Abstract
Objective
The study’s objective was to assess factors contributing to the use of smart devices by general practitioners (GPs) and patients in the health domain, while specifically addressing the situation in Germany, and to determine whether, and if so, how both groups differ in their perceptions of these technologies.
Methods
GPs and patients of resident practices in the Hannover region, Germany, were surveyed between April and June 2014. A total of 412 GPs in this region were invited by email to participate via an electronic survey, with 50 GPs actually doing so (response rate 12.1%). For surveying the patients, eight regional resident practices were visited by study personnel (once each). Every second patient arriving there (inclusion criteria: of age, fluent in German) was asked to take part (paper-based questionnaire). One hundred and seventy patients participated; 15 patients who did not give consent were excluded.
Results
The majority of the participating patients (68.2%, 116/170) and GPs (76%, 38/50) owned mobile devices. Of the patients, 49.9% (57/116) already made health-related use of mobile devices; 95% (36/38) of the participating GPs used them in a professional context. For patients, age (P < 0.001) and education (P < 0.001) were significant factors, but not gender (P > 0.99). For doctors, neither age (P = 0.73), professional experience (P > 0.99) nor gender (P = 0.19) influenced usage rates. For patients, the primary use case was obtaining health (service)-related information. For GPs, interprofessional communication and retrieving information were in the foreground. There was little app-related interaction between both groups.
Conclusions
GPs and patients use smart mobile devices to serve their specific interests. However, the full potentials of mobile technologies for health purposes are not yet being taken advantage of. Doctors as well as other care providers and the patients should work together on exploring and realising the potential benefits of the technology.
Keywords: mHealth, general practitioners, acceptance, smartphone, tablet, mobile health, digital divide
Introduction
Apps and smart mobile devices are now being used ubiquitously. While previously, many perceived them as necessary, but nevertheless bothersome tools that should best be avoided by non-technical users, the devices have meanwhile become an integral part of everyday life, both for private use, but often also in professional contexts. For example, in 2014, 58% of the German population already used a smartphone and over 50% had access to mobile internet services.1 Usage rates are continually growing.2
This trend also applies to medicine and health. Here, patients use mobile devices and apps to obtain health information or to keep track of and manage their own health-related issues or those of their loved ones.3,4 Typical applications in this context are, for example, medication reminders or fitness and health apps that are able to record and possibly evaluate bodily functions (e.g. blood pressure or blood glucose) or fitness data. While there are a number of recent studies dealing with using mobile devices and apps in medicine,5 these are often about pilot projects for specific problems6 or focus on economic aspects.7–9
Evaluating factors affecting the use of information technology
Research into the use of mobile and other information technology (IT) in health-related contexts often focuses on specific design or implementation aspects,10 specific use cases and health problems11 or non-user-centred technical aspects,12 but does not always consider how end users, e.g. clinicians or patients, perceive the available mobile offers in a more general sense. Similarly, the influence the use of the technology may have on the relationship between both sides is often not taken into account. Nevertheless, both the (positive or negative) perceptions users have of specific technologies as well their influences on the patient–physician relationship may have an impact on the outcome, i.e. on whether the technology can benefit users on an individual or even societal level.13
Technology’s influence on the patient–physician relationship
There has long been a call for transforming the relationship between patients and physicians from one that was traditionally rather paternalistic,14,15 with the physicians deciding the best course of action without including the patients in the decision process, to a participatory approach, with patients taking a more active role. While previously, e.g. as described by Emanuel and Emanuel,14 models meant to increase ‘patient involvement’ still assigned a central role to the physicians as those providing the information or at least helping with its interpretation, possibly agreeing on the best course of action via deliberation between both parties, in the context of mobile and internet-based dissemination of information, ‘technology’ – with apps and other mHealth solutions being no exception – is now often taking on the role of ‘information provider’ for patients, albeit often without the filtering and interpretation physicians are capable of based on their knowledge. It is questionable, e.g. as once again noted by Lupton and Jutel,16 to what extent users lacking a professional medical background are actually capable of using the information they thus obtain in a manner that is beneficial for them. Here, the main problems are whether they are able to determine the validity and applicability of the content provided (or the lack thereof), and whether they realise that they may need help with its interpretation or application in order to be able to use it as a basis for their ‘empowerment’.
On the other hand, considering the possibilities mobile technologies offer for gaining access to health datasets that were previously hard to obtain, ‘participation’ and ‘empowerment’ also need to extend to the professional side. In the surveys performed in the context of our work, it was therefore of interest whether general practitioners (GPs), but also patients, were already making use of mobile technologies and whether they did so on an individual or on a collaborative level. An investigation into the relationship between the surveyed GPs and patients was therefore also attempted in the line of the presented study, similar to our previous work, where this was covered for a clinical setting.17
Evaluating user acceptance
Regarding user acceptance, there is also an additional aspect to consider. Whether a specific technology is not only seen as expedient but actually successful also rests with the customers, and in professional contexts, may well be decided on the work floor.18 While for IT systems in general contexts, this is a well-known aspect, for health-related settings, this interest in the demand side has only recently increased. Here, there is now greater recognition of the fact that the perception of users regarding usefulness, ease of use, reliability as well as security and privacy – often taken as independent factors, but nevertheless contributing towards user satisfaction – can serve as driving influences for a successful adoption of mHealth (mobile health) solutions.19–21
Over time, numerous approaches have been proposed, evaluated and applied to gain insights into the factors that drive users towards or away from using specific IT-based solutions. Models often mentioned for this purpose are for example the ‘technology acceptance model’ (TAM and TAM2),22–24 originally proposed in the late 1980s, as well as the newer ‘unified theory of acceptance and use of technology’ (UTAUT).25 Essentially, TAM builds on the ‘theory of reasoned action’ (TRA),26,27 which tries to explain individual’s voluntary behaviour via the relationship between attitudes and behaviours within human action, which has proved useful for understanding a variety of behaviours.10 Following this theory, intent always precedes the actual behaviour.28 TAM, as an extension of TRA, extends TRA’s attitude measures with two technology acceptance measures,10 namely perceived ease of use and perceived usefulness.
The newer TAM2 model, as an extension of TAM29 removes the attitude component, but adds a variable that aims at capturing the social influences others (e.g. peers) exert on users. In turn, these and other social factors (subjective norm, image and voluntariness) influence the perceived usefulness of the original TAM model.30 Both TAM and TAM2 were originally developed for general use, but have often been portrayed as suitable for the specific aspects one needs to consider in healthcare contexts. For example, Chismar and Wiley-Patton30 looked into whether either of the two aforementioned models are appropriate for physicians and other health professionals, and found TAM2 to be partially adequate and applicable for them. While they found a significant link between perceived usefulness and physicians’ usage intention when perceived usefulness was high, there was no such significance for perceived ease of use, the latter being a validated factor of the model that is often considered a key aspect for applying the model outside the health domain. Bearing this in mind, at least for the physicians’ evaluation, making use of this model in our study did not seem appropriate.30
Aside from the partially questionable applicability of the aforementioned models for the two user groups we wanted to evaluate, there was also another aspect that led us to refrain from using standardised and validated questionnaires as they are, for example, available for TAM or TAM2. They predominantly centre around the individual perception of usefulness and ease of use of the technology being scrutinised, in the case of TAM2 also extending to social influences exerted by peers or colleagues (see Holden and Karsh)10 that foster individuals’ positive perceptions and acceptance of technology, but often do not account for influences from beyond this group of peers. In addition, even studies making use of these and other standardised models aiming at evaluating technology acceptance often add variables to understand better the antecedents of acceptance for the IT solutions they evaluate.10
Altogether, we came to the conclusion that in the line of our chosen setting, a self-developed questionnaire not based on standardised approaches such as TAM, TAM2 or UTAUT, would better serve our purpose. We therefore took a rather generic approach in order to obtain a broad picture of the situation, with a specific focus on Germany.
Objectives
We were not only interested in identifying the manner and frequency of health-related usage of mobile technologies (devices as well as apps) by GPs and their patients, but also aimed at identifying elements contributing to their acceptance and appeal as well as barriers undermining their use. In particular, with a focus on the situation in Germany – as there are notable differences in the usage of mobile devices between different countries even within the EU31 – we wanted to determine how doctors working in general practices as well as an outpatient clientele view the use of mobile technologies, specifically apps and the smart devices used to run these apps, in health-related contexts and whether there are any notable differences between these groups.
Materials and methods
A multi-perspective study design largely similar to a study we had previously conducted17 was used. While in the previous study, clinical physicians and patients at a German university hospital were surveyed, this time, GPs and patients at GP offices in the Hannover region, Germany, were asked to participate in order to gain a better understanding of the attitudes of both parties towards mobile device usage in the context of patient care.
Instruments
Because of the reasons listed above, self-developed, non-standardised questionnaires were used for both groups of participants, with only few adaptations or additions to the questionnaires used in Illiger et al.,17 mostly to account for differences to the previously evaluated (clinical) setting. The questions covered areas such as demographics, mobile device ownership, as well as desired and actual health-related usage scenarios (see Appendices 1 and 2 for translations of the two questionnaires). Apart from single and multiple choice questions, there were also several questions in which free text answers could be given in order to gain insights into qualitative aspects.
