited number of studies conducted among children and adolescents; a limited coverage of several important PA/SB research topics, such as environmental factors. To provide stronger evidence and further improve the evidence base on PA and SB, future studies may consider several recommendations stemming from this review. First, given that SB research is less developed in the Thai context and that SB is emerging as a new and important health-risk factor among the Thai population [16], more studies on determinants of, outcomes of, and ways to reduce SB in the Thai population are needed. Future studies in Thailand would also be strengthened by using validated device-based and self-report measures of PA and SB. For a better understanding of determinants and outcomes of PA and SB in Thailand, future studies should aim to use longitudinal study designs. Additionally, to allow for better generalisation, more studies should use large, population-representative samples. Besides, future studies are needed specifically focusing on topics relevant to children and adolescents. Finally, research shows that PA is influenced by a number of individual, social, environmental, and policy factors [27, 619]. Whilst socio-demographic, psychological, and social correlates have been the topic of a number of Thai studies, more research is needed on environmental and policy-related correlates of PA and SB in Thailand.
Conclusions
Thai research on PA and SB has rapidly evolved and received increasing attention in the last two decades. Substantial literature was mapped in this review, showing that existing research has a great potential to support the development of healthy lifestyles by increasing PA and reducing SB in Thailand. However, current evidence could be strengthened, particularly by conducting more research on SB, using sound research methods, and covering the full range of research topics on determinants and outcomes of PA and SB. By following the recommendations provided in this systematic scoping review, future studies may provide even stronger evidence needed to inform public health efforts to promote PA and reduce SB in Thailand.
Additional files
Search keywords. Detailed search keywords including the full search syntaxes used for each database. (PDF 183 kb)
Data extraction table. The detailed table of all data extracted from each study included in this review. (XLSX 245 kb)
Acknowledgments
This article is a part of a PhD project of the first author, NL, supervised by MC, SJHB, and ZP (principal supervisor).
Availability of data and materials
The summary of reviewed articles is available in Tables, Figures, and Additional files.
Abbreviations
- GPAQ
Global Physical Activity Questionnaire
- GSLTPAQ
Godin-Shephard Leisure-Time Physical Activity Questionnaire
- IPAQ
International Physical Activity Questionnaire
- MAQA
Modifiable Activity Questionnaire for Adolescents
- MVPA
Moderate-to-Vigorous Physical Activity
- NCDs
Non-Communicable Diseases
- NDLTD
Networked Digital Library of Theses and Dissertations
- PA
Physical Activity
- PBEPAS
Perceived Benefits to Physical Activity Scale
- SB
Sedentary Behaviour
- WHO
World Health Organization
Authors’ contributions
NL and ZP conceived the idea for the review. NL, ZP, SJHB and JAB conceptualised the review. NL took the lead in writing the study protocol. NL and ZP designed the systematic search strategies. NL and KS conducted the study selection. NL did the data extraction and analysed the data. NL drafted the initial manuscript. ZP, JAB, MC, SJHB, and KS contributed to writing the manuscript. All authors read and approved the final draft.
Ethics approval and consent to participate
Not applicable.
Competing interests
Biddle: Funding has been received since 2013 for consultancy work from Fitness First, Nuffield Health, and Unilever. None of these are currently active. Funding was received in 2016 for consultancy work for Halpern PR Limited. In-kind support through the provision of a sit-to-stand desk was provided by Ergotron from 2012-2014. Advice has been requested by and offered to Active Working, Get Britain Standing, Bluearth, and WellKom, none with funding.
The other authors declare no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12889-018-5643-y) contains supplementary material, which is available to authorized users.
Contributor Information
Nucharapon Liangruenrom, Email: nucharapon.liangruenrom@live.vu.edu.au, Email: nucharapon.lia@mahidol.ac.th.
Kanyapat Suttikasem, Email: kanyapat.sut@mahidol.ac.th.
Melinda Craike, Email: Melinda.Craike@vu.edu.au.
Jason A. Bennie, Email: Jason.Bennie@usq.edu.au
Stuart J. H. Biddle, Email: stuart.biddle@usq.edu.au
Zeljko Pedisic, Email: zeljko.pedisic@vu.edu.au.
References
- 1.The World Bank: WHO's World Health Statistics. http://data.worldbank.org/indicator/SH.DTH.NCOM.ZS. Accessed 9 Jan 2017.
- 2.World Health Organization . Global recommendations on physical activity for health. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 3.Miles L. Physical activity and health. British Nutrition Foundation Nutrition Bulletin. 2007;32:314–363. doi: 10.1111/j.1467-3010.2007.00668.x. [DOI] [Google Scholar]
- 4.Warburton DE, Charlesworth S, Ivey A, Nettlefold L, Bredin SS. A systematic review of the evidence for Canada’s Physical Activity Guidelines for Adults. Int J Behav Nutr Phys Act. 2010;7:39. doi: 10.1186/1479-5868-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee I-M, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Rezende LFM, Lopes MR, Rey-Loṕez JP, Matsudo VKR, Luiz ODC. Sedentary behavior and health outcomes: An overview of systematic reviews. PLoS ONE. 2014; 10.1371/journal.pone.0105620. [DOI] [PMC free article] [PubMed]
- 7.Pedišić Ž. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behaviour research: The focus should shift to the balance between sleep, sedentary behaviour, standing and activity. Kinesiol. 2014;46(1):135–146. [Google Scholar]
- 8.Dumuid D, Stanford TE, Martin-Fernandez JA, Pedišić Ž, Maher CA, Lewis LK, et al. Compositional data analysis for physical activity, sedentary time and sleep research. Statistical Methods in Medical Research. 2017; 10.1177/0962280217710835. [DOI] [PubMed]
- 9.Pedišić Ž, Dumuid D, Olds T. Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time-use epidemiology: definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiol. 2017;49(2):1–18. doi: 10.26582/k.49.2.14. [DOI] [Google Scholar]
- 10.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Lancet Physical Activity Series Working Group. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012; 10.1016/S0140-6736(12)60646-1. PMID:22818937 [DOI] [PubMed]
- 11.Dumith SC, Hallal PC, Reis RS, Kohl HW., III Worldwide prevalence of physical inactivity and its association with human development index in 76 countries. Prev Med. 2011;53:24–28. doi: 10.1016/j.ypmed.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 12.LFM d R, de Sá TH, Mielke GI, Viscondi JYK, Rey-López JP, Garcia LMT. All-cause mortality attributable to sitting time: Analysis of 54 countries worldwide. Am J Prev Med. 2016; 10.1016/j.amepre.2016.01.022. [DOI] [PubMed]
- 13.Worldometers: Thailand population. Elaboration of data by United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2015 Revision. http://www.worldometers.info/world-population/thailand-population/ (2015). Accessed 17 Jan 2017.
- 14.Ketwongsa P. Physical activity survey of Thailand 2015. Nakornpathom: Population and Social Research Institute, Mahidol University; 2015. [Google Scholar]
- 15.The World Bank: The World Bank in Thailand. http://www.worldbank.org/en/country/thailand/overview. Accessed 17 Jan 2017.
- 16.Centre for Global Development: Thailand’s Universal Coverage Scheme. http://millionssaved.cgdev.org/case-studies/thailands-universal-coverage-scheme. Accessed 17 Jan 2017.
- 17.Topothai T, Chandrasiri O, Liangruenrom N, Tangcharoensathien V. Renewing commitments to physical activity targets in Thailand. The Lancet comment. 2016;388(10051):1258–60. doi: 10.1016/S0140-6736(16)30929-1. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . NCD global monitoring framework. Geneva: World Health Organization; 2013. [Google Scholar]
- 19.World Health Organization . Thailand’s physical activity drive is improving health by addressing NCDs. 2017. [Google Scholar]
- 20.Katewongsa P, Sawangdee Y, Yousomboon C, Choolert P. Physical activity in Thailand: The general situation at national level. J Sci Med Sport. 2014;18:e100–e1e1. doi: 10.1016/j.jsams.2014.11.374. [DOI] [Google Scholar]
- 21.Division of Physical Activity and Health. Department of Health . Physical activity guideline for Thai people. Nonthaburi: Ministry of Public Health; 2016. [Google Scholar]
- 22.Office of National Health Examination Survey . National Health Examination Survey 2008. Bangkok: Ramathibodi Hospital; 2008. [Google Scholar]
- 23.Office of National Health Examination Survey . National Health Examination Survey 2014. Bangkok: Health System Research Institute; 2016. [Google Scholar]
- 24.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012;13(8):659–680. doi: 10.1111/j.1467-789X.2011.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katzmarzyk PT, Mason C. The physical activity transition. J Phys Act Health. 2009;6(3):269–280. doi: 10.1123/jpah.6.3.269. [DOI] [PubMed] [Google Scholar]
- 26.Knuth AG, Hallal PC. Temporal Trends in Physical Activity: A Systematic Review. J Phys Act Health. 2009;6:548–559. doi: 10.1123/jpah.6.5.548. [DOI] [PubMed] [Google Scholar]
- 27.Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJF, Martin BW. Lancet Physical Activity Series Working Group. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380:258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 28.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med. Sci. Sports Exerc. 2000;32(5):963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med. Sci. Sports Exerc. 2002;34(12):1996–2001. [DOI] [PubMed]
- 30.Rhodes RE, Mark RS, Temmel CP. Adult sedentary behavior: a systematic review. Am J Prev Med. 2012;42(3):e3–28. doi: 10.1016/j.amepre.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 31.Pearson N, Biddle SJH. Sedentary Behavior and Dietary Intake in Children, Adolescents, and Adults: A Systematic Review. Am J Prev Med. 2011;41(2):178–188. doi: 10.1016/j.amepre.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 32.Mabry R, Koohsari MJ, Bull FC, Owen N. A systematic review of physical activity and sedentary behaviour research in the oil-producing countries of the Arabian Peninsula. BMC Public Health. 2016; 10.1186/s12889-016-3642-4. [DOI] [PMC free article] [PubMed]
- 33.Schoeppe S, Alley S, Lippevelde WV, Bray NA, Williams SL, Duncan MJ, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016; 10.1186/s12966-016-0454-y. [DOI] [PMC free article] [PubMed]
- 34.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 35.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid-Based Healthc. 2015;13(3):141–146. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 36.A-piwong C. Exercise behaviors of students at university of the Thai Chamber of Commerce. Bangkok: Graduate School, Srinakharinwirot University; 2011. [Google Scholar]
- 37.Adulyanon S, Vourapukjaru J, Sheiham A. Oral impacts affecting daily performance in a low dental disease Thai population. Community Dent Oral Epidemiol. 1996;24(6):385–389. doi: 10.1111/j.1600-0528.1996.tb00884.x. [DOI] [PubMed] [Google Scholar]
- 38.Aekplakorn W, Satheannoppakao W, Putwatana P, Taneepanichskul S, Kessomboon P, Chongsuvivatwong V, et al. Dietary Pattern and Metabolic Syndrome in Thai Adults. J Nutr Metab. 2015;2015:1–10. doi: 10.1155/2015/468759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahmed SM, Hadi A, Razzaque A, Ashraf A, Juvekar S, Ng N, et al. Clustering of chronic non-communicable disease risk factors among selected Asian populations: levels and determinants. Global Health Action. 2009;2:68–75. doi: 10.3402/gha.v2i0.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Akkayagorn L, Tangwongchai S, Worakul P. Cognitive profiles, hormonal replacement therapy and related factors in Thai menopausal women. Asian Biomedicine. 2009;3(4):439–444. [Google Scholar]
- 41.Amini M, Alavi-Naini A, Doustmohammadian A, Karajibani M, Khalilian A, Nouri-Saeedloo S, et al. Childhood obesity and physical activity patterns in an urban primary school in Thailand. Rawal Med J. 2009;34(2):203–206. [Google Scholar]
- 42.Amitrapai Y. Effect of exercise programs on weight and health related fitness of Prathom Suksa 5-6 level over nutritional status students in Banbanglen School, Banglen district, Nakhonpathom province. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2007. [Google Scholar]
- 43.Amnatsatsue K. Measurement of physical function in Thai older adults. Chapel Hill: University of North Carolina; 2002. [Google Scholar]
- 44.Amornsriwatanakul A, Nakornkhet K, Katewongsa P, Choosakul C, Kaewmanee T, Konharn K, et al. Results from Thailand’s 2016 Report Card on Physical Activity for Children and Youth. J Phys Act Health. 2016;13(11 Suppl 2):S291–S2S8. doi: 10.1123/jpah.2016-0316. [DOI] [PubMed] [Google Scholar]
- 45.Andrews A. Factors affecting adult obesity in a large city in Thailand. US: ProQuest Information & Learning; 2014. [Google Scholar]
- 46.Anek A, Bunyaratavej N. Effects of circuit aerobic step exercise program on musculoskeletal for prevention of falling and enhancement of postural balance in postmenopausal women. J Med Assoc Thailand. 2015;98:S88–S94. [PubMed] [Google Scholar]
- 47.Anek A, Kanungsukasem V, Bunyaratavej N. Effects of aerobic step combined with resistance training on biochemical bone markers, health-related physical fitness and balance in working women. J Med Assoc Thailand. 2015;98:S42–S51. [PubMed] [Google Scholar]
- 48.Angkurawaranon C, Lerssrimonkol C, Jakkaew N, Philalai T, Doyle P, Nitsch D. Living in an urban environment and non-communicable disease risk in Thailand: Does timing matter? Health Place. 2015;33:37–47. doi: 10.1016/j.healthplace.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 49.Ar-Yuwat S, Clark MJ, Hunter A, James KS. Determinants of physical activity in primary school students using the health belief model. J Multidiscip Healthc. 2013;6:119–126. doi: 10.2147/JMDH.S40876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aree P, Wangsrikhun S, Kantawang S, Boonyasopun U, Phienchai K, Buranapin S, et al. Nutritional status, food consumption, and physical activity in adolescents: a pilot study. Nurs J. 2007;34(2):98–105. [Google Scholar]
- 51.Aree-Ue S, Petlamul M. Osteoporosis Knowledge, Health Beliefs, and Preventive Behavior: A Comparison between Younger and Older Women Living in a Rural Area. Health Care Women Int. 2013;34(12):1051–1066. doi: 10.1080/07399332.2012.736565. [DOI] [PubMed] [Google Scholar]
- 52.Aree-Ue S, Pothiban L. Osteoporosis knowledge, osteoporosis prevention behavior, and bone mass in older adults living in Chiang Mai. Thai J Nurs Res. 2003;7(1):1–11. [Google Scholar]
- 53.Aree-Ue S, Pothiban L, Belza B. Join the Movement to Have Healthy Bone Project (JHBP): Changing behavior among older women in Thailand. Health Care Women Int. 2005;26(8):748–760. doi: 10.1080/07399330500179846. [DOI] [PubMed] [Google Scholar]
- 54.Artitdit P, Iamopas O, Bhakta D. Effect of Dietary and Physical Activity Intervention in Overweight and Obese Thai Adults. Ann Nutr Metab. 2013;63:1152. [Google Scholar]
- 55.Asawachaisuwikrom W. Physical activity and its predictors among older Thai adults. J Sci, Technol Human. 2003;1(1):65–76. [Google Scholar]
- 56.Asawachaisuwikrom W. Factors influencing physical activity among older adults in Saensuk sub-district, Chonburi Province. Chonburi: Faculty of Nursing, Burapha University; 2004. [Google Scholar]
- 57.Assantachai P, Maranetra N. Nationwide Survey of the Health Status and Quality of Life of Elderly Thais Attending Clubs for the Elderly. J Med Assoc Thai. 2003;86(10):938–946. [PubMed] [Google Scholar]
- 58.Assantachai P, Sriussadaporn S, Thamlikitkul V, Sitthichai K. Body composition: Gender-specific risk factor of reduced quantitative ultrasound measures in older people. Osteoporos Int. 2006;17(8):1174–1181. doi: 10.1007/s00198-006-0117-y. [DOI] [PubMed] [Google Scholar]
- 59.Atchara P, Kasem N, Mayuree T, Suporntip P, Seabra A, Carvalho J. Associations between Physical Activity, Functional Fitness, and Mental Health among Older Adults in Nakornpathom, Thailand. Asian J Exerc Sports Sci. 2014;11(2):25–35. [Google Scholar]
- 60.Aung MN, Lorga T, Srikrajang J, Promtingkran N, Kreuangchai S, Tonpanya W, et al. Assessing awareness and knowledge of hypertension in an at-risk population in the Karen ethnic rural community, Thasongyang. Thailand. Int J Gen Med. 2012;5:553–61. doi: 10.2147/IJGM.S29406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aungsusuknarumol C. Exercise for health behavior of community college students in Northern colleges of physical education. Bangkok: Graduate School, Srinakharinwirot University; 2000. [Google Scholar]
- 62.Aunprom-me S, Aunprom-me S. Self-efficacy, decisional balance, and stages of change in physical activity among first year nursing students. J Nurses Assoc Thai, North-Eastern Division. 2012;3(4):22–29. [Google Scholar]
- 63.Aunprom-me S, Aunprom-me S, editors. Physical Activity in Graduating Fourth Year Nursing Students: A comparative study using the Transtheoretical Model and the Stages of Change. Bangkok: ANPOR Conference Bangkok 2015; 2015. [Google Scholar]
- 64.Auvichayapat P, Prapochanung M, TunkamnerdThai O, B-o S, Auvichayapat N, Thinkhamrop B, et al. Effectiveness of green tea on weight reduction in obese Thais: A randomized, controlled trial. Physiol Behav. 2008;93(3):486–491. doi: 10.1016/j.physbeh.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 65.Awikunprasert C, Vongjaturapat N, Li F, Sittiprapaporn W. Therapeutic use of music and exercise program on the quality of life in Thai cancer patients. Res J Applied Sci. 2012;7(6):297–300. [Google Scholar]
- 66.Ayudthaya WCN, Kritpet T. Effects of low impact aerobic dance and fitball training on bone resorption and health-related physical fitness in Thai working women. J Med Assoc Thai. 2015;98:S52–SS7. [PubMed] [Google Scholar]
- 67.Baiya N, Tiansawad S, Jintrawet U, Sittiwangkul R, Pressler SJA. Correlational Study of Physical Activity Comparing Thai Children With and Without Congenital Heart Disease. Pacific Rim Int J Nurs Res. 2014;18(1):29–41. [Google Scholar]
