Abstract
Introduction
Patients Know Best (PKB) provides a patient portal with integrated, patient-controlled digital care records. Patient-controlled personal health records facilitate coordinated management of chronic disease through improved communications among, and about, patients across professional and organisational boundaries. An NHS foundation trust hospital has used PKB to support self-management in patients with inflammatory bowel disease; this paper presents a case study of usage.
Methods
The stakeholder empowered adoption model provided a framework for consulting variously placed stakeholders. Qualitative interviews with clinical stakeholders and a patient survey.
Results
Clinicians reported PKB to have enabled a new way of managing stable patients, this facilitated clinical and cost effective use of specialist nurses; improved two-way communications, and more optimal use of outpatient appointments and consultant time. The portal also facilitated a single, rationalised pathway for stable patients, enabling access to information and pro-active support. For patients, the system was a source of support when unwell and facilitated improved communication with specialists. Three main barriers to adoption were identified; these related to concerns over security, risk averse attitudes of users and problems with data integration.
Conclusions
Patient-controlled personal health records offer significant potential in supporting self-management. Digital connection to healthcare can help patients to understand their condition better and access appropriate, timely clinical advice.
Keywords: Integrated digital care record, self-management, long-term conditions, digital health adoption, PHRs, e-health, electronic patient-controlled health record, electronic personal health record, patient reported outcomes, irritable bowel disease
Introduction
Patient held personal health records (PHRs) are recognised as ‘a convenient tool to help patients organize their health information so that multiple medical professionals can share the information effectively’.1 The most advanced PHRs contain all health (and possibly social care) information for that individual. However, many systems offer partial functionality, within a single service or department. Nonetheless, this functionality is a significant improvement on paper based systems, where input from the different users cannot be easily captured and shared dynamically. Notwithstanding, as noted by Kelsey,2 ‘the online revolution that has transformed so much of the rest of our lives does not support us nearly well enough as patients, citizens or caregivers’.
This paper examines usage of an electronic patient held PHR known as Patients Know Best (PKB). Consideration of the use of electronic PHRs is timely due to the UK policy initiative that ‘all patient and care records will be digital, real-time and interoperable by 2020’.3
Previous studies of electronic PHRs have highlighted a host of benefits. Electronic PHRs have been found to facilitate the integration of information from different systems1 and to have enabled better coordination and communication of information to improve patient care.1,4 PHRs allow improved communications among and about patients across professional and organisational boundaries, which facilitates coordinated management of chronic disease and reductions in duplicated procedures and prescription errors.1,4–6 Communications between patients and providers are also improved.7 Further, it has been found that patient usage of PHRs improves patient knowledge of their condition,7as well as compliance to treatment and to drug regime,8 to the extent that patients become active participants in their own health care.1,4,7,9 PHRs lead to improved patient self-management.7,10–13
PKB is an integrated patient portal and information exchange system that aims to help clinicians share information, engage with patients and to empower patients to manage their care. Patient portals tend to be provider-tethered applications that enable patient access to selected health information that is produced and managed by a healthcare provider.11 This means that some portals allow patient access to health information but not control of it.13 The PKB PHR system differs by offering a range of features, some of which allow patient interaction and control. When fully integrated with hospital information systems PKB facilitates self-management by allowing patients to interact with care plans, medication regimes and information libraries via the portal. PKB is internet based and can be accessed securely via mobile devices and personal computers. PKB allows communication via video-conferencing and through secure messaging using the UK National Health Service (NHS) N3 network; data is encrypted for transfer and storage. Patients can upload information to their record and can access lab results and letters from the provider. Further, in PKB the patient controls their personal record and can permit access to others thus overcoming technico-legal difficulties in sharing access across health providers and organisational boundaries. Therefore, PKB combines portal access with an electronic, integrated, PHR.
The PKB PHR system has been used with inflammatory bowel disease (IBD) patients in the Gastroenterology Department of an English NHS Foundation Trust Hospital (Trust1) since late 2013; three factors prompted use:
Trust1 were participants in the national Inflammatory Bowel Disease Registry (a large patient database ‘set up to provide the first ever UK-wide repository of pseudonymised IBD adult and paediatric patient data for prospective audit and research purposes’);14 clinicians wanted to enable patient access to personal information held on the registry.
People with IBD can experience periods of severe symptoms (flare-ups), as well as long periods of ‘remission’ when they have few or no symptoms at all. Clinicians wanted an improved system for managing patients in remission (i.e. stable patients), instead of continuing outpatient care or discharge to primary care. Clinicians were aware of a variety of issues relating to patient care in the community such as: patients being lost to follow up; maintenance therapy not being continued; GPs stopping prophylactic therapy; patients believing they no longer had IBD; and patients feeling ‘not wanted’ and ‘unloved’. These issues had resulted in patients being re-referred to Trust1 with significant flare-ups.
Clinicians wanted to support patients to self-manage their condition.
Consequently, Trust1 desired a new approach to the management of stable IBD patients that would be proactive; improve the integration of primary and secondary care; and provide patients with a ‘safe and efficient’ self-management system. Self-management can be an effective way for IBD patients to maintain a full and healthy lifestyle, whilst maximising their quality of life. The National IBD Standard (2013) supports the notion that this is best achieved by using specialists to help support, guide and empower patients to better self-manage.15 So to support self-management Trust1 devised a new system comprised of: a functional database (the National IBD Registry); condition monitoring via virtual clinics and faecal calprotectin tests (recommended by NICE to ‘help doctors distinguish between inflammatory bowel diseases’);16 and a communication portal – provided by PKB.
The PKB PHR system was central to the new management system at Trust1 wherein patients choosing to activate a PHR would be provided with a secure and safe personalised website facilitating worldwide access to: a library of advice leaflets; instant IBD symptomatic assessment with direct alert system to the IBD Team and rapid response management advice; and a portal of access to hospital specialists. Further, the planned integration of the PKB PHR system with the National IBD Registry and with hospital records would, when established, allow patients to view, and share with others, their health information and test results. Taken together these aspects of PKB would help Trust1 reach elements of IBD Standards A, C, D, E.15 At the time this study was conducted, full integration of PKB with hospital records and the National IBD Registry had not been completed.
The authors were commissioned by PKB to work with them and a senior gastroenterologist at Trust1 in order to understand from the viewpoint of user stakeholders the barriers to and benefits from using the PKB PHR system, and to share these findings with the aim of facilitating wider adoption of the technology. This work is presented here as a case study.
