Abstract
Background: Obesity prevalence among low-income preschool-aged children in the United States decreased between 2010 and 2014. However, this decreasing trend may be varied across socioeconomic subgroups. This study examined trends in obesity prevalence among low-income children from 2003 to 2014 by child's age and household and neighborhood socioeconomic status (SES).
Methods: This study used administrative data for all children, aged 2–4 years, participating in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in Los Angeles County (LAC) during the years 2003–2014. Obesity was defined as having a BMI ≥95th percentile of CDC's age- and sex-specific growth charts. Household income and household educational attainment were indicators of household SES. Neighborhood median household income was an indicator of neighborhood SES.
Results: Childhood obesity prevalence increased sharply from 15.7% in 2003 to 19.1% in 2005, and remained constant until 2010, when it started decreasing. During most years, the prevalence of obesity was higher among the lowest SES groups. Despite the recent decreasing trend, the 2014 estimates were still generally higher than the 2003 levels except among some low-income children living in less-poor and more-educated households.
Conclusions: The decreasing trend between 2010 and 2014 among WIC-participating children in LAC is encouraging and mirrors national trends among WIC-participating children. However, continued efforts should be made to focus obesity prevention efforts on low-income children, especially those who are the most vulnerable as they have experienced significant gains in obesity since 2003.
Keywords: : childhood obesity, socioeconomic disparities, socioeconomic status, trends, WIC
Introduction
In the United States, childhood obesity prevalence among 2–19-year-olds has more than tripled since the 1970s, reaching over 18% in 2015–2016.1–3 Despite this increasing trend,1,2 a 2014 report in JAMA noted that obesity prevalence among United States preschool-aged children had started to reverse, reaching a low of 8.4% in 2011–2012.4 This decreasing trend was also observed among low-income children5,6 who are at greater risk for obesity.7 Specifically, obesity prevalence among preschool-aged participants of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), a federal nutrition assistance program, decreased from a peak of 15.9% in 2010 to 14.5% in 2014.6 WIC serves over 9 million low-income [≤185% federal poverty level (FPL)] pregnant and breastfeeding women and children up to age five who are at nutritional risk.8 It is unclear if this decreasing trend can be maintained or if it has been experienced across all socioeconomic subgroups in the WIC population. Recent estimates show that obesity prevalence among 2–5-year-olds increased by more than half between 2011–2012 and 2015–2016 in the general United States population.1,2
Because only low-income children are eligible to participate in WIC, obesity prevalence trends among WIC-participating children have mostly been examined by race/ethnicity,5,9 but not by socioeconomic status (SES). However, socioeconomic disparities in obesity exist even among WIC-participating children.10 Emerging efforts have begun to examine obesity trends among these children by household- and neighborhood-level socioeconomic indicators10,11 since this information can be helpful for improving program delivery to the most vulnerable families.
In the United States and other developed countries, an inverse relationship between SES and childhood obesity risk has been observed.7,12 Using 2011–2014 National Health and Nutrition Examination Survey (NHANES) data, Ogden et al. found that obesity prevalence increased as head of household education decreased: 10% of children aged 2–19 years living in college-educated households were obese compared to 18% and 22%, respectively, of children living in households where the head of household had some college education and where the head of household had a high school degree or less.7 However, the relationship between SES and obesity risk is contextual, varying over time and across race/ethnicity, age, and gender.7,12 For example, Wang and Zhang examined the association between household income and childhood obesity between the 1970s and early 2000s and found that the inverse association weakened over time as obesity became more prevalent among higher income children.12 In comparison between the early 2000s and 2011–2014, obesity became more prevalent among lower income girls than higher income girls, strengthening the inverse association between SES and obesity risk among girls but not among boys.7
By determining access to resources and quality of life, a child's SES—generally operationalized as household income, parent's educational attainment and/or neighborhood median household income—can influence risk of obesity by shaping diet and physical activity behaviors. For instance, as young children spend a considerable amount of time in early childhood education settings, their diet and physical activity behaviors are, in part, influenced by the type and quality of the setting that their parents can afford.13,14 Among WIC-participating families, living in low socioeconomic neighborhoods may prevent families from reaping the full benefits of WIC participation (i.e., nutrition education and supplemental foods) due to the inaccessibility of healthy foods and increased exposure to unhealthy foods in such neighborhoods, and fewer safe recreational areas where children can play.15 Furthermore, the changes and events that occurred in the past decade, such as the 2009 WIC food package change (72 Federal Register 68966) which aligned the composition of the packages with the Dietary Guidelines for Americans and increased the cash value voucher amount for produce,16 and the 2008–2009 economic recession which disproportionately affected low-income families,17 might differentially impact WIC-participating families of varying socioeconomic resources.
Understanding the impact of socioeconomic factors on obesity among low-income children during significant economic, policy and environmental changes is critical for designing effective population-level interventions for the most vulnerable. This study aims to (1) examine secular trends in obesity among preschool-aged WIC-participating children in Los Angeles County (LAC) from 2003 to 2014 and (2) determine whether these trends vary by household and neighborhood SES.
Methods
Data Source
We used administrative data containing sociodemographic and anthropometric information on children aged 2–4 years participating in WIC in LAC during the years 2003–2014. The data are owned by the State of California and maintained by the WIC Data Mining Project, a research partnership between First 5 LA and Public Health Foundation Enterprises-WIC (www.phfewic.org), the largest local WIC agency in the country. Half of all preschool-aged children in LAC participate in WIC.18
Children's heights and weights are measured every 6 months during clinic visits by trained WIC staff who use a standardized protocol.19 Wall-mounted stadiometers (Model PE-WM-60-76; Prospective Enterprises, Portage, MI) and calibrated beam scales (Health-O-Meter 402LB; Prospective Enterprises) are used for heights and weights, respectively. Shoes and outerwear are removed before taking measurements. The same staff member does not necessarily take the child's measurements every time; however, staff are trained regularly. Children's measurements that are taken by a healthcare provider within 60 days of his/her WIC visit can be used instead19; 20% of measurements are obtained this way. Measurements obtained in LAC on children aged 2–4 years have been assessed to have high validity.19
WIC participants' addresses are geocoded at the census tract level. Neighborhood socioeconomic information obtained from the Census Bureau's American Community Survey (ACS) was linked to the census tracts. Five-year estimates (the only ACS estimates available at this geographic level) from 2005 to 2009 were linked to WIC measurements taken during the years 2003–2009 and those of 2010–2014 to WIC measurements taken during the years 2010–2014.