In accordance with the requirements of the institutional review board at Hannover Medical School, before filling out the questionnaire, both patients and doctors were provided with informed consent information. For the patient-related part of the evaluation, in order to disturb the workflow in the participating practices as little as possible and to not record any personally identifying information, patient consent was obtained verbally, with those not giving their consent immediately being excluded from the study. Doctors gave their consent by filling out the electronic survey form. The evaluation was solely performed on the data obtained from the questionnaires; neither for the participating doctors nor the patients included in the study were there any face-to-face interviews, and neither were any incentives given for participation.
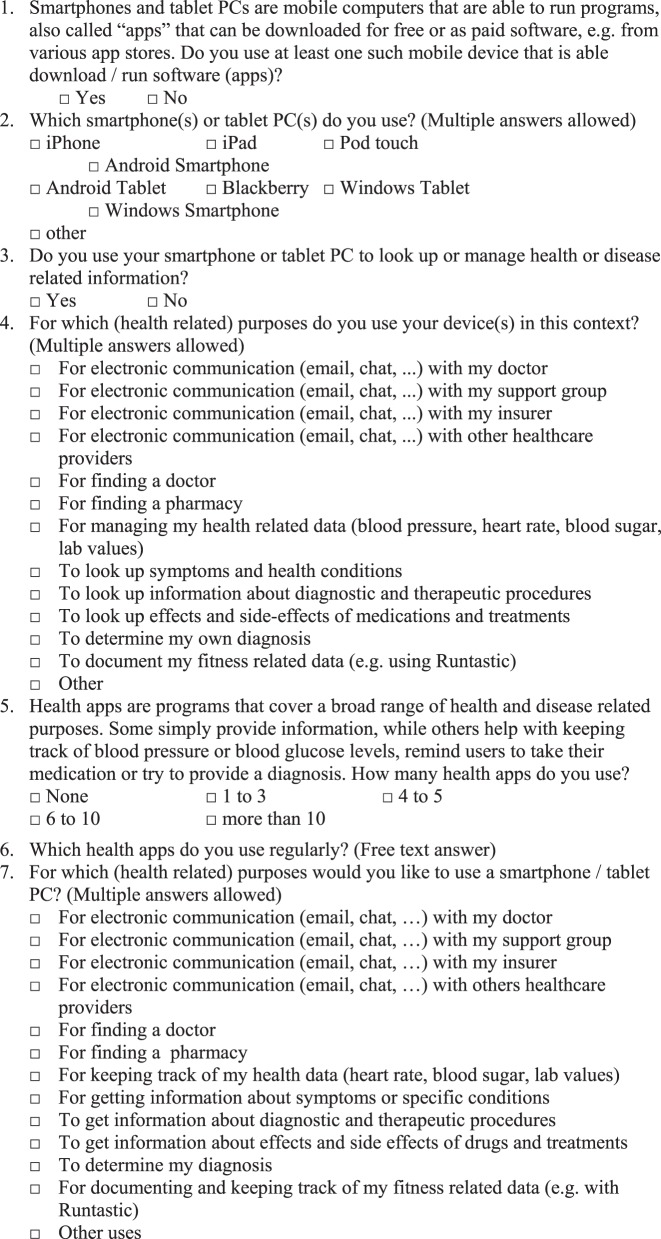
Patients’ questionnaire
The questionnaire used for the patients (see Appendix 1) consisted of altogether 20 items and started off with several questions related to the participants’ current use of smart devices (six items). This included availability, the type(s) of device(s) in use, along with items covering actual health-related uses and the number of apps used for such purposes. An additional five questions dealt with potential future use scenarios of mobile devices for health and fitness-related purposes as well as the patient’s opinions about doctors using mobile technologies for specific use cases and whether the patients confronted their doctors with information or data they had obtained using (health) apps (and whether this was done by accessing a mobile web page rather than a distinct app). There were also questions regarding the patients’ knowledge about quality initiatives for health apps and websites, which was, however, published separately.32
The questionnaire ended with three questions asking for demographic information (age, gender, school-leaving qualifications) and a final free text question to give participants an opportunity for additional comments. There were no questions related to the patients’ current or general health status.
Once collected, the paper-based questionnaires, which had been formatted according to the requirements of the EvaSys (Electric Paper Evaluationssysteme GmbH) software employed for this purpose, were scanned and the results entered into a database. A manual check for inconsistencies between the questionnaires and the scan results was also performed, because, unfortunately, several participants had not marked the answers as required by the scanning software (e.g. with check marks only marginally touching the corresponding checkboxes).
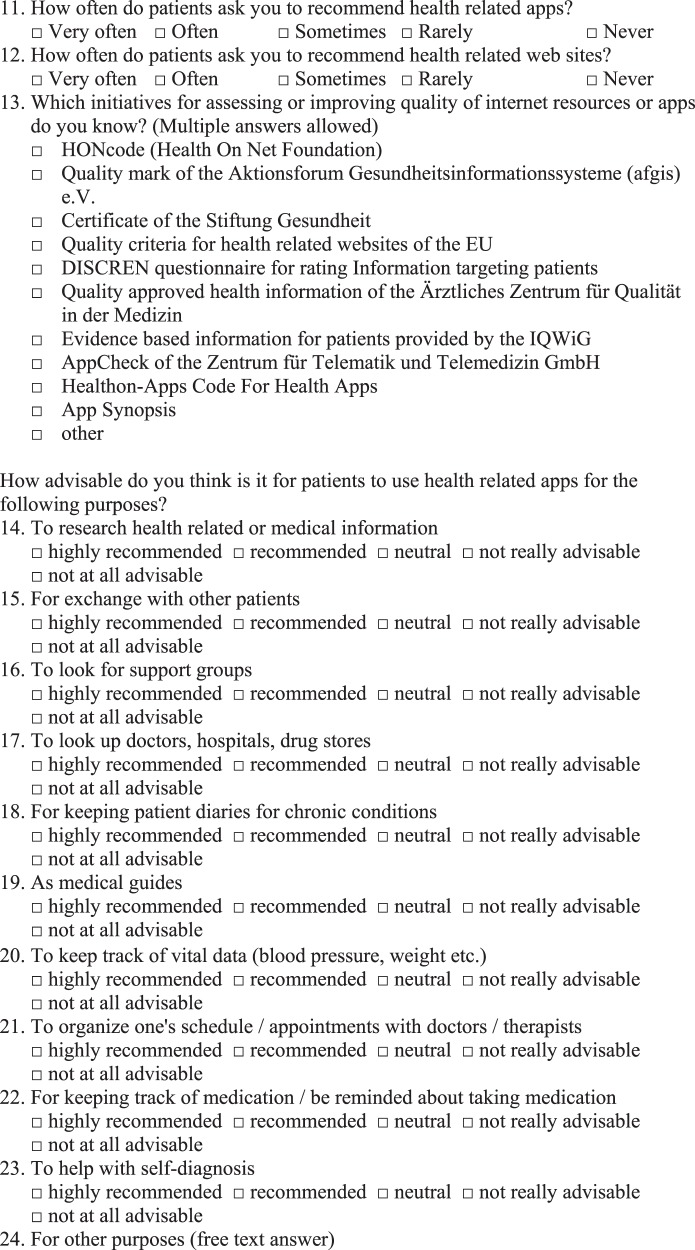
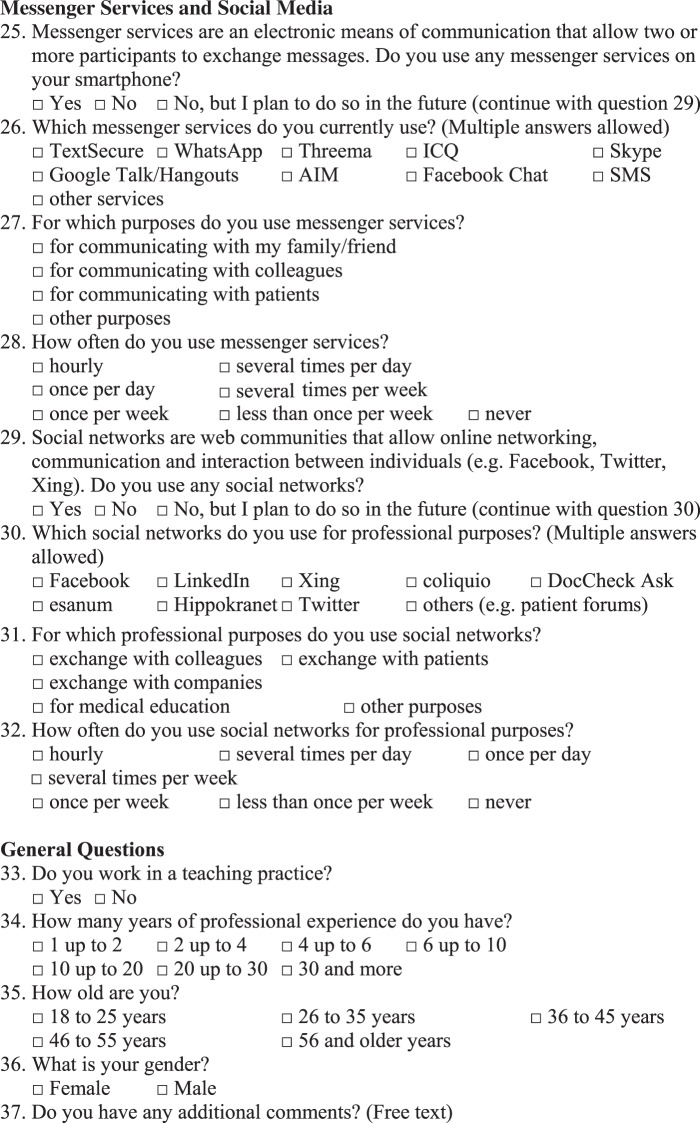
Doctors’ questionnaire
For the participating doctors, the electronically administered questionnaire (see Appendix 2) consisted of 37 questions, covering aspects of availability of mobile technologies as well as actual usage of mobile technologies (five questions) and perceived future use (three questions), but also items related to patients using mobile technologies (including both current use and advisability of mobile technologies for patients, 15 questions) and quality-related aspects (one question, evaluated separately, see Behrends et al., 2015).32 An additional set of questions (eight questions) dealt with the use of social media-related apps and services for (professional) medical purposes by the participating GPs (evaluated separately, see Behrends et al., 2015).32 Finally, there were also four questions related to demographic data (age, gender, professional experience and whether the doctors had a teaching practice) and one free field giving the participants the opportunity for additional statements. Again, the demographic data were collected in order to be able to determine whether factors such as age, gender or professional experience have an influence on the use of mobile technologies or not.