Methods
This technology adoption study employed the stakeholder empowered adoption model (StEAM),17 which was developed to overcome the difficulties experienced in digital health adoption, scale-up and implementation. Many pilots are undertaken and evaluated, but frequently produce evidence that is not appropriate to decision-making. Stakeholder perspectives can be neglected, but frequently are at the root of barriers to adoption and implementation. The StEAM model provides a framework for consulting all stakeholders, in four categories: professional users, patient users (user stakeholders), organisational management and technology supplier (economic stakeholders), to inform the design of the study by seeking to understand what measures of success are required. Measures of success tend to be specific to the different stakeholder groups. In particular, the attitudes and requirements of professional staff – and their roles in advocacy, service development and improvement – are often neglected. Enabling all stakeholders to understand perspectives of the other stakeholder groups can also be extremely powerful in driving change.
Timescale
The study was undertaken over four months beginning November 2014.
Study preliminaries
Initial planning meetings were held with PKB, Trust1 and a representative of Trust1’s Clinical Commissioning Group in order to identify what measures of success were required. These meetings informed the design of the study and a study protocol was then developed and submitted to Trust1 in December 2014. In mid-January 2015 the study was approved as a service evaluation with agreed procedures for access to relevant staff and anonymised patients. Data collection was undertaken during January and February 2015 using semi-structured interviews with clinical stakeholders and a patient survey.
Semi-structured interviews
Semi-structured interviews were chosen in order to facilitate the collection of in-depth data in a short timeframe. Semi-structured interviews allow for guided yet open, two-way discussions wherein interviewees are able to introduce evidence they perceive to be important The interview schedule, used with all interviewees, involved eight questions designed to encourage discussion about (i) interviewees’ expectations compared to the reality of using PKB; (ii) the impacts of PKB use (negative and/or positive) on different stakeholders (i.e.: interviewees, patients and hospital department/organisation), (iii) pitfalls and potential barriers to adoption. The interview schedule was designed to facilitate data collection along general themes but from particular stakeholder perspectives and to encourage the introduction of new ideas.
The research team aimed to gather data from user stakeholders; PKB wanted to understand the factors effecting uptake after their product had been commissioned. In terms of clinical stakeholders, seven potential interviewees with user experience of PKB were identified by the gastroenterologist at Trust1 and by PKB (four consultant gastroenterologists and three IBD nurse specialists); of these five were available for a telephone interview within the timescale of the study: one consultant gastroenterologist (CGT1 – duration: 80 min) and two IBD nurse specialists from Trust1 (IBDNS1T1 and IBDNS2T1 – one interview, duration: 35 min). An introduction was also given to a second trust (Trust2) by PKB; this trust was also using the PKB PHR system and one telephone interview was conducted with an IBD nurse specialist referred to here as IBDNS3T2 (duration: 25 min). The planning meeting with the commissioner from Trust1 was face-to-face and lasted forty minutes. All interviews and meetings were recorded and transcribed then analysed by the authors with the aim of identifying themes and areas of congruence as well as dissensus; direct quotations from transcripts are used here to illustrate these key themes.
Patient e-survey
Interviews with patients were not in scope due to time and funding restrictions and so a patient e-survey was chosen. Survey questions were informed by the statements made by economic and clinical stakeholders during planning meetings and in interviews; these related to specific features of the PKB PHR system and the perceived benefits of use. The aim was to test the validity of clinical stakeholders’ perceptions of benefits. The e-survey is described below.18
The survey, which was constructed using Bristol Online Surveys,19 took about 15 min to complete and included mostly ‘tick-box’ type questions together with places to add comments if desired – survey questions can be found in the supplementary file to this paper. Staff at PKB and our contact at Trust1 commented upon the survey during development; they and colleagues tested it later. In early February 2015, a letter and survey link was sent out by PKB, via MailChimp,20 to the last known email address of all patients (N = 544) of Trust1 with PHRs – the researchers did not have access to the email addresses or any personal data. The accompanying letter explained: the reasons for the study; why the person was asked to take part; that participation was entirely voluntary; that all survey responses were anonymous and stored on a password protected computer on a password protected network in an encrypted folder. It also made clear that only members of the research team would have access to the data and that it would be written into a summary report for PKB and a paper for submission to an academic journal. Details of the investigators, who to contact to ask questions and who to complain to were given. Participants were advised that by clicking on the link they were giving their permission for members of the evaluation team to analyse answers and quote anonymous responses.
The initial response rate was low; the email was opened by 323 of the 544 addresses and prompted only 23 responses. A reminder email was sent one week later which prompted 17 more responses and a final reminder was sent one week after the second and prompted a further 16 responses. This gave a total of 56 completed surveys and a response rate of just over 17% of emails opened. Consequently, the quantitative data gathered was subjected to basic descriptive analysis only (i.e. frequencies); qualitative data was collated according to the quantitative responses and considered in that light.
PKB data
PKB supplied us with data on patient registration involving monthly totals of patients invited to sign up accounts and the numbers doing so. No data was available at individual level.
Literature search
A literature search was undertaken in order to gain an understanding of best practice and the state of the art in use of electronic, patient held PHRs, the benefits to stakeholders and challenges in implementation. Using library search engines (including Dawsonera, OneSearch and Quest) we searched for a variety of keywords/phrases: personal health records, PHR, electronic health record, EHR, electronic medical record, electronic patient record, e-health, personally controlled health record/medical record.
The clinical context was also reviewed to enable the researchers to understand scenarios and stories provided by interviewees. This literature was largely provided by the consultant (CGT1), with further examination of related references. A key document was the IBD Framework, this was used to provide a context for understanding the patient management system at Trust1 and why the PKB PHR System in Trust1 was customised as it was.
In the next section we report the perspectives of clinical stakeholders.
Results
The views of clinical user stakeholders
Clinical users were enthusiastic and cited many benefits to both the department and patients from PKB usage. Most significant was that it facilitated a new way of dealing with stable disease and had enabled an innovative two-tiered system of patient management:
One group of patients who have to be seen through the so-called Rolls Royce outpatients appointment and then another group of patients who are more stable and need to be over-viewed by a specialist but they don’t really need that full on hospital based, face-to-face, outpatients appointment. (CGT1)
Stable patients participated in a twice yearly virtual, telephone clinic and in between times were invited to undertake an IBD symptomatic assessment via PKB. This method of patient management was said by clinical team members at Trust1 to release outpatient appointments to be used for acute patients or emergency admissions and to reduce waiting times:
We’re getting more of those who need to be seen and less of those who come to say hello. Definitely. And that’s what clinics should be for. (IBDNS1T1)
The new management system therefore allowed more optimal use of staff time with consultants concentrating on acute care whilst nurse specialists took over responsibility for the monitoring and management of stable patients:
We’re not getting rid of work, the work is moving sideways … But rather than it being coordinated through doctors we’ve got some very experienced IBD nurses who manage this service and if necessary will discuss it with the consultants. (CGT1).