- 68.Bandasak R, Narksawat K, Tangkanakul C, Chinvarun Y, Siri S. Association between hypertension and stroke among Young Thai adults in Bangkok, Thailand. Southeast Asian J Trop Med Public Health. 2011;42(5):1241–1248. [PubMed] [Google Scholar]
- 69.Banks E, Lim L, Seubsman SA, Bain C, Sleigh A. Relationship of obesity to physical activity, domestic activities, and sedentary behaviours: Cross-sectional findings from a national cohort of over 70,000 Thai adults. BMC Public Health. 2011;11(1):762. doi: 10.1186/1471-2458-11-762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Banwell C, Lim L, Seubsman SA, Bain C, Dixon J, Sleigh A. Body mass index and health-related behaviours in a national cohort of 87 134 Thai open university students. J Epidemiol Community Health. 2009;63(5):366–372. doi: 10.1136/jech.2008.080820. [DOI] [PubMed] [Google Scholar]
- 71.Bhoopat L, Rojnuckarin P, Hiransuthikul N, Intragumtornchai T. Low vegetable intake is strongly associated with venous thromboembolism in Thai population. Blood Coagul Fibrinolysis. 2010;21(8):758–763. doi: 10.1097/MBC.0b013e3283403537. [DOI] [PubMed] [Google Scholar]
- 72.Bhuripanyo K, Mahanonda N, Leowattana W, Ruangratanaamporn O, Sriratanasathavorn C, Chotinaiwattarakul C, et al. A 5-year prospective study of conventional risk factors of coronary artery disease in Shinawatra employees: A preliminary prevalence survey of 3,615 employees. J Med Assoc Thai. 2000;83(SUPPL. 2):S98–S105. [PubMed] [Google Scholar]
- 73.Binhosen V, PanuThai S, Srisuphun W, Chang E, Sucamvang K, Cioffi J. Physical activity and health related quality of life among the urban Thai elderly. Thai J Nurs Res. 2003;7(4):231–243. [Google Scholar]
- 74.Boonchuaykuakul J. Effectiveness of applying the transtheoretical model to improve physical activity behavior of university students. Oregon: Oregon State University; 2005. [Google Scholar]
- 75.Boonkwamdee S. A study of health behavior of overweight persons in Bangkok Metropolis. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 1998. [Google Scholar]
- 76.Boonrat N. Relationships among personal factors, spouse support, and physical activity of postpartum women. Bangkok: Faculty of Nursing, Chulalongkorn University; 2004. [Google Scholar]
- 77.Boonrin P, Choeychom S, Nantsupawat W. Predictive factors on exercise behaviors of nursing students. J Nurs Health Care. 2015;33(2):176–186. [Google Scholar]
- 78.Boonyaratavej N, Suriyawongpaisal P, Takkinsatien A, Wanvarie S, Rajatanavin R, Apiyasawat P. Physical activity and risk factors for hip fractures in Thai women. Osteoporos Int. 2001;12(3):244–248. doi: 10.1007/s001980170136. [DOI] [PubMed] [Google Scholar]
- 79.Buarapha S. Relationships between personal factors, perception of symptoms severity, self-efficacy, social support, and physical activity in patients with chronic heart failure. Bangkok: Faculty of Nursing, Chulalongkorn University; 2004. [Google Scholar]
- 80.Bunprajun T, Henriksen TI, Scheele C, Pedersen BK, Green CJ. Lifelong Physical Activity Prevents Aging-Associated Insulin Resistance in Human Skeletal Muscle Myotubes via Increased Glucose Transporter Expression. PLoS ONE. 2013;8(6):1–10. doi: 10.1371/journal.pone.0066628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Buranruk O. Effect of chi-kung exercise on chest expansion and lung volume in elderly people. KKU Res J. 2000;5(1):18–25. [Google Scholar]
- 82.Buranruk O, Eungpinitpong W. Effects of Ruesidadton, Chikung, and combination exercises on stress and quality of life in sedentary women. J Med Technol Phys Ther. 2013;25(3):280–288. [Google Scholar]
- 83.Buranruk O, La Grow S, Ladawan S, Makarawate P, Suwanich T, Leelayuwat N. Thai yoga as an appropriate alternative physical activity for older adults. Journal of Complementary and Integrative Medicine. 2010;7(1):1–14. doi: 10.2202/1553-3840.1290. [DOI] [Google Scholar]
- 84.Butraprom C. Factors affecting internet addiction behavior of adolescence in Bangkok Metropolis. Bangkok: Faculty of Political Science, Chulalongkorn University; 2002. [Google Scholar]
- 85.Chadchavalpanichaya N, Intaratep N. Exercise behavior and knowledge among the DM type II patients. J Med Assoc Thai. 2010;93(5):587–593. [PubMed] [Google Scholar]
- 86.Chanavirut R, Khaidjapho K, Jaree P, Pongnaratorn P. Yoga exercise increases chest wall expansion and lung volumes in young healthy Thais. Faseb J. 2006;20(5):A1257–A125A. [Google Scholar]
- 87.Chanchalor S. Online games and Thai youth case studies of impact. Soc Sci (Pakistan). 2013;8(2):129–134. [Google Scholar]
- 88.Chanruengvanich W, Kasemkitwattana S, Charoenyooth C, Towanabut S, Pongurgsorn C. RCT: self-regulated exercise program in transient ischemic attack and minor stroke patients. Thai J Nurs Res. 2006;10(3):165–179. [Google Scholar]
- 89.Chansarn S. Active ageing of elderly people and its determinants: Empirical evidence from Thailand. Asia-Pac Soc Sci Rev. 2012;12(1):1–18. [Google Scholar]
- 90.Charoenkitkarn V. The study of perceived self-efficacy and interpersonal influences to exercise behavior in the elderly with essential hypertension. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2000. [Google Scholar]
- 91.Charoensook K. Factors affecting exercise behaviors of teachers in Nakhonpanom province in academic year 2007. Bangkok: Graduate School, Srinakharinwirot University; 2007. [Google Scholar]
- 92.Charoenying W, Asawachaisuwikrom W, Junprasert S. Factors affecting exercise behavior of upper secondary level school students in schools upper the office of Prachinburi educational service area. J Fac Nurs Burapha Univ. 2006;11(1):23–34. [Google Scholar]
- 93.Charupash R. The self care behaviors of the western son's in laws Isaan's rural of Thailand. 7th World Conference on Educational Sciences. Procedia Soc Behav Sci. 2015;197:2310–2314. doi: 10.1016/j.sbspro.2015.07.258. [DOI] [Google Scholar]
- 94.Chawla N, Panza A. Assessment of childhood obesity and overweight in Thai children grade 5-9 in BMA bilingual schools, Bangkok, Thailand. J Health Res. 2012;26(6):317–322. [Google Scholar]
- 95.Chidnok W, Weerapun O, Srirung T, Pacharean R. Permsuwan A. the study of types and obstacle of exercise in personals of Naresuan University. J Sports Sci Technol. 2007;7(1 and 2):101–108. [Google Scholar]
- 96.Chidnok W, Wiangkham T, Pukyod N, Nitikul P, Inchom A. The study on information of exercise services requirement in students of Naresuan University. J Sports Sci Technol. 2008;8(1):131–141. [Google Scholar]
- 97.Chinuntuya P. A causal model of exercise behavior of the elderly in Bangkok metropolis. Bangkok: Faculty of Graduate Studies, Mahidol University; 2001. [Google Scholar]
- 98.Chirawatkul S. Alternative health used among menopausal women in the northeast of Thailand. 9th International Menopause Society World Congress on the Menopause. 1999. pp. 21–25. [Google Scholar]
- 99.Chompaisal S. The perceived influence of television on achievement in children and adolescents in Thailand. Illinois: the United States: Department of Educational Administrational and Foundations, Illinois State University; 1994. [Google Scholar]
- 100.Chonchaiya W, Nuntnarumit P, Pruksananonda C. Comparison of television viewing between children with autism spectrum disorder and controls. Acta Paediatrica. 2011;100(7):1033–1037. doi: 10.1111/j.1651-2227.2011.02166.x. [DOI] [PubMed] [Google Scholar]
- 101.Chonchaiya W, Pruksananonda C. Television viewing associates with delayed language development. Acta Paediatrica. 2008;97(7):977–982. doi: 10.1111/j.1651-2227.2008.00831.x. [DOI] [PubMed] [Google Scholar]
- 102.Chongwatpol P, Gates GE. Differences in body dissatisfaction, weight-management practices and food choices of high-school students in the Bangkok metropolitan region by gender and school type. Public Health Nutr. 2016;19(7):1222–1232. doi: 10.1017/S1368980016000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Choosakul C, Taweesuk D, Piyasuwan S. The Influence of personal characteristics, behavior specific-cognitions and psychological factors on exercise commitment of Thai adult populations in the Northeast. Int J Psychol. 2008;43(3-4):133. [Google Scholar]
- 104.Chotibang J, Fongkaew W, Mo-suwan L, Meininger JC, Klunklin P. Development of a family and school collaborative (FASC) Program to promote healthy eating and physical activity among school-age children. Thai J Nurs Res. 2009;13(2):133–146. [Google Scholar]
- 105.Chotikacharoensuk P. Physical activity and psychological well-being among the elderly. Chiang Mai: Graduate School, Chiang Mai University; 2002. [Google Scholar]
- 106.Chuamoor K, Kaewmanee K, Tanmahasamut P. Dysmenorrhea among Siriraj nurses; Prevalence, quality of life, and knowledge of management. J Med Assoc Thai. 2012;95(8):983–991. [PubMed] [Google Scholar]
- 107.Chukumnerd P, Hatthakit U, Chuaprapaisilp A. The experience of persons with allergic respiratory symptoms: practicing yoga as a self-healing modality. Holist Nurs Pract. 2011;25(2):63–70. doi: 10.1097/HNP.0b013e31820dbbae. [DOI] [PubMed] [Google Scholar]
- 108.Churangsarit S, Chongsuvivatwong V. Spatial and social factors Associated with transportation and recreational physical activity among adults in Hat Yai city, Songkhla, Thailand. J Phys Act Health. 2011;8(6):758–765. doi: 10.1123/jpah.8.6.758. [DOI] [PubMed] [Google Scholar]
- 109.Churproong S, Khampirat B, Ratanajaipan P, Tattathongkom P. The effect of the arm swing on the heart rate of non-athletes. J Med Associ Thai. 2015;98:S79–S86. [PubMed] [Google Scholar]
- 110.Dajpratham P, Chadchavalpanichaya N. Knowledge and practice of physical exercise among the inhabitants of Bangkok. J Med Assoc Thai. 2007;90(11):2470–2476. [PubMed] [Google Scholar]
- 111.Dancy C, Lohsoonthorn V, Williams MA. Risk of dyslipidemia in relation to level of physical activity among Thai professional and office workers. Southeast Asian J Trop Med Public Health. 2008;39(5):932–941. [PubMed] [Google Scholar]
- 112.Danyuthasilpe C, Amnatsatsue K, Tanasugarn C, Kerdmongkol P, Steckler AB. Ways of healthy aging: A case study of elderly people in a Northern Thai village. Health Promot Int. 2009;24(4):394–403. doi: 10.1093/heapro/dap038. [DOI] [PubMed] [Google Scholar]
- 113.Daraha K. The effect of the Internet use on high school students: A case study of Pattani province of Thailand. Psu-Usm International Conference on Humanities and Social Sciences. Procedia Soc Behav Sci. 2013;91:241–256. doi: 10.1016/j.sbspro.2013.08.422. [DOI] [Google Scholar]
- 114.Dasa P. Exercise behaviors and perceived barriers to exercise among female faculty members in Chiang Mai University. Chiang Mai: Graduate School, Chiang Mai University; 2001. [Google Scholar]
- 115.Decharat S, Phethuayluk P, Maneelok S. Prevalence of Musculoskeletal Symptoms among Dental Health Workers. Southern Thailand. Adv Prev Med. 2016;2016:1–6. doi: 10.1155/2016/5494821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dedkhard S. Risk factors of cardiovascular disease in rural Thai women. PhD [dissertation]. Arizona: University of Arizona; 2006.
- 117.Deenan A. A Comparative Study of Exercise Behaviors, Eating Behaviors, Serum Lipids, and Body Mass Index of Thai Adolescents: Urban and Rural Areas of the Eastern Seaboard of Thailand. Chonburi: Faculty of Nursing, Burapha University; 2001. [Google Scholar]
- 118.Deenan A. Testing the health promotion model with Thai adolescents. PhD [dissertation]. Missouri: Saint Louis University; 2003.
- 119.Deesomboon S. The home-based physical activities program in daily life among older adults. Bangkok: Faculty of Graduate Studies, Mahidol University; 2008. [Google Scholar]
- 120.Dennerstein L, Lehert P, Heinemann K. Global study of women's experiences of premenstrual symptoms and their effects on daily life. Menopause Int. 2011;17(3):88–95. doi: 10.1258/mi.2011.011027. [DOI] [PubMed] [Google Scholar]
- 121.Duangchan P, Yoelao D, Macaskill A, Intarakamhang U, Suprasonsin C. Interventions for healthy eating and physical activity among obese elementary schoolchildren: observing changes of the combined effects of behavioral models. Int J Behav Sci. 2010;5(1):46–59. [Google Scholar]
- 122.Duangtep Y, Narksawat K, Chongsuwat R, Rojanavipart P. Association between an unhealthy lifestyle and other factors with hypertension among hill tribe populations of Mae Fah Luang district, Chiang Rai Province, Thailand. Southeast Asian J Trop Med Public Health. 2010;41(3):726–734. [PubMed] [Google Scholar]
- 123.Eiamudomkan M, Sirirassamee T, Sirirassamee B. Consumption of vegetables, fruits, physical activity, and sedentary behaviors in Thai adolescents. J Med Health Sci. 2014;21(2):40–48. [Google Scholar]
- 124.Ekpanyaskul C, Sithisarankul P, Wattanasirichaigoon S. Overweight/obesity and related factors among Thai medical students. Asia-Pac J Public Health. 2013;25(2):170–180. doi: 10.1177/1010539511428665. [DOI] [PubMed] [Google Scholar]
- 125.Ethisan P, Chapman R, Kumar R, Somrogthong R. Effectiveness of group-mediated lifestyle physical activity program for health benefit in physical activity among elderly people at rural Thailand. Journal Ayub Med Col, Abbottabad: JAMC. 2015;27(2):292–295. [PubMed] [Google Scholar]
- 126.Ethisan P, Somrongthong R, Ahmed J, Kumar R, Chapman RS. Factors Related to Physical Activity Among the Elderly Population in Rural Thailand. J Prim Care Community Health. 2016;8(2):71–76. doi: 10.1177/2150131916675899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Fuangswasdi S. Need for exercising of personnel of the department of Foreign Ministry of Commerce. Bangkok: Graduate School, Ramkhamhaeng University; 1998. [Google Scholar]
- 128.Fuzhong L, Harmer P, Fisher KJ, Junheng X, Fitzgerald K, Vongjaturapat N. Tai Chi-Based Exercise for Older Adults With Parkinson's Disease: A Pilot-Program Evaluation. J Aging Phys Act. 2007;15(2):139–151. doi: 10.1123/japa.15.2.139. [DOI] [PubMed] [Google Scholar]
- 129.Geurgoolgitjagan N, Chongchareon W. Factors influencing Tai Chi-Chigong exercise by people in Southern Thailand. Songkla: Faculty of Nursing, Prince of Songkla University; 2008. [Google Scholar]
- 130.Gidlöf L, Retta Belay H. Habits related to television, computer games and eating among school children in a rural and an urban area of Thailand. Uppsala: Uppsala University; 2011. [Google Scholar]
- 131.Halvorsen A. Facebook usage in Thailand: The plurilingual competencies of Thai high school students and teachers. US: ProQuest Information & Learning; 2015. [Google Scholar]
- 132.Hamirattisai T, Johnson RA, Kawinwonggowit V. Evaluating functional activity in older Thai adults. Rehabil Nurs. 2006;31(3):124–128. doi: 10.1002/j.2048-7940.2006.tb00016.x. [DOI] [PubMed] [Google Scholar]
- 133.Harnirattisai T, Johnson RA. Effectiveness of a behavioral change intervention in Thai elders after knee replacement. Nurs Res. 2005;54(2):97–107. doi: 10.1097/00006199-200503000-00004. [DOI] [PubMed] [Google Scholar]
- 134.Henry CJ, Webster-Gandy J, Varakamin C. A comparison of physical activity levels in two contrasting elderly populations in Thailand. Am J Hum Biol. 2001;13(3):310–315. doi: 10.1002/ajhb.1054. [DOI] [PubMed] [Google Scholar]
- 135.Hirohide Y, Motoyuki Y, Nedsuwan S, Moolphate S, Hiroshi F, Tsutomu K, et al. Daily salt intake estimated by overnight urine collections indicates a high cardiovascular disease risk in Thailand. Asia Pac J Clin Nutr. 2016;25(1):39–45. doi: 10.6133/apjcn.2016.25.1.22. [DOI] [PubMed] [Google Scholar]
- 136.Hiruntrakul A, Nanagara R, Emasithi A, Borer K. Effect of once a week endurance exercise on fitness status in sedentary subjects. J Med Assoc Thai. 2010;93(9):1070–1074. [PubMed] [Google Scholar]
- 137.Hiruntrakul A, Nanagara R, Emasithi A, Borer KT. Effect of endurance exercise on resting testosterone levels in sedentary subjects. Cent Eur J Public Health. 2010;18(3):169–172. doi: 10.21101/cejph.a3589. [DOI] [PubMed] [Google Scholar]
- 138.Howteerakul N, Suwannapong N, Rittichu C, Rawdaree P. Adherence to regimens and glycemic control of patients with type 2 diabetes attending a tertiary Hospital Clinic. Asia-Pac J Public Health. 2007;19(1):43–49. doi: 10.1177/10105395070190010901. [DOI] [PubMed] [Google Scholar]
- 139.Howteerakul N, Suwannapong N, Sittilerd R, Rawdaree P. Health risk behaviors, awareness, treatment and control of hypertension among rural community people in Thailand. Asia-Pac J Public Health. 2006;18(1):3–9. doi: 10.1177/10105395060180010201. [DOI] [PubMed] [Google Scholar]
- 140.Howteerakul N, Suwannapong N. Than M. Cigarette, alcohol use and physical activity among Myanmar youth workers, Samut Sakhon Province, Thailand. Southeast Asian J Trop Med Public Health. 2005;36(3):790–796. [PubMed] [Google Scholar]
- 141.In-Iw S, Manaboriboon B, Chomchai C. A comparison of body-image perception, health outlook and eating behavior in mildly obese versus moderately-to-severely obese adolescents. J Med Assoc Thai. 2010;93(4):429–435. [PubMed] [Google Scholar]
- 142.In-iw S, Suchritpongsa S, Manaboriboon B, Chomchai C. Obesity in Thai adolescents: lifestyles, health attitudes and psychosocial concerns. Siriraj Med J. 2010;62(6):245–249. [Google Scholar]
- 143.Ing-Arahm R, Suppuang A, Imjaijitt W. The study of medical students’ attitudes toward exercise for health promotion in Phramongkutklao College of Medicine. J Med Assoc Thai = Chotmaihet thangphaet. 2010;93(Suppl 6):S173–S178. [PubMed] [Google Scholar]
- 144.Insawang T, Selmi C, Cha'on U, Pethlert S, Yongvanit P, Areejitranusorn P, et al. Monosodium glutamate (MSG) intake is associated with the prevalence of metabolic syndrome in a rural Thai population. Nutr Metab. 2012;9:1–6. doi: 10.1186/1743-7075-9-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Intachat N. The Influence of Bio-Sociology and Behavioral Factors on Thai Adult Mortality in the Northeastern Community of Thailand. Crisis Management in the Time of Changing World. Adv Intell Syst Res. 2012;63:365–374. [Google Scholar]
- 146.Intarakamhang P, Chintanaprawasee P. Effects of Dao De Xin Xi exercise on balance and quality of life in Thai elderly women. Glob J Health Sci. 2012;4(1):237–244. doi: 10.5539/gjhs.v4n1p237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Intipanya P. Relationships between personal factors, lifestyle, and health outcomes in gestational diabetes mellitus women. Bangkok: Faculty of Nursing, Chulalongkorn University; 2005. [Google Scholar]
- 148.Intorn S. Relationships between selected factors and exercise behaviors of middle aged adult in Nakorn Sawan province. Bangkok: Faculty of Nursing, Chulalongkorn University; 2003. [Google Scholar]
- 149.Intusoma U, Mo-Suwan L, Chongsuvivatwong V. Duration and practices of television viewing in Thai infants and toddlers. J Med Assoc Thai. 2013;96(6):650–653. [PubMed] [Google Scholar]
