Abstract
Objective
Compare the maximal isokinetic muscle strength of knee extensor and flexor muscles between patients with knee osteoarthritis and patients submitted to total knee arthroplasty.
Methods
Volunteers were divided into five groups (n = 20): Control; Ahlbäck I and II; Ahlbäck IV; six months after total knee arthroplasty; 12 months after total knee arthroplasty. An isokinetic knee strength evaluation was conducted for the quadriceps and hamstrings at 60°/s.
Results
Significant differences in the peak torque of the quadriceps and hamstrings were found among the groups (p < 0.001). The Ahlbäck IV, six-month, and 12-month postoperative groups demonstrated lower values when compared to the Control and Ahlbäck I and II groups. When percentage values were compared to the Control group, mean differences ranged from 7% to 41%.
Conclusion
Patients with healthy knees or early stage osteoarthritis have higher quadriceps and hamstrings strengths than those with a more advanced stage of the disease, even after knee replacement. These findings suggest that the traditional rehabilitation programs do not recover strength to levels observed in individuals without knee osteoarthritis.
Keywords: Muscle strength; Arthroplasty, replacement, knee; Osteoarthritis
Resumo
Objetivo
Comparar a força muscular isocinética máxima dos músculos extensores e flexores do joelho entre pacientes com osteoartrite do joelho e pacientes submetidos à artroplastia total do joelho.
Métodos
Os voluntários foram divididos em cinco grupos (n = 20): Controle, Ahlbäck I e II; Ahlbäck IV; seis meses após artroplastia total do joelho; 12 meses após artroplastia total do joelho. O teste de força voluntária isocinética máxima foi feito para mensuração da força do quadríceps e isquiotibiais a 60/s.
Resultados
Foram achadas diferenças significativas entre o pico de torque do quadríceps e dos isquiotibiais (p < 0,001). Os grupos Ahlbäck IV, seis meses e 12 meses após cirurgia mostraram valores mais baixos quando comparados com os grupos controle e Ahlbäck I e II. Quando os valores percentuais foram comparados com o grupo Controle, as diferenças médias variaram de 7% a 41%.
Conclusão
Os pacientes com joelhos saudáveis ou osteoartrite em estágio inicial apresentaram maior força no quadríceps e nos isquiotibiais do que pacientes em estágio mais avançado da doença, mesmo após a ATJ. Esses achados sugerem que os programas tradicionais de reabilitação não recuperam a força nos níveis observados em indivíduos sem osteoartrite do joelho.
Palavras-chave: Força muscular, Artroplastia do joelho, Osteoartrite
Introduction
Knee osteoarthritis (OA) is the most common orthopedic disorder among the pathologies of this joint.1 OA clinical management is age-related; this condition has a major impact on function and independence, including limitations in locomotion and domestic tasks.2, 3, 4 Recent research associates the functional decline in OA with muscle weakness, particularly in the quadriceps and hamstrings.5, 6
In addition to physical exercise, pharmacological treatment and lifestyle changes are suggested as a conservative treatment for OA.7 As the disease progresses, with the reduced effect of the therapeutic interventions and the high impairment of the patient's functionality a total knee arthroplasty (TKA) is often considered as the best treatment option.8 Despite the fact that TKA decreases pain levels in patients with OA, the quadriceps and hamstring muscle strength deficits persist after surgery.9, 10, 11
Although the causes of quadriceps and hamstring weakness are unknown, the main causes appear to be disuse atrophy and activation deficits.12 Thus it has been observed that the main focus of attention regarding muscle strength deficit in OA and TKA is directed to quadriceps strength.13, 14 In turn, the interpretation of the importance of hamstrings in OA and TKA has not increased, despite the fact that, together with the quadriceps, the hamstrings provide the structural and functional stability of this joint.14 Understanding the magnitude of muscle strength in OA and TKA can help identify disease-modifying triggers and refine rehabilitation procedures to improve patients’ quality of life. Therefore, this study is aimed at comparing the maximal isokinetic muscle strength of the knee extensor and flexor muscles between patients with knee OA and those undergoing TKA, and to analyze the percentage alteration rate and the ratio of maximal isokinetic muscle strength between the knee extensors and flexors. The authors’ hypothesis was that the 12-month post-TKA group would present higher values of muscle strength than the other groups.