Further, clinicians considered the IBD symptomatic assessment facility within PKB very important. Building on the PKB ‘Symptom Tracker’ Trust1 designed a ‘traffic light’ system wherein patients were prompted to rate their symptoms on thirteen clinical indicators twice yearly (see the example screenshot in Figure 1). An underlying algorithm, designed and clinically validated by the lead consultant, combined the responses and converted them into a disease activity score which then produced a rating of red, amber or green. The scoring was designed to differentiate between ‘flare-ups’ and ‘irritable bowel disease’:
We’ve tried to set it up so those who have irritable symptoms don’t score highly, so they may be scoring lots of reds but that won’t necessarily create an alert for us. (CGT1)
In the majority of cases the rating produced was ‘green’ so no further action was taken, beyond a simple message and reference to educational materials stored in the PKB library. Alternatively, an amber or red rating sent an alert to the IBD nurse specialists at the hospital with red ratings prompting telephone contact. The scoring system had been set relatively low to optimize the prevention of flare-ups and it was noted that a red alert usually resulted in a change of patient management. It was said that patients could, and did, use this facility when unwell prompting reassurance or proactive support depending on the score. Consequently, the traffic light system facilitated patient access to more immediate specialist assistance and replaced a process that would previously have involved hospital visits.
Figure 1.
Example PKB symptom monitoring page.
Improved communication was another key benefit identified. Clinicians asserted that improved communication had contributed to reduced emergency outpatient appointments amongst stable patients; the explanation being that as patients were no longer fully ‘discharged’ then lines of communication remained open. The facility to mass message users was welcomed, as was freedom from being tied to telephone communications. Opinions differed as to whether email communication saved time when compared to telephone communications, IBNS3T2 believed email to be quicker: “when you phone them you usually get involved in a longer conversation about something else”. Alternatively, for IBDNS1T1 and IBDNS2T1 savings in time were not as clear cut:
The phone call you get it over and done with, the PKB ones, they come back with another question and you can have multiple conversations in one day rather than get it over and done with. But then it’s also much more to the point, there’s less waffle.
Hence, clinical stakeholders at Trust1 reported a range of benefits that had been produced through PKB usage. In summary, PKB was said to have enabled a new way of managing stable patients which then facilitated: more optimal use of outpatient appointments and consultants’ time, clinical and cost effective use of specialist nurses, and improved two-way communication.
Perceived benefits to patients
The clinical users identified a number of benefits to patients and provided anecdotal evidence in their feedback. Primarily, the intervention enabled development of a rationalised patient pathway channelled through one access point:
The website [PKB portal] offers an umbilical cord really, a connection to us in the hospital so that [patients] know they’ve got instant access if they need it, and that offers them a support crutch. (CGT1)
Improved access to specialist support was believed to facilitate increased patient confidence, so:
Although they’re being transferred to the community they still have that connection to us and so they feel more confident in taking on self-management in the first place. (CGT1)
Accordingly, this led patients to ‘own’ their condition:
One of the big problems we have in IBD is patients accepting that they have a long term condition and then adjusting their lifestyle around that and when someone comes in for hospital appointments it’s almost like it’s someone else’s problem that they have to deal with; it’s not their disease, so this focusses people’s attention. (CGT1)
Moreover, the act of owning one’s condition together with ongoing monitoring was seen to lead to greater compliance with medication regimes. Consequently, PKB was said to have contributed to improved levels of self-management and patient empowerment and this was believed to have resulted in increased mobility for patients and allowed them to lead ‘normal lives’:
Because this is a web based programme we’ve been contacted by people with flare ups on cruise ships in the Mediterranean; we’ve been contacted by people who had been admitted to other hospitals who are checking if their new medication clashed with the IBD medication; we’ve had people getting married [abroad] who couldn’t speak [the language] and were able to open their website and the GP understood some of the medical terminology and was able to treat their flare. (CGT1)
Email communication was perceived to have facilitated more openness and frank discussion from patients due to them feeling less inhibited online than in face-to-face situations or on the telephone; this was thought especially the case with younger patients and some male patients (all interviewees).
PKB was also thought to be particularly beneficial for patients with co-morbidities and the facility for them to share their record with others was viewed as extremely important:
This jumping between hospitals, between their local hospital and their tertiary referral unit, their specialist unit, is a prime example of how PKB works its magic and works best; shared records seen between two hospitals. I get stuff sent out from other hospitals; I’ll be lucky if I see those in several months. If it were shared with the patient directly, that information would be available to each group instantly – provided the patient is happy to share. (CGT1)
Last, it was said that patients benefitted from the ‘convenience’ of not attending hospital appointments that PKB had facilitated:
… at a point in time where that patient is completely well and has been for the last year, and who finds it rather frustrating to have to come in and battle for a car parking space, pay £8 for the delight of parking there, to wait another hour because [the doctor’s] clinic has overrun and for me to tell him that there’s nothing wrong and to wave him off until the next six-month clinic. (CGT1)
In summary then, clinical stakeholders reported that the PKB PHR system had improved accessibility and facilitated a single, rationalised pathway for stable IBD patients to access information and pro-active support which led to patient empowerment: increased patient confidence (not alone); increased ownership of condition; increased compliance with medication regimes; increased self-management.
Whilst respondents to the survey reported benefits from PKB most did not report positive changes to their health management as a consequence of usage and therefore contradicted the perspectives of clinicians at Trust1. For instance, most were not: ‘more aware of health changes’ (39 respondents from N = 56), ‘better able to manage their condition’ (41), nor ‘better able to make health decisions’ (41). Further most did not have ‘greater understanding of their health condition’ (40), follow ‘medication more closely’ (42), ‘feel more in control’ of their IBD (42), experience ‘fewer flares’ (45) or have ‘fewer appointments’ (45). It may be that some respondents were already self-efficacious with regards their IBD management and so did not perceive PKB usage to have altered this. However, some respondents were sceptical as to whether a patient portal could prompt such changes:
This implies that a website is a medical tool to control the conditions!!! (White British male, age missing)
I fail to see correlation between using website and flare-ups … Using website not going to stop flare-up. (White British female, aged 65–74 years)
Nonetheless, patients corroborated the clinician perception that PKB was a source of support for those feeling unwell and facilitated improved communication with IBD specialists. In terms of accessing support via the portal, 23 respondents reported logging in at least once a month and a further 12 at least once a year. Six reported that they logged in on an ‘as needed’ basis, for example: “Often when unwell but rarely when in remission” and “Just when necessary for consolation and help” (see Table 1).
Table 1.
