Abstract
Objectives
While digital health technologies hold potential for improving healthcare and the generation and dissemination of health information, there are many issues to be resolved in facilitating their provision and efficacy and ensuring ethical management of personal health data. In the face of high-stakes digital health initiatives, debates and controversies, eliciting the views and experiences of the diverse constituents in the digital health ecosystem is important.
Methods
A digital health stakeholder workshop was held in Canberra, Australia, to address two key questions: 1) What is currently working and not working in digital health? and 2) Where should digital health go in the future? As part of a living lab approach, the 25 workshop participants from research, industry, patient and other healthcare consumer groups and government, engaged in participatory design activities directed at stimulating ideas and discussion. The design artefacts and videos generated during the workshop were thematically analysed.
Results
Digital health technologies offer valuable ways for healthcare consumers, providers, community groups and health industries to create and share information about health, medicine and healthcare. However, members of some social groups are currently excluded from full participation in the digital health ecosystem. Mechanisms for facilitating further consultation between the various stakeholders involved in digital health, including patients and carers, need to be established. The rights and responsibilities of the different stakeholders involved in connected digital health also need to be better identified and highlighted. At the same time, personal data privacy and security need protection.
Conclusion
Establishing the effective and responsible delivery of digital health technologies and collection, protection and sharing of health data is highly complex. Infrastructure, ethical and social issues need to be considered.
Keywords: Design research, design sociology, digital health, health data, living lab, participatory design, stakeholders
Introduction
In recent years, much attention in the popular media and the medical, health services and public health literature has been devoted to the possibilities and potential of new digital health technologies.1,2 Digital devices and software have been developed to diagnose and treat illness and disease, facilitate the self-management of chronic diseases and help people monitor their bodily functions and activities. Digital technologies are increasingly used in medical training and education and for patients and other healthcare consumers to access, share and create health information. The digital data generated from devices and software provide opportunities to enhance knowledge and understanding about health, illness and disease, and improve medical diagnosis and care.
Like the citizens of other countries with high-level internet access and high smart device ownership and use, Australians are able to go online to seek health information from websites, join patient support communities, rank and rate healthcare professionals and make medical appointments. Australians are among the highest users of digital technologies globally: 88% own a smartphone, and the average Australian spends almost seven hours online per day.3 They can choose from the tens of thousands of health and medical apps available on the major app stores and purchase wearable devices to track their biometrics. Some Australians use medical devices to treat or self-manage health conditions or have access to telemedicine facilities. The Australian Department of Health is currently establishing My Health Record, aiming for a comprehensive national patient electronic medical record system, and working to encourage all Australians to sign up. It has also introduced the Health Care Homes model, in which patients with chronic health conditions will be encouraged to use digital at-home self-care, medical management and telemedicine technologies.
The digital health ecosystem is complex, involving actors and agencies from the general public, community and not-for-profit groups, health services, industry and government, often with different and sometimes conflicting or competing interests and agendas to pursue.1,2,4 There are numerous questions and issues to be resolved in facilitating the provision and efficacy of digital health, including use of and access to electronic medical records and patient portals by healthcare consumers and providers.5–7 Many telemedicine and telehealth technologies are still not adequately meeting patients’ and providers’ needs, often demanding invisible and unacknowledged labour to implement.8–10 Despite the vast array of health and medical apps available, only a very small number of them are actively used.11 Some health and medical apps are inaccurate, and could be potentially dangerous by providing incorrect medical diagnoses or the wrong medical advice.12–14
Access to and interest in using digital health technologies is also an important factor. In Australia, people with disabilities, indigenous people, older people, people living in rural areas and those with lower levels of education and employment and in low-income households are less digitally included than other groups.15,16 A market research survey of Australians found that while more than half had searched for health information online, only 15% were using a digital fitness tracker device.3 Another market survey found that only 8% of Australians had used telemedicine consultations, and most preferred in-person medical care.17
Managing the sensitive health information generated from digital health use is a further key issue requiring serious consideration. Many opportunities exist for digital health data to be leaked, hacked or breached at the time of transmission or storage, as they are often not adequately encrypted or otherwise protected.14,18,19 At the same time as Australians are being encouraged by government and industry agencies to use digital technologies for health and medical purposes, several controversies concerning the leaking, breach or government misuse of Australians’ personal data have received high public attention. These include reports in the news media from late 2016 that the government was using citizens’ social security and tax data to unfairly and inaccurately target welfare fraud (the so-called robo-debt fiasco) and media revelations in mid-2017 that details from Australians’ Medicare records were available for purchase on the ‘dark web’. Powerful lobby groups such as the Australian Privacy Foundation have raised concerns about the potential privacy risk to citizens posed by My Health Record.
In the face of these high-stakes digital health initiatives and associated debates and controversies, eliciting the views and experiences of the diverse constituents in the digital health ecosystem is important. In this article, I report on the findings of a digital health stakeholder workshop held in Canberra, Australia, in June 2017, convened by the Smart Technology Living Lab at the University of Canberra. As part of a living lab approach using participatory design methods, the workshop participants engaged in hands-on activities addressing two key questions: 1) What is currently working and not working in digital health in Australia? and 2) Where should digital health go in the future? Following an overview explaining the living labs approach and participatory design research methods, some examples of previous research using these methods to investigate digital health technologies are provided. I then outline the methods used in the digital health workshop and discuss its outcomes.
Background
The Smart Technology Living Lab was established to use social and design research methods to work on topics across a range of digital technologies. There are several interpretations of the term ‘living lab’ and no agreed definition, but they are usually characterised as a method of research or problem-solving that brings stakeholders together to generate or assess new ideas, products or solutions.20,21 The idea is to include the views of potential users, including citizens, industry, community and not-for-profit groups and government entities, when designing and planning solutions. This is often referred to as ‘co-creation’, ‘participatory design’, ‘co-design’ or ‘open innovation’.22,23 Living labs are therefore incubators for research, innovation and engagement. Depending on the approach, stakeholders can be informants (contributing understanding of users’ lives), testers (evaluating current solutions), contributors (collaborating with other stakeholders) and co-creators (of new solutions or ideas).21 The results and recommendations of living lab activities can be taken up by industry, government, community and policy agencies to improve goods and services or develop new ones.
Design research approaches involve developing an idea and creating a way of executing it, involving iterative processes of problem-solving and improvements.24 This approach has some similarities with action research or other participatory research methods. These methods include a focus on adopting an interventionist approach, including stakeholders in the research process as co-researchers and an emphasis on identifying problems.25 However, participatory design methods are somewhat different from these other methods in adopting an approach that invites end-users to create new ideas by engaging in creative activities that draw on design approaches and have more of a future-oriented perspective.26 In particular, participatory design activities work to generate new ways of thinking and experimentation that go beyond usual norms and assumptions, as well as mutual learning for all participants, including the researchers running the activities.27
Design research projects can range the spectrum from being mostly interested in the user experience for commercial and utilitarian purposes to a more cultural or critical social research approach. They can be used for commercial purposes to test new goods and services for industry or generate ideas for the development of future goods and services.20,28 In the ‘social living lab’ approach, they deal with social problems, activism and policy initiatives or seek to improve people’s lives as part of social innovation projects.29 As outlined by Kimbell and Julier,23 participatory design methods for social research tend to involve one or more of four key modes: exploring, making sense, proposing, and iterating. In the exploring mode, participants work to get a sense of the situation under investigation by taking a broad perspective. In the making sense mode, the participant group works towards defining specific issues, problems or questions that need addressing. The proposing mode involves generating and sharing new solutions or ideas that address the identified issues. The iterative phase is the process of testing ideas and exploring how they might work in practice. These modes are not linear, and may include going back to redevelop or refine ideas or solutions.
Most design research approaches involve participants engaging with design artefacts that are used to challenge standard ways of thinking and provoke new ideas.23,30 These artefacts may include making maps, scenarios, flow diagrams, stories, diaries, prototypes, videos, drawings, engaging in card sorting tasks, developing personas (user archetypes) and many other methods.
