Abstract
Objective
The objective of this study was to describe participant engagement and examine predictors of weight loss and points earned through the point-based incentive system of the Social Pounds Off Digitally (POD) app.
Materials and methods
Overweight and obese adults with Android smartphones/tablets (body mass index 25–49.9 kg/m2; N = 24) were recruited for a 3-month weight loss intervention. Participants completed a survey assessing demographics and personality and had their weight measured. Participants received the content of the intervention via podcasts and used the Social POD app to self-monitor diet, physical activity, and weight. The Social POD app contained: tracking features; in-app notifications to track; pre-set goals for tracking; newsfeed for updates on others’ goal attainment; ability to earn and track points for usage (exchanged for study-provided prizes); and a message screen. Analyses examined relationships between percent weight loss, personality characteristics, and total points earned.
Results
A total of 4843 points were earned (mean = 202 ± 105 points/participant). Most participants earned all three prizes (62.5%), followed by two prizes (21%), no prizes (12.5%), and one prize (4%). Total points earned significantly predicted percent weight loss (B = −0.02, p = .01), and higher conscientiousness significantly predicted greater total points earned (B = 10.27, p = .01), but other personality characteristics assessed did not.
Conclusion
A mobile app yielded moderately high participant engagement, as demonstrated by points earned. Earning points was significantly associated with percent weight loss, and conscientiousness was significantly associated with total points earned. Future research should examine whether point systems impact health behavior and weight loss when rewards are discontinued.
Clinical trial registration number
Keywords: mHealth, weight loss, obesity, incentives, reinforcement, Social Cognitive Theory
Introduction
Rates of overweight and obesity remain high among US adults, with 71% meeting this criterion (body mass index (BMI) >25 kg/m2).1 Interventions developed using health behavior theories to improve diet and physical activity (PA) have been successful in promoting weight loss.2 Mobile health (mHealth), the use of mobile technology (e.g. smartphones, tablets, activity monitors) to improve health behaviors, is an emerging mode of delivery for behavioral interventions.3–6 Novel mobile applications (apps) have been developed and tested by researchers to deliver weight loss interventions,7,8 and results demonstrate significant short-term weight loss outcomes.9 While there are many benefits of delivering weight loss interventions using remote methodologies, such as mobile apps, finding ways to maintain participant engagement (i.e. use) over time can be a challenge.10
Past research has focused on providing social support to help maintain participant engagement in remotely delivered interventions. Existing mobile platforms, such as social media (Twitter6,11 and Facebook),12–15 text messaging,15–18 and online support communities,19 have been used as modes of communication to foster social support and maintain participant engagement in previous weight loss interventions. Others have used principles of social gaming and financial incentives to promote engagement in an electronic health intervention for weight loss.20 Among overweight and obese adolescents, video games have been used to promote engagement with a PA intervention.21 A mobile app has also been developed using gaming principles to promote healthy eating among children.22 Most of the current research examining the efficacy of using incentives to promote weight loss among adults has been conducted via face-to-face interventions and typically consists of financial incentives.23 While a few commercially available apps marketed for weight loss include some type of incentive system (My Diet Coach (Inspired Apps) and Jillian Michaels (Everyday Health, Inc.)), to our knowledge, the incentive systems in these apps have not been rigorously tested to examine how these apps impact weight loss.24,25
This paper focuses on the development of a new mobile app (the Social Pounds Off Digitally (POD) app) to test theoretically driven research hypotheses. The main weight loss intervention used constructs from behavioral theories, including Social Cognitive Theory (SCT),26,27 to promote self-monitoring of diet, PA, and weight and promote participant engagement and motivation to enhance weight loss in this remotely delivered intervention. Based on feedback from participants during the pilot testing of the Social POD app,28 the mobile app point-based incentive system allowed participants to earn points for using the diet, PA, and weight self-monitoring features of the app and for sending others encouragement (targeting positive reinforcement from SCT26 and operant conditioning).29–31
The purpose of this paper is to fill the gap in existing mHealth literature surrounding incentive systems and weight loss by describing participant engagement with the Social POD point system, examining the association between percent weight loss and total points earned, and examining predictors (personality characteristics) of points earned through the incentive system of the Social POD app. Demographic characteristics were also assessed as potential confounders associated with point-earning behavior. A description of the development and refinement of the Social POD app28 and main outcomes, including weight loss and changes in psychosocial characteristics,32 can be found elsewhere. Briefly, main outcomes from the randomized clinical trial demonstrated that participants using the Social POD app (which incentivized self-monitoring with a point system; the Social POD group) lost significantly more weight than comparison group participants using a commercial self-monitoring mobile app (without an incentive system; the comparison group) within the context of a remotely delivered behavioral weight loss intervention.32 This current study seeks to examine associations with point-earning behaviors as well as to examine whether earning points was associated with percent weight loss in order to inform future attempts to engage participants in remotely delivered mHealth interventions for weight loss.
