Abstract
A 50-year-old female presented to us with features of obstructive jaundice. Investigations revealed cholelithiasis with single large impacted calculus in the common bile duct (CBD) and significant dilatation of extrahepatic biliary tree. Incidentally, the patient was also detected to have situs inversus totalis (SIT). Attempt at extraction of the calculus in the CBD by endoscopic retrograde cholangiography failed, and a 7F stent was placed. The patient was subjected to laparoscopic cholecystectomy, CBD exploration with the extraction of the offending calculus and laparoscopic choledochoduodenostomy (LCDD). The patient had an uneventful recovery and is since discharged. PubMed search did not reveal LCDD in SIT as a procedure reported in literature to the best of our knowledge.
Keywords: Cholecystectomy, choledochoduodenostomy, common bile duct exploration, laparoscopy, situs inversus
INTRODUCTION
Situs inversus totalis (SIT) is a condition where the organs in the body are mirror image of the normal anatomy. Mayo and Rice report the incidence to be 1:10,000–1:20,000 population.[1] Due to the mirror image anatomy, surgery becomes challenging as the normal orientation of a surgeon is completely changed. Laparoscopic surgery with its inherent difficulties becomes even more challenging as the nondominant hand becomes the active hand. With increasing adaptation of laparoscopic anatomy in SIT, biliary procedures such as cholecystectomy[2,3,4] and even common bile duct (CBD) exploration[5,6,7] have been described. We had a case of calculus cholecystitis with CBD calculus (and a dilated CBD) requiring a bypass procedure. Laparoscopic cholecystectomy with choledochoduodenostomy (CDD) was performed. Review of literature on PubMed failed to reveal any such report.
CASE REPORT
A 50-year-old female presented to us with obstructive jaundice. The investigation revealed SIT with a heart on the right side. Abdominal sonography followed by magnetic resonance cholangiopancreatography revealed evidence of gallstones and a large CBD calculus (1.8 cm) leading to dilatation of CBD >2 cm [Figure 1]. Endoscopic retrograde cholangiography (ERC) failed to extract the calculus. The CBD was stented with 7 F stent. After stabilisation of liver function, the patient was subjected to laparoscopic approach.
Figure 1.
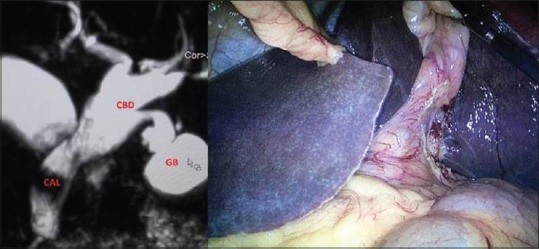
MRI showing large impacted calculus in CBD (left) and image of GB in situs inversus. GB: Gall bladder; CBD: Common bile duct; CAL: Calculus; MRI: Magnetic resonance imaging
The monitor was placed on the left side of the patient and ports were mirror image of standard laparoscopic cholecystectomy. Subumbilical 10 mm telescope port, three working ports (all 5 mm) were placed around xiphisternum, left midclavicular and anterior axillary line, respectively. SIT was confirmed [Figure 1]. The gallbladder was distended with a wide cystic duct. The CBD was dilated approximately 2 cm with stone easily felt in the supraduodenal region by instrument palpation. Slow careful dissection and continuous ergonomic adjustments led us to successful laparoscopic cholecystectomy, clearance of the CBD and completion of CDD [Figure 2]. Specimen of gallbladder, CBD stone and stent were bagged and retrieved through the umbilical port. The patient had an uneventful recovery and was discharged.
Figure 2.
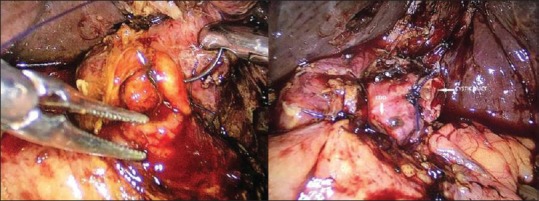
Choledochoduodenostomy
DISCUSSION
SIT is a condition where the organs in the abdomen are mirror image of the normal anatomy, and the heart is on the right instead of left side. Mayo and Rice report the incidence to be 1:10,000–1:20,000 population.[1] Due to the mirror image anatomy, surgery becomes challenging as the normal orientation of a surgeon is completely changed. Laparoscopic surgery is even more challenging as there is a complete change in setup, orientation and ergonomics. Further, the entire team including the camera assistant and assistant should be ready with this change for successful completion of laparoscopic procedure.
Laparoscopic cholecystectomy has now become the standard of care over the world. SIT, laparoscopic cholecystectomy was described by Campos and Sipes[8] in 1991. Since then, there has been a steady inflow of reports in literature.[2,3,4] Most reports deliberate on adjustments and solutions to problems caused by SIT – mirror image anatomy, setup changes, surgeon and port positioning to overcome ergonomic changes.[9] Even a single port approach has been described indicating control of laparoscopic surgeons over cholecystectomy SIT.[10]
ERC, extraction of stone/s followed by laparoscopic cholecystectomy is the procedure followed in this part of the world. Some surgeons, however, would advocate one-time laparoscopic CBD exploration and clearance.[11] Primary closure of the CBD,[12] closure of CBD over a stent[13] or over T-tube[14] and bypass procedures[15] are the described variants after CBD clearance depending on the pre- and intra-operative findings. In our case, the CBD was dilated (2 cm) and hence decision to perform a bypass procedure was taken. Laparoscopic CDD requires advanced skills in suturing and becomes even more demanding in SIT.