Since very young children grow rapidly and are developmentally different at every age,20 we examined the trends in obesity separately within age strata (2, 3, and 4 years). Given the potential for misclassification, children whose caregivers (primarily the mother) were not Hispanic, non-Hispanic (NH) white, NH black, or NH Asian were excluded from the analyses. Children with missing data on any variable were also excluded. To ensure independence of observations, we used the first measurement if a child was measured more than once in a calendar year, and if twins or triplets participated in WIC, only one of the children was included in our sample. The final sample size was 2,017,058 measurements from 739,893 two-year-olds, 708,349 three-year-olds, and 568,816 four-year-olds. The fewer 4-year-olds reflect their decreased participation in WIC.8 The same child could be included in each of these samples. Consent was not required for this study since administrative data were used. The University of California, Los Angeles (UCLA) Institutional Review Board approved this study.
Variables
The outcome variable was child's obesity status, defined as having a BMI ≥95th percentile of CDC's gender- and age-specific growth reference values.21 The independent variables were household- and neighborhood-level socioeconomic indicators, each representing a different facet of a child's SES. Household income, an indicator of a child's standard of living,22 includes income from all sources, of which proof is required, and is assessed at each WIC certification or recertification appointment. It was operationalized as a percentage of the FPL and categorized into ≤50.0% FPL, 50.1%–100.0% FPL, 100.1%–133.0% FPL, and 133.1%–185.0% FPL. Household education, an indicator of parents' occupation, knowledge, and skills and a relatively stable indicator of SES,22 was the highest grade completed by the child's caregiver during enrollment in WIC and was categorized as less than high school, high school, some college, and college or more. Median household income of residents living in the child's census tract, an indicator of community and environmental resources, was categorized according to quartiles of its distribution among WIC participants (≤$32,738; $32,739–40,278; $40,279–51,534; ≥$51,535).
Statistical Analysis
The crude yearly prevalence of obesity for each age and SES or racial/ethnic group was calculated by dividing the number of obese children by its corresponding sample size. Log-linear regression with permutation was used to obtain the optimal regression model and the inflection years for the trends. Tests of parallelism determined whether two secular trends were parallel, that is, had the same slopes. If so, tests of coincidence determined whether they had identical log-linear regression models. To describe how trends in obesity varied by SES and age, the average annual percent changes (AAPCs) between the overall inflection years (2005 and 2010) as well as over the entire 12-year time period were examined. All of the AAPCs and the results of the tests of parallelism and coincidence are in Supplementary Tables S1–S4 (Supplementary Data are available online at www.liebertpub.com/chi). Since the majority of our sample is Hispanic, we conducted a sensitivity analysis that stratified the age- and SES-specific trends in obesity prevalence by race/ethnicity. Descriptive analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC). Log-linear regression was conducted using Joinpoint version 4.5.0.1 (National Cancer Institute, https://surveillance.cancer.gov/joinpoint/).
Results
The majority of children had caregivers who were Hispanic (Table 1). Despite all children being from low-income households, variability in income existed with a quarter of children from households with income ≤50% FPL, and nearly 30% from households with income ≥100% FPL (Table 1). More than half of the caregivers did not graduate from high school, while about 12% had at least some college education. Household income and median household income were weakly correlated with each other, with 29.0% of those in extreme poverty living in the poorest neighborhoods (≤$32,738) compared with 22.6% living in the higher income neighborhoods (≥$51,535). Changes in the population's sociodemographic characteristics occurred during the study's 12 years, with greater percentages of children living in extremely poor households, in higher educated households, and in higher-income neighborhoods in 2014 than in 2003 (Table 1).
Table 1.
Sociodemographic Characteristics of WIC-Participating Children by Age: Los Angeles County, 2003–2014
| 2-Year-olds | 3-Year-olds | 4-Year-olds | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall % 2003–2014, N = 739,893 | % in 2003, N = 68,259 | % in 2014, N = 56,694 | Overall % 2003–2014, N = 708,349 | % in 2003, N = 65,741 | % in 2014, N = 56,991 | Overall % 2003–2014, N = 568,816 | % in 2003, N = 50,412 | % in 2014, N = 44,815 | ||
| Gender (female) | 49.0 | 49.2 | 49.1 | 48.9 | 48.7 | 48.8 | 48.9 | 48.9 | 49.2 | |
| Parent race/ethnicity | ||||||||||
| NH white | 3.7 | 4.9 | 3.6*** | 3.6 | 4.6 | 3.5*** | 3.6 | 4.9 | 3.2*** | |
| NH black | 7.3 | 7.7 | 7.9 | 7.0 | 7.5 | 7.6 | 6.6 | 7.3 | 6.7 | |
| NH Asian | 4.0 | 4.3 | 4.5 | 3.8 | 4.3 | 3.8 | 3.8 | 4.0 | 3.6 | |
| Hispanic | 85.0 | 83.1 | 84.0 | 85.6 | 83.5 | 85.2 | 86.0 | 83.8 | 86.6 | |
| Household income | ||||||||||
| ≤50% FPL | 26.5 | 25.5 | 31.8*** | 26.1 | 25.6 | 31.2*** | 25.7 | 25.6 | 30.4*** | |
| 50.1%–100.0% FPL | 45.4 | 43.3 | 44.1 | 46.1 | 43.4 | 45.2 | 46.8 | 43.8 | 46.5 | |
| 100.1%–133.0% FPL | 16.1 | 17.4 | 14.2 | 16.0 | 17.4 | 14.2 | 15.9 | 17.2 | 13.9 | |
| 133.1%–185.0% FPL | 12.0 | 13.8 | 9.8 | 11.9 | 13.7 | 9.5 | 11.6 | 13.5 | 9.2 | |
| Household education | ||||||||||
| <High school | 54.8 | 60.6 | 46.1*** | 56.0 | 62.0 | 47.4*** | 57.4 | 62.5 | 49.6*** | |
| High school | 32.8 | 28.9 | 37.4 | 32.1 | 28.1 | 37.1 | 31.3 | 27.9 | 36.1 | |
| Some college | 9.3 | 8.2 | 11.6 | 8.9 | 7.8 | 11.1 | 8.5 | 7.6 | 10.2 | |
| College or more | 3.1 | 2.3 | 4.9 | 2.9 | 2.2 | 4.5 | 2.8 | 2.0 | 4.1 | |
| Median household income | ||||||||||
| ≤$32,738 | 25.0 | 24.9 | 24.9*** | 25.2 | 25.3 | 24.9*** | 25.2 | 25.0 | 25.7*** | |
| $32,739–40,278 | 24.9 | 26.6 | 23.1 | 25.0 | 26.3 | 23.6 | 25.1 | 26.6 | 23.5 | |
| $40,279–51,534 | 25.0 | 25.2 | 24.9 | 25.0 | 25.5 | 25.0 | 25.1 | 25.6 | 24.8 | |
| ≥$51,535 | 25.2 | 23.3 | 27.2 | 24.8 | 23.0 | 26.6 | 24.6 | 22.8 | 26.0 | |
Chi-square test of significant change between 2003 and 2014 at *p < 0.05; **p < 0.01; ***p < 0.001.
