Abstract
Objective
The objective of this study was to determine the feasibility of Facebook as a dissemination strategy for the People Getting a Grip on Arthritis self-management program by arthritis health professionals to their patients.
Methods
The feasibility study comprised a single arm, pre-post design that included a convenience sample of 78 arthritis health professionals across Canada. Assessments were performed at baseline, two-weeks post-intervention, and at three-months follow-up using online questionnaires. The primary outcome measure was change in perceived usability of Facebook as a dissemination strategy for the People Getting a Grip on Arthritis program with patients at two-weeks post-intervention using an instrument based on an extended version of the Technology Acceptance Model 2. Comparisons with baseline were assessed using t-test analyses.
Results
Statistically significant improvements from baseline were seen for all items of the Technology Acceptance Model 2 domains: perceived ease of use (four items), intention to use (two items) and output quality (two items) domains. Variable results were seen for the job relevance, perceived usefulness, voluntariness, and result demonstrability domains of the Technology Acceptance Model 2. There were no statistically significant improvements for the subjective norm and image domains.
Conclusions
Facebook may provide arthritis health professionals with an additional option of how to best share evidence-based information to allow their patients to successfully self-manage their arthritis.
Keywords: Social media, Facebook, osteoarthritis, rheumatoid arthritis, self-management, dissemination, evidence-based practice, clinical practice guidelines, patient education
Introduction
With an increasing aging Canadian population with chronic diseases such as arthritis,1 there is an urgent need for health professionals to promote evidence-based arthritis self-management support to their patients. As we continue to move towards a paradigm of patient and health professional partnerships for the collaborative care of chronic diseases involving self-management support, health professionals are complementing traditional patient education by providing patients with technical skills and information to identify problems, allowing them to make appropriate decisions, and take action to manage their conditions.2 Self-management support refers to the systematic provision by healthcare professionals to provide education, coaching, and other interventions to help patients gain confidence, knowledge, skills, and motivation to manage the physical, social, and emotional impacts of their disease.3 Self-management begins with patient education, the process of learning technical skills related to patients’ specific conditions.3 Self-management support can involve a variety of techniques including the creation of small actions plans and goal setting, providing personalized feedback, enlisting social support, and determining goal achievement.4
While the effective self-management of chronic diseases among patients continues to be essential in optimizing health outcomes, there is uncertainty as to how health professionals can enhance self-management support among their patients.5 Lack of time and resources have also been identified as barriers to the delivery of evidence-based patient education and behavior change counseling.6,7 Furthermore, ensuring that patients are willing and able to understand instructions can be challenging for health professionals.8 Increasing the use and discovering new methods of providing successful self-management support may facilitate patient education and help reduce the demand for more human health resources to care for chronic diseases.
Web 2.0 refers to the next generation of the Internet allowing individuals to share information and collaborate online.9 Web 2.0 technologies, such as social media, continue to rise in popularity, as they allow users to add or change content on the Web.10 eHealth interventions, which may include Web 2.0 technologies, provide health information from electronic resources10 and is defined by Health Canada as “the application of information and communication technologies within the health sector.”11 eHealth interventions and Web 2.0 technologies can enhance self-management support as they provide a time-saving and a potential demand-reducing option for health professionals,2,12,13 and have increasingly become more popular among chronic disease patients to access health information.12 Online chronic disease self-management interventions have shown to reach a broad population of chronically ill patients,13 and online communities have allowed for improved social support and knowledge acquisition.13,14 A systematic review by Stellefson et al.12 concluded that older adults with chronic disease may be associated with improvements in health behaviors and health status when using Web 2.0 self-management interventions. The increasing popularity of social media and social networking applications offers health professionals with a communication tool to share health education information with patients. Positive uses of social media among health professionals include disseminating accurate information to enhance education, countering inaccuracies, and engaging learners.15 With its capabilities to allow for multimedia-sharing such as disease management videos, podcasts, and wikis, social media has shown to be successful in public health promotion and advocacy,16 disseminating evidence-based health information,17 responding to public concerns during outbreaks,18 and as an effective medical teaching tool.19
Different types of social media include collaborative projects, blogs, content communities, and social networking sites.20 Facebook, one of the most popular social networking sites with more than a billion active users,21 allows for the sharing of opinions and information through pictures, texts, and links,22 allowing for new forms of interaction between health professionals and their patients.23 While current research has been undertaken to measure the effectiveness of Web 2.0 and online interventions for the self-management of chronic disease among patients,13,14 there is limited research on how health professionals, specifically working in arthritis care, perceive the usability of Facebook to disseminate self-management programs to their patients. A recent scoping review of the literature on social media use by health professionals and trainees24 included 96 studies of which, only 16 (17%) included a social networking site. The most common types of social media use were discussion forums (45%), blogs or micro blogs (28%), and collaborative projects (21%). The most common medical specialties as categorized by the authors were the combination of administration, critical appraisal and research (11/96, 11.5%), public health (9/96, 9.4%), and mental health (6/94, 6.3%). The most common outcomes measured in the included studies were clinicians’ peer-to-peer communication (43/96, 44.8%), clinicians’ satisfaction (36/96, 37.5%), and clinicians’ knowledge of conditions and complications (22/96, 22.8%). Only two of 16 studies (12.5%) that used a social networking site intervention measured clinicians’ perceived usability of social media tools. The scoping review concluded a paucity of studies using a randomized controlled trial (RCT) design (five of 96 studies (5.2%)) and few studies assessed a social networking site (16 of 96 (16.7%)).24 Furthermore, only three studies (3.1%) and two studies (2.1%) consisted of allied health professionals and nurses in a practice setting respectively.
Among health professionals, Facebook has shown to be a useful tool for sharing knowledge and health promotion with patients,23,25 to obtain up-to-date information and maintain professional connections,23,26 and to facilitate networking, building social capital and community outreach.27 Among arthritis patients, Facebook has shown to be a useful tool for accessing evidence-based educational information to improve their knowledge of non-pharmacological arthritis treatment.28
Web-based arthritis self-management programs, such as The Arthritis Society’s People Getting a Grip on Arthritis (PGrip)29 and the Stanford School of Medicine’s Better Choices Better Health – Arthritis,30 have been shown to improve patients’ health status,31 health literacy,32,33 and self-efficacy.31,32,34 The use of Web 2.0 technologies in arthritis self-management, including interactive web-based educational modules and online discussion boards, have been used for arthritis self-management programs, and allow for social support and interactivity among patients.31–33 While the effectiveness of Web 2.0 technologies for arthritis self-management has been studied among patients,31–34 there is a need for further research to measure the perceived usability of these technologies, such as Facebook, as a dissemination strategy among arthritis health professionals. This feasibility study was designed to address this knowledge gap and further explore Facebook as an innovative dissemination strategy for self-management programs.
Objectives
The objective of this study was to determine the feasibility of using Facebook as a dissemination strategy for the PGrip program by arthritis health professionals to patients. We refer to a dissemination strategy as a method to distribute evidence-based information and materials to arthritis health professionals. We defined arthritis health professionals as individuals who are involved with the care of people with rheumatic disease. The hypothesis of the proposed feasibility study was that arthritis health professionals would demonstrate improvements in the perceived usability of Facebook to share information from the PGrip program with patients after two weeks and three months. We refer to usability as the behavior intention to use a system as determined by its perceived usefulness and perceived ease of use.35 In addition, we hypothesized that the Facebook group page could improve practice behavior change among arthritis health professionals as a strategy to disseminate PGrip after two weeks and three months. We refer to practice behavior change as an improvement in the adoption and implementation of evidence based interventions into routine practice behaviors that may be influenced by a range of individual, organizational, and social factors.36
Methods
Arthritis self-management program
PGrip29 is a bilingual (English/French), educational, evidence-based online self-management program for patients with osteoarthritis (OA) and rheumatoid arthritis (RA). The PGrip program is based on results of comparative controlled trials which investigated the efficacy of various self-management interventions for people living with arthritis and the findings were synthesized and graded by the Ottawa Panel.37–42 Through knowledge synthesis, systematic reviews were performed and rigorous methods were used to develop the Ottawa Panel clinical practice guidelines (CPGs) for the self-management of arthritis. The self-management interventions presented in PGrip were those that achieved positive recommendations (Grades A, B and C+) in the Ottawa Panel CPGs.37–42 According to the Ottawa Panel grading recommendations, a Grade C+ is considered positive and acceptable as it signifies ≥20% in clinical importance although the finding may not be statistically significant (p < 0.05). The Ottawa Panel CPGs for OA and RA43–47 are recognized as high quality CPGs according to several systematic reviews using the Appraisal of Guidelines Research and Evaluation (AGREE I & II)48 criteria. Knowledge from the Ottawa Panel CPGs has been translated into lay terms and tailored into a set of didactic videos for the PGrip program. The Ottawa Panel self-management interventions for OA included: ice massage, hand exercises, aquatic therapy exercises, weight management, and a stationary bicycling program. The RA self-management interventions included: insoles and footwear, yoga, Tai Chi, aquatic jogging, wrist orthotics, and transcutaneous electrical nerve stimulation. For each self-management intervention identified in the Ottawa Panel CPGs, two video presentations were created: (a) a narrated PowerPoint presentation of simplified instructions on how to perform/apply the self-management intervention with case scenarios illustrating the appropriateness and relevance of each; and (b) practical sessions with an arthritis health professional providing step by step instructions while performing/applying the self-management intervention with a patient.
For the current study, a PGrip Facebook group page was created and videos of the presentations and practical sessions for various PGrip self-management interventions were posted on the page. To simplify access, the videos were clearly labeled and categorized by type of arthritis (i.e. OA or RA) and type of video (i.e. narrated presentation or practical session). Other information on the page was provided, including the “About” section which provides a brief description of the PGrip program, and a web link to The Arthritis Society’s PGrip website. Additionally, instructions on how to access the videos and how to post comments or questions were also provided on the page.
Advisory Committee
To engage potential knowledge users in the research process, an Advisory Committee consisting of six arthritis health professional users (two registered nurses, two physiotherapists, and two occupational therapists) was convened to identify barriers of using and accessing Facebook as a dissemination strategy for the PGrip program and to identify how the PGrip Facebook group page can be tailored to improve usability among arthritis health professionals.
To be eligible to participate, Advisory Committee members must have been: (a) trained as a nurse, or physical/occupational therapist; (b) registered with their provincial professional regulatory body; (c) currently practicing clinically which was defined as spending a minimum of 50% of their time (work week) in direct arthritis patient care; (d) had Internet access; (e) able to communicate in English. Additionally, to ensure that measured barriers were solely reflective of the Facebook intervention, and not the content of the PGrip program, Advisory Committee members were previous PGrip users who were familiar with the content of the program. Advisory Committee members were often reminded of this throughout the discussion by the facilitator to prevent response bias. The Advisory Committee members were recruited from local hospitals (The Ottawa Hospital and Children’s Hospital of Eastern Ontario) and The Arthritis Society (Ottawa branch) by poster, e-mail or social media sites of their respective institutions. The Advisory Committee met on three separate occasions that were facilitated by the principal investigator (GD).
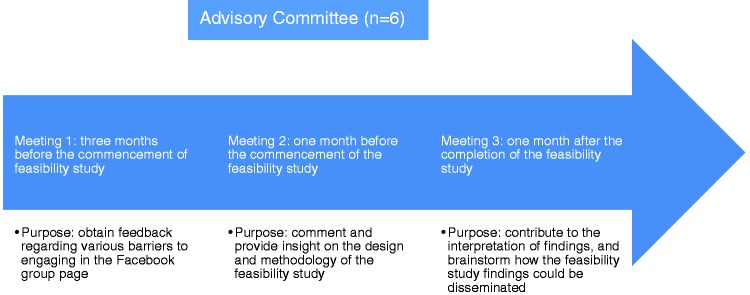
The timeline and purpose of each Advisory Committee meeting is presented in Figure 1. The purpose of the first meeting, which took place three months prior to commencing the feasibility study, was to obtain detailed feedback regarding various barriers to engaging in a Facebook group page to disseminate educational material (such as the PGrip program) to patients and to provide recommendations of how the Facebook group page could be tailored to improve usability. Advisory Committee members were provided with instructions on how to access the Facebook group page prior to the first meeting. The Advisory Committee was asked to provide feedback on the usability of the Facebook intervention using the Technology Acceptance Model 2 (TAM2) questionnaire,35 an extension of the original model.49 A discussion to obtain feedback on barriers took place with an interview guide based on the theoretical domains framework (TDF).36 Results were analyzed by two assessors and differences were resolved by consensus.