Material and methods
The sample consisted of patients attended to at the outpatient clinic of the Specialized Knee Surgery Care Center (Centro de Atenção Especializada em Cirurgia do Joelho [CAECJ]) of the National Institute of Traumatology and Orthopedics Jamil Haddad (Instituto Nacional de Traumatologia e Ortopedia Jamil Haddad [Into]). Table 1, Table 2, Table 3, Table 4, Table 5 describe the inclusion and exclusion criteria used for patient selection, as well as the composition of the following experimental groups (n = 20 in each): (1) asymptomatic individuals (control); (2) radiological diagnosis of OA – Ahlbäck grades I and II (OA-1/2); (3) radiological diagnosis of OA – Ahlbäck grade IV (OA-4); (4) six months after TKA (TKA-6); and (5) 12 months after TKA (TKA-12). All participants read and signed an Informed Consent Form in which the aims of the experiment and the evaluation conditions were described in detail. All procedures were previously approved by Into's Ethics Committee, in accordance with the Resolution of the National Health Council No. 466, of 12/12/2012.° Project registration number: CAAE 34971714.0.0000.5273.
Table 1.
Inclusion and exclusion criteria – Control group.
| Inclusion | Exclusion |
|---|---|
| With a medical record of muscular injuries in the lower limbs and articular injuries in the knees. |
Table 2.
Inclusion and exclusion criteria – OA-1/2 group.
| Inclusion | Exclusion |
|---|---|
| Ahlbäck grade I ou II | With a medical record of trauma |
| Infection or previous surgery in the studied joint | |
| Knee varus or valgus > 10° | |
| Previous surgery in the affected knee |
Table 3.
Inclusion and exclusion criteria – OA-4 group.
| Inclusion | Exclusion |
|---|---|
| Ahlbäck grade IV | With a medical record of trauma |
| Infection or previous surgery in the studied joint | |
| Knee varus or valgus > 10° | |
| Previous surgery in the affected knee |
Table 4.
Inclusion and exclusion criteria – TKA-6 group.
| Inclusion | Exclusion |
|---|---|
| Knee range of motion > 100° | Infection or previous surgery in the studied joint |
| 6 months post-operative | Muscle contracture with knee flexion > 15° |
| Rheumatic infections | |
| Severe osteoporosis | |
| Knee varus or valgus > 10° |
Table 5.
Inclusion and exclusion criteria – TKA-12 group.
| Inclusion | Exclusion |
|---|---|
| Knee range of motion > 100° | Infection or previous surgery in the studied joint |
| 12 months post-operative | Muscle contracture with knee flexion > 15° |
| Rheumatic infections | |
| Severe osteoporosis |
Ahlbäck radiological classification
Anteroposterior (AP) and lateral (P) view knee radiographs were obtained with monopedal support15; the ray was centered on the inferior pole of the patella, with 1 m tube-to-film distance. For the lateral view, the patient was placed in lateral decubitus on the side of the affected knee, which was flexed at 20°. The central ray was directed vertically to the medial side of the knee joint, with cephalic angulation of 5° and tube-to-film distance of 1 m. All radiographs were taken in the same radiology department during routine outpatient care; no other images were required just for the purpose of the study. The classification proposed by Ahlbäck,16 modified by Keyes et al.,17 was used to classify the degree of OA.
Maximum isokinetic voluntary strength
For muscle strength assessments, an isokinetic dynamometer (CSMI®, Humac Norm®, MA, United States) was used. All subjects were seated, with the lateral femoral condyle aligned with the dynamometer's rotational axis and the ankle attached to the rod of the knee evaluation assessment tool by a velcro strip. A concentric-concentric test was performed for knee extension and flexion, with a fixed velocity (60°/s) and five repetitions.18 Initially, the volunteers underwent a warm-up routine and familiarized themselves with the equipment and the isokinetic contraction, through repetitions at the same velocity used for the test. The highest instantaneous torque found for quadriceps (QUA) and hamstring (HAM) groups was considered the peak torque. Evaluations were performed only on the affected limb of each patient; for the control group, the dominant limb was assessed.