- 150.Intusoma U, Mo-suwan L, Ruangdaraganon N, Panyayong B, Chongsuvivatwong V. Effect of television viewing on social-emotional competence of young Thai children. Infant Behav Dev. 2013;36(4):679–685. doi: 10.1016/j.infbeh.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 151.Isarabhakdi P, Pewnil T. Engagement with family, peers, and Internet use and its effect on mental well-being among high school students in Kanchanaburi Province, Thailand. Int J Adolesc Youth. 2016;21(1):15–26. doi: 10.1080/02673843.2015.1024698. [DOI] [Google Scholar]
- 152.Ishimaru T, Arphorn S. Hematocrit levels as cardiovascular risk among taxi drivers in Bangkok. Thailand. Industrial health. 2016;54:433–8. doi: 10.2486/indhealth.2015-0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ivanovitch K, Klaewkla J, Chongsuwat R, Viwatwongkasem C, Kitvorapat W. The intake of energy and selected nutrients by Thai urban sedentary workers: an evaluation of adherence to dietary recommendations. J Nutr Metab. 2014;2014:17. doi: 10.1155/2014/145182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Jaarsma T, Strömberg A, Ben Gal T, Cameron J, Driscoll A, Duengen HD, et al. Comparison of self-care behaviors of heart failure patients in 15 countries worldwide. Patient Educ Couns. 2013;92(1):114–120. doi: 10.1016/j.pec.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 155.Jaikhamwang N. Risk behaviors of diabetes and hypertension risk groups: a case study in Ban Pak Ka Yang sub-district, health promoting hospital, Sukhothai province. J Community Dev Life Qual. 2015;3(2):173–184. [Google Scholar]
- 156.Jaitam A. Factors affecting health promoting behaviors of hypertensive patients at Chaturapakpiman hospital, Roi Et province. Khon Kaen: Graduate School, Khon Kaen University; 2002. [Google Scholar]
- 157.Jaiyungyuen U, Suwonnaroop N, Priyatruk P, Moopayak K. Factors influencing health-promoting behaviors of older people with hypertension. 1st Mae Fah Luang University International Conference 2012. Chiang Rai: Mae Fah Luang University; 2012. pp. 1–9. [Google Scholar]
- 158.Jalayondeja C, Jalayondeja W, Suttiwong J, Sullivan PE, Nilanthi D. Physical Activity, Self-Esteem, and Quality of Life among People with Physical Disability. Southeast Asian J Trop Med Public Health. 2016;47(3):546–558. [PubMed] [Google Scholar]
- 159.Jalayondeja C, Jalayondeja W, Vachalathiti R, Bovonsunthonchai S, Sakulsriprasert P, Kaewkhuntee W, et al. Cross-cultural adaptation of the compendium of physical activity: Thai translation and content validity. J Med Assoc Thai. 2015;98(Suppl 5):S53–SS9. [PubMed] [Google Scholar]
- 160.Jamjan L, Maliwan V, Pasunant N, Sirapo-ngam Y, Porthiban L. Self-Image of Aging: A Method for Health Promotion. Nurs Health Sci. 2002;4(3):A6. doi: 10.1046/j.1442-2018.2002.01140_14.x. [DOI] [Google Scholar]
- 161.Janbumrung S. Need for exercising of personnel in Pramongkutklao hospital. Bangkok: Physical Education, Ramkhamhaeng University; 1998. [Google Scholar]
- 162.Jantarapakde J, Phanuphak N, Chaturawit C, Pengnonyang S, Mathajittiphan P, Takamtha P, et al. Prevalence of metabolic syndrome among antiretroviral-naive and antiretroviral-experienced HIV-1 infected Thai adults. AIDS Patient Care STDs. 2014;28(7):331–340. doi: 10.1089/apc.2013.0294. [DOI] [PubMed] [Google Scholar]
- 163.Janyacharoen T, Kunbootsri N, Arayawichanon P, Chainansamit S, Sawanyawisuth K. Responses of Six-Weeks Aquatic Exercise on the Autonomic Nervous System, Peak Nasal Inspiratory Flow and Lung Functions in Young Adults with Allergic Rhinitis. Iran J Allergy, Asthma Immunol. 2015;14(3):280–286. [PubMed] [Google Scholar]
- 164.Janyacharoen T, Laophosri M, Kanpittaya J, Auvichayapat P, Sawanyawisuth K. Physical performance in recently aged adults after 6 weeks traditional Thai dance: A randomized controlled trial. Clin Interv Aging. 2013;8:855–859. doi: 10.2147/CIA.S41076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Janyacharoen T, Phusririt C, Angkapattamakul S, Hurst CP, Sawanyawisuth K. Cardiopulmonary effects of traditional Thai dance on menopausal women: A randomized controlled trial. J Phys Ther Sci. 2015;27(8):2569–2572. doi: 10.1589/jpts.27.2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Janyacharoen T, Sirijariyawat K, Nithiatthawanon T, Pamorn P, Sawanyawisuth K. Modified stepping exercise improves physical performances and quality of life in healthy elderly subjects. J Sports Med Phys Fitness. 2016;57(10):1344–8. doi: 10.23736/S0022-4707.16.06439-2. [DOI] [PubMed] [Google Scholar]
- 167.Jareonpol O, Paisanpattanasakul Y, Chottidao M. Physical activity and physical fitness level of Mahidol University Employee, s Salaya Campus. Thammasat Med J. 2014;14(4):562–571. [Google Scholar]
- 168.Jarupanich T. Prevalence and risk factors associated with osteoporosis in women attending menopause clinic at Hat Yai Regional Hospital. J Med Assoc Thai. 2007;90(5):865–869. [PubMed] [Google Scholar]
- 169.Jaruratanasirikul S, Wongwaitaweewong K, Sangsupawanich P. Electronic game play and school performance of adolescents in Southern Thailand. Cyberpsychol Behav. 2009;12(5):509–512. doi: 10.1089/cpb.2009.0035. [DOI] [PubMed] [Google Scholar]
- 170.Jaruwan P, Arpaporn P, Sunee L, Jeeranun K. The diamond level health promoting schools (DLHPS) program for reduced child obesity in Thailand: lessons learned from interviews and focus groups. Asia Pac J Clin Nutr. 2014;23(2):293–300. doi: 10.6133/apjcn.2014.23.2.17. [DOI] [PubMed] [Google Scholar]
- 171.Jermsuravong W, Vongjaturapat N, Li F. The influence of exercise motivation on exercise behavior among Thai youth. J Popul Soc Stud. 2008;17(1):93–114. [Google Scholar]
- 172.Jewpattanakul Y, Reungthongdee U, Tabkaew T. The effect of the arm swing exercise with family participation program on exercise behavior in elderly with essential hypertension. J Nurs Sci. 2012;30(2):46–57. [Google Scholar]
- 173.Jiamjarasrangsi W, Attavorrarat S, Navicharern R, Aekplakorn W, Keesukphan P. Assessment of 5-year system-wide type 2 diabetes control measures in a Southeast Asian metropolis. Asian Biomedicine. 2014;8(1):75–82. doi: 10.5372/1905-7415.0801.264. [DOI] [Google Scholar]
- 174.Jindawong B, Kuhiranyaratn P, Paileeklee S, Ratanasiri A, See-Ubpalad W. Type, duration, and effect of physical exercise on chronic health diseases among urban elderly in Khon Kaen Province, Thailand. J Aging Phys Act. 2008;16:S57. [Google Scholar]
- 175.Jirapinyo P, Wongarn R, Limsathayourat N, Maneenoy S, Somsa-Ad K, Thinpanom N, et al. Adolescent Height : Relationship to Exercise, Milk Intake and Parents’ Height. J Med Assoc Thai. 1997;80(10):641–646. [PubMed] [Google Scholar]
- 176.Jirasatmathakul P, Poovorawan Y. Prevalence of video games among Thai children: Impact evaluation. J Med Assoc Thai. 2000;83(12):1509–1513. [PubMed] [Google Scholar]
- 177.Jirojanakul P, Skevington SM, Hudson J. Predicting young children's quality of life. Soc Sci Med. 2003;57(7):1277–1288. doi: 10.1016/S0277-9536(02)00507-5. [DOI] [PubMed] [Google Scholar]
- 178.Jitapunkul S, Yuktananandana P, Parkpian V. Risk factors of hip fracture among Thai female patients. J Med Assoc Thai. 2001;84(11):1576–1581. [PubMed] [Google Scholar]
- 179.Jitnarin N, Kosulwat V, Boonpraderm A, Haddock CK, Poston WS. The relationship between smoking, BMI, physical activity, and dietary intake among Thai adults in central Thailand. J Med Assoc Thai. 2008;91(7):1109–1116. [PubMed] [Google Scholar]
- 180.Jitramontree N. Predicting exercise behavior among Thai elders: Testing the theory of planned behavior. PhD [dissertation] Iowa: University of Iowa; 2003. [Google Scholar]
- 181.Jitsacorn C. Perceived benefits and barriers to exercise behavior in coronary artery disease patients. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2000. [Google Scholar]
- 182.Jordan S, Lim L, Berecki-Gisolf J, Bain C, Seubsman SA, Sleigh A, et al. Body mass index, physical activity, and fracture among young adults: longitudinal results from the Thai cohort study. J Epidemiol. 2013;23(6):435–442. doi: 10.2188/jea.JE20120215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Jordan S, Lim L, Vilainerun D, Banks E, Sripaiboonkij N, S-a S, et al. Breast cancer in the Thai Cohort Study: an exploratory case-control analysis. Breast. 2009;18(5):299–303. doi: 10.1016/j.breast.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Julvanichpong T. Predictive Factors of Exercise Behaviors of Junior High School Students in Chonburi Province. World Acad Sci, Eng Technol, Int J Soc, Behav, Educ, Econ, Bus Ind Eng. 2015;9(7):2633–2638. [Google Scholar]
- 185.Junhasiri N. The effect of an aerobic exercise upon the physical fitness components in elderly women. Bangkok: Srinakharinwirot University; 1993. [Google Scholar]
- 186.Junlapeeya P. Model testing of exercise behavior in Thai female registered nurses in an urban hospital. Baltimore: University of Maryland; 2005. [Google Scholar]
- 187.Kabkaew T. Factors affecting exercise behavior of assistant-nurse students, Hospital for Tropical Disease, Mahidol University. Bangkok: Graduate School, Kasetsart University; 2006. [Google Scholar]
- 188.Kaewanuchit C. A path analysis of mental health among Thai elderly with diabetes mellitus. Pertanika J Sci Technol. 2016;24(2):285–294. [Google Scholar]
- 189.Kaewboonchoo O, Saleekul S, Powwattana A, Kawai T. Blood lead level and blood pressure of bus drivers in Bangkok, Thailand. Ind Health. 2007;45(4):590–594. doi: 10.2486/indhealth.45.590. [DOI] [PubMed] [Google Scholar]
- 190.Kaewpan W, Kalampakorn S. Health status and health promoting behaviors among aging workers in Thailand. J Med Assoc Thai. 2012;95(SUPPL 6):S16–S20. [PubMed] [Google Scholar]
- 191.Kaewpan W, Kalampakorn S, Luksamijarulkul P. Factors related to health-promoting behaviors among Thai middle-aged men. J Med Assoc Thai= Chotmaihet thangphaet. 2007;90(9):1916–1924. [PubMed] [Google Scholar]
- 192.Kaewthong P, Buranruk O, Eungpinitpong W, Soontarapa S. Comparison of Ruesidadton-Chikung combination exercise and Taichi exercise on lower extremities strength and balance in sedentary middle-aged women. J Med Technol Phys Ther. 2015;27(1):79–86. [Google Scholar]
- 193.Kaewthummanukul T, Brown KC, Weaver MT, Thomas RR. Predictors of exercise participation in female hospital nurses. J Adv Nurs. 2006;54(6):663–675. doi: 10.1111/j.1365-2648.2006.03854.x. [DOI] [PubMed] [Google Scholar]
- 194.Kaewthummanukul T, Chanprasit C, Poosawang R, Tripibool D, Songkham W. Predictors of exercise among practical nurses. Nurs J. 2008;35(1):22–35. [Google Scholar]
- 195.Kaewwit R. Factors Influencing the Internet Using Behavior of Undergraduate Students in Bangkok and Suburban Areas. BU Acad Rev. 2007;6(1):26–33. [Google Scholar]
- 196.Kallaya K, Thasanasuwan W, Wimonpeerapattana W, Seaburin W, Srichan W, Kunapan P. Relationship of Physical Activity Level, Percent Body Fat, Percent Lean Body Mass and Bone Z-Score in Thai Adolescents. Ann Nutr Metab. 2009;55:717. [Google Scholar]
- 197.Kanchanomai S, Janwantanakul P, Jiamjarasrangsi W. One-year Incidence and Risk Factors of Thoracic Spine Pain in Undergraduate Students. J Phys Ther Sci. 2013;25(1):15–20. doi: 10.1589/jpts.25.15. [DOI] [Google Scholar]
- 198.Kanchanomai S, Janwantanakul P, Pensri P, Jiamjarasrangsi W. Prevalence of and factors associated with musculoskeletal symptoms in the spine attributed to computer use in undergraduate students. Work. 2012;43(4):497–506. doi: 10.3233/WOR-2012-1387. [DOI] [PubMed] [Google Scholar]
- 199.Kantachuvessiri A, Sirivichayakul C, Kaewkungwal J, Tungtrongchitr R, Lotrakul M. Factors associated with obesity among workers in a metropolitan waterworks authority. Southeast Asian J Trop Med Public Health. 2005;36(4):1057–1065. [PubMed] [Google Scholar]
- 200.Kanthamalee S, Panuthai S, Chaiwan S. Effects of the self-efficacy and social support enhancement program on exercise behavior and blood pressure among hypertensive elderly. Nurs J. 2007;34(4):93–103. [Google Scholar]
- 201.Karoonngamphan M, Suvaree S, Numfone N. Health Behaviors and Health Status of Workers: A Case Study of Workplaces in Sathorn District, Bangkok Metropolitan. Songklanagarind J Nurs. 2012;32(3):51–66. [Google Scholar]
- 202.Karuncharernpanit S. The effect of an exercise intervention on physical and cognitive function, psychological health and quality of life among older adults with dementia in Bangkok, Thailand. Western Australia: Faculty of Computing, Health and Science, Edith Cowan University; 2012. [Google Scholar]
- 203.Karuncharernpanit S, Hendricks J, Toye C. Perceptions of exercise for older people living with dementia in Bangkok, Thailand: an exploratory qualitative study. Int J Older People Nurs. 2016;11(3):166–175. doi: 10.1111/opn.12091. [DOI] [PubMed] [Google Scholar]
- 204.Keawduangdee P, Puntumetakul R, Swangnetr M, Laohasiriwong W, Settheetham D, Junichiro Y, et al. Prevalence of low back pain and associated factors among farmers during the rice transplanting process. J Phys Ther Sci. 2015;27(7):2239–2245. doi: 10.1589/jpts.27.2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Keawvilai S. The predictive factors on exercise behaviors of undergraduate students Rajamangala University of Technology Phra Nakhon. Bangkok: Rajamangala University of Technology Phra Nakhon; 2009. [Google Scholar]
- 206.Ketkasan N, Pongpanich S. Examining stages of readiness exercise behavior change among Thai university students. Seoul: KPEAW International Symposium; 2013. pp. 175–176. [Google Scholar]
- 207.Kheawwan P, Chaiyawat W, Aungsuroch Y, Bill Wu YW. Patient readiness to exercise after cardiac surgery development of the readiness to change exercise questionnaire. J Cardiovasc Nurs. 2016;31(2):186–193. doi: 10.1097/JCN.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 208.Kheokao J, Siriwanij W, Yingrengreung S, Krirkgulthorn T, Panidchakult K. Media Use of Nursing Students in Thailand. 2015 4th International Symposium on Emerging Trends and Technologies in Libraries and Information Services (Ettlis) 2015. pp. 123–127. [Google Scholar]
- 209.Khongprasert S, Bhidayasiri R, Kanungsukkasem V. A Thai dance exercise regimen for people with Parkinson's disease. J Health Res. 2012;26(3):125–129. [Google Scholar]
- 210.Khongprasert S, Bhidayasiri R, Kanungsukkasem V. Thai Classical Dance: From being part of the culture to being an exercise. Mov Disord. 2014;29:S15–S1S. doi: 10.1002/mds.25741. [DOI] [Google Scholar]
- 211.Khotcharrat R, Patikulsila D, Hanutsaha P, Khiaocham U, Ratanapakorn T, Sutheerawatananonda M, et al. Epidemiology of age-related macular degeneration among the elderly population in Thailand. J Med Assoc Thai. 2015;98(8):790–797. [PubMed] [Google Scholar]
- 212.Khruakhor S, Sritipsukh P, Siripakar Y, Vachalathit R. Prevalence and risk factors of low back pain among the university staff. J Med Assoc Thai. 2010;93(SUPPL 7):S142–S1S8. [PubMed] [Google Scholar]
- 213.Khui-apai K. Effect of Tai Chi Qigong exercise on blood pressure and drug use among the elderly with essential hypertension. Chiang Mai: Graduate School, Chiang Mai University; 2005. [Google Scholar]
- 214.Khumprommarach S. Effects of minifitball exercise program on health-related physical fitness and quality of life in working women. Bangkok: Faculty of Sports Science, Chulalongkorn University; 2010. [Google Scholar]
- 215.Khumsri J, Yingyeun R, Manwong M, Hanprathet N, Phanasathit M. Prevalence of facebook addiction and related factors among Thai high school students. J Med Assoc Thai. 2015;98:S51–S60. [PubMed] [Google Scholar]
- 216.Khunphasee A. Attitude to exercise and cardiopulmonary endurance fitness in staff of rehabilitation department at Phramongkutklao hospital. Royal Thai Army Med J. 2010;63(3):125–134. [Google Scholar]
- 217.Khuntongkaew S. Exercise behavior among health group members at Ratchaburi province. Bangkok: Graduate School, Silpakorn University; 2005. [Google Scholar]
- 218.Khwanchuea R, Thanapop S, Samuhasaneeto S, chartwaingam S, Mukem S. Bone Mass, Body Mass Index, and Lifestyle Factors: A Case Study of Walailak University Staff. Walailak J Sei & Teeh. 2012;9(3):263-75.
- 219.Kiatrungrit K, Hongsanguansri S. Cross-sectional study of use of electronic media by secondary school students in Bangkok, Thailand. Shanghai Arch Psychiatry. 2014;26(4):216–226. doi: 10.3969/j.issn.1002-0829.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Kijboonchoo K, Thasanasuwan W, Seaburin W, Wimonpeerapattana W, Srichan W, Kunapan PI. There Any Gender Difference in Physical Activity Level in Thai Adolescents? Ann Nutr Metab. 2009;55:570. [Google Scholar]
- 221.Kijboonchoo K, Thasanasuwan W, Yamborisut U, Tatsameesopaporn W, Jitjang U, Srichan W. Report of the development of validated body fat, body mass index, and physical activity assessment for Thai children. Bangkok: Institute of Nutrition, Mahidol University; 2007. [Google Scholar]
- 222.Kitrungpipat N, Phannithit A. Self-health care behavior student in Silpakorn University Phrtchaburi IT Campus. Bangkok: Faculty of Management Science, Silpakorn University; 2012. [Google Scholar]
- 223.Kittipimpanon K. Factors Associated with Physical Performance Among Elderly in Urban Poor Community. Nakorn Pathom: Faculty of Graduate Studies, Mahidol University; 2006. [Google Scholar]
- 224.Klainin-Yobas P, He HG, Lau Y. Physical fitness, health behavior and health among nursing students: A descriptive correlational study. Nurse Educ Today. 2015;35(12):1199–1205. doi: 10.1016/j.nedt.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 225.Klanarong S. Socio-demographic distribution of health-related fitness of Thai children. South Australia: University of South Australia; 2005. [Google Scholar]
- 226.Kongcheewasakul C, Klanarong S, Sathirapanya C. Exercise behavior for health of Rajamangala Srivijaya university students, Songkhla Campus. AL-NUR. 2014;9(16):59–70. [Google Scholar]
- 227.Kongin W. Self-care of the rural Thai elderly. PhD [dissertation]. District of Columbia (DC): Catholic University of America; 1998.
- 228.Kongkanand A. Prevalence of erectile dysfunction in Thailand. Thai Erectile Dysfunction Epidemiological Study Group. Int J Androl. 2000;23(Suppl 2):77–80. doi: 10.1046/j.1365-2605.2000.00022.x. [DOI] [PubMed] [Google Scholar]
- 229.Konharn K, Karawa J, Maneetam T, Puangsuwan A, Kosolsak M, Nakornkhet K. Validity and reliability of the physical activity questionnaire for Thai children and youth 2015 in age 14–17 year. Bangkok: Physical Activity Research Centre, Thai Health Promotion Foundation; 2016.