Frequency of logins to PKB personal health record.
| n | % | |
|---|---|---|
| Other | 21 | 37.5 |
| At least once a year | 12 | 21.4 |
| At least once a month | 17 | 30.4 |
| At least once a week | 5 | 8.9 |
| At least once a day | 1 | 1.8 |

| ||
Patients were positive about the PKB facility to communicate with specialists: 35 respondents reported having found it easier to contact and communicate with specialist staff (only 6 had not); 11 respondents used PKB to communicate at least once a month and 15 at least once a year; 18 respondents had never used PKB to communicate with specialist staff (see Table 2).
Table 2.
Frequency of logins to communicate with health professionals.
| n | % | |
|---|---|---|
| Other | 12 | 21.40 |
| Never | 18 | 32.10 |
| At least once a year | 15 | 26.80 |
| At least once a month | 7 | 12.50 |
| At least once a week | 4 | 7.10 |
| At least once a day | 0 | 0 |
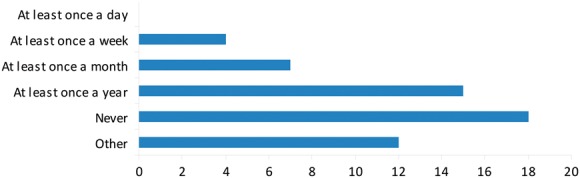
| ||
Of the 12 that answered ‘other’, seven reported communicating via PKB on an ‘as needed’ basis, for example: “More regularly when having tests/have active disease”; “When I have a flare”; “When specific advice is needed”. Patients appeared to value the facility to contact specialists via secure messaging:
Communicating with professionals was a god send during a period of having hospital tests and getting a diagnosis. (White British male, aged 55–64 years)
It was extremely useful during my flare and I could contact my IBD nurse easily and communicate symptoms I may have found uncomfortable to discuss by phone. (White British female, aged 45–54 years)
I feel that there is direct response from professionals that was lacking by visiting my own GP who didn't seem too familiar with the condition. (White British female, aged 45–54 years)
Contacting professionals has given me more confidence to begin to deal with my symptoms. (White British male, aged 55–64 years)
PKB data showed the proportion of patients signing up to PKB to be high. In the period April 2014 to February 2015 of the 177 people invited to register for a PKB PHR 172 (97%) did so; at the time of the study there were 544 patients registered. Survey respondents were asked about changes to their usage over time (Table 3).
Table 3.
Changes in usage of PKB over time.
| n | % | |
|---|---|---|
| Prefer not to say | 9 | 16.10 |
| The amount of time has decreased | 17 | 30.40 |
| The amount of time I spend has stayed the same | 24 | 42.90 |
| The amount of time I spend has increased | 6 | 10.70 |

| ||
Five of the 17 respondents whose usage had decreased reported this was because of an improvement to their health. Of the six whose usage had increased two mentioned it had so because they were unwell. The usage of 24 respondents had remained the same. Most respondents reported being familiar with computers and internet technology (50) and of these 25 agreed that PKB was easy to us. However, 13 patients did not and were either critical of the site or gave feedback on specific design and usability issues. Notwithstanding, the inability to view personal data due to the lack of integration with existing systems seems to have been the most significant reason for reduced usage with many comments being made about this throughout the survey, for example: “Couldn’t work out why it was useful to me”; “It’s a framework with little information relevant to me”; “Logged on once and couldn’t work out how it could be useful to me”.
With regards to specific features of PKB, 24 respondents reported being aware of the facility to share their health record with others yet only one had done so (with their GP). Only 24 respondents reported using the IBD symptomatic assessment facility whilst 23 reported never having used it. (Some survey respondents were relatively new to the system and may not yet have been invited to use this facility.) Further, there was little comment from patients with regards the information library, although 24 of the respondents indicated that they had used this feature and 11 used it once a month or more. Again, this could simply be because respondents were already knowledgeable on their condition, for example: “I researched it thoroughly when originally diagnosed” and “I have done extensive research on the web”.
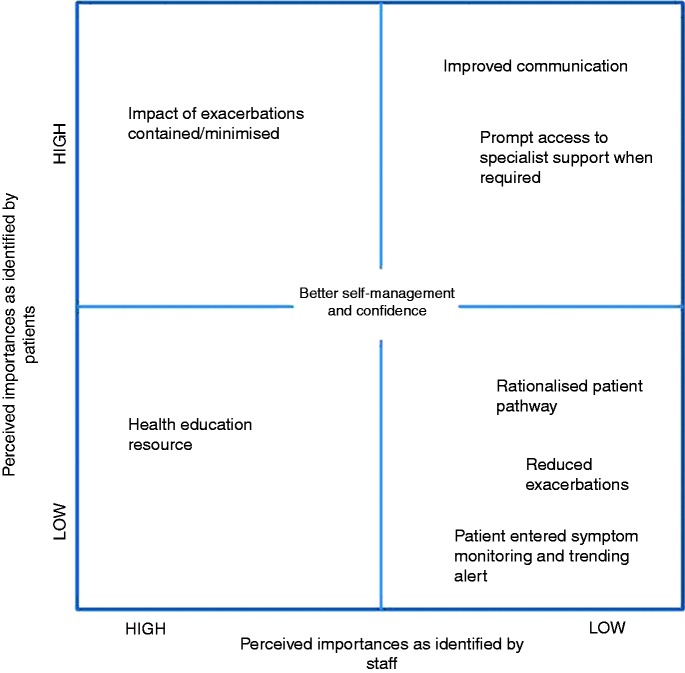
What is clear from our analysis is that the different types of user place different values on the beneficial features of PHRs and of the PKB system; patients valued improved communications and prompt access to specialist support most whilst clinical users at Trust1 most valued the new method of patient management which they believed led to reduced exacerbations (see Figure 2).
Figure 2.
The key features of the PKB PHR system are shown graphically in terms of their perceived importance to the different stakeholder groups.
N.B. The benefits may be greater to patients than they perceive; however, patient perception limits the use of certain features.
Barriers to adoption
Security
When asked to think again about the prospect of using an externally provided health record system clinicians recalled security as their main concern. They were aware that concerns over security might hinder adoption of the system by the hospital trust and use by patients. However, clinicians were reassured by the fact that PKB passed all relevant checks:
It was the Government assessment that they were safe and our information governance people went and checked them to make sure it was safe and the IT department … So it wasn’t just picking something out of an App store; there were lots of people involved. (IBDNS1T1)
Patients also expressed concerns about data security, privacy and confidentiality:
Not sure how secure data is on this site. (White British Male, age missing)
Can press hack it? How do I know it’s safe to put my results automatically on system? (White British female, 45–54 years)
Confidentiality – as with all online health records (White British female, 45–54 years)
Data security is clearly a concern heightened by high profile cases reported in the press and perceptions of risks around this factor should not be underestimated. Although there was no suggestion that there was an issue with PKB’s solution, this highlights the importance of not only being secure, but also being seen to be secure.