It was hypothesized that total points earned would be significantly associated with weight loss (via self-regulation).27 Given the research supporting the association between high conscientiousness and protective health behaviors33,34 as well as health outcomes later in life (low conscientiousness associated with greater adiposity, BMI, morbidity, and mortality),33,35–37 it was hypothesized that higher conscientiousness would be significantly associated with more points earned. This study, to our knowledge, is the first to examine results from a point-based incentive system incorporated into a mobile app for adults, which is significant given the need to find methods to sustain long-term diet, PA, and weight self-monitoring behaviors over time to promote weight loss and maintenance.38
Methods
Participant recruitment and measures
Overweight and obese men and women (BMI 25–49.9 kg/m2; N = 51) from two mid-size cities in South Carolina with Android smartphones/tablets were recruited for a 3-month weight loss intervention. Participants were recruited via university and worksite listserv announcements, community/worksite flyers, newspaper advertisements, university/worksite electronic newsletters, social media posts, handouts at a local research fair, and word of mouth.
Exclusion criteria included not having an Android phone/tablet, BMI outside the range of 25.0–49.9 kg/m2, being unable to attend required meetings, being unable to access a computer or the internet to complete assessments, having a psychiatric illness, receiving treatment for drug or alcohol dependency, having an eating disorder, participating in another weight loss program, reporting weight loss of 10 pounds or more in the past 6 months, being pregnant or planning on becoming pregnant during the study, or currently breastfeeding. Exclusion criteria also included endorsing select items from the PA Readiness Questionnaire:39 being told by a doctor that they have a heart condition and should only participate in approved PA; feeling chest pain with or without engaging in PA in the past month; and ever losing balance, becoming dizzy, or losing consciousness. If participants reported a bone or joint problem that could be made worse by participating in PA, or were taking blood pressure medication, they were required to submit a physician consent form to participate in the study.39 Participants received a total of $10 for completion of all assessments.
Participants attended a total of three in-person measurement sessions. The first was an orientation session, where they received a detailed description of the study and received instruction for completing all baseline assessments. Following orientation, participants completed a baseline survey assessing demographics (age, ethnicity, educational attainment, employment status, and marital status). The previously validated Big Five Inventory, measuring the personality characteristics of extraversion (energetic and lively traits), neuroticism (negative and anxious traits), openness (creative and open-minded traits), conscientiousness (task-oriented and organized traits), and agreeableness (trusting and compliant traits) was also completed at baseline.40 Three of five scales from the Big Five were used in this study—neuroticism, extraversion, and conscientiousness—as the other two have not been found to be associated with weight-related behaviors.34 Participants who completed the baseline questionnaire were randomized to one of two groups and attended a training session, where they were told to which intervention group they were assigned and received instruction regarding how to use the intervention components. Baseline and 3-month weight measures (SECA 869, Hamburg, Germany, calibrated digital scale accurate to 0.01 kg) were obtained by trained staff at the training and final sessions. All participants provided written consent, and this study was approved by the University of South Carolina Institutional Review Board.