- 230.Konharn K, Santos MP, Ribeiro JC. Socioeconomic status and objectively measured physical activity in Thai adolescents. J Phys Act Health. 2014;11(4):712–720. doi: 10.1123/jpah.2011-0424. [DOI] [PubMed] [Google Scholar]
- 231.Konharn K, Santos MP, Ribeiro JC. Differences between weekday and weekend levels of moderate-to-vigorous physical activity in Thai adolescents. Asia-Pac J Public Health. 2015;27(2):NP2157–NPNP66. doi: 10.1177/1010539512459946. [DOI] [PubMed] [Google Scholar]
- 232.Kornanong Y. Effects of 10,000 steps a day on physical and mental health in overweight participants in a community setting: a preliminary study. Braz J Phys Ther / Revista Brasileira de Fisioterapia. 2016;20(4):367–373. doi: 10.1590/bjpt-rbf.2014.0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Kraithaworn P, Sirapo-ngam Y, Piaseu N, Nityasuddhi D, Gretebeck KA. Factors predicting physical activity among older Thais living in low socioeconomic urban communities. Pac Rim Int J Nur Res. 2011;15(1):39–56. [Google Scholar]
- 234.Krittatunmakul S. Guidelines for transport system improvement for promoting physical activities of Trang city. Bangkok: Faculty of Architecture, Chulalongkorn University; 2013. [Google Scholar]
- 235.Kruavit A, Chailurkit LO, Thakkinstian A, Sriphrapradang C, Rajatanavin R. Prevalence of Vitamin D insufficiency and low bone mineral density in elderly Thai nursing home residents. BMC Geriatrics. 2012;12(1):49. doi: 10.1186/1471-2318-12-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Kuhiranyaratn P, Jindawong B, Paileeklee S, Ratanasiri A, See-Ubpalad W. Social support and physical exercise among rural elderly in Khon Kaen province, Thailand. J Aging Phys Act. 2008;16:S186–S18S. [Google Scholar]
- 237.Kuhirunyaratn P, Prasomrak P, Jindawong B. Factors related to falls among community dwelling elderly. Southeast Asian J Trop Med Public Health. 2013;44(5):906–915. [PubMed] [Google Scholar]
- 238.Kumkate B, Wongpat P, Sanjaroensuttikul N. Effect of Tai Chi Chun exercise on balance in Thai elderly people. J Thai Rehabil Med. 2007;17(3):73–78. [Google Scholar]
- 239.Kuptniratsaikul V, Tosayanonda O, Nilganuwong S, Thamalikitkul V. The Efficacy of a Muscle Exercise Program to Improve Functional Performance of the Knee in Patients with Osteoarthritis. J Med Assoc Thai. 2002;85(1):33–40. [PubMed] [Google Scholar]
- 240.Kuramasuwan B, Howteerakul N, Suwannapong N, Rawdaree P. Diabetes, impaired fasting glucose, daily life activities, food and beverage consumption among Buddhist monks in Chanthaburi Province, Thailand. Int J Diabetes Dev Countries. 2013;33(1):23–28. doi: 10.1007/s13410-012-0094-y. [DOI] [Google Scholar]
- 241.Kurmlue P. Factors affecting Payap university students. Chiang Mai: Graduate School, Chiang Mai University; 2000. [Google Scholar]
- 242.L-Y, Lim L, Kjellstrom T, Sleigh A, Khamman S, Seubsman S-A, Dixon J, et al. Associations between urbanisation and components of the health-risk transition in Thailand. A descriptive study of 87,000 Thai adults. Global Health Action. 2009;2(1):1914. [DOI] [PMC free article] [PubMed]
- 243.Lam LCW, Ong PA, Dikot Y, Sofiatin Y, Wang H, Zhao M, et al. Intellectual and physical activities, but not social activities, are associated with better global cognition: A multi-site evaluation of the cognition and lifestyle activity study for seniors in Asia (CLASSA) Age Ageing. 2015;44(5):835–840. doi: 10.1093/ageing/afv099. [DOI] [PubMed] [Google Scholar]
- 244.Laophosri M, Kanpittaya J, Sawanyawisuth K, Auvichayapat P, Janyacharoen T. Effects of Thai dance on balance in Thai elderly. Chula Med J. 2013;57(3):345–357. [Google Scholar]
- 245.Laosupap K, Sota C, Laopaiboon M. Factors affecting physical activity of rural Thai midlife women. J Med Assoc Thai. 2008;91(8):1269–1275. [PubMed] [Google Scholar]
- 246.Lau EM, Suriwongpaisal P, Lee JK, Das De S, Festin MR, Saw SM, et al. Risk factors for hip fracture in Asian men and women: the Asian osteoporosis study. J Bone Miner Res. 2001;16(3):572–580. doi: 10.1359/jbmr.2001.16.3.572. [DOI] [PubMed] [Google Scholar]
- 247.Lavichant A. Factors affecting the internet usage behavior of undergraduate and graduate students in Bangkok metropolitan area. Bangkok: Graduate School, Srinakharinwirot University; 2006. [Google Scholar]
- 248.Lazzarino AI, Yiengprugsawan V, Sam-ang S, Steptoe A, Sleigh AC. The associations between unhealthy behaviours, mental stress, and low socio-economic status in an international comparison of representative samples from Thailand and England. Glob Health. 2014;10(1):1–18. doi: 10.1186/1744-8603-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Le D, Garcia A, Lohsoonthorn V, Williams MA. Prevalence and risk factors of hypercholesterolemia among Thai men and women receiving health examinations. Southeast Asian J Trop Med Public Health. 2006;37(5):1005–1014. [PubMed] [Google Scholar]
- 250.Leelacharas S, Kerdonfag P, Chontichachalalauk J, Sanongdej W. Illness Perceptions, Lifestyle Behaviors, Social Support, and Cardiovascular Risks in People with Hypertension in Urban and Rural Areas of Thailand. Pac Rim Int J Nurs Res. 2015;19(3):245–256. [Google Scholar]
- 251.Leelarungrayub D, Pratanaphon S, Pothongsunun P, Sriboonreung T, Yankai A, Bloomer RJ. Vernonia cinerea less supplementation and strenuous exercise reduce smoking rate: relation to oxidative stress status and beta-endorphin release in active smokers. J Int Soc Sports Nutr. 2010;7:21–30. doi: 10.1186/1550-2783-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Leelarungrayub D, Saidee K, Pothongsunun P, Pratanaphon S, YanKai A, Bloomer RJ. Six weeks of aerobic dance exercise improves blood oxidative stress status and increases interleukin-2 in previously sedentary women. J Bodyw Mov Ther. 2011;15(3):355–362. doi: 10.1016/j.jbmt.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 253.Leelayuwat N, Tunkumnerdthai O, Donsom M, Punyaek N, Manimanakorn A, Kukongviriyapan U, et al. An alternative exercise and its beneficial effects on glycaemic control and oxidative stress in subjects with type 2 diabetes. Diabetes Res Clin Pract. 2008;82(2):e5–e8. doi: 10.1016/j.diabres.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 254.Leemingsawat W, Chakraphan D, Benjapalakorn B, Kamawatana U, Siripatt A. A study of exercise behaviors of students in higher education institutes. J Sports Sci Health. 2007;8(1):24–37. [Google Scholar]
- 255.Leethong-in M. A causal model of physical activity in healthy older Thai people. Bangkok: Faculty of Nursing, Chulalongkorn University; 2009. [Google Scholar]
- 256.Leethong-in M, Yunibhand J, Aungsuroch Y, Magiivy JK, Leethong-in M, Yunibhand J, et al. Assessment of the environmental support for physical activity scale among Thai elderly. Chula Med J. 2011;55(5):421–435. [Google Scholar]
- 257.Leggat PA, Chowanadisai S, Kedjarune U, Kukiattrakoon B, Yapong B. Health of dentists in southern Thailand. Int Dental J. 2001;51(5):348–352. doi: 10.1002/j.1875-595X.2001.tb00848.x. [DOI] [PubMed] [Google Scholar]
- 258.Lerssrimongkol C, Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, Lam KB. Active commuting and cardiovascular risk among health care workers. Occup Med (Oxford, England). 2016;66(6):483–487. doi: 10.1093/occmed/kqw029. [DOI] [PubMed] [Google Scholar]
- 259.Liangchawengwong S, Pothiban L, Panuthai S, Boonchuang P. Prevalence, Stages of Change for Lifestyle-Related Cardiovascular Risk Factors, and Influencing Factors of Physical Activity among Thai Young Adults. Pac Rim Int J Nurs Res. 2013;17(3):217–233. [Google Scholar]
- 260.Limachan R. Physical activity and health status of professional nurses at Bangkok Metropolitan Administration Medical College and Vajira hospital. Bangkok: Graduate School, Srinakharinwirot University; 2006. [Google Scholar]
- 261.Limpaphayom K, Bunyavejchevin S, Panyakhamlerd K, Poshyachinda M, Taechakraichana N. Risk factors of osteoporosis in Thai postmenopausal women attending menopause clinic at Chulalongkorn Hospital. 1st Asian-European Congress on the Menopause. 1998. pp. 181–185. [Google Scholar]
- 262.Limpawattana P, Assantachai P, Krairit O, Kengkijkosol T, Wittayakom W, Pimporm J, et al. The predictors of skeletal muscle mass among young Thai adults: A study in the rural area of Thailand. Biomed Res (India). 2016;27(1):29–33. [Google Scholar]
- 263.Lindholm A, Baylis R. Food consumption, physical activity and sedentary activities among 12-13 year old school children in a rural and an urban area of Thailand. Uppsala: Uppsala University; 2009. [Google Scholar]
- 264.Loipha S. Thai Elderly Behavior of Internet Use. 3rd International Conference on Integrated Information. Procedia Soc Behav Sci. 2014;147:104–110. doi: 10.1016/j.sbspro.2014.07.125. [DOI] [Google Scholar]
- 265.Lundberg PC, Thrakul S. Diabetes type 2 self-management among Thai Muslim women. J Nurs Healthc Chronic Illn. 2011;3(1):52–60. doi: 10.1111/j.1752-9824.2011.01079.x. [DOI] [Google Scholar]
- 266.Mahanonda N, Bhuripanyo K, Leowattana W, Kangkagate C, Chotinaiwattarakul C, Panyarachun S, et al. Regular exercise and cardiovascular risk factors. J Med Assoc Thai. 2000;83(Suppl 2):S153–S1S8. [PubMed] [Google Scholar]
- 267.Mai-um W, Hiransuthikul N, Sritara P, Tunlayadechanont S, Larbcharoensub N, Wongwichai S, et al. Stroke incidences and related factors among employees working at the central office of the electricity generating authority of Thailand (EGAT): a prospective-descriptive study. J Health Res. 2014;28(1):13–21. [Google Scholar]
- 268.Makesrithongkum B, editor. Internet use of Thai children and youth at various stages of age development. 2009. [Google Scholar]
- 269.Mamom J. AOS8 Effectiveness of an education-combining exercise programme for chemotherapy-related fatigue in women with breast cancer. Eur J Cancer. 2012;48(s4):S6–SS. doi: 10.1016/j.ejca.2012.02.025. [DOI] [Google Scholar]
- 270.Mandal GK. Physical activity, dietary habits and blood pressure of hypertensive patients in Phutthamonthon district, Nakorn Pathom province, Thailand. Nakorn Pathom: Faculty of Graduate Studies, Mahidol University; 2009. [Google Scholar]
- 271.Maneedang P. The Effectiveness of Dietary and Exercise Behavior Development Program for Overweight Students. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2007. [Google Scholar]
- 272.Mateeskunkan S. A Motivational Study of Exerciser in Bangkok Metropolitan Administration Public Parks. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2003. [Google Scholar]
- 273.McCaffrey R, Ruknui P, Hatthakit U, Kasetsomboon P. The effects of yoga on hypertensive persons in Thailand. Holist Nurs Pract. 2005;19(4):173–180. doi: 10.1097/00004650-200507000-00009. [DOI] [PubMed] [Google Scholar]
- 274.Merakate J. Leisure participation of youths aged between 12-18 at Suk Samran district, Ranong Province. Kasetsart J - Soc Sci. 2007;28(2):202–209. [Google Scholar]
- 275.Methapatara W, Srisurapanont M. Pedometer walking plus motivational interviewing program for Thai schizophrenic patients with obesity or overweight: A 12-week, randomized, controlled trial. Psychiatry Clin Neurosc. 2011;65(4):374–380. doi: 10.1111/j.1440-1819.2011.02225.x. [DOI] [PubMed] [Google Scholar]
- 276.Mhaopech K, Choupanich K, Lapho P, Teamtaokerd W. Behaviors for exercises of personnel in Kasetsart University, Kampheangsaen Campus. Bangkok: Kasetsart University, and Thai Health Promotion Foundation; 2012. [Google Scholar]
- 277.Mizumoto K. Hypertension and risk factors related to lifestyle among women aged 40 years and over in Phuthamontthon district, Nakhon Pathom province, Thailand. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2004. [Google Scholar]
- 278.Mo-suwan L, Junjana C, Puetpaiboon A. Increasing obesity in school children in a transitional society and the effect of the weight control program. Southeast Asian J Trop Med Public Health. 1993;24(3):590–594. [PubMed] [Google Scholar]
- 279.Mo-suwan L, Nontarak J, Aekplakorn W, Satheannoppakao W. Computer Game Use and Television Viewing Increased Risk for Overweight among Low Activity Girls: Fourth Thai National Health Examination Survey 2008–2009. Int J Paediatr. 2014;2014:1–6. doi: 10.1155/2014/364702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Mo-Suwan L, Pongprapai S, Junjana C, Puetpaiboon A. Effects of a controlled trial of a school-based exercise program on the obesity indexes of preschool children. Am J Clin Nutr. 1998;68(5):1006–1011. doi: 10.1093/ajcn/68.5.1006. [DOI] [PubMed] [Google Scholar]
- 281.Mo-Suwan L, Tongkumchum P, Puetpaiboon A. Determinants of overweight tracking from childhood to adolescence: A 5 y follow-up study of Hat Yai schoolchildren. Int J Obes. 2000;24(12):1642–1647. doi: 10.1038/sj.ijo.0801432. [DOI] [PubMed] [Google Scholar]
- 282.Mongkhonsiri P. The mindful self: sense of self and health-promoting lifestyle behaviors among Thai college women. Palmerston North: Massey University; 2007. [Google Scholar]
- 283.Morinaka T, Limtrakul PN, Makonkawkeyoon L, Sone Y. Comparison of variations between percentage of body fat, body mass index and daily physical activity among young Japanese and Thai female students. J Physiol Anthropol. 2012;31:21. doi: 10.1186/1880-6805-31-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Mosuwan L, Geater AF. Risk factors for childhood obesity in a transitional society in Thailand. Int J Obes. 1996;20(8):697–703. [PubMed] [Google Scholar]
- 285.Murayama N, Ohtsuka R. Heart rate indicators for assessing physical activity level in the field. Am J Hum Biol. 1999;11(5):647–657. doi: 10.1002/(SICI)1520-6300(199909/10)11:5<647::AID-AJHB8>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 286.Nabkasorn C, Miyai N, Sootmongkol A, Junprasert S, Yamamoto H, Arita M, et al. Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms. Eur J Public Health. 2006;16(2):179–184. doi: 10.1093/eurpub/cki159. [DOI] [PubMed] [Google Scholar]
- 287.Naka K. Life-style and self-care of the elderly in a Thai village in Southern Thailand. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 1999. [Google Scholar]
- 288.Nakhern P, Kananub P. Exercise behavior of public health officer in Nakhorn Pathom province. Div Epidemiol Minist Public Health. 2000;31(1):1–6. [Google Scholar]
- 289.Nakornkhet K. Physical activity attitude as a function of sociocultural differences. Eugene: Microform Publications, College of Human Development and Performance, University of Oregon; 1987. [Google Scholar]
- 290.Namphonkrung P, Jitpanya C, Lueboonthavatchai O. Factors related to exercise behavior in coronary artery disease patients. J Nurs Sci Chulalongkorn Univ. 2005;17(2):97–110. [Google Scholar]
- 291.Nanakorn S, Osaka R, Chusilp K, Tsuda A, Maskasame S, Ratanasiri A. Gender differences in Health-Related practices among University students in Northeast Thailand. Asia-Pac J Public Health. 1999;11(1):10–15. doi: 10.1177/101053959901100103. [DOI] [PubMed] [Google Scholar]
- 292.Nankpong W, Laothamyingyong C. Exercise behavior of staffs in Chumphon police station, Chumphon province. Bangkok: Management for Development College, Thaksin University; 2013. [Google Scholar]
- 293.Napradit P, Pantaewan P, Nimit-arnun N, Souvannakitti D, Rangsin R. Prevalence of overweight and obesity in Royal Thai Army personnel. J Med Assoc Thai. 2007;90(2):335–340. [PubMed] [Google Scholar]
- 294.Naraphong W. Effects of a Culturally Sensitive Exercise Program on Fatigue, Sleep, Mood, and Symptom Distress among Thai Women with Breast Cancer Receiving Adjuvant Chemotherapy: A Pilot Randomized Controlled Trial. PhD [dissertation] Ohio: University of Cincinnati; 2013. [Google Scholar]
- 295.Narin J, Taravut T, Sangkoumnerd T, Thimachai P, Pakkaratho P, Kuhirunyaratn P, et al. Prevalence and factors associated with sufficient physical activity among medical students in Khon Kaen University. Srinagarind Med J. 2008;23(4):389–395. [Google Scholar]
- 296.National Statistical Office. Report on survey of physical activity and sports participation of people with ages of 15 years and over 2001. Bangkok: Ministry of Information and Communication Technology; 2001.
- 297.National Statistical Office. Report of the exercise behaviour survey 2004. Bangkok: Ministry of Information and Communication Technology; 2004.
- 298.National Statistical Office. Report of the exercise behaviour survey 2007. Bangkok: Ministry of Information and Communication Technology; 2007.
- 299.National Statistical Office. Survey on population behaviour in playing sport or physical exercise and mental health 2011. Bangkok: Ministry of Information and Communication Technology; 2011.
- 300.National Statistical Office. The 2015 Physical Activity Survey. Bangkok: Ministry of Information and Communication Technology; 2016.
- 301.Nelson K, Lohsoonthorn V, Williams MA. Preterm delivery risk in relation to maternal occupational and leisure time physical activity among Thai women. Asian Biomed. 2009;3(3):267–277. [PMC free article] [PubMed] [Google Scholar]
- 302.Newman S, Clemmer-Smith R, Yhoung-aree J. Food, lifestyle and fitness: obesity in central Thailand. Faseb Journal. 2008;22(1 Suppl 866):11. [Google Scholar]
- 303.Ng N, Hakimi M, Minh HV, Juvekar S, Razzaque A, Ashraf A, et al. Prevalence of physical inactivity in nine rural INDEPTH Health and Demographic Surveillance Systems in five Asian countries. Glob Health Action. 2009;2:44–53. doi: 10.3402/gha.v2i0.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Ng N, Van Minh H, Juvekar S, Razzaque A, Bich TH, Kanungsukkasem U, et al. Using the INDEPTH HDSS to build capacity for chronic non-communicable disease risk factor surveillance in low and middle-income countries. Glob Health Action. 2009;2:7–18. doi: 10.3402/gha.v2i0.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Ngamjaroen A. Factors affecting exercise behavior among health group members at Ratchaburi province. Bangkok: Graduate School, Silpakorn University; 2005. [Google Scholar]
- 306.Ngaosomskul S. A study of perceived benefits of action and self-efficacy to exercise behavior in coronary artery disease patients after revascularization. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2000. [Google Scholar]
- 307.Ngowsiri K, Tanmahasamut P, Sukonthasab S. Rusie Dutton traditional Thai exercise promotes health related physical fitness and quality of life in menopausal women. Complement Ther Clin Pract. 2007;20(3):164–171. doi: 10.1016/j.ctcp.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 308.Niamsawan A, Oba N, Tansupasawasdikun S. Effects of Ponglang music aerobic exercise on physical fitness and blood pressure among the elderly with hypertension. J Nurs Health Sci. 2012;6(2):62–75. [Google Scholar]
- 309.Nilpetch P, Muktabhant B. Dietary Patterns, Leisure-time Activity and Nutritional Status of Early Adolescent Students at Mo din daeng Demonstration School Khon Kaen University. KKU J Public Health Res (KKU-JPHR). 2012;(Special Issue):1–10.
- 310.Nintachan P. Resilience and risk-taking behavior among Thai adolescents living in Bangkok, Thailand. PhD [dissertation]. Virginia: Virginia Commonwealth University; 2007.