Statistical analysis
The analyses were initiated by normalizing the peak torque values by each participant's body weight. Subsequently, to analyze the proportionality of muscle strength, the HAM/QUA ratio values were calculated from the peak torque values of the QUA and HAM muscles. Thus, the dependent variables of the study were: (1) peak QUA torque, (2) peak HAM torque, and (3) HAM/QUA ratio. Demonstrative statistics (mean ± standard deviation) were used for data presentation. One-way ANOVA was calculated separately for group comparisons. Subsequently, Tukey's post hoc test was used to assess the differences between pairs. For all analyses, the significance level was set at p ≤ 0.05. In order to qualitatively analyze the rate of alteration, degradation, preservation, or growth of the QUA and HAM muscular strength, calculations were made to convert these values into percentage difference indices (Δ%). It is understood that Δ%, as the calculated index, has as reference the mean values of the extensor and flexor muscles of the control group 1.11 and 0.76 Nm kg−1, respectively (described in the results section) and calculated according to the formula presented below.
Results
To check the changes in muscle strength of the knee extensor and flexor muscles in OA patients who underwent TKA, 100 volunteers aged between 46 and 87 years (50 women and 50 men) were selected and divided into five experimental groups. All patients in the OA group underwent the same analgesic procedure; and the patients who underwent TKA followed the institutional protocol of physiotherapeutic rehabilitation to improve range of motion and strength. During the execution of strength evaluations, no patient complained of excessive pain and/or presented limitations during the isokinetic test. Table 6 presents the demographic data of the patients allotted to their respective groups.
Table 6.
Demographic data of the patients (mean ± SD).
| Control | OA-1/2 | OA-4 | TKA-6 | TKA-12 | |
|---|---|---|---|---|---|
| Men | 7 | 10 | 10 | 13 | 10 |
| Women | 13 | 10 | 10 | 7 | 10 |
| Age (years) | 67.9 ± 7.2 | 56.3 ± 5.4 | 66.1 ± 9.3 | 69.1 ± 7.0 | 65.8 ± 6.1 |
| Height (cm) | 156.8 ± 11.8 | 167.2 ± 9.2 | 165.7 ± 5.8 | 161.0 ± 6.9 | 164.7 ± 7.4 |
| Body weight (kg) | 70.5 ± 24.0 | 81.6 ± 12.6 | 78.2 ± 12.5 | 83.1 ± 15.7 | 78.9 ± 11.8 |
| BMI (kg/m2) | 28.3 ± 5.9 | 29.1 ± 2.9 | 25.2 ± 4.9 | 32.0 ± 5.2 | 26.2 ± 5.6 |
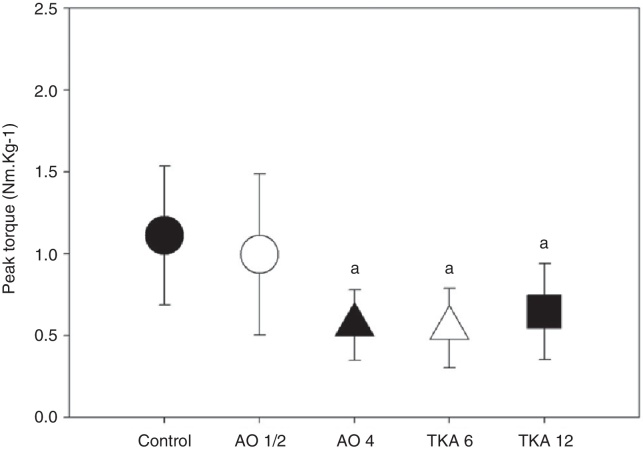
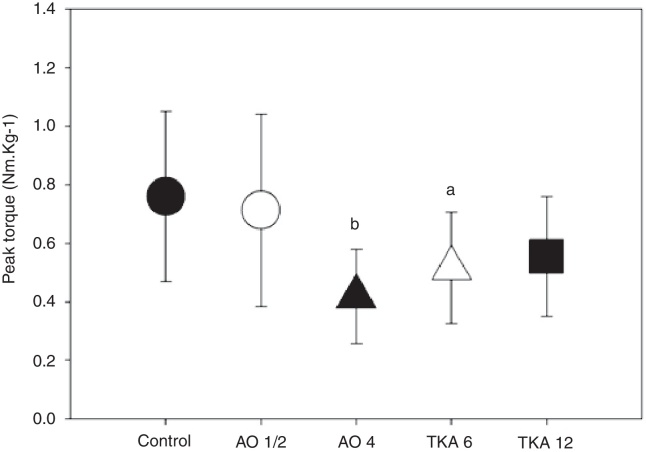
The peak QUA and HAM torque values are listed in Table 7 and represented graphically in Fig. 1, Fig. 2, Fig. 3. The variance analysis showed a significant difference for the extension strength (F = 11.15; p < 0.001), as well as for flexion (F = 6.75; p < 0.001).