Figure 1.
Timeline and purpose of Advisory Committee meetings.
The purpose of the second meeting, one month before the commencement of the feasibility study, was to provide an opportunity for the Advisory Committee members to comment and provide insight on the design and methodology of the feasibility study. Specifically, Advisory Committee members discussed the findings from the first meeting and how the Facebook group page could be tailored to address the identified barriers and facilitators discussed. Based on results from the usability questionnaire in the first meeting, the Facebook group page was to be deemed “usable” if the majority of participants (at least four of the six respondents) achieved an overall mean item score of five (somewhat agree) or greater out of a possible seven points on a tailored 24-item TAM2 questionnaire (Appendix 1). The threshold score of five out of seven was chosen a priori and was considered to be the minimum score representing a positive response regarding usability. In the event that the Facebook intervention was not found to be “usable”, the Advisory Committee would have reconvened at a later date following the second meeting to complete the usability questionnaire once again after the Facebook intervention had been tailored. This process was to be followed until the Committee came to a consensus that the Facebook intervention was deemed to be “usable” and ready for the feasibility study.
The purpose of the third and final meeting, one month after the completion of the feasibility study, was to allow the Advisory Committee members an opportunity to contribute to the interpretation of findings, and brainstorm ideas on how the feasibility study results could be disseminated. They were also asked to provide guidance on the methodology for a future RCT.
Feasibility study
A single arm, pre-post design was used for the feasibility study. Arthritis health professionals were recruited and provided with instructions on how to access the Facebook group page.
Participants
A convenience sample of 78 arthritis health professionals was recruited across Canada by online advertisements using email or online newsletters from the following organizations: Arthritis Health Professions Association, The Arthritis Society, Canadian Physiotherapy Association, Vancouver Coastal Health, St Elizabeth Health Care, Ontario Physiotherapy Association, and Montfort Hospital. A representative from each organization either forwarded the email advertisement to their colleagues or had the advertisement published in their respective organization’s online newsletter. New PGrip users and those already familiar with the PGrip program were invited to participate. In order to be eligible for the feasibility study, participants must have been: (a) trained as a nurse, or physical/occupational therapist; (b) registered with their provincial professional regulatory body; (c) currently practicing clinically which was defined as spending a minimum of 50% of their time (work week) in direct arthritis patient care; (d) had Internet access; (e) communicate in English; and (f) did not participate in the Advisory Committee. Individuals not meeting all inclusion criteria were excluded and were not deemed eligible for the study. Prior to being enrolled in the study, participants were assessed for eligibility through the use of an online admission questionnaire. If deemed eligible, participants registered to the study by contacting the research coordinator by email who later responded and provided further instructions to accessing the Facebook group page. All participants completed an electronic consent form approved by the University of Ottawa Research Ethics Board (H11-12-10).
Measures
Participants completed three assessments using the Fluid Survey online platform.50 The survey links were sent to participants by email. The first assessment included baseline measurements prior to participating in the Facebook group page. The second assessment was performed immediately after posting the material on the Facebook group page (two weeks after baseline). The third and final assessment was at three-months post-intervention.
The primary outcome measure was change in perceived usability of Facebook as a dissemination strategy for the PGrip program with patients at two-weeks post-intervention, measured using an instrument based on the TAM2 questionnaire, a validated tool showing internal consistency reliability and construct validity.35 Change in perceived usability at three-months post-intervention was also assessed. The TAM2 is a 26-item questionnaire consisting of nine domains: intention to use (two items), perceived usefulness (four items), perceived ease of use (four items), subjective norm (two items), voluntariness (three items), image (three items), job relevance (two items), output quality (two items), and result demonstrability (four items). The TAM2 questionnaire is measured on a seven-point Likert scale (1 = strongly disagree to 7 = strongly agree). Given that Facebook may not be accessible due to firewalls in the workplace for all study participants, two items from the image domain were removed. Thus a tailored 24-item TAM2 questionnaire was used (Appendix 1). Definitions for each domain of the TAM2 questionnaire can be found in Appendix 2.
Other outcomes included: (a) change in perceptions of barriers to using Facebook as a dissemination strategy for the PGrip program with patients at two-weeks post-intervention and three-months follow-up; (b) practice behavior change in using Facebook as a dissemination strategy for the PGrip with patients at two-weeks post-intervention and three-months follow-up; and (c) changes in Facebook use and impact measures at two-weeks post-intervention and three-months follow-up
To measure change in perceptions of barriers, participants were asked to identify their top three barriers to engaging in the Facebook group page. Each identified barrier was coded and categorized according to constructs of the TDF and was analyzed descriptively. For example, a lack of experience or skill was categorized as a “skill” barrier, while a lack of Internet access at the workplace was categorized as an “environmental context and resources” barrier.
Practice behavior change was measured using an instrument based on the TDF questionnaire.36 The TDF questionnaire is a validated tool that has shown high internal consistency reliability and discriminant validity.36 As identified by Huijg et al.,36 the TDF questionnaire is generic and can be used to measure TDF-based determinants of healthcare professionals’ specific implementation behaviors. The TDF questionnaire is a 32-item tool that allows for application within a range of different contexts in which implementation research takes place. Each domain contains a different amount of items: knowledge (four items), skills (three items), social/professional role and identity domain (four items), optimism (two items), beliefs about capabilities (three items), beliefs about consequences (two items), intentions (four items), memory/attention /decision (four items), environmental context and resources (two items), social influences (two items), and emotion (two items). The TDF questionnaire is scored by a five-point Likert scale (1 = strongly disagree to 5 = strongly agree) for most domains, though not all 32 items use the same five-point Likert scale. For example, one item in the tailored questionnaire asks “For how many of the next 10 patients do you intend to use the Facebook group page to disseminate PGrip?” Options for this question consisted of a five-point Likert scale ranging from no patients to >4 patients. Another question asked “How strong is your intention to use Facebook to implement (share/discuss) PGrip with patients?” Options for this question consisted of a five-point Likert scale ranging from 5 = very strong to 1 = very weak. Four items (one from the skills domain, one from the beliefs about capabilities domain, and two from the emotions domain) were removed, as they were not deemed to be appropriate for the nature of the Facebook intervention in the health professional workplace. As a result, the emotion domain was not evaluated. Thus, a tailored 28-item TDF questionnaire was used (Appendix 3). Definitions for each domain of the TDF questionnaire can be found in Appendix 4.
Facebook impact measures were assessed by asking participants to rank the number of times they used the following Facebook tools using a five-point Likert scale ranging from one (>8 times) to five (0 times): (a) posted a comment on the “Wall” of the Facebook page; (b) posted a comment on a video on the Facebook page; (c) used the “Like” feature on a comment and/or video on the Facebook page; and (d) shared a link to a video or other website on the Facebook page.
Statistical analyses
For the Advisory Committee, the discussion was digitally recorded and field notes were taken by a non-participant observer. Following the first meeting, results from the usability questionnaire were analyzed descriptively using means and standard deviations (SDs) for items and domains. Discussion responses surrounding perceived barriers were analyzed and coded following the constructs of the TDF (Appendix 4).
For the feasibility study, data analyses were performed using SPSS v. 22. Descriptive statistics such as proportions, mean and SD were used to summarize baseline characteristics. For the primary outcome of usability, a paired t-test was conducted to compare changes from baseline scores to two-weeks post-intervention for each item of the TAM2 questionnaire. Additional paired t-test analyses were conducted comparing baseline scores to the three-month follow-up period. Adjustments for multiple comparisons were not made to the statistical testing. To facilitate the interpretation of findings, mean scores and SDs were calculated for each TAM2 domain. The data was deemed to be normally distributed. For the secondary outcome of TDF domain item scores, the same analysis strategy using paired t-tests to compare changes from baseline to two-weeks post-intervention and baseline to three-month follow-up was considered. Mean scores and SDs were also calculated for each TDF domain. Descriptive statistics were used to summarize the perceived barriers and Facebook impact measures. For perceived barriers, the proportion of all responses was calculated for each identified barrier according to TDF construct, while for Facebook impact measurement, the proportion of participants using Facebook was calculated for each question. For the analyses of the TAM2 and TDF scores, missing values were imputed using the last observation carried forward approach. Additionally, complete case analyses, in which missing data were omitted, were performed for all outcomes.
Results
Advisory Committee
During the first Advisory Committee meeting, several common barriers and facilitators to using Facebook as a dissemination strategy were discussed. The Advisory Committee felt that the Internet is an easier method for accessing clinical practice guidelines and evidence-based material using printed articles and materials. Ultimately, Committee members would not have initially thought to use Facebook as a dissemination strategy but, if they were aware that the information was there, they would refer it to their patients. Generally, the Committee members were not familiar with Facebook. However, after using the group page, it was deemed more straightforward than what was previously believed. Several barriers to using the Facebook group page with patients were brought forward including privacy concerns using social media platforms. Initially, one Committee member stated “I wouldn’t join a page made specifically for patients because of personal confidentiality.” While there was a consensus and hesitancy for both clinicians and patients to use personal accounts to interact and post comments, this concern was mitigated after it was identified that personal accounts were not needed to access the content of the group page. Another common theme identified as a barrier was access to the Internet, computer, and mobile devices. One Committee member stated “Computers with access to high speed Internet may be hard to find at times.” The Advisory Committee members felt that their patients’ general computer skills may be another potential barrier. One Committee member stated that “Certain clients may have issues with using social media platforms.” Committee members felt that Facebook was useful for patients in clinical settings indicating that “patients in the waiting room can scroll through the page.” They also felt that the group page was appropriate and liked the idea of providing patients with a web link, as opposed to a pamphlet. In order to tailor and improve the PGrip Facebook group page for the feasibility study, each Advisory Committee member provided feedback, such as minor glitches in some of the videos, and suggestions on page accessibility (e.g. instructions on navigating the site, and improved ordering of videos) were provided. These comments were addressed prior to commencing the feasibility study. Results from the TAM2 questionnaire revealed that all Advisory Committee members believed that the Facebook group page was “usable” as four of six respondents achieved an overall mean item score of five (somewhat agree) or greater out of a possible seven points. Total mean (SD) item scores ranged from 4.8 (1.6) (neutral) to 5.8 (1.0) (somewhat agree). Consensus on the usability was further confirmed after discussing these findings with all Advisory Committee members at the second meeting. The consensus agreed upon by all committee members was that the Facebook group page was a “usable” tool that warranted further investigation in a feasibility study.
During the second Advisory Committee meeting, members brainstormed and discussed the methodology for the proposed feasibility study. In addition to Facebook being a dissemination strategy for arthritis health professionals to use with patients, the original scope of the proposed feasibility study was to also examine the use of Facebook as a tool for health professionals to access evidence-based material, such as the PGrip program, to improve their own knowledge. The Committee members came to a consensus and decided that the usability questionnaire (TAM2) should only focus on Facebook as a dissemination tool for health professionals with patients. The Committee felt that questions pertaining to the use of Facebook as an information source for health professionals could be omitted. While the Committee was enthusiastic about Facebook as a dissemination tool that health professionals can use with their patients, they did not believe that Facebook would be as useful as an information source for health professionals. The main reasoning for this was that according to one of the inclusion criterion “spending a minimum 50% of the time in direct patient care,” health professionals should already have the knowledge of the material presented in PGrip. This important feedback was considered and implemented in the feasibility study.