- 311.Noinawakul U, Pinyopasakul W, Kimpee S, Puwarawuttipanit W. The effects of a walking exercise program on perceived self-efficacy and functional capacity in stroke patients with hemiparesis. J Nurs Sci. 2010;28(4):45–53. [Google Scholar]
- 312.Nuntavipavong S, Rattanapongpinyo T, editors. Factors relating exercise decision of elders at Bung Ta Lua Water Park, Nakhon Ratchasima. Phayao Research Conference 5. Phayao: University of Phayao; 2016. [Google Scholar]
- 313.Orawan B. Development of Thai Yoga-Chi Kung Neuromotor Combination Exercise for Active Aging. J Aging Phys Act. 2012;20:S72–SS3. [Google Scholar]
- 314.Osaka R, Nanakorn S, Chusilp K. Cornell medical index: A comparative study on health problems among Thai and Japanese nursing students. Southeast Asian J Trop Med Public Health. 1998;29(2):293–298. [PubMed] [Google Scholar]
- 315.Osaka R, Nanakorn S, Sanseeha L, Nagahiro C, Kodama N. Healthy dietary habits, body mass index, and predictors among nursing students, northeast Thailand. Southeast Asian J Trop Med Public Health. 1999;30(1):115–121. [PubMed] [Google Scholar]
- 316.Othaganont P, Sinthuorakan C, Jensupakarn P. Daily living practice of the life-satisfied Thai elderly. J Transcult Nurs. 2002;13(1):24–29. doi: 10.1177/104365960201300105. [DOI] [PubMed] [Google Scholar]
- 317.Ounprom S. Effects of Health Educational Program on Health Promotion Behaviors Among Pre-Diabetes Adults. J Nurs Sci Naresuan Univ. 2007;1(1):100–111. [Google Scholar]
- 318.Page RM, Suwanteerangkul J. Self-rated health, psychosocial functioning, and health-related behavior among Thai adolescents. Paediatr Int. 2009;51(1):120–125. doi: 10.1111/j.1442-200X.2008.02660.x. [DOI] [PubMed] [Google Scholar]
- 319.Page RM, Taylor J, Suwanteerangkul J, Novilla LM. The influence of friendships and friendship-making ability in physical activity participation in Chiang Mai, Thailand high school students. Int Electron J Health Educ. 2005;8:95–103. [Google Scholar]
- 320.Paileeklee S, Kuhiranyaratn P, Jindawong B, Ratanasiri A, See-Ubpalad W. Prevalence of physical exercise and its factors among the elderly in Khon Kaen Municipality, Khon Kaen Thailand. J Aging Phys Act. 2008;16:S40–S4S. [Google Scholar]
- 321.Palasuwan A, Margaritis I, Soogarun S, Rousseau AS. Dietary intakes and antioxidant status in mind-body exercising pre- and postmenopausal women. J Nutr, Health Aging. 2011;15(7):577–584. doi: 10.1007/s12603-011-0060-2. [DOI] [PubMed] [Google Scholar]
- 322.Palasuwan A, Suksom D, Margaritis I, Soogarun S, Rousseau A-S. Effects of Tai Chi Training on Antioxidant Capacity in Pre- and Postmenopausal Women. J Aging Res. 2011;2011:1–8. doi: 10.4061/2011/234696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Pancharean S, Wanjan P. Influencing factors of exercise behavior among high school students. Thai J Nurs Council. 2007;22(3):80–90. [Google Scholar]
- 324.Pandejpong D, Ratanapitak U, Krainuwatr K, Jaisue N, Pandejpong T, Nopmaneejumruslers C. The effect of a life style modification campaign for Bangkok provincial electricity officers. Siriraj Med J. 2010;62(2):62–65. [Google Scholar]
- 325.Panidchakul K. Determinants of readiness to adopt regular physical activity among Thai patients at risk for cardiovascular disease: A trans-theoretical model. Birmingham: University of Alabama; 2003. [Google Scholar]
- 326.Panidchakul K. Determinants of Readiness to Adopt Regular Physical Activity among Thai Employers in Workplaces, Thailand: A Transtheoretical Model. Int J Behav Med. 2010;17:103. [Google Scholar]
- 327.Pasiri P, Kuhirunyaratn P. Knowledge, attitude and practice related to physical exercise among health volunteers in Amphoe Meuang, Nong Bua Lam Phu province. 34th The National Graduate Research Conference. Khon Kaen: Khon Kaen University; 2015. [Google Scholar]
- 328.Pawloski LR, Kitsantas P, Ruchiwit M. Determinants of overweight and obesity in Thai adolescent girls. Archives: The. Int J Med. 2010;3(2):352–356. [Google Scholar]
- 329.Peltzer K, Pengpid S. Fruits and Vegetables Consumption and Associated Factors among In-School Adolescents in Five Southeast Asian Countries. Int J Environ Res Public Health. 2012;9(10):3575–3587. doi: 10.3390/ijerph9103575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Peltzer K, Pengpid S. Sitting time and its associated factors in university students from 18 low, middle and emerging economy countries. Afr J Physical, Health Educ, Recreat Dance. 2014;20(4.1):1379–1389. [Google Scholar]
- 331.Peltzer K, Pengpid S. Depressive symptoms and social demographic, stress and health risk behaviour among university students in 26 low-, middle- and high-income countries. Int J Psychiatry Clin Pract. 2015;19(4):259–265. doi: 10.3109/13651501.2015.1082598. [DOI] [PubMed] [Google Scholar]
- 332.Peltzer K, Pengpid S. Correlates of healthy fruit and vegetable diet in students in low, middle and high income countries. Int J Public Health. 2015;60(1):79–90. doi: 10.1007/s00038-014-0631-1. [DOI] [PubMed] [Google Scholar]
- 333.Peltzer K, Pengpid S. Leisure time physical inactivity and sedentary behaviour and lifestyle correlates among students aged 13–15 in the association of Southeast Asian nations (ASEAN) member states, 2007–2013. Inter J Environ Res Public Health. 2016;13:217. [DOI] [PMC free article] [PubMed]
- 334.Peltzer K, Pengpid S, Amuleru-Marshall O, Mufune P, Zeid AA. Religiosity and health risk behaviour among university students in 26 low, middle and high income countries. J Relig Health. 2016;55(6):2131–40. doi: 10.1007/s10943-016-0260-5. [DOI] [PubMed] [Google Scholar]
- 335.Peltzer K, Pengpid S, Apa P, Somchai V. Obesity and Lifestyle Factors in Male Hospital Out-patients in Thailand. Gender Behav. 2015;13(2):6668–6674. [Google Scholar]
- 336.Peltzer K, Pengpid S, Apidechkul T. Heavy Internet use and its associations with health risk and health-promoting behaviours among Thai university students. Int J Adolesc Med Health. 2014;26(2):187–194. doi: 10.1515/ijamh-2013-0508. [DOI] [PubMed] [Google Scholar]
- 337.Peltzer K, Pengpid S, Samuels T, Özcan NK, Mantilla C, Rahamefy OH, et al. Prevalence of overweight/obesity and its associated factors among university students from 22 countries. Int J Environ Res and Public Health. 2014;11(7):7425–7441. doi: 10.3390/ijerph110707425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Peltzer K, Pengpida S. Multiple health risk behaviours and posttraumatic stress disorder symptoms among university students from 22 countries. J Psychol Afr. 2014;24(6):499–503. doi: 10.1080/14330237.2014.997038. [DOI] [Google Scholar]
- 339.Pengpid S, Peltzer K. Bullying and its associated factors among school-aged adolescents in Thailand. Sci World J. 2013;2013:1–6. doi: 10.1155/2013/254083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Pengpid S, Peltzer K. Overweight and obesity and associated factors among school-aged adolescents in Thailand. Afr J Phys, Health Educ, Recreat Dance. 2013;19(2):448–458. [Google Scholar]
- 341.Pengpid S, Peltzer K. Prevalence of overweight and underweight and its associated factors among male and female university students in Thailand. HOMO- J Comp Hum Biol. 2015;66(2):176–186. doi: 10.1016/j.jchb.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 342.Pengpid S, Peltzer K. Dietary health behaviour and beliefs among university students from 26 low, middle and high income countries. Asia Pac J Clin Nutr. 2015;24(4):744–52. doi: 10.6133/apjcn.2015.24.4.21. [DOI] [PubMed] [Google Scholar]
- 343.Pengpid S, Peltzer K. Gender Differences in Health Risk Behaviour among University Students: An International Study. Gender Behav. 2015;13(1):6576–6583. [Google Scholar]
- 344.Pengpid S, Peltzer K, Kassean HK, Tsala JPT, Sychareun V, Müller-Riemenschneider F. Physical inactivity and associated factors among university students in 23 low-, middle- and high-income countries. Int J Public Health. 2015;60(5):539–549. doi: 10.1007/s00038-015-0680-0. [DOI] [PubMed] [Google Scholar]
- 345.Pengpid S, Peltzer K, Samuels TA, Gasparishvili A. Factors associated with self-rated health status among university students from 26 low, middle and high income countries. J Psychol Afr. 2015;25(5):448–453. doi: 10.1080/14330237.2015.1101274. [DOI] [Google Scholar]
- 346.Pensri P, Janwantanakul P. Effectiveness of Brief Education Combined with a Home-Based Exercise Program on Pain and Disability of Office Workers with Chronic Low Back Pain: a Pilot Study. J Phys Ther Sci. 2012;24(2):217–222. doi: 10.1589/jpts.24.217. [DOI] [Google Scholar]
- 347.Pensri P, Janwantanakul P, Chaikumarn M. Biopsychosocial risk factors for musculoskeletal symptoms of the spine in salespeople. Int J Occup Environ Health. 2010;16(3):303–311. doi: 10.1179/oeh.2010.16.3.303. [DOI] [PubMed] [Google Scholar]
- 348.Pensri P, Janwantanakul P, Chaikumarn M. Biopsychosocial Factors and Musculoskeletal Symptoms of the Lower Extremities of Saleswomen in Department Stores in Thailand. J Occup Health. 2010;52(2):132–141. doi: 10.1539/joh.L9093. [DOI] [PubMed] [Google Scholar]
- 349.Permsirivanich W, Lim A, Promrat T. Long stick exercise to improve muscular strength and flexibility in sedentary individuals. Southeast Asian J Trop Med Public Health. 2006;37(3):595–600. [PubMed] [Google Scholar]
- 350.Petcharoen N, Prasartkul P, Gray R, Vapattanawong P. Adult mortality of cardiovascular disease by socioeconomic status in Thailand. J Public Health Dev. 2006;4(2):61–72. [Google Scholar]
- 351.Peungsuwan P, Sermcheep P, Harnmontree P, Eungpinichpong W, Puntumetakul R, Chatchawan U, et al. The effectiveness of Thai exercise with traditional massage on the pain, walking ability and QOL of older people with knee osteoarthritis: A randomized controlled trial in the community. J Phys Ther Sci. 2014;26(1):139–144. doi: 10.1589/jpts.26.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Phaisal S. Knowledge, attitude and self-practice in exercise for health of personnels of the teachers council of Thailand. Bangkok: Ramkhamhaeng University; 1998. [Google Scholar]
- 353.Phaitrakoon J, Powwattana A, Lagampan S, Klaewkla J. Effects of an Obesity Control Program for Thai Elementary School Children: A Quasi-Experimental Study. Pac Rim Int J Nurs Res. 2014;18(4):290–304. [Google Scholar]
- 354.Phoosuwan M. The effects of weight bearing yoga training on the bone resorption markers of the postmenopausal women. Bangkok: School of Sports Science, Chulalongkorn University; 2008. [PubMed] [Google Scholar]
- 355.Piaseu N, Komindr S, Chailurkit LO, Ongphiphadhanakul B, Chansirikarn S, Rajatanavin R. Differences in bone mineral density and lifestyle factors of postmenopausal women living in Bangkok and other provinces. J Med Assoc Thai. 2001;84(6):772–781. [PubMed] [Google Scholar]
- 356.Piaseu N, Schepp K, Belza B. Causal analysis of exercise and calcium intake behaviors for osteoporosis prevention among young women in Thailand. Health Care Woman Int. 2002;23(4):364–376. doi: 10.1080/0739933029008937. [DOI] [PubMed] [Google Scholar]
- 357.Pipatkasira K. The comparison of physical activity in urban and rural Thai school children using validated Thai physical activity questionnaire. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2008. [Google Scholar]
- 358.Piravej K, Saksirinukul R. Survey of patterns, attitudes, and the general effects of exercise during pregnancy in 203 Thai pregnant women at King Chulalongkorn Memorial Hospital. J Med Assoc Thai. 2001;84(Suppl 1):S276–SS82. [PubMed] [Google Scholar]
- 359.Piravej K, Wiwatkul W. Risk factors for stroke in Thai patients. J Med Assoc Thai. 2003;86(Suppl 2):S291–S2S8. [PubMed] [Google Scholar]
- 360.Piyakhachornrot N, Aree-Ue S, Putwatana P, Kawinwonggowit V. Impact of an integrated health education and exercise program in middle-aged Thai adults with osteoarthritis of the knee. Orthop Nurs. 2011;30(2):134–142. doi: 10.1097/NOR.0b013e31821130bf. [DOI] [PubMed] [Google Scholar]
- 361.Podang J, Sritara P, Narksawat K. Prevalence and factors associated with metabolic syndrome among a group of Thai working population: a cross sectional study. J Med Assoc Thai = Chotmaihet thangphaet. 2013;96(Suppl 5):S33–S41. [PubMed] [Google Scholar]
- 362.Polin S. Relationships between personal factors, self-efficacy in exercise, perceived benefits of exercise, college environment and exercise behaviors of nursing students. Bangkok: Faculty of Nursing, Chulalongkorn University; 1999. [Google Scholar]
- 363.Pongchaiyakul C, Nguyen T, Kosulwat V, Rojroongwasinkul N, Charoenkiatkul S, Eisman J, et al. Effects of physical activity and dietary calcium intake on bone mineral density and osteoporosis risk in a rural Thai population. Osteoporos Int. 2004;15(10):807–813. doi: 10.1007/s00198-004-1613-6. [DOI] [PubMed] [Google Scholar]
- 364.Pongpaew P, Tungtrongchitr R, Phonrat B, Vudhivai N, Jintaridhi P, Vorasanta S, et al. Activity, dietary intake, and anthropometry of an informal social group of Thai elderly in Bangkok. Arch Gerontol Geriatr. 2000;30(3):245–260. doi: 10.1016/S0167-4943(00)00051-0. [DOI] [PubMed] [Google Scholar]
- 365.Pongpaiboon P, Sornprasit K, Lawantrakul J, Youngwanichsetha S. The effect of long stick exercise on female adolescents’ physical fitness and health. Songklanagarind Med J. 2007;25(6):521–529. [Google Scholar]
- 366.Pongurgsorn C. A questionnaire for assessment of physical activity in Thailand. Illinois: the United States: Graduate College, University of Illinois at Urbana-Champaign; 2002. [Google Scholar]
- 367.Pongwecharak J, Treeranurat T. Screening for pre-hypertension and elevated cardiovascular risk factors in a Thai community pharmacy. Pharm World Sci. 2010;32(3):329–333. doi: 10.1007/s11096-010-9373-1. [DOI] [PubMed] [Google Scholar]
- 368.Pongwecharak J, Treeranurat T. Lifestyle changes for prehypertension with other cardiovascular risk factors: Findings from Thailand. J Am Pharm Assoc. 2011;51(6):719–726. doi: 10.1331/JAPhA.2011.10129. [DOI] [PubMed] [Google Scholar]
- 369.Poolsawat W. Physical activity of the older adults in Bangkok. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2007. [Google Scholar]
- 370.Poomsrikaew O. Social-cognitive factors and exercise behavior among Thais. Illinois: the United States: College of Nursing, University of Illinois at Chicago; 2011. [Google Scholar]
- 371.Poomsrikaew O, Berger BE, Kim MJ, Zerwic JJ. Age and gender differences in social-cognitive factors and exercise behavior among Thais. West J Nurs Res. 2012;34(2):245–264. doi: 10.1177/0193945911424170. [DOI] [PubMed] [Google Scholar]
- 372.Pornsakulvanich V. Internet motives and use among Thai youths. Univ Thai Chamber of Commerce J. 2007;27(2):29–41. [Google Scholar]
- 373.Pornsakulvanich V, Dumrongsiri N. Internal and external influences on social networking site usage in Thailand. Comp Hum Behav. 2013;29(6):2788–2795. doi: 10.1016/j.chb.2013.07.016. [DOI] [Google Scholar]
- 374.Pornviriyasup P. A study of health behaviors of women with diabetes mellitus in the western region. Bangkok: Graduate School, Mahidol University; 1997. [Google Scholar]
- 375.Posri T. The effect of Combined Exercise and Meditation on Physical Fitness and Autonomic Nervous System. Bangkok: Suan Sunandha Rajabhat University; 2012. [Google Scholar]
- 376.Pothiban L. Risk factor prevalence, risk status, and perceived risk for coronary heart disease among Thai elderly. Biringham: University of Alabama; 1993. [Google Scholar]
- 377.Pothirat C, Chaiwong W, Phetsuk N, Liwsrisakun C, Bumroongkit C, Deesomchok A, et al. Long-term efficacy of intensive cycle ergometer exercise training program for advanced COPD patients. Int J COPD. 2015;10:133–144. doi: 10.2147/COPD.S73398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Poungkeaw A. A study of health behaviors of women with coronary heart disease in the Bangkok metropolitan area. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 1997. [Google Scholar]
- 379.Prachapiphat C. Impact of a Health Education Program on Exercise for Health Behavior of Bang Pakong Power Plant Personnel in Chachoengsao Province. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2000. [Google Scholar]
- 380.Prakhinkit S, Suppapitiporn S, Tanaka H, Suksom D. Effects of Buddhism Walking Meditation on Depression, Functional Fitness, and Endothelium-Dependent Vasodilation in Depressed Elderly. J Altern Complem Med. 2014;20(5):411–416. doi: 10.1089/acm.2013.0205. [DOI] [PubMed] [Google Scholar]
- 381.Prapimporn Chattranukulchai S, Pariya P, Orawan P, La-or C, Tanarat L, Suwannee C, et al. Vitamin D status is a determinant of skeletal muscle mass in obesity according to body fat percentage. Nutr. 2015;31(6):801–806. doi: 10.1016/j.nut.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 382.Prasetsin U, Suvarnakuta P. The effect of internet using behaviors upon the physical and mental health of Thai children and youths: case study in Bangkok. International Journal of Cyber Society and. Educ. 2011;4(2):117–126. [Google Scholar]
- 383.Prombumroong J, Janwantanakul P, Pensri P. Prevalence of and biopsychosocial factors associated with low back pain in commercial airline pilots. Aviat Space Environ Med. 2011;82(9):879–884. doi: 10.3357/ASEM.3044.2011. [DOI] [PubMed] [Google Scholar]
- 384.Prompiw S, Tumnong C, Wongkpratoom S, Wongvipaporn C. The effects of a perceived self-efficacy program on the exercise and diet behaviors of patients with acute coronary syndrome post percutaneous coronary intervention. J Nurs Health Care. 2015;33(1):23–33. [Google Scholar]
- 385.Promthet S, Saranrittichai K, Kamsa-ard S, Senarak W, Vatanasapt P, Wiangnon S, et al. Situation analysis of risk factors related to non-communicable diseases in Khon Kaen province, Thailand. Asian Pac J Cancer Prev. 2011;12(5):1337–1340. [PubMed] [Google Scholar]
- 386.Prueksaritanond S, Tubtimtes S, Asavanich K, Tiewtranon V. Type 2 diabetic patient-centered care. J Med Assoc Thai. 2004;87(4):345–352. [PubMed] [Google Scholar]
- 387.Pruksasri P, Kongin W, Jittanoon P. The effects of social-dance exercise program on balance among the fall-risk elderly. Songklanagarind Med J. 2008;26(4):323–337. [Google Scholar]
- 388.Puengsuwan P, Promdee K, Sruttabul W, Na Nagara R, Leelayuwat N. Effectiveness of Thai Wand Exercise training on health-related quality of life in sedentary older adults. Chula Med J. 2008;52(2):107–121. [Google Scholar]
- 389.Rachiwong S, Panasiriwong P, Saosomphop J, Widjaja W, Ajjimaporn A. Effects of modified hatha yoga in industrial rehabilitation on physical fitness and stress of injured workers. J Occup Rehabil. 2015;25(3):669–674. doi: 10.1007/s10926-015-9574-5. [DOI] [PubMed] [Google Scholar]
- 390.Rapheeporn K, Sasithorn T, Suchittra S, Suree C, Sirirak M. Waist Circumference: A Key Determinant of Bone Mass in University Students. Walailak J Sci Technol. 2013;10(5/6):665–676. [Google Scholar]
- 391.Rasmidatta S, Khunsuk-Mengrai K, Warunyuwong C. Risk Factors of Diabetic Retinopathy in Non-insulin Dependent Diabetes Mellitus. J Med Assoc Thai. 1998;81(3):169–174. [PubMed] [Google Scholar]
- 392.Rattanagreethakul S, Lapvongwatana P, Thiangtham W, Sunsern R, McMullen PC. Development of a model of family management for overweight prevention in urban Thai pre-schoolers. Pac Rim Int J Nurs Res. 2010;14(1):45–60. [Google Scholar]
- 393.Rattanapun S, Fongkeaw W, Chontawan R, Panuthai S, Wesumperuma D. Characteristics healthy ageing among the elderly in Southern Thailand. Chiang Mai Univ J Nat Sci. 2009;8(2):143–160. [Google Scholar]
- 394.Rattanawiwatpong P, Khunphasee A, Pongurgsorn C, Intarakamhang P. Validity and reliability of the Thai version of short format International Physical Activity Questionnaire (IPAQ) J Thai Rehabil. 2006;16(3):147–160. [Google Scholar]
- 395.Raungratanaamporn S, Yunibhand J, Jitpanya C, Pudtong N, Aungsuroch Y, Thutsaringkarnsakul S. Factors predicting physical activity after hospitalization among new coronary artery disease patients. J Health Res. 2015;29(2):127–133. [Google Scholar]
- 396.Rawiworrakul T, Sirapo-ngam Y, Davis AHT, Malathum P, Kulthanan T. Vorapongsathorn T. A community-based exercise program promotes self-efficacy for exercise among Thai women with osteoarthritis of the knee. Thai J Nurs Res. 2007;11(2):132–150. [Google Scholar]
- 397.Razzaque A, Nahar L, Minh HV, Ng N, Juvekar S, Ashraf A, et al. Social factors and overweight: evidence from nine Asian INDEPTH Network sites. Glob Health Action. 2009;2:54–59. doi: 10.3402/gha.v2i0.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Rerksuppaphol L, Rerksuppaphol S. Excessive television viewing increases BMI, yet not a risk factor for childhood obesity or thinness: A cross sectional study on Thai school children. HealthMED. 2011;5(6 Suppl 1):1895–1901. [Google Scholar]
- 399.Ritsmitchai S, Geater AF, Chongsuviwatvong V. Prolonged standing and physical exertion at work during pregnancy increases the risk of preterm birth for Thai mothers. J Occup Health. 1997;39(3):217–222. doi: 10.1539/joh.39.217. [DOI] [Google Scholar]
- 400.Rojanakul K, Liang H, editors. Initiatives and challenges in countering inappropriate internet use. ICCTD 2009 - 2009 International Conference on Computer Technology and Development. 2009. [Google Scholar]
- 401.Ruangdaraganon N, Chuthapisith J, Mo-suwan L, Kriweradechachai S, Udomsubpayakul U, Choprapawon C. Television viewing in Thai infants and toddlers: impacts to language development and parental perceptions. BMC Pediatrics. 2009;9(1):34. doi: 10.1186/1471-2431-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Ruangdaraganon N, Kotchabhakdi N, Udomsubpayakul U, Kunanusont C, Suriyawongpaisal P. The association between television viewing and childhood obesity: A national survey in Thailand. J Med Assoc Thai. 2002;85(Suppl 4):S1075–S1S80. [PubMed] [Google Scholar]
- 403.Ruangrat A. An investigation into the factors affecting the behavior of internet use of students at vocational diploma level 2 in technical colleges under Vocational Department at Bangkok zone. Bangkok: Graduate School, King Mongkut's University of Technology Thonburi; 2001. [Google Scholar]
- 404.Rungruang S, Pattanittum P, Kamsa-ard S. Physical Exercise of Khon Kaen University Students. J Health Sci. 2006;15(2):315–322. [Google Scholar]
- 405.Saelao K, Kanungsukkasem V. Effects of arm swing exercise, walking and walking exercise combined with arm swing exercise on health-related physical fitness of the elderly women. J Sports Sci Health. 2012;13(1):92–103. [Google Scholar]
- 406.Saengdidtha B, Kasemkijwattana P, Kaoaiem H. Prevalence of chronic diseases risk factors among persons attending six administrative courses in the Army Training Command area in 2006. J Med Assoc Thai = Chotmaihet thangphaet. 2009;92(Suppl 1):S67–S73. [PubMed] [Google Scholar]
- 407.Saengsuwan J, Boonyaleepan S, Tiamkao S. Diet, exercise, sleep, sexual activity, and perceived stress in people with epilepsy in NE Thailand. Epilepsy Behav. 2015;45:39–43. doi: 10.1016/j.yebeh.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 408.Saengsuwan J, Laohasiriwong W, Boonyaleepan S, Sawanyawisuth K, Tiamkao S, Talkul A. Seizure-related vehicular crashes and falls with injuries for people with epilepsy (PWE) in north eastern Thailand. Epilepsy Behav. 2014;32:49–54. doi: 10.1016/j.yebeh.2013.12.021. [DOI] [PubMed] [Google Scholar]
- 409.Saiseesub Y. A study of perceived self-efficacy and situational influences on exercise behavior in coronary artery disease patients at Uttaradit Hospital. Nakorn Pathom: Faculty of Graduate Studies, Mahidol University; 2000. [Google Scholar]
- 410.Saithong T, Boonyasopun U, Naka K. Relationships among situational influences, interpersonal influences, commitment to exercise and exercise behavior of exercise group members in Phang-nga province. Thai J Nurs Council. 2004;19(2):39–52. [Google Scholar]
- 411.Samnak N, Eukuyi M, Boonrod T, Somrak K. Modification of health behavior in a group of patients with pre-hypertension at the Pakphanang District, Nakhon Si Thammarat Province. KKU J Public Health Res (KKU-JPHR). 2011;4(2):21–28. [Google Scholar]
- 412.Samnieng P, Ueno M, Zaitsu T, Shinada K, Wright FA, Kawaguchi Y. The relationship between seven health practices and oral health status in community-dwelling elderly Thai. Gerontol. 2013;30(4):254–261. doi: 10.1111/j.1741-2358.2012.00672.x. [DOI] [PubMed] [Google Scholar]
- 413.Sampahangsit T. Leisure time use through exercises of Srinakharinwirot University students. Bangkok: Srinakharinwirot University; 1988. [Google Scholar]
- 414.Samranbua A. The Lived Experience of Rural Thai Older Adults with Poorly Controlled Hypertension. PhD [dissertation]. District of Columbia (DC): Catholic University of America; 2011.
