Abstract
Objective
To analyze and characterize data about clinical outcome and complication rates in three-column osteotomies (3 CO) for treatment of rigid adult spine deformity (ASD).
Methods
Baseline and postoperative clinical outcomes, considering the Oswestry Disability Index (ODI) and Scoliosis Research Society-22 (SRS-22) questionnaires, radiographic parameters, and demographic data of patients who underwent 3 CO procedure for fixed ASD treatment were collected. Surgical characteristics and reports of perioperative complications were recorded, as well as those that occurred at a minimum follow-up of 12 months.
Results
Ten patients underwent 3 CO and had a minimum follow-up of 12 months (mean 24 months). The patients showed significantly improved health-related quality of life scores (ODI, SRS-22 total, function/activity, pain, and appearance). They also presented a significant improvement in all radiographic parameters considered in the study. Taking into account the surgical procedure, the operative time was significantly higher in patients with staged procedure than in patients with single-stage surgery (p = 0.003), with similar estimated blood loss and complication incidence. There were ten complications in six patients (60%), with a mean of 1.0 complication per patient.
Conclusions
Despite of the high complication rates, 3 CO was an effective technique, considering clinical and radiographic outcomes, to treat complex cases of rigid ASD in a sample of patients operated in a Brazilian spine center, with a minimum follow-up of 12 months.
Keywords: Bone malalignment, Scoliosis, Osteotomy, Treatment outcome, Postoperative complications
Resumo
Objetivo
Analisar e descrever dados sobre o resultado clínico e as taxas de complicações em pacientes submetidos a osteotomia das três colunas (O3 C) para o tratamento de deformidade da coluna vertebral no adulto (DCVA) rígida em um mesmo serviço no Brasil.
Métodos
Foram coletados dados clínicos, considerando os questionários Oswestry Disability Index (ODI) e Scoliosis Research Society-22 (SRS-22), e radiográficos pré- e pós-operatórios, além de dados demográficos, de pacientes submetidos a O3 C para tratamento de DCVA rígidas. Também foram coletados dados sobre o procedimento cirúrgico e complicações perioperatórias e no seguimento dos pacientes, com tempo mínimo de 12 meses.
Resultados
O estudo incluiu dez pacientes com mínimo de 12 meses de seguimento (média de 24 meses). Houve melhoria significante nos indicadores de qualidade de vida (ODI, SRS-22 Total, Função/Atividade, Dor e Aparência). Houve melhoria significante de todos os parâmetros radiográficos analisados. Considerando o procedimento cirúrgico, o tempo de cirurgia foi significativamente maior nos pacientes com cirurgia estagiada do que naqueles com apenas um tempo cirúrgico (p = 0,003), foram similares o sangramento estimado e a incidência de complicações entre tais pacientes. Dez complicações foram observadas em seis (60%) pacientes, com média de uma complicação por paciente.
Conclusões
Apesar da elevada taxa de complicações, demonstrou-se que a O3 C é uma técnica bem-sucedida considerando o resultado clínico e radiográfico no tratamento de casos complexos de DCVA rígida em uma amostra de pacientes operados em um serviço de saúde brasileiro, com mínimo de 12 meses de seguimento.
Palavras-chave: Mau alinhamento ósseo, Escoliose, Osteotomia, Resultado do tratamento, Complicações pós-operatórias
Introduction
The prevalence of adult spinal deformity (ASD) has tended to increase, associated to population aging.1, 2 In Brazil, a recent study showed a prevalence of 18.5% of ASD in outpatients, reaching 28.8% in individuals over 60 years of age.3 Among the causes of ASD, iatrogenesis is noteworthy after long lumbar arthrodeses; other causes include deformities associated with multiple fractures due to bone insufficiency (osteoporosis), rheumatologic diseases, such as ankylosing spondylitis, or even degenerative disc disease.4
The treatment of rigid ASD is of one of the major challenges in spinal surgery; these are often revision procedures, performed in elderly patients with comorbidities, and osteotomies are frequently required in order to achieve deformity correction.4, 5, 6, 7, 8 Schwab et al.9 described a classification system for spinal osteotomy, based on the extent of bone resection. The greater the resection, which increases the degree of instability, the greater the possibility in correcting the deformity. Thus, according to the three-column spine concept proposed by Denis,10 osteotomies that compromise the three-column stability have the greatest possibility of angular correction for the deformity.