During the third Advisory Committee meeting, results from the feasibility study (presented below), were presented. The Committee also provided ideas for disseminating the results of this study which included publishing the findings in a peer-reviewed journal and providing an electronic information brief to patient organization groups who could then include them in their newsletters, websites, or social media pages. The Committee also brainstormed ideas for a future full-scale RCT that would compare the Facebook group page with other information and communication technologies such as websites, YouTube channels, or device applications (“apps”).
Feasibility study
A summary of baseline demographic information can be found in Table 1. A total of 78 arthritis health professionals, comprising 14 (17.9%) occupational therapists, 53 (67.9%) physiotherapists, and 11 (14.1%) registered nurses participated in the study. The mean age of participants was 40.0 years and the majority resided in Ontario (65.4%) and were female (93.4%). While the majority had a Facebook account (93.6%), only 39.7% had access to Facebook at the workplace, though 89.7% stated they would use Facebook outside work hours. In regards to work setting, 54.1% worked in group practice, seeing on average approximately nine patients per day. Most (29.5%) worked in a hospital, 23.0% worked in private practice, 16.4% in a community health center, 9.8% in a rehabilitation facility, and 21.3% in other settings (e.g. home or outpatient). Most had greater than 20 years of clinical experience (31.1%) and were not familiar with the PGrip program (88.5%). All 78 participants completed the baseline questionnaire, 76 (97.4%) completed the second questionnaire at two-weeks post-intervention and 75 (96.2%) completed the final questionnaire at three-months post-intervention. A study flowchart of feasibility study participants is presented in Figure 2.
Table 1.
Baseline characteristics and Facebook use (n = 78).
| n | % | |
|---|---|---|
| Province of residence | ||
| Ontario | 51 | 65.4 |
| Quebec | 6 | 7.7 |
| British Columbia | 17 | 21.8 |
| Other | 4 | 5.1 |
| Profession | ||
| OT | 14 | 17.9 |
| PT | 53 | 67.9 |
| RN | 11 | 14.1 |
| Agea | ||
| Mean (SD)a | 40.0 (10.3) | |
| Sexa | ||
| Male | 4 | 6.6 |
| Female | 57 | 93.4 |
| Practice locationa | ||
| Urban | 37 | 60.7 |
| Rural | 11 | 18.0 |
| Suburban | 13 | 21.3 |
| In which of the following settings do you usually work?a | ||
| Private practice | 14 | 23.0 |
| Hospital | 18 | 29.5 |
| Rehabilitation facility | 6 | 9.8 |
| Community health center | 10 | 16.4 |
| Other (home, outpatient, community care) | 13 | 21.3 |
| What is your primary employment role?a | ||
| Clinician | 57 | 93.4 |
| Other | 4 | 5.1 |
| On average, how many clients do you see per day?a | ||
| Mean (SD) | 8.64 (4.68) | |
| In regards to your work setting, do you work ina | ||
| Solo practice | 28 | 45.9 |
| Group practice | 33 | 54.1 |
| Group practice role: | ||
| Primary therapist | 23 | 37.7 |
| Educator | 3 | 4.9 |
| Multidisciplinary | 2 | 3.3 |
| Interdisciplinary | 2 | 3.3 |
| Manager/chair of team | 1 | 1.6 |
| Did not state | 2 | 3.3 |
| Level of education (as practitioner degree)a | ||
| Diploma | 4 | 6.6 |
| Bachelor's degree | 35 | 57.4 |
| Master's degree | 22 | 36.1 |
| How many years of clinical experience do you have as a PT/OT/RNa | ||
| 0–4 | 8 | 13.1 |
| 5–9 | 14 | 23.0 |
| 10–14 | 8 | 13.1 |
| 15–19 | 10 | 16.4 |
| >20 | 19 | 31.1 |
| Familiar with Facebook | ||
| Yes | 72 | 92.3 |
| No | 5 | 6.4 |
| Did not respond | 1 | 1.3 |
| Has a Facebook account | ||
| Yes | 73 | 93.6 |
| No | 5 | 6.4 |
| Has access to Facebook at the workplace | ||
| Yes | 31 | 39.7 |
| No | 46 | 59.0 |
| Did not respond | 1 | 1.3 |
| Would use Facebook outside work hours | ||
| Yes | 70 | 89.7 |
| No | 3 | 3.8 |
| Did not respond | 5 | 6.4 |
OT: occupational therapist; PT: physiotherapist; RN: registered nurse; SD: standard deviation.
Based on responses from 61 participants.
Figure 2.
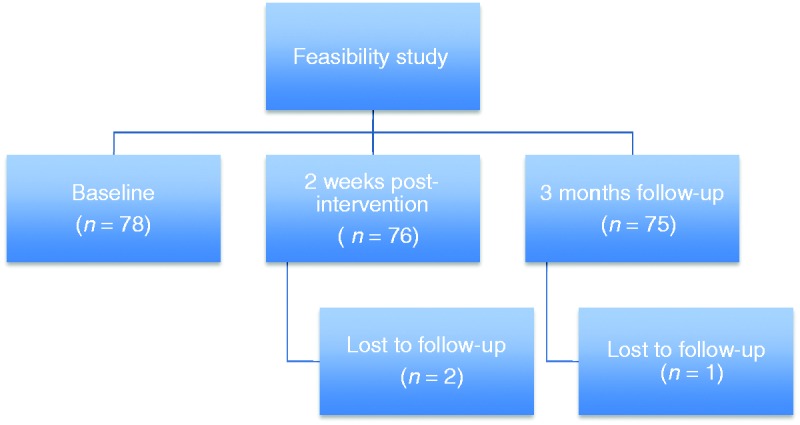
Feasibility study flowchart.
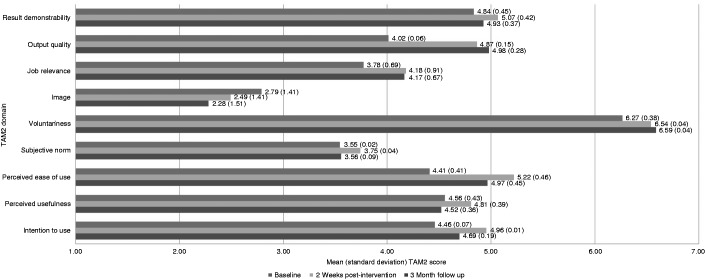
Change in perceived usability
For the primary outcome of usability based on the TAM2 questionnaire at two-weeks post-intervention, the mean absolute changes from baseline for each item, is presented in Appendix 5. Figure 3 presents the mean usability scores for each domain at baseline, two-weeks post-intervention, and three-months follow-up. At two-weeks post-intervention, the mean (SD) score numerically improved, though responses remained categorized as neutral for the intention to use domain from 4.46 (0.07) to 4.96 (0.01) (both items statistically significant), the perceived usefulness domain from 4.56 (0.43) to 4.81 (0.39) (two of four items statistically significant), and the output quality domain from 4.02 (0.06) to 4.87 (0.15) (both items statistically significant). The mean score improved from somewhat disagree to neutral for the job relevance domain from 3.78 (0.69) to 4.18 (0.91) (one of two items statistically significant). The mean scores improved from neutral to somewhat agree for the perceived ease of use domain from 4.41 (0.41) to 5.22 (0.46) (all four items statistically significant) and result demonstrability domain from 4.84 (0.45) to 5.07 (0.42) (one of four items statistically significant). The mean score numerically improved, but the response remained categorized as moderately agree for the voluntariness domain from 6.27 (0.38) to 6.54 (0.04) (one of three items statistically significant). There were no statistically significant improvements for the subjective norm or image domains.
Figure 3.
Mean usability scores by Technology Acceptance Model 2 (TAM2) domain.
At three months, the mean score numerically improved from baseline, though responses remained categorized as neutral for the perceived ease of use domain from 4.41 (0.41) to 4.97 (0.45) (three of four items statistically significant), and the output quality domain from 4.02 (0.06) to 4.98 (0.28) (both items statistically significant). The mean score improved from somewhat disagree to neutral for the job relevance domain from 3.78 (0.69) to 4.17 (0.67) (one of two items statistically significant). The mean score numerically improved, but remained categorized as moderately agree for the voluntariness domain from 6.27 (0.38) to 6.59 (0.04) (one of three items statistically significant). There were no statistically significant improvements for the intention to use, perceived usefulness, subjective norm or result demonstrability domains. There was a numeric decrease in mean score from baseline for the image domain from 2.79 (1.41) to 2.28 (1.51), however the response remained categorized as moderately disagree (the one item was statistically significant). There were no differences between the complete case analysis and last observation carried forward analysis at two weeks and three months.
Change in perceptions of barriers
Prior to receiving the Facebook intervention at baseline, the most common barriers to using Facebook as a dissemination strategy for the PGrip with patients, as categorized by the TDF, were environmental context and resources (environmental constraints) (45.6%). Other common barriers included social/professional role and identity (16.4%) and beliefs about consequences (anticipated outcomes/ attitude) (9.7%) (Table 2). Following the intervention after two weeks, the most common barriers were environmental context and resources (50.2%), skills with using the Facebook group page (11.0%) and knowledge about Facebook (10.1%). After three months, the most common barriers were environmental context and resources (56.5%), beliefs about capabilities (self-efficacy) in using Facebook (10.6%), and skills with using the Facebook group page (10.1%).
Table 2.
Perceived barriers to engaging in Facebook group page.
| Barrier (based on TDF)a | Baseline (n = 226) | 2 Weeks (n = 219) | 3 Months (n = 207) |
|---|---|---|---|
| Knowledge | 9.3% | 10.1% | 7.3% |
| Skills | 9.7% | 11.0% | 10.1% |
| Social/professional role and identity | 16.4% | 10.1% | 5.3% |
| Beliefs about capabilities (self-efficacy) | 7.1% | 7.7% | 10.6% |
| Beliefs about consequences (anticipated outcomes/ attitude) | 9.7% | 10.1% | 7.3% |
| Motivation and goals (intention) | 0.4% | 0.0% | 0.0% |
| Memory, attention and decision processes | 0.4% | 0.0% | 0.0% |
| Environmental context and resources (environmental constraints) | 45.6% | 50.2% | 56.5% |
| Emotion | 1.3% | 0.5% | 0.5% |
| Nature of behaviors (habits) | 0.0% | 0.5% | 2.4% |
TDF: theoretical domains framework.
Participants provided multiple responses as they were instructed to list their top three barriers.
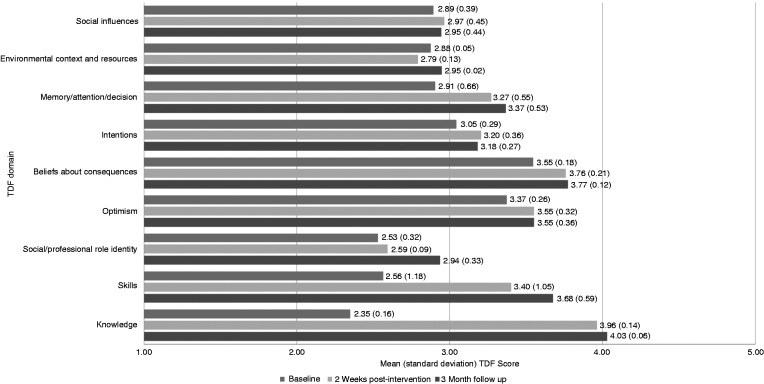
Practice behavior change
For the outcome of practice behavior change based on the TDF questionnaire at two weeks post-intervention, the mean absolute change from baseline for each item is presented in Appendix 6. Figure 4 presents the mean practice behavior change scores for each domain at baseline, two-weeks post-intervention, and three-months follow-up.