- 415.Samranbua A, Thamcharoentakul B. The factors affected on stage of change for exercise behavior among patients with hypertension. J Boromarajonani Coll Nurs. 2015;21(1):65–77. [Google Scholar]
- 416.Sanamthong B. Food consumption and exercise behaviors of obese children attending a weight-control program. Khon Kaen: Graduate School, Khon Kaen University; 2005. [Google Scholar]
- 417.Sangrajrang S, Chaiwerawattan A, Ploysawang P, Nooklang K, Jamsri P, Somharnwong S. Obesity, diet and physical inactivity and risk of breast cancer in Thai women. Asian Pac J Cancer Prev. 2013;14(11):7023–7027. doi: 10.7314/APJCP.2013.14.11.7023. [DOI] [PubMed] [Google Scholar]
- 418.Sangthong R, Wichaidit W, McNeil E, Chongsuvivatwong V, Chariyalertsak S, Kessomboon P, et al. Health behaviors among short- and long- term ex-smokers: Results from the Thai National Health Examination Survey IV, 2009. Prev Med. 2012;55(1):56–60. doi: 10.1016/j.ypmed.2012.04.022. [DOI] [PubMed] [Google Scholar]
- 419.Sanguanrungsirikul S, Somboonwong J, Nakhanakhup C, Pruksananonda C. Energy expenditure and physical activity of obese and non-obese Thai children. J Med Assoc Thai. 2001;84(Suppl 1):S314–SS20. [PubMed] [Google Scholar]
- 420.Sarakarn W, Somboon L, Tongswas T. Factors influencing health promoting behaviors among female workers in garment factories. Nurs J. 2002;29(1):18–35. [Google Scholar]
- 421.Saranrittichai K, Senarak W, Promthet S, Wiangnon S, Vatanasapt P, Kamsa-ard S, et al. Health behavior after a multi professional intervention and training for ongoing volunteer-based community health programme intervention in the north-east of Thailand: What changed and what not? Asian Pac J Cancer Prev. 2012;13(9):4801–4805. doi: 10.7314/APJCP.2012.13.9.4801. [DOI] [PubMed] [Google Scholar]
- 422.Sasivimonluk K, Tanvatanangul W, Tanvatanangul V. Statistical analysis of health preventive behavior of population under universal coverage health insurance project in Chiang Mai municipal area (Thailand) J Interdisciplinary Math. 2005;8(3):435–448. doi: 10.1080/09720502.2005.10700419. [DOI] [Google Scholar]
- 423.Sawangdee Y, Yousomboon C, Pongpradit K. Consequences of physical activities officers on villagers’ sport, exercise, and recreation participation in Thailand. J Sci Med Sport. 2014;18:e157. doi: 10.1016/j.jsams.2014.11.176. [DOI] [Google Scholar]
- 424.Senarak W, Chirawatkul S, Markovic M. Health promotion for middle-aged Isan women, Thailand: A participatory approach. Asian Pac J Cancer Prev. 2006;7(1):55–59. [PubMed] [Google Scholar]
- 425.Settheetham-Ishida W, Premsri N, Khrisanapant W. Effect of Aerobic Exercise on Salivary Alpha-amylase and White Blood Cell Count among Sedentary Thais. ศรีนครินทร์ เวช สาร (Srinagarind Med J) 2016;31(1):1–7. [Google Scholar]
- 426.Siangsai C, Sukonthasab S. Factors related physical activities of higher education institutes students in Bangkok metropolis. J Sports Sci Health. 2015;16(3):63–75. [Google Scholar]
- 427.Sihawong R, Janwantanakul P, Jiamjarasrangsi W. A prospective, cluster-randomized controlled trial of exercise program to prevent low back pain in office workers. Eur Spine J. 2014;23(4):786–793. doi: 10.1007/s00586-014-3212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Sinthanayothin P. The study of health perceptions and health promoting behaviors in midlife working women in Bangkok. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2000. [Google Scholar]
- 429.Siramaneerat I, Sawangdee Y. Socioeconomic-demographic factors and health-risk behaviors in the Thai population. Popul. 2015;29(6):457–463. [Google Scholar]
- 430.Sirikulchayanonta C, Pavadhgul P, Chongsuwat R, Klaewkla J. Participatory action project in reducing childhood obesity in Thai primary schools. Asia-Pac J Public Health. 2011;23(6):917–927. doi: 10.1177/1010539510361965. [DOI] [PubMed] [Google Scholar]
- 431.Sirikulchayanonta C, Ratanopas W, Temcharoen P, Srisorrachatr S. Self discipline and obesity in Bangkok school children. BMC Public Health. 2011;11(1):158. doi: 10.1186/1471-2458-11-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Siriphakhamongkhon S, Sawangdee Y, Pattaravanich U, Mongkolchati A, Hlaing ZN, Rattanapan C, et al. Determinants and consequences of childhood overweight-health status and the child s school achievement in Thailand. J Health Res. 2016;30(3):165–171. [Google Scholar]
- 433.Siriphorn A, Chamonchant D. Wii balance board exercise improves balance and lower limb muscle strength of overweight young adults. J Phys Ther Sci. 2015;27(1):41–46. doi: 10.1589/jpts.27.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Siripul P. Risk factors for cardiovascular disease in Thai adolescents. PhD [dissertation]. Ohio: Case Western Reserve University (Health Sciences); 2000.
- 435.Sithisarankul P, Piyasing V, Boontheaim B, Ratanamongkolgul S, Wattanasirichaigoon S. Longevity of Thai physicians. J Med Assoc Thai = Chotmaihet thangphaet. 2004;87(Suppl 4):S23–S32. [PubMed] [Google Scholar]
- 436.Sithisarankul P, Piyasing V, Boontheaim B, Ratanamongkolgul S, Wattanasirichaigoon S. Longevity of Thai physicians: Phase 2 and policy implications. J Med Assoc Thai. 2005;88(9):1257–1260. [PubMed] [Google Scholar]
- 437.Sitthipornvorakul E, Janwantanakul P, Lohsoonthorn V. The effect of daily walking steps on preventing neck and low back pain in sedentary workers: a 1-year prospective cohort study. Eur Spine J. 2015;24(3):417–424. doi: 10.1007/s00586-014-3577-3. [DOI] [PubMed] [Google Scholar]
- 438.Sitthipornvorakul E, Janwantanakul P, Van Der Beek AJ. Correlation between pedometer and the Global Physical Activity Questionnaire on physical activity measurement in office workers. BMC Research Notes. 2014;7(1):280. doi: 10.1186/1756-0500-7-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Sittisart V, Sukdee J, Limkamontip S. Health Promotion Behaviors of Elderly in the Community of Watprix Tumbon Phitsanuloke Province. Boromrajonani College of Nursing Phutthachinnarat: Phitsanulok; 2007. [Google Scholar]
- 440.Sittiwicheanwong R, Ariyapitipun T, Gulsatitporn S, Nopponpunth V, Abeywardena M, Dahlan W. Alterations of atherogenic low-density lipoproteins and serum fatty acids after 12 week moderate exercise training in sedentary Thai women. Asia Pac J Clin Nutr. 2007;16(4):602–608. [PubMed] [Google Scholar]
- 441.Skulpant N. The relationship between social support, related factors and self-care behavior of the diabetic patients. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 1992. [Google Scholar]
- 442.Somnil P, Khaothin T. Factors Affecting Exercise Adherence Behavior of University Students in Upper North eastern, Thailand. Asian Soc Sci. 2016;12(12):205–12. doi: 10.5539/ass.v12n12p205. [DOI] [Google Scholar]
- 443.Somsap Y, Kasetsomboon P, Krischareon S, Polain K. The effects of yoga on female adolescents’ health. Songklanagarind Med J. 2005;23(3):165–176. [Google Scholar]
- 444.Somsap Y, Lertpaiboon J. Health Promoting Experiences of Female Teenagers with Yoga. Thai J Nurs Council. 2009;24(4):83–94. [Google Scholar]
- 445.Somwatee T, Pothiban L, Nanasilp P. Effect of Thai Qigong meditation exercise on blood pressure of the elderly with hypertension. Nurs J. 2011;38(4):81–92. [Google Scholar]
- 446.Sophonratanapokin B, Chaiyawat P, Sawangdee Y. Reasons of exercise and no-exercise in the young-old elderly in Tambon Salaya, Nakhon Pathom. Thammasat Med J. 2011;11(2):137–146. [Google Scholar]
- 447.Sota C. Game play behavior of students in a school in Khon Kaen province, Thailand. Soc Sci. 2011;6(3):186–193. [Google Scholar]
- 448.Sranacharoenpong K, Udomkarnjananan S, Chirdkiatisak M. Promoting Healthy Lifestyle Using Complex Community-Based Approach for at-Risk Populations of Diabetes in Thailand: Formative Evaluation. Ann Nutr Metab. 2013;63:975. [Google Scholar]
- 449.Srichaisawat P. Factors affecting exercise behaviors of undergraduate students, Srinakharinwirot University. J Fac Phys Educ. 2006;9(2):5–18. [Google Scholar]
- 450.Srimatavorakul P, Naka K, Noopetch P. Physical Activity among Older persons in Rural Southern Thailand. Thai J Nurs Council. 2010;25(1):112–120. [Google Scholar]
- 451.Sriramatr S, Berry TR, Rodgers WM. Validity and Reliability of Thai Versions of Questionnaires Measuring Leisure-time Physical Activity, Exercise-Related Self-Efficacy, Outcome Expectations and Self-Regulation. Pac Rim Int J Nurs Res. 2013;17(3):203–216. [Google Scholar]
- 452.Sriramatr S, Berry TR, Spence JC. An Internet-based intervention for promoting and maintaining physical activity: a randomized controlled trial. Am J Health Behav. 2014;38(3):430–439. doi: 10.5993/AJHB.38.3.12. [DOI] [PubMed] [Google Scholar]
- 453.Srirojana S, Mapanao Y. Factors Affecting Exercise Behavior of Medical Students in Kalasin Hospital. Srinagarind Med J. 2015;30(3):292–298. [Google Scholar]
- 454.Srisodsaluk P. The factors influencing health promotion behaviors of nurse instructors under the Central Network of Ministry of Public Health. Bangkok: Graduate School, Christian University of Thailand; 2014. [Google Scholar]
- 455.Sritara C, Thakkinstian A, Ongphiphadhanakul B, Pornsuriyasak P, Warodomwichit D, Akrawichien T, et al. Work- and travel-related physical activity and alcohol consumption: Relationship with bone mineral density and calcaneal quantitative ultrasonometry. J Clin Densitom. 2015;18(1):37–43. doi: 10.1016/j.jocd.2014.04.117. [DOI] [PubMed] [Google Scholar]
- 456.Sritippayawan S, Harnruthakorn C, Deerojanawong J, Samransamruajkit R, Prapphal N. Optimal level of physical activity in children with chronic lung diseases. Acta Paediatr. 2008;97(11):1582–1587. doi: 10.1111/j.1651-2227.2008.00976.x. [DOI] [PubMed] [Google Scholar]
- 457.Sriyuktasuth A. Utility of Pender's model in describing health-promoting behaviors in Thai women with systemic lupus erythematosus. Birmingham: University of Alabama; 2002. [Google Scholar]
- 458.Stewart O, Yamarat K, Neeser KJ, Lertmaharit S, Holroyd E. Buddhist religious practices and blood pressure among elderly in rural Uttaradit Province, northern Thailand. Nurs Health Sci. 2014;16(1):119–125. doi: 10.1111/nhs.12075. [DOI] [PubMed] [Google Scholar]
- 459.Sukrasorn S. Decision making process and determinants of exercise among urban elderly in Prachuapkhirikhan province. Nakhon Pathom: Faculty of Graduate School, Mahidol University; 2008. [Google Scholar]
- 460.Suksom D, Phanpheng Y, Soogarun S, Sabvarobon S. Effects of Step Aerobics Combined with Resistance Training on Microvascular Function in Overweight Women. Med Sci Sports Exerc. 2011;43:278–279. doi: 10.1249/01.MSS.0000400765.67612.fa. [DOI] [Google Scholar]
- 461.Sumkaew J. Physical exercise behaviors for health of nursing students in Bangkok Metropolis. Bangkok: Faculty of Education, Chulalongkorn University; 2002. [Google Scholar]
- 462.Sumpowthong K. Physical activity assessment and determinants of active living: the development of a model for promoting physical activity among older Thais. Adelaide: University of Adelaide; 2002. [Google Scholar]
- 463.Sunsern R. Effects of exercise on stress in Thai postmenopausal women. Health Care Women Int. 2002;23(8):924–932. doi: 10.1080/07399330290112425. [DOI] [PubMed] [Google Scholar]
- 464.Sununta Y, Sasitorn P, Thitiporn I. The effects of mindfulness eating and yoga exercise on blood sugar levels of pregnant women with gestational diabetes mellitus. Appl Nurs Res. 2014;27(4):227–230. doi: 10.1016/j.apnr.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 465.Supavititpatana B, Phancharoenworakul K, Soen Ae Y, Sinsuksai N, Vorapongsathorn T. Using Theory of Planned Behavior to Predict Physical Activity Intention among Pregnant Thais. Pac Rim Int J Nurs Res. 2012;16(3):192–205. [Google Scholar]
- 466.Supoken A, Chaisrisawatsuk T, Chumworathayi B. Proportion of gynaecologic cancer patients using complementary and alternative medicine. Asian Pac J Cancer Prev. 2009;10(5):779–782. [PubMed] [Google Scholar]
- 467.Suppich D. The development of a model to increase physical activity for adolescences school: participatory action research. Bangkok: Graduate School, Srinakharinwirot University; 2012. [Google Scholar]
- 468.Suriyawongpaisal P, Rajatanavin R, Takkinstien A, Wanvarie S, Apiyasawat P. Physical activity and risk factors for hip fractures in Thai men. Southeast Asian J Trop Med Public Health. 2001;32(1):196–202. [PubMed] [Google Scholar]
- 469.Sutthajunya C. Factors related to the exercise behaviors of Rajabhat institutes undergraduate students in Bangkok Metropolis. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2003. [Google Scholar]
- 470.Suwan K, Hatthachote P, Panichkul S, Phromphetcharat V. Comparision of overweight and obesity in medical cadets before and after 6 months studying at Phramongkutklao College. J Med Assoc Thai = Chotmaihet thangphaet. 2012;95(Suppl 5):S142–S148. [PubMed] [Google Scholar]
- 471.Suwanachaiy S. Six minute walk test in healthy persons with sufficient and insufficient levels of physical activity. Bangkok: Faculty of Medicine, Chulalongkorn, University; 2007. [Google Scholar]
- 472.Suwanachaiy S, Kulaputana O, Chaiwanichsiri D. Walk performance in Thai men and women: Physical activity dependence. Asian Biomed. 2010;4(1):87–93. doi: 10.2478/abm-2010-0010. [DOI] [Google Scholar]
- 473.Suwankruhasn N, Pothiban L, Panuthai S, Boonchuang P. Effects of a Self-management Support Program for Thai People Diagnosed with Metabolic Syndrome. Pac Rim Int J Nurs Res. 2013;17(4):371–383. [Google Scholar]
- 474.Suwanpasu S, Aungsuroch Y, Jitapanya C. Post-surgical physical activity enhancing program for elderly patients after hip fracture: A randomized controlled trial. Asian Biomed. 2014;8(4):525–532. doi: 10.5372/1905-7415.0804.323. [DOI] [Google Scholar]
- 475.Taboonpong S, Puthsri N, Kong-In W, Saejew A. The effects of Tai Chi on sleep quality, well-being and physical performances among older adults. Thai J Nurs Res. 2008;12(1):1–13. [Google Scholar]
- 476.Taechaboonsermsak P, Pitikultang S, Munsawaengsub C, Charupoonphol P. Quality of life and health promoting behaviors among disabled people in two provinces of Thailand. J Med Assoc Thai = Chotmaihet thangphaet. 2009;92(Suppl 7):S54–S58. [PubMed] [Google Scholar]
- 477.Tanasugarn L, Natearpha P, Kongsakon R, Chaosaowapa M, Choatwongwachira W, Seanglaw D, et al. Physical effects and cognitive function after exercising “Rue-si-dad-ton” (Exercise using the posture of the hermit doing body contortion): A randomized controlled pilot trial. J Med Assoc Thai. 2015;98(3):306–313. [PubMed] [Google Scholar]
- 478.Tantayothin S. Factors influencing nutritional and exercise behaviors of hypertensive patients in Sainoi district, Nonthaburi province. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2004. [Google Scholar]
- 479.Tapanee P, Nutritional Status AP. Unhealthy Eating Habits and Physical Activity in Thai Women. Ann Nutr Metab. 2013;63:1773. [Google Scholar]
- 480.Tawata A, Yodmongkon P. Learning in the Context of Inappropriate Internet use Among Students of a Provincial High School in Northern Thailand. Proceedings of the 8th International Conference on Intellectual Capital, Knowledge Management and Organisational Learning. 2011. pp. 539–546. [Google Scholar]
- 481.Taweesak J, Methiya T, Wanwisa B, Nussamol J, Kittisak S. Effects of resistance exercise on cardiopulmonary factors in sedentary individuals. J Phys Ther Sci. 2016;28(1):213–217. doi: 10.1589/jpts.28.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 482.Techatassanasoontorn AA, Thaiprasert N, editors. Internet use and well-being of young adults. International Conference on Information Systems (ICIS 2013): Reshaping Society through Information Systems Design. 2013. [Google Scholar]
- 483.Teeranut H, Borwarnluck T, Parinya R. The Effects of a Physical Activity Program for Fall Prevention among Thai Older Adults. Pac Rim Int J Nurs Res. 2015;19(1):4–18. [Google Scholar]
- 484.Teerarungsikul N, Phuphaibul R, Loveland-Cherry CJ, Pookboonmee R, Kijboonchoo K, Nityasuddhi D. Effectiveness of a physical activity promotion program on perceived self-efficacy, physical activity and physical fitness among Thai adolescent girls. Thai J Nurs Res. 2009;13(2):81–93. [Google Scholar]
- 485.Teparatana C. Factors predicting exercise behaviors in lower secondary school students. Chiang Mai: Graduate School, Chiang Mai University; 1997. [Google Scholar]
- 486.Thanakwang K. Social relationships influencing positive perceived health among Thai older persons: A secondary data analysis using the National Elderly Survey. Nurs Health Sci. 2009;11(2):144–149. doi: 10.1111/j.1442-2018.2009.00438.x. [DOI] [PubMed] [Google Scholar]
- 487.Thanakwang K, Soonthorndhada K. Attributes of Active Ageing among Older Persons in Thailand: Evidence from the 2002 Survey. Asia-Pac Popul J. 2006;21(3):113–135. [Google Scholar]
- 488.Thanakwang K, Soonthorndhada K, Mongkolprasoet J. Perspectives on healthy aging among Thai elderly: A qualitative study. Nurs Health Sci. 2012;14(4):472–479. doi: 10.1111/j.1442-2018.2012.00718.x. [DOI] [PubMed] [Google Scholar]