Social researchers interested in mundane practices can use participatory design research methods to identify how people incorporate objects or services into their everyday routines.26,31 Design researchers can also approach topics with a critical perspective. Participatory design methods can offer a way of identifying social problems and attempting to imagine alternative possibilities and futures rather than generating solutions.32 What has been termed ‘agonistic’ or ‘adversarial’ participatory design research has an explicitly social justice and activist agenda in identifying and challenging social inequities or injustices.33 If researchers wish to adopt a critical perspective, these processes can involve identifying the points of contention, anger or frustration that objects, systems or services may inspire, as well as their benefits and pleasures, and the ways in which socioeconomic disadvantage or marginalisation may affect access or even be exacerbated by these objects, systems or services.32,33
Design research methods have yet to make a significant impact in the social sciences.27 Using these methods for digital health topics is perhaps most well-established in the field of human computer interaction (HCI) studies, which has a tradition of adopting an end-user experience perspective and design approach. Examples of HCI research on digital health include using participatory design methods to explore the types of health indicators older people would like to track with digital devices,34 the development of a speech interface for people with speech difficulties35 and devising digital health technologies to address the needs of immigrant women.36 Some social researchers from other disciplines or working in multidisciplinary teams have used participatory design methods to address digital health topics. For example, Clemensen and colleagues25 used this approach to determine how people with diabetic foot ulcers could be treated effectively at home using telemedicine technologies. In another study, Wherton and colleagues37 conducted participatory design workshops with users of telehealth and telecare, their carers, service providers and technology suppliers. Another study38 involved people with diabetes and their families in co-creating ideas and prototypes for digital technologies to support everyday living with the disease.
In these studies, the primary objective was to identify the ways in which digital health technologies and services could be improved for end-users, focusing predominantly on specific patient groups and technologies. The digital health stakeholder workshop described in this article took a broader view on digital health. I was interested in eliciting the participants’ views and experiences of the range of digital health technologies they knew about or had used for either personal or professional purposes.
Methods
Potential participants for the stakeholder workshop were identified by using an online resource of community health groups and charities in Canberra, and drawing on my established contacts among researchers at the University of Canberra who were interested in digital health, and their own networks of professionals who worked in health-related government, professional associations or community or patient organisations. Most of these organisations were located in Canberra, which, as the Australian national capital, is home to many government departments and agencies and peak bodies. A list of potential participants was generated from these sources, and invitations were sent to them to be involved. Approximately half of all those invited agreed to attend the workshop. Ethics approval to conduct this project was granted by the University of Canberra Human Research Ethics Committee.
The workshop was directed at answering two key questions: What is currently working and not working in digital health in Australia? Where should digital health go in the future? Three hands-on participatory design activities were used to stimulate discussion and ideas relating to these key questions.
1. Current digital health landscape
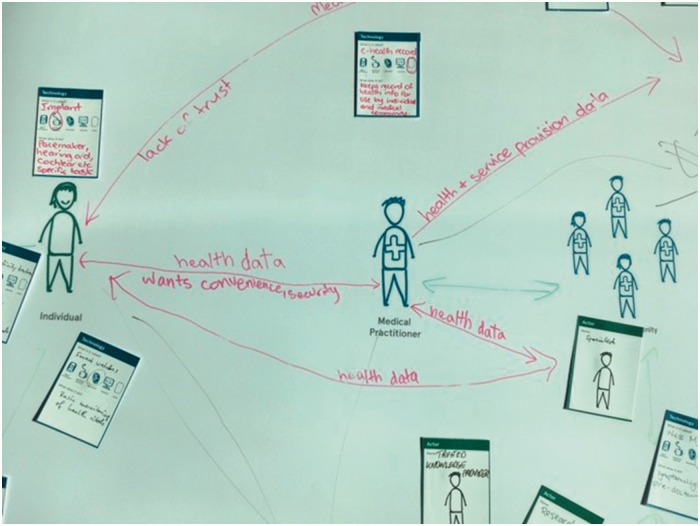
In this activity, participants worked in groups of 5–6 people to collaboratively map the technologies and social relationships contributing to the current digital health landscape. The point of this activity was to identify shared understandings in the group of what technologies are currently available and how they are embedded in social interactions and social groups.
Each group was provided with a large-scale laminated paper map template showing various actors in the digital health ecosystem. These included a patient and a medical practitioner at the centre of the map, with other potentially involved groups at either side: family and friends, the medical community, industry, and community and government organisations.
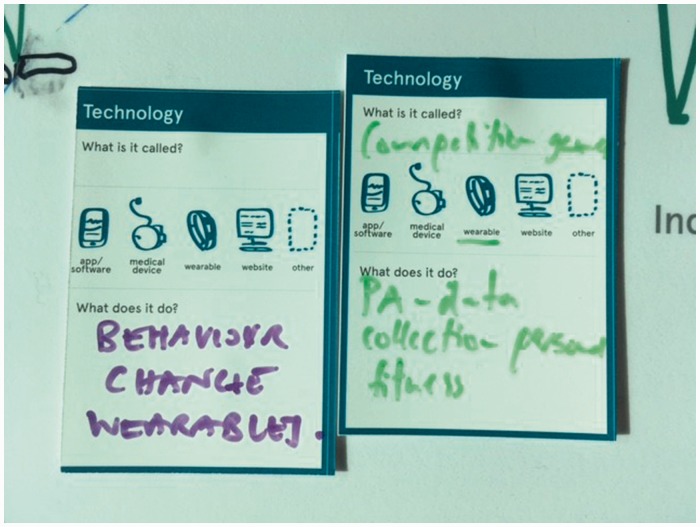
Participants were given a set of ‘technology’ cards to fill in the details of the kinds of digital technologies they wanted to place on the map, as well as actor cards to contribute additional people. The technology cards invited participants to fill in details such as the name of the technology, what kind of technology it was (app/software, medical device, wearable technology, website or other), and to provide a description of what it does. The participants were asked to fill in as many cards as they could in the time allowed, and to stick the cards on the map. They were also asked to draw on the map with pens to show the relationships between the human actors and the technologies. The groups then presented their map to the other groups, describing the details of the landscape they had created and explaining the advantages and disadvantages their group had identified in this landscape.
Figures 1 and 2 show details from two of the maps, including the completed technology and actor cards.
2. New digital health opportunities
Figure 1.
Detail from one of the digital health maps.
Figure 2.
Detail of cards used on the maps.
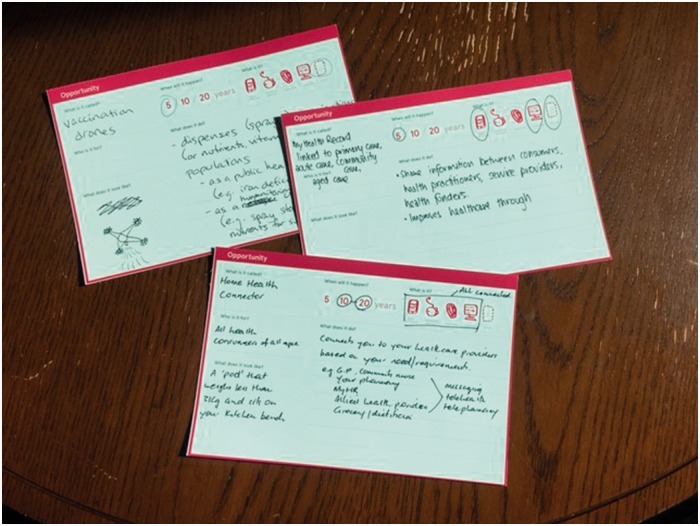
In this activity, participants were given ‘opportunity’ cards that invited them to identify new digital technologies for future use. The cards included questions that asked participants to fill in details about the name of this new technology, the time frame it was likely to take for this technology to emerge (five, 10 or 20 years), what type of technology it was, what it would be used for, what it would do and what it might look like. Figure 3 shows a group working on this task, while Figure 4 details some examples of completed cards.