However, three-column osteotomies (3 CO) present significant risks for patients, with a high incidence of potentially serious complications.4, 6, 8, 11, 12 The vast majority of the information on complication rates and clinical outcomes of 3 CO in the treatment of rigid ASD comes from studies of patients operated in the United States; data on 3 CO patients in Brazil is scarce. The present study is aimed at analyzing and describing data on clinical outcome and complication rates in patients who underwent 3 CO for the treatment of rigid ASD in a single healthcare service in Brazil.
Material and methods
This is a retrospective observational analysis of a prospective database that included patients who underwent 3 CO surgical treatment for ASD in a single healthcare service. The data were analyzed after approval by the Research Ethics Committee of the healthcare service responsible for the study. Patients over 18 years of age with complete data and who had completed a minimum postoperative follow-up of 12 months were included.
Primary data were collected immediately prior to surgery, and included demographic data such as age, gender, body mass index (BMI), and history of prior surgery, as well as clinical and functional assessment using the Oswestry Disability Index (ODI) and the Scoliosis Research Society-22 (SRS-22), translated to and validated into Brazilian Portuguese.13, 14 The data referring to the surgical procedure were: type of osteotomy (according to the classification proposed by Schwab et al.9), site of osteotomy, extent of arthrodesis (proximal and distal fusion level), use or non-use of a screw in the iliac bone, one-time or staged surgery, total surgery time, and estimated blood loss. In the postoperative follow-up, clinical and functional parameters were assessed in order to identify the clinical result obtained in the surgical procedure.
Information on any clinical and neurological complications was collected. Any alteration in the neurological examination of the patient, upon waking or during the entire follow-up period, was considered a neurological complication when compared with findings from examination immediately before the surgical procedure.
The radiographic evaluation was made using total (panoramic view) radiographs of the spine in orthostasis and followed a specific pattern.15 The scanned images were analyzed with the Surgimap Spine software (Nemaris Inc. New York, USA) for the measurement of the radiographic parameters of interest in ASD assessment: sagittal vertical axis (SVA), thoracic kyphosis (TK), lumbar lordosis (LL), pelvic version (PV), pelvic incidence (PI), and discrepancy between PI and LL (PI-LL). The recently standardized nomenclature for such parameters in Brazilian Portuguese was adopted.16
The pre and postoperative clinical and radiographic parameters were compared using the paired and unpaired Student's t-test. The Shapiro–Wilk test was used to check the normality of the variables. Statistical analysis was performed with Stata® 11 SE, and the significance level was set at 5%. Thus, results considered statistically significant had a p-value of less than 0.05.
Results
Ten patients with completed data were included, one man and nine women (Table 1). The mean age at surgery was 66.6 years (range: 57–79 years). The mean BMI of the patients was 29.5 kg/m2 (range: 25.5–32.4 kg/m2). The patients were classified in accordance with the SRS-Schwab classification17: seven (70%) had no coronal plane deformity (type N), two (20%) had a lumbar deformity (type L), and one (10%) had a double curve (type D). As for the sagittal modifiers, all patients had at least “+” for the three modifiers (SVA, PV, and PI-LL). Only one patient did not have a history of previous surgery; the mean of the sample was 1.6 prior surgical procedures, ranging from 1 to 3. The mean follow-up time was 24 months (range: 14–34). One patient died in the perioperative period; her postoperative data were not considered.
Table 1.
Summary of demographic characteristics and SRS-Schwab classification of patients included in the study.
| Patients | Gender | Age (years) | BMI (kg/m2) | Classification SRS-SCHWAB |
No. of previous surgeries |
|---|---|---|---|---|---|
| 1 | F | 70 | 28.2 | N; SVA++; PT++; PI-LL++ | 1 |
| 2 | F | 60 | 25.5 | D; SVA+; PT++; PI-LL+ | 3 |
| 3 | F | 78 | 28.6 | N; SVA++; PT++; PI-LL++ | 2 |
| 4 | F | 66 | 32.4 | N; SVA++; PT++; PI-LL++ | 3 |
| 5 | F | 65 | 28.3 | N; SVA+; PT++; PI-LL++ | 1 |
| 6 | F | 66 | 28.6 | L; SVA+; PT++; PI-LL++ | 0 |
| 7 | F | 67 | 26.7 | L; SVA++; PT++; PI-LL++ | 2 |
| 8 | F | 79 | 29.7 | N; SVA++; PT++; PI-LL++ | 1 |
| 9 | M | 58 | 31.3 | N; SVA++; PT++; PI-LL++ | 2 |
| 10 | F | 57 | 31.2 | N; SVA+; PT++; PI-LL++ | 1 |
F, female; BMI, body mass index; M, male.