Table 7.
Maximum isokinetic force at 60°/s of knee extensors and flexors (peak torque/body weight – Nm kg−1 and percentage difference of the control – mean ± SD).
| Groups | Quadriceps |
Hamstrings |
||
|---|---|---|---|---|
| Peak torque (Nm kg−1) | Δ% | Peak torque (Nm kg−1) | Δ% | |
| Control | 1.11 ± 0.47 | 0 | 0.76 ± 0.29 | 0 |
| OA-1/2 | 0.99 ± 0.49 | −11.0 | 0.71 ± 0.33 | −7.0 |
| OA-4 | 0.56 ± 0.22a | −50.0 | 0.42 ± 0.16b | −45.0 |
| TKA-6 | 0.54 ± 0.24a | −51.0 | 0.51 ± 0.19c | −33.0 |
| TKA-12 | 0.65 ± 0.29a | −41.0 | 0.55 ± 0.20 | −28.0 |
Significantly different from QUA control and QUA OA1/2 (p < 0.01).
Significantly different from HAM OA-1/2 and control (p < 0.001; both).
Significantly different from HAM control (p = 0.016).
Fig. 1.
Quadriceps peak torque – 60°/s in the knee (mean ± SD).
a Significantly different from control and OA-1/2 (p < 0.001). Black circle = control; white circle = AO 1/2; black triangle = AO 4; white triangle = TKA 6; and black square = TKA 12.
Fig. 2.
Hamstring peak torque – 60°/s in the knee (mean ± SD).
a Significantly different from control (p = 0.016). b Significantly different from control and AO-1/2 (p < 0.0001; both). Black circle = control; white circle = AO 1/2; black triangle = AO 4; white triangle = TKA 6; and black square = TKA 12.
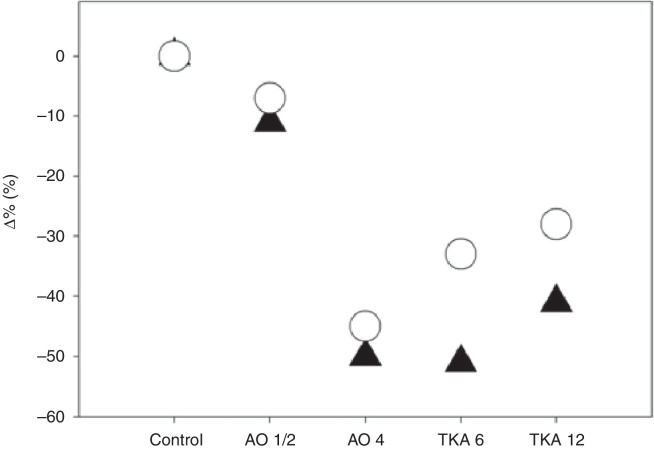
Fig. 3.
Percentage variation of QUA and HAM muscular force in the different stages of OA evolution and after TKA (mean).
In the OA-4, TKA-6, and TKA-12 groups, the peak QUA torque values were significantly lower than in the control and OA-1/2 groups (p < 0.001). The values observed in the OA-4, TKA-6, and TKA-12 groups were not different from each other; the same was found for the control and OA-1/2 groups. In the OA-4, TKA-6, and TKA-12 groups, the mean peak HAM torque values were lower than in the control and OA-1/2 groups.
The control group presented a significantly higher torque peak when compared with the OA-4 (p < 0.001) and TKA-6 groups (p = 0.016). The OA-1/2 group also presented a significantly higher value than that observed in the OA-4 group (p < 0.001). The values observed in the TKA-12 group were borderline significant when compared with those in the control group (p = 0.069). The same was observed when comparing the OA-1/2 and TKA-6 groups (p = 0.082).
