Abstract
Aims and objectives
To determine the effects of nursing interventions for people's nutrition, elimination, mobility and hygiene needs.
Background
Patient experience of health care is sensitive to nursing quality. A refocus on fundamental nursing care is undermined by lack of evidence of effectiveness for interventions in core areas such as elimination, nutrition, mobility and hygiene.
Design
Systematic review.
Methods
We searched for and included experimental studies on interventions by professionally qualified and unregistered nurses that addressed participants' nutrition, elimination, mobility and hygiene needs. We extracted data on scope, quality and results of studies followed by descriptive narrative synthesis of included study outcomes using a novel form of harvest plots.
Results
We included 149 studies, 35 nutrition, 56 elimination, 16 mobility, 39 hygiene and three addressing two or more areas simultaneously (67 randomised controlled trials, 32 non‐randomised controlled trials and 50 uncontrolled trials). Studies into interventions on participant self‐management of nutrition (n = 25), oral health (n = 26), catheter care (n = 23) and self‐management of elimination (n = 21) were the most prevalent. Most studies focussed their outcomes on observational or physiological measures, with very few collecting patient‐reported outcomes, such as quality of life, experience or self‐reported symptoms. All but 13 studies were of low quality and at significant risk of bias. The majority of studies did not define primary outcomes, included multiple measures of identical concepts, used inappropriate analyses and did not conform to standard reporting quality criteria.
Conclusions
The current evidence for fundamental nursing care interventions is sparse, of poor quality and unfit to provide evidence‐based guidance to practising nurses.
Relevance to clinical practice
Researchers in nursing internationally should now undertake a programme of work to produce evidence for clinical practice in the fundamentals of care that is reliable, replicable and robust.
Keywords: fundamental care, experimental design, nursing, systematic review
1. BACKGROUND
When nursing care is sub‐optimal, patients experience health care negatively (Rathert, Wyrwich, & Boren, 2013; Suhonen, Leino‐Kilpi, & Valimaki, 2005). Failure to assure the quality of nursing care leads not only to distress and dissatisfaction, but also to wider patient safety failures. Studies internationally (Bureau of Health Information, 2014, Garling, 2008; Kalisch, 2006) have highlighted the prevalence and potentially catastrophic consequences of poor nursing care (Department of Health, 2012, 2013). Missed or incomplete nursing care has been identified as a key mechanism explaining the widely demonstrated association between nurse staffing levels and patient outcomes including mortality (Aiken et al., 2014; Ball, Murrells, Rafferty, Morrow, & Griffiths, 2014). Optimising the quality of care is essential in healthcare settings internationally, particularly for older people, which for the example of the United Kingdom includes care for more than half a million people over 65 per annum, and costs more than £12 billion (Care Quality Commission, 2014).
Arising from such concerns, a number of initiatives have sought to refocus nursing on central tenets of practice including “compassion” (Commissioning Board Chief Nursing Officer and DH Chief Nursing Adviser, 2012) and “fundamental nursing care” (Kitson, Robertson‐Malt, & Conroy, 2013), in the latter case accompanied by an international campaign to identify and emphasise the components of essential (or fundamental) nursing care (Kitson, Conroy, Wengstrom, Profetto‐McGrath, & Robertson‐Malt, 2010)—defined as action to address safety, comfort, communication, dignity, respiration, privacy, eating and drinking, respecting choice, elimination, mobility, personal cleansing and dressing, expressing sexuality, temperature control, rest and sleep (Kitson, Conroy, Kuluski, Locock, & Lyons, 2013). Unfortunately, this drive to refocus nursing on its core values and functions has exposed the paucity of systematic evidence to guide practising nurses.
In an evidence‐based healthcare environment, improving nursing care requires action to produce robust evidence that ensures nurses do more good than harm to those in their care. Much recent work (Richards, Coulthard, & Borglin, 2014) has confirmed the findings of previous reviews that the nursing research literature remains descriptive (Mantzoukas, 2009), largely irrelevant to practising nurses (Hallberg, 2009) and a prime candidate for the term “research waste” (Chalmers & Glasziou, 2009; Richards et al., 2014). In this situation, it is difficult for practising nurses to follow clear evidence‐based guidelines. Therefore, we conducted a review of four of the elements of fundamental nursing care rated as most important in a previous international consensus study (Kitson, Conroy, et al., 2013). Although our overall programme of research has also reviewed nonexperimental descriptive and qualitative studies, in this report, we outline the findings from our review of experimental interventions only, using the PRISMA guidelines for reporting reviews of effectiveness.
2. REVIEW QUESTION
What is the effectiveness of nursing interventions that address the nutrition, elimination, mobility and hygiene needs of people in hospital and residents in care homes as investigated in experimental studies?
3. METHODS
3.1. Eligibility criteria
We included experimental studies on any intervention undertaken by either professionally qualified and/or unregistered nurses for people in hospital or resident in care/nursing homes that aimed to address and measure the impact on participants' nutrition, elimination, mobility and hygiene needs. We defined interventions related to nutrition as those assisting or supporting people in consuming adequate food and fluids to achieve optimum nutritional and hydration status; elimination to address people's toileting needs, and assist them to eliminate urine and faeces conventionally or by catheterisation; mobility including assistance or support for people to move to meet their own care needs and to remain independent; hygiene including assisting or supporting patients to maintain bodily cleanliness and to dress themselves independently.
We included reports of randomised controlled trials (RCTs), nonrandomised controlled trials (nRCTs) and uncontrolled experimental trials (UCTs) such as before‐after trials. We excluded reports that solely investigated medical devices (such as catheter type, washing products, incontinence devices, food supplements and mobility aids), and observational studies where there was no experimental manipulation of an intervention. We included studies in English.