Table 2 shows the pre and postoperative values of the radiographic parameters. A statistically significant improvement was observed in all parameters considered (SVA, PV, LL, and PI-LL; p ≤ 0.001). Regarding clinical features (Table 3), a significant improvement was observed in the ODI and SRS-22 total scores, and in the Function/Activity, Pain, and Appearance domains (p < 0.003). A trend toward improvement was observed in the SRS-22 Mental Health domain score, albeit not significant (p = 0.080).
Table 2.
Comparison of pre and postoperative radiographic parameters.
| Radiographic parameter | Preoperative period Mean (SD) |
Postoperative period Mean (SD) |
p |
|---|---|---|---|
| SVA (cm) | 13.3 (5.6) | 5.6 (2.3) | 0.001 |
| PV (°) | 39.5 (5.3) | 25.3 (6.8) | <0.001 |
| LL (°) | 11.2 (12.1) | 41.0 (8.3) | <0.001 |
| PI-LL (°) | 44.7 (16.9) | 15.9 (8.9) | <0.001 |
SD, standard deviation; SVA, sagittal vertical axis; PI-LL, discrepancy between pelvic incidence and lumbar lordosis; LL, lumbar lordosis; PV, pelvic version.
Table 3.
Comparison of pre and postoperative quality of life indicators.
| Scores | Preoperative period Mean (SD) |
Postoperative period Mean (SD) |
p |
|---|---|---|---|
| ODI | 60.4 (7.6) | 32.2 (8.7) | <0.001 |
| SRS-22 total | 2.1 (0.5) | 3.4 (0.6) | <0.001 |
| Function/activity | 2.1 (0.5) | 3.0 (0.6) | 0.003 |
| Pain | 2.2 (0.8) | 3.7 (0.7) | 0.6 |
| Appearance | 1.6 (0.6) | 3.0 (0.9) | <0.001 |
| Mental health | 2.9 (0.7) | 3.6 (0.7) | 0.08 |
SD, standard deviation; ODI, Oswestry Disability Index; SRS-22, Scoliosis Research Society-22.
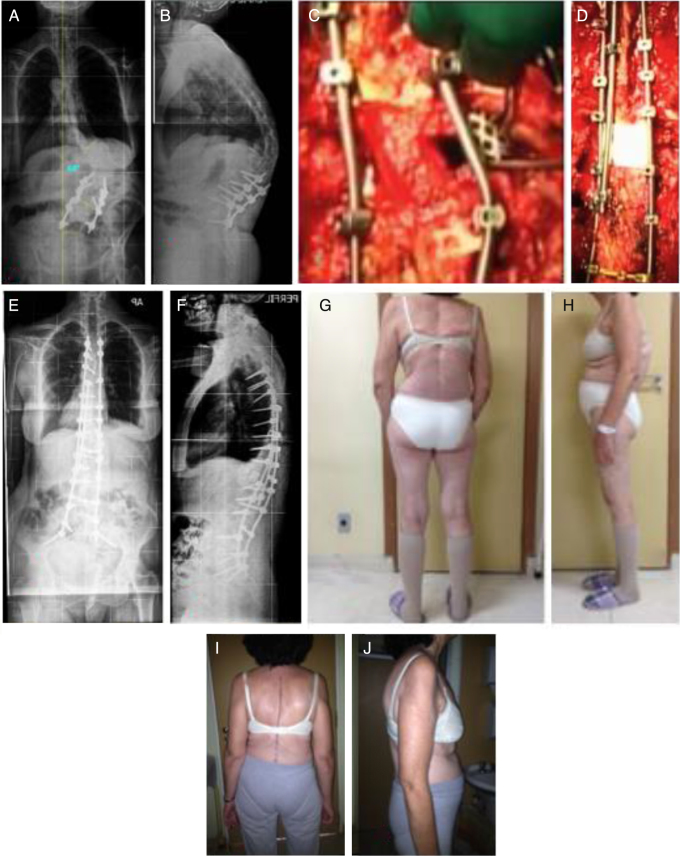
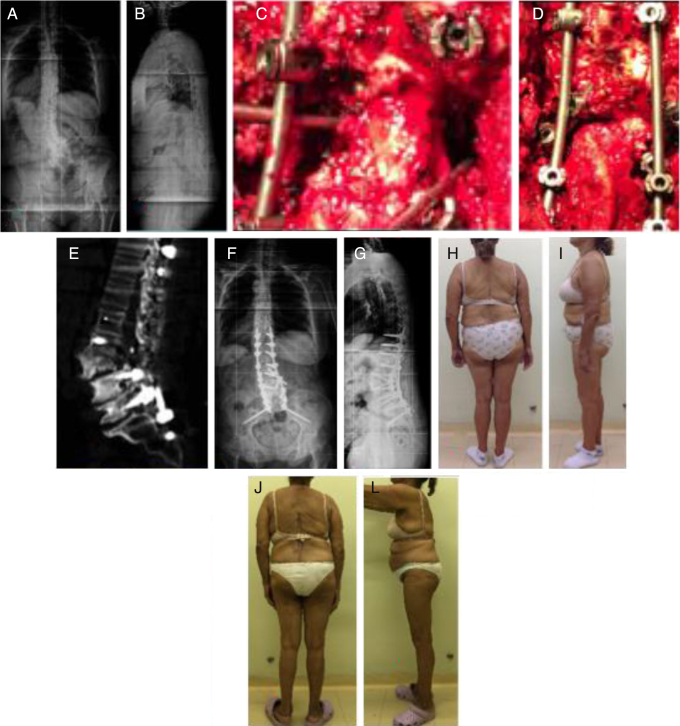
Table 4 presents data on surgical procedures. Three patients (30%) had one stage surgery, while six (60%) had two stages, and one (10%), three stages. The mean time of surgery (considering the sum of the surgical times in cases of more than one surgery) was 505 min (392–640), significantly higher in patients undergoing staged surgery than in those undergoing only one surgery (549.3 min ± 58.6 min vs. 403.3 min ± 9.9 min, p = 0.003). The mean estimated blood loss was 3630 ml (2600–4600 ml), also considering the sum of the surgical times in cases of more than one surgery. There was a trend toward greater estimated blood loss in patients who underwent staged surgery than in those who underwent only one surgery, but it was not significant (3914.3 ml ± 651.7 ml vs. 2966.7 ml ± 472.6 ml, p = 0.055). Regarding the type of osteotomy, one (10%) patient underwent grade 5 osteotomy (Fig. 1), corresponding to vertebral column resection (VCR); four (40%), grade 4 osteotomy (Fig. 2), corresponding to pedicle subtraction osteotomy extended to the resection of the vertebral plateau and superior intervertebral disc; and five (50%), grade 3 osteotomy, conventional pedicle subtraction. Grade 5 osteotomy (VCR) was performed at T12 level, and all pedicle subtraction osteotomies, both grade 3 and 4, were performed at L3 level. The mean lumbar lordosis gain in patients who underwent pedicle subtraction osteotomy was 34.2°, ranging from 25° to 46°.
Table 4.
Summary of data on the characteristics of surgical procedures and occurrence of complications.
| Patient | Surgical stages | Estimated blood loss (ml) | Surgery time (min) | Fusion level | Osteotomy | Osteotomy classification | No. of nails° | Complications |
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 4200 | 560 | T4-ILIAC | Sub P L3 | 3 | 2 | 1 |
| 2 | 2 | 4500 | 615 | T4-ILIAC | VCR T12 | 5 | 3 | 0 |
| 3 | 1 | 2600 | 410 | T4-ILIAC | Sub P L3 | 3 | 2 | 1 |
| 4 | 2 | 3500 | 525 | T4-ILIAC | Sub P L3 | 4 | 4 | 1 |
| 5 | 2 | 2700 | 495 | T10-ILIAC | Sub P L3 | 3 | 4 | 0 |
| 6 | 1 | 3500 | 408 | T10-ILIAC | Sub P L3 | 4 | 4 | 2 |
| 7 | 2 | 3900 | 520 | T4-ILIAC | Sub P | 3 | 4 | 0 |
| 8 | 3 | 4600 | 640 | T4-ILIAC | Sub P | 4 | 4 | 1 |
| 9 | 1 | 2800 | 392 | T10-S1 | Sub P | 3 | 2 | 0 |
| 10 | 2 | 4000 | 490 | T10-ILIAC | Sub P | 4 | 4 | 4 |
Min, minute; N°, number; Sub P, pedicle subtraction; VCR, vertebral column resection.
Fig. 1.