- 489.Thanyawinichkul P, Aung MN, Moolphate S, Katonyoo C, Chawapong W, Sennun P, et al. Dependency, Disability, Depression and Health Behaviors of the Oldest of the Old Community Residents: A Community Survey in Chiang Mai, Thailand. J Public Health Dev Countries. 2016;2(2):183–198. [Google Scholar]
- 490.Tharnwipat K, Sawakejun T, editors. The study of behaviors and effects of internet technology focus on online game exposure by Thai high school students. ICCTD 2010 - 2010 2nd International Conference on Computer Technology and Development, Proceedings. 2010. [Google Scholar]
- 491.Thasanasuwan W, Srichan W, Kijboonchoo K, Yamborisut U, Wimonpeerapattana W, Rojroongwasinkul N, et al. Low sleeping time, high TV viewing time, and physical inactivity in school are risk factors for obesity in pre-adolescent Thai children. J Med Assoc Thai. 2016;99(3):314–321. [PubMed] [Google Scholar]
- 492.Thavillarp P. Health beliefs and exercise behavior among health science students Chiang Mai University. Chiang Mai: Graduate School, Chiang Mai University; 2004. [Google Scholar]
- 493.Thawornchaisit P, de Looze F, Reid CM, Seubsman S-A, Sleigh A, Team TCS Health-risk factors and the prevalence of hypertension: cross-sectional findings from a national cohort of 87 143 Thai Open University students. Glob JHealth Sci. 2013;5(4):126–141. doi: 10.5539/gjhs.v5n4p126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 494.Thawornchaisit P, de Looze F, Reid CM, Seubsman SA, Sleigh AC. Health risk factors and the incidence of hypertension: 4-year prospective findings from a national cohort of 60 569 Thai Open University students. BMJ Open. 2013;3:e002826. [DOI] [PMC free article] [PubMed]
- 495.Thiamwong L, McManus MS, Suwanno J. Development of the Thai healthy aging model: A grounded theory study. Nurs Health Sci. 2013;15(2):256–261. doi: 10.1111/nhs.12028. [DOI] [PubMed] [Google Scholar]
- 496.Thiamwong L, Suwanno J. Effects of simple balance training on balance performance and fear of falling in rural older adults. Int J Gerontol. 2014;8(3):143–146. doi: 10.1016/j.ijge.2013.08.011. [DOI] [Google Scholar]
- 497.Thitisak H. A study of health behaviors of women with hypertension in the Bangkok metropolitan area. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 1997. [Google Scholar]
- 498.Thojampa S. Preliminary Results of the Moderating Effect of Social Cognitive Factors on Self-Management Activities and HbA1c in Thai Adults with Type 2 Diabetes. Nurs Res. 2016;65(2):E21. doi: 10.1016/j.ijnss.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 499.Thongbai W, Fongkaew W, Kennedy CM, Aree P, Patumanond J. Risk factors contributing to overweight among preschool children. Pac Rim Int J Nurs Res. 2011;15(1):13–27. [Google Scholar]
- 500.Thongkambunjong W, ChooChom O, Intasuwan P, Supparerkchaisakul N. Causal factors and effect of internet dependency behavior of high school students in Bangkok Metropolis. J Behav Sci. 2011;17(2):103–120. [Google Scholar]
- 501.Thonglong T. Lifestyle and health behaviors of Thai people in Ubon Ratchathani province. Bangkok: Faculty of Sports Science, Chulalongkorn University; 2013. [Google Scholar]
- 502.Thongmuang P, Suwannahong K. Health behaviors of undergraduate students in Suan Sunandha Rajabhat University. 7th World Conference on Educational Sciences. Procedia Soc Behav Sci. 2015;197:973–976. doi: 10.1016/j.sbspro.2015.07.285. [DOI] [Google Scholar]
- 503.Thongtanunam Y, Salveson C. Perceived barriers & social support for physical activity among Thai working women. Commun Nurs Res. 2010;43:342. [Google Scholar]
- 504.Thongthawee B, Sangwatanaroj S, Sanguanrungsirikul S. Effects of Guang-Im-Ju-Jai-Gong Qigong on Endothelial Function, Cardio-Ankle Vascular Index (CAVI), Ankle Brachial Index (ABI) in Female Adults with Metabolic Syndrome. J Exerc Physiol Online. 2016;19(1):39–49. [Google Scholar]
- 505.Thuree C. Effect of brisk walking exercise and aerobic dance on blood pressure among persons with hypertension. Chiang Mai: Graduate School, Chiang Mai University; 2004. [Google Scholar]
- 506.Tongprasert S, Wattanapan P. Aerobic capacity of fifth-year medical students at Chiang Mai University. J Med Assoc Thai. 2007;90(7):1411–1416. [PubMed] [Google Scholar]
- 507.Tongtiam W. Predicting factors of physical activity in patients after post coronary artery bypass graft surgery. Bangkok: Faculty of Nursing, Chulalongkorn University; 2013. [Google Scholar]
- 508.Topothai T, TopoThai C, Phonguttha S, Suriyawongpisarn W, Chantrasiri O, Thamrungsi T. The Daily Energy Expenditure of 4 Domains of Physical Activity of Thai Adults. J Health Syst Res. 2015;9(2):168–180. [Google Scholar]
- 509.Totermsuck V. The study of perceived benefits and situational influences to exercise behavior in the elderly with diabetes mellitus. Nakorn Pathom: Faculty of Graduate Studies, Mahidol University; 2000. [Google Scholar]
- 510.Triprakong S, Sangmanee W, Thavalphasit K. Factors Influencing Exercise Behavior of Nursing Department Personnel in Songklanagarind Hospital. J Fac Nurs Burapha Univ. 2012;20(2):75–92. [Google Scholar]
- 511.Tunkamnerdthai O, Auvichayapat P, Donsom M, Leelayuwat N. Improvement of pulmonary function with arm swing exercise in patients with type 2 diabetes. J Phys Ther Sci. 2015;27(3):649–654. doi: 10.1589/jpts.27.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 512.Upala S, Sanguankeo A, Homsanit M. Lifestyle behaviors as predictors of bad quality of life in Thai resident physicians. Qual Life Res. 2013;22:44. [Google Scholar]
- 513.Usman Y. Factors related to obesity in primary school children: A case study of Nakhon Pathom province. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2004. [Google Scholar]
- 514.Vannarit T. Predictors of exercise activity among rural Thai older adults. Alabama: the United States: School of Nursing, University of Alabama at Birmingham; 1999. [Google Scholar]
- 515.Varothai C, Siengsanor C, Hematorn J, Poomriew R, Silpasuwan P, Vongjaturapat N. The development of an exercise program focusing on elderly participation in elderly home, Banglamung, Cholburi province. J Public Health. 1996;26(1):15–26. [Google Scholar]
- 516.Vathesatogkit P, Sritara P, Kimman M, Hengprasith B, E-Shyong T, Wee HL, et al. Associations of Lifestyle Factors, Disease History and Awareness with Health-Related Quality of Life in a Thai Population. PLoS ONE. 2012;7(11):e49921. doi: 10.1371/journal.pone.0049921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 517.Vichiansiri R, Saengsuwan J, Manimmanakorn N, Patpiya S, Preeda A, Samerduen K, et al. The prevalence of dyslipidaemia in patients with spinal cord lesion in Thailand. Cholesterol. 2012;2012:1–6. doi: 10.1155/2012/847462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 518.Vijakkhana N, Wilaisakditipakorn T, Ruedeekhajorn K, Pruksananonda C, Chonchaiya W. Evening media exposure reduces night-time sleep. Acta Paediatr. 2015;104(3):306–312. doi: 10.1111/apa.12904. [DOI] [PubMed] [Google Scholar]
- 519.Vinijkul S. The effect of an exercise program applying trans-theoretical model on obesity in people in community of Bangplat district, Bangkok metropolitan. Ramathibodi Nurs J. 2010;16(3):327–340. [Google Scholar]
- 520.Visuthipanich V, Sirapo-ngam Y, Malathum P, Kijboonchoo K, Vorapongsathorn T, Winters-Stone K. Physical activity questionnaire development and testing among elderly community-dwelling Thais. Thai J Nurs Res. 2009;13(4):249–267. [Google Scholar]
- 521.Voraroon S, Phosuwan A, Jaiyangyeun U, Bunyasit P. The predictors of exercise behavior among health volunteers, Sanamchai, Mueng district, Suphanburi province. J Nurs Educ. 2011;4(1):52–61. [Google Scholar]
- 522.Wachirapon S. An analysis of youth behaviors related playing computer games. Nakhon Pathom: Faculty of Graduate Studies, Mahidol University; 2005. [Google Scholar]
- 523.Wakabayashi M, McKetin R, Banwell C, Yiengprugsawan V, Kelly M, Sam-ang S, et al. Alcohol consumption patterns in Thailand and their relationship with non-communicable disease. BMC Public Health. 2015;15:1–9. doi: 10.1186/s12889-015-2662-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 524.Wanajak K. Internet use and its impact on secondary school students in Chiang Mai, Thailand. Western Australia: Faculty of Computing, Health and Science, Edith Cowan University; 2011. [Google Scholar]
- 525.Wangsrikhun S. Assessment of factors that influence bone mass among postmenopausal Thai women. PhD [dissertation] Illinois: University of Illinois at Chicago; 2003. [Google Scholar]
- 526.Wanitkun N. Validation of questionnaires for exercise research among Thai middle-aged and older adults with coronary artery disease. Oregon: the United States: School of Nursing, Oregon Health & Science University; 2003. [Google Scholar]
- 527.Wannasuntad S. Factors predicting Thai children's physical activity. San Francisco: University of California; 2007. [Google Scholar]
- 528.Watcharathanakij S, Moolasarn S, Phanritdam S, Noobome M. Physical Exercise Behavior of Ubon Ratchathani University Undergraduate Students. Isan J Pharm Sci (IJPS). 2012;8(3):35–47. [Google Scholar]
- 529.Wattanapisit A, Fungthongcharoen K, Saengow U, Vijitpongjinda S. Physical activity among medical students in Southern Thailand: a mixed methods study. BMJ open. 2016;6(9):e013479. doi: 10.1136/bmjopen-2016-013479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 530.Wattanapisit A, Gaensan T, Anothaisintawee T, editors. Prevalence of physical activity and associated factors of medium and high activity among medical students at Ramathibodi Hospital. The 6th International Conference on Sport and Exercise Science 2015. Pattaya: Institute of Physical Education (IPE), Faculty of Sports and Health Science; 2015. [Google Scholar]
- 531.Wattanasirichaigoon S, Polboon N, Ruksakom H, Boontheaim B, Sithisarankul P, Visanuyothin T. Thai physicians’ career satisfaction. J Med Assoc Thai = Chotmaihet thangphaet. 2004;87(Suppl 4):S5–S8. [PubMed] [Google Scholar]
- 532.Wattanasirichaigoon S, Ruksakom H, Polboon N, Sithisarankul P, Visanuyothin T. Thai physicians health survey. J Med Assoc Thai = Chotmaihet thangphaet. 2004;87(Suppl 4):S1–S4. [PubMed] [Google Scholar]
- 533.Wattanasit P. Determinants of physical activity in Thai adolescents: Testing the youth physical activity promotion model. Songkla: Nursing (International Program), Prince of Songkla University; 2009. [Google Scholar]
- 534.Wattanasit P, Prateepchaikul L, Petpichetchian W, Meininger JC, Kijboonchoo K. Validity and reliability of the modified Thai adolescent's physical activity questionnaire. Pac Rim Int J Nurs Res. 2010;14(1):79–92. [Google Scholar]
- 535.Weiangkham D, Kerdmongkol P, Amnatsatsue K, Sasat S, Steckler AB. Problems and needs of the elderly in Northern Thailand remote area. Kasetsart J - Nat Sci. 2014;35(3):516–523. [Google Scholar]
- 536.Wichaidit W, Sangthong R, Chongsuvivatwong V, McNeil E, Chariyalertsak S, Kessomboon P, et al. Religious affiliation and disparities in risk of non-communicable diseases and health behaviors: Findings from the fourth Thai National Health Examination Survey. Glob Public Health. 2014;9(4):426–435. doi: 10.1080/17441692.2014.894549. [DOI] [PubMed] [Google Scholar]
- 537.Wichitsranoi J, Pilarit J, Klomkamonl W, Ploynamngern N, Wongsathikun J, editors. Effects of Thai wand exercise on lung capacity in sedentary young adults. The 40th PST Annual Meeting International Conference. Khon Kaen: Journal of Physiological and Biomedical Sciences (JPBS).; 2011. [Google Scholar]
- 538.Wimonpeerapattana W. Physical Activity Questionnaire Development and Norms Setting for Thai Children. Ann Nutr Metab. 2009;55:186. [Google Scholar]
- 539.Wimonpeerapattana W, Kijboonchoo K, Thasanasuwan W, Pongurgsorn C. Development and Validation of the Physical Activity Questionnaire for Thai Children. KKU Res J. 2013;18:548–557. [Google Scholar]
- 540.Wongsapan A. Effect of walking exercise program with social support on blood pressure reduction and self-care behavior in patients with essential hypertension. Khon Kaen: Graduate School, Khon Kaen University; 2006. [Google Scholar]
- 541.Wongvilai N. Psychological factors affecting the continuing exercise behavior of customers at Nalinrut fitness centre. Bangkok: Graduate School, Kasem Bundit University; 2004. [Google Scholar]
- 542.Woratanarat P, Kijkunastian C, Wajanavisit W, Suppaphol S, Woratanarat T, Rajatanavin R, et al. A comparative study of risk factors of femoral neck and intertrochanteric fracture in Thai men. J Med Assoc Thai = Chotmaihet thangphaet. 2009;92(Suppl 6):S165–S171. [PubMed] [Google Scholar]
- 543.Woratanarat P, Kijkunastian C, Wajanavisit W, Suppaphol S, Woratanarat T, Rajatanavin R, et al. Different risk magnitudes of femoral neck and intertrochanteric fractures in Thai women. J Med Assoc Thai = Chotmaihet thangphaet. 2009;92(Suppl 6):S172–S180. [PubMed] [Google Scholar]
- 544.Xuto P, Sinsuksai N, Piaseu N, Nityasuddhi D, Phupong VA. Causal Model of Postpartum Weight Retention among Thais. Pac Rim Int J Nurs Res. 2012;16(1):48–63. [Google Scholar]
- 545.Yamchanchai W. The relationship between perceived self-efficacy, perceived health status and health-promoting behaviors in elderly persons. Nakhon Pathom: Faculty of Graduate School, Mahidol University; 1995. [Google Scholar]
- 546.Yamwong N, Limpisopon T, Yamwong A. Effectiveness of walking meditation on physical fitness, short memory and emotional quotient of the aged in Nakhon Nayok province. Bangkok: Physical Activity Research Centre, Thai Health Promotion Foundation; 2015.
- 547.Yiammit C. The study of exercise behavior of Rambhai Barni Rajabhat in academic year 2010. Bangkok: Graduate School, Srinakharinwirot University; 2013. [Google Scholar]
- 548.Yiengprugsawan V, Banwell C, S-a S, Sleigh AC, Team TCS. Short sleep and obesity in a large national cohort of Thai adults. BMJ Open. 2012;2(1):e000561. doi: 10.1136/bmjopen-2011-000561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 549.Yingyong P. Risk factors for refractive errors in primary school children (6-12 years old) in Nakhon Pathom province. J Med Assoc Thai. 2010;93(11):1288–1293. [PubMed] [Google Scholar]
- 550.Yoo S, Kim H, Cho HI. Heterogeneity in obesity status and cardiovascular risks in multiethnic Asian female immigrants in South Korea. Asia-Pac J Public Health. 2015;27(2):NP448–NNP56. doi: 10.1177/1010539512459751. [DOI] [PubMed] [Google Scholar]
- 551.Yotharin C, Pumpaibool T, Chapman RS. Risk factors of type II diabetes mellitus among people aged 40 years and above in Ban-Na Makhuea sub-district, sahatsakhan district, Kalasin province, Thailand. J Health Res. 2014;28:S7–S14. [Google Scholar]
- 552.Youngpradith A, Gretebeck KA, Charoenyooth C, Phancharoenworakul K, Vorapongsathorn T. A causal model of promoting leisure-time physical activity among middle-aged Thai women. Thai J Nurs Res. 2005;9(1):49–62. [Google Scholar]
- 553.Youngwanichsetha S, Phumdoung S, Cersosimo E. Effects of a metabolic syndrome self-management programme for women with pre-diabetes. Focus Altern Complement Ther. 2015;20(2):74–80. doi: 10.1111/fct.12176. [DOI] [Google Scholar]
- 554.Youngwanichsetha S, Phumdoung S, Ingkathawornwong T. The effects of tai chi qigong exercise on plasma glucose levels and health status of postpartum Thai women with type 2 diabetes. Focus Altern Complement Ther. 2013;18(4):182–187. doi: 10.1111/fct.12064. [DOI] [Google Scholar]
- 555.Yousomboon C, Choolert P, Pensirinapa N, Katewongsa P. The same but different: Workplace, occupational style, and physical activity of Thai urban worker. J Sci Med Sport. 2014;18:e156. doi: 10.1016/j.jsams.2014.11.174. [DOI] [Google Scholar]
- 556.Yuenyongchaiwat K. The Effects of The Pedometer-based Intervention on Body Composition in Middle-aged Thais with Overweight: A Preliminary Study. Thammasat Int J Sci Technol. 2015;20(4):38–45. [Google Scholar]
- 557.Zhao J, Pachanee C-a, Yiengprugsawan V, Seubsman S-a, Sleigh A. Smoking, smoking cessation, and 7-year mortality in a cohort of Thai adults. Popul Health Metrics. 2015;13(1):30. doi: 10.1186/s12963-015-0062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 558.Zhao J, Seubsman S-a, Sleigh A, Thai Cohort Study Team t Timing of urbanisation and cardiovascular risks in Thailand: evidence from 51 936 members of the Thai cohort study, 2005–2009. J Epidemiol. 2014;24(6):484–493. doi: 10.2188/jea.JE20140063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 559.กระแจะจันทร์ สวก. การศึกษาพฤติกรรมการออกกำลังกายและการเล่นกีฬาของนักศึกษาในสถาบัน เทคโนโลยีราชมงคลและสถาบันราชภัฏ [A Study of exercise and sporting behaviors of students in Rajaman gala Institutes of Technology and Rajabhat Institutes]. Bangkok: Graduate School, Chulalongkorn University; 2001.
- 560.กาญจนกิจ สต, เมรานนท์ สร, ดามาพงศ์ พด, กองจินดา วสต. รูปแบบการส่งเสริมการเคลื่อนไหว ร่างกาย/ออกกำลังกาย สำหรับประชาชนในองค์กรบริหารส่วนตำบล (อบต.) [Patterns of physical activity/exercise promotion for people in local government administration]. Nonthaburi: Division of Physical Activity & Health, Department of Health, Ministry of Public Health; 2005.