3.2. Information sources
We undertook searches during a period of time from May 2015–March 2016. We searched all relevant databases including embase, medline, cinahl, psychlit, psychinfo, science citation, bids and cancerlit, in process and other nonindexed citations, COCHRANE reviews databases using the OVID® platform, and individual database searches. We contacted the authors of studies where we were unable to access the full report through online databases and journals.
3.3. Search
We undertook four unique searches, one for each fundamental care area, using MeSH and free‐text terms and adapted to each of the specific databases searched. Our search strategy was designed to be extremely sensitive and was part of a larger programme of work that also searched for nonexperimental designs. We had searched identified reviews for all citations identified in them and identified additional citations through conference attendance and networks. Appendix S1 details a specimen search strategy for nutrition. Other searches are available from the authors.
3.4. Study selection
We downloaded all results to a citation management system and removed duplicates of retrieved reports. Two of our team of reviewers independently screened titles and abstracts for inclusion, merged their decisions and resolved disagreements through discussion. We retrieved full texts of potentially relevant articles and two reviewers independently assessed each one for inclusion, again resolving discrepancies by discussion or involvement of a third reviewer as necessary.
3.5. Data collection
We extracted data from included studies to a bespoke data extraction sheet adapted from our previous reviews (Richards et al., 2014).
3.6. Data items
One reviewer extracted data on lead author, year of publication, study origin country, participant demographic characteristics, essential nursing care category/ies addressed, interventions, comparisons, outcome measures, and study design, and categorised study design using a priori definitions of study types. A second reviewer checked 20% of the extracted data at random, discussed discrepancies and advised where further checking was required.
3.7. Risk of bias and study quality
We assessed the risk of bias for each study as a combination of study design and internal quality criteria. We regarded nRCTs and UCTs as inherently more prone to bias than RCTs, but also assessed the internal quality characteristics of each individual study, independent of design. Using the Cochrane Collaboration's Tool for Assessing Risk of Bias, we assessed each study report against criteria for bias (random sequence generation, allocation concealment, participant & staff blinding, outcome assessment blinding, incomplete outcome data, selective reporting) (The Cochrane Collaboration, 2011). Following this procedure, we judged the quality of studies as high when studies met more criteria for low risk of bias than for high risk or unclear, assuming that unclear risk of bias represented poor study reporting according to established standards. Where criteria were evenly balanced, we applied judgements as to the relative importance of criteria, guided by the Cochrane procedure. We rated the remaining studies as of low quality.
3.8. Summary measures
We extracted all recorded outcomes in each study report. We adapted typologies from Valderas and Alonso (2008), Wilson and Cleary (1995) and the World Health Organisation (2016) to categorise outcomes as (i) ratings of objective biological/physiological variables (e.g., blood pressure); (ii) observational measures of performance or behaviour (e.g., walking distance); (iii) patient‐reported outcomes (PROs) of phenomena such as symptoms, functional ability, health perception, quality of life and other health‐related constructs; (iv) nurse variables (e.g., nursing knowledge).
3.9. Synthesis of results and risk of bias across studies
Given the heterogeneity of interventions and outcomes reported, we undertook a descriptive narrative synthesis of results. We examined each report individually and categorised interventions into conceptual areas using consensus discussions within the team. We constructed “harvest plots” (Ogilvie et al., 2008) to map the interventions, research designs, study quality and reported outcomes for each essential nursing care area to delineate the scope and strength of the evidence for each intervention and care area. Mapping study quality allowed us to examine the risk of bias across all studies. We report in more detail interventions with the most high‐quality evidence of effect.
4. RESULTS
4.1. Study selection
We identified 21,608 potential studies (4,462 nutrition, 4,944 elimination, 6,086 mobility and 6,116 hygiene). We excluded 16,486 studies after title and abstract review. We identified 572 full text reports (114 nutrition, 218 elimination, 83 mobility and 157 hygiene), excluded 423 reports (78 nutrition, 161 elimination, 66 mobility and 118 hygiene) and included 149 reports (35 nutrition, 56 elimination, 16 mobility, 39 hygiene and three studies that addressed two or more fundamental care areas) (Figure 1).
Figure 1.
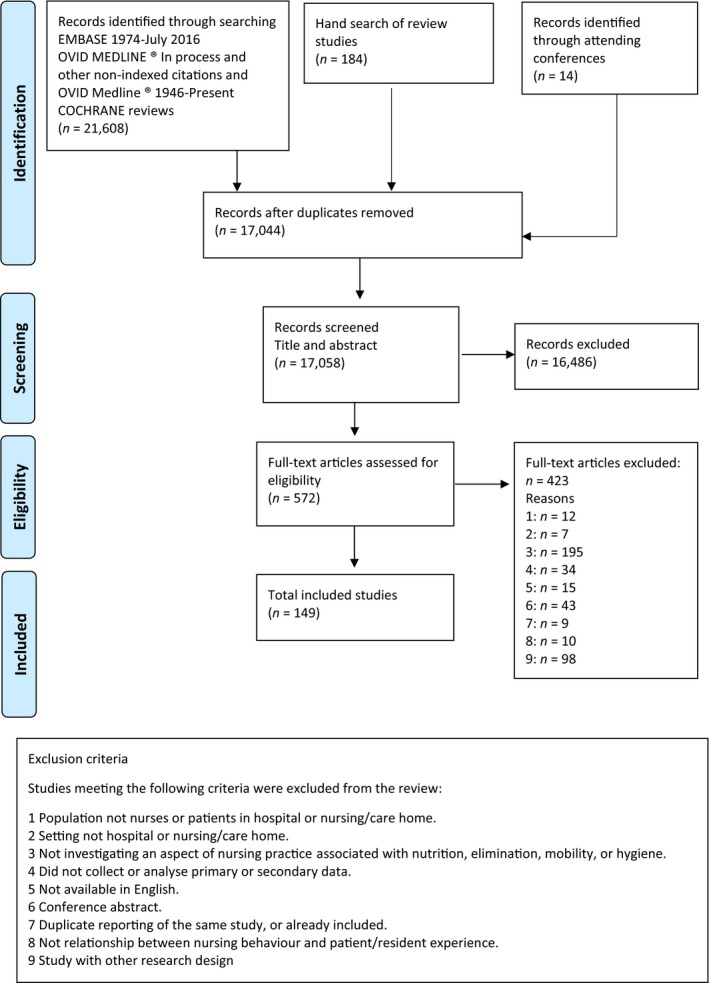
PRISMA diagram [Colour figure can be viewed at http://wileyonlinelibrary.com]
4.2. Study characteristics
Tables S1–S5 display the characteristics of each included study, Table S6 displays risk of bias and outcomes reported.