3. Opportunity storyboards
Figure 3.
Participants working on the opportunities activity.
Figure 4.
Examples of the opportunities cards.
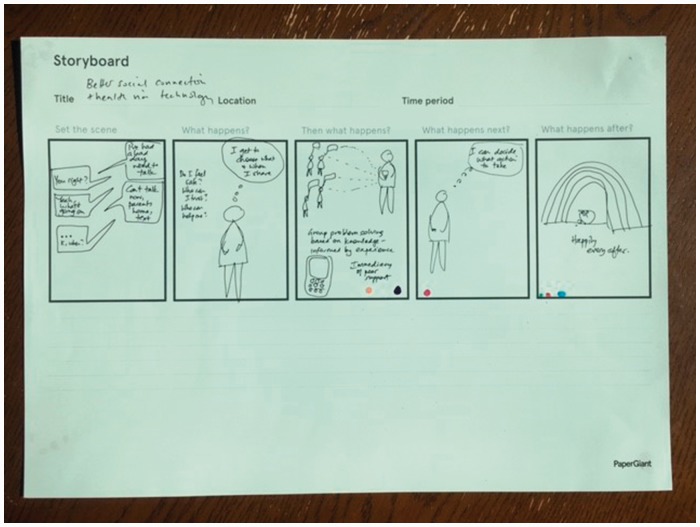
In the final activity, participants were given storyboard templates. They were asked to choose one of the new opportunities identified by the group, and work in pairs to create a narrative in which this technology was used. Five boxes were included in the storyboard, with the headings ‘Set the scene’, ‘What happens?’, ‘Then what happens?’, ‘What happens next?’ and ‘What happens after?’. The participants were asked to fill the boxes with simple drawings and provide some text below each box explaining what was happening. The purpose of this activity was to encourage participants to further consider how the new technologies they had invented would work in the context of end-users’ everyday lives. When they were completed, the storyboards were placed on the wall. As they helped themselves to the lunch that had been provided at this end-part of the workshop, participants were invited to move around the room viewing and discussing the other storyboards displayed on the wall.
Research materials analysis
The research materials that were analysed and discussed in this article include videos of the participants presenting one of the tasks to the group, and the design artefacts they created in responding to the tasks asked of them in the workshop’s activities. I commissioned a design research company to work with me in close consultation to develop the activities and materials that were used. Two members of the company ran the workshop and recorded it with photographs and a video camera. I attended the workshop as the convenor and observer, and greeted the participants individually as they arrived as well as making a welcome and introductory address to start the workshop. I spent the workshop time moving between the tables observing how the participants engaged in the tasks and listening to their comments.
I conducted all of the analysis of the materials. This involved viewing and transcribing the videos of participants’ presentations (each was about 3 min long), viewing other video documentation of the workshop and using the contents of the design artefacts that were created by the participants as evidence of their views and experiences concerning the present state of digital health and its future. All direct quotations presented below are from the presentations. The presentation transcripts and artefacts were thematically analysed using iterative comparisons between and across these materials. I paid close attention to the topics that were included in the presentations and artefacts, the words used to describe digital technologies and people’s use of them, the connections that were made between actors and devices in the maps, and the images employed in the storyboards. My observation of the workshop activities, including noticing how well the activities generated discussion in and between the participant groups and what kinds of issues they raised while working on the activities, also informed my analysis. I did not take field notes during the workshop, but used the documentary material generated (videos and photographs) as aide-memoires of the events.
Participant details
A total of 25 participants attended the workshop. Most participants (20) were from an Anglo-Celtic or northern European ethnic background. The five exceptions were all of Asian ethnicity. They ranged in age from 26 to 60 years, with four participants aged between 26 and 35, nine aged between 36 and 45, 11 aged between 46 and 55 and one aged 56 or older. The gender balance was equal, with 12 female and 13 male participants. The participants were a highly educated group (all had been educated at university level). They worked in research or health-related professional roles such as in government health agencies, health services provision, patient and healthcare consumer advocacy and community groups, healthcare provider, sporting or allied health associations, and urban planning and technology consultancies. At the workshop introduction, the participants were also asked to offer their perspectives as patients and carers themselves. In my observations of their discussions as they worked on the activities, I noted that insights based on their personal experiences as well as those from their professional work were often put forward.
Findings
Current digital health landscape
The five groups each created maps with many different technologies and relationships shown. The maps illustrate the complex relations between individual healthcare consumers and healthcare providers, social groups, organisations and the digital health technologies that are currently used in Australia. The technologies included across the five landscapes that were created are shown in Table 1.
Table 1.
Technologies shown on the digital health landscapes.
| apps and self-monitoring wearable devices such as Fitbits and smartwatches |
| fitness platforms like Strava |
| online search engines (e.g. Google Search) |
| online counselling services |
| medical implants and internal monitoring devices (e.g. pacemakers) |
| medical websites like WebMD |
| blogs |
| electronic health records and patient portals |
| online health surveys |
| health-related games |
| rehabilitation activities |
| online direct-to-consumer medical testing facilities |
| augmented reality technologies |
| social media |
| devices to promote mobility and safety |
| payment and health insurance systems |
| medical training and education software |
| online portals for registering healthcare providers |
| clinical diagnosis |
| prescription and decision-making software |
| messaging services |
| artificial intelligence |
| medical appointment and practice management software |
| telehealth technologies |
| crowdsourcing platforms for medical funding |
| video-sharing software |
| online communities for patient or carer support |
| online clinical terminology and healthcare identifiers services |
| ‘smart’ devices linked to each other as part of ‘smart cities’ and the Internet of Things |
| big data linkage and extraction software and national digital infrastructure |
In addition to the actors or groups already included on the map as involved in the digital health landscapes, participants added medical specialists, carers, government agencies, peak bodies, legislators and policy bodies, health advocates, researchers and academics, software and device vendors and entrepreneurs, advertising agencies and non-government organisations.
When each group presented their maps to the other groups and explained what they considered to be working or not working in contemporary digital health, several dominant topics emerged. These topics related to two key themes: infrastructural and organisational issues; and healthcare consumers’ rights and responsibilities. These are outlined below.
Infrastructural and organisational issues
All groups drew attention to issues concerning the digital infrastructure required to successfully implement health data collection and sharing. It was noted that some elements of the Australian health digital data collection and sharing system and infrastructure are working well.
What’s working is there’s some established mechanisms, like your interaction between community pharmacies and government on a transactional basis. So PBS [Pharmaceutical Benefits Scheme] online and those sorts of things are working (Group 4).
Australia has got off to a phenomenal beginning to get us to a point where we will just go in leaps and bounds beyond what other countries can do internationally, because we’ve established critical foundational pieces like the Healthcare Identifiers Service. The legislation that supports My Health Record is world-leading. We are well beyond a lot of other countries with respect to that (Group 2).
However, all groups observed that the accuracy and efficiency of collecting and sharing health and medical data across the health sector and with relevant actors such as government agencies, the digital technology industry and health researchers needs much more work.
Particularly with things like My Health Record and a lot of the other apps that people are having, is that they are only as good and as valuable as the data that’s being entered into it. So if people are having these fantastic My Health Records and it collects a lot of their medical data, it’s not necessarily collecting a lot of information about the specialist that they went and saw. So unless the specialist is writing a discharge summary or transfer summary, and uploading, and then their GP’s collecting it, and checking it out, reading it, and the patient’s having a look at it and making sure it is accurate, then it’s not necessarily being shifted from one person to another. Unless the hospital is uploading their discharge summary, and then the GP is collecting that from the device or the app in a timely fashion, then it’s not necessarily being used or valuable (Group 1).
That whole area of data access and interoperability and data linkage is holding us back as a country. You know, there are parts of Europe where they’ve got much better access to their data and use their data much more intelligently. We’re like 20, 50 years behind, and we obviously can’t access that data for research. And it’s frustrating that there’s so much data that’s collected administratively and routinely, but they’re all there siloed into different areas, and we can’t access it at the levels of aggregation that we would want (Group 4).