Figure 4.
Mean practice behavior change scores by theoretical domains framework (TDF) domain.
At two-weeks post-intervention, the mean (SD) score numerically improved, though responses remained categorized as neutral for the optimism domain from 3.37 (0.26) to 3.55 (0.32) (three of four items statistically significant), beliefs about capabilities domain from 3.55 (0.18) to 3.76 (0.21) (one of two items statistically significant), and the intentions domain from 3.05 (0.29) to 3.20 (0.36) (one of four items statistically significant). The mean score improved from somewhat disagree to neutral for the knowledge domain from 2.35 (0.16) to 3.96 (0.14) (four of four items statistically significant), skills domain from 2.56 (1.18) to 3.40 (1.05) (two of two items statistically significant), and memory/attention/decision domain from 2.91 (0.66) to 3.27 (0.55) (three of four items statistically significant). There was a numerical improvement in mean score for the social/professional role identity domain from 2.53 (0.32) to 2.59 (0.09) (two of four items statistically significant), however the responses remained categorized as somewhat disagree. Items of the social/professional role and identity domain demonstrated variable findings as there was a statistically significant improvement for one of the four items, and a statistically significant decrease for another item. There were no statistically significant improvements for the environmental context and resources and social influences domains.
At three months, the mean knowledge domain score improved from somewhat disagree to agree from 2.35 (0.16) to 4.03 (0.06) (four of four items statistically significant). The mean score numerically improved, though responses remained categorized as neutral for the optimism domain from 3.37 (0.26) to 3.55 (0.36) (one of four items statistically significant), and beliefs about capabilities domain from 3.55 (0.18) to 3.77 (0.12) (one of two items statistically significant). The mean domain score improved from somewhat disagree to neutral for skills domain from 2.56 (1.18) to 3.68 (0.59) (two of two items statistically significant), and memory/attention/decision domain from 2.91 (0.66) to 3.37 (0.53) (three of four items statistically significant). There were no statistically significant improvements for the optimism, intentions, environmental context and resources and social influences domain.
Facebook use and impact measures
Facebook use and impact measures at two-weeks post-intervention and three-months follow-up is presented in Table 3. After two weeks, the majority of participants (93.6%) did not post a comment on the “Wall” of the Facebook group page, while one participant (1.3%), and two participants (2.6%) posted a comment once and three times respectively. Similarly, the majority of participants (93.6%) did not post a comment on a video of the Facebook group page, while one participant (1.3%), and two participants (2.6%) posted a comment once and three times respectively. Most participants (64.1%) did not use the “like” feature on a comment and/or video on the Facebook group page, while 15 participants (19.2%) used the like feature once, six participants (7.7%) used the like feature three times, three participants (3.8%) used the like feature five times, and one participant (1.3%) used the like feature eight times or greater. Most participants (85.9%) did not share a link to a video or other websites on the Facebook group page, while six participants (7.7%), two participants (2.6%), and one participant (1.3%) shared a link once, three times, and eight times or greater, respectively. After three months, the number or participants who posted a comment on the “Wall”, posted a comment on a video, used the “like” feature, and shared a link to a video or other website generally increased in comparison with the assessment at two weeks (Table 3).
Table 3.
Facebook use (n = 78).
| 2 Weeks |
3 Months |
Absolute mean change |
|||
|---|---|---|---|---|---|
| n | % | n | % | % | |
| Posted a comment on the "Wall" of the Facebook group page | |||||
| >8 times | 0 | 0.0% | 0 | 0.0% | 0.0% |
| 5 times | 0 | 0.0% | 1 | 1.3% | 1.3% |
| 3 times | 1 | 1.3% | 0 | 0.0% | –1.3% |
| 1 time | 2 | 2.6% | 6 | 7.7% | 5.1% |
| 0 times | 73 | 93.6% | 68 | 87.2% | –6.4% |
| No response | 2 | 2.6% | 3 | 3.8% | 1.3% |
| Posted a comment on a video on the Facebook group page | |||||
| >8 times | 0 | 0.0% | 1 | 1.3% | 1.3% |
| 5 times | 0 | 0.0% | 0 | 0.0% | 0.0% |
| 3 times | 2 | 2.6% | 2 | 2.6% | 0.0% |
| 1 time | 1 | 1.3% | 6 | 7.7% | 6.4% |
| 0 times | 72 | 92.3% | 66 | 84.6% | –7.7% |
| No response | 3 | 3.8% | 3 | 3.8% | 0.0% |
| Used the "Like" feature on a comment and/or video on the Facebook group page | |||||
| >8 times | 1 | 1.3% | 3 | 3.8% | 2.6% |
| 5 times | 3 | 3.8% | 5 | 6.4% | 2.6% |
| 3 times | 6 | 7.7% | 3 | 3.8% | –3.8% |
| 1 time | 15 | 19.2% | 16 | 20.5% | 1.3% |
| 0 times | 50 | 64.1% | 48 | 61.5% | –2.6% |
| No response | 3 | 3.8% | 3 | 3.8% | 0.0% |
| Shared a link to a video or other website on the Facebook group page | |||||
| >8 times | 1 | 1.3% | 2 | 2.6% | 1.3% |
| 5 times | 0 | 0.0% | 0 | 0.0% | 0.0% |
| 3 times | 2 | 2.6% | 3 | 3.8% | 1.3% |
| 1 time | 6 | 7.7% | 7 | 9.0% | 1.3% |
| 0 times | 67 | 85.9% | 63 | 80.8% | –5.1% |
| No response | 2 | 2.6% | 3 | 3.8% | 1.3% |
Discussion
We hypothesized that arthritis health professionals would demonstrate improvements in the perceived usability of Facebook to share information from the PGrip program with patients after two weeks and three months. The sample of participants included a diversity of work settings. As nearly almost all participants (89%) were not previously familiar with the PGrip program, this study highlights the need for additional dissemination strategies. Two weeks after its introduction, the feasibility of the Facebook group page being an easy to use tool was confirmed as arthritis health professionals indicated a greater intention to use the group page, agreeing that they would share it with patients. Participants demonstrated improved ease of use as they agreed that the group page was clear and understandable, did not require a significant amount of mental effort, was easy to use with patients, and easy to accomplish what they intended to do with the page. There were also improvements in output quality as participants agreed that the output they got from the group page was high, and that they had no problem with the quality of group page. There remains uncertainty with improvements regarding the perceived usefulness of the group page (perceived usefulness domain) and relevance of the group page in relation to participants’ jobs (job relevance domain). While numerical improvements were seen for all items of these domains, not all items demonstrated statistically significant changes from baseline. Both the perceived usefulness and job relevance domains included multiple items. While all domain items pertain to a common theoretical construct (domain), each item was intended to capture various components of their respective domains. For example, the perceived usefulness domain asked patients whether the Facebook group page improved their job performance, increased their productivity, enhanced their job effectiveness, and whether they perceived the tool to be useful in their job. Only items pertaining to increased productivity and usefulness of the tool in their job demonstrated statistically significant differences, while the remaining items did not. The statistically significant findings are in line with the discussion of the Advisory Committee, which concluded that the Facebook group page was a useful tool to refer the PGrip program to their patients and that it provides clinicians with another resource or tool to teach their patients about RA and OA self-management. Another study that surveyed 485 primary care physicians and oncologists in the USA concluded that social media was perceived as being a useful and efficient method to share medical knowledge.25 Similar to our study, the Technology Acceptance Model was used to explore physician’s attitudes towards social media, and their perceptions on its usefulness and ease of use. Approximately 46.0% of respondents used social media on a weekly basis to scan or explore medical information, 57.5% perceived social media to be beneficial and engaging as a method to access high-quality information, 57.9% felt it was useful and enabled them to care for patients more effectively, and 60% felt it improved the quality of the care that they delivered. In our feasibility study, the job relevance domain asked patients whether the use of the Facebook group page was both important and relevant in their job; only the latter item was statistically significant. Although unclear, non-significant findings may be explained by the lack of a clear definition of what is considered ‘important’. These findings were also consistent with discussions among the Advisory Committee who commented that the use of a Facebook group page was relevant to their jobs as most hospitals, rehabilitation facilities and community health centers have similar social media pages to share information with patients and clients; there were no comments or indications on the importance of using the Facebook page in their jobs.
With variable findings (i.e. some items showing improvements and others showing declines from baseline), further uncertainty remains in relation to the voluntariness of using the group page (voluntariness domain), and difficulties in communicating the findings, benefits, and consequences of the group page with others (result demonstrability domain). The variable results of the voluntariness and image domains may be explained by the nature of the intervention, in which the introduction of a Facebook page would likely not have an impact on change in voluntariness (i.e. organization policies would not change because of the intervention), and image (i.e. difficult to change perception of one’s image or status in a social system in such a short period of time); however, reasoning for the variable results of the result demonstrability domain remains unclear. Furthermore, the variable results of the voluntariness and image domains may be explained by the baseline mean scores, which were numerically higher for the voluntariness domain, and lower for the image domain, in comparison to other domains scores, suggesting that participants had strong beliefs about these two domains prior to the study, which may not have allowed for a large margin of change. The Facebook group page did not appear to have an impact on image, as participants did not agree that using the group page would enhance how they would be viewed by their organizations for using the group page. Additionally, it remains unclear exactly how long it takes to change the perception of one’s image or status in a social system. Thus, this study may not have been of sufficient duration to measure and assess whether the Facebook group page can have a positive effect on image. As seen in other research that has used the TAM2, the impact of image on perceived usefulness is not significant when the usage of a technology or system is optional.35,51 Peluchette et al. found that while the use of social media in the work setting can elicit positive reactions such as improving job satisfaction and strengthening relationships, social media use may be seen as unprofessional or inappropriate, creating possibilities for confidentiality breaches.27 Similar privacy and patient confidentiality concerns were also identified in this feasibility study, which may explain the health professionals’ negative implication on image. There is also uncertainty regarding the perception that that most people believe they should be using Facebook as a dissemination strategy as there were no statistically significant improvements in the subjective norm domain. While social media continues to grow in popularity, its use in a work environment is not always accepted as it is sometimes seen as mixing professional and personal boundaries.27
Findings at three months suggest that the overall perceived usability of the Facebook group page appeared to marginally decline over time as changes from baseline were generally similar though inferior to measurements at two weeks for the intention to use, perceived ease of use, subjective norm, job relevance and result demonstrability domains. However, changes in the intention to use and perceived usefulness domains no longer remained statistically significant at three months. In contrast, improvements in output quality were superior after three months, which may be a result of participants having more time to explore the content and videos of the group page. The findings from the use of the group page suggest that the majority of participants did not use it regularly in their everyday practice, which may explain the marginal decline in item scores after three months.
The successful implementation of evidence-based practice in arthritis care requires an interprofessional approach to identify barriers.47 This study included physiotherapists, occupational therapists and nurses who work in arthritis care. Numerous barriers to engaging in the Facebook group page to disseminate the PGrip program to patients were identified. The most common barriers identified were those related to environmental context and resources. Most participants were concerned about Internet access or not having access to a computer or mobile devices in the workplace. Similarly, they were concerned whether their patients had Internet access, or access to computers and mobile devices. In addition, several participants also felt that they did not have a sufficient amount of time in their work environment to go through the Facebook group page with patients as timing is limited to performing comprehensive assessments. As clinics and hospital settings continue to evolve, there is a need for access to Internet and technologies by health professionals in these institutions. Technology in the work setting has shown to facilitate clinical and patient shared decision making.2 If health professionals have limited time to go through the PGrip content, they can simply provide patients with the link to the Facebook group page to allow them to access the content on their own, and perhaps answer any questions at a future visit. Another common concern of participants was the social/professional role and identity. Some institutions prohibit the use of social media while working and some identified that it is perceived “unprofessional” to use Facebook at work. Additionally, participants were hesitant of whether the group page would allow for theirs and their patients’ privacy and confidentiality to be maintained. While these were common barriers identified at baseline, after three months, there was a decrease in the proportion of participants who identified barriers relating to social/professional role and identity. After engaging in the PGrip Facebook group page, health professionals may have realized that the group page can be used in a professional manner to assist patients to self-manage their arthritis. In recent years, social media in the workplace has evolved,15 and more and more organizations are creating organizational Facebook pages.23 The PGrip Facebook group page does not require patients or health professionals to identify themselves. While the use of some tools such as posting comments or writing on the “Wall” requires individuals to create an account, the content and videos on the group page are accessible for everyone with or without a Facebook account. Other barriers identified were knowledge relating to Facebook as some participants and their patients were not familiar with the social networking website. Participants were also concerned about their patients not possessing the necessary general computer skills to navigate to the Facebook group page. Findings at three months suggest that barriers associated with knowledge and skills were marginally reduced after participants grew more familiar with the group page. This may suggest that this barrier may continue to be reduced after a longer period of time and greater exposure.