4.3. Synthesis of results and risk of bias across studies
4.3.1. Nutrition
The 35 experimental studies of interventions to aid patients' nutrition (Table S1) included 3,241 patient participants, aged from 46–101, with a range of healthcare conditions such as neurological including dementia(s) or severe cognitive impairment (12 studies, 9% of the participants, 280 of 3,241), oral and gastrointestinal including dysphagia (two studies, 4% of the participants, 127 of 3,241), stroke (one study, 12% of the participants, 400 of 3,241), musculoskeletal including hip fracture, hip or knee replacement (one study, 8%, 253 of 3,241) or renal and urogenital (one study, 2% of the participants, 63 of 3,241). The health conditions of 65% (18 studies, 2,118 of 3,241) of the patients/residents remained unspecified. Eleven trials were undertaken in hospitals, and 24 in nursing/care/residential homes. Twenty‐four of the trials were conducted in multiple sites.
We categorised interventions into three types: (i) nursing interventions using nutritional support compounds; (ii) strategies to promote patient self‐care of nutrition and hydration; (iii) patient feeding protocols. We identified 12 RCTs (three of nutritional support, seven for self‐care and two of feeding), 10 nRCTs (two nutritional support and eight self‐care) and 13 UCTs (one nutritional support, two feeding protocols and 10 self‐care). Methodologically, one of the 12 RCTs was of high quality, and the remaining 11 were low quality. All of the 10 nRCTs were low quality, and all but one of the 13 UCTs were low quality (Table S6).
We found a wide range of outcomes reported, with multiple outcomes per trial and few trials identifying a clear primary outcome. Thirty‐two trials reported observational outcomes, 12 physiological/biological, eight nursing and only three PROs. Many trials reported an equivocal mix of outcomes. Findings in favour of the intervention were more prevalent in nRCTs, inherently more prone to bias, and in poor‐quality trials, or often offset by findings of no difference on other measures in the same trial. The harvest plot for nutrition (Figure 2) displays the numbers of trials reporting outcomes in favour of the intervention (shown as +ve numbers on the x‐axis) or outcomes in favour of the control/comparison or with no between‐group or pre–post differences (−ve numbers) for all trials of nutrition interventions, charted by intervention, research method and methodological quality.
Figure 2.
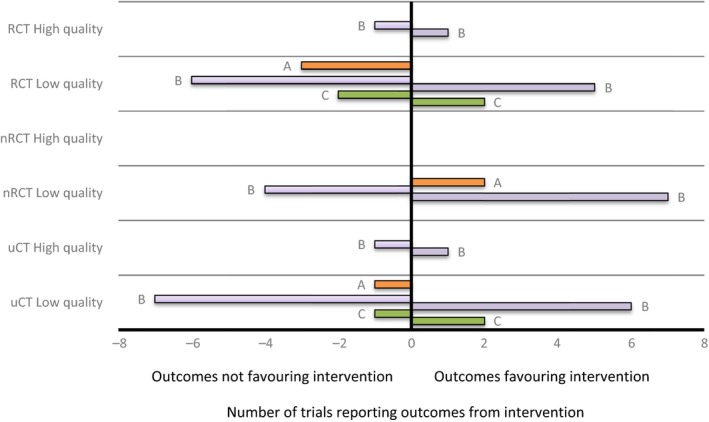
Harvest plot displaying outcomes of trials of nutrition interventions. (a) nutritional support (N = 6); (b) self‐care (N = 25); (c) feeding protocols (N = 4). Positive values are the numbers of trials reporting outcomes in favour of the intervention, negative values indicate outcomes in favour of the control or reporting no between group or pre–postdifferences [Colour figure can be viewed at http://wileyonlinelibrary.com]
The only high‐quality RCT in this area (Hickson et al., 2004), which tested the introduction of supernumerary nonregistered healthcare assistants onto ward environments to support staff and patients with nutritional intake, found an effect in favour of the intervention in reducing IV antibiotics and fluids but no difference in a large range of other measures including weight, length of hospital stay, grip strength and BMI. The UCT trial (Ragneskog, Kihlgren, Karlsson, & Norberg, 1996) rated as of high quality in terms of its conduct (albeit in a design inherently prone to bias) tested the use of music during dining times and found both positive and negative effects on self‐feeding behaviours.
4.3.2. Elimination
The 56 experimental studies of interventions to aid patients' elimination needs (Table S2) included 7,361 patient participants, aged from 18–100, with a range of healthcare problems including those postsurgery 55% (23 studies, 4,061/7,361) such as transurethral resection of the prostate, hysterectomy, hip replacement, vaginal repair and bowel resection. About 40% (29 studies, 2,934 of 7,361) of the study participants experienced incontinence, 31% (nine studies, 2,292 of 7,361) had indwelling catheters and 34% (nine studies, 2,474 of 7,361) had urinary retention.