Table 8 presents the HAM/QUA ratio values. ANOVA demonstrated a significant difference (F = 3.806 and p < 0.01). Post hoc analysis demonstrated that the OA-1/2 and TKA-6 groups were significantly different from the control group. The values observed in the TKA-12 group were borderline significant when compared with those in the OA-1/2 group (p = 0.07) and in the control group (p = 0.09).
Table 8.
HAM/QUA ratio at 60°/s in the knee (mean ± SD).
Significantly different from control (p < 0.001).
Discussion
Understanding changes in quadriceps and hamstring muscle strength in patients with OA and after TKA is important to improve treatment procedures in joint disease and after arthroplasty. Experiments measuring the strength of knee extensors have identified losses of around 50% in the preoperative phase and one month after TKA,19 which makes QUA muscle weakness a characteristic in patients with knee OA.5 The systematic review and meta-analysis by Øiestad et al.6 demonstrated that weakness of knee extensors is associated with the risk of developing OA. In this sense, this study observed knee extensor strength deficit in patients with OA Ahlbäck grade IV. In turn, the low disease severity presented by patients with Ahlbäck grades I-II knee OA was not enough to present a significant impact on QUA strength.
Despite some recommendations for HAM strength improvement in OA,5, 12, 20 few studies compared flexor strength in different stages of OA and TKA. Slemenda et al.21 failed to observe significant alterations in knee flexor strength in patients with Kellgren and Lawrence grades 2 or higher. In another study, also with patients with Kellgren and Lawrence grades 2 or higher, it was observed that the isometric torque of patients with OA was poor when compared with healthy controls (Cheing and Hui-Chan).22 The discrepancy between the studies by Slemenda et al.21 and Cheing and Hui-Chan22 should be attributed to the fact that between Kellgren and Lawrence grades 2 and 4, the impact of disease severity on muscle strength may be different. In the present study, flexor strength deficit was observed only in Ahlbäck grade IV.
When comparing results of patients with OA Ahlbäck grades I and II and grade IV, a possible inability to achieve normal patterns of muscular strength of patients in the last stage of the disease was observed in both extensor and flexor muscles of the knee. In OA Ahlbäck grades I-II, the decrease and obliteration of the joint space observed on the radiographs15, 23 were not sufficient to generate significant differences in the QUA and HAM strength when compared with a control group without these radiological changes.
The authors believe that the low performance in QUA and HAM strength in the group of patients with OA Ahlbäck grade IV is clinically important, since the integration of these muscle groups is associated with knee stability.2 In this relationship between agonists and antagonists, on one hand there are the QUA muscles, which are the primary extensor mechanism of the knee when walking, running, or other activities of daily living24 and on the other hand there are the HAM muscles, which, besides being the primary mechanism of knee flexion, they also protect the knee from eccentric contraction during the support phase, both to cushion the joint and to generate limb deceleration during gait.25 The QUA is the largest set of muscles that act on the knee joint, with great potential to produce and absorb the forces acting on that joint. Several clinical studies have demonstrated the development of QUA strength after an exercise program, showing pain reduction and improvements in functional abilities in cases of OA.26, 27 In turn, in the agonist and antagonist relationship, the HAM muscles have multiple roles in controlling knee flexion and hip extension, maintaining the stability of this set of joints during displacement tasks.12 Interventions through exercise in the HAM muscles have provided increased range of motion, greater muscle power and stability, with improved pain symptoms and functionality in patients with AO.5 Therefore, adequate functioning of knee extensors and flexors, not only isolated but in a united and integrated manner, is essential to provide dynamic stability for this joint.22
The relation between HAM and QUA strength has been reported in different studies.28, 29 The ratio of HAM/QUA isokinetic for healthy subjects has been established to range between 0.6 and 0.7 at an angular velocity of 60°/s.18, 28, 29 The mathematical ratio between the peak HAM and QUA torque observed in this study demonstrated that the control group followed the trend of the indexes expressed in the literature.28, 29 Recent studies of this ratio in OA patients show different values, due to QUA weakening.13, 20 In the present study, borderline values for the HAM/QUA ratio were observed in the OA-1-2 and OA-4 groups. The groups of patients who underwent TKA (TKA-6 and TKA-12) also showed values outside the normal range, with results close to 1, which demonstrate a high degradation of QUA strength. The present results demonstrate that there is a greater discrepancy in the HAM/QUA ratio in relation to the control group.