The questionnaires were made available using the EvaSys survey tool (Electric Paper Evaluationssysteme GmbH). Only fully completed surveys were included in the evaluation. There was no possibility to determine the timespan the participating physicians had needed for filling out the questionnaire, and neither was there a possibility to determine how many had started, but not finished, the questionnaire.
Recruitment
Patients’ recruitment
The patients were surveyed in eight local general practices located in the greater Hannover area. Eight students of the University of Applied Sciences and Arts Hannover, professionally trained in interview techniques by a social scientist, conducted the interviews. Each practice was only visited on a single date during the survey period (between 29 April 2014 and 20 May 2014) and these visits took place during the morning hours (approx. 09.00–12.00 hours). During the visits, every second patient arriving at these practices was asked to participate, and once they had given their verbal consent, they were provided with a paper-based questionnaire. The students administered the survey, explained the background of the study, asked for informed consent and gave basic assistance to the participants. However, there were no face-to-face interviews.
Thus, a sample of 170 patients out of the 185 who had initially been invited to participate was obtained, corresponding to a participation rate of 91.9%. Fifteen patients who met the inclusion criteria (being of age, i.e. at least 18 years old, competent in the German language, no reading disabilities) but did not give their consent were excluded.
Doctors’ recruitment
Using an email sent by the local branch of the professional association of family physicians, GPs in the Hannover region were invited to participate in a separately conducted, anonymous electronic survey. For this part of the study, answers were obtained between 24 April 2014 and 3 June 2014. Altogether, 50 out of 412 (12.1%) eligible doctors responded.
Statistical evaluation
Fisher’s exact test (two-sided, alpha = 0.05 with Monte Carlo approximation, 2000 replicates) was used to test for dependencies between age, gender and education or professional experience, respectively. The test was applied using GNU R (version 3.1.2). For the participating patients, regarding schooling, the numbers of those who had attended primary school or lower secondary school were aggregated because there was only a single participant who had finished only primary school.
Results
Patients’ survey
Sociodemographics
The acquired sociodemographic data of the participating patients is shown in Table 1.
Table 1.
Sociodemographic data of the participating patients (N = 170).
| Feature | Attribute | n (%) |
|---|---|---|
| Gender | Female | 86 (50,6) |
| Male | 71 (41.8) | |
| Not specified | 13 (7.7) | |
| Age | 18 to 25 | 33 (19.4) |
| 26 to 35 | 28 (16.5) | |
| 36 to 45 | 21 (12.4) | |
| 46 to 55 | 15 (8.8) | |
| 56 to 67 | 33 (19.4) | |
| 68 and older | 29 (17.1) | |
| Not specified | 11 (6.5) | |
| Highest school-leaving qualification | Primary school | 1 (0.6) |
| Lower secondary school | 26 (15.3) | |
| Intermediate secondary school | 66 (38.8) | |
| Upper secondary school | 62 (36.5) | |
| Not specified | 15 (8.8) |
General aspects of usage
More than two-thirds of the participating patients were already using at least one mobile device (smartphone or tablet PC) with the ability to download and run mobile applications on various platforms (Table 2), with almost every sixth respondent indicating the use two or more types of devices. Android seemed to be the preferred platform for the participating patients.
Table 2.
Use of mobile devices and mobile platforms for the participating patients (N = 170).
| Feature | Attribute | n (%) | % of those using a mobile device (n = 116) |
|---|---|---|---|
| Mobile device users | Use of one or more mobile devices | 116 (68.2) | – |
| Use of at least two different types of devices (related to platform or form factor) | 28 (16.5) | 24.1 | |
| Device type | Android devices (smartphones, tablets aggregated) | 70 (41.2) | 60.3 |
| iOS-based devices (iPads, iPhones, iPod touch) | 51 (30.0) | 43.9 | |
| Windows-based mobile devices | 10 (5.9) | 8.6 | |
| BlackBerry devices | 2 (1.2) | 1.7 | |
| Other mobile platforms | 6 (3.5) | 5.2 |
While every patient between 18 and 25 years of age owned a mobile device (100%, 33/33), for those in their late fifties, this was only true for every second patient (48%, 16/33), and for every third patient in his late sixties (31%, 9/29). It was also the younger up to 25 years of age that used the technology for assisting them in health-related matters. Two out of three patients of this age group stated they were making use of mobile devices in health-related contexts (67%, 22/33). In contrast, such use was much less frequent for older patients: only 38% of those in their mid-thirties up to the mid-forties (14/21) and only 3% (1/29) of the pensioners (68 years and older) used their devices for health-related purposes; for the patients included in this survey, the use of smart devices (both regarding everyday use and use in a medical context) did depend on age (P < 0.01 for both purposes).
Gender did not appear to be an influencing factor for those surveyed (P > 0.99). General usage rates for mobile devices varied with educational attainment, and even more so when considering the use of mobile devices in a health-related context. While only 15% (4/26) of those who had only finished primary or lower secondary school used a mobile device for health-related purposes, this number was considerably higher for those who had finished intermediate secondary (25%, 16/65) or upper secondary school (48%, 30/62). Therefore, aside from the aforementioned significant (negative) correlation between age and the use of mobile devices (with older participants using mobile devices less often), both everyday use and use in a health-related context were also associated with school-leaving qualification (both P < 0.001): usage rates rose for those with better education. This part of the evaluation was based on the data of 168 participants, as two participants had omitted information on whether they were using a mobile device.
Health-related activities assisted by mobile devices
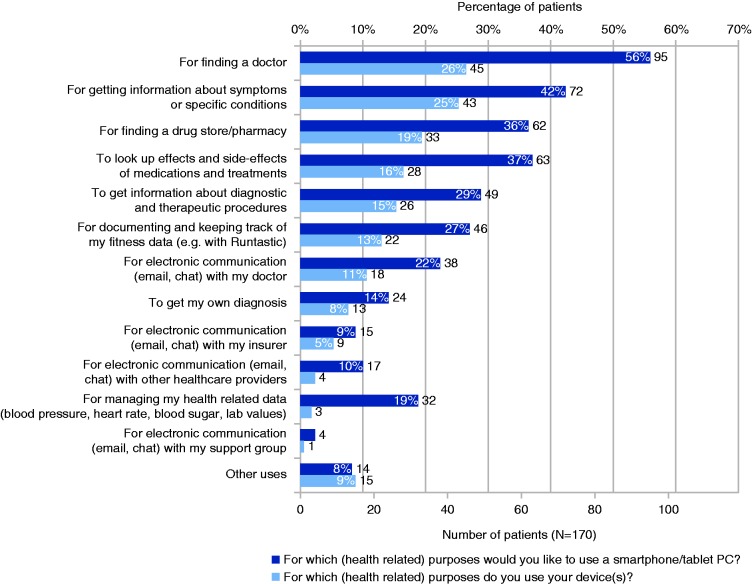
Overall, 33.5% (57/170; 41.9% or 47/116 of those owning a mobile device) of the participating patients admitted to using their device(s) for managing their health-related data, for looking up information related to questions of health and medicine, communication with their doctors or other care providers or other health-related purposes (Figure 1). For those acknowledging health-related usage, finding doctors, researching information about specific symptoms or diseases and pharmacies were frequently mentioned, as was looking for information about the (adverse) effects of drugs and treatments as well as finding out specifics about diagnostic or therapeutic procedures or the use of mobile devices for fitness-related purposes. Mobile communication was most commonly used for exchanging information with doctors. Fewer than one in every four patients already using a smart device admitted to using it for trying to determine their own diagnosis (23% or 13/57).
Figure 1.
Actual health-related use cases versus potential future usage scenarios of mobile devices (N = 170).
Potential future use scenarios envisaged by patients
When asking the participants what they would potentially like to use mobile devices for, searching for doctors and pharmacies were again frequently mentioned, as were looking up information about symptoms and medical conditions, (adverse) effects of drugs and treatments in general, and seeking information about diagnostic and therapeutic procedures. The participants also found keeping track of their fitness-related data to be modestly attractive (Figure 1). Regarding communication purposes, only about every fifth patient envisioned using mobile technology to keep in touch with doctors or other healthcare providers as well as insurers or patient support groups. Determining one’s own diagnosis was also not given high priority as a potential (future) use case for mobile devices and apps (Figure 1). For all potential use cases, the proportion of those who could envision specific health-related usage scenarios for the future was higher for those patients who were already using mobile devices.