NH, non-Hispanic; FPL, federal poverty level; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
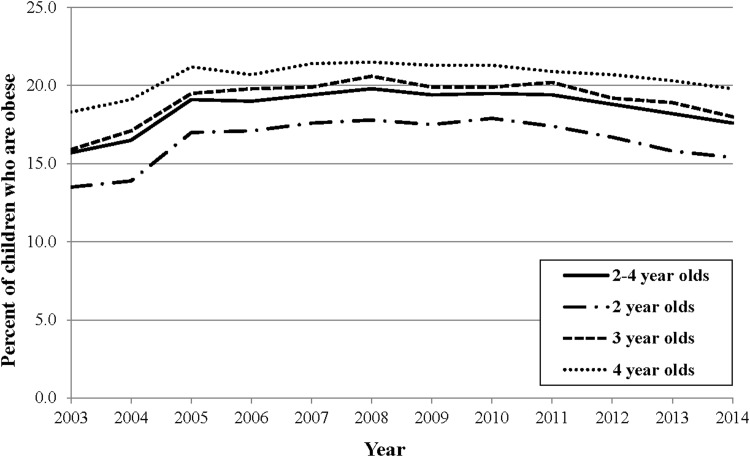
Secular Trends in Obesity
Overall, obesity prevalence increased sharply from 15.7% in 2003 to 19.1% in 2005, remained relatively constant until 2010, when it decreased to 17.6% in 2014 (Fig. 1). Trends in obesity by age group varied, and at every year, obesity prevalence was higher among the older children (Fig. 1; Table 2). A similar pattern existed across age groups, however, 2-year-olds experienced a sharper increase until 2005 and a steeper decline after 2010 than 4-year-olds (Supplementary Table S1).
Figure 1.
Trends in obesity prevalence among WIC-participating children by age: Los Angeles County, 2003–2014. WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Table 2.
Prevalence of Obesity among WIC-Participating Children by Age, Race/Ethnicity, and Socioeconomic Characteristics: Los Angeles County, 2003–2014
| 2-Year-olds | 3-Year-olds | 4-Year-olds | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Obesity prevalence (%) | AAPCa | Obesity prevalence (%) | AAPCa | Obesity prevalence (%) | AAPCa | ||||||||||
| 2003 | 2005 | 2010 | 2014 | 2003–2014 | 2003 | 2005 | 2010 | 2014 | 2003–2014 | 2003 | 2005 | 2010 | 2014 | 2003–2014 | |
| All | 13.5 | 17.0 | 17.9 | 15.4 | 1.5 (0.6 to 2.2) | 15.9 | 19.5 | 19.9 | 17.9 | 1.5 (0.9 to 1.9) | 18.2 | 21.2 | 21.3 | 19.8 | 0.8 (0.5 to 1.2) |
| Parent race/ethnicity | |||||||||||||||
| NH white | 10.3 | 14.2 | 14.3 | 9.1 | −0.5 (−3.5 to 2.4) | 11.6 | 13.8 | 14.1 | 12.0 | −0.1 (−1.1 to 0.8) | 13.5 | 15.7 | 13.5 | 11.4 | −1.1 (−2.8 to −0.4) |
| NH black | 9.7 | 11.2 | 11.5 | 9.4 | 0.4 (−0.9 to 1.6) | 10.2 | 12.6 | 11.2 | 11.4 | 0.4 (−1.2 to 2.0) | 12.8 | 14.3 | 14.7 | 12.1 | −0.2 (−1.4 to 0.8) |
| NH Asian | 10.9 | 10.9 | 10.2 | 7.3 | −2.9 (−4.8 to −1.0) | 12.3 | 14.4 | 11.2 | 9.2 | −2.8 (−4.4 to −1.8) | 14.0 | 13.4 | 11.4 | 9.8 | −3.7 (−5.1 to −2.4) |
| Hispanic | 14.2 | 18.0 | 18.9 | 16.7 | 1.9 (0.9 to 2.9) | 16.8 | 20.6 | 21.0 | 19.2 | 1.6 (1.0 to 2.0) | 19.3 | 22.4 | 22.4 | 21.2 | 1.0 (0.7 to 1.2) |
| Household income | |||||||||||||||
| ≤50% FPL | 14.4 | 17.6 | 18.7 | 16.5 | 1.6 (0.7 to 2.6) | 16.0 | 19.8 | 19.8 | 18.6 | 1.4 (1.1 to 1.7) | 18.2 | 21.3 | 21.6 | 19.9 | 0.9 (0.4 to 1.2) |
| 50.1%–100.0% FPL | 13.5 | 17.2 | 17.7 | 15.2 | 1.4 (0.2 to 2.5) | 15.7 | 19.7 | 20.5 | 18.4 | 1.7 (1.0 to 2.3) | 18.5 | 21.3 | 21.7 | 20.5 | 1.1 (0.7 to 1.4) |
| 100.1%–133.0% FPL | 13.4 | 16.5 | 17.6 | 14.6 | 1.1 (−0.1 to 2.1) | 16.3 | 19.3 | 19.1 | 17.2 | 0.7 (−0.2 to 1.6) | 18.4 | 21.3 | 20.0 | 18.7 | 0.1 (−0.8 to 0.8) |
| 133.1%–185.0% FPL | 12.4 | 16.3 | 16.9 | 14.1 | 1.2 (0.4 to 1.8) | 15.4 | 18.5 | 18.2 | 15.7 | 0.1 (−0.6 to 0.7) | 17.7 | 20.8 | 20.1 | 17.8 | 0.4 (−1.1 to 1.4) |