Intervention components
In addition to using a tracking app to self-monitor diet, PA, and weight, participants in both conditions received two theory-based podcasts each week. Specific information regarding podcast development and testing in previous interventions can be found elsewhere.4,6 Podcast topics included: nutrition and PA information focused on achieving a healthy weight; a male and a female character documenting their weight loss progress and challenges through an audio diary; a weight loss drama depicting the challenges of overcoming social barriers to weight loss; and a goal-setting activity related to healthy behaviors that promote weight loss at the end of each episode.
Social POD group participants used the Social POD app developed by the authors for the Android platform. The Social POD app included diet, PA, and weight tracking features, as well as a journal feature, calorie database, weight graph, in-app notifications, message page, newsfeed, goals page, and point tracker. A description of the development, pilot testing, and subsequent revision of the Social POD app has been previously documented.28
Within-app notifications were sent via the Social POD app at specific times throughout the day to remind participants to self-monitor diet, PA, and weight each day. Participants entered calories consumed from all meals and snacks, minutes of PA completed, and body weight in order to promote self-regulation.27 Participants who regularly used the Social POD app were also prompted by notifications to send pre-written encouraging messages to participants who had not entered data in the app over the previous 48 hours. These messages were developed targeting social support11 and using constructs from SCT to target self-efficacy26,27 and outcome expectations,41 which, together, were believed to encourage self-monitoring of diet, PA, and weight.
An incentive system to promote weight loss with goals, newsfeed, and point tracker (targeting reinforcement from SCT26 and operant conditioning)29–31 was incorporated into the Social POD app. Goals were set by the study team for using the Social POD app for tracking diet, PA, and weight (e.g. logging diet, weight, and 30 minutes of PA for the day) and for sending daily encouragement to others. Goals were chosen based on past research demonstrating greater weight loss outcomes for participants who engage in self-monitoring behaviors. Participants could view other participants’ progress with these goals on the newsfeed and send them encouraging messages (“stars”) for achieving goals. During the training session, participants were told how many prizes they could earn for each point level. Points were redeemed for study-provided prizes at the final meeting at 3 months.
The number of points that a participant could earn was based on the total number of points possible over the course of the study for the following activities: 1) tracking calories every day (one point for logging at least one meal or snack each day); 2) tracking weight every day (one point for doing this one time per day); 3) logging at least 30 minutes of physical activity per day (one point for logging at least 30 minutes per day); 4) sending an encouraging message to another participant; and 5) sending a “star” from the newsfeed to other participants as encouragement for completing a goal (maximum of one point per day). Participants could earn a total of five points per day for a total of 420 possible points over the course of the 12-week study. The prizes and numbers of points needed to earn each prize were as follows: Level One, pedometer, 60 points; Level Two, pedometer and sweat towel, 120 points; and Level Three, pedometer, water bottle, and sweat towel, 180 points.
A secure network server collected and stored all participant activity with the Social POD app throughout the intervention. Participants in the comparison group used a standard tracking app called Calorie Counter (Fat Secret, © 2015), which included a number of features: calorie database and meal tracker; PA database and PA tracker; weight tracker with a graph; recipe index; periodic email reminders to weigh in; and journaling feature. Following the intervention, all participants attended a final session where final weight measurements were obtained.
Statistical analysis
The goals of the analyses were to describe participant use of a point-based incentive system and to examine predictors of weight loss and points earned among Social POD group participants in the Social POD Study. Data from comparison group participants is not included in this analysis. Linear regression was used to first assess potential associations between demographics (age, gender, ethnicity, and educational attainment) and total points earned, to rule out potential confounders in subsequent models assessing for significant relationships between points earned and weight loss and between points earned and personality characteristics.
A linear regression model was used to assess the relationship between percent weight loss and total points earned at 3 months. As demographic characteristics were not significantly associated with percent weight loss, they were not included as a confounder in the model examining total points earned and percent weight loss. Multiple regression was used to assess the relationship between total points earned and the three personality characteristics shown to be related to weight loss behaviors.34 Responses for participant ethnicity were collapsed to form two groups (White, n = 14, and Other, n = 10). Responses for educational attainment were collapsed to some college or college degree (n = 16) and graduate degree (n = 8). Scores from the previously validated Big Five Inventory were continuous variables in the multiple regression model assessing for significant associations between personality and total points earned.