The groups noted that better solutions need to be devised to find ways for all relevant stakeholders to be able to input data into the electronic medical record system and for these data to be shared between healthcare consumers and providers.
There are a lot of allied healthcare practitioners and specialists, and particularly, the aged care sector, where the software is actually physically not present. So in order for them to connect with the national digital infrastructure, it’s obviously critically important that we can think of other ways that they can do that, through technology that might be in their pockets. Everyone’s carrying a pretty sophisticated piece of kit in their pockets. So we need to be cleverer about the way we can enable the community, consumers, but also the clinical community, who don’t necessarily have the power to invest in the technology that they see might be needed to get connected to things like the My Health Record system. We need to offer lots of options for people to get on (Group 2).
It was suggested that the government needs to work with industry, peak bodies and other agencies in developing solutions for developing and improving digital infrastructure for health data collection and sharing.
The peak bodies are important to work with the key government agencies and to work with the business community – the sector that’s actually developing these apps and technologies – and how they work within the system, within the framework, standards and with compliance and privacy and all that (Group 4).
Another topic that emerged in the participants’ maps and discussions referred to major organisational differences between government and industry, and how these influenced the speed at which new technologies could be developed and the nature of the technologies themselves. It was noted that the digital technology industry is able to work more quickly than government agencies in developing and promoting their products. Participants also drew attention to the ways in which industry could be more spontaneous and take risks, while government agencies needed to be more cautious and risk-aversive in achieving their objectives when introducing new digital technologies into healthcare, as they have a greater responsibility for accountability and protecting citizens’ wellbeing and privacy.
The business community is very good at putting things out there – at trying new things and seeing what the community picks up on and what they don’t, and what sells and what doesn’t. Government haven’t been quite so quick with that (Group 5).
[Commercial technology developers] are pushing accountability, responsibility and risk onto the consumer by accepting terms and conditions and absolving themselves of liability, whereas government doesn’t have that luxury to push responsibility as much onto medical practitioners as well as the individual (Group 2).
Healthcare consumers’ rights and responsibilities
The importance to patients of their relationships with healthcare providers and close family or friends was emphasised in the maps that the groups created. Digital health technologies were positioned both on the maps and in the participants’ discussions as ideally strengthening these relationships by enabling better communication, and the generation of knowledge about their health for individuals and for the healthcare system overall.
All groups observed that healthcare consumers should be able to share their health data with healthcare providers and chosen family members or carers. Patients also need to be able to access the health data collected about them by their healthcare providers.
If, for example, you’re looking at the individual, then the most important relationships would be with their immediate family and friends, and then their medical practitioner to share the data each way (Group 5).
Relationships that are probably most important are about having that caring support group of peers and family. So that for individuals who are perhaps more vulnerable, having those people around them who know the information that’s happening about them, and having access to some of that data and being able to share it … Patients are not necessarily having that capacity to feed the information back to their practitioners. And they’re also having that change in power about the access to the medical information that the practitioner has that they don’t necessarily have access to (Group 1).
It was noted in several groups that the ideal of the engaged patient that receives expression in digital health polices and promotion can be difficult to achieve in practice. One reason for this is that ‘empowered’ patients who are able to seek and share health information with each other pose a challenge and possible threat to the medical profession, allied bodies and government.
The relationship between the individual and their clinicians has changed quite dramatically, because there’s a lot more power to that patient and they collect a lot more data [about themselves] (Group 1).
What works about digital is the empowerment. And that’s what digital is all about. It’s about empowering people, no matter what industry you’re talking about. You’re seeing the medical establishment potentially threatened by having consumers empowered. And I think that’s the sort of challenge that digital is going to have, because that is going to play out over the coming years – this tension between what’s working on one side about empowering people (Group 3).
The topic of the privacy and security of citizens’ health and medical information was recognised as important in all groups. Participants asserted that healthcare consumers are becoming concerned about the privacy and security of their personal data and want the government to take the required steps to adequately protect their information.
People are more willing to trust – or are more ignorant of – sharing their data with the business community through apps and websites and stuff like that. But they seem to be more aware of the potential security risks of sharing their data with governments – say, with e-health records and things like that. And there’s a trust issue there that’s quite big. But it’s interesting that they are more willing to share all that info with the business community (Group 5).
New digital health opportunities
As shown in Table 2, 37 digital health opportunities were created. The participants presented ideas for a diverse range of new digital health opportunities they imagined could contribute to improving healthcare into the future. The ideas can be clustered around three major types of technologies: health services-oriented data integration; medical testing, diagnosis and treatment; and consumer-oriented health and medical information.
Table 2.
New digital health opportunities created by participants.
| Name and type of new technology | What it does | Time frame (years) |
|---|---|---|
| Health Services-Oriented Data Integration | ||
| Linked Health Data | For the research community and population health. Software that links health data across healthcare and social services such as the National Disability Insurance Scheme and aged care. Provides greater information for all to provide appropriate healthcare to connect communities. It will improve care provision and data integration and decrease silos. | 5 |
| My Health Record | Medical data software linked to primary care, acute care, community care, aged care. Used to share information between consumers, health practitioners, service providers, health funders. Improves healthcare. | 5 |
| National Digital Child Health Record (linked to My Health Record) | Unified and digitally accessible child health record. | 5 |
| Open API Interoperability Framework | For everyone. It connects all the technology in a way like Uber does with Google Maps with PayPal with calendar apps. | 5 |
| Vocal Documentation and Transmittal of Health Records | Software for clinicians. It looks like a microphone linked to Computerised Imaging Services (CIS). Codes using spoken language (natural language processing) and electronically stores via My Health Record. Eliminates need for manual entry of electronic health records (data). | 10 |
| Precision Medicine Digital Systems | Software to stratify healthcare – combines genomic and phenotypic information and individualises care. | 20 |
| Medical Testing, Diagnosis and Treatment | ||
| Balance Tester | Software for elderly, people after concussion. Includes smart home technologies and a smartphone app. Unobtrusively measures balance and gait parameters as people walk down the corridor (at home or in aged care facility) to access small changes over time that indicate an increased likelihood of a fall occurring. | 5 |
| Sleep Apnoea Device | Medical device for sleep apnoea suffers [sic] (and their partners). It does effectively what existing machines do but because of advances in technology, they will be less restrictive and terrifying. | 5 |
| Vaccination Drones | The drone dispenses (sprays) vaccinations (or nutrients, vitamins) on populations as a public health measure (e.g. iron deficiency) and as a humanitarian tool (e.g. spray starving people with nutrients for survival). | 5 |
| Dr Toilet | A smart toilet for everyone. It provides diagnostic data, at the individual or population level. Tracks ‘samples’ [human waste] and identifies indicators of conditions: i.e. bowel cancer, pregnancy, medication use/overuse etc. Feedback to users or government. | 5 |
| HD Ultrasound Scan | An app or wearable for 24/7 surveillance of baby in utero. Parents can see (and healthcare providers can monitor) baby’s health from conception to birth. | 10–20 |
| Wearable Diabetes Monitoring Device | For patients with diabetes. Generates data for blood glucose monitoring: e.g. contact lens. | 5 |
| Educated Lifestyle Assessment | For medical practitioners. Software and devices combine to provide information about people’s everyday life routines and assessment of their environment. Helps to assess state of health holistically (social determinants). Improves advice system for preventive health, | 5–10 |