Engaging users: perceptions and pre-conceptions
Changing processes within the NHS is complex and requires involvement, commitment and approval from variously placed actors. In this case, as in many others, getting senior management approval of a clinician led innovation “was a hurdle in itself” (CGT1). Co-operation from the IT department was reported as being very important and two factors assisted this cooperation: PKB did most of the development, and the development was externally funded through a research grant.
Getting senior clinicians to use PKB was particularly problematic; their reluctance was thought to be due to the belief it would create extra work. When PKB was first introduced to Trust2, IBDNS3T2 was “really, really worried about the amount of work that it would generate”; as were colleagues: “We had a big gastroenterology MDT meeting and we thought that if the medium was there to be contacted all the time that [patients] may contact you more than they normally would.” In practice this fear was not well-founded, using PKB had “not been as onerous” and an increase in contacts never happened (IBDNS3T2). Moreover, whilst the potential of PKB to facilitate multidisciplinary working was recognised the thought of increased workload prevented this:
We were hoping that the dietetic team would use it a bit more because a lot of the queries we get are about diet and I think our dietician came on board but I think they had the same fears as the consultants, that this will be a lot more work. But actually, once all the diet sheets, advice, are loaded up that would actually be a really good medium for passing information. (IBDNS3T2)
Patient engagement was also an issue. Clinicians at Trust1 had used a combination of reassurance and encouragement to foster patient engagement:
Reassurance: We don’t push anyone, this is something we offer the patients and if they’re keen to try it they know that they have a lifeline to come straight back into clinic if needs be.
Encouragement: … patient nights where we teach patients about how to use the system … I think that when some of the uncertain patients start to hear from … other patients using this system that will give them the confidence to maybe try it themselves (CGT1)
Nevertheless, disappointment was expressed that fewer patients than hoped were using the system; it was thought some patients were “nervous of taking over some degree of control” (CGT1). It was also apparent that the severity of patient condition impacted upon usage. At Trust2, PKB was trialled with acute patients (i.e. those with active IBD) but in retrospect this was thought a mistake as acute patients have less need of patient portals:
These patients are in hospital every eight weeks for infusions and things anyway so they … use that opportunity to ask questions. It’s been used for changing appointments and just general advice but not to the extent that we thought it would be used. I think it would be better used in a population that aren’t coming into hospital so frequently anyway. (IBDNS3T2)
In addition, Trust2 served a population in close proximity and it was said this made PKB seem less relevant to patients (IBDNS3T2).
Data integration
The full functionality of the PKB patient portal required integration with existing information systems, a resource-intensive task that could not be given priority in either Trust. Similarly, integration with the externally held national IBD registry,14 which had been delayed at Trust1, was being tested at the time of the study:
We’ve got a bit of fine tuning because essentially … there’s a lot of information on there, all the patient letters, screening, MDT outcomes, community screening, cancer surgery, diagnosis, systemic disease scores. There’s a lot of information constantly topped up, every time you see them; the phone calls that go on. So basically we wanted them to have all of that information; it’s a case of finding, mapping; this piece of data is on this site and we want it put on this area of this site. So at the moment they’re making sure that the mapping process is effective (CGT1).
Notwithstanding, at the time of writing integration at Trust1 had still not occurred, which we note as a limitation.
Similarly, integration with the existing systems at Trust2 had not happened as hoped at the time of data collection; this was thought to have limited patient use and engagement:
The interface was supposed to happen so that the patients could see their blood tests in real time; that was a real selling point for our patients because they’re all expert patients in their own areas and they like to know what their bloods are. I think that would have helped the utilisation … And we monitor what we call their faecal calprotectin, to see what inflammation levels they’ve got; they’re always really keen to know that. It just hasn’t happened … the two systems haven’t been sort of married up. (IBDNS3T2)
In summary, three main barriers to adoption were identified, these related to concerns over the security of the system; risk averse attitudes of clinical and patient users; and problems with data integration.
The lack of integration with existent hospital records at the time of the study meant that patients could access their personal care plan and medications page, and could upload information into their record but not view their clinical records and test results as was intended. Whilst this may have consoled those for whom confidentiality was an issue it was a significant disappointment for many others:
I would like to be able to look up my record and see how I'm doing. (White British Female, aged over 75 years)
I have not tried the site recently but the times I tried there was no information other than that I put in myself. (White British female, aged 65–74 years)
Respondents were also asked about improvements they would like to see; most wanted better access to their health data:
Access to actual test data and more info such as X-rays and scan images. (Pakistani male, aged 25–34 years)
More of my information online would be great, i.e. access to my blood test results so that I can keep a track of levels etc. (White British male, aged 35–44 years)
Such feedback suggests that data integration is crucial to continued patient usage and satisfaction with the system (i.e. patient adoption).
Discussion
The study showed some evidence that direct portal access was perceived to have benefitted clinicians and patients alike. It facilitated two-way communications between clinicians and patients and allowed patients to send messages to specialist IBD nurses directly at any time. The fear amongst clinicians that this facility might lead to an overwhelming increase in communications was not well-founded. Clinicians agreed that patients were more frank and to the point in emails. Komura et al. found similarly,1 especially for those patients discussing embarrassing or personal issues. The patient survey showed that patients clearly valued these improved channels of communication and this was especially the case when patients were feeling unwell or experiencing an IBD flare-up.
The benefits of improved two-way communication have been noted in studies of patient health records elsewhere.1,12,21 In the USA there are two major implementations of shared electronic health record systems by health insurance companies Kaiser Permanente and the American Veterans Association. A large scale study of the Kaiser Permanente system looked at both physician and patient attitudes to virtual consultations via secure messaging and found that on the whole attitudes were favourable.22 They also noted a tendency for this practice to reduce patient attendances (in the USA this is seen as a negative outcome, but the paper discusses reimbursement issues to offset this). A second study,23 using Kaiser Permanente with HIV patients, noted that patients mostly used it for communicating with physicians, booking appointments and ordering prescriptions, rather than using the facilities to enter their own data; acute patients at Trust2 used PKB in a similar way. A qualitative study of around 40 patients using the Veterans Association system indicated that patients find the sharing of data useful, but largely to check accuracy of verbal instructions rather than to proactively control the record with their own data.21
Another of the elements cited as significant by the Trust1 clinical team was the IBD symptomatic assessment facility which prompted automatic alerts from patient-entered data (referred to clinically as patient reported outcomes or ‘PROs’). This feature replaced a process that would previously have involved one or more hospital visits; it also facilitated patient access to more immediate specialist assistance, with the assumption that this reduced unplanned admissions and GP consultations.