The health conditions of participants included renal and urogenital problems (39 studies, 59% of the participants, 4,320 of 7,361), musculoskeletal (two studies, 4% of the participants, 271 of 7,361), stroke (three studies, 2% of the participants, 143 of 7,361), cancer (one study, 1% of the participants, 110 of 7,361), reproductive health and childbirth (one study, 3% of the participants, 250 of 7,361) and problems with mental health and congenital or neurological disorders (one study, 2% of the participants, 151 of 7,361). The health conditions of 29% (eight studies, 2,101 of 7,361) of the patients/residents were unspecified. 28 trials were undertaken in hospitals, 28 in nursing/care/residential homes. 20 of the trials were conducted in multiple sites.
We categorised interventions into four types: (i) interventions for promoting independent self‐care of elimination; (ii) bladder training; (iii) catheter care; (iv) multi‐component management including elements of the previous three categories. We identified 32 RCTs (eight promoting self‐care, three bladder training and 21 catheter care), 10 nRCTs (six self‐care, two catheter care and two multi‐component management) and 14 UCTs (seven self‐care and eight multi‐component management). Methodologically, six RCTs were of high quality and 26 of low quality. All of the nRCTs and UCTs were of low quality (Table S6).
As in other fundamental care areas, a wide range of outcomes was reported, with multiple outcomes per trial and few trials identifying a clear primary outcome. Fifty‐four trials reported observational outcomes, 29 physiological/biological, three nursing outcomes and 10 PROs. Most trials were of poor quality and many reported an equivocal mix of outcomes distributed between those in favour of the intervention and those showing no difference. The harvest plot for elimination (Figure 3) displays outcomes using the same conventions as Figure 2.
Figure 3.
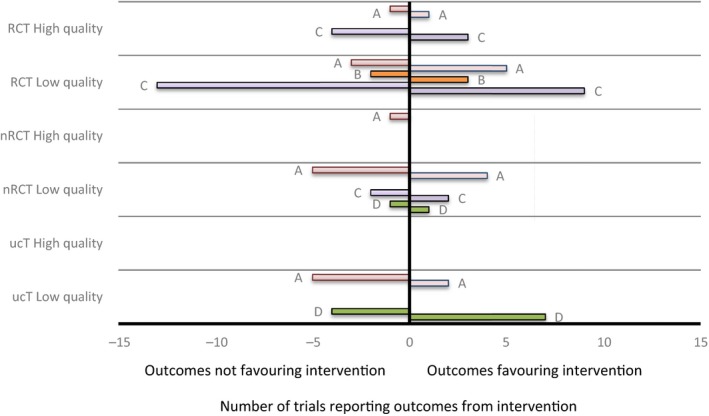
Harvest plot displaying outcomes of trials of elimination interventions. (a) self‐care (n = 20); (b) bladder training (N = 3); (c) catheter care (N = 23); (d) multi‐component management (N = 10). Positive values are the numbers of trials reporting outcomes in favour of the intervention, negative values indicate trials reporting outcomes in favour of the control or reporting no between group or pre–postdifferences [Colour figure can be viewed at http://wileyonlinelibrary.com]
Of the six high‐quality RCTs, one focussed on self‐care and five on catheter care. As can be seen from Figure 3, results were very mixed. The one self‐care trial (Hansen & Olsen, 2015) found that compared to using bedpans and urine bottles, postoperative ambulant toileting in the recovery room reduced the frequency of catheterisation but had a mixed effect on variables such as mobilisation, pain relief and nausea. The catheter care studies included three investigating immediate or early postoperative vs. delayed catheter removal (Alessandri, Mistrangelo, Lijoi, Ferrero, & Ragni, 2006; Dunn, Shlay, & Forshner, 2003; Kamilya, Seal, Mukherji, Bhattacharyya, & Hazra, 2010). Results were conflicting, with two demonstrating no between‐group differences in infection rates but one positive for early removal. Other positive effects included less pain and reduced hospital stays in the immediate groups, but increased frequency of urinary retention. In a further study (Webster et al., 2006), evening removal of catheters had no effect on hospital length of stay. Finally, a study on three different catheter washout regimes (Moore et al., 2009) found no advantages of saline, acidic washouts vs. no washouts in terms of re‐catheterisation or infection rates.
4.3.3. Mobility
The 16 experimental studies of interventions to aid patients' mobility needs (Table S3) included 49,917 patient participants, aged from 17–103, with largely unspecified medical diagnoses (six studies, 97% of the participants, 48,410 of 49,917), and to a much lesser degree with neurological (seven studies, 3% of the participants, 1,332 of 49,917), cardiovascular (one study, 0.2% of the participants, 86 of 49,917), renal and urogenital (one study, 0.1% of the participants, 65 of 49,917), and blood (one study, 0.05% of the participants, 24 of 49,917) conditions. Ten trials were undertaken in hospitals, six in nursing/care homes. Eight of the trials were conducted in multiple sites.
We categorised interventions into three types: (i) exercise interventions; (ii) promoting independent mobility; (iii) risk reduction. We identified five RCTs (two exercise interventions, one independent mobility and two for risk reduction), four nRCTs (two exercise interventions and two independent mobility) and seven UCTs (one exercise intervention, five promoting mobility and one risk reduction). Methodologically, one RCT was of high quality and four of low quality. All of the nRCTs and UCTs were of low quality (Table S6).
Similar to other areas, multiple outcomes per trial were reported and few trials identified a clear primary outcome. Fifteen trials reported observational outcomes, six physiological/biological, three nursing outcomes and two PROs. Most trials were of poor quality and many reported an equivocal mix of outcomes distributed between those in favour of the intervention and those showing no difference. Findings in favour of the intervention were more prevalent in poor‐quality trial designs and often offset by findings of no difference in the same trial or other trials of the intervention type. The harvest plot for mobility (Figure 4) displays outcomes using the same conventions as other Figures.
Figure 4.