| Apple Medical Service | For anybody using Apple technology: e.g. phones, other wearables, sensors and implants. Apple will establish a franchise of medical professionals, and people using Apple technologies have their health data collected and uploaded in real-time to Apple. Trends in their data are monitored, and specific changes generate alerts or acute changes are flagged for immediate action. | 20 |
| Life Length Predicator | Software to integrate information – genetic diagnostic, treatment and lifestyle – to predict life expectancy. By changing behaviours and community engagement, individuals can extend their life expectancy if they choose. | 10 |
| Personal (DNA) Medicine Proteomics Predictive | Allows self-diagnosis, prediction and prescription using DNA analysis and dynamic constant self-quantification. | 10 |
| Proactive Predictive Information | Used for decision-making about individual health. Not only provides information on likely outcomes but tracks and enables change using precision health. Consumer empowerment: removes uncertainty, opens up bounded rationality. | 5–10 |
| Nanites | For consumers. A medical device using nano-scale particles to facilitate the visibility of mechanisms (e.g. how cancer works), provides invasive procedures without bad side effects, and ongoing monitoring and modulation of bodily functions. | 20 |
| Enhancing Implants for Patients | Medical implant devices for people with disabilities/chronic conditions. They solve conditions such as neurological vision/hearing problems, epilepsy, Parkinson’s. They can relieve mental health symptoms: e.g. by triggering serotonin or inhibiting cortisol. They prompt healthy behaviours: e.g. exercise, controlling over-eating, sleep to prevent relapse. | 5–10 |
| Enhancing Implants for People in Good Health | Implants that enhance ability to perform physical or neurological tasks: e.g. triggering hormones in brain, forcing muscle activity etc. | 10–20 |
| Service Robots | Humanoid robots that provide services around the home, including detecting health indicators. | 20 |
| Modelling for Community Sports | Software for sports players and coaches. Helps them to work out ways to improve gameplay/not break rules, without injuring players or incurring penalties in the game. | 5 |
| Baby Transporter | Teleports baby out of pregnant woman safely, so she can give birth without pain (like in Star Trek). | |
| Energy Scanner | Wearable device that measures energy intake for weight loss or gain. Measures energy in a meal or food item by scanning it. Can also calculate nutrients and other nutritional information. | 10 |
| Consumer-Oriented Health and Medical Information | ||
| Health Professional Rater | Website for consumers to rate/grade health professionals and health facilities (like My Hospital but with better data thus more user friendly). Like Trip Advisor. It will improve consumer awareness and choice and patient outcomes and drive continuous healthcare improvement. | 5 |
| Personal Life Data Communicator | A wearable device that looks like something familiar – phone, watch, ear-piece, glasses, jewellery etc. It collects personal health data for logs stored in the cloud. Sends alert to doctor/family if risk to life: e.g. heart attack. Can log all health data so individual can choose to easily share with medical professionals or for health insurance refunds, pharmaceutical benefit scheme. | 5 |
| Care Navigator | App and website for consumers and carers. It will support consumers to make better decisions about access to care and treatment. It will provide an antidote to our complicated, fragmented systems across the public and private sector. Tracks our interactions with all health services, sends reminders, helps us maintain motivation and gives us confidence to act. Links our information from different providers. Tracks our medical observations and results. Like a GP on our desktop. | 10 |
| Safer Care | Website for consumers and carers. Provides data on clinical competence of registered health professionals: e.g. how many times they have performed the surgery, infection rates, complication rates and return to theatre, unplanned readmission etc., so consumers and carers can make more informed decisions about who they see and let operate on them. | 20 |
| Open Notes | Software for patients to provide them access to their health info in their clinicians’ records. It will empower patients and improve their understanding and adherence to treatments and potentially allow co-creation of clinical records between people and their care providers. | 5 |
| Push Health Prompts | Provides notifications to [sic] about their health and care to patients from mobile apps supported by My Health Record and clinical information systems. | 5–10 |
| Insights Through Data | A range of devices and software that can deliver insights through intuitive interfaces that lead to new behaviours related to health, e.g. reduces obesity or alcohol consumption. | 5 |
| Personal Blockchain | Used by consumers – allows them to control access to their own data, which is distributed across multiple systems. Controlled via your smartphone. Empowered individuals. As records created across the ecosystem an entry needs to be made to the personal blockchain. You then control who gets to see what. | 10 |
| Health Data Integrator | Capacity for IT systems to integrate data from a range of sources for monitoring health status. Health and health outcomes for the end user. | 5 |
| Integrate You | For consumers and medical professionals. It places all your medical stuff in one place so that it can be accessed and you don’t have to continue to share with everyone. Can only access areas specific to the condition: e.g. mental health records. | 10 |
| Digital Clone | A virtual reality device or software for patients. Stores all data generated by an individual – similar to the human brain. | 10 |
| Home Health Connector | For all health consumers. A ‘pod’ that weighs less than 3 kg and sits on your kitchen bench. Connects you to your healthcare providers based on your need/requirements (e.g. GP, community nurse, your pharmacy, My Health Record, allied health provider, grocery store, dietician). A messaging system that connects all devices and software used by the consumer. | 10–20 |
| Databot | A small device or software for patients. Fills in the gaps of data silos. Uses predictive technology based on partial data. Collects all conscious and unconscious data and links it to a larger system. | 10 |
The importance of making health data systems easy to operate, including the data entry and sharing functions was again prominent in these ideas for new digital health technologies. Several participants imagined current systems like My Health Record working better than they do currently. The ‘Linked Health Data’ proposal included the following features:
For the research community and population health. Software that links health data across healthcare and social services such as the National Disability Insurance Scheme and aged care. Provides greater information for all to provide appropriate healthcare to connect communities. It will improve care provision and data integration and decrease silos.
Others proposed new technologies that could be developed to facilitate entering health data. One example is the ‘Vocal Documentation and Transmittal of Health Records’ technology. This was described as:
Software for clinicians. It looks like a microphone linked to CIS [computerised imaging services]. Codes using spoken language (natural language processing) and electronically stores via My Health Record. Eliminates need for manual entry of electronic health records (data).
Some people created ideas for new devices that could contribute to preventive health and diagnosis as well as treatment efforts. These included a better sleep apnoea machine, a ‘smart’ toilet that could use human waste to test for disease, various types of monitoring devices that could be worn on or implanted in the body, and robots for offering healthcare and diagnostics. The ‘Balance Tester’, for example, was described as:
Software for elderly, people after concussion. Includes smart home technologies and a smartphone app. Unobtrusively measures balance and gait parameters as people walk down the corridor (at home or in aged care facility) to access small changes over time that indicate an increased likelihood of a fall occurring.
More speculative ideas included the ‘Vaccination Drones’:
The drone dispenses (sprays) vaccinations (or nutrients, vitamins) on populations as a public health measure (e.g. iron deficiency) and as a humanitarian tool (e.g. spray starving people with nutrients for survival).
‘Dr Toilet’:
A smart toilet for everyone. It provides diagnostic data, at the individual or population level. Tracks ‘samples’ [human waste] and identifies indicators of conditions: i.e. bowel cancer, pregnancy, medication use/overuse etc. Feedback to users or government.
‘Nanites’:
For consumers. A medical device using nano-scale particles to facilitate the visibility of mechanisms (e.g. how cancer works), provides invasive procedures without bad side effects and ongoing monitoring and modulation of bodily functions.
Other people imagined devices that enabled healthcare consumers to have better access to information. These included platforms for patients to rank and rate providers or view details relating to their competence. One example is the ‘Health Professional Rater’:
Website for consumers to rate/grade health professionals and health facilities (like My Hospital but with better data thus more user friendly). Like Trip Advisor. It will improve consumer awareness and choice and patient outcomes and drive continuous healthcare improvement.
There were also several suggestions for devices that healthcare consumers could use to generate or access health information about themselves. The ‘Home Health Connector’ was a device for this purpose:
For all health consumers. A ‘pod’ that weighs less than 3 kg and sits on your kitchen bench. Connects you to your healthcare providers based on your need/requirements (e.g. GP, community nurse, your pharmacy, My Health Record, allied health provider, grocery store, dietician). A messaging system that connects all devices and software used by the consumer.
The ‘Digital Clone’ was even more imaginative, described as ‘A virtual reality device or software for patients. Stores all data generated by an individual – similar to the human brain’.