Assumptions were checked for regression models. For the main outcome of percent weight loss and total points earned, Shapiro–Wilk was used to assess the assumption of normality of residuals, and results were not significant for violations of this assumption (p = .06). The Cook–Weisburg test was used to assess for heteroskedasticity, and results were not significant (p = .66). A scatterplot of data points was used to assess for linearity and the presence of significant outliers, and there were no violations of linearity and no significant outliers were detected or removed. Collinearity was examined and found not to be present in the model assessing the relationship between personality characteristics and total points earned. Intent-to-treat analysis with baseline observations carried forward was used in the calculation of percent weight loss for missing final weight values for Social POD group participants (n = 3). All data was collected and analyzed between February and September 2015 using Stata version 13.1 (StataCorp, 2013) with p < .05 to detect statistical significance.
Results
Main study outcomes
Outcomes from the main trial are included in a separate publication.32 There were 26 participants randomized to the Social POD group in the main study (with n = 25 randomized to the comparison group). Two participants were excluded from all analyses due to reported contraindicated medication and surgery affecting body weight. Participants in this study were mostly White (58%) women (83%) with a mean BMI of 36.2 ± 6.5 kg/m2 and mean age of 49.0 ± 11.3 years (Table 1).
Table 1.
Sample baseline characteristics (N = 24).
| Characteristics | Social POD group |
|---|---|
| Mean age, years (±SD) | 49.0 (±11.3) |
| Gender, n (%) | |
| Female | 20 (83) |
| Male | 4 (17) |
| Race, n (%) | |
| Black | 9 (38) |
| White | 14 (58) |
| Mixed race | 1 (4) |
| Mean body mass index, kg/m2 (±SD) | 36.2 (±6.5) |
| Educational attainment, n (%) | |
| Some college | 3 (13) |
| College degree | 13 (54) |
| Graduate degree | 8 (33) |
| Employment status, n (%) | |
| Student | 2 (8) |
| Part-time | 1 (5) |
| Full-time | 19 (79) |
| Retired | 0 (0) |
| Out of work | 0 (0) |
| Other | 2 (8) |
| Marital status, n (%) | |
| Married | 9 (38) |
| Divorced | 4 (17) |
| Living with partner | 2 (8) |
| Never married | 8 (33) |
| Separated | 1 (4) |
Engagement with the Social POD point system
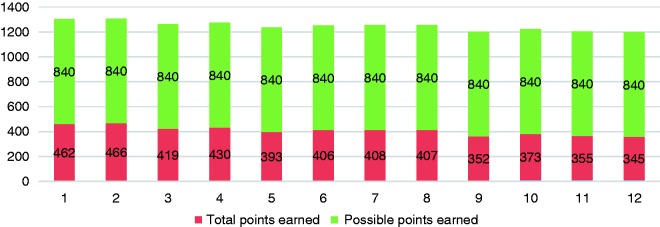
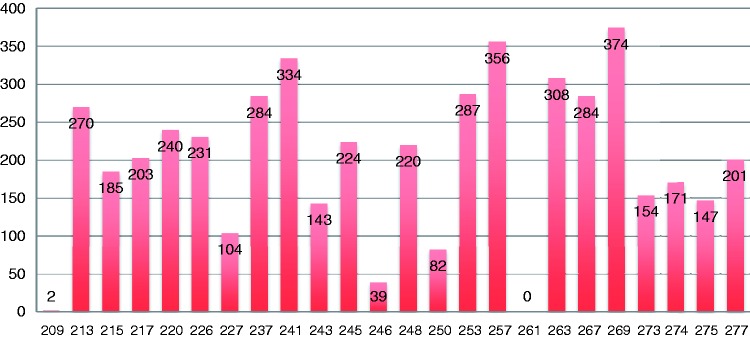
The total number of Social POD app entries was 11,298, with a mean of 470.8 entries per participant (SD ± 296.8, minimum 0, maximum 981 entries). A total of 4843 points were earned by participants, with a mean of 201.8 points earned per participant (SD ± 104.7, minimum 0, maximum 374 points). The total number of points earned by participants decreased over time during the intervention (Figure 1). However, at the end of the 3-month intervention, most Social POD group participants earned all three prizes (n = 15, 62.5%), followed by two prizes (n = 5, 21%), no prizes (n = 3, 12.5%), and one prize (n = 1, 4%). The total number of points earned by each of the participants can be viewed in Figure 2.