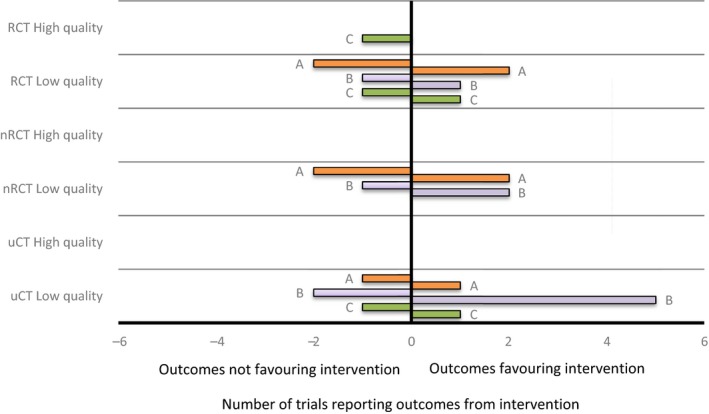
Harvest plot displaying outcomes of trials of mobility interventions. (a) exercise (N = 5); (b) independent mobility (N = 8); (c) risk reduction (N = 3). Positive values are the numbers of trials reporting outcomes in favour of the intervention, negative values indicate trials reporting outcomes in favour of the control or reporting no between group or pre–postdifferences [Colour figure can be viewed at http://wileyonlinelibrary.com]
The one high‐quality RCT (Barker et al., 2016) in this area, which tested a complex intervention of a fall risk tool, combined with an individualised falls prevention programme (6‐PACK), found no effect of the intervention on fall rates and injuries.
4.3.4. Hygiene
The 39 experimental studies of interventions to aid patients' hygiene needs (Table S4) included 7,625 patient participants, aged from 18–105, with healthcare conditions including neurological (12 studies, 34% of the participants, 2,615 of 7,625), oral and gastrointestinal (three studies, 3% of the participants, 248 of 7,625), respiratory (three studies, 14% of the participants, 1,033 of 7,625, two studies did not specify participant numbers), renal and urogenital (two studies, 2% of the participants, 176 of 7,625), mental health (two studies, 1% of the participants, 91 of 7,625) and cardiovascular (one study, 1% of the participants, 71 of 7,625). The population of one study had a combination of neurological, stroke and unspecified health conditions (2% of the participants, 131 of 7,625). The health conditions of 43% (14 studies, 3,260 of 7,625) of the patients/residents were unspecified. The participants were admitted to hospital (11 trials) and residential care (28 trials) facilities. Seventeen of the trials were conducted in multiple sites.
We categorised interventions into three types: (i) the promotion of self‐care of hygiene and dressing; (ii) washing/cleaning patients; (iii) oral health. We identified 15 RCTs (one self‐care, three washing/cleaning and 11 for oral health), eight nRCTs (one self‐care, one washing/cleaning and six oral health) and 16 UCTs (one self‐care, six washing/cleaning and nine oral health). Methodologically, two RCTs and one UCT were of high quality, the remaining trials all of low quality (Table S6).
Multiple outcomes per trial were reported and few trials identified a clear primary outcome. Twenty‐nine trials reported physiological/biological outcomes, 15 observational, eight nursing outcomes and four PROs. All but three trials were of poor quality and many reported an equivocal mix of outcomes distributed between those in favour of the intervention and those showing no difference. Findings in favour of the intervention were more prevalent in trials more prone to bias. The harvest plot for hygiene (Figure 5) displays outcomes using the same conventions as other similar Figures.
Figure 5.
Harvest plot displaying outcomes of trials of hygiene interventions. (a) self‐care assistance (N = 3); (b) washing/cleaning (N = 11); (c) oral care (N = 25). Positive values are the numbers of trials reporting outcomes in favour of the intervention, negative values indicate trials reporting outcomes in favour of the control or reporting no between group or pre–postdifferences [Colour figure can be viewed at http://wileyonlinelibrary.com]
The two high‐quality RCTs in this area (Juthani‐Mehta et al., 2015; Prendergast, Jakobsson, Renvert, & Hallberg, 2012), which tested comprehensive oral care protocols found no effects in favour of the interventions on pneumonia, lower respiratory tract infections or oral health. The UCT trial (Cuccio et al., 2012) rated as of high quality in terms of its conduct (but likewise a design inherently prone to bias) tested an oral care protocol including chlorhexidine rinses and found effects in favour of the intervention on ventilator‐associated pneumonia rates.
4.3.5. Studies addressing two or more fundamental care areas
The three experimental studies about interventions addressing two or more fundamental care areas (Table S5) included 353 participants in two of these studies, mean ages between 87–89. Participants in these two studies had renal and urogenital medical diagnoses. One study of an organisational quality improvement strategy did not report the number, ages or diagnoses of patient participants. All three trials were undertaken in multiple nursing/care home sites.
All three studies were RCTs testing interventions for self‐care (Figure 6). Methodologically, one RCT was of high quality, the other two of low quality (Table S6). Two trials reported observational outcomes, one physiological/biological outcomes, two nursing outcomes and one reported PROs. Similar to other areas, multiple outcomes per trial were reported.
Figure 6.

Harvest plot displaying outcomes of trials of interventions (self‐care) addressing two or more fundamental care areas (N = 3). Positive values are the numbers of trials reporting outcomes in favour of the intervention, negative values indicate trials reporting outcomes in favour of the control or reporting no between group or pre–postdifferences [Colour figure can be viewed at http://wileyonlinelibrary.com]
The high‐quality RCT in this area (Schnelle et al., 2002), a combination of exercise and scheduled toileting, found effects in favour of the intervention for mobility and incontinence frequency.