Wicks et al, report successful development and trial of a web-based PRO tool for paediatric use called KLIK e-PROfile.24–27 The tool has been positively evaluated by patients, parents and clinicians and found to improve clinical outcomes. Web-based monitoring tools have also been successfully used in oncology treatment,28 and there is further evidence of a trial using touch-screen collection of quality of life data from patients attending clinician appointments.29 An example within telehealth systems (telemonitoring) is the Whole System Demonstrator using the Tunstall system for COPD and CHF patients, in which an automated red/green/amber system was monitored by a nurse-call centre.30 There are other examples, but relatively little analysis of the value to patients or the hospital. The Whole Systems Demonstrator evaluation was striking in its neutrality in this respect – no strong statement has been found to demonstrate the economic or clinical value.
Although highly significant to Trust1 and a key component of the business case, patients did not make particular reference to the alerting system. This was possibly because they did not realise the significance of this procedure and simply used it when asked to.
PKB was used to provide an extensive library of patient education resources and links giving patients constant access wherever they are, stored and relevant to them. The expectation was that this would improve self-care and reduce pressure on all parts of the system. Again, patients did not comment on this feature, although 24 reported having used the libraries. In this information-saturated age it is possible that patients do not value the libraries specifically. Some may not remember where they read particular information. Others come with significant prior knowledge. This is a difficult feature therefore to assess. If patients are already information-literate they are unlikely to value it, but others may use it as their primary source. It is also likely that some patients may be reluctant to learn more about their condition as they are feeling negative about the impact it will have on their lives, although we have not specifically collected any data to explore this issue. Moreover, the provision of information alone will not guarantee self-management or self-efficacy. The Health Foundation published a review of evidence on the value of supported self-management which indicated the importance of different strategies.31 Whilst PHRs and information provision were recognised as important to self-efficacy, more active measures including self-monitoring and goal setting were considered important to effectively support behaviour change.
A potentially powerful feature of many PHR systems, and in particular PKB, is that patients can invite others (health professionals, carers or family members) to share access to their health record. Clinicians thought this a very good idea but were unaware of how patients used this facility. Anecdotally clinicians were aware of patients asking a family member who was perhaps more IT literate to help them, but not necessarily through a separate login. The patient survey showed that this was an under-used (and under-appreciated) feature. Over half of respondents were unaware that they could share their record and of those aware only one respondent had shared their record with a GP. Kerai et al found whilst people were generally willing to share access to their PHR with GPs and hospital staff they were less willing to give access to allied health professionals.32
Security emerged as a potential barrier to adoption. Concerns over security and privacy have been shown to be a major barrier to the implementation of electronic health records elsewhere.6–8,32–35 PKB has good security credentials and it is important that these are made explicit in order to assist adoption; this should include communicating that safeguards are in place and that no incidents have occurred.
Another barrier identified related to user attitudes to risk and change. Even within the two clinical teams we surveyed it appeared to have proved difficult to extend the use of PKB more widely. At Trust1, we were aware that one consultant was actively using it and usage had not been extended to dieticians or psychologists, who have an important role in supporting IBD patients to self-manage. The same issue around professional use was reported at Trust2, where use was limited to two consultants: “We’ve got six gastroenterologists here; top gastroenterologists and only two of them were willing to add their name” (IBDNS3T2). Clinicians were said to be concerned that PKB would produce extra work and this is a fear shared by others; the burden on clinical work and reduced productivity has been reported as a prohibitory factor elsewhere.8,12,21,36 In research by Cresswell et al.,36 most users reported that implementation caused them additional work without bringing the promised benefits, however informants did not report this here.
With regards to patients, evidence from other studies points to a tendency for patient registration to be slow.5,31,37,38 In this scenario however, patient registration was high (97% of patients invited to register did so); this may have been due to clinical staff personally inviting patients to use PKB. Nevertheless, some respondents to the e-survey indicated their reduced usage over time. Factors that have been found to impact on patient usage elsewhere include: poor portal design;12 lack of interoperability between systems;8,32 and user perception of usefulness.5,39 Whilst some respondents to the survey expressed dissatisfaction with portal design, the inability to view the personal data that was contained within both the registry database and other hospital systems seems to have been most significant; patients wanted access to results and medical records (blood, CT scan, histology); the fact that this was not possible impacted negatively upon patients’ perceived usefulness of PKB. It is clear that prompt integration with clinical records and test results is essential to keeping patients engaged in using the system.
Innovators (whether technology companies or clinicians) need to be aware of these barriers in designing and planning pilots. There are considerable risks in piloting an innovation which is not technically complete. Concerns of both staff and patient users are often much more significant than may be anticipated by those with enthusiasm and technical confidence, which can severely limit user engagement. Any attempt to generate evidence of effective success for an intervention may be compromised by these ‘teething troubles’. Users are clearly concerned that innovations may have limited usefulness or may be hard to use. Some of the issues have been identified here and need to be addressed by communications and training – possibly with much more intensity than may be anticipated.
A central rationale for patient health records is improved patient self-management.7,8,10–12 Trust1 chose PKB to be one component of a new supported self-management system; a primary objective was for patients to be empowered and become proactive in managing their condition. Patient empowerment denotes a change in patient role from passive recipient to active participant,40 wherein the patient is expected to be ‘a responsible, autonomous and competent partner in his or her own care’.13
Nevertheless, the patient survey suggested that some patients are not ready, able or willing to engage with PKB as intended. Inevitably, technology will be a barrier for some. But others will not desire empowerment.35 Other studies have noted unwillingness to participate from patients, for instance in research by Kerai et al. ‘the majority of respondents felt that their usual GP practice should oversee their records’,32 and Komura et al. found many patients ‘wanted to leave the decisions to their doctor’.1 Moreover, our data suggests that patient usage correlated with the status or severity of their IBD. PKB was said to be less relevant to acute patients due to them being in regular contact with clinicians, consequently acute patients used PKB to change appointments. With stable patients however, it appears that usage increases when they are unwell and reduces as their condition improves. This is a good start, but the ultimate aim would be for patients to engage with the system in ways that prevented them feeling unwell in the first place.
The literature identifies numerous factors which impact upon patient engagement. Moreover, there is evidence that patients are more likely to use electronic health systems if they have higher self-efficacy,5 higher socio-economic status and higher levels of education,41 show competency in information elicitation and an ability to understand their health information.10 As Falcão-Reis and Correia assert,42 twenty-first century patients are required to be ‘deeply connected with emergent new technologies and highly motivated to assume control and responsibility over [their] own health care’. These are important considerations in planning services, but targeting such patients will at least give the opportunity to reduce resource consumption by this group to hopefully enable resources to be focused on those less able to access care.