Figure 1.
Total points earned out of total possible points earned by week.
Figure 2.
Total points earned by user ID.
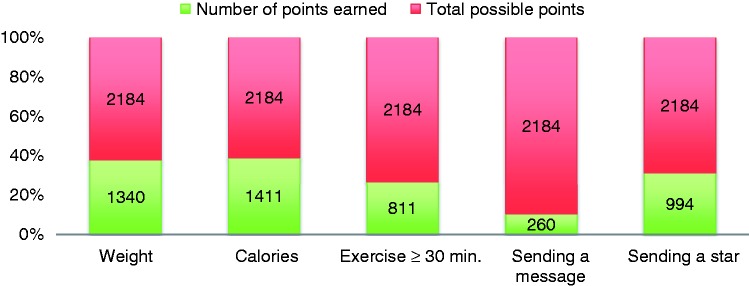
Of the activities participants could complete to earn points, logging calories consumed was the most frequently completed activity, followed by logging body weight, sending a star to another participant through the newsfeed, logging exercise (at least 30 minutes), and sending an encouraging message to another participant (Figure 3).
Figure 3.
Number of points earned out of total possible points earned by activity type.
Weight loss, points earned, and predictors of points earned
None of the demographic characteristics significantly predicted total points earned, including age (B = −0.79, p = .69), gender (B = 39.02, p = .47), ethnicity (B = −75.9, p = .07), and education (B = 61.1, p = .06), and they were therefore not controlled for in subsequent models. Total points earned significantly predicted percent weight loss, such that for every point earned, participants lost an additional 0.02% of body weight (B = −0.02, p = .01). Greater conscientiousness significantly predicted total points earned (B = 10.27, p = .01), but none of the other three personality characteristics assessed was a significant predictor of earning points, including neuroticism (B = −1.63, p = .66) and extraversion (B = −2.1, p = .50).
Discussion
Participant engagement with point systems
The present study examined the role of a mobile app that used a point system to engage participants in a remotely delivered weight loss intervention for overweight and obese adults. In this current study, participant engagement with the point system was moderately high, with most participants achieving the highest prize level (>180 points) and earning all three study-provided prizes. While most participants earned all three prizes, some participants were not highly engaged or not at all engaged with the point system throughout the intervention. Currently, there is little research on the use of mobile app-based point systems to engage adults participating in remotely delivered weight loss interventions. In the current literature examining researcher-developed mobile apps for weight loss among adults, none included any type of incentive system.7,8
Weight loss and points earned
The Social POD app fills gaps in the literature regarding the development and testing of a point system to incentivize use of a weight loss mobile app for adults. In the Social POD study, points earned significantly predicted percent weight loss, indicating that providing overweight adults with the ability to earn incentives for self-monitoring their diet, PA, and weight and sending encouragement to others could help promote weight loss. A review of randomized controlled trials providing incentives to improve levels of PA concluded that incentives successfully improved PA outcomes during the interventions examined.31 A review by Burns et al. suggested that using material incentives could especially help motivate those individuals who are not intrinsically motivated to perform healthy behaviors to promote weight loss.29 However, other reviewers have concluded that providing external rewards during interventions does not undermine performance of healthy behaviors related to weight loss and PA, even when initial levels of intrinsic motivation for performing these behaviors are high.30 As the current study did not examine this, future research should examine which types of point-earning activities (e.g. self-monitoring diet, PA, and weight, and sending/receiving encouragement) are related to weight loss outcomes in the context of this type of remotely delivered weight loss intervention. As indicated in Figure 3, logging calories and weight, followed by sending a star to another participant via the newsfeed, were the top three utilized point-earning activities. It could be that participants were more focused on logging their diet and weight as part of this intervention than on the other point-earning activities (such as entering at least 30 minutes of PA or sending a pre-written message), as their primary goal for participating in the study was weight loss. It could also be possible that participants preferred sending a star through the newsfeed rather than sending pre-written messages to re-engage inactive users, as clicking a star to send to another user was less burdensome than reading and selecting a pre-written message to encourage another user. Future research should examine whether messages written by users would be utilized more frequently than pre-written messages using behavioral theory to re-engage inactive users.