| Household education | |||||||||||||||
| <High school | 14.1 | 18.0 | 18.6 | 16.5 | 2.0 (0.9 to 3.0) | 16.7 | 20.6 | 21.0 | 19.3 | 1.6 (1.0 to 2.0) | 19.1 | 22.3 | 22.0 | 21.2 | 1.3 (0.7 to 1.8) |
| High school | 13.2 | 16.3 | 17.8 | 15.4 | 1.6 (0.6 to 2.6) | 14.9 | 18.1 | 19.1 | 17.7 | 1.8 (1.3 to 2.2) | 17.2 | 20.1 | 20.7 | 19.2 | 1.0 (0.5 to 1.5) |
| Some college | 11.1 | 14.9 | 16.2 | 13.4 | 1.8 (1.2 to 2.4) | 13.9 | 17.0 | 17.8 | 15.0 | 0.7 (−0.3 to 1.7) | 16.8 | 18.2 | 20.2 | 17.5 | 0.8 (−0.1 to 1.7) |
| College or more | 10.6 | 11.8 | 13.5 | 10.6 | 0.2 (−1.5 to 2.0) | 11.9 | 16.1 | 15.1 | 14.0 | 0.4 (−1.7 to 2.5) | 15.2 | 17.0 | 18.2 | 14.9 | −0.5 (−3.2 to 2.0) |
| Median household income | |||||||||||||||
| ≤$32,738 | 14.7 | 18.2 | 18.7 | 16.3 | 1.3 (0.3 to 2.3) | 16.9 | 20.6 | 20.7 | 19.6 | 1.4 (0.9 to 1.8) | 18.7 | 22.4 | 22.7 | 20.4 | 1.0 (0.3 to 1.5) |
| $32,739–40,278 | 13.9 | 17.5 | 18.4 | 15.9 | 1.5 (0.1 to 2.7) | 16.0 | 20.4 | 20.8 | 18.5 | 1.3 (0.8 to 1.8) | 18.3 | 21.9 | 22.5 | 20.9 | 1.1 (0.7 to 1.4) |
| $40,279–51,534 | 13.0 | 16.8 | 17.9 | 15.7 | 1.8 (0.7 to 2.7) | 15.4 | 19.2 | 19.8 | 17.9 | 1.5 (0.8 to 2.2) | 19.1 | 21.2 | 20.9 | 19.4 | 0.3 (−0.7 to 1.3) |
| ≥$51,535 | 12.4 | 15.5 | 16.7 | 14.0 | 1.4 (0.5 to 2.1) | 15.1 | 17.7 | 18.2 | 16.3 | 1.1 (0.3 to 1.8) | 17.1 | 19.2 | 19.1 | 18.7 | 0.8 (0.2 to 1.3) |
Obesity is having a BMI ≥95th percentile of CDC's gender- and age-specific growth reference values.
Average annual percent change (AAPC) based on log-linear regression model. Bold AAPC (95% confidence interval) represent statistically significant changes over the specified time period.
WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; NH, non-Hispanic; FPL, federal poverty level.
Trends in Obesity by Race/Ethnicity
Consistent with other studies,5,6 the prevalence of obesity differed by ethnicity with Hispanic children having the highest rates (Table 2). From 2003 to 2012, obesity prevalence among most NH black and white children did not change while it significantly increased for Hispanic children and significantly decreased for NH Asian children (Table 2).
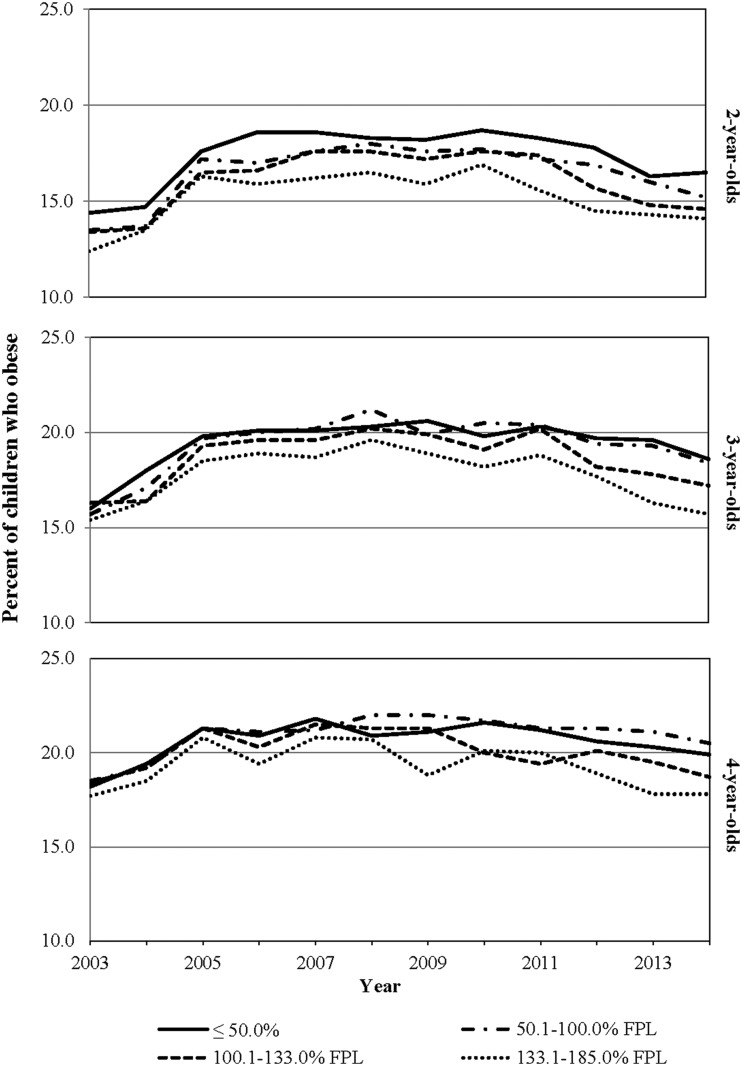
Trends in Obesity by Household Income
In general, at every year and across all three age groups, obesity prevalence was higher among children living in the lowest income households (Fig. 2; Table 2). Based on joinpoint analysis, obesity prevalence for the majority of household income levels for the three age groups significantly increased until 2005, remained relatively constant until 2010, and then significantly decreased until 2014 (Supplementary Table S2). Furthermore, the trends in obesity prevalence were the same for children living in poor (50.1%–100.0% FPL) and extremely poor households (<50% FPL) (Supplementary Table S2).