Of those already using one or more smart devices, 18.1% (21/116) used one or more health or fitness-related apps on their device(s). In the corresponding free text field, fitness-related apps were mentioned most often (10 mentions), with medication-related apps (drug databases, pill reminders) following (two mentions). There were also mentions of apps helping with finding doctors and pharmacies as well as allergy-related and calorie counting apps (one each). The majority of the listed apps were clearly health apps rather than medical apps.
The role of apps in the relationship between patients and doctors
To determine whether patients’ use of apps is a potential factor in the relationship between doctors and patients, patients were also asked about how often they confront their doctors with information from health-related apps. Only one participant admitted to doing so ‘often’, another 5.3% (9/170) participants admitted to ‘sometimes’ presenting such information to their doctor, while 8.2% (14/170) of them ‘rarely’ did so. A majority of 77.6% (132/170) of the participants said they had ‘never’ shown such information to their doctor; 8.2% (14/170) participants had chosen not to answer this question.
It is also noteworthy that out of the 162 patients who had answered the question about whether their doctor had ever recommended a health-related app, there was not even a single participant who had actually received such a recommendation.
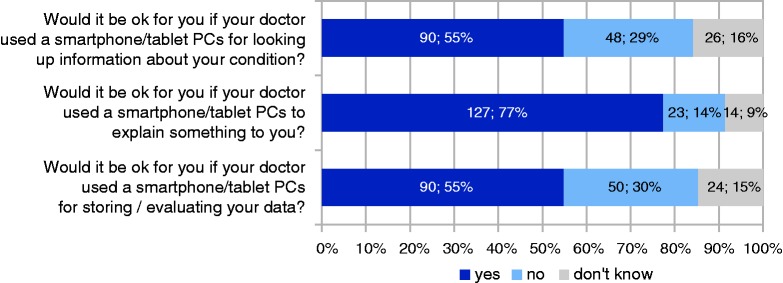
Patients’ opinions about doctors using mobile devices for specific reasons
In addition to aspects related to their own use of mobile devices, we also wanted to identify if patients had possible reservations about their doctors employing mobile devices in care contexts (Figure 2). A little more than half of those who had chosen to answer the corresponding questions were comfortable with their doctor using a mobile device to store and evaluate their data or to look up specifics about their condition. More than three out of four participants approved their doctor’s use of mobile devices for explanatory purposes.
Figure 2.
Patients’ approval of their doctors’ use of smart devices (percentages and absolute numbers for N = 164 participants who had answered these questions).
Doctors’ results
Sociodemographics
The sociodemographic data of the responding physicians are listed in Table 3; the proportions are a close match for the data available for physicians in Germany.33
Table 3.
Sociodemographic data of the participating doctors (N = 50).
| Feature | Attribute | n (%) |
|---|---|---|
| Gender | Female | 17 (34%) |
| Male | 33 (66%) | |
| Age | 36–45 | 12 (24%) |
| 46–55 | 21 (41%) | |
| 55 and older | 17 (34%) | |
| Work experience (years) | Min. 4, less than 6 | 1 (2%) |
| Min. 6, less than 10 | 3 (6%) | |
| Min. 10 less than 20 | 13 (26%) | |
| Min. 20, less than 30 | 25 (50%) | |
| 30 and longer | 8 (16%) | |
| Teaching practice? | Yes | 25 (50%) |
| No | 25 (50%) |
General aspects of usage
About three-quarters (76%, 38/50) of the participating GPs were already using at least one mobile smart device (phone or tablet PC). In contrast to the patients’ results, doctors seemed to favour the iOS. Most of the doctors had originally purchased their devices for private purposes, only few had also done so with professional use in mind (Table 4).
Table 4.
Use of mobile devices and mobile platforms for the participating doctors (N = 50).
| Feature | Attribute | n (%) | % of those using a mobile device (n = 38) |
|---|---|---|---|
| Mobile device users | Use of one or more mobile devices | 38 (76) | – |
| Use of at least two different types of devices (related to platform or form factor) | 13 (26) | 34 | |
| Device type | Android devices (smartphones, tablets aggregated) | 17 (34) | 45 |
| iOS-based devices (iPads, iPhones, iPod touch) | 28 (56) | 74 | |
| Windows-based mobile devices | 5 (10) | 13 | |
| BlackBerry devices | 0 (0) | 0 | |
| Other mobile platforms | 5 (10) | 13 | |
| Original reason for purchasing the mobile devices | Private purposes | 36 (72) | 95 |
| Private as well as professional purposes | 22 (44) | 58 | |
| Solely professional purposes | 3 (6) | 8 |
Age, gender, and work experience in context with the usage of mobile devices and apps
Regarding everyday use, compared to the participating patients, the differences in usage rates between the various age groups were comparatively small. Seventy-five per cent (9/12) of those below 45 years of age and 81% (172/21) of those between 46 and 55 years already used mobile devices, and for doctors above 56 years of age, 65% were still using mobile devices. For professional use versus age, there was even less variation: while all of those below the age of 45 years who were using a mobile smart device for any purpose admitted to professional use (75%, 9/12), for the two groups between 46 and 55 years of age as well as 56 years and older, there was only one participant each who did not use mobile devices accordingly (46–55 years: 76% or 16/21; 56 years and older: 65% or 11/17). Thus, in contrast to the patients, the usage of mobile devices, specifically in a professional (health-related) context did not correlate with age (P = 0.73). Also, while usage rates for female doctors were somewhat lower both with respect to use in general (65%, 11/17) as well as regarding professional use (59%, 10/17) than they were for male participants (everyday use: 82%, 27/33; professional use: 79%, 26/33), this difference was not significant (P = 0.19 for both everyday as well as professional use).
Neither did the use of mobile devices for professional purposes depend on the years of professional experience (P > 0.99). While there was only a single participant with less than 6 years of professional experience who was using a mobile device and was using it for professional purposes as well, variations for the other groups were again relatively small and ranged from 67% to 80% for use in everyday contexts and 67% to 75% regarding the use of mobile devices in a professional context. The exact numbers for each group are shown in Table 5.
Table 5.
Everyday and professional use vs. professional experience.
| Professional experience | Percentage of those using a mobile device for any purpose (n/N) | Percentage of those using a mobile device for professional purposes (n/N) |
|---|---|---|
| Min. 4, less than 6 years | 100% (1/1) | 100% (1/1) |
| Min 6, less than 10 years | 67% (2/3) | 67% (2/3) |
| Min 11, less than 20 years | 69% (9/13) | 69% (9/13) |
| Min. 20, less than 30 years | 80% (20/25) | 72% (18/25) |
| 30 years and more | 75% (6/8) | 75% (6/8) |
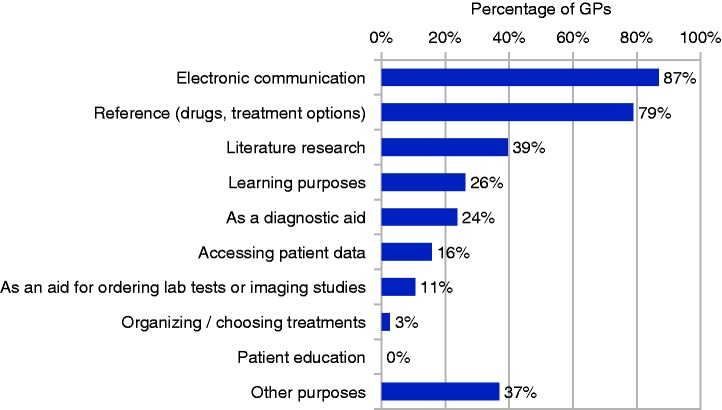
Doctors’ use of mobile devices in a medical context
The majority of those GPs who were using mobile device(s) were employing them for professional purposes (see Table 4 and Table 5), independent of whether they had originally been acquired with professional or private use in mind. The most common areas of device usage in professional contexts were electronic communication as well as reference purposes, e.g. looking up information about drug or treatment options. The devices were less frequently employed for other purposes (see Figure 3).
Figure 3.
Percentages of GPs already using their mobile devices for various use scenarios in a professional medical contexts (N = 38).
When asked about the apps they were already using on their devices, apps providing drug-related information (e.g. medication databases) were mentioned by more than half of the doctors who had provided a free text answer in this context (53%, 16/30), and apps offering information about specific diseases or medical specialties were similarly popular (53%, 16/30). One third of those who had answered (33%, 10/30) also used apps providing access to literature, journals and medical news (not including eBooks). Apps containing reimbursement and documentation-specific information (International Classification of Disease/billing codes) were mentioned five times.
There were also several references to apps for accessing internet-based reference services (e.g. Wikipedia), for looking up other healthcare providers and services (e.g. pharmacies) and for eLearning or training purposes; one participant was already using an app allowing access to his office-based medical records system. Two participants explicitly stated that they were using their smart devices for nothing but communication.
Additional use scenarios general practitioners envisage
For those GPs who had provided information about additional usage scenarios where they thought mobile devices might be helpful in their practice, using them for support during home visits or access to their office-based systems was most often mentioned. Most other mentions dealt with looking up various kinds of information (Table 6).