A mean reduction difference of 11% in extension force was observed between the control group and OA Ahlbäck grade I and II patients; in the Ahlbäck grade IV group, when compared to the control group, it was possible to observe an exacerbated drop of 50% in QUA strength. The HAM strength followed the same trend, with declines of 7% for Ahlbäck grades I and II, and 45% for grade IV. No significant differences in the proportion of strength decline between knee extensors and flexors was observed in this study. Both muscle groups weakened in the same proportion in patients with OA Ahlbäck grades I and II and Ahlbäck grade IV.
Despite the emphasis on rehabilitation procedures on muscle strength, OA patients with Ahlbäck grade IV may present inhibition of muscle activation, especially of the quadriceps.30, 31 QUA weakening and central activation failure are common in knee joint injuries.31 The persistent phenomenon of weakening and failure in the activation of knee extensors can be attributed to arthrogenic muscle inhibition, a continuous reflex inhibition of the muscle mass acting on an injured joint. This response is inherent to the joint; it is intended to protect it from further damage, discouraging the use of the injured joint, possibly to prevent painful movements.30, 31 This protective mechanism has a high cost, resulting in muscle weakness that often cannot be corrected in the rehabilitation process. Considering that the muscular strength performance of patients classified as Ahlbäck grade I and II did not present significant differences in relation to the control group, unlike the group of patients classified as Ahlbäck grade IV, it can be inferred that the degree of injury is related to the magnitude of the arthrogenic muscle inhibition. The fact that our study demonstrated that the hamstrings also show a reduction in strength in patients with Grade IV OA (Ahlbäck), in the same proportion as the quadriceps, suggests that the flexors of this joint also undergo a arthrogenic effect caused by OA.
When conservative treatment fails to alleviate OA symptoms, TKA becomes the therapeutic intervention of choice to improve debilitating pain and functional capacity.32 In the present study, it was observed that in patients who underwent TKA, knee extensor and flexor strength presented the same pattern identified in patients with Ahlbäck grade IV. The results of the study by Yoshida et al.33 indicated an inverse relationship, in which the strongest patients submitted to TKA tended to show lower QUA recruitment, with three months postoperatively. The altered neuromuscular patterns of the QUA and HAM during gait can influence the strength of the former after TKA.34 Patients who undergo unilateral TKA tend to unload the operated limb and shift the mechanical load to the contralateral limb joints, even one year after surgery.35 The likely asymmetry in QUA and HAM strength caused by the weakening of these muscle structures, which in the present study was identified for both OA and TKA groups, may play a role in asymmetric loading in TKA patients, as addressed by Alnahdi et al.35
Conclusion
Arthrogenic muscle inhibition prevents the rehabilitation of both QUA and HAM strength in this degenerative process between Ahlbäck grade IV of OA and 12 months after TKA. If activation and atrophy deficits are not specifically identified and corrected during rehabilitation interventions, they will tend to persist. In agreement with the literature that addresses the strength deficit in OA and TKA, the present findings indicate that traditional rehabilitation programs may not be enough to reverse QUA and HAM strength deficiencies.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at Instituto Nacional de Traumatologia e Ortopedia, Rio de Janeiro, RJ, Brazil.