5. DISCUSSION
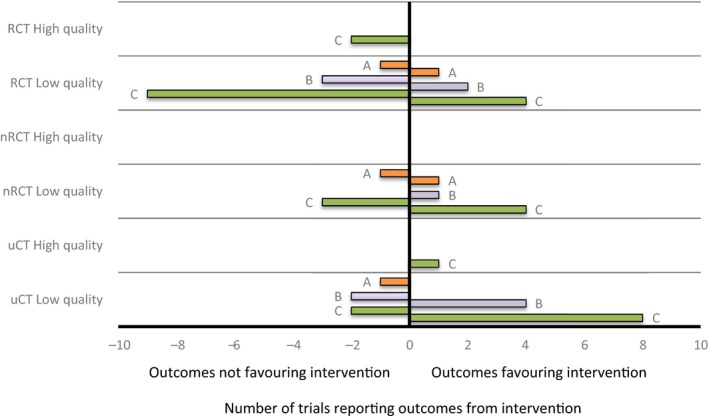
In this systematic review, we identified 149 experimental trials of interventions by nurses to address people's nutrition, elimination, mobility and hygiene needs; 67 RCTs, 32 nRCTs and 50 uCTs. All but 13 trials (8.7%) were of low quality and at risk of bias from their basic methodological design or from their conduct. Studies into interventions to assist in patient self‐management of nutrition (n = 25), oral health (n = 26), catheter care (n = 23) and interventions to help patient self‐manage their elimination needs (n = 21) were the most prevalent. Studies into nursing interventions to assist patients with mobility (n = 16) were the least frequently reported, although there were also surprisingly few studies on interventions to assist patients with self‐care of their hygiene needs (n = 3) and feeding protocols (n = 4), core fundamental nursing care activities.
Most studies focussed their outcomes on a mix of observational and physiological measures with very few studies using outcomes collected directly from patients themselves, such as quality of life, experience or self‐reported symptoms. Further, studies collected multiple measures and rarely prespecified the primary outcome of interest. We observed frequent attempts to overestimate the outcomes of studies. For example, the authors of many RCTs and nRCTs claimed positive effects for experimental interventions by reporting within group rather than between‐group outcomes. Few attempts were made to control for other potentially confounding variables affecting outcomes, and multiple testing was the norm in these studies.
Although we found papers reporting findings in favour of many fundamental care interventions, these were generally from low‐quality RCTs at high risk of bias or from equally low quality, less rigorous nRCT or UCT studies and were usually offset by results from the same trials or from others that demonstrated no effects in favour of the experimental interventions. The 13 high‐quality trials investigated interventions for improving self‐care of nutrition (n = 2), catheter care (n = 5), self‐care of elimination (n = 1), risk reduction in mobility (n = 1), oral health (n = 3) and interventions addressing two or more fundamental care areas (n = 1). Few of these trials provide information on routine care practices that could be implemented by nurses. For nutrition, the trials of supernumerary workers and music provide little information to guide nurses giving fundamental care. In terms of elimination, all but one trial were on variations of catheter care, mainly removal regimes, and had equivocal results, whilst the self‐care trial was only applicable to the specific postoperative recovery room context. In mobility and hygiene, the falls prevention and oral health RCTs did not demonstrate any reliable intervention effects. The only high‐quality study to show real promise tested a multi‐component intervention and found effects in favour of the intervention on mobility and incontinence frequency.
The sparsity of robust results for the effectiveness of nursing interventions for fundamental care is sobering indeed. Our mapping of these results using harvest plots dramatically illustrates the methodological status and the sources of the evidence upon which nurses must draw when planning the fundamental care of their patients. We can only surmise that in the absence of clear evidence, nurses must conduct their duties using a combination of guesswork, folk knowledge and tradition or else utilise evidence from studies that are at substantial risk of bias. This situation is not tenable for a profession positioning itself at the heart of modern healthcare provision.
5.1. Limitations
We restricted our searches to studies examining interventions that were undertaken by nurses. Given that health care is a multi‐professional endeavour, there may be studies from other clinical disciplines investigating fundamental care behaviours that could be used by nurses. We also restricted our search to studies published in English so that it is possible that additional studies are present in professional journals written in other languages. However, it is generally the case that English is the primary language of science and we did indeed identify and include studies from a range of countries outside the native English speaking world. We found it very difficult to identify primary outcome variables in many studies and, therefore, synthesised all outcomes as of equivalent importance. This might mean that we have not represented the most significant variables accurately, although our strategy was to err on the side of caution given that many of the studies demonstrating effects in favour of experimental interventions did so only by collecting many multiple outcomes. As in all reviews, it is possible that we might not have found all relevant studies, however, we feel secure that any missed studies would not alter the overall pattern of results substantially, given the large number of studies we did include.
6. CONCLUSIONS
As surmised by the editorial call for papers for this special edition of the Journal of Clinical Nursing, the evidence base for fundamental nursing care is characterised by studies at high risk of bias producing negative or at best equivocal findings. Not one nursing intervention stands out as a clear evidence‐based solution to the many calls to improve the quality of essential nursing care and enhance the experience of our patients. It cannot be beyond the wit of the current generation of researchers in nursing to construct and undertake high‐quality trials using modern health services research methods such as those espoused by amongst others the UK Medical Research Council (Craig et al., 2008; Richards & Rahm‐Hallberg, 2015) and reported using transparent criteria. We call on all researchers in nursing internationally to undertake a programme of work, collaboratively if possible, to produce evidence that is reliable, replicable and robust, evidence that is sorely needed indeed.
CONTRIBUTIONS
Study design: DAR, CP; data collection and analysis: DAR, AH, CP, VAG, JF; and manuscript preparation: DAR, AH, CP, VAG, JF.
Supporting information
ACKNOWLEDGEMENTS
This study was funded by a Programme Development Grant from the UK National Institute of Health Research (NIHR). RP‐DG‐1214‐10001. David Richards and Victoria Goodwin receive funding support from the UK National Institute for Health Research South West Peninsula Collaboration for Leadership in Applied Health Research and Care.