The barriers and concerns that emerged in this study are summarised below in Table 4, illustrating the key points and how they could be mitigated to ensure the highest chance of success.
Table 4.
Summary of barriers and concerns of users.
| Barriers and concerns | ||
|---|---|---|
| Data security | User reluctance to engage | Limited access to full record |
| • Privacy, confidentiality of personal data. • Concerns that data could be ‘hacked’ and shared (e.g. with press). | • Several separate concerns ○ Will create further work (staff) ○ Will be difficult to use (staff and patients) ○ Not perceived as providing value. • Limited engagement, using only basic features of the system (Trust2). • Deeper underlying concerns by patients not wishing to self-manage or to be in control. | • Only able to see limited data, largely own-entered. • Users discontinue use of system as do not find anything they have not entered themselves. |
| Mitigation | ||
| • Confirm and communicate that safeguards are in place and that no incidents have occurred. | • Engage staff and patients more fully in intervention design and development. • Develop understanding of which patients most likely to benefit. Ongoing training and communications for staff and patients. | • Complete technical development fully before deployment. |
Limitations
The PKB PHR system was introduced alongside a number of other changes in patient care, including the introduction of the IBD Registry and a greater involvement of specialist IBD nurses to support self-management by patients. The identification of simple causal relationships between the PHR itself and the outcomes was therefore difficult. Instead, we have highlighted differing stakeholder perceptions of the benefits and barriers. In addition, at the time of data collection the integration of PKB with the IBD registry and hospital records had not been established which might help explain the limited enthusiasm of patients.
Further, the StEAM model recommends attention to the viewpoints of four stakeholder groups:17 professional users, patient users (user stakeholders), organisational management and technology supplier (economic stakeholders) yet in this study we engaged only with user stakeholders. Fewer interviews than hoped were conducted with clinical stakeholders, particularly senior clinicians who had other priorities at the time of study. In addition, the response rate to the e-survey was disappointing. Consequently there are data limitations in this study and we could not make statements with statistical confidence. Further research is now needed to understand better the perspectives of patient users and whether and how the PKB PHR system is utilised differently by different types of patient; this would assist in targeting the PKB PHR system at patients most likely to engage and benefit.
Conclusion
This case study has highlighted clinician perceived benefits achieved through usage of a patient held PHR system, as part of a more complex intervention to support self-management of IBD. Identified benefits were: more optimal use of hospital resources; improved two-way communications; increased confidence and self-management amongst stable patients.
A central aim of the new patient management system was to improve patient self-management; clinical informants at Trust1 believed this process had begun. However, identified benefits cannot be easily ascribed directly to the PKB PHR system in the clinical context due to the complex nature of the intervention and the limitations of data collection and metrics in place. Nevertheless, the PKB PHR system is an important cog in a wheel that supports patient empowerment and ultimately should reduce pressures on the system, enabling resources to be deployed more effectively and reduce waiting times elsewhere.
Notwithstanding, only some of the benefits identified by clinical staff were corroborated by patient feedback; indeed many patients contradicted clinician opinion on the benefits of a number of PKB features. In both Trusts surveyed the system was not considered to have achieved its full potential. Barriers were data security and privacy concerns, lack of data integration with core systems, stakeholder reluctance to engage and some usability issues with the software. The use of PHRs to change behaviours and improve self-management is thought to be further limited by patient choices, attitudes and capabilities. However, for those for whom it is suitable it can be revolutionary.
Three generic recommendations follow: (1) information security, confidentiality and governance procedures need to be not only in place, but communicated clearly as such to all users. (2) Engagement with all users, but particularly patients, needs to include much more training and communications of the benefits. (3) Integrate fully with other hospital systems before rolling out – although we note that this is often in tension with project timescales and deadlines.
This study has nevertheless shown that PHRs offer significant potential as a component of a well-designed service to support self-management. The evidence from both professional and some patient users is that providing a digital connection to healthcare can enable patients to live a more normal life, to travel and go on holiday, to understand their condition better and to get more appropriate, timely clinical advice. The long term benefits to the health service of reducing hospital outpatient appointments and in transferring care from consultants to specialist nurses is clear.
Supplementary Material
Acknowledgements
In developing the ideas presented here we received helpful input from Christopher Heginbotham OBE FRSPH, visiting Professorship at the University of Cumbria. We thank contributors from Trust1 and Trust2 for their input. We also thank the reviewers for their useful and constructive comments of earlier versions of this paper.
Contributorship
Both authors researched literature and conceived the study. Both authors undertook qualitative interviews and site visits. EB was involved in protocol development, securing approval from Trust1, survey development and distribution, and data analysis. EB wrote the first draft of the manuscript. Both authors reviewed and edited the manuscript and approved the final version of the manuscript.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
Ethical approval was not required; the study was approved by Trust1 as a service evaluation, with an agreed protocol for access to staff and anonymised patients.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Patients Know Best, Ltd. Registered in England and Wales Number: 6517382. Individuals at Patients Know Best commented on draft versions of this paper but final editorial decisions rested with the authors.
Guarantor
AM
Peer review
This manuscript was reviewed by Paul Wicks, PatientsLikeMe and one other reviewer who has chosen to remain anonymous.
Supplemental material
The online supplementary material is available at http://dhj.sagepub.com/supplemental.
References
- 1.Komura K, et al. Patient-perceived usefulness and practical obstacles of patient-held records for cancer patients in Japan: OPTIM study. J Palliat Med 2013; 27: 179–184. [DOI] [PubMed] [Google Scholar]
- 2.Kelsey T. Urgent action on a digital NHS is a moral imperative. Health Service Journal, 1 September, www.hsj.co.uk/comment/kelsey-urgent-action-on-a-digital-nhs-is-a-moral-imperative/5089831.article (2015, accessed 13 October 2015).
- 3.National Information Board and Department for Health. Personalised health and care 2020: using data and technology to transform outcomes for patients and citizens. A framework for action, www.gov.uk/government/uploads/system/uploads/attachment_data/file/384650/NIB_Report.pdf (2014, accessed 14 October 2015).