Here again, the ideas presented in this future-facing activity demonstrated the value the participants placed on developing a health digital data system that is interoperable and allows access from all relevant parties, including healthcare consumers. Participants could imagine several possibilities for digital technologies to improve health and medical diagnosis and care and prevent illness and disease. They developed ideas for facilitating patient access to their personal health data, but also to information about health services and providers, so that they could make informed decisions.
Opportunity storyboards
Eleven storyboards were created by the group. The ideas presented in the storyboards are displayed in Table 3.
Table 3.
Storyboard narratives.
| Home Health Connector. ‘Mrs Smith, aged 75, with co-morbidities, has come to the end of her prescription and repeats of medication and needs to see her GP for a new script. She is alerted by the device. Mrs Smith uses the device to book telehealth consultation with GP. GP confirms appointment for 3 pm and calls Mrs Smith and conducts telehealth review of Mrs Smith’s conditions. GP writes a new script. Script is sent to Mrs Smith’s pharmacy where script is verified and filled at 4 pm. Pharmacist finds issue with potential drug interaction on one of Mrs Smith’s OTC [over-the-counter] meds. Contacts GP to resolve. GP and pharmacist resolve issue and a new script is written and re-sent to the pharmacy. Pharmacy delivers med to Mrs Smith’s home and refills dose administration and within device and also refills any other authorised repeat medications. All activity is then recorded and reconciled on Mrs Smith’s My Health Record. All other notifications for medication delivery are re-set. Confirmation message sent to Mrs Smith’s GP when the device has completed the tasks.’ |
| Supersize Me. The text in this storyboard was: ‘Born/pre-birth. Blood drawn. Genome sequenced and shared, stored. Predisposition, risk profile established. Get sick. Genome used (shared securely) for pharmacogenomic prescribing.’ [Problems are:] ‘Personalised pharmaceuticals facilitate complete decadence and hyper-indulgence. Gattaca?! Breaking the mind/body connection. White/worried/well.’ |
| Better Social Connection and Health Via Technology. No text was supplied with this storyboard – the narrative was conveyed by graphics and accompanying dialogue. These showed an individual dealing with a bad day and wanting to talk to someone to receive emotional support. The person considers who s/he might be able to trust and feel safe to talk to, but knows that ‘I get to choose what and when I share’. The person uses a smartphone to talk to peers, knowing that ‘I can decide what action to take’ based on their advice. The story ends with the person living ‘happily ever after’. |
| Nanites/Nanobots. The drawings show a cancer patient injected with nanites [robots at the nano scale], that then attack the cancer and stay in the body to attack any new cancers. Questions raised in the accompanying text included: ‘What is the energy source for these nanites? What if the nanites go rogue or become contagious? iRobot 2.0. Who develops the technology, injects them, and talks to the individual? Who is responsible for the maintenance/fixes? Who funds/pays for this expensive technology? How do we decide which cancers get treated by nanites? If you engage in risk behaviour, do you get excluded from access to this treatment?’. |
| Predict My Health. This storyboard included a diagram showing an end-user with implants and a wearable device, with data emanating from the devices, integrated and then returned to the user, as well as shared with healthcare providers. The text gave the following details: ‘Smart use of data. Connecting siloed health providers. Effective feedback on health issues. Wearables/implants/devices (smart) send data to central hub. Using predictive technology, they are monitored, analysed and distributed. Alerts and warning are delivered to the individual and health providers, [leading to] recommendations and appropriate action. Risks [include] security, privacy, misuse, non-use, excluded users, affordability. [Benefits include] preventive measures and healthy lifestyle and cost savings’. |
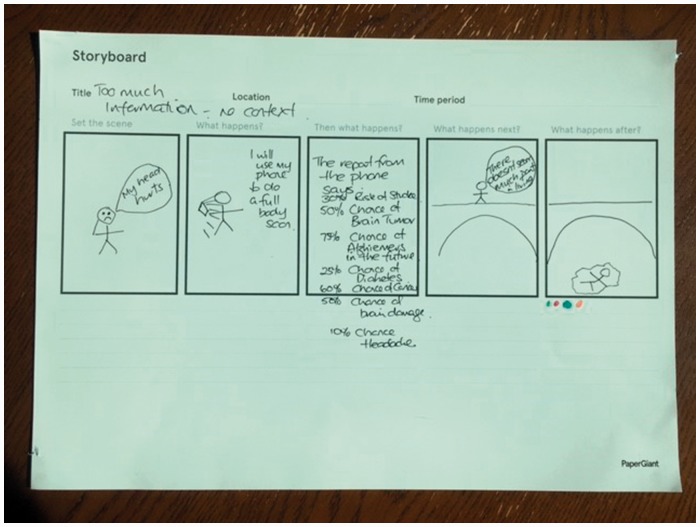
| Too Much Information. This storyboard showed a person whose head hurts. S/he uses a smartphone to conduct a ‘full body scan’. ‘The report from the phone says: 30% risk of stroke, 50% chance of brain tumour, 75% chance of Alzheimer’s in the future, 25% chance of diabetes, 60% chance of cancer, 50% chance of brain damage, 10% chance of headache.’ This person decides that ‘There doesn’t seem much point in living’, and commits suicide by leaping off a bridge. |
| Dr Toilet. In this storyboard, the ‘smart’ toilet idea is used. The graphics show a man with a stomach ache. The man visits the toilet and receives a message on his smartphone: ‘Go see your doctor soon. Love, Dr Toilet.’ He visits his GP, who already has received his test results and is ready to discuss them with the man. |
| Companion Robots. The idea of the companion robot is included in a narrative. The robot is shown interacting with an elderly person in the home, performing cleaning duties and sending health data to other parties. A medical problem is detected and the person is taken by ambulance to hospital. Benefits identified are a ‘focus on elderly, keep at home for as long as possible, quality of life, social interactions, sensing health states – raising alarm, providing services’. |
| Personal Health Assistant. This storyboard details how a personal health-monitoring device used on a smartphone or smartwatch can be used. The images show the device monitoring the user’s blood pressure, weight, physical activities and blood glucose levels, sending the data to My Health Record and hospital CIS [Clinical Information System]. The user receives notifications about the preventive actions they should be taking and lives to 101 years. The accompanying text provides further details: ‘Selection of health/wellness inputs enabled by the IoT [Internet of Things]. Devices, wearables are contributing big data about your health, shopping, lifestyle, work/attendance, genomic info. The information is combined with datasets held with your permission, e.g. My Health Record, hospital CIS and community that you access/control. The personal health assistant integrates and analyses your information – AI, machine learning. Presents information to you tailored to the areas of interest to you and prompts for care of existing health conditions and preventive care. Medicines/treatment, shopping, activity/exercise. Healthier, happier lives. Regulatory framework – who owns [the data], who ensures safety and quality?’. |
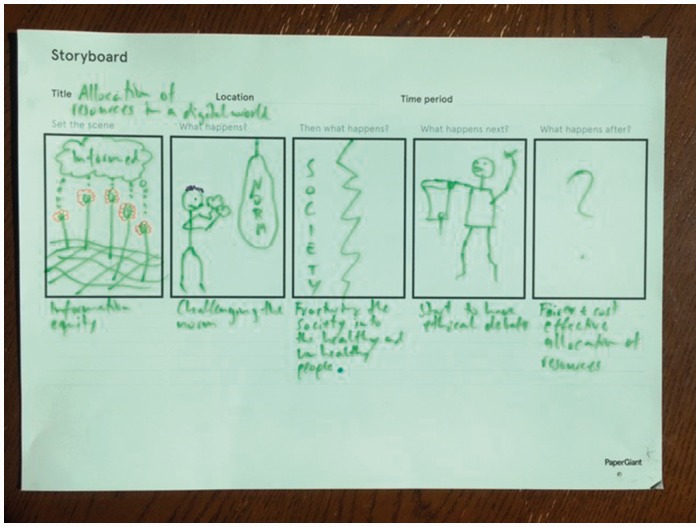
| Allocation of Resources in a Digitised World. In this storyboard, issues of ‘information equity’ are raised. A person is shown ‘challenging the norm’ (wearing boxing gloves ready to strike a punching bag labelled ‘Norms’) and society is shown as being divided into ‘the healthy and unhealthy people’. This leads to an ‘ethical debate’ in which questions are raised relating to ‘fair and cost-effective allocation of resources’. |
| Monitoring Pregnancy. A digital device for monitoring pregnancy is shown in this storyboard. The text explains: ‘Women at home, universal extension of what is already happening – monitoring and surveillance. Gets rapid support and early intervention from midwife. Becomes pre-occupied with machine rather than with baby. Anxiety/stress, hypervigilance. Medicalised, technologized, disconnected from own body.’ |
The narratives developed by the participants again drew attention to both the potential benefits offered by digital health and the harms and risks that can be involved. The benefits identified in these stories included opportunities to deal with mental distress by receiving support from peers, having individualised medical assessments conducted, filling prescriptions more easily, curing cancer and receiving information to assist preventive health efforts and to live to a happy and healthy old age.