Patient with deformity classified as D; SVA+;PT++;IP-LL+: (A) Rigid lumbar curve post-arthrodesis with Cobb of 68° and thoracic curve of 35°; (B) rigid sagittal deformity with SVA: 9.5 cm, PV: 40°, PI-LL: 13°; (C) patient underwent grade 5 arthrodesis (VCR) at T12, to correct the deformity in the sagittal and coronal planes; (D) the correction achieved using three rods that crossed the osteotomy site; (E) postoperative radiograph shows the correction achieved in the coronal plane, with lumbar curve of 13° (80%), and arthrodesis (T4 to the iliac bone); (F) postoperative radiograph shows correction in the sagittal plane, with SVA: 0.4 cm, PV: 12°, IP-LL: −7°; (G) preoperative clinical aspect of the patient's back; (H) preoperative clinical aspect, lateral side; (I) postoperative clinical aspect of the patient's back and (J) clinical aspect of the lateral view. SVA, sagittal vertical axis; PV, pelvic version; PI-LL, discrepancy between pelvic incidence and lumbar lordosis; VCR, vertebral column resection.
Fig. 2.
Patient with deformity classified as L;SVA+;PT++;PI-LL++: (A) Cobb rigid lumbar curve of 32°; (B) rigid sagittal deformity with SVA: 9.3 cm, PV: 34°, IP-LL: 57°; (C) patient underwent grade 4 (Sub P) L3 arthrodesis to correct the deformity; (D) the correction achieved using four rods crossing the osteotomy site; (E) postoperative computed tomography showing the resection of the superior plateau and the superior intervertebral disc with sagittal angular correction; (F) postoperative radiograph showing the correction obtained in the coronal plane, with lumbar curve of 8° (75%), and arthrodesis (T10 to iliac bone); (G) postoperative radiograph showing correction in the sagittal plane, with SVA: 6.1 cm, PV: 21, IP-LL: 11°; (H) preoperative clinical aspect of the patient's back; (I) preoperative clinical aspect, lateral view; (J) postoperative clinical aspect of the patient's back and (L) postoperative clinical aspect, lateral view. SVA, sagittal vertical axis; PV, pelvic version; PI-LL, discrepancy between pelvic incidence and lumbar lordosis; Sub P, pedicle subtraction.
Considering the level of fusion, T10 was the proximal level in six patients (60%) and T4 in four (40%). Regarding the distal level, all patients (100%) had sacrum involvement; nine (90%) with fixation to the iliac and one (10%) without. In all patients (100%) with iliac fixation, the S2 alar-iliac technique was used.18 In three patients (30%), two rods that crossed the level of osteotomy were used; in one (10%), three rods, and in six (60%), four rods were used.
Six (60%) patients had at least one complication, in a total of ten events, with a mean of one complication per patient. Three (30%) patients woke up from surgery with some degree of reduction in motor strength in the lower limbs compared to the preoperative state; two recovered and one did not. Four (40%) presented surgical wound complications, be it dehiscence or infection, and all required a second surgical procedure, with a mean of 1.7 procedures per patient. One (10%) patient evolved with proximal junctional kyphosis deformity >10° (considering the angle measured between the most proximal instrumented vertebrae and two levels above), but the patient had no related complaints and did not undergo any other surgical procedure. One case of pulmonary thromboembolism was observed, and managed with drug treatment. One (10%) patient died on the 23rd day of hospitalization due to complications. The mean number of hospitalization days was 23.3, ranging from seven to 61. The incidence of complications was similar between patients submitted to staged surgery and only one surgery (p = 0.849).
Discussion
The global aging of the population is associated with an increased prevalence of age-related health problems, including spinal deformity. It has recently been shown that the impact of spinal deformity on patients’ quality of life is comparable to that of other chronic diseases such as pneumopathies, diabetes, and cardiopathy.19, 20 Thus, an increase in the number of ASD correction procedures is to be expected. These procedures often require the use of osteotomies, especially in rigid deformities,5, 6, 8 and are often associated with complications. Publications have shown that patients undergoing 3 CO are subject to even greater risks of complications, including neurological deficits.12 Thus, the present study presented a series of patients who underwent 3 CO for ASD correction, analyzing the patients’ profile, details of the surgery, the correction of radiographic parameters, clinical outcomes, and complications in these patients.