Table 6.
Mentions of specific use scenarios in the free text answers provided by the GPs (N = 38).
| Envisioned usage | n (%) |
|---|---|
| General support during home visits | 12 (32) |
| Access to the office-based software and patient records (e.g. for documenting a visit or retrieving information from a patient’s file) | 9 (24) |
| Mentions of researching information in general | 9 (24) |
| Looking up specific information (lab values, current medical guidelines, evidence-based information) | 6 (16) |
| Communication-related (phone calls in emergency situations, video consultations with colleagues) | 3 (8) |
| eLearning, providing information to patients, looking up colleagues or other care providers, reimbursement specific information | Single mentions each |
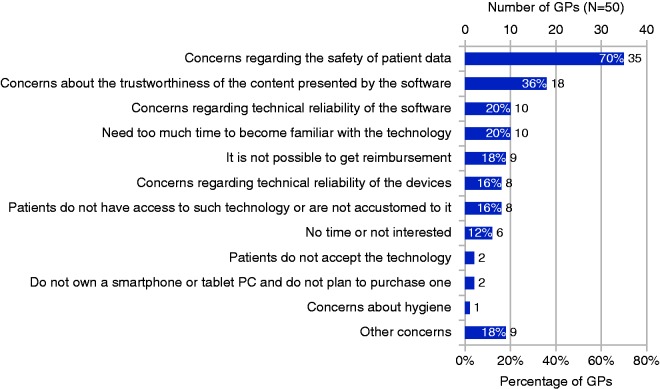
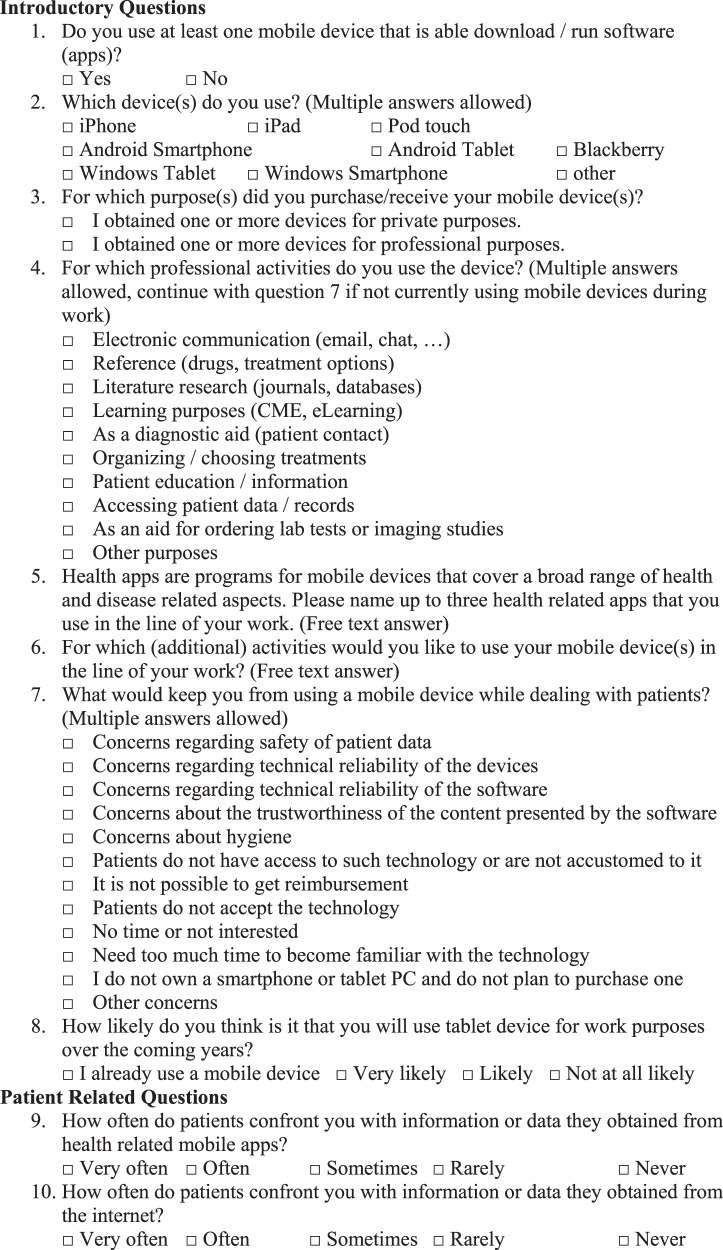
Doctors’ concerns with respect to health apps
Irrespective of their actual use, qualms about using mobile devices and apps (Figure 4) were primarily voiced about the safety of the patients’ data, but also about the trustworthiness of the presented content and the software’s technical reliability. For some, a lack of familiarity with mobile technologies was also seen as a deterrent for professional use. Despite hygiene (or the lack thereof) often having a serious impact on the patient safety in healthcare environments,34 there was only one participant admitting to being concerned about hygiene issues being caused by mobile devices.
Figure 4.
Factors that could potentially contribute to doctors (N = 50) not using mobile technologies in professional contexts.
Mobile health-related activities doctors think advisable for their patients
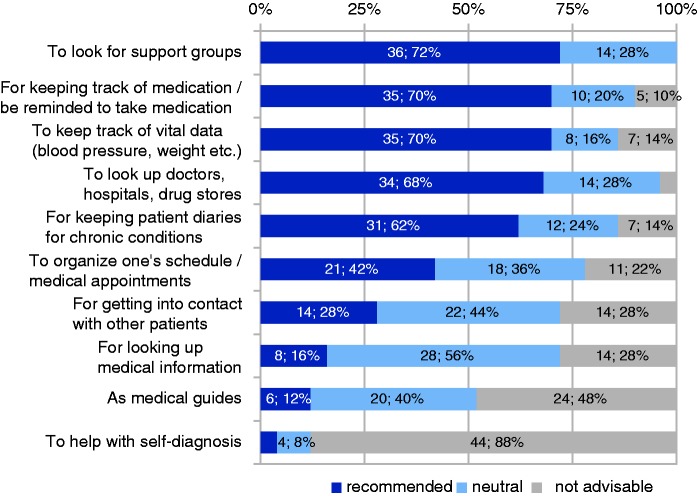
When asked about health-related use cases for mobile devices they thought advisable for patients (Figure 5), mentions of looking up support groups, keeping track of vital data, using medication reminders, looking up doctors, hospitals or pharmacies and keeping patient diaries for chronic conditions were particularly frequent, while most respondents frowned upon their patients using mobile devices and apps for helping with self-diagnosis or as medical guides (Figure 5).
Figure 5.
Opinions regarding the advisability of patients using mobile devices for various use cases (N = 50 participating GPs). In contrast to the original data, in which a five-point scale was used (‘highly recommended’, ‘recommended’, ‘neutral’, ‘not really advisable’, ‘not at all advisable’), the values for ‘highly recommended’, ‘recommended’ are aggregated, as are the values for ‘not really advisable’ and ‘not at all advisable’.
Apps versus the web as a source of patient information
Just over half of the participating GPs (52%, 26/50) indicated that their patients sometimes confronted them with information they had found on the internet, and for 38% (19/50) this was a relatively common occurrence. In contrast, with app-based information, this happened less frequently: Only for 10% (5/50) of the participants was this a common occurrence (values for ‘very often’ or ‘often’ being aggregated), while for 32% (16/50) this only happened sometimes. Another 30% (15/50) were only rarely in this situation and 28% (14/50) could not remember any occurrence of this. Similarly, most GPs were rarely or never asked to recommend health-related apps (78%, 39/50), while this happened ‘often’ or ‘very often’ to 10% (5/50) of the participating doctors. In contrast, recommendations for health-related web sites were requested more often: 40% (20/50) of the participants had often or sometimes been asked about such recommendations. To the other 60% (30/50) this happened rarely or never.
Discussion
Demographic factors influence the way mobile devices are used
Similar to other studies, our results confirm that the acceptance and use of mobile technologies are inextricably linked with various sociodemographic factors.17,35,36 For patients, education (and age) were crucial factors, with those with higher education (and/or being younger) more frequently using the technology, while for GPs (with a generally high level of education) these factors had less influence. Similar dependencies are often described for the level of income. A preference for Android-based devices for low(er) incomes versus iOS for those with higher incomes is sometimes described in the literature,37 and indeed there was a preference towards Android for the participating patients (41.2%, 70/116 of those using mobile devices), while iOS was the most popular mobile operating system for the participating GPs (74%, 28/38 again of those already using mobile devices), with an expected income higher than that of most patients. Similar to educational attainment, income can have a significant influence on health-related behaviours in general.38 Altogether, our results are indicative of the ‘digital divide’ that is often mentioned in the literature and typically attributed to factors such as age, gender (which we were unable to confirm from our results), income or education39–42 for various populations. Nevertheless, while for healthcare the (health) app ecosystems for the various mobile platforms have been shown to differ on the supply as well as the demand side,43 and we would have liked to find further evidence for this in our data, based on the relatively few apps named by the participants on ‘both sides of the stethoscope’, we were unable either to support or refute such a difference with any degree of certainty, e.g. with respect to the proportion of apps being in use on each platform, for specific health purposes, for providing certain functionalities, or as a means of interaction with other individuals or IT systems. Due to the constantly evolving nature of apps and mobile technologies, questions arising in this context, namely identifying reasons for variations between ecosystems and their potential positive as well as negative impact (e.g. related to the accessibility of specific mHealth solutions for certain user groups and its correlation to demographics), warrant continuous monitoring from the scientific community as well as commercial players in the field.