Figure 2.
Trends in obesity prevalence by household income and age among WIC-participating children: Los Angeles County, 2003–2014. WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; FPl, federal poverty level.
Although obesity trends significantly decreased since 2010, obesity prevalence in 2014 was higher than in 2003 for most children (Table 2). It had decreased to 2003 levels only for 3- and 4-year-olds from the least poor households (>133% FPL and >100% FPL for 3- and 4-year-olds, respectively) (Table 2). As evident by the AAPC in obesity prevalence in Table 2, obesity worsened among 3- and 4-year-olds from poor households (<100% FPL) during the 12 years, while it did not for low-income children (>100% FPL).
Different patterns were observed by race/ethnicity. A similar pattern as mentioned above was observed for Hispanic children, however, different patterns existed among NH white and NH Asian children. Trends in obesity did not vary by household income for NH black children.
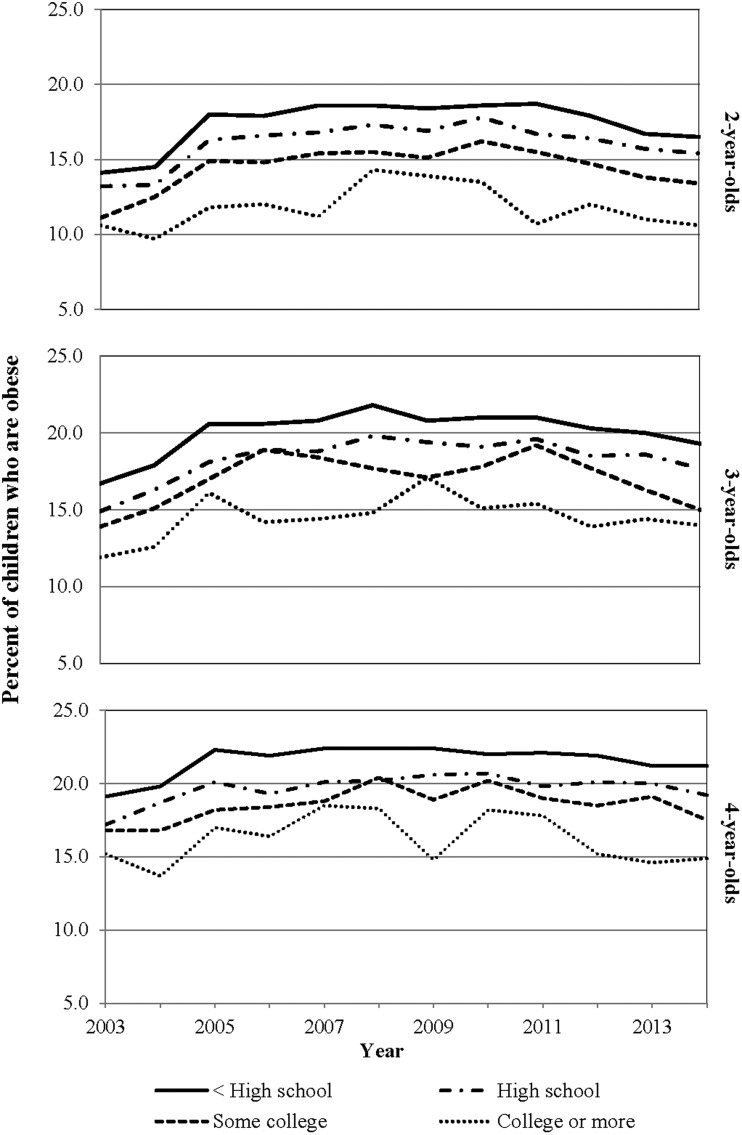
Trends in Obesity by Household Education
At every year and across all three age groups, a consistent gradient in obesity by household education existed with obesity prevalence higher among children living in the lowest educated households (Fig. 3; Table 2). Based on joinpoint analysis, obesity prevalence among the majority of household education levels and across the three age groups significantly increased until 2005, either continued to increase until 2010 or remained constant, and significantly decreased from 2010 to 2014 (Supplementary Table S3). The variability in obesity prevalence observed for 3- and 4-year-olds whose caregivers were college graduates translated into their regression being linear and without any inflection years (Supplementary Table S3).
Figure 3.
Trends in obesity prevalence by household education and age among WIC-participating children: Los Angeles County, 2003–2014. WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
While obesity trends significantly decreased since 2010, 2014 obesity prevalence estimates were still higher than in 2003 for most children although they had decreased to 2003 levels for 2- and 4-year-olds from college-educated households (Table 2). As evident by the AAPC in obesity prevalence in Table 2, obesity did not change for the higher educated households, however, it worsened among the lower educated households (i.e., households without a college degree among 2-year-olds, and households with no more than a high-school degree among 3- and 4-year-olds) (Table 2).
Different patterns were observed by race/ethnicity. A similar pattern as mentioned above was observed for Hispanic children, however, different patterns existed among NH white and NH Asian children. Trends in obesity did not vary by household education for NH black children.