References
- 1.Iwamoto J., Sato Y., Takeda T., Matsumoto H. Effectiveness of exercise for osteoarthritis of the knee: a review of the literature. World J Orthop. 2011;2(5):37–42. doi: 10.5312/wjo.v2.i5.37. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.Felson D., Niu J., Neogi T., Goggins J., Nevitt M.C., Roemer F. Synovitis and the risk of knee osteoarthritis: the MOST Study. Osteoarthr Cartil. 2016;24(3):458–464. doi: 10.1016/j.joca.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lastayo P.C., Meier W., Marcus R.L., Mizner R., Dibble L., Peters C. Reversing muscle and mobility deficits 1 to 4 years after TKA: a pilot study. Clin Orthop Relat Res. 2009;467(6):1493–1500. doi: 10.1007/s11999-009-0801-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitney J.C., Lord S.R., Close J.C. Streamlining assessment and intervention in a falls clinic using the Timed Up and Go Test and Physiological Profile Assessments. Age Ageing. 2005;34(6):567–571. doi: 10.1093/ageing/afi178. [DOI] [PubMed] [Google Scholar]
- 5.Al-Johani A.H., Kachanathu S.J., Ramadan Hafez A., Al-Ahaideb A., Algarni A.D., Meshari Alroumi A. Comparative study of hamstrings and quadriceps strengthening treatments in the management of knee osteoarthritis. J Phys Ther Sci. 2014;26(6):817–820. doi: 10.1589/jpts.26.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Øiestad B.E., Juhl C.B., Eitzen I., Thorlund J.B. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthr Cartil. 2015;23(2):171–177. doi: 10.1016/j.joca.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Uthman O.A., van der Windt D.A., Jordan J.L., Dziedzic K.S., Healey E.L., Peat G.M. Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. BMJ. 2014;48(21):1579. doi: 10.1136/bjsports-2014-5555rep. [DOI] [PubMed] [Google Scholar]
- 8.Cross W.W., Saleh K.J., Wilt T.J., Kane R.L. Agreement about indications for total knee arthroplasty. Clin Orthop Relat Res. 2006;(446):34–39. doi: 10.1097/01.blo.0000214436.49527.5e. [DOI] [PubMed] [Google Scholar]
- 9.Meier W., Mizner R., Marcus R., Dibble L., Peters C., Lastayo P.C. Total knee arthroplasty: muscle impairments, functional limitations, and recommended rehabilitation approaches. J Orthop Sports Phys Ther. 2008;38(5):246–256. doi: 10.2519/jospt.2008.2715. [DOI] [PubMed] [Google Scholar]
- 10.Singh J.A., Lewallen D.G. Time trends in the characteristics of patients undergoing primary total knee arthroplasty. Arthritis Care Res (Hoboken) 2014;66(6):897–906. doi: 10.1002/acr.22233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas A.C., Judd D.L., Davidson B.S., Eckhoff D.G., Stevens-Lapsley J.E. Quadriceps/hamstringss co-activation increases early after total knee arthroplasty. Knee. 2014;21(6):1115–1119. doi: 10.1016/j.knee.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hafez A.R., Al-Johani A.H., Zakaria A.R., Al-Ahaideb A., Buragadda S., Melam G.R. Treatment of knee osteoarthritis in relation to hamstrings and quadriceps strength. J Phys Ther Sci. 2013;25(11):1401–1405. doi: 10.1589/jpts.25.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adegoke B., Mordi E., Akinpelu O., Jaiyesimi A. Isotonic quadriceps-hamstrings strength ratios of patients with knee osteoarthritis and apparently healthy controls. Afr J Biomed Res. 2007;10:211–216. [Google Scholar]
- 14.Furu M., Ito H., Nishikawa T., Nankaku M., Kuriyama S., Ishikawa M. Quadriceps strength affects patient satisfaction after total knee arthroplasty. J Orthop Sci. 2015;21(1):38–43. doi: 10.1016/j.jos.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968;(Suppl. 277):7–72. [PubMed] [Google Scholar]
- 16.Ahlback S., Rydberg J. X-ray classification and examination technics in gonarthrosis. Läkartidningen. 1980;77(22):2091–2093. [PubMed] [Google Scholar]
- 17.Keyes G.W., Carr A.J., Miller R.K., Goodfellow J.W. The radiographic classification of medial gonarthrosis. Correlation with operation methods in 200 knees. Acta Orthop Scand. 1992;63(5):497–501. doi: 10.3109/17453679209154722. [DOI] [PubMed] [Google Scholar]