Richards DA, Hilli A, Pentecost C, Goodwin VA, Frost J. Fundamental nursing care: A systematic review of the evidence on the effect of nursing care interventions for nutrition, elimination, mobility and hygiene. J Clin Nurs. 2018;27:2179–2188. https://doi.org/10.1111/jocn.14150
REFERENCES
- Aiken, L. H. , Sloane, D. M. , Bruyneel, L. , Van den Heede, K. , Griffiths, P. , Busse, R. , … Sermeus, W. (2014). Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. The Lancet, 383, 1824–1830. https://doi.org/10.1016/S0140-6736(13)62631-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alessandri, F. , Mistrangelo, E. , Lijoi, D. , Ferrero, S. , & Ragni, N. (2006). A prospective, randomized trial comparing immediate versus delayed catheter removal following hysterectomy. Acta Obstetricia Et Gynecologica Scandinavica, 85, 716–720. https://doi.org/10.1080/00016340600606976 [DOI] [PubMed] [Google Scholar]
- Ball, J. E. , Murrells, T. , Rafferty, A. M. , Morrow, E. , & Griffiths, P. (2014). ‘Care left undone’ during nursing shifts: Associations with workload and perceived quality of care. BMJ Quality & Safety, 23, 116–125. https://doi.org/10.1136/bmjqs-2012-001767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker, A. L. , Morello, R. T. , Wolfe, R. , Brand, C. A. , Haines, T. P. , Hill, K. D. , … Kamar, J. (2016). 6‐PACK programme to decrease fall injuries in acute hospitals: Cluster randomised controlled trial. BMJ, 352, h6781 https://doi.org/10.1136/bmj.h6781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Health Information (2014). Adult admitted patient survey 2013 results. Snapshot report NSW patient survey program. Sydney, NSW: Bureau of Health Information. [Google Scholar]
- Care Quality Commission (2014). The state of health care and adult social care in England 2013/2014. London, UK: Care Quality Commission. [Google Scholar]
- Chalmers, I. , & Glasziou, P. (2009). Avoidable waste in the production and reporting of research evidence. The Lancet, 374, 86–89. https://doi.org/10.1016/S0140-6736(09)60329-9 [DOI] [PubMed] [Google Scholar]
- Commissioning Board Chief Nursing Officer and DH Chief Nursing Adviser (2012). Compassion in practice. Leeds, UK: Department of Health. [Google Scholar]
- Craig, P. , Dieppe, P. , MacIntyre, S. , Michie, S. , Nazareth, I. , & Petticrew, M. (2008). Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ, 337, a1655 https://doi.org/10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuccio, L. , Cerullo, E. , Paradis, H. , Padula, C. , Rivet, C. , Steeves, S. , & Lynch, J. (2012). An evidence‐based oral care protocol to decrease ventilator‐associated pneumonia. Dimensions of Critical Care Nursing, 31, 301–308. https://doi.org/10.1097/DCC.0b013e3182619b6f [DOI] [PubMed] [Google Scholar]
- Department of Health (2012). Transforming care: A national response to Winterbourne View Hospital: Department of Health Review Final Report. London, UK: Department of Health. [Google Scholar]
- Department of Health (2013). Report of the Mid Staffordshire NHS Foundation Trust public enquiry. London, UK: Department of Health. [Google Scholar]
- Dunn, T. S. , Shlay, J. , & Forshner, D. (2003). Are in‐dwelling catheters necessary for 24 hours after hysterectomy? American Journal of Obstetrics and Gynecology, 189, 435–437. https://doi.org/10.1067/S0002-9378(03)00496-4 [DOI] [PubMed] [Google Scholar]
- Garling, P. (2008). Final report of the special commission of inquiry acute care services in NSW public hospitals. Sydney, NSW: NSW Department of Premier and Cabinet. [Google Scholar]
- Hallberg, I. R. (2009). Moving nursing research forward towards a stronger impact on health care practice? International Journal of Nursing Studies, 46, 407–412. https://doi.org/10.1016/j.ijnurstu.2009.02.005 [DOI] [PubMed] [Google Scholar]
- Hansen, A. B. , & Olsen, K. S. (2015). The number of in‐out catheterisations is reduced by mobilising the postoperative patient with bladder needs to the toilet in the recovery room A randomised clinical trial. European Journal of Anaesthesiology, 32, 486–492. https://doi.org/10.1097/EJA.0000000000000214 [DOI] [PubMed] [Google Scholar]
- Hickson, M. , Bulpitt, C. , Nunes, M. , Peters, R. , Cooke, J. , Nicholl, C. , & Frost, G. (2004). Does additional feeding support provided by health care assistants improve nutritional status and outcome in acutely ill older in‐patients? – A randomised control trial. Clinical Nutrition, 23, 69–77. https://doi.org/10.1016/S0261-5614(03)00090-6 [DOI] [PubMed] [Google Scholar]
- Juthani‐Mehta, M. , Van Ness, P. H. , McGloin, J. , Argraves, S. , Chen, S. , Charpentier, P. , … Quagliarello, V. J. (2015). A cluster‐randomized controlled trial of a multicomponent intervention protocol for pneumonia prevention among nursing home elders. Clinical Infectious Diseases, 60, 849–857. https://doi.org/10.1093/cid/ciu935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalisch, B. J. (2006). Missed nursing care: A qualitative study. Journal of Nursing Care Quality, 21, 306–313. https://doi.org/10.1097/00001786-200610000-00006 [DOI] [PubMed] [Google Scholar]