The patients were classified by the SRS-Schwab system, and the majority presented no deformity in the coronal plane (Type N). In the study that proved the clinical relevance of the SRS-Schwab classification,21 it was observed that the incidence of patients with Type N deformity was lower than that of those with coronal deformities, but patients with Type N deformity had a significantly higher incidence of surgery and more frequently needed osteotomies. The fact that the present study included only patients who underwent surgery and 3 CO explains the vast majority of cases classified as Type N. Regarding the sagittal modifiers, all patients in the present study presented alterations in the three modifiers, which is also in agreement with the literature; patients who undergo surgery have worse sagittal modifiers; the worse these modifiers, the more frequent the need for osteotomies.21
3 CO is a technique with high corrective possibility for deformities in the sagittal plane and coronal plane, or in both.5, 6 However, due to the high morbidity associated with this procedure, its indication should be restricted to cases in which there is severe global sagittal disequilibrium and/or rigid deformities, often in patients with long arthrodesed segments of the spine.22 All but one patient, in this 3 CO study, had previously been submitted to surgery on some segment for lumbar arthrodesis. Although the present study considered patients with rigid deformity, a high deformity correction possibility was observed. A significant improvement in all radiographic parameters considered was noted, and the mean gain of lumbar lordosis was 34.2° in patients who underwent pedicle subtraction. The literature indicates that a pedicle subtraction osteotomy has a correction possibility between 25° and 35°.9, 23, 24, 25 In addition to presenting even greater possibility in correcting rigid deformities of the spine, grade 5 osteotomy (VCR) is indicated when there is a concomitant imbalance in the sagittal and coronal planes.23 A grade 5 osteotomy was performed in one patient, classified as SRS-Schwab type D, SVA+, PT++, PI-LL +, who had, in addition to sagittal imbalance and a lumbar curve of 68° in a previously arthrodesed region, a thoracic curve of 35° and coronal imbalance. After surgery, the coronal deformity was corrected to 13° (correction of 55°, 80%), in addition a 9.1 cm SVA correction.
The occurrence of complications in 60% of the patients (6/10), with a mean of one complication/patient, reinforces the high morbidity and complexity of the treatment of ASD with 3 CO described in the literature, with rates of up to 82%.5, 7, 13, 23, 26, 27 Recently, Kelly et al.12 presented the results of a multicentric retrospective analysis of complications in 3 CO surgeries, considering this technique by the main specialists in the United States, and demonstrated complications in 50.8% of the patients. Regarding the occurrence of neurological complications, Lenke et al.27 presented a prospective multicenter study in which they evaluated the neurological outcome in patients undergoing surgical treatment for complex ASD, 79% of whom underwent 3 CO. It was observed that, at the time of discharge, 22.18% of the patients presented some level of loss of strength in the lower limbs and, after sixth months, 10.82% persisted with some loss of strength in the lower limbs. In the present study, three (30%) of the patients presented some degree of loss of strength in the lower limbs and only one (10%) maintained this loss in the postoperative follow-up.
Among the most frequently described complications is pseudarthrosis, followed by implant rupture.5, 24, 28 However, in the present study, no patient presented implant rupture or clinical or radiological suspicion of pseudoarthrosis, with a mean follow-up of 24 months (minimum of 14). The use of multiple-rod constructs crossing the 3 CO site has been recommended to increase stability, and to prevent implant failure and the occurrence of pseudarthrosis.28 More recently, Gupta et al.29 showed that in addition to the number of rods crossing the 3 CO site, the fact that the third or fourth rod was independent (satellite rod), i.e., not connected to the primary rods, presented a significantly lower rate of implant failure and/or pseudarthrosis. In the present study, in most cases the 3 CO site was crossed by two or more rods; in all cases, the rods were “satellites”, without connection to the primary rods, which may have had a protective effect against complications related to implant failure.
A recent study demonstrated the benefits of surgery over conservative treatment in clinical improvement and considered indicators of quality of life for patients with ASD.30 Studies have shown that even patients with clinical and/or surgical complications, including those requiring reoperation, presented improved quality of life indicators after 3 CO.11, 24 The present study demonstrated a significant improvement in quality of life indicators, even with a complication rate of 60% of the cases.
The main limitation of the present study is the small sample size analyzed and the fact that patients from only one healthcare service were included, which reduces the possibility of statistical analysis. However, this study presented data that considered patients submitted to the complex 3 CO surgical procedure, with a minimum of 12 months postoperative follow-up, considering the structure of a Brazilian health service, data still little reported in our midst. One of the purposes of the present study is to raise interest in other healthcare services for the development of multicentric analyses, increase sample size, and improve the possibility for interpretation of data.