Another study found similar results to those of the Social POD study when examining the correlation between financial incentives and weight loss. This study, conducted by John et al.,42 found a significant correlation between performance (weight loss) and receiving financial incentives in a deposit-contract group as compared with a control group (without financial incentives).42 Similarly to Social POD, the results of this study indicated that incentives (frequency and the total number of deposits) were significantly correlated with weight loss in the deposit-contract group.42
Predictors of point earning
The Social POD study also sought to identify characteristics, specifically personality traits, of participants who earned points with the Social POD app to aid in potentially tailoring future incentive systems. A higher conscientiousness score on the Big Five Inventory significantly predicted greater total points earned in the Social POD Study. This finding is supported by the literature, which shows that higher neuroticism and lower conscientiousness are associated with higher adiposity, BMI, morbidity, and mortality.33,35–37 As personality traits are fairly stable in adulthood, results from this study suggest that it could be important to train adult participants with low conscientiousness to perform behaviors typically associated with this trait to promote weight loss (e.g. using frequent reminders to promote self-monitoring of dietary behaviors).36 A meta-analysis of personality traits, outcomes, and opportunities for targeting personality through interventions suggested that it is possible to target facets of conscientiousness, such as re-evaluation and overcoming resistance to change (as part of the industriousness facet of conscientiousness), as methods of fostering healthy behaviors (e.g. engaging in PA).36
Limitations and strengths
There are some limitations worth noting. This study had a short duration, and future research should test whether the Social POD app could assist with weight loss maintenance. The Social POD app was only available for the Android operating system, the sample size was small, and the sample consisted of mainly highly educated, middle-aged, working women, which could limit the generalizability of the results. As the power calculation was computed based on the main outcome,32 the sample size for this study was small; therefore, detection of differences in demographic characteristics and points earned was not possible. Also, this study may not have been adequately powered to detect significant differences in points earned and personality characteristics. Objective measures of engagement with the control app could not be obtained, which presents a limitation, as group comparisons for this outcome are not possible. While earning points did predict a change in weight from pre- to-post intervention, points only accounted for 4% of the variance in change in weight; furthermore, this study did not examine the difference between different point-earning activities and change in weight. There are also several strengths of this study. Participant engagement and weight were measured objectively, versus via self-report, which could be subject to bias. This intervention was remotely delivered, and therefore less time-intensive for staff and participants than many in-person interventions, and could easily be disseminated to reach a much larger population using fewer resources than are typically required by traditional face-to-face interventions.
Conclusions
A mobile app developed by researchers for overweight and obese adults demonstrated high participant engagement with a point-based incentive system. This study demonstrated that earning points was significantly associated with percent weight loss and that high conscientiousness was significantly associated with total points earned, whereas demographic characteristics of participants were not. Future research should examine whether point systems, like that of the Social POD app, continue to impact health behavior and weight loss when rewards are discontinued, as well as whether varying point values could be used to differentially enhance the performance of specific behaviors related to weight loss (e.g. valuing especially important or difficult behaviors at higher point values than others).