- Kamilya, G. , Seal, S. L. , Mukherji, J. , Bhattacharyya, S. K. , & Hazra, A. (2010). A randomized controlled trial comparing short versus long‐term catheterization after uncomplicated vaginal prolapse surgery. Journal of Obstetrics and Gynaecology Research, 36, 154–158. https://doi.org/10.1111/j.1447-0756.2009.01096.x [DOI] [PubMed] [Google Scholar]
- Kitson, A. , Conroy, T. , Kuluski, K. , Locock, L. , & Lyons, R. (2013). Reclaiming and redefining the Fundamentals of Care: Nursing's response to meeting patients' basic human needs. Adelaide, SA: The University of Adelaide. [Google Scholar]
- Kitson, A. , Conroy, T. , Wengstrom, Y. , Profetto‐McGrath, J. , & Robertson‐Malt, S. (2010). Defining the fundamentals of care. International Journal of Nursing Practice, 16, 423–434. https://doi.org/10.1111/j.1440-172X.2010.01861.x [DOI] [PubMed] [Google Scholar]
- Kitson, A. , Robertson‐Malt, S. , & Conroy, T. (2013). Identifying the fundamentals of care within cochrane systematic reviews: The role of the cochrane nursing care field fundamentals of care node. International Journal of Nursing Practice, 19, 109–115. https://doi.org/10.1111/ijn.12059 [DOI] [PubMed] [Google Scholar]
- Mantzoukas, S. (2009). The research evidence published in high impact nursing journals between 2000 and 2006: A quantitative content analysis. International Journal of Nursing Studies, 46, 479–489. https://doi.org/10.1016/j.ijnurstu.2008.12.016 [DOI] [PubMed] [Google Scholar]
- Moore, K. N. , Hunter, K. F. , McGinnis, R. , Bacsu, C. , Fader, M. , Gray, M. , … Voaklander, D. C. (2009). Do catheter washouts extend patency time in long‐term indwelling urethral catheters? A randomized controlled trial of acidic washout solution, normal saline washout, or standard care. Journal of Wound Ostomy and Continence Nursing, 36, 82–90. https://doi.org/10.1097/01.WON.0000345181.37656.de [DOI] [PubMed] [Google Scholar]
- Ogilvie, D. , Fayter, D. , Petticrew, M. , Sowden, A. , Thomas, S. , Whitehead, M. , & Worthy, G. (2008). The harvest plot: A method for synthesising evidence about the differential effects of interventions. BMC Medical Research Methodology, 8, 8 https://doi.org/10.1186/1471-2288-8-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast, V. , Jakobsson, U. , Renvert, S. , & Hallberg, I. R. (2012). Effects of a standard versus comprehensive oral care protocol among intubated neuroscience ICU patients: Results of a randomized controlled trial. Journal of Neuroscience Nursing, 44, 134–146. https://doi.org/10.1097/JNN.0b013e3182510688 [DOI] [PubMed] [Google Scholar]
- Ragneskog, H. , Kihlgren, M. , Karlsson, I. , & Norberg, A. (1996). Dinner music for demented patients: Analysis of video‐recorded observations. Clinical Nursing Research, 5, 262–277; discussion 278–282. https://doi.org/10.1177/105477389600500302 [DOI] [PubMed] [Google Scholar]
- Rathert, C. , Wyrwich, M. D. , & Boren, S. A. (2013). Patient‐centered care and outcomes: A systematic review of the literature. Medical Care Research and Review: MCRR, 70, 351–379. https://doi.org/10.1177/1077558712465774 [DOI] [PubMed] [Google Scholar]
- Richards, D. , Coulthard, V. , & Borglin, G. (2014). The state of European nursing research: Dead, alive, or chronically diseased? A systematic literature review. Worldviews on Evidence‐Based Nursing, 11, 147–155. https://doi.org/10.1111/wvn.12039 [DOI] [PubMed] [Google Scholar]
- Richards, D. A. , & Rahm‐Hallberg, I. (2015). Complex interventions in health: An overview of research methods. London, UK: Routledge. [Google Scholar]
- Schnelle, J. F. , Alessi, C. A. , Simmons, S. F. , Al‐Samarrai, N. R. , Beck, J. C. , & Ouslander, J. G. (2002). Translating clinical research into practice: A randomized controlled trial of exercise and incontinence care with nursing home residents. Journal of the American Geriatrics Society, 50, 1476–1483. https://doi.org/10.1046/j.1532-5415.2002.50401.x [DOI] [PubMed] [Google Scholar]
- Suhonen, R. , Leino‐Kilpi, H. , & Valimaki, M. (2005). Development and psychometric properties of the Individualized Care Scale. Journal of Evaluation in Clinical Practice, 11, 7–20. https://doi.org/10.1111/j.1365-2753.2003.00481.x [DOI] [PubMed] [Google Scholar]
- The Cochrane Collaboration (2011). Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). Hoboken, NJ: Wiley‐Blackwell. [Google Scholar]
- Valderas, J. M. , & Alonso, J. (2008). Patient reported outcome measures: A model‐based classification system for research and clinical practice. Quality of Life Research, 17, 1125–1135. https://doi.org/10.1007/s11136-008-9396-4 [DOI] [PubMed] [Google Scholar]
- Webster, J. , Osborne, S. , Woollett, K. , Shearer, J. , Courtney, M. , & Anderson, D. (2006). Does evening removal of urinary catheters shorten hospital stay among general hospital patients? A randomized controlled trial. Journal of Wound Ostomy and Continence Nursing, 33, 156–163. https://doi.org/10.1097/00152192-200603000-00010 [DOI] [PubMed] [Google Scholar]
- Wilson, I. B. , & Cleary, P. D. (1995). Linking clinical variables with health‐related quality of life. A conceptual model of patient outcomes. JAMA, 273, 59–65. https://doi.org/10.1001/jama.1995.03520250075037 [PubMed] [Google Scholar]
- World Health Organisation (2016). International classification of functioning disability and health, Geneva. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