Conclusion
Despite the high rate of complications, 3 CO was shown to be a successful technique considering the clinical and radiographic results in the treatment of complex cases of rigid ASD in a sample of patients operated in a Brazilian healthcare service, with a minimum of 12 months follow-up.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at Hospital do Servidor Público Estadual (HSPE), Serviço de Ortopedia e Traumatologia, Grupo de Coluna Vertebral, São Paulo, SP, Brazil.
References
- 1.Schwab F., Dubey A., Gamez L., El Fegoun A.B., Hwang K., PAgala M. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005;30(9):1082–1085. doi: 10.1097/01.brs.0000160842.43482.cd. [DOI] [PubMed] [Google Scholar]
- 2.Schwab F.J., Lafage V., Farcy J.P., Bridwell K.H., Glassman S., Shainline M.R. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976) 2008;33(20):2243–2247. doi: 10.1097/BRS.0b013e31817d1d4e. [DOI] [PubMed] [Google Scholar]
- 3.Barreto M.V., Pratali R.R., Barsotti C.E., Santos F.P., Oliveira C.E., Nogueira M.P. Incidence of spinal deformity in adults and its distribution according SRS-Schwab classification. Coluna/Columna. 2015;14(2):93–96. [Google Scholar]
- 4.Smith J.S., Sansur C.A., Donaldson W.F., 3rd, Perra J.H., Mudiyam R., Choma T.J. Short-term morbidity and mortality associated with correction of thoracolumbar fixed sagittal plane deformity: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 2011;36(12):958–964. doi: 10.1097/BRS.0b013e3181eabb26. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell K.H., Lewis S.J., Rinella A., Lenke L.G., Baldus C., Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am. 2004;86(Suppl 1):44–50. doi: 10.2106/00004623-200403001-00007. [DOI] [PubMed] [Google Scholar]
- 6.Suk S.I., Chung E.R., Lee S.M., Lee J.H., Kim S.S., Kim J.H. Posterior vertebral column resection in fixed lumbosacral deformity. Spine (Phila Pa 1976) 2005;30(23):E703–E710. doi: 10.1097/01.brs.0000188190.90034.be. [DOI] [PubMed] [Google Scholar]
- 7.Yang B.P., Ondra S.L., Chen L.A., Jung H.S., Koski T.R., Salehi S.A. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5(1):9–17. doi: 10.3171/spi.2006.5.1.9. [DOI] [PubMed] [Google Scholar]
- 8.Lenke L.G., Sides B.A., Koester L.A., Hensley M., Blanke K.M. Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res. 2010;468(3):687–699. doi: 10.1007/s11999-009-1037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwab F., Blondel B., Chay E., Demakakos J., Lenke L., Tropiano P. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2014;74(Suppl 1):112–120. doi: 10.1227/NEU.0000000000000182o. [DOI] [PubMed] [Google Scholar]
- 10.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8(8):817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Oʼneill K.R., Lenke L.G., Bridwell K.H., Hyun S.J., Neuman B., Dorward I. Clinical and radiographic outcomes after 3-column osteotomies with 5-year follow-up. Spine (Phila Pa 1976) 2014;39(5):424–432. doi: 10.1097/BRS.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 12.Kelly M.P., Lenke L.G., Shaffrey C.I., Ames C.P., Carreon L.Y., Lafage V. Evaluation of complications and neurological deficits with three-column spine reconstructions for complex spinal deformity: a retrospective Scoli-RISK-1 study. Neurosurg Focus. 2014;36(5):E17. doi: 10.3171/2014.2.FOCUS1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vigatto R., Alexandre N.M., Correa Filho H.R. Development of a Brazilian Portuguese version of the Oswestry Disability Index: cross-cultural adaptation, reliability, and validity. Spine (Phila Pa 1976) 2007;32(4):481–486. doi: 10.1097/01.brs.0000255075.11496.47. [DOI] [PubMed] [Google Scholar]
- 14.Carriço G., Meves R., Avanzi O. Cross-cultural adaptation and validity of an adapted Brazilian Portuguese version of Scoliosis Research Society-30 questionnaire. Spine (Phila Pa 1976) 2012;37(1):E60–E63. doi: 10.1097/BRS.0b013e31823c7cd6. [DOI] [PubMed] [Google Scholar]