- 4.Kensing F. Personal health records. In: Mantas J, et al. (ed). Quality of life through quality of information, Amsterdam: IOS Press, 2012, pp. 9–13. [Google Scholar]
- 5.Agarwal R, et al. If we offer it, will they accept? Factors affecting patient use intentions of personal health records and secure messaging. J Med Internet Res 2013; 15: e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lehnbom EC, Brien JE, McLachlan AJ. Knowledge and attitudes regarding the personally controlled electronic health record: an Australian national survey. Intern Med J 2014; 44: 406–409. [DOI] [PubMed] [Google Scholar]
- 7.Van der Vaart R, et al. Giving rheumatology patients online home access to their electronic medical record (EMR): advantages, drawbacks and preconditions according to care providers. Rheumatol Int 2013; 33: 2405–2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Etzioni A. Personal health records: why good ideas sometimes languish. Issues Sci Technol 2010; 26: 59–66. [Google Scholar]
- 9.Logue MD, Effken JA. Validating the personal health records adoption model using a modified e-Delphi. J Adv Nurs 2013; 69: 685–696. [DOI] [PubMed] [Google Scholar]
- 10.Alpay L, Van der Boog P, Dumaij A. An empowerment-based approach to developing innovative e-health tools for self-management. Health Inf J 2011; 17: 247–255. [DOI] [PubMed] [Google Scholar]
- 11.Bourgeois FC, et al. MyChildren’s: integration of a personally controlled health record with a tethered patient portal for a pediatric and adolescent population. In: AMIA 2009 symposium proceedings, www.ncbi.nlm.nih.gov/pmc/articles/PMC2815447/?report=classic (2009, accessed 14 October 2015).
- 12.Kruse CS, et al. Patient and provider attitudes toward the use of patient portals for the management of chronic disease: a systematic review. J Med Internet Res 2015; 17: e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ammenwerth E, Schnell-Inderst P and Hoerbst A. Patient empowerment by electronic health records: First results of a systematic review on the benefit of patient portals. In: e-Health across borders without boundaries, proceedings of the EFMI special topic conference (ed Stoicu-Tivadar L, et al), Laško, Slovenia, 14–15 April 2011, pp.63-67. Amsterdam: IOS Press. [PubMed]
- 14.IBD Registry, http://ibdregistry.org.uk/ (2016, accessed 29 March 2016).
- 15.IBD Standards, www.ibdstandards.org.uk/ (2016, accessed 29 March 2016).
- 16.National Institute for Health and Care Excellence (NICE). Faecal calprotectin diagnostic tests for inflammatory diseases of the bowel, www.nice.org.uk/guidance/dg11 (2013, accessed 29 March 2016).
- 17.Marshall A. Designing telemedicine apps that health commissioners will adopt. In: Proceedings of the 14th conference of the open innovations association (FRUCT), Espoo, Finland, 11–15 November 2013, pp.63-68. IEEE.
- 18.Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 2004; 6: e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bristol Online Surveys. The online survey tool designed for academic research, education and public sector organisations, www.onlinesurveys.ac.uk/ (2016, accessed 29 March 2016).
- 20.MailChimp, http://mailchimp.com/ (2016, accessed 29 March 2016).
- 21.Woods S, et al. Patient experiences with full electronic access to health records and clinical notes through the My HealtheVet personal health record pilot: qualitative study list. J Med Internet Res 2013; 15: e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palen TE, et al. Comparing virtual consults to traditional consults using an electronic health record: an observational case–control study. BMC Med Inf Decis Making 2012; 12: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ralston JD, et al. Use of web-based shared medical records among patients with HIV. Am J Manag Care 2013; 19: e114. [PMC free article] [PubMed] [Google Scholar]
- 24.Wicks P, et al. Innovations in e-health. Qual Life Res 2014; 23: 195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Engelen V, et al. Reporting health-related quality of life scores to physicians during routine follow-up visits of pediatric oncology patients: is it effective? Pediatr Blood Cancer 2012; 58: 766–774. [DOI] [PubMed] [Google Scholar]
- 26.Haverman L, et al. Monitoring health-related quality of life in paediatric practice: development of an innovative web-based application. BMC Pediatr 2011; 11: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haverman L, et al. Effectiveness of a web-based application to monitor health-related quality of life. Pediatrics 2013; 131: e533–e543. [DOI] [PubMed] [Google Scholar]
- 28.Snyder C, et al. PatientViewpoint: a website for patient-reported outcomes assessment. Qual Life Res 2009; 18: 793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Velikova G, et al. Patients report improvements in continuity of care when quality of life assessments are used routinely in oncology practice: secondary outcomes of a randomised controlled trial. Eur J Cancer 2010; 46: 2381–2388. [DOI] [PubMed] [Google Scholar]
- 30.Bower P, et al. A comprehensive evaluation of the impact of telemonitoring in patients with long-term conditions and social care needs: protocol for the whole systems demonstrator cluster randomised trial. BMC Health Serv Res 2011; 11: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Silva D. Evidence: helping people help themselves, London: The Health Foundation, 2011. [Google Scholar]
- 32.Kerai P, Wood P, Martin M. A pilot study on the views of elderly regional Australians of personally controlled electronic health records. Int J Med Inform 2014; 83: 201–209. [DOI] [PubMed] [Google Scholar]
- 33.Cucciniello M, et al. Understanding key factors affecting electronic medical record implementation: a sociotechnical approach. BMC Health Serv Res 2015; 15: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fetter M. Health information technology and literacy column: Personal health records: protecting behavioral health consumers’ rights. Issues Ment Health Nurs 2009; 30: 720–722. [PubMed] [Google Scholar]
- 35.Chan D, et al. Revolutionizing patient control of health information. Can Fam Physician 2013; 59: 823–824. [PMC free article] [PubMed] [Google Scholar]
- 36.Cresswell K, et al. Anything but engaged: user involvement in the context of a national electronic health record implementation. Inf Primary Care 2011; 19: 191–206. [DOI] [PubMed] [Google Scholar]
- 37.De Lusignana S and Seroussi B. A comparison of English and French approaches to providing patients access to summary care records: scope, consent, cost. In: Data and knowledge for medical decision support, Proceedings of the EFMI special topic conference (ed Blobel B, et al.), Prague, Czech Republic, 17–19 April 2013, pp.61–65. Amsterdam: IOS Press. [PubMed]
- 38.Kim EH, et al. Challenges to using an electronic personal health record by a low-income elderly population. J Med Internet Res 2009; 11: e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Venkatesh V, et al. User acceptance of information technology: toward a unified view. MIS Q 2003; 27: 425–478. [Google Scholar]
- 40.Koch S. Improving quality of life through ehealth – the patient perspective. In: Mantas J, et al. (ed). Quality of life through quality of information, Amsterdam: IOS Press, 2012, pp. 25–29. [PubMed] [Google Scholar]
- 41.Yamin CK, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med 2011; 171: 568–574. [DOI] [PubMed] [Google Scholar]
- 42.Falcão-Reis F, Correia ME. Patient empowerment by the means of citizen-managed electronic health records: Web 2.0 health digital identity scenarios. In: Bos L, et al. (ed). Medical and care compunetics 6, Amsterdam: IOS Press, 2010, pp. 214–228. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.