Concerns about apps and mobile technology
One of the most surprising results in our study was that in spite of the growing popularity of health-related apps, the majority of the participating patients had never confronted their doctors with information obtained from an app (77.6%, 132/170), and none of them had asked for recommendations regarding health-related apps. In comparison, many of the interviewed GPs had at least sometimes been confronted with app-based health information (42%, 21/50), and almost a third of the surveyed GPs (32%, 16/50) had already asked for app recommendations. The seeming contradiction between the results for both parties can be partly explained by the simple fact that, on average, GPs in Germany see a little more than 5044 patients per day, and thus their chance of being asked for such recommendations by any of their patients is relatively high.
With 68.2% (116/170), the distribution of smartphones and tablets (including iOS, Android, Blackberry and Windows phone-based phones and tablets as well as other mobile smart devices) in the patients’ stratum was somewhat above the average for the German population, with 63%,45 possibly due to the limited geographical area (Hannover region) where our data were obtained; 49.9% (57/116) of the surveyed patients who were using a mobile device additionally used their devices in health-related contexts. Despite this, our results showed only little app or mobile device-related interaction between doctors and patients. As mobile technologies were quite popular with GPs (76%, 38/50), who were more than willing to use them in a professional health context (95%, 36/38), this leads to the question as to why our data showed so little cooperation between the two parties in this matter.
On the physician’s side, this may be due to the fact that many health-related mobile apps and services that are available for patients have only limited compatibility with the IT systems GPs employ in their practices, e.g. due to non-standardised data formats or mechanisms for sharing data,46 but there are also data protection concerns, as voiced by a large number of the participants (70%, 35/50). On the other hand, any interruption of the normal workflow (and thus interference with the efficiency of care and loss of valuable time), may further increase potential barriers. With only a few minutes of direct contact being available per patient (evident from the large number of patients seen on average),44 reviewing detailed records acquired by patients may not have seemed worthwhile, e.g. due to doubts about the quality of such data and scepticism about the benefits of evaluating the data.46 Open questions related to reimbursement13 may also have contributed to the lack of interest in (collaborative) app use, and in fact, this was mentioned by 18% (9/50) of the participating GPs as keeping them from using apps (see also Figure 4).
For patients, there were also several factors that could be identified as potential deterrents for using apps in health-related contexts, be it at all or in contact with their physicians. Almost every third patient (28.2%, 48/170) had qualms about their doctors using a mobile device to look up information specific to their condition during a visit, some of them specifically voicing their distaste by stating in the free text field at the end of the survey that they felt they would be unable to trust physicians who were using ‘new media’ to inform themselves while caring for them, although in contrast to the patients’ reservations, only about a quarter (24%, 9/38) of the participating GPs did so.
While the majority of the patients considered it all right for their data to be stored or evaluated on their physicians’ mobile devices (52.0%, 90/170), almost a third of the patients did not like the idea of their doctors doing so (30.5%, 50/164), with some of them explicitly mentioning data protection concerns in the free text answer field at the end of the survey, some of them stating a fear of ‘too much internet’, ‘questionable data protection’, or specifying that they were ‘not using either internet or apps, not in the past and not in the future, due to never having trusted them’. The GPs shared the patients’ sense of necessity for good data protection. They refused to use solutions that could lead to the safety of their patients’ data being compromised (70%, 35/50). It is noteworthy, that for Germany, data protection concerns have been shown to be a key issue, much more so than in other countries,47 often keeping potential users from actually accepting new technologies or (online) services,48 and this is at least partially mirrored by the answers we obtained.
Actual use cases
Superficially viewed, patients and doctors used their mobile devices for similar reasons, mostly related to reference, albeit there is a different main focus. While patients already using mobile technologies primarily searched for healthcare providers, e.g. doctors (79%, 45/57) or pharmacies (58%, 33/57), and also informed themselves about specific symptoms or conditions (75%, 43/57), they rarely employed their devices to communicate with their doctor (32%, 18/57), insurances (16%, 9/57) or other care providers (7%, 4/57). For those who had specified which apps they were using, keeping track of data for fitness-related purposes, e.g. by using apps such as Runtastic,49 was much more common (39%, 22/57) than for actual medical areas of application such as recording blood pressure or blood glucose levels (5%, 3/57). Due to the relatively low number of patients who provided insights into the health-related apps they were using, it was, however, impossible to establish whether there were any correlations between specific app types more commonly being used on a specific mobile platform. In contrast, GPs who were already using mobile technologies mainly did so for interprofessional communication (87%, 33/38), secondly for reference purposes (79%, 30/38) and literature searches (39%, 15/38), and much less frequently for aiding their diagnostic processes (24%, 9/38) or accessing patient data on their office-based systems (16%, 6/38). Notably, although many patients were comfortable with their doctors making use of mobile technologies to explain something (77.4% or 127/164 who had answered this), none of the participating doctors actually admitted to having done so.
Future expectations
Regarding communication-related activities, when asked about mobile activities they would expect to be helpful, about one fifth of the patients in our survey mentioned communication with their GPs (22.4%, 38/170). As for the actual use cases, finding information about healthcare providers such as doctors (55.9%, 95/170) and pharmacies (36.5%, 62/170) and about symptoms and conditions (42.4%, 72/170) had the highest appeal. GPs were also interested in accessing medical guidelines, information about specific medications or laboratory values as well as evidence-based information in general, but primarily they wished to use mobile technologies as a means of support during home visits (32%, 12/38) as well for accessing their office-based data during such visits (24%, 9/38). Thus, their main interest was in practical solutions providing them with access to patient-related information at the point of care, but there were no mentions of actually wanting to use mobile applications for interacting with patients, e.g. by using the devices to illustrate something to those under their care.
Technical affinity versus conservativeness in processes
It is known from earlier studies that doctors are familiar with smart mobile technology.50 However, it is surprising that one fifth of the interviewed GPs (20%, 10/50) were concerned about the possibly of having to invest too much time to become sufficiently familiar with the technology. In our opinion, this is not a contradiction. The GPs do not reject the technology itself. However, they may have reservations about having to change established processes or implementing any (new) processes that may slow down the routine in their daily practice – an issue to be clearly avoided. In this context, it would be of interest to learn how much time GPs would be willing to invest in an evaluation of whether an app meets their needs. While for the general population, applications with poor usability will often fail, physicians are said to place a much higher emphasis on perceived usefulness than on usability aspects.30 In fact, as seen in the literature,51,52 many IT applications (with mHealth being no exception) available for the medical sector are quite complicated. However, for solutions such as apps and mobile devices that are currently perceived as add-ons that exceed current (administrative, legal and economic) requirements and still need to establish themselves in current busy medical practices, ease of use, along with trustworthiness and other aspects may well be decisive. Manufacturers of devices and apps, along with those providing health-related content, need to adapt their products better to their target groups’ specific needs and this includes well prepared, reliable and attractive content that is easily accessible and can also be well integrated into the processes of a busy medical practice.53 Another factor contributing to an often rather conservative-appearing attitude may be that for apps, especially those with diagnostic or therapeutic functionalities, there are often open legal and regulatory questions and, as mentioned above, reimbursement, which may prevent actual use within care.13 Solving these issues will require a joint effort by a number of stakeholders, encompassing policy makers, manufacturers and distributors as well as those using the apps.
Meet the needs
While, as mentioned above, most of the patients in our survey were in agreement with their doctor using a mobile device for explaining health-related issues to them, none of the participating doctors had actually done so. This may not even be an issue related only to the technology, but may rather represent a key issue related to communication barriers in medical practices. Increasing interaction between doctors and patients, especially in educational matters, is often seen as an important part of patient empowerment. However, while GPs are aware of the obvious possibility to use multimedia functionalities – mobile or otherwise – for educational reasons, they are still not using them for these (communicative) purposes. As GPs only have a little time they can spend per patient, the time spent for communication is also limited.54 Communication is a time-consuming, but nevertheless important, factor for care processes in which patients can play a more active role,55 and may therefore be an aspect that needs to be handled with better efficiency, for which mobile technologies and apps can play an important role. Only when this is recognised by all concerned will additional material or technology be successfully used for explanatory or other reasons. As mentioned before, this will necessitate a joint effort in analysing the needs, providing adequate solutions, and educating potential users about how they can take advantage of the technologies to their benefit.
Do apps affect the relationship between patients and doctors?
It remains unclear whether health-related apps already have an influence on the relationship between doctors and patients. ‘Dr Google’ has previously been shown to have an impact on the information- seeking behaviour of consumers of health-related information56 as well as on patients’ communication behaviour when dealing with medical professionals.57,58 However, from our results, we were unable to confirm a similar impact for health-related apps. In general, information is lacking as to whether the use of health-related mobile devices and apps can improve the relationship between GPs and their patients, e.g. by offering physicians the opportunity to focus better on the patients (who may have used the technology to record certain relevant data before their visits) instead of on data acquisition. Various studies demonstrate that most patients, if they were asked, would like to play a more active role in healthcare decisions,59 and, as previously shown, patient centredness often improves patients’ knowledge about the conditions they suffer from and leads to more realistic expectations about the course of their diseases.60 Still, while mobile devices cannot replace the doctor–patient dialogue and the long-term relationship that GPs have with their patients, they may contribute to a more active patient participation in the treatment process, e.g. if both groups use the same health-related apps or if those apps become part of the consultation in order to prioritise health problems and ameliorate care planning.