- 15.Horton W.C., Brown C.W., Bridwell K.H., Glassman S.D., Suk S.I., Cha C.W. Is there an optimal patient stance for obtaining a lateral 36‘radiograph? A critical comparison of three techniques. Spine (Phila Pa 1976) 2005;30(4):427–433. doi: 10.1097/01.brs.0000153698.94091.f8. [DOI] [PubMed] [Google Scholar]
- 16.Pratali R.R., Hennemann S.A., Amaral R., Silva L.E., De Carvalho M.O., Daher M.T. Standardized terminology of adult spine deformity for Brazilian Portuguese. Coluna/Columna. 2015;14(4):281–285. [Google Scholar]
- 17.Schwab F., Ungar B., Blondel B., Buchowski J., Coe J., Deinlein D. SRS-schwab adult spinal deformity classification. A validation study. Spine (Phila Pa 1976) 2012;37(12):1077–1082. doi: 10.1097/BRS.0b013e31823e15e2. [DOI] [PubMed] [Google Scholar]
- 18.Kebaish K.M. Sacropelvic fixation. Techniques and complications. Spine (Phila Pa 1976) 2010;35(25):2245–2251. doi: 10.1097/BRS.0b013e3181f5cfae. [DOI] [PubMed] [Google Scholar]
- 19.Bess S., Line B., Fu K.M., McCarthy I., Lafage V., Schwab F. The health impact of symptomatic adult spinal deformity: comparison of deformity types to United States population norms and chronic diseases. Spine (Phila Pa 1976) 2016;41(3):224–233. doi: 10.1097/BRS.0000000000001202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pellisé F., Vila-Casademunt A., Ferrer M., Domingo-Sàbat M., Bagó J., Pérez-Grueso F.J. Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J. 2015;24(1):3–11. doi: 10.1007/s00586-014-3542-1. [DOI] [PubMed] [Google Scholar]
- 21.Terran J., Schwab F., Shaffrey C.I., Smith J.S., Devos P., Ames C.P. The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery. 2013;73(4):559–568. doi: 10.1227/NEU.0000000000000012. [DOI] [PubMed] [Google Scholar]
- 22.Silva F.E., Lenke L.G. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus. 2010;28(3):E1. doi: 10.3171/2010.1.FOCUS09271. [DOI] [PubMed] [Google Scholar]
- 23.Bridwell K.H. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 2006;31(19 Suppl):S171–S178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 24.Auerbach J.D., Lenke L.G., Bridwell K.H., Sehn J.K., Milby A.H., Bumpass D. Major complications and comparison between 3-Column Osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 2012;37(14):1198–1210. doi: 10.1097/BRS.0b013e31824fffde. [DOI] [PubMed] [Google Scholar]
- 25.Boachie-Adjei O., Ferguson J.A., Pigeon R.G., Peskin M.R. Transpedicular lumbar wedge resection osteotomy for fixed sagittal imbalance: surgical technique and early results. Spine (Phila Pa 1976) 2006;31(4):485–492. doi: 10.1097/01.brs.0000199893.71141.59. [DOI] [PubMed] [Google Scholar]
- 26.Smith J.S., Gupta M.C., Klineberg E.O., Shaffrey C.I., Schwab F.J., Lafage V. Scoliosis Research Society (SRS) Annual Meeting; Prague, Czech Republic: 2016. Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with minimum 2-yr follow-up. [DOI] [PubMed] [Google Scholar]
- 27.Lenke L.G., Fehlings M.G., Shaffrey C.I., Cheung K.M., Carreon L., Dekutoski M.B. Neurologic outcomes of complex adult spinal deformity surgery results of the prospective, multicenter Scoli-RISK-1 study. Spine (Phila Pa 1976) 2016;41(3):204–212. doi: 10.1097/BRS.0000000000001338. [DOI] [PubMed] [Google Scholar]
- 28.Hyun S.J., Lenke L.G., Kim Y.C., Koester L.A., Blanke K.M. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976) 2014;39(22):1899–1904. doi: 10.1097/BRS.0000000000000556. [DOI] [PubMed] [Google Scholar]
- 29.Gupta M.C., Henry J.K., Lafage V., Schwab F.J., Ames C.P., Klineberg E.O. Scoliosis Research Society (SRS) Annual Meeting; Minneapolis, USA: 2015. Reducing rod breakage and nonunion in pedicle subtraction osteotomy: the importance of rod number and configuration in 264 patients with 2-year follow up. [Google Scholar]
- 30.Smith J.S., Lafage V., Shaffrey C.I., Schwab F., Lafage R., Hostin R. Outcomes of operative and nonoperative treatment for adult spinal deformity: a prospective, multicenter, propensity-matched cohort assessment with minimum 2-year follow-up. Neurosurgery. 2016;78(6):851–861. doi: 10.1227/NEU.0000000000001116. [DOI] [PubMed] [Google Scholar]