We also hypothesized that the Facebook group page can improve practice behavior change among arthritis health professionals as a strategy to disseminate PGrip after two weeks and three months. While improvements were seen after two weeks, participants overall did not feel that the Facebook group page had an impact on their practice behavior in regards to the dissemination of the PGrip program. Based on findings from the TDF questionnaire, baseline scores indicated that participants’ had negative or neutral feelings regarding the various domains. Arthritis health professionals indicated improvements in understanding the content, objectives and how to use the Facebook group page (knowledge domain). Participants demonstrated improved skills (skills domain), agreeing that they had the skills to use the group page. While other improvements were seen across other domains, participants either remained neutral or in disagreement on whether the Facebook group page had an impact on their practice behavior. Though mostly similar to comparisons at two weeks, there were marginal improvements in several domains (e.g. knowledge, social/professional role and identity, beliefs about capabilities, memory/attention/decision, and environmental context and resources) after three months. Two weeks, and three months may not have been a sufficient amount of time to detect meaningful differences in practice behavior change. Change in practice can take several years, with some estimates even suggesting between one to two decades for original research to be incorporated into routine practice.52
Research has shown that most health professionals already have basic knowledge of how to use Facebook with colleagues and patients, and the implication of using it.23 Another study similarly concluded that social media has a limited impact on change in practice as adding social media-based outreach dissemination methods to traditional methods did not improve awareness of the CPG and knowledge of CPG recommendations, nor did it affect implementation of the recommendations.53
The majority of participants did not use features of the Facebook group page such as the “Wall” or “Like” button, or posted comments on the videos. There were marginal increases in the use of these features over time, which may suggest that participants grew more comfortable or had more time to use them, however overall usage remained low. Although previous research has shown that health professionals frequently use social media even though the perceived barriers are high,34 the barriers identified in this study by have impacted the overall use of the Facebook group page. One potential reason for the low rate of usage of these features may be related to concerns over confidentiality and privacy as noted in both the Advisory Committee discussion and the findings of barriers. Based on these concerns, there have been recommendations made to health professionals to not contact patients through Facebook and to use high privacy settings.54 Laliberté et al. surveyed 322 physiotherapists and physical rehabilitation therapists practicing in Quebec, Canada to determine their knowledge and practice behavior of using Facebook.23 While the majority (84.3%) had a personal Facebook account, only 3% of respondents reported having a professional profile. Several respondents (35.5%) stated that their workplace had a professional page, 27% had employers as online friends, while 21% had patients as online friends. A study that explored the attitudes and experiences of 682 health professional students using Facebook concluded that 44% of respondents had colleagues as online friends.55 Health professional students were more cautions with Facebook use with patients as only less than 1% had current patients/clients as online friends and 40% felt it was unprofessional to post any information relating to a patient/client, even in the absence of identifying information. There was a consensus that posting material to Facebook was associated with risks to their current position and future prospects.55
Both perceived usability and practice behavior change are complex outcomes, influenced by various factors (domains).35,56–59 The use of questionnaires based on theoretical frameworks (i.e. TDF and TAM2) allowed for the identification of change across various domains. As highlighted above, greater improvements were seen in certain domains for perceived usability (e.g. intention to use, ease of use, output quality) and certain practice behavior domains (e.g. knowledge and skills) compared to others. The TDF framework also allowed for the categorization of barriers, highlighting that environmental context and resources were by far the biggest concern for arthritis health professionals to using the Facebook group page.
From the overall findings of this feasibility study, we can infer that Facebook offers arthritis health professionals with another option as a dissemination strategy to share evidence-based information, such as the PGrip program, with their patients to successfully self-manage their arthritis. More patients are using the Internet to access health information.12 Over a billion people around the world are currently on Facebook,21 and approximately one in every three older adults who use the Internet access social networking sites such as Facebook, and approximately 20% contribute to these sites by commenting or sharing the health and medical information.60,61 A study by Brosseau et al. used Facebook to disseminate the PGrip program to older patients with arthritis.33 Overall, the Facebook group page successfully enhanced patients’ knowledge and improved intention to use PGrip self-management strategies. Facebook may provide arthritis health professionals with an additional option to enhance self-management support among their patients. Furthermore, directing patients to explore the Facebook group page on their own may help reduce the amount of time needed during consultations for patient education and behavior change counseling.
While social media is increasingly becoming more popular among health professionals,15,23 further research to determine its usability as a dissemination strategy to share evidence is needed. A RCT comparing Facebook with other information and communication technology dissemination strategies would provide further insight on whether it is more usable than other social media platforms or other technologies such as email or websites. Studies should be adequately powered and exploratory subgroup analyses should be performed to consider important factors noted above. Future studies should focus on the strengths of domains that demonstrated successful improvements in this study, as should strive to understand how other perceived usability domains can be improved. As noted in similar research,23,55 there is a need to establish guidelines on social media use in the workplace as professional communications and interaction continue to evolve. Health professionals should be informed on whether current guidelines exist in their workplace23 as guidance on the use of social networking software can help health professionals maintain professionalism while being able to share material and use these technologies.55
Limitations
There were limitations of this study that should be considered. Firstly, this feasibility study used a convenience sample and, as a result, it remains uncertain whether it was adequately powered to detect meaningful differences. Additionally, the study was not designed to assess specific subgroups to determine the effects of factors such as age, practice setting, and clinical experience. Though based on previously validated tools, the questionnaires used were tailored specifically for the Facebook intervention and this study, thus they were not validated prior to this study. The study was also limited by the pre-post design with measurements at two-weeks post-intervention and three-month follow-up. Specifically, the design did not allow for a comparison group, randomization, and used a short time frame of three months. A longer period of six months or greater would provide useful insight on the long-term effects of the dissemination strategy. Given the nature of the survey-based assessments, response bias regarding whether participants felt obligated to provide socially desirable responses cannot be ruled out. As the majority of participants were female, physiotherapists, resided in Ontario, worked in a hospital and urban setting, it remains unclear whether the limited sample of participants was representative of all arthritis health professionals in Canada and may be subject to selection bias. The sample of participants was middle aged (mean age of 40 years), yet the majority possessed several years of clinical experience (>20 years). Previous research has shown that age and gender do not have a significant impact on the adoption or usage of social media among physicians and that practice-related characteristics do not appear to be associated with use of Internet-based communication technologies.62 Another study showed that health professionals with a Facebook account were primarily clinicians, younger, with less work experience.23 Whether older professionals, or those with fewer years of experience would yield similar results remains unclear. Furthermore, while the majority of participants were not familiar with the PGrip program prior to enrolling in the study, the majority were familiar with Facebook and had a registered account. It remains unseen whether familiarity of either the PGrip program or Facebook may have impacted the findings.
Conclusions
This feasibility study suggests that a Facebook group page may be used as a dissemination strategy for the PGrip program by arthritis health professionals, as it was perceived to be usable with patients after two weeks and three months in regards its ease of use and high output quality. There remains uncertainty in regards to the group page’s perceived usefulness, relevance to arthritis health professionals’ jobs, the perception of whether these individuals should be using Facebook as a dissemination strategy, the voluntariness of using the group page, and difficulties in communicating the findings, benefits, and consequences of the group page with others. The Facebook group page did not appear to have an impact on arthritis health professionals’ image and how they would be viewed by their organizations for using the group page. The most common barriers to engaging in the Facebook group page to disseminate the PGrip program to patients included those related to environmental context and resources such as access to Internet and technology in the workplace, and patients having this same access at home. While participants’ knowledge and skills improved over time, they did not feel that the Facebook group page had an impact on their practice behavior in regards to the dissemination of the PGrip program. The overall usage of features such as the “Wall”, “Like” button, and posting of comments was low, though marginally increased over time.
The potential implications of this work are twofold. Firstly, this research provides new knowledge on how a Facebook group page as a dissemination strategy for an evidence-based self-management program for patients is perceived by arthritis health professionals. Secondly, social media, such as Facebook may provide arthritis health professionals with an additional option of how to best share evidence-based information to allow their patients to successfully self-manage their arthritis, while potentially reducing the amount of time needed during consultations for patient education and behavior change counseling.
Acknowledgements
The authors thank all participants of the Advisory Committee and the feasibility study. They would like to thank Arlanna Pugh for her contribution with assisting with the Advisory Committee Meetings and to express thanks to the Arthritis Health Professions Association, The Arthritis Society, Canadian Physiotherapy Association, Vancouver Coastal Health, St Elizabeth Health Care, Ontario Physiotherapy Association, and Montfort Hospital for assistance with participant recruitment.
Appendix
Appendix 1.
Tailored Technology Acceptance Model 2 (TAM2) questionnaire.
| Domain |
1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| Item # | Strongly disagree | Moderately disagree | Somewhat disagree | Neutral (neither disagree or agree) | Somewhat agree | Moderately agree | Strongly agree |
| Intention to use | |||||||
| 1 | Assuming I have access to the Facebook group page, I intend to use it with patients | ||||||
| 2 | Given that I have access to the Facebook group page, I predict that I would use it with patients | ||||||
| Perceived usefulness | |||||||
| 3 | Using the Facebook group page may improve my performance in my job | ||||||
| 4 | Using the Facebook group page in my job may increase my productivity | ||||||
| 5 | Using the Facebook group page may enhance my effectiveness in my job | ||||||
| 6 | I find the Facebook group page may be useful in my job | ||||||
| Perceived ease of use | |||||||
| 7 | My interaction with the Facebook group page is clear and understandable | ||||||
| 8 | Interacting with the Facebook group page does not require a lot of my mental effort | ||||||
| 9 | I find the Facebook group page easy to use with patients | ||||||
| 10 | I find it easy to get to the Facebook group page to do what I want it to do | ||||||
| Subjective norm | |||||||
| 11 | People who influence my behavior think that I should use the Facebook group page with patients | ||||||
| 12 | People who are important to me think that I should use the Facebook group page with patients | ||||||
| Voluntariness | |||||||
| 13 | My use of the Facebook group page with patients is voluntary | ||||||
| 14 | My supervisor does not require me to use the Facebook group page with patients | ||||||
| 15 | Although it might be helpful, using the Facebook group page with patients is certainly not compulsory in my job | ||||||
| Image | |||||||
| 16 | People in my organization who use the Facebook group page with patients have more prestige than those who do not | ||||||
| Job relevance | |||||||
| 17 | In my job, usage of the Facebook group page with patients is important | ||||||
| 18 | In my job, usage of the Facebook group page with patients is relevant | ||||||
| Output quality | |||||||
| 19 | The quality of the output I get from the Facebook group page is high | ||||||
| 20 | I have no problem with the quality of the Facebook group page output | ||||||
| Result demonstrability | |||||||
| 21 | I have no difficulty telling others about the results of using the Facebook group page with patients | ||||||
| 22 | I believe I could communicate to others the consequences of using the Facebook group page with patients | ||||||
| 23 | The results of using the Facebook group page with patients are apparent to me | ||||||
| 24 | I would have no difficulty explaining why using the Facebook group page with patients may or may not be beneficial | ||||||
Source: Adapted from Venkatesh and Davis.35
Appendix 2.