For example, one pair called their story ‘Better Social Connection and Health via Technology’ (see Figure 5). No text was supplied with this storyboard – the narrative was conveyed by graphics and accompanying dialogue. These showed an individual dealing with a bad day and wanting to talk to someone to receive emotional support. The person considers who s/he might be able to trust and feels safe to talk to, but knows that ‘I get to choose what and when I share’. The person uses a smartphone to talk to peers, knowing that ‘I can decide what action to take’ based on their advice. The story ends with the person living ‘happily ever after’. Another pair presented a story entitled ‘Companion Robots’ (Figure 6). The idea of the companion robot is included in a narrative. The robot is shown interacting with an elderly person in the home, performing cleaning duties and sending health data to other parties. A medical problem is detected and the person is taken by ambulance to hospital. Benefits identified are a ‘focus on elderly, keep at home for as long as possible, quality of life, social interactions, sensing health states – raising alarm, providing services’.
Figure 5.
‘Better Social Connection and Health via Technology’ storyboard.
Figure 6.
‘Companion Robots’ storyboard.
However, some of the stories raised questions of whether too much information about their health delivered to patients could make them complacent – or conversely, demoralise or depress them, or divert attention from their own knowledge of their bodies. This narrative was particularly evident in the story entitled ‘Too Much Information’ (Figure 7). This storyboard showed a person whose head hurts. S/he uses a smartphone to conduct a ‘full body scan’. ‘The report from the phone says: 30% risk of stroke, 50% chance of brain tumour, 75% chance of Alzheimer’s in the future, 25% chance of diabetes, 60% chance of cancer, 50% chance of brain damage, 10% chance of headache’. This person decides that ‘There doesn’t seem much point in living’, and commits suicide by leaping off a bridge.
Figure 7.
‘Too Much Information’ storyboard.
Issues of the costs of offering the technologies, their maintenance, which conditions might be appropriate to treat with them, who might be excluded from access to new technologies or which social groups might be privileged over others were included in some narratives. For example, in the story entitled ‘Allocation of Resources in a Digitised World’, issues of ‘information equity’ are raised (Figure 8). A person is shown ‘challenging the norm’ (wearing boxing gloves ready to strike a punching bag labelled ‘Norms’), and society is shown as being divided into ‘the healthy and unhealthy people’. This leads to an ‘ethical debate’, in which questions are raised relating to ‘fair and cost-effective allocation of resources’.
Figure 8.
‘Allocation of Resources in a Digital World’ storyboard.
Discussion
The digital health stakeholder workshop provided an opportunity for a diverse range of stakeholders interested in digital health to come together and co-create ideas about what is and is not working in current digital health and where the future lies. It was acknowledged by the workshop members that digital health technologies offer potentially valuable ways for patients and other healthcare consumers, healthcare providers, community groups and health industries to create and share information about health, medicine and healthcare. These technologies can effectively provide information, support and social networks for consumers and improve healthcare access and delivery. However, they also pointed out that ethical and social issues need to be further considered, including whether some individuals or social groups might be stigmatised by a focus on self-management of health. The participants noted that some social groups, including both healthcare consumers and healthcare providers, are currently excluded from full participation in the digital health ecosystem, due to lack of necessary infrastructure, social disadvantage or economic factors, their health status, lack of skills or interest, or because their needs are not adequately recognised.
Workshop participants identified numerous ways in which the health data generated by digital technologies are potentially valuable to all stakeholders, albeit in different ways. They argued that while Australia is leading the way in some respects in terms of developing the legislation, digital infrastructure and systems required, there is much still to be accomplished. Mechanisms for facilitating further consultation between the various stakeholders involved in digital health, including patients and carers, need to be established, so that their needs and interests can be incorporated into future policy development and planning. Participants emphasised that it is important to find an effective and ethical way to connect health data with all involved stakeholders. Siloed data should be better shared across sectors and parties. At the same time, personal data privacy and security need protection. Patients and other healthcare consumers need to be able to invest their trust in government and other stakeholders to protect their health data.
Another key finding of the workshop was the idea that the rights and responsibilities of the different stakeholders involved in connected digital health should be better identified and highlighted. It was noted across the participant groups and activities that despite the ideal of the engaged and empowered patient that frequently is espoused in policy and healthcare services literature, their rights are often marginalised or neglected in government’s or industry’s attempts to introduce new digital health solutions. An important distinction was made between commercial developers of new digital health technologies and government agencies. It was pointed out that government must be much more risk-averse and cautious when introducing digital health technologies so that it meets its duty of care to its citizens. It needs to play a central role in ensuring the digital health data are efficiently and effectively generated and archived, and in protecting its citizens’ data. Industry is often able to act more quickly in bringing new technologies to market, but the commercial imperatives that drive industry innovation can mean that it sometimes abrogates its responsibilities to consumers.
The participants focused for the large part on issues relating to diagnosis, testing and medical care technologies, medical and self-monitoring apps and devices, electronic health records and the digital data all these technologies generate. The ways in which online discussion forums, websites and social media (e.g. Facebook, Twitter, Instagram and YouTube) provide opportunities for patients and other stakeholders to create and share health information and health-related experiences received far less attention. There was also very little specific mention or discussion of the digital health needs of unpaid carers and marginalised groups such as people who identify as LGBQTI or as indigenous Australians, or those from culturally and ethnically diverse communities.
Other aspects that did not attract detailed discussion were: the socioeconomic determinants of digital health use in Australia for healthcare consumers, healthcare providers and other stakeholders; the value different stakeholder groups attribute to health data and how they use the data; how different needs and values should be balanced across the digital health ecosystem; the role of online discussion forums, websites and social media in creating and sharing health information and health experiences for and between stakeholders in the context of the broader digital health ecosystem; issues of access to healthcare consumers’ personal health data, and how this is facilitated; and the protection of security of personal health data and consumers’ privacy. These are all areas on which future research should focus.
Conclusion
As an initial living lab approach to identifying broad current and future trends in and uses of digital health in Australia, this workshop was productive in generating many important ideas and stimulating discussion. As such, it involved co-creation activities concerning the exploring and making sense modes of participatory design research rather than developing or testing solutions. The findings offer recommendations that can be taken forward into planning and policy for digital health. Future research using participatory design methods could usefully focus more closely on the issues identified in the workshop by bringing more specific and targeted stakeholder groups into the conversation, and building on this preliminary work by beginning to formulate more specific solutions to some of the ‘wicked’ problems identified in the workshop.
Acknowledgements
The Paper Giant design research company, as consultants with DL, devised the design research activities used in the workshop and ran the workshop activities.
Contributorship
DL is the sole author of the manuscript. She performed all the analysis of the research material and the writing of the manuscript.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
Ethics approval to conduct this project was granted by the University of Canberra Human Research Ethics Committee (reference number HREC 17-92). Participants gave written consent for photographs to be taken and published of them participating in the workshop and for video-taping parts of the workshop as a way of recording their discussions.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by internal research funds awarded to DL by the University of Canberra as part of her research professor appointment.