Contributorship
GTM, MH, HV, and SW conceived the project. MH, HV, and AF contributed to the programming of the Social POD app. Data acquisition and interpretation were conducted by GTM and SH. SH performed the statistical analyses and wrote the manuscript, and all authors were responsible for the research concept and design as well as critical revision of the manuscript, and approved the final version.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
The ethics committee of The University of South Carolina Institutional Review Board approved this study.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Advanced Support for Innovative Research Excellence – II program. This project was also supported by the South Carolina Clinical & Translational Research Institute with an academic home at the Medical University of South Carolina CTSA NIH/NCATS grant number UL1TR000062, National Institute of General Medical Sciences P20GM103499. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Guarantor
Not applicable.
Peer review
The authors have chosen for the 3 individuals who reviewed this manuscript to remain anonymous.
References
- 1.Flegal KM, Carroll MD, Kit BK. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 2012; 307: 491–497. [DOI] [PubMed] [Google Scholar]
- 2.Dombrowski SU, Avenell A, Sniehott FF. Behavioural interventions for obese adults with additional risk factors for morbidity: Systematic review of effects on behaviour, weight and disease risk factors. Obes Facts 2010; 3: 377–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: A systematic review. PLoS Med 2013; 10: e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turner-McGrievy GM, Campbell MK, Tate DF, et al. Pounds Off Digitally Study: A randomized podcasting weight-loss intervention. Am J Prev Med 2009; 37: 263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turner-McGrievy GM, Beets MW, Moore JB, et al. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J Am Med Inform Assoc 2013; 20: 513–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turner-McGrievy G, Tate D. Tweets, Apps, and Pods: Results of the 6-month mobile Pounds Off Digitally (Mobile POD) randomized weight-loss intervention among adults. J Med Internet Res 2011; 13: e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martin CK, Miller AC, Thomas DM, et al. Efficacy of SmartLossSM, a smartphone-based weight loss intervention: Results from a randomized controlled trial. Obesity 2015; 23: 935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fukuoka Y, Gay CL, Joiner KL, et al. A novel diabetes prevention intervention using a mobile app: A randomized controlled trial with overweight adults at risk. Am J Prev Med 2015; 49: 223–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bacigalupo R, Cudd P, Littlewood C, et al. Interventions employing mobile technology for overweight and obesity: An early systematic review of randomized controlled trials. Obes Rev 2013; 14: 279–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang T, Chopra V, Zhang C, et al. The role of social media in online weight management: Systematic review. J Med Internet Res 2013; 15: e262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turner-McGrievy GM, Tate DF. Weight loss social support in 140 characters or less: Use of an online social network in a remotely delivered weight loss intervention. Transl Behav Med 2013; 3: 287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavallo DN, Tate DF, Ward DS, et al. Social support for physical activity-role of Facebook with and without structured intervention. Transl Behav Med 2014; 4: 346–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hales S, Davidson CR, Turner-McGrievy GM. Varying social media message types differentially impacts engagement in a behavioural weight loss intervention. Transl Behav Med 2014; 4: 355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merchant G, Weibel N, Patrick K, et al. Click “like” to change your behavior: A mixed methods study of college students’ exposure to and engagement with Facebook content designed for weight loss. J Med Internet Res 2014; 16: e158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Napolitano MA, Hayes S, Bennett GG, et al. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity (Silver Spring) 2013; 21: 25–31. [DOI] [PubMed] [Google Scholar]