Definitions of Technology Acceptance Model 2 (TAM2) domains.
| Domain | Definitiona |
|---|---|
| Intention to use | Determined by perceived usefulness and perceived ease of use |
| Perceived usefulness | The degree to which a person believes that a particular system would enhance his or her performance |
| Perceived ease of use | The degree to which a person believes that a particular system would be free from effort |
| Subjective norm | Perception that most people who are important think he should or should not perform the behavior in question |
| Voluntariness | The degree to which use of the innovation is perceived as being voluntary, or of free will |
| Image | The degree to which use of an innovation is perceived to enhance one’s image or status in one’s social system |
| Job relevance | Perception regarding the degree to which the target system is applicable to his or her job |
| Output quality | What tasks a system is capable of performing and the degree to which those tasks match their job goals (job relevance) |
| Result demonstrability | Tangibility of the results of using the innovation will directly influence perceived usefulness |
Source: Venkatesh and Davis.35
Appendix 3.
Tailored theoretical domains framework questionnaire.
| 1 |
2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| Item # | Strongly disagree | Disagree | Neutral (neither disagree or agree) | Agree | Strongly agree |
| Knowledge | |||||
| 1 | I am aware of the content and objectives of the Facebook group page | ||||
| 2 | I know the content and objectives of the Facebook group page | ||||
| 3 | I am familiar with the content and objectives of the Facebook group page | ||||
| 4 | I am aware of how to use the Facebook group page to disseminate PGrip with patients | ||||
| Skills | |||||
| 5 | I have the skills to use the Facebook group page to disseminate PGrip with patients | ||||
| 6 | I have practiced using the Facebook group page to disseminate PGrip with patients | ||||
| Social/professional role and identity | |||||
| 7 | Using the Facebook group page to disseminate PGrip with patients is part of my work as an arthritis health professional | ||||
| 8 | As an arthritis health professional, it is my job to use the Facebook group page to disseminate PGrip with patients | ||||
| 9 | It is my responsibility as an arthritis health professional to use the Facebook group to disseminate PGrip with patients | ||||
| 10 | Using the Facebook group page to disseminate PGrip with patients is consistent with my job as a health professional | ||||
| Optimism | |||||
| 11 | I am confident that I can use the Facebook group page to disseminate PGrip with patients even when there is little time | ||||
| 12 | I am confident that if I wanted I could use the Facebook group page to disseminate PGrip with patients | ||||
| 13 | With regard to using the Facebook page to disseminate PGrip with patients in uncertain times, I usually expect the best | ||||
| 14 | With regard to using the Facebook group page to disseminate PGrip with patients I'm always optimistic about the future | ||||
| Beliefs about consequences | |||||
| 15 | If I use the Facebook page to disseminate PGrip with patients, it will benefit public health | ||||
| 16 | If I use the Facebook group page to disseminate PGrip with patients, it will not have disadvantages for my relationship with them | ||||
| Intentions | |||||
| 17a | For how many of the next 10 patients do you intend to use the Facebook group page to disseminate PGrip? | ||||
| 18 | I will definitely use the Facebook group page to disseminate PGrip with patients | ||||
| 19 | I intend to use the Facebook group page to disseminate PGrip with patients | ||||
| 20 b | How strong is your intention to use the Facebook group page to disseminate PGrip with patients? | ||||
| Memory/attention/decision | |||||
| 21 c | How often do you forget to use the Facebook group page to disseminate PGrip with patients? | ||||
| 22 | When I need to concentrate to use the Facebook group page to disseminate PGrip with patients, I have no trouble focusing my attention | ||||
| 23 | When trying to focus my attention on using the Facebook group page to disseminate PGrip with patients, I have no difficulty blocking out distracting thoughts | ||||
| 24 | When concentrating on using the Facebook group page to disseminate PGrip with patients, I can focus my attention so that I become unaware of what's going on around me | ||||
| Environmental context and resources | |||||
| 25 | Within the socio-political context (clinical unit) there is sufficient financial support (e.g. from local authorities, insurance companies) for using the Facebook group page to disseminate PGrip with patients | ||||
| 26 | Within the socio-political context (clinical unit) there are good networks between parties involved in using the Facebook group page to disseminate PGrip with patients | ||||
| Social influences | |||||
| 27 | Most people who are important to me think that I should use the Facebook group page to disseminate PGrip with patients | ||||
| 28 | Most people whose opinion I value would approve me of using the Facebook group page to disseminate PGrip with patients | ||||
PGrip: People Getting a Grip on Arthritis.
Source: Adapted from Huijg et al.36
one = 1; one patient = 2; two patients = 3; three patients = 4; >4 patients = 5.
Very weak = 1; weak = 2; neutral = 3; strong = 4; very strong = 5.
Never = 1; almost never = 2; occasionally = 3; almost always = 4; always = 5.
Appendix 4.
Definitions of theoretical domains framework domains.
| Domain | Definitiona |
|---|---|
| Knowledge | An awareness of the existence of something |
| Skills | An ability or proficiency acquired through practice |
| Social/professional role and identity | A coherent set of behaviors and displayed personal quality s of an individual in a social or work setting |
| Beliefs about capabilities (self-efficacy) | Acceptance of the trust, reality, validity about an ability, talent, or facility that a person can put to constructive us |
| Beliefs about consequences (anticipated outcomes/ attitude) | Acceptance of the truth, reality, or validity about outcomes of a behavior in a given situation |
| Motivation and goals (intention) | A conscious decision to perform a behavior or a resolve to act in a certain way/ mental representations of outcomes or end states that an individual wants to achieve |
| Memory, attention and decision processes | The ability to retain information, focus selectively on aspects of the environment and choose between two or more alternatives |
| Environmental context and resources (environmental constraints) | Any circumstance of a person’s situation or environment that discourages or encourages the development of skills and abilities, independence, social competence, and adaptive behavior |
| Social influences (norms) | Those interpersonal processes that can cause individuals to change their thoughts, feelings, or behaviors |
| Emotions | A complex reaction pattern, involving experiential, behavioral, and physiological elements, by which the individual attempts to deal with a personally significant matter or event |
| Behavioral regulation | Anything aimed at managing or changing objectively observed or measured actions |
| Nature of behaviors (habits)b | Behaviors that are routine, automatic, or habits |
Source: Cane J, O’Connor D and Michie S. Validation of the theoretical domains framework for use in behavior change and implementation research. Implement Sci 2012; 7: 37.
Source: Michie et al.59
Appendix 5.
Usability (Technology Acceptance Model 2 (TAM2)), n = 78.
| TAM2 domain | Baseline |
Absolute change Baseline to 2 weeks |
Absolute change Baseline to 3 months |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Question # | Mean | SD | Mean | SD | 95% CI | p Value | Mean | SD | 95% CI | p Value | |||
| Intention to use | |||||||||||||
| 1 | Assuming I have access to the Facebook group page, I intend to use it with patients | 4.41 | 1.78 | 0.54 | 1.82 | 0.13 | 0.95 | 0.01 | 0.42 | 2.02 | –0.03 | 0.88 | 0.07 |
| 2 | Given that I have access to the Facebook group page, I predict that I would use it with patients | 4.51 | 1.68 | 0.47 | 1.44 | 0.14 | 0.80 | 0.01 | 0.05 | 2.01 | –0.40 | 0.51 | 0.82 |
| Perceived usefulness | |||||||||||||
| 3 | Using the Facebook group page may improve my performance in my job | 4.51 | 1.26 | 0.33 | 1.50 | 0.00 | 0.67 | 0.05 | 0.09 | 1.64 | –0.28 | 0.46 | 0.63 |
| 4 | Using the Facebook group page in my job may increase my productivity | 4.06 | 1.42 | 0.21 | 1.32 | –0.09 | 0.50 | 0.18 | –0.04 | 1.56 | –0.39 | 0.31 | 0.83 |
| 5 | Using the Facebook group page may enhance my effectiveness in my job | 4.56 | 1.25 | 0.36 | 1.39 | 0.05 | 0.67 | 0.03 | –0.01 | 1.56 | –0.36 | 0.34 | 0.94 |
| 6 | I find the Facebook group page may be useful in my job | 5.10 | 1.20 | 0.09 | 1.39 | –0.22 | 0.40 | 0.57 | –0.21 | 1.52 | –0.55 | 0.14 | 0.24 |
| Perceived ease of use | |||||||||||||
| 7 | My interaction with the Facebook group page is clear and understandable | 4.08 | 1.41 | 1.21 | 1.72 | 0.82 | 1.59 | 0.00 | 1.10 | 1.60 | 0.74 | 1.46 | 0.00 |
| 8 | Interacting with the Facebook group page does not require a lot of my mental effort | 4.82 | 1.48 | 0.69 | 1.62 | 0.33 | 1.06 | 0.00 | 0.55 | 1.79 | 0.15 | 0.96 | 0.01 |
| 9 | I find the Facebook group page easy to use with patients | 4.03 | 1.06 | 0.53 | 1.45 | 0.20 | 0.85 | 0.00 | 0.34 | 1.43 | 0.02 | 0.67 | 0.04 |
| 10 | I find it easy to get to the Facebook group page to do what I want it to do | 4.71 | 1.42 | 0.83 | 1.78 | 0.43 | 1.24 | 0.00 | 0.28 | 1.90 | –0.15 | 0.71 | 0.19 |
| Subjective norm | |||||||||||||
| 11 | People who influence my behavior think that I should use the Facebook group page with patients | 3.56 | 1.29 | 0.15 | 1.60 | –0.21 | 0.52 | 0.40 | –0.08 | 1.55 | –0.43 | 0.27 | 0.66 |
| 12 | People who are important to me think that I should use the Facebook group page with patients | 3.53 | 1.36 | 0.24 | 1.51 | –0.10 | 0.58 | 0.16 | 0.09 | 1.56 | –0.26 | 0.44 | 0.61 |
| Voluntariness | |||||||||||||
| 13 | My use of the Facebook group page with patients is voluntary | 5.85 | 1.41 | 0.69 | 1.45 | 0.36 | 1.02 | 0.00 | 0.73 | 1.48 | 0.40 | 1.07 | 0.00 |
| 14 | My supervisor does not require me to use the Facebook group page with patients | 6.35 | 1.30 | 0.23 | 1.29 | –0.06 | 0.52 | 0.12 | 0.28 | 1.53 | –0.06 | 0.63 | 0.11 |
| 15 | Although it might be helpful, using the Facebook group page with patients is certainly not compulsory in my job | 6.60 | 0.92 | –0.09 | 1.07 | –0.33 | 0.15 | 0.46 | –0.05 | 1.32 | –0.35 | 0.25 | 0.73 |
| Image | |||||||||||||
| 16 | People in my organization who use the Facebook group page with patients have more prestige than those who do not | 2.79 | 1.41 | –0.31 | 1.78 | –0.71 | 0.09 | 0.13 | –0.51 | 1.74 | –0.91 | –0.12 | 0.01 |
| Job relevance | |||||||||||||
| 17 | In my job, usage of the Facebook group page with patients is important | 3.29 | 1.36 | 0.24 | 1.50 | –0.10 | 0.58 | 0.16 | 0.40 | 1.73 | 0.01 | 0.79 | 0.05 |
| 18 | In my job, usage of the Facebook group page with patients is relevant | 4.26 | 1.44 | 0.56 | 1.68 | 0.19 | 0.94 | 0.00 | 0.38 | 1.77 | –0.02 | 0.78 | 0.06 |
| Output quality | |||||||||||||
| 19 | The quality of the output I get from the Facebook group page is high | 3.97 | 0.94 | 0.78 | 1.31 | 0.49 | 1.08 | 0.00 | 0.81 | 1.33 | 0.51 | 1.11 | 0.00 |
| 20 | I have no problem with the quality of the Facebook group page output | 4.06 | 1.06 | 0.91 | 1.39 | 0.60 | 1.22 | 0.00 | 1.12 | 1.46 | 0.79 | 1.44 | 0.00 |
| Result demonstrability | |||||||||||||
| 21 | I have no difficulty telling others about the results of using the Facebook group page with patients | 4.94 | 1.47 | 0.24 | 1.62 | –0.12 | 0.61 | 0.19 | 0.18 | 1.66 | –0.19 | 0.55 | 0.34 |
| 22 | I believe I could communicate to others the consequences of using the Facebook group page with patients | 5.19 | 1.46 | –0.03 | 1.59 | –0.38 | 0.33 | 0.89 | –0.23 | 1.55 | –0.58 | 0.12 | 0.19 |
| 23 | The results of using the Facebook group page with patients are apparent to me | 4.18 | 1.25 | 0.28 | 1.56 | –0.07 | 0.63 | 0.12 | 0.22 | 1.54 | –0.13 | 0.57 | 0.22 |
| 24 | I would have no difficulty explaining why using the Facebook group page with patients may or may not be beneficial | 5.03 | 1.40 | 0.41 | 1.42 | 0.09 | 0.73 | 0.01 | 0.21 | 1.66 | –0.17 | 0.58 | 0.28 |
CI: confidence interval; SD: standard deviation.