Guarantor
DL.
Peer review
This manuscript was reviewed by Joseph Wherton, University of Oxford, UK and Chrysanthi Papoutsi, University of Oxford, UK.
References
- 1.Lupton D. Digital health: Critical and cross-disciplinary perspectives, London: Routledge, 2017. [Google Scholar]
- 2.Powell J, Newhouse N, Boylan A-M, et al. Digital health citizens and the future of the NHS. Digital Health 2, http://journals.sagepub.com/doi/full/10.1177/2055207616672033 (2016, accessed 31 August 2017).
- 3.EY Sweeney. Digital Australia: State of the nation. The 2017 edition, https://digitalaustralia.ey.com (2017, accessed 21 August 2017).
- 4.Hendy J, Chrysanthaki T, Barlow J, et al. An organisational analysis of the implementation of telecare and telehealth: the whole systems demonstrator. BMC Health Services Research 12, http://dx.doi.org/10.1186/1472-6963-12-403 (2012, accessed 31 August 2017).
- 5.Greenhalgh T, Hinder S, Stramer K, et al. Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. BMJ 341, http://www.bmj.com/content/341/bmj.c5814 (2010, accessed 12 July 2017).
- 6.Sarkar U, Karter AJ, Liu JY, et al. The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system—results from the Diabetes Study of Northern California (DISTANCE). J Health Commun 2010; 15: 183–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mort M, Smith A. Beyond information: intimate relations in sociotechnical practice. Sociology 2009; 43: 215–231. [Google Scholar]
- 8.Edwards L, Thomas C, Gregory A, et al. Are people with chronic diseases interested in using telehealth? A cross-sectional postal survey. J Med Internet Res 2014; 16: e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenhalgh T, Wherton J, Sugarhood P, et al. What matters to older people with assisted living needs? A phenomenological analysis of the use and non-use of telehealth and telecare. Soc Sci Med 2013; 93: 86–94. [DOI] [PubMed] [Google Scholar]
- 10.Procter R, Wherton J, Greenhalgh T, et al. Telecare call centre work and ageing in place. CSCW 2016; 25: 79–105. [Google Scholar]
- 11.IMS Institute for Healthcare Informatics. Patient adoption of mHealth: use, evidence and remaining barriers to mainstream acceptance, Parsipanny, NJ: IMS Institute for Healthcare Informatics, 2015. [Google Scholar]
- 12.van Velthoven M and Powell J. Do health apps need endorsement? Challenges for giving advice about which health apps are safe and effective to use. Digital Health 3, http://dx.doi.org/10.1177/2055207617701342 (2017, accessed 31 August 2017).
- 13.Jutel A and Lupton D. Digitizing diagnosis: a review of mobile applications in the diagnostic process. Diagnosis 2, https://www.degruyter.com/view/j/dx.2015.2.issue-2/dx-2014-0068/dx-2014-0068.xml (2015, accessed 2 December 2015).
- 14.Wicks P and Chiauzzi E. ‘Trust but verify' – five approaches to ensure safe medical apps. BMC Medicine 13, http://www.biomedcentral.com/1741-7015/13/205 (2015, accessed 8 October 2015).
- 15.Thomas J, Barraket J, Wilson C, et al. Measuring Australia's digital divide: the Australian Digital Inclusion Index, Melbourne: RMIT University, for Telstra, 2017. [Google Scholar]
- 16.Baum F, Newman L, Biedrzycki K. Vicious cycles: digital technologies and determinants of health in Australia. Health Promot Int 2014; 29: 349–360. [DOI] [PubMed] [Google Scholar]
- 17.Accenture Consulting. Accenture 2016 Consumer Survey on Patient Engagement, Accenture Consulting, 2016. [Google Scholar]
- 18.Ali M, Khan SU, Vasilakos AV. Security in cloud computing: opportunities and challenges. Inform Sciences 2015; 305: 357–383. [Google Scholar]
- 19.Thilakanathan D, Chen S, Nepal S, et al. A platform for secure monitoring and sharing of generic health data in the Cloud. Future Gener Comp Sy 2014; 35: 102–113. [Google Scholar]
- 20.Bergvall-Kareborn B, Stahlbrost A. Living Lab: an open and citizen-centric approach for innovation. IJIRD 2009; 1: 356–370. [Google Scholar]
- 21.Leminen S, Nyström A-G, Westerlund M. A typology of creative consumers in living labs. J Eng Technol Manage 2015; 37: 6–20. [Google Scholar]
- 22.Bjögvinsson E, Ehn P, Hillgren P-A. Design things and design thinking: contemporary participatory design challenges. Des Issues 2012; 28: 101–116. [Google Scholar]
- 23.Kimbell L, Julier J. The social design methods menu, London: Fieldstudio Ltd, 2012. [Google Scholar]
- 24.Bergman M, Lyytinen K, Mark G. Boundary objects in design: an ecological view of design artifacts. J Assoc Inf Syst 2007; 8: 546–568. [Google Scholar]
- 25.Clemensen J, Larsen SB, Kyng M, et al. Participatory design in health sciences: using cooperative experimental methods in developing health services and computer technology. Qual Health Res 2007; 17: 122–130. [DOI] [PubMed] [Google Scholar]
- 26.Kjærsgaard MG, Halse J, Smith RC, et al. Introduction: design anthropological futures. In: Smith RC, Vangkilde KT, Kjærsgaard MG, et al.(eds). Design anthropological futures, London: Bloomsbury Academic, 2016, pp. 1–18. [Google Scholar]
- 27.Lupton D. Towards design sociology. Sociol Compass 2017, forthcoming.
- 28.Veeckman C, Schuurman D, Leminen S, et al. Linking Living Lab characteristics and their outcomes: towards a conceptual framework. TIM Review 2013; 3: 6–15. [Google Scholar]
- 29.Dezuanni M, Foth M, Mallan K, et al. Social living labs for digital participation: designing with regional and rural communities. In: Companion to Designing Interactive Systems Conference 2016 Proceedings (DIS ‘16 Companion) Brisbane, Australia, 4–8 June 2016, pp.49–52. ACM.
- 30.Drazin A. The social life of concepts in design anthropology. In: Gunn W, Otto T, Smith RC. (eds). Design anthropology: theory and practice, London: Bloomsbury, 2013, pp. 33–50. [Google Scholar]
- 31.Kimbell L. Rethinking design thinking: Part I. Design and Culture 2011; 3: 285–306. [Google Scholar]
- 32.Kimbell L. Rethinking design thinking: Part II. Design and Culture 2012; 4: 129–148. [Google Scholar]
- 33.DiSalvo C. Adversarial design, Cambridge, MA: The MIT Press, 2012. [Google Scholar]
- 34.Davidson JL and Jensen C. What health topics older adults want to track: a participatory design study. In: Proceedings of the 15th International ACM SIGACCESS Conference on Computers and Accessibility Bellevue, US, 21–23 October 2013, pp.1–8. ACM.
- 35.Hamidi F, Baljko M, Ecomomopoulos C, et al. Co-designing a speech interface for people with dysarthria. J Assist Technol 2015; 9: 159–173. [Google Scholar]
- 36.Brown D, Ayo V and Grinter RE. Reflection through design: immigrant women’s self-reflection on managing health and wellness. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ‘14), Toronto, Canada, 26 April–1 May 2014, pp.1605–1614. ACM.
- 37.Wherton J, Sugarhood P, Procter R, et al. Co-production in practice: how people with assisted living needs can help design and evolve technologies and services. Implement Sci 2015; 10: 75 http://dx.doi.org/10.1186/s13012-015-0271-8 (2015, accessed 10 July 2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kanstrup AM, Bertelsen P, Nøhr C. Patient innovation: an analysis of patients’ designs of digital technology support for everyday living with diabetes. Health Inf Manag J 2015; 44: 12–20. [DOI] [PubMed] [Google Scholar]