Limitations
Several limitations need to be considered for our study. First, the recruitment strategies for both groups differed.
While email invitations were the sole method of recruitment for the GPs and the survey was performed electronically, without any personal contact with the study personnel, for the patients, a paper-based questionnaire was used. The patients were approached in the waiting room of their respective doctor’s office, thus giving them less opportunity to evade participation, contributing to an acceptable response rate despite no incentive being offered for participation. In comparison, for the physicians, the lack of direct contact seems to have been a decisive factor: Similar to the patients, there were no incentives, but neither was there any direct contact between doctors and the study personnel. Altogether, the response rate for the physicians who had been invited to participate was thus much lower than that obtained for the patient population; however, due to limited time and resources, administering the interviews in a manner similar to the patient population (e.g. by personal visits to the doctors’ offices), extending the survey period, offering incentives, or repeating the survey were out of the question.
Unfortunately, differences caused by the somewhat inconsistent recruitment strategies contributed to a potential selection bias in the data obtained for the physicians, as probably only those with an interest in the subject at hand (and sufficient time to spare) answered our survey. For future studies, changes in the recruitment strategy seem advisable; for example, by offering incentives or using additional follow-up reminders regarding participation. With respect to sociodemographics, the subdivisions used for age (patients and physicians) and work experience (physicians) may have been overly broad, e.g. with age cohorts being divided into intervals of 10 years or more. Unfortunately, while designing the questionnaires, it was decided to employ the default items for sociodemographic factors offered by the EvaSys software (Electric Paper Evaluationssysteme GmbH), but these are unfortunately not well adapted to capturing possible transformations taking place with respect to digital literacy at certain age levels. Also, digital literacy itself was not evaluated as a separate factor: as for example shown by Neter and Brainin,41 factors such as age and education closely correlate to eHealth literacy, which, when designing our questionnaires, was part of the reasoning behind choosing not to include items specifically targeting digital or eHealth/mHealth literacy.
Conclusions
Apparently GPs and patients already apply mobile technologies in health-related contexts. Whereas self-centred health-oriented processes prevail, our results show limited interaction between both sides. Neither a negative nor a positive impact on the patient–physician relationship was detectable, although this remains a possibility. While there are efforts under way to determine the impact apps can have, at least for specific health-related applications,61 the general situation in this regard is still unclear, requiring further research.
Also, special care needs to be taken to ensure that the rising use of mobile technologies does not further exacerbate existing healthcare disparities, which other studies also emphasise for mHealth-related solutions and for health information technologies in general.62 Moreover, the potentials that are offered by this exciting technology have not yet been fully exploited.13 Most existing solutions simply aim at supporting or reproducing established conservative processes. For fully leveraging the possibilities mobile technologies offer, several steps need to be taken. Patients need to form a clear picture of their own needs and they also have to find the courage to demand changes to existing processes with respect to interacting with their doctors. As even for those patients not (yet) using mobile devices, a non-negligible number can envision various health-related use scenarios (although at a lower rate than those already making use of mobile technologies), there is a need for policy makers, manufacturers as well as care providers and other stakeholders to heighten their efforts to determine factors contributing to this and to ensure that all (potential) users are given the opportunity to use mobile technologies.
On the other hand, GPs should venture towards a more daring train of thought about implementing new processes as well, of course while staying within the bounds of existing rules and regulations; however, they should try to leverage the potentials mobile technologies have for them as well as their patients. Much of this relates to adapting organisational processes. Once these are straightened out, technical aspects will probably be the less significant one of the two challenges, if all stakeholders collaborate.
Acknowledgements
The authors would like to thank the participating patients and physicians for their help. Special thanks go to Dr Stephan Bortfeldt of the Deutscher Hausärzteverband – Landesverband Niedersachsen e.V. and Professor Nils Schneider, director of the Institute for Family Medicine, Hannover Medical School for support with convincing the general practices to participate. Thanks also go to Ms Annika Meusel and Mr Markus Hupka representing for the group of students of the University of Applied Sciences of Hannover, who conducted the patient surveys at the general practices. The authors also thank Mr Harald Bietenduewel for technical support.
Appendix 1: Patients’ questionnaire
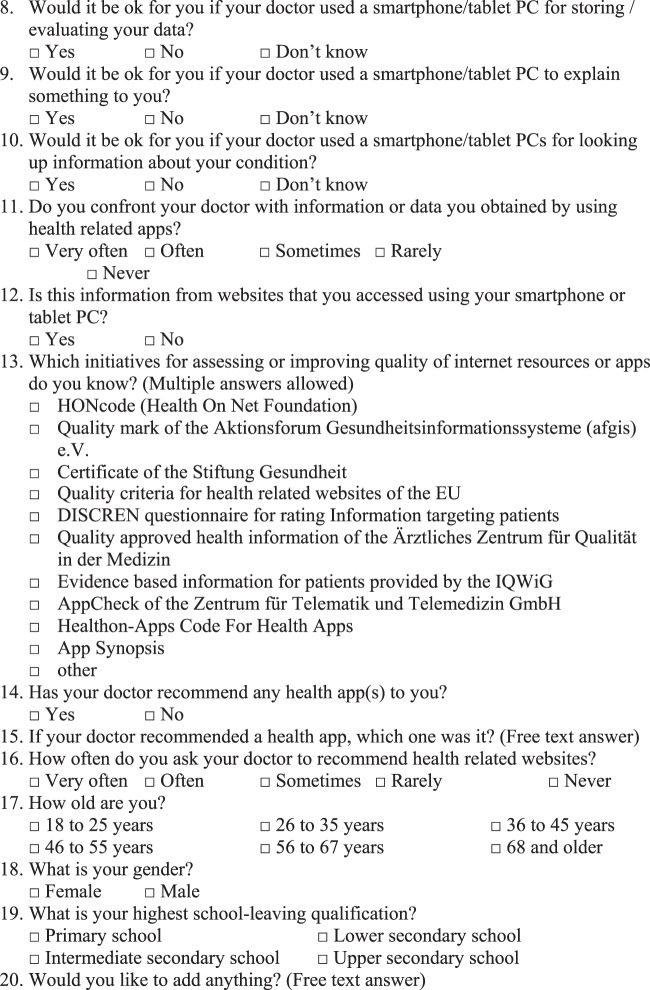
Appendix 2: Doctors’ questionnaire
Contributorship
All authors contributed equally.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
The institutional review board of Hannover Medical School approved this study (trial number 1206-2011, amended on 03/19/2014).
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor
UVA
Peer review
This manuscript was peer-reviewed by Jack A Hyman, George Washington University, Joanna Milward, King s College London and one other who have chosen to remain anonymous..
References
- 1.Initiative D21. Mobile Internetnutzung 2014 – Gradmesser für die digitale Gesellschaft. http://www.initiatived21.de/wp-content/uploads/2014/12/Mobile-Internetnutzung-2014_WEB.pdf (2014, accessed 13 July 2016).
- 2.eMarketer Inc. www.emarketer.com. http://www.emarketer.com/Article/Smartphones-Tablets-Drive-Internet-Use-Germany/1013757 (2016, accessed 17 October 2016).
- 3.Garabedian LF, Ross-Degnan D, Wharam JF. Mobile phone and smartphone technologies for diabetes care and self-management. Curr Diab Rep 2015; 15: 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson K, Burford O, Emmerton L. Mobile health apps to facilitate self-care: a qualitative study of user experiences. PLoS One 2016; 11: e0156164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pliakos I, Kefaliakos A, Kalokerinou A, et al. m-Health: integration of mobile phones and applications for a better healthcare system. Stud Health Technol Inform 2014; 202: 315. [PubMed] [Google Scholar]
- 6.Dubey D, Amritphale A, Sawhney A, et al. Smart phone applications as a source of information on stroke. J Stroke 2014; 16: 86–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HS, Choi W, Baek EK, et al. Efficacy of the smartphone-based glucose management application stratified by user satisfaction. Diabetes Metab J 2014; 38: 204–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fritz F, Balhorn S, Riek M, et al. Qualitative and quantitative evaluation of EHR-integrated mobile patient questionnaires regarding usability and cost-efficiency. Int J Med Inform 2012; 81: 303–313. [DOI] [PubMed] [Google Scholar]
- 9.Leventhal R. How a N.J. medical center saved millions with mHealth technology. Healthcare Inform 2014; 31: 30, 32, 35. [PubMed] [Google Scholar]
- 10.Holden RJ, Karsh BT. The technology acceptance model: its past and its future in health care. J Biomed Inform 2010; 43: 159–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang MWB, Ward J, Ying JJB, et al. The alcohol tracker application: an initial evaluation of user preferences. BMJ Innov 2016; 2: 8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bierbrier R, Lo V, Wu RC. Evaluation of the accuracy of smartphone medical calculation apps. J Med Internet Res 2014; 16: e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Albrecht UV, Ed. Chances and Risks of Mobile Health Apps (CHARISMHA). Abridged version. Hannover: Medizinische Hochschule Hannover; 2016. http://publikationsserver.tu-braunschweig.de/receive/dbbs_mods_00060023 (2016, accessed 1 February 2017).