Missing values were imputed using last observation carried forward method; Scores based on 1 = Strongly disagree to 7 = Strongly agree.
Appendix 6.
Practice behavior (theoretical domains framework (TDF)), n = 77.a
| TDF domain |
Baseline |
Absolute change Baseline to 2 weeks |
Absolute change Baseline to 3 months |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Question # | Mean | SD | Mean | SD | 95% CI | p Value | Mean | SD | 95% CI | p Value | |||
| Knowledge | |||||||||||||
| 1 | I am aware of the content and objectives of the Facebook group page | 2.58 | 1.21 | 1.58 | 1.28 | 1.29 | 1.88 | 0.00 | 1.52 | 1.31 | 1.22 | 1.82 | 0.00 |
| 2 | I know the content and objectives of the Facebook group page | 2.26 | 1.07 | 1.69 | 1.23 | 1.41 | 1.97 | 0.00 | 1.74 | 1.23 | 1.46 | 2.02 | 0.00 |
| 3 | I am familiar with the content and objectives of the Facebook group page | 2.27 | 1.10 | 1.60 | 1.26 | 1.31 | 1.88 | 0.00 | 1.77 | 1.23 | 1.49 | 2.05 | 0.00 |
| 4 | I am aware of how to use the Facebook group page to disseminate PGrip with patients | 2.29 | 1.22 | 1.58 | 1.27 | 1.30 | 1.87 | 0.00 | 1.69 | 1.35 | 1.38 | 1.99 | 0.00 |
| Skills | |||||||||||||
| 5 | I have the skills to use the Facebook group page to disseminate PGrip with patients | 3.40 | 1.34 | 0.74 | 1.23 | 0.46 | 1.02 | 0.00 | 0.69 | 1.34 | 0.38 | 0.99 | 0.00 |
| 6 | I have practiced using the Facebook group page to disseminate PGrip with patients | 1.73 | 0.87 | 0.94 | 1.34 | 0.63 | 1.24 | 0.00 | 1.53 | 1.28 | 1.24 | 1.82 | 0.00 |
| Social/professional role and identity | |||||||||||||
| 7 | Using the Facebook group page to disseminate PGrip with patients is part of my work as an arthritis health professional | 2.34 | 0.94 | 0.36 | 1.01 | 0.13 | 0.59 | 0.00 | 0.56 | 1.01 | 0.33 | 0.79 | 0.00 |
| 8 | As an arthritis health professional, it is my job to use the Facebook group page to disseminate PGrip with patients | 2.34 | 1.05 | 0.14 | 1.16 | –0.12 | 0.41 | 0.28 | 0.31 | 1.03 | 0.08 | 0.55 | 0.01 |
| 9 | It is my responsibility as an arthritis health professional to use the Facebook group to disseminate PGrip with patients | 2.45 | 1.06 | 0.14 | 1.43 | –0.18 | 0.47 | 0.38 | 0.34 | 1.02 | 0.11 | 0.57 | 0.01 |
| 10 | Using the Facebook group page to disseminate PGrip with patients is consistent with my job as a health professional | 3.00 | 0.99 | –0.40 | 1.44 | –0.73 | –0.07 | 0.02 | 0.42 | 1.13 | 0.16 | 0.67 | 0.00 |
| Optimism | |||||||||||||
| 11 | I am confident that I can use the Facebook group page to disseminate PGrip with patients even when there is little time | 3.10 | 0.94 | 0.05 | 1.00 | –0.17 | 0.28 | 0.65 | –0.04 | 1.19 | –0.31 | 0.23 | 0.77 |
| 12 | I am confident that if I wanted I could use the Facebook group page to disseminate PGrip with patients | 3.64 | 1.00 | 0.27 | 1.06 | 0.03 | 0.51 | 0.03 | 0.21 | 1.10 | –0.04 | 0.46 | 0.10 |
| 13 | With regard to using the Facebook page to disseminate PGrip with patients in uncertain times, I usually expect the best | 3.19 | 0.81 | 0.27 | 0.79 | 0.09 | 0.45 | 0.00 | 0.30 | 0.93 | 0.09 | 0.51 | 0.01 |
| 14 | With regard to using the Facebook group page to disseminate PGrip with patients I'm always optimistic about the future | 3.56 | 0.80 | 0.12 | 0.76 | –0.06 | 0.29 | 0.18 | 0.25 | 0.89 | 0.04 | 0.45 | 0.02 |
| Beliefs about consequences | |||||||||||||
| 15 | If I use the Facebook page to disseminate PGrip with patients, it will benefit public health | 3.68 | 0.87 | 0.23 | 0.83 | 0.05 | 0.42 | 0.02 | 0.18 | 0.94 | –0.03 | 0.40 | 0.09 |
| 16 | If I use the Facebook group page to disseminate PGrip with patients, it will not have disadvantages for my relationship with them | 3.42 | 0.91 | 0.19 | 0.96 | –0.02 | 0.41 | 0.08 | 0.27 | 1.03 | 0.04 | 0.51 | 0.02 |
| Intentions | |||||||||||||
| 17 | For how many of the next 10 patients do you intend to use the Facebook group page to disseminate PGrip? | 2.64 | 1.51 | 0.09 | 1.23 | –0.19 | 0.37 | 0.52 | 0.29 | 1.46 | –0.05 | 0.62 | 0.09 |
| 18 | I will definitely use the Facebook group page to disseminate PGrip with patients | 3.12 | 0.84 | 0.14 | 0.94 | –0.07 | 0.36 | 0.19 | 0.14 | 0.97 | –0.08 | 0.36 | 0.20 |
| 19 | I intend to use the Facebook group page to disseminate PGrip with patients | 3.32 | 0.90 | 0.29 | 0.97 | 0.07 | 0.51 | 0.01 | 0.19 | 0.97 | –0.03 | 0.42 | 0.08 |
| 20 | How strong is your intention to use the Facebook group page to disseminate PGrip with patients? | 3.10 | 1.02 | 0.12 | 1.09 | –0.13 | 0.36 | 0.35 | –0.08 | 1.16 | –0.34 | 0.18 | 0.56 |
| Memory/attention /decision | |||||||||||||
| 21 | How often do you forget to use the Facebook group page to disseminate PGrip with patients? | 1.92 | 1.00 | 0.58 | 1.15 | 0.32 | 0.85 | 0.00 | 0.73 | 1.24 | 0.45 | 1.01 | 0.00 |
| 22 | When I need to concentrate to use the Facebook group page to disseminate PGrip with patients, I have no trouble focusing my attention | 3.26 | 0.75 | 0.36 | 0.89 | 0.16 | 0.57 | 0.00 | 0.44 | 0.88 | 0.24 | 0.64 | 0.00 |
| 23 | When trying to focus my attention on using the Facebook group page to disseminate PGrip with patients, I have no difficulty blocking out distracting thoughts | 3.29 | 0.84 | 0.44 | 0.85 | 0.25 | 0.63 | 0.00 | 0.55 | 0.93 | 0.34 | 0.76 | 0.00 |
| 24 | When concentrating on using the Facebook group page to disseminate PGrip with patients, I can focus my attention so that I become unaware of what's going on around me | 3.16 | 0.76 | 0.08 | 0.89 | –0.12 | 0.28 | 0.44 | 0.13 | 0.98 | –0.09 | 0.35 | 0.25 |
| Environmental context and resources | |||||||||||||
| 25 | Within the socio-political context (clinical unit) there is sufficient financial support (e.g. from local authorities, insurance companies) for using the Facebook group page to disseminate PGrip with patients | 2.91 | 0.81 | –0.21 | 1.02 | –0.44 | 0.02 | 0.08 | 0.03 | 0.86 | –0.17 | 0.22 | 0.79 |
| 26 | Within the socio-political context (clinical unit) there are good networks between parties involved in using the Facebook group page to disseminate PGrip with patients | 2.84 | 0.76 | 0.04 | 0.98 | –0.18 | 0.26 | 0.73 | 0.12 | 0.90 | –0.09 | 0.32 | 0.26 |
| Social influences | |||||||||||||
| 27 | Most people who are important to me think that I should use the Facebook group page to disseminate PGrip with patients | 2.62 | 0.91 | 0.03 | 0.85 | –0.17 | 0.22 | 0.79 | 0.01 | 0.82 | –0.18 | 0.20 | 0.89 |
| 28 | Most people whose opinion I value would approve me of using the Facebook group page to disseminate PGrip with patients | 3.17 | 0.89 | 0.12 | 0.96 | –0.10 | 0.33 | 0.29 | 0.09 | 1.00 | –0.14 | 0.32 | 0.43 |
CI: confidence interval; PGrip: People Getting a Grip on Arthritis; SD: standard deviation.
One participant did not complete the TDF questionnaire. Additionally one participant provided no responses for question #27 (n = 76).
Scores based on 1 = strongly disagree, 5 = strongly agree; missing values were imputed using last observation carried forward method.
Contributorship
GD, LB, GAW, BD, JK, and JM conceived and designed the feasibility study. GD collected and analyzed the data. BD, JK, GAW, and LB contributed to the methods and review. GD wrote the paper.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
Ethical permission for the feasibility study (H11-12-10) and Advisory Committee meetings (H12-14-07) was obtained from the University of Ottawa Ethics Board. All participants provided informed consent.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors are thankful for the financial support of the Canadian Institutes of Health Research Doctoral Research Award. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. There are no patents, products in development or marketed products to declare.
Guarantor
GD
Peer review
This manuscript was reviewed by Dan Dumbrell, University of Sydney, and one other individual who has chosen to remain anonymous.
References
- 1.Public Health Agency of Canada. Life with arthritis in Canada: A personal and public health challenge, http://www.phac-aspc.gc.ca/cd-mc/arthritis-arthrite/lwaic-vaaac-10/index-eng.php (2010, accessed 11 September 2016).
- 2.Bodenheimer T, Willard-Grace R. The chronic care model and the transformation of primary care. In: Jeffrey IM, Robert FK. (eds). Lifestyle medicine, Switzerland: Springer International Publishing, 2016, pp. 89–96. [Google Scholar]
- 3.Health Council of Canada (2012). Self-management support for Canadians with chronic health conditions: A focus for primary health care. Toronto: Health Council of Canada.
- 4.Ministry of Health B. Self-Management Support: A Health Care Intervention. Victoria, British Columbia, Canada: British Columbia Ministry of Health, https://www.livinghealthynortheast.ca/Portals/0/Documents/Self-Management%20Support%20healt%20care%20intervention%20BC%20MOH%202011.pdf (accessed 6 June 2016).