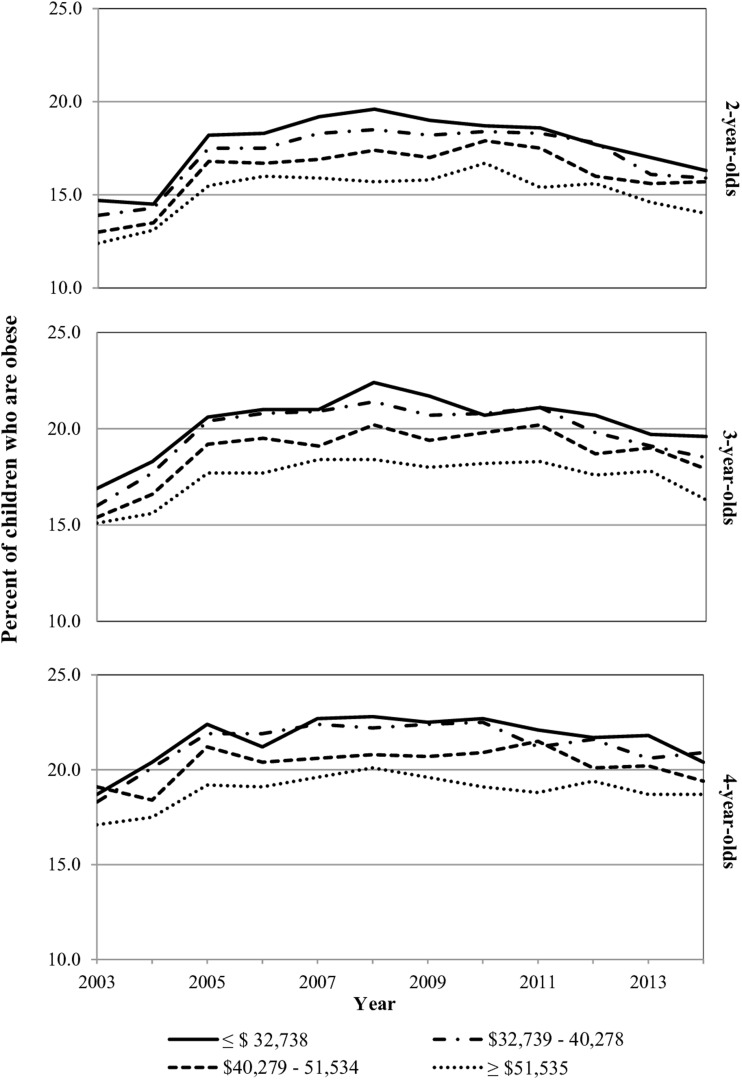
Trends in Obesity by Neighborhood Median Household Income
For the most part, and across all three age groups, obesity prevalence was higher among children living in poorer neighborhoods (Table 2; Fig. 4). Based on joinpoint analysis, obesity prevalence among the majority of neighborhoods and across the three age groups significantly increased until 2005, remained constant until 2010, and significantly decreased from 2010 to 2014 (Supplementary Table S4). The variability in obesity prevalence observed for 4-year-olds living in $40,279–51,534 neighborhoods translated into a linear regression model without any inflection years (Supplementary Table S4). Among 2- and 4-year-olds, the trends in obesity prevalence were the same for children living in the two poorest neighborhoods (lower two quartiles) (Supplementary Table S4).
Figure 4.
Trends in obesity prevalence by median household income and age among WIC-participating children: Los Angeles County, 2003–2014. WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
While obesity trends significantly decreased since 2010, obesity prevalence in 2014 was still higher than in 2003 for children living in the four different types of neighborhoods (Table 2). As evident from the AAPC in obesity prevalence in Table 2, for the most part, obesity worsened from 2003 to 2014, regardless of neighborhood median household income.
Trends in obesity by median household income did vary by race/ethnicity. A similar pattern as mentioned above was observed for Hispanic children but NH black, white, and Asian children had different patterns.
Discussion
In this article, we report trends in obesity by household- and neighborhood-level socioeconomic indicators among WIC-participating preschool-aged children in LAC, a large metropolitan region where income inequality is among the highest in the country.23 Consistent with a recent national study of WIC preschool-aged participants,6 the overall secular trend in obesity prevalence in our study significantly increased sharply from 2003 to 2005, then remained constant until 2010 when obesity prevalence began to decrease until 2014. While it varied by age group, for the most part, this trend existed regardless of socioeconomic indicator. Despite the decreasing trend between 2010 and 2014, the 2014 estimates were not back to 2003 levels except among some higher SES children.
The recent decreasing trend could, in part, be due to community-based interventions implemented to address childhood obesity in LAC over the past decade.24–26 Since 2005, the local health department and major funders have allocated considerable resources to establish major initiatives to address adult and childhood obesity in underresourced communities.24–26 These initiatives have supported both educational and environmental approaches with the former aiming to promote healthy eating and physical activity behaviors and the latter seeking to increase the capacity of communities to improve access to healthy food, provide opportunities for exercise and play, and/or provide environments that support children's optimal growth and development. The decreasing trend could also be due to the 2009 WIC food package change that increased access, availability and consumption of fruits and vegetables and whole grains, and decreased consumption of fruit juice and whole milk.16
Children from less educated and poorer households also experienced significant increases in the AAPC in obesity prevalence from 2003 to 2014, while children from more educated and less poor households generally did not experience a significant change. Drawing on Link and Phelan's theory of fundamental causes,27 we speculate that these differences by household-level socioeconomic indicators may be partially attributed to the capacity of these less poor and more educated households to more readily take advantage of the benefits of these environmental interventions or that these interventions may not have reached all communities equally. The differences by household-level socioeconomic indicators may, in part, also be due to differences in literacy, including health literacy, and numeracy among low-SES households.13,28 Although findings are inconclusive as to whether these are risk factors for childhood obesity,28 additional efforts might have been needed to tailor these interventions to low-SES households such as by having educational materials be at a fourth to sixth grade reading level or by using colors to help distinguish healthy from unhealthy foods.29
Across all age groups, the trends in obesity by household education were parallel highlighting the pronounced and consistent gradient in obesity by household education compared to household income. This supports the argument in a recent systematic review of educational attainment and adult obesity30 that household education is more important than income among those with fewer resources,30,31 or when prevention and treatment are known.32 Parents with higher education may be creating an “obesoprotective” environment for their children by engaging in healthier behaviors.22,31
Similar to other studies, we found that neighborhood socioeconomic conditions influence child's weight early on and that a negative relationship exists with obesity.33–35 Since 2003, the prevalence of obesity has worsened among children from all neighborhoods. With the median household income in LAC at $55,746 in 2014,36 most of these neighborhoods were of low-income. It could be that these neighborhoods are identical in terms of the resources and amenities, such as grocery stores and physical activity facilities, available. Hence, we were not able to detect a difference in the change in obesity prevalence over time.