- 561.กาวิละพภ.กระบวนการออกกำลังกายอย่างต่อเนื่องของนักเรียนที่เข้ามาใช้บริการออกกำลังกายในสถาบันการพลศึกษาวิทยาเขตลำปา [Continuing exercises process in student exerting exercise at Institute of Physical Education Lampang]. วารสารวิชาการ สถาบันการพลศึกษา [Academic Journal Institute of Physical Education]. 2012; 4(1): 45-65.
- 562.ขจรบุญ ศร, กนกสุนทรรัตน์ นโ, ศิริพิทยาคุณกิจ อญ. กิจกกรมทางกายในผู้เป็นเบาหวานชนิดที่ 2 ที่ควบคุมระดับน้ำตาลในเลือดไม่ได้ [Physical activities in persons with uncontrolled type 2 diabetes mellitus]. การประชุมวิชาการเสนอผลงานวิจัยระดับบัณฑิตศึกษาแห่งชาติครั้งที่ 23; มหาวิทยาลัยเทคโนโลยีราชมงคลอีสาน 2011.
- 563.ขัติยะ กตพ. กิจกรรมทางกายของนักศึกษาระดับปริญญาตรี มหาวิทยาลัยแม่โจ้ จังหวัดเชียงใหม่ [Physical activity of Maejo University undergraduates, Chiang Mai province]. Chiang Mai, Thailand: 2015.
- 564.ขันธบุตร น. การศึกษาพฤติกรรมการออกกำลังกายและการเล่นกีฬาของนักศึกษามหาวิทยาลัยแม่โจ้ [A Study of exercise taking behaviors and sporting of Maejo University Students]. Chiang Mai, Thailand: 2005.
- 565.คำรศ ว, ภูมิฤทธิกุล พม, มัททวางกูร ชด, นวลแจ่ม เญง, จันทร์เจริญ กลด, หงษ์ไกรเลิศ เ, et al. พฤติกรรมและการเข้าถึงการออกกำลังกายของคนภาษีเจริญ [Behavior and accessibility for exercise of Pasi Charoen persons]. Bangkok, Thailand: 2013.
- 566.เงินทอง วชน, ทองวินิชศิลป์ เยย, เงินทอง กง. ปัจจัยที่มีอิทธิพลต่อพฤติกรรมการออกกำลังกายของสมาชิกชมรมสร้างสุขภาพจังหวัดสุโขทัย [Factors affecting exercising behavior of member in the health promotion clubs, SukhoThai province]. วารสารวิชาการ สถาบันการพลศึกษา. 2014; 6(2): 51-63.
- 567.จงถาวรสถิตย์ สกญ, ลักษณากร วภ, สานุศิษย์ สว. โปรแกรมกิจกรรมทางกาย สำหรับผู้ป่วยความดันโลหิตเริ่มสูงหรือความดันโลหิตสูงปานกลางที่มารักษาศูนย์การแพทย์กาญจนาภิเษก [Physical activity program for prehypertension or mild hypertension patients at Golden Jubilee Medical Centre]. Bangkok, Thailand.
- 568.จรรยาเจริญ ทศก.ผลของการออกกำลังกายแบบรำเซิ้งอีสานต่อความสามารถทางกายและคุณภาพชีวิตในผู้สูงอายุชาวไทย [Effects of Isaan dance on physical performance and quality of life in Thai elderly]. Bangkok, Thailand: 2016.
- 569.ชลานุภาพ บศน. การศึกษาความสัมพันธ์ระหว่างทัศนคติในการดูแลสุขภาพกับพฤติกรรมการออกกำลังกายของบุคคลวัยทำงานในเขตกรุงเทพมหานคร [A study of the association between attitude of healthcare and exercise behavior of working adults in Bangkok metropolitan]. Bangkok, Thailand: Graduate School, Bangkok University; 2009.
- 570.ชาติวงศ์ พสษ. การใช้เวลาว่างและพฤติกรรมการออกกำลังกายของนักเรียนชั้นมัธยมศึกษาตอนต้นของโรงเรียนมัธยมศึกษาในเขตเทศบาลนครยะลา [The use of free time and exercise behaviors of lower secondary school students in Yala municipality]. วารสารวิชาการ สถาบันการพลศึกษา. 2014; 6(1): 1-15.
- 571.ชื่นวัฒนา ว, สอนภักดี ณช. พฤติกรรมการดูแลสุขภาพตนเองของผู้ป่วยโรคเบาหวาน ตำบลบางแม่นาง อำเภอบางใหญ่ จังหวัดนนทบุรี [Self-care behaviors of diabetic patients in Bang Maenang sub-district, Bang Yai district, Nonthaburi province]. วารสารวิชาการ มหาวิทยาลัยปทุมธานี. 2014; 6(3): 163-70.
- 572.เชยชม กอย. พฤติกรรมการออกกำลังกายของนักเรียนประถมศึกษาในจังหวัดกระบี่ [Exercise behavior of pupils in Krabi province]. วารสารวิชาการ สถาบันการพลศึกษา. 2015; 7(1): 29-38.
- 573.เซ็ม สว. การศึกษาพฤติกรรมการออกกำลังกายและการเล่นกีฬาของนิสิตนักศึกษาในมหาวิทยาลัยของรัฐ [A study of exercise and sport behaviors of the students of the government universities]. Bangkok, Thailand: Graduate School, Chulalongkorn University; 1999.
- 574.ทองสุขนอก จน, ธีระวิวัฒน์ มรต, อิมามี นรต. ปัจจัยที่มีผลต่อพฤติกรรมการออกกำลังกายของผู้สูงอายุ ชมรมผู้สูงอายุ โรงพยาบาลเจริญกรุงประชารักษ์ [Factors associated to exercise behaviors of elderly, elderly club, Charoenkrunk Pracharak hospital]. วารสารสุขศึกษา [Journal of Health Education]. 2008; 31(110): 107-23.
- 575.นนทะคุณ มร. พัฒนากิจกรรมการส่งเสริมให้ประชาชนออกกำลังกาย กรณีศึกษา บ้านโคกแสง ตำบลคูสะคาม อำเภอวานรนิวาส จังหวัดสกลนคร [The development of activities for promoting people's exercise: a case study in Khoksaeng village, Tambon Kusakham, Amphoe Wanonniwaat, Changwat Sakon Nakhon]. วารสารบัณฑิตศึกษา มหาวิทยาลัยราชภัฏสกลนคร [Graduate Studies Journal]. 2007 (ฉบับพิเศษ): 276-89.
- 576.นาคะ ขษ, ตะบูนพงศ์ สนต, คู่พันธวี เ. สถานการณ์การออกกำลังกายของผู้สูงอายุในจังหวัดสงขลา [Exercise situation of the elderly in Songkla province]. Songkla, Thailand: 2002.
- 577.นิ่มมาก ณฤ, สิงห์น้อย ฉต. แรงจูงใจในการออกกำลังกายของผู้ที่มาใช้บริการศูนย์วิทยาศาสตร์การกีฬาของสถาบันการพลศึกษา วิทยาเขตศรีสะเกษ [Exercise motivation for people who come to use services of the sports science centre at the Institute of Physical Education, Sisaket campus]. วารสารวิชาการ สถาบันการพลศึกษา. 2015; 7(2): 1-13.
- 578.บุญรอง ผ. การออกกำลังกายและการเล่นกีฬาของนักศึกษาระดับอุดมศึกษาในจังหวัดศรีสะเกษ [Exercises and sports of undergraduate students in Srisaket province]. Maha Sarakham, Thailand: Mahasarakham University; 2007.
- 579.พลนิล ศว. พฤติกรรมการออกกำลังกายของนักศึกษาปริญญาตรี สถาบันการพลศึกษา วิทยาเขตใต้ [The exercise behaviors of undergraduate students in institutes of physical education in South campus regions]. Chumphon, Thailand: Chumphon Campus Physical Education Institute; 2010.
- 580.พลรัตน์ นรน, ศิลาดี ก, ประทีปแก้ว นรน, ชื่นม่วง อช, โอกาศรัตน์ ส, พุตกรณ์ ว. ปัจจัยที่เกี่ยวข้องกับการออกกำลังกายของนักศึกษามหาวิทยาลัยธรรมศาสตร์ศูนย์รังสิต [Related factors to student's exercise at Thammasat University Rangsit Campus]. วารสารวิทยาศาสตร์และเทคโนโลยี มหาวิทยาลัยธรรมศาสตร์. 2004; 12(1): 65-71.
- 581.เพียรพึ่งตน เมต, พฤฒิสาร เ, ชูชาติ พ. ปัจจัยที่มีอิทธิพลต่อการออกกำลังกายของบุคลากรทางการแพทย์และสาธารณสุขที่อาศัยอยู่ในโรงพยาบาลพุทธชินราช จังหวัดพิษณุโลก [Factors influencing exercise among medical personnel residing in Buddhachinnaraj hospital]. Phitsanulok, Thailand: 2012.
- 582.มัททวางกูร ชด, นวลแจ่ม เญง, ภูมิฤทธิกุล พม, คำรศ ว, จันทร์เจริญ กลด, หงษ์ไกรเลิศ เ, et al. ภูมิปัญญาท้องถิ่นและวิถีชีวิตที่ส่งเสริมกิจกรรมทางกายและการออกกำลังกายของคนภาษีเจริญ [Local wisdom and life style of Pasi Charoen persons for promoting physical activity and exercise]. Bangkok, Thailand.
- 583.มากเจริญ กช. พฤติกรรมการออกกำลังกายของนักศึกษาระดับปริญญาตรี มหาวิทยาลัยราชภัฏบุรีรัมย์ [Physical exercise behavior of Buriram Rajabhat University undergraduate students]. วารสารวิจัยและพัฒนา มหาวิทยาลัยราชภัฏบุรีรัมย์. 2015; 10(2): 38-47.
- 584.ยือแร กย, ลิ้มชัยอรุณเรือง สต, สิงห์ช่างชัย เอ. การส่งเสริมการออกกำลังกายตามหลักศาสนาอิสลาม ในกลุ่มแม่บ้าน จังหวัดปัตตานี [Principles of physical activity promotion and exercise in Muslim]. วารสาร AL-NUR บัณฑิตวิทยาลัย. 2010; 5(9): 83-96.
- 585.ราชรุจิทอง พ, วงศ์จตุรภัทร น, นิยมางกูร สรน. ผลของการแทรกกิจกรรมทางกายที่มีต่อแรงจูงใจตามสถานการณ์ ความเชื่อมั่นตนเองเฉพาะด้าน และความรู้สึกที่ดีต่อร่างกายตนเอง [Effect of physical activities intervention on situational motivation, self-efficacy and body self-esteem]. Chonburi, Thailand.
- 586.รีรมย์ วญ. ความต้องการจัดบริการด้านการออกกำลังกายเพื่อสุขภาพของประชาชน อำเภอร้องกวาง จังหวัดแพร่ [The need for services for exercising for health by personal at Rongkwang Phrae]. Chiang Mai, Thailand: 2009.
- 587.ไวยวรรณจิตร สรย, มะเก็ง มฮดร, จินตารา นร. วิถีชีวิตของประชาชนมุสลิมที่ส่งผลต่อการสร้างเสริมสุขภาพผ่านการมีกิจกรรมทางกายอย่างเพียงพอ [Effects of the way of life of Muslim on health promotion through sufficient physical activity]. Bangkok, Thailand.
- 588.ศรภิรมย์ สญช, ทำนอง ชศ. ปัจจัยที่มีอิทธิพลต่อพฤติกรรมการออกกำลังกายของผู้ป่วยโรคหลอดเลือดหัวใจภายหลังการขยายหลอดเลือดหัวใจ [Factors effecting exercise behaviors of patients with coronary artery disease post percutaneous coronary intervention]. วารสารพยาบาลศาสตร์และสุขภาพ [Journal of Nursing Science and Health]. 2009; 32(1): 25-35.
- 589.ศิริแพทย์ อต. พฤติกรรมการออกกำลังกายของนิสิตที่เรียนรายวิชาการออกกำลังกายเพื่อสุขภาพ [Exercise behaviors of exercise for health's students]. วารสารคณะพลศึกษา. 2012; 15 (ฉบับพิเศษ): 452-8.
- 590.สริยุทธ วธ. พฤติกรรมการออกกำลังกายด้วยการเต้นแอโรบิกของประชาชนเขตกรุงเทพมหานคร [Exercise behaviors using aerobics of residents in the Bangkok metropolitan area]. วารสารวิชาการ สถาบันการพลศึกษา. 2012; 4(2): 51-65.
- 591.สุขชัยสงค์ นต, พิชยภิญโญ ปน, กลัมพากร สรน. การประยุกต์ทฤษฎีขั้นตอนการเปลี่ยนแปลงพฤติกรรมในการส่งเสริมการออกกำลังกายของนักศึกษาพยาบาล วิทยาลัยพยาบาลเกื้อการุณย์ สำนักการแพทย์ กรุงเทพมหานคร [An exercise promotion program applying the trans-theoretical model in nursing students at Kuakarun College of Nursing, Department of Medicine, Bangkok Metropolitan Administration]. วารสารพยาบาลสาธารณสุข [Journal of Public Health Nursing]. 2011; 25(1): 1-15.
- 592.สุรกิจ จม, ธีรเวชเจริญชัย สพฒ. ปัจจัยที่มีผลต่อพฤติกรรมการออกกำลังกายเพื่อสุขภาพของบุคลากรในสังกัดสำนักงานสาธารณสุขจังหวัดสมุทรสงคราม [Factors affecting exercise behaviors for health among the provincial public health officers of Samut Songkhram province]. วารสารวิทยาลัยพยาบาลพระปกเกล้า จันทบุรี [Journal of Phrapokklao Nursing College]. 2007; 18(2): 22-32.
- 593.สุริยะกาญจน์ ภภ. พฤติกรรมการออกกำลังกายของประชาชนที่มาออกกำลังกายด้วยการเต้นแอโรบิกส์ในบริเวณสวนหลวง ร.9 [Exercise behaviors of people who come to aerobics exercising group at Suanluang XI park]. Chonburi, Thailand: Graduate School of Public Administration, Burapha University; 2006.
- 594.หลวงทิพย์ กนก, สีนวล ดณ. การศึกษาพฤติกรรมการออกกำลังกายของบุคลากรในโรงพยาบาลสามชุก อำเภอสามชุก จังหวัดสุพรรณบุรี [The study of exercise behavior of staffs in Samchook hospital, Samchook district, Suphanburi province]. Nakhon Pathom, Thailand: Science and Technology, Nakhon Pathom Rajabhat University; 2007.
- 595.อนันตพงศ์ วรน. พฤติกรรมส่งเสริมสุขภาพด้านการออกกำลังกายของนักศึกษาวิทยาลัยการ สาธารณสุขสิรินธรจังหวัดยะลา [Health promotion behavior by exercise of the students at Sirindhorn College of Public Health, Yala province]. Bangkok, Thailand: National Institute of Development Administration (NIDA); 2002.
- 596.เอกพลากร วชย, ปรปักษ์ขาม เต, ฐานีพานิชสกุล สรก, พรรคเจริญ หย, เสถียรนพเก้า ว, ไทยกล้า กษ. รายงานการสำรวจสุขภาพประชาชนไทยโดยการตรวจร่างกาย ครั้งที่ 4 พ.ศ. 2551-2 [The 4th National Health Examination 2008-2009]. เอกพลากร วชย, editor. จังหวัดนนทบุรี ประเทศไทย: สถาบันวิจัยระบบสาธารณสุข (สวรส.); 2008.
- 597.เอกพลากร วชย, พรรคเจริญ หย, ไทยกล้า กษ, เสถียรนพเก้า ว. รายงานการสำรวจสุขภาพประชาชนไทยโดยการตรวจร่างกาย ครั้งที่ 5 พ.ศ. 2557-8 [The 5th National Health Examination 2014-2015]. เอกพลากร วชย, editor. จังหวัดนนทบุรี ประเทศไทย: สถาบันวิจัยระบบสาธารณสุข (สวรส.); 2014.
- 598.โอนสูงเนิน อวน, อินต๊ะหล่อ พม. สภาพแวดล้อมทางกายภาพและสิ่งอำนวยความสะดวกของพื้นที่ที่ใช้ในการเต้นแอโรบิกที่มีผลต่อพฤติกรรมการออกกำลังกายด้วยการเต้นแอโรบิก [The relationship between physical environment and venue facilities for aerobic dance on aerobic dance exercise behavior]. วารสารวิชาการ สถาบันการพลศึกษา. 2014; 6(2): 31-49.
- 599.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(Suppl 9):S498–S516. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 600.Caspersen CJ, Powell KE, Christenson G. Physical activity, exercise and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- 601.Rhodes RE, Lubans DR, Karunamuni N, Kennedy S, Plotnikoff R. Factors associated with participation in resistance training: a systematic review. Br J Sports Med. 2017;51(20):1466–1472. doi: 10.1136/bjsports-2016-096950. [DOI] [PubMed] [Google Scholar]
- 602.Bennie JA, Pedisic Z, van Uffelen JGZ, Charity MJ, Harvey JT, Banting LK, et al. Pumping Iron in Australia: Prevalence, Trends and Sociodemographic Correlates of Muscle Strengthening Activity Participation from a National Sample of 195,926 Adults. PLoS ONE. 2016;11(4):e0153225. doi: 10.1371/journal.pone.0153225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 603.Division of Physical Activity and Health. Department of Health . Thailand Recommendations on Physical Activity, Non-Sedentary Lifestyles and Sleeping. Nonthaburi: Ministry of Public Health; 2017. [Google Scholar]
- 604.Owen N, Leslie E, Salmon J, Fotheringham MJ. Environmental determinants of physical activity and sedentary behavior. Exerc Sport Sci Rev. 2000;28(4):153–158. [PubMed] [Google Scholar]
- 605.Marshall SJ, Biddle SJH, Sallis JF, McKenzie TL, Conway TL. Clustering of sedentary behaviors and physical activity among youth: A cross-national study. Paediatr Exerc Sci. 2002;14(4):401–417. [Google Scholar]
- 606.Owen N, Bauman A, Brown W. Too much sitting: A novel and important predictor of chronic disease risk? Br J Sports Med. 2009;43(2):81–83. doi: 10.1136/bjsm.2008.055269. [DOI] [PubMed] [Google Scholar]
- 607.Pate RR, O'Neill JR, Lobelo F. The evolving definition of “sedentary”. Exerc Sport Sci Rev. 2008;36(4):173–178. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 608.Dumuid D, Pedišić Ž, Stanford TE, Martín-Fernández JA, Hron K, Maher C, et al. The Compositional Isotemporal Substitution Model: A method for estimating changes in a health outcome for reallocation of time between sleep, sedentary behaviour, and physical activity. Stat Methods Med Res. in press [DOI] [PubMed]
- 609.Tremblay MS, Carson V, Chaput J-P, Gorber SC, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl Physiol, Nutr Metab. 2016; 10.1139/apnm-2016-0151. [DOI] [PubMed]
- 610.New Zealand Ministry of Health . Sit less, move more, sleep well: Physical activity guidelines for children and young people. 2017. [Google Scholar]
- 611.Okely AD, Ghersi D, Hesketh KD, Santos R, Loughran SP, Cliff DP, et al. A collaborative approach to adopting/adapting guidelines-The Australian 24-Hour Movement Guidelines for the early years (Birth to 5 years): an integration of physical activity, sedentary behavior, and sleep. BMC Public Health. 2017;17(5):869. doi: 10.1186/s12889-017-4867-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 612.Welk G. Physical Activity Assessments for Health-Related Research. Champaign: Human Kinetics; 2002. [Google Scholar]
- 613.Shephard RJ, Aoyagi Y. Measurement of human energy expenditure, with particular reference to field studies: An historical perspective. Eur J Appl Physiol. 2012;112(8):2785–2815. doi: 10.1007/s00421-011-2268-6. [DOI] [PubMed] [Google Scholar]
- 614.Pedišić Ž, Bauman A. Accelerometer-based measures in physical activity surveillance: current practices and issues. Br J Sports Med. 2015;49(4):219–223. doi: 10.1136/bjsports-2013-093407. [DOI] [PubMed] [Google Scholar]
- 615.Lee I-M, Shiroma EJ. Using accelerometers to measure physical activity in large-scale epidemiological studies: issues and challenges. Br J Sports Med. 2014;48:197–201. doi: 10.1136/bjsports-2013-093154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 616.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 617.Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011;22(1):7–14. [PubMed] [Google Scholar]
- 618.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, et al. American college of sports medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 619.Bauman AE, Sallis JF, Dzewaltowski DA, Owen N. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med. 2002;23(Suppl 2):5–14. doi: 10.1016/S0749-3797(02)00469-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search keywords. Detailed search keywords including the full search syntaxes used for each database. (PDF 183 kb)
Data extraction table. The detailed table of all data extracted from each study included in this review. (XLSX 245 kb)
Data Availability Statement
The summary of reviewed articles is available in Tables, Figures, and Additional files.