Search of PubMed reveals only 3 case reports of laparoscopic CBD exploration in a patient with SIT.[5,6,7] None of these mention a bypass procedure being performed. In our case, the CBD was dilated (2 cm), and hence, bypass procedure was deemed procedure of choice. Laparoscopic bilioenteric anastomosis in a patient with SIT requires a focused team effort, ambidexterity in suturing countering increased difficulty in ergonomics created for success. We believe that this is first such case in review of available literature.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the Dean, Seth G S Medical College and KEM Hospital for allowing us to publish hospital data.
REFERENCES
- 1.Mayo CW, Rice RG. Situs inversus totalis; a statistical review of data on 76 cases with special reference to disease of the biliary tract. Arch Surg. 1949;58:724–30. [PubMed] [Google Scholar]
- 2.Yaghan RJ, Gharaibeh KI, Hammori S. Feasibility of laparoscopic cholecystectomy in situs inversus. J Laparoendosc Adv Surg Tech A. 2001;11:233–7. doi: 10.1089/109264201750539763. [DOI] [PubMed] [Google Scholar]
- 3.Takei HT, Maxwell JG, Clancy TV, Tinsley EA. Laparoscopic cholecystectomy in situs inversus totalis. J Laparoendosc Surg. 1992;2:171–6. doi: 10.1089/lps.1992.2.171. [DOI] [PubMed] [Google Scholar]
- 4.Crosher RF, Harnarayan P, Bremner DN. Laparoscopic cholecystectomy in situs inversus totalis. J R Coll Surg Edinb. 1996;41:183–4. [PubMed] [Google Scholar]
- 5.Wong J, Tang CN, Chau CH, Luk YW, Li MK. Laparoscopic cholecystectomy and exploration of common bile duct in a patient with situs inversus. Surg Endosc. 2001;15:218. doi: 10.1007/s004640040037. [DOI] [PubMed] [Google Scholar]
- 6.Kang SB, Han HS. Laparoscopic exploration of the common bile duct in a patient with situs inversus totalis. J Laparoendosc Adv Surg Tech A. 2004;14:103–6. doi: 10.1089/109264204322973880. [DOI] [PubMed] [Google Scholar]
- 7.Weber-Sánchez A, Bravo-Torreblanca C, Garteiz-Martínez D, Carbó-Romano R, Vega-Rivera F, Hernández R, et al. Case report: Laparoscopic cholecystectomy and common bile duct exploration in a 60 year-old patient with situs inversus. Rev Gastroenterol Mex. 2011;76:255–9. [PubMed] [Google Scholar]
- 8.Campos L, Sipes E. Laparoscopic cholecystectomy in a 39-year-old female with situs inversus. J Laparoendosc Surg. 1991;1:123–5. doi: 10.1089/lps.1991.1.123. [DOI] [PubMed] [Google Scholar]
- 9.Aydin U, Unalp O, Yazici P, Gurcu B, Sozbilen M, Coker A. Laparoscopic cholecystectomy in a aptient with situs inversus totalis. World J Gastroentrol. 2006;12:7717–9. doi: 10.3748/wjg.v12.i47.7717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khiangte E, Newme I, Patowary K, Phukan P. Single-port laparoscopic cholecystectomy in situs inversus totalis using the E.K. Glove port. J Minim Access Surg. 2013;9:180–2. doi: 10.4103/0972-9941.118838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kadam R, Saxena D, Rana AS, Chhabra S, Ahmed Z, Vij V, et al. Laparoscopic common bile duct exploration versus ERCP/stenting and cholecystectomy: Is a single staged procedure better? Int J Hepatobiliary Pancreat Dis. 2016;6:57–63. [Google Scholar]
- 12.Dong ZT, Wu GZ, Luo KL, Li JM. Primary closure after laparoscopic common bile duct exploration versus T-tube. J Surg Res. 2014;189:249–54. doi: 10.1016/j.jss.2014.03.055. [DOI] [PubMed] [Google Scholar]
- 13.Dietrich A, Alvarez F, Resio N, Mazza O, de Santibañes E, Pekolj J, et al. Laparoscopic management of common bile duct stones: Transpapillary stenting or external biliary drainage? JSLS. 2014;18:pii: e201400277. doi: 10.4293/JSLS.2014.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lien HH, Huang CC, Huang CS, Shi MY, Chen DF, Wang NY, et al. Laparoscopic common bile duct exploration with T-tube choledochotomy for the management of choledocholithiasis. J Laparoendosc Adv Surg Tech A. 2005;15:298–302. doi: 10.1089/lap.2005.15.298. [DOI] [PubMed] [Google Scholar]
- 15.Priego P, Escrig J, Ángel V, Villegas C, Salvador JL. Laparoscopic choledochoduodenostomy: An option in cases of obstructive biliary tract. Am Surg. 2015;81:E195–7. [PubMed] [Google Scholar]