Low-income neighborhoods have improved in recent years, partly due to the 2009 WIC food package change that improved access to healthy foods in WIC-participants' neighborhoods,16 and the aforementioned obesity-prevention efforts that occurred in low-income communities in LAC.24–26 However, given that the prevalence of obesity has significantly increased since 2003, additional community-level efforts are needed to overcome the deprivation and obesogenic nature of these neighborhoods.
During this study's 12-year period, 2- and 3-year-olds experienced the greatest increase in obesity, suggesting that the first few years of childhood are a key opportunity to prevent obesity among at-risk, low-income children. The association of disadvantage in early childhood with outcomes later in life is often examined37; however, this study lends support that early disadvantage increases the risk of obesity in early childhood. We found that socioeconomic disparities were pronounced among low-income children as young as 2 years of age, and Jones-Smith et al. found that trajectories of obesity risk by SES begin to diverge as early as 9 months of age.38 Since early childhood obesity tracks into adulthood,39,40 every effort should be made to target obesity risk factors during pregnancy and child's infancy such as mother's gestational weight gain, child's high birthweight, exclusive breastfeeding, and timing of complementary foods.41,42
To our knowledge, this is the first study to examine obesity trends among low-income preschool-aged children by multiple SES measures, including neighborhood SES. The trends observed are not uniform across these children, and the different patterns observed highlight the need for effective prevention efforts for the most vulnerable children. We examined obesity trends every year instead of every two as done by Pan et al.6 which allowed us to determine the specific year of the inflection points. Our large sample size enabled us to have four categories for each SES measure and not three as is sometimes the case.43 This level of disaggregation provided a more complete understanding of the trends in obesity. Finally, measured heights and weights of high validity were used.19
One limitation of this study is that the findings are not generalizable to WIC-participating children outside of LAC and where the racial/ethnic composition is different. The observed trends were primarily due to the trends among Hispanic children. Compared to the other racial/ethnic groups, Hispanic children experienced the highest rates of obesity. The prevalence of obesity in this population has also worsened since 2003, whereas among other racial/ethnic groups it remained constant, and in the case of NH Asian children, it even improved. Variability also existed in the trends in obesity among the children whose caregivers had at least a college degree, possibly due to the relatively small numbers of these children (1000–2800).
Conclusion
While trends in obesity among WIC-participating children in LAC decreased between 2010 and 2014, differences exist by child's SES. In the fight against childhood obesity, low-income families' socioeconomic circumstances should be targeted as our findings suggest that they are at increased risk of obesity and may not be reaping the greatest benefit from obesity-prevention efforts. Prevention efforts should occur during the first 2 years of childhood as by age 2 socioeconomic differences in obesity already exist. Future research should explore the role of SES on obesity among low-income preschool-aged children and the most effective interventions for these vulnerable children.
Supplementary Material
Acknowledgments
We thank Lizbeth Delatorre and Andrew Nguyen for assistance with formatting the article, and gratefully acknowledge Dr. Evelyn Blumenberg, Dr. Judith Siegel, Kiran Saluja, Judy Gomez, Mike Whaley, and Armando Jimenez for their contributions to this work. This study was supported by 1R01HD072296 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and by First 5 LA, a child advocacy and grant-making organization created by California voters to invest Proposition 10 tobacco taxes to improve the lives of children from prenatal to age 5 in Los Angeles County. The funders were not involved in any part of the study, including reviewing the content of this article.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Skinner AC, Ravanbakht SN, Skelton JA, et al. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics 2018;141:e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hales CM, Fryar CD, Carroll MD, et al. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA 2018; [Epub ahead of print]; DOI: 10.1001/jama.2018.3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden C, Carroll M. Prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2007–2008. 2010. NCHS Health E-Stat; 2010. Available at https://cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.pdf Last accessed April6, 2018 [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sekhobo J, Edmunds L, Whaley S, et al. Obesity prevalence among low-income, preschool-aged children—New York city and Los Angeles County, 2003–2011. MMWR Morb Mortal Wkly Rep 2013;62:17–22 [PMC free article] [PubMed] [Google Scholar]
- 6.Pan L, Freedman DS, Sharma AJ, et al. Trends in obesity among participants aged 2–4 years in the Special Supplemental Nutrition Program for Women, Infants, and Children—United States, 2000–2014. MMWR Morb Mortal Wkly Rep 2016;65:1256–1260 [DOI] [PubMed] [Google Scholar]
- 7.Ogden CL, Carroll MD, Fakhouri TH, et al. Prevalence of obesity among youths by household income and education level of head of household—United States 2011–2014. MMWR Morb Mortal Wkly Rep 2018;67:186–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thorn B, Tadler C, Huret N, et al. WIC Participant and Program Characteristics 2014. Alexandria, VA; Insight Policy Research, 2015 [Google Scholar]
- 9.Pan L, McGuire LC, Blanck HM, et al. Racial/ethnic differences in obesity trends among young low-income children. Am J Prev Med 2015;48:570–574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freedman DS, Sharma AJ, Hamner HC, et al. Trends in weight-for-length among infants in WIC From 2000 to 2014. Pediatrics 2017;139:pii: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaparro MP, Wang MC, Whaley SE. Neighborhood obesity trends among 2–5 year old children participating in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) in Los Angeles County, 2002–2011. Los Angeles, CA; First 5 LA; 2013. Available at https://first5la.org/files/08149_FinalReport_06302013.pdf Last accessed Februrary 15, 2018 [Google Scholar]