- 14.Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA 1992; 267: 2221–2226. [PubMed] [Google Scholar]
- 15.Siegler M. The progression of medicine. From physician paternalism to patient autonomy to bureaucratic parsimony. Arch Intern Med 1985; 145: 713–715. [DOI] [PubMed] [Google Scholar]
- 16.Lupton D, Jutel A. ‘It's like having a physician in your pocket!’ A critical analysis of self-diagnosis smartphone apps. Soc Sci Med 2015; 133: 128–135. [DOI] [PubMed] [Google Scholar]
- 17.Illiger K, Hupka M, von Jan U, et al. Mobile technologies: expectancy, usage, and acceptance of clinical staff and patients at a university medical center. JMIR Mhealth Uhealth 2014; 2: e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berg M. Implementing information systems in health care organizations: myths and challenges. Int J Med Inform 2001; 64: 143–156. [DOI] [PubMed] [Google Scholar]
- 19.Shareef MA, Kumar V, Kumar U. Predicting mobile health adoption behaviour: a demand side perspective. J Custom Behav 2014; 13: 187–205. [Google Scholar]
- 20.Hyman JA. Towards an understanding of mobile website contextual usability and its impact on mobile commerce. Dissertation. Fort Lauderdale, FL, USA: Nova Southeastern University, 2012.
- 21.Wang YS, Liao YW. The conceptualization and measurement of m-commerce user satisfaction. Comput Human Behav 2007; 23: 381–398. [Google Scholar]
- 22.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly 1989; 13: 319–340. [Google Scholar]
- 23.Davis FD. User acceptance of information technology: system characteristics, user perceptions and behavioral impacts. Int J Man-Machine Stud 1993; 38: 475–487. [Google Scholar]
- 24.Bagozzi RP, Davis FD, Warshaw PR. Development and test of a theory of technological learning and usage. Human Relations 1992; 45: 659–686. [Google Scholar]
- 25.Venkatesh V, Morris MG, Davis GB, et al. User acceptance of information technology: toward a unified view. MIS Quarterly 2003; 27: 425–478. [Google Scholar]
- 26.Fishbein M and Ajzen I. Belief, attitude, intention and behavior: an introduction to theory and research. Reading, MA, USA: Addison-Wesley, 1975.
- 27.Ajzen I and Fishbein M. Understanding attitudes and predicting social behaviour. NJ, USA: Pearson, 1980.
- 28.Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Management Sci 2000; 46: 186–204. [Google Scholar]
- 29.Ajzen I, Madden TJ. Prediction of goal-directed behavior: attitudes, intentions, and perceived behavioral control. J Exp Soc Psychol 1986; 22: 453–474. [Google Scholar]
- 30.Chismar WG and Wiley-Patton S. Does the extended technology acceptance model apply to physicians. Proceedings of the 36th Annual Hawaii International Conference on System Sciences, 2003.
- 31.Fortunati L, Taipale S. The advanced use of mobile phones in five European countries. Br J Sociol 2014; 65: 317–337. [DOI] [PubMed] [Google Scholar]
- 32.Behrends M, von Jan U, Illiger K, et al. Gesundheitsapps und Gesundheitsinformationen im Internet für Laien - auch ein Thema für Ärzte? GMDS 2015: 60. Jahrestagung der Deutschen Gesellschaft für Medizinische Informatik, Biometrie und Epidemiologie e.V. (GMDS). Düsseldorf: German Medical Science GMS Publishing House, 2015, p. DocAbstr. 029. doi: 10.3205/15gmds017.
- 33.German Medical Association. Official Statistics of the German Medical Association Regarding Physicians for 2014, Berlin, 2014, www.bundesaerztekammer.de/ueber-uns/aerztestatistik/aerztestatistik-2014 (accessed 13 February 2017).
- 34.Albrecht UV, von Jan U, Sedlacek L, et al. Standardized, app-based disinfection of iPads in a clinical and nonclinical setting: comparative analysis. J Med Internet Res 2013; 15: e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kontos E, Blake KD, Chou WYS, et al. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res 2014; 16: e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tennant B, Stellefson M, Dodd V, et al. eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers and older adults. J Med Internet Res 2015; 17: e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Travis B. Android vs. iOS: User Differences Every Developer Should Know. Reston, Virginia, USA: comScore, 2013, www.comscore.com/Insights/Blog/Android-vs-iOS-User-Differences-Every-Developer-Should-Know (accessed 13 February 2017).
- 38.Haught HM, Rose JP, Brown JA. Social-class indicators differentially predict engagement in prevention vs. detection behaviours. Psychol Health 2016; 31: 21–39. [DOI] [PubMed] [Google Scholar]
- 39.Bender MS, Choi J, Arai S, et al. Digital technology ownership, usage, and factors predicting downloading health apps among Caucasian, Filipino, Korean, and Latino Americans: the digital link to health survey. JMIR Mhealth Uhealth 2014; 2: e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. JAMA 2011; 18: 318–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neter E, Brainin E. eHealth literacy: extending the digital divide to the realm of health information. J Med Internet Res 2012; 14: e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Becker S, Kribben A, Meister S, et al. User profiles of a smartphone application to support drug adherence – experiences from the iNephro project. PloS one 2013; 8: e78547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Karhu K, Tang T, Hämäläinen M. Analyzing competitive and collaborative differences among mobile ecosystems using abstracted strategy networks. Telemat Informat 2014; 31: 319–333. [Google Scholar]
- 44.Osterloh F. Ärztemonitor – Ärzten macht ihre Arbeit Spass. Deutsches Ärtzeblatt 2012; 109: A1212–A1213. [Google Scholar]
- 45.Weicksel J and Pentsi A. 4 Millionen Deutsche nutzen ein Smartphone. Berlin: Bitkom, 2015, www.bitkom.org/Presse/Presseinformation/44-Millionen-Deutsche-nutzen-ein-Smartphone.html.
- 46.Chung CF, Cook J, Bales E, et al. More than telemonitoring: health provider use and nonuse of life-log data in irritable bowel syndrome and weight management. J Med Internet Res 2015; 17: e203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Freude A, Freude T. Echos of History: Understanding German Data Protection, Washington, DC: Bertelsmann Foundation, 2016. [Google Scholar]
- 48.Akkaya C, Obermeier M, Wolf P, et al. Components of trust influencing egovernment adoption in Germany. In: Janssen M, Scholl HJ, Wimmer MA, et al. Electronic Government. Proceedings of the 10th IFIP WG 8.5 International Conference, EGOV 2011, Delft, The Netherlands. 28 August–2 September 2011. Berlin, Heidelberg: Springer, 2011, pp. 88–99.
- 49.Runtastic GmbH. Runtastic: Running, Cycling & Fitness GPS Tracker. https://www.runtastic.com/en/ (2016, accessed 30 October 2016).
- 50.Park Y, Chen JV. Acceptance and adoption of the innovative use of smartphone. Ind Manage Data Syst 2007; 107: 1349–1365. [Google Scholar]
- 51.Vincent CJ, Niezen G, O’Kane AA, et al. Can standards and regulations keep up with health technology? JMIR Mhealth and Uhealth 2015; 3: e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zapata BC, Fernández-Alemán JL, Idri A, et al. Empirical studies on usability of mHealth apps: a systematic literature review. J Med Syst 2015; 39: 1. [DOI] [PubMed] [Google Scholar]
- 53.Becker S, Miron-Shatz T, Schumacher N, et al. mHealth 2.0: experiences, possibilities, and perspectives. JMIR Mhealth Uhealth 2014; 2: e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Konrad TR, Link CL, Shackelton RJ, et al. It’s about time: physicians’ perceptions of time constraints in primary care medical practice in three national healthcare systems. Med Care 2010; 48: 95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Teutsch C. Patient–doctor communication. Med Clin North Am 2003; 87: 1115–1145. [DOI] [PubMed] [Google Scholar]
- 56.Lee K, Hoti K, Hughes JD, et al. Dr Google and the consumer: a qualitative study exploring the navigational needs and online health information-seeking behaviors of consumers with chronic health conditions. J Med Internet Res 2014; 16: e262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Silver MP. Patient perspectives on online health information and communication with doctors: a qualitative study of patients 50 years old and over. J Med Internet Res 2015; 17: e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ahmad F, Hudak PL, Bercovitz K, et al. Are physicians ready for patients with Internet-based health information? J Med Internet Res 2006; 8: e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Butzlaff M, Floer B and Isfort J. Gesundheitsmonitor 2003. In: Böcken J, Braun B, Schnee M, eds. Gütersloh, Gütersloh: Verlag Bertelsmann Stiftung, 2003, pp. 41–55.
- 60.Simon D, Loh A, Härter M. Development and evaluation of interventions to support shared decision making – framework and measuring instruments. Z Med Psychol 2008; 17: 149–159. [Google Scholar]
- 61.Choo S, Kim JY, Jung SY, et al. Development of a weight loss mobile app linked with an accelerometer for use in the clinic: usability, acceptability, and early testing of its impact on the patient–doctor relationship. JMIR Mhealth Uhealth 2016; 4: e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lyles C, Schillinger D, Sarkar U. Connecting the dots: health information technology expansion and health disparities. PLoS Med 2015; 12: e1001852. [DOI] [PMC free article] [PubMed] [Google Scholar]