- 16.Buis LR, Hirzel L, Turske SA, et al. Use of a text message program to raise type 2 diabetes risk awareness and promote health behavior change (part I): Assessment of participant reach and adoption. J Med Internet Res 2013; 15: e281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerber BS, Stolley MR, Thompson AL, et al. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: A feasibility study. Health Informatics J 2009; 15: 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lim MSC, Wright C, Hellard ME. The medium and the message: Fitting sound health promotion methodology into 160 characters. JMIR MHealth UHealth 2014; 2: e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hwang KO, Ottenbacher AJ, Green AP, et al. Social support in an Internet weight loss community. Int J Med Inform 2010; 79: 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leahey T, Rosen J. DietBet: A web-based program that uses social gaming and financial incentives to promote weight loss. JMIR Serious Games 2014; 2: e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Staiano AE, Abraham AA, Calvert SL. The Wii Club: Gaming for weight loss in overweight and obese youth. Games Health J 2012; 1: 377–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hswen Y, Murti V, Vormawor AA, et al. Virtual avatars, gaming, and social media: Designing a mobile health app to help children choose healthier food options. J Mob Technol Med 2013; 2: 8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Purnell JQ, Gernes R, Stein R, et al. A systematic review of financial incentives for dietary behavior change. J Acad Nutr Diet 2014; 114: 1023–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pagoto S, Schneider K, Jojic M, et al. Evidence-based strategies in weight-loss mobile apps. Am J Prev Med 2013; 45: 576–582. [DOI] [PubMed] [Google Scholar]
- 25.Pagoto S, Bennett GG. How behavioral science can advance digital health. Transl Behav Med 2013; 3: 271–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004; 31: 143–164. [DOI] [PubMed] [Google Scholar]
- 27.Bandura A. Social cognitive theory of self-regulation. Theor Cogn Self-Regul 1991; 50: 248–287. [Google Scholar]
- 28.Hales S, Turner-McGrievy G, Fahim A, et al. A mixed-methods approach to the development, refinement, and pilot testing of social networks for improving healthy behaviors. JMIR Hum Factors 2016; 3: e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burns RJ, Donovan AS, Ackermann RT, et al. A theoretically grounded systematic review of material incentives for weight loss: Implications for interventions. Ann Behav Med 2012; 44: 375–388. [DOI] [PubMed] [Google Scholar]
- 30.Promberger M, Marteau TM. When do financial incentives reduce intrinsic motivation? Comparing behaviors studied in psychological and economic literatures. Health Psychol 2013; 32: 950–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Strohacker K, Galarraga O, Williams DM. The impact of incentives on exercise behavior: A systematic review of randomized controlled trials. Ann Behav Med 2014; 48: 92–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hales S, Turner-McGrievy GM, Wilcox S, et al. Social networks for improving healthy weight loss behaviors for overweight and obese adults: A randomized clinical trial of the social pounds off digitally (Social POD) mobile app. Int J Med Inf 2016; 94: 81–90. [DOI] [PubMed] [Google Scholar]
- 33.Sutin AR, Ferrucci L, Zonderman AB, et al. Personality and obesity across the adult lifespan. J Pers Soc Psychol 2011; 101: 579–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Munro IA, Bore MR, Munro D, et al. Using personality as a predictor of diet induced weight loss and weight management. Int J Behav Nutr Phys Act 2011; 8: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sutin AR, Terracciano A. Personality traits and body mass index: Modifiers and mechanisms. Psychol Health 2016; 31: 259–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hampson SE, Edmonds GW, Goldberg LR, et al. Childhood conscientiousness relates to objectively measured adult physical health four decades later. Health Psychol 2013; 32: 925–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jokela M, Batty GD, Nyberg ST, et al. Personality and all-cause mortality: Individual-participant meta-analysis of 3,947 deaths in 76,150 adults. Am J Epidemiol 2013; 178: 667–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: A systematic review of the literature. J Am Diet Assoc 2011; 111: 92–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shephard R. PAR-Q, Canadian Home Fitness Test and exercise screening alternatives. Sports Med 1988; 5: 185–195. [DOI] [PubMed] [Google Scholar]
- 40.Benet-Martinez V, John OP. Los Cinco Grandes across cultures and ethnic groups: Multitrait multimethod analyses of the Big Five in Spanish and English. J Pers Soc Psychol 1998; 75: 729–750. [DOI] [PubMed] [Google Scholar]
- 41.National Cancer Institute. Theory at a glance: A guide for health promotion practice. http://www.sbccimplementationkits.org/demandrmnch/wp-content/uploads/2014/02/Theory-at-a-Glance-A-Guide-For-Health-Promotion-Practice.pdf (2005, accessed 11 March 2014).
- 42.John LK, Loewenstein G, Troxel AB, et al. Financial incentives for extended weight loss: A randomized, controlled trial. J Gen Intern Med 2011; 26: 621–626. [DOI] [PMC free article] [PubMed] [Google Scholar]