- 12.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr 2006;84:707–716 [DOI] [PubMed] [Google Scholar]
- 13.Cohen AK, Syme SL. Education: A missed opportunity for public health intervention. Am J Public Health 2013;103:997–1001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Briley M, McAllaster M. Nutrition and the child-care setting. J Am Diet Assoc 2011;111:1298–1300 [DOI] [PubMed] [Google Scholar]
- 15.Lovasi GS, Hutson MA, Guerra M, et al. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009;31:7–20 [DOI] [PubMed] [Google Scholar]
- 16.Schultz DJ, Byker Shanks C, Houghtaling B. The impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children food package revisions on participants: A systematic review. J Acad Nutr Diet 2015;115:1832–1846 [DOI] [PubMed] [Google Scholar]
- 17.Pfeffer FT, Danziger S, Schoeni RF. Wealth disparities before and after the Great Recession. Ann Am Acad Pol Soc Sci 2013;650:98–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.PHFE-WIC. First5LA. Los Angeles County WIC data. Available at http://lawicdata.org/ Last accessed September12, 2017
- 19.Crespi CM, Alfonso VH, Whaley SE, et al. Validity of child anthropometric measurements in the Special Supplemental Nutrition Program for Women, Infants, and Children. Pediatr Res 2012;71:286–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tanner JM. Foetus into Man: Physical Growth from Conception to Maturity (revised and enlarged edition). Cambridge, MA; Harvard University Press, 1990 [Google Scholar]
- 21.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat 11 2002;1–190 [PubMed] [Google Scholar]
- 22.Duncan GJ, Daly MC, McDonough P, et al. Optimal indicators of socioeconomic status for health research. Am J Public Health 2002;92:1151–1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.PolicyLink PERE. An equity profile of the Los Angeles region. Oakland, CA: PolicyLink and USC PERE; 2017. Available at http://dornsife.usc.edu/assets/sites/242/docs/EquityProfile_LA_Region_2017_Full_Final_Web.pdf Last accessed February19, 2018 [Google Scholar]
- 24.ChooseHealthLA! Early childhood obesity prevention initiative. Los Angeles, CA: Los Angeles County Department of Public Health; 2013. Available at http://publichealth.lacounty.gov/chronic/docs/20131227_Early_Childhood.pdf Last accessed February19, 2018 [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC). Communities putting prevention to work: Los Angeles County, California obesity and tobacco use prevention. Los Angeles, CA: Los Angeles County Department of Public Health; Available at http://publichealth.lacounty.gov/docs/CommunityProfileLosAngeles.pdf Last accessed February19, 2018 [Google Scholar]
- 26.First 5 LA. Reducing early childhood obesity in Los Angeles County. Los Angeles, CA: First 5 LA; 2014. Available at http://first5la.org/index.php?r=site/article&id=3092 Last accessed February19, 2018 [Google Scholar]
- 27.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav 1995;Spec No:80–94 [PubMed] [Google Scholar]
- 28.Berkman ND, Sheridan SL, Donahue KE, et al. Health literacy interventions and outcomes: An updated systematic review. Evid Rep Technol Assess (Full Rep) 2011;1–941 [PMC free article] [PubMed] [Google Scholar]
- 29.Sanders LM, Perrin EM, Yin HS, et al. “Greenlight study”: A controlled trial of low-literacy, early childhood obesity prevention. Pediatrics 2014;133:e1724–e1737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cohen AK, Rai M, Rehkopf DH, et al. Educational attainment and obesity: A systematic review. Obes Rev 2013;14:989–1005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mirowsky J, Ross CE. Education, Social Status and Health. New York: Walter de Gruyter, 2003 [Google Scholar]
- 32.Cutler DM, Lleras-Muney A. Education and health: Evaluating theories and evidence. National Bureau of Economic Research. 2006. Available at https://ideas.repec.org/p/nbr/nberwo/12352.html Last accessed September10, 2017
- 33.Kimbro RT, Denney JT. Neighborhood context and racial/ethnic differences in young children's obesity: Structural barriers to interventions. Soc Sci Med 2013;95:97–105 [DOI] [PubMed] [Google Scholar]
- 34.Nobari TZ, Wang MC, Chaparro MP, et al. Immigrant enclaves and obesity in preschool-aged children in Los Angeles County. Soc Sci Med 2013;92:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chaparro MP, Whaley SE, Crespi CM, et al. Influences of the neighbourhood food environment on adiposity of low-income preschool-aged children in Los Angeles County: A longitudinal study. J Epidemiol Commun Health 2014;68:1027–1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.U.S. Census Bureau. 2014 American community survey 1-year estimates. Table B19013: Median household income in the past 12 months. Available at https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_14_1YR_B19013&prodType=table Last accessed February19, 2018
- 37.Lee H, Andrew M, Gebremariam A, et al. Longitudinal associations between poverty and obesity from birth through adolescence. Am J Public Health 2014;104:e70–e76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones-Smith JC, Dieckmann MG, Gottlieb L, et al. Socioeconomic status and trajectory of overweight from birth to mid-childhood: The early childhood longitudinal study-birth cohort. PLoS One 2014;9:e100181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Freedman DS, Khan LK, Serdula MK, et al. The relation of childhood BMI to adult adiposity: The Bogalusa Heart Study. Pediatrics 2005;115:22–27 [DOI] [PubMed] [Google Scholar]
- 40.Guo SS, Wu W, Chumlea WC, et al. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr 2002;76:653–658 [DOI] [PubMed] [Google Scholar]
- 41.Woo Baidal JA, Locks LM, Cheng ER, et al. Risk factors for childhood obesity in the first 1,000 days. Am J Prev Med 2016;50:761–779 [DOI] [PubMed] [Google Scholar]
- 42.Hunsberger M. Early feeding practices and family structure: Associations with overweight in children. Proc Nutr Soc 2014;73:132–136 [DOI] [PubMed] [Google Scholar]
- 43.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health 2010;100 (Suppl 1):S186–S196 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.