- 5.Battersby, M, Von Korff M, Schaefer J, et al. Twelve evidence-based principles for implementing self-management support in primary care. Jt Comm J Qual Patient Saf 2010; 36: 561–570. [DOI] [PubMed]
- 6.Aghakhani N, Nia HS, Ranjbar H, et al. Nurses’ attitude to patient education barriers in educational hospitals of Urmia University of Medical Sciences. Iran J Nurs Midwifery Res 2012; 17: 12–15. [PMC free article] [PubMed] [Google Scholar]
- 7.Ritsema TS, Bingenheimer JB, Scholting P, et al. Differences in the delivery of health education to patients with chronic disease by provider type, 2005–2009. Prev Chronic Dis 2014; 11: 130175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balestra M. Clinical patient education challenges and risks. Nurse Pract 2013; 38: 8–11. [DOI] [PubMed] [Google Scholar]
- 9.What is Web 2.0? Webopedia definition 2016, http://www.webopedia.com/TERM/W/Web_2_point_0.html (2016, accessed 6 June 2016).
- 10.Tennant B, Stellefson M, Dodd V, et al. eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers and older adults. J Med Internet Res 2015; 17: e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Government of Canada. eHealth – Health Care System – Health Canada, http://www.hc-sc.gc.ca/hcs-sss/ehealth-esante/index-eng.php (2010, accessed 11 September 2016).
- 12.Stellefson M, Chaney B, Barry AE, et al. Web 2.0 chronic disease self-management for older adults: A systematic review. J Med Internet Res 2013; 15: e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bennett GG, Glasgow RE. The delivery of public health interventions via the Internet: Actualizing their potential. Annu Rev Public Health 2009; 30: 273–292. [DOI] [PubMed] [Google Scholar]
- 14.Pulman A. A patient centred framework for improving LTC quality of life through Web 2.0 technology. Health Informatics J 2010; 16: 15–23. [DOI] [PubMed] [Google Scholar]
- 15.Kind T, Patel PD, Lie DD, et al. Twelve tips for using social media as a medical educator. Med Teach 2014; 36: 284–290. [DOI] [PubMed] [Google Scholar]
- 16.Neiger BL, Thackeray R, Van Wagenen SA, et al. Use of social media in health promotion: Purposes, key performance indicators, and evaluation metrics. Health Promot Pract 2012; 13: 159–164. [DOI] [PubMed] [Google Scholar]
- 17.Bull SS, Levine DK, Black SR, et al. Social media-delivered sexual health intervention: A cluster randomized controlled trial. Am J Prev Med 2012; 43: 467–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chew C, Eysenbach G. Pandemics in the age of Twitter: Content analysis of tweets during the 2009 H1N1 outbreak. PLoS One 2010; 5: e14118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George DR, Dellasega C. Use of social media in graduate-level medical humanities education: Two pilot studies from Penn State College of Medicine. Med Teach 2011; 33: e429–e434. [DOI] [PubMed] [Google Scholar]
- 20.Kaplan AM, Haenlein M. Users of the world, unite! The challenges and opportunities of Social Media. Bus Horiz 2010; 53: 59–68. [Google Scholar]
- 21.Facebook. Facebook Newsroom–Company Info, http://newsroom.fb.com/company-info/ (accessed 6 June 2016).
- 22.Andersen NB and Söderqvist T. Social media and public health research. Frederiksberg (Denmark), http://www.museion.ku.dk/wp-content/uploads/FINAL-Social-Media-and-Public-Health-Research.pdf (2012, accessed 6 June 2016).
- 23.Laliberté M, Beaulieu-Poulin C, Campeau Larrivée A, et al. Current uses (and potential misuses) of facebook: An online survey in physiotherapy. Physiother Canada 2016; 68: 5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamm MP, Chisholm A, Shulhan J, et al. Social media use by health care professionals and trainees: A scoping review. Acad Med 2013; 88: 1376–1383. [DOI] [PubMed] [Google Scholar]
- 25.McGowan BS, Wasko M, Vartabedian BS, et al. Understanding the factors that influence the adoption and meaningful use of social media by physicians to share medical information. J Med Internet Res 2012; 14: e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giordano C, Giordano C. Health professions students’ use of social media. J Allied Health 2011; 40: 78–81. [PubMed] [Google Scholar]
- 27.Peluchette JVE, Karl K, Fertig J. A Facebook “friend” request from the boss: Too close for comfort? Bus Horiz 2013; 56: 291–300. [Google Scholar]
- 28.Brosseau L, Lineker S, Bell M, et al. People getting a grip on arthritis: A knowledge transfer strategy to empower patients with rheumatoid arthritis and osteoarthritis. Health Educ J 2012; 71: 255–267. [Google Scholar]
- 29.The Arthritis Society. People getting a grip on arthritis - videos, http://arthritis.ca/manage-arthritis/educational-resources-tools/people-getting-a-grip-on-arthritis-videos (2016, accessed 6 June 2016).
- 30.Standford School of Medicine. Online healthier living with arthritis – patient education – Department of Medicine. Better Choice, Better Health ©Arthritisor Healthier Living With Arthritis (Internet Arthritis Self-Management Program), http://patienteducation.stanford.edu/internet/arthritisol.html (2016, accessed 6 June 2016).
- 31.Lorig KR, Ritter PL, Laurent DD, et al. The Internet-based arthritis self-management program: A one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Care Res 2008; 59: 1009–1017. [DOI] [PubMed] [Google Scholar]
- 32.Willis E. The making of expert patients: The role of online health communities in arthritis self-management. J Health Psychol 2014; 19: 1613–1625. [DOI] [PubMed] [Google Scholar]
- 33.Brosseau L, Wells GA, Brooks S, et al. People getting a grip on arthritis II: An innovative strategy to implement clinical practice guidelines for rheumatoid arthritis and osteoarthritis patients through Facebook. Health Educ J 2014; 73: 109–125. [Google Scholar]
- 34.Trudeau KJ, Pujol LA, DasMahapatra P, et al. A randomized controlled trial of an online self-management program for adults with arthritis pain. J Behav Med 2015; 38: 483–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Manage Sci 2000; 46: 186–204. [Google Scholar]
- 36.Huijg JM, Gebhardt WA, Crone MR, et al. Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement Sci 2014; 9: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brosseau L. Ottawa Panel evidence-based clinical practice guidelines for therapeutic exercises in the management of rheumatoid arthritis in adults. Phys Ther 2004; 84: 934–972. [PubMed] [Google Scholar]
- 38.Brosseau L, Wells GA, Tugwell P, et al. Ottawa Panel evidence-based clinical practice guidelines for electrotherapy and thermotherapy interventions in the management of rheumatoid arthritis in adults. Phys Ther 2004; 84: 1016–1043. [PubMed] [Google Scholar]
- 39.Brosseau L, Wells GA, Tugwell P, et al. Ottawa Panel evidence-based clinical practice guidelines for therapeutic exercises and manual therapy in the management of osteoarthritis. Phys Ther 2005; 85: 907–971. [PubMed] [Google Scholar]
- 40.Brosseau L, Egan M, Wells GA, et al. Ottawa Panel evidence-based clinical practice guidelines for patient education programmes in the management of osteoarthritis. Health Educ J 2011; 70: 318–358. [Google Scholar]
- 41.Brosseau L, Wells GA, Tugwell P, et al. Ottawa Panel evidence-based clinical practice guidelines for the management of osteoarthritis in adults who are obese or overweight. Phys Ther 2011; 91: 843–861. [DOI] [PubMed] [Google Scholar]
- 42.Loew L, Brosseau L, Wells GA, et al. Ottawa Panel evidence-based clinical practice guidelines for aerobic walking programs in the management of osteoarthritis. Arch Phys Med Rehabil 2012; 93: 1269–1285. [DOI] [PubMed] [Google Scholar]
- 43.Poitras S, Avouac J, Rossignol M, et al. A critical appraisal of guidelines for the management of knee osteoarthritis using appraisal of guidelines research and evaluation criteria. Arthritis Res Ther 2007; 9: R126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hurkmans EJ, van der Giesen FJ, Bloo H, et al. Physiotherapy in rheumatoid arthritis: Development of a practice guideline. Acta Reum Port 2011; 36: 146–158. [PubMed] [Google Scholar]
- 45.Brosseau L, Rahman P, Poitras S, et al. A systematic critical appraisal of non-pharmacological management of rheumatoid arthritis with appraisal of guidelines for research and evaluation II. PLoS One 2014; 9: e95369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brosseau L, Rahman P, Toupin-April K, et al. A systematic critical appraisal for non-pharmacological management of osteoarthritis using the appraisal of guidelines research and evaluation II instrument. PLoS One 2014; 9. doi: 10.1371/journal.pone.0082986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nelson AE, Allen KD, Golightly YM, et al. A systematic review of recommendations and guidelines for the management of osteoarthritis: The chronic osteoarthritis management initiative of the U.S. bone and joint initiative. Semin Arthritis Rheum 2014; 43: 701–712. [DOI] [PubMed] [Google Scholar]
- 48.AGREE. The Appraisal of Guidelines for Research and Evaluation (AGREE) instrument, http://www.agreetrust.org/ (accessed 10 June 2016).
- 49.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 1989; 13: 319. [Google Scholar]
- 50.FluidSurveys. FluidSurveys, http://fluidsurveys.com/ (accessed 6 June 2016).
- 51.Wu M-Y, Chou H-P, Weng Y-C, et al. TAM2-based Study of Website User Behaviour – Using Web 2.0 Websites as an Example. WSEAS Transactions on Business and Economics 2011; 8: 133–151.
- 52.Sussman S. Translation in the health professions: Converting science into action. Eval Health Prof 2006; 29: 7–32. [DOI] [PubMed] [Google Scholar]
- 53.Narayanaswami P, Weiss M, Selcen D, et al. Evidence-based guideline summary: Diagnosis and treatment of limb-girdle and distal dystrophies: Report of the Guideline Development Subcommittee of the American Academy of Neurology and the Practice Issues Review Panel of the American Association of Neurology. Neurology 2014; 83: 1453–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Farnan JM, Sulmasy LS, Worster BK, et al. Online medical professionalism: Patient and public relationships: Policy statement from the American College of Physicians and the federation of State Medical Boards. Ann Intern Med 2013; 158: 620–627. [DOI] [PubMed] [Google Scholar]
- 55.White J, Kirwan P, Lai K, et al. “Have you seen what is on Facebook?” The use of social networking software by healthcare professions students. BMJ Open 2013; 3: e003013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Venkatesh V, Morris MG, Davis GB, et al. User acceptance of information technology: Toward a unified view. MIS Q 2003; 27: 425–478. [Google Scholar]
- 57.Venkatesh V, Ramesh V. Web and wireless site usability: Understanding differences and modeling use. MIS Q 2006; 30: 181–206. [Google Scholar]
- 58.French SD, Green SE, O’Connor DA, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: A systematic approach using the theoretical domains framework. Implement Sci 2012; 7: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: A consensus approach. Qual Saf Health Care 2005; 14: 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fox S and Purcell K. Chronic disease and the internet. Washington DC: Pew Research Center's Internet & American Life Project, http://www.pewinternet.org/files/old-media/Files/Reports/2010/PIP_Chronic_Disease_with_topline.pdf (2010, accessed on June 6, 2016).
- 61.Zickuhr K, Madden M. Older adults and Internet use. Pew Res Cent 2012. org/Reports/2012/Older-adults-and-internet-use. aspx. 2012. [Google Scholar]
- 62.Cooper CP, Gelb CA, Rim SH, et al. Physicians who use social media and other Internet-based communication technologies. J Am Med Informatics Assoc 2012; 19: 960–964. [DOI] [PMC free article] [PubMed] [Google Scholar]