- 18.Dvirr Z. Manole; São Paulo: 2002. Isocinética: avaliações musculares, interpretações e aplicações clínicas. [Google Scholar]
- 19.Stevens J.E., Mizner R.L., Snyder-Mackler L. Quadriceps strength and volitional activation before and after total knee arthroplasty for osteoarthritis. J Orthop Res. 2003;21(5):775–779. doi: 10.1016/S0736-0266(03)00052-4. [DOI] [PubMed] [Google Scholar]
- 20.Hall K.D., Hayes K.W., Falconer J. Differential strength decline in patients with osteoarthritis of the knee: revision of a hypothesis. Arthritis Care Res. 1993;6(2):89–96. doi: 10.1002/art.1790060208. [DOI] [PubMed] [Google Scholar]
- 21.Slemenda C., Brandt K.D., Heilman D.K., Mazzuca S., Braunstein E.M., Katz B.P. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997;127(2):97–104. doi: 10.7326/0003-4819-127-2-199707150-00001. [DOI] [PubMed] [Google Scholar]
- 22.Cheing G.L., Hui-Chan C.W. The motor dysfunction of patients with knee osteoarthritis in a Chinese population. Arthritis Rheum. 2001;45(1):62–68. doi: 10.1002/1529-0131(200102)45:1<62::AID-ANR85>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 23.Hernández-Vaquero D., Fernández-Carreira J.M. Relationship between radiological grading and clinical status in knee osteoarthritis. A multicentric study. BMC Musculoskelet Disord. 2012;13(1):194. doi: 10.1186/1471-2474-13-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Earp J.E., Newton R.U., Cormie P., Blazevich A.J. The influence of loading intensity on muscle–tendon unit behavior during maximal knee extensor stretch shortening cycle exercise. Eur J Appl Physiol. 2014;114(1):59–69. doi: 10.1007/s00421-013-2744-2. [DOI] [PubMed] [Google Scholar]
- 25.Brandt K.D., Dieppe P., Radin E.L. Etiopathogenesis of osteoarthritis. Rheum Dis Clin North Am. 2008;34(3):531–559. doi: 10.1016/j.rdc.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 26.Pelland L., Brosseau L., Wells G., Macleay L., Lambert J., Lamothe C. Efficacy of strengthening exercises for osteoarthritis (part I): a meta-analysis. Phys Ther Rev. 2004;9(2):77–108. [Google Scholar]
- 27.Fransen M., Mcconnell S. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2008;(4):CD004376. doi: 10.1002/14651858.CD004376.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Wilk K.E., Romaniello W.T., Soscia S.M., Arrigo C.A., Andrews J. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;2(2):73–90. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]
- 29.Maly T., Zahálka F., Malá L. Isokinetic strength, ipsilateral and bilateral ratio of peak muscle torque in knee flexors and extensor in elite young soccer players. Acta Kinesiol. 2010;4(1):17–23. [Google Scholar]
- 30.Palmieri R.M., Ingersoll C.D., Edwards J.E., Hoffman M.A., Stone M.B., Babington J.P. Arthrogenic muscle inhibition is not present in the limb contralateral to a simulated knee joint effusion. Am J Phys Med Rehabil. 2003;82(12):910–916. doi: 10.1097/01.PHM.0000098045.04883.02. [DOI] [PubMed] [Google Scholar]
- 31.Rice D.A., Mcnair P.J., Lewis G.N., Dalbeth N. Quadriceps arthrogenic muscle inhibition: the effects of experimental knee joint effusion on motor cortex excitability. Arthritis Res Ther. 2014;16(6):502. doi: 10.1186/s13075-014-0502-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ibrahim S.A.R., Ghafar S., Salah M., Abo Alnas M., Al Misfer A., Farouk H. Surgical management of traumatic knee dislocation with posterolateral corner injury. Arthroscopy. 2013;29(4):733–741. doi: 10.1016/j.arthro.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 33.Yoshida Y., Mizner R.L., Ramsey D.K., Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech. 2008;23(3):320–328. doi: 10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoshioka Y., Siu D., Cooke T. The anatomy and functional axes of the femur. J Bone Jt Surg Am. 1987;69(6):873–880. [PubMed] [Google Scholar]
- 35.Alnahdi A.H., Zeni J.A., Snyder-Mackler L. Quadriceps strength asymmetry predicts loading asymmetry during sit-to-stand task in patients with unilateral total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(8):2587–2594. doi: 10.1007/s00167-015-3827-x. [DOI] [PubMed] [Google Scholar]