Abstract
Objective
The objective was to determine whether brief, Web‐based instruction several weeks prior to tourniquet application improves layperson success compared to utilizing just‐in‐time (JiT) instructions alone.
Background
Stop the Bleed is a campaign to educate laypeople to stop life‐threatening hemorrhage. It is based on U.S. military experience with lifesaving tourniquet use. While previous research shows simple JiT instructions boost laypeople's success with tourniquet application, the optimal approach to educate the public is not yet known.
Methods
This is a prospective, nonblinded, randomized study. Layperson participants from the Washington, DC, area were randomized into: 1) an experimental group that received preexposure education using a website and 2) a control group that did not receive preexposure education. Both groups received JiT instructions. The primary outcome was the proportion of subjects that successfully applied a tourniquet to a simulated amputation. Secondary outcomes included mean time to application, mean placement position, ability to distinguish bleeding requiring a tourniquet from bleeding requiring direct pressure only, and self‐reported comfort and willingness to apply a tourniquet.
Results
Participants in the preexposure group applied tourniquets successfully 75% of the time compared to 50% success for participants with JiT alone (p < 0.05, risk ratio = 1.48, 95% confidence interval = 1.21–1.82). Participants place tourniquets in a timely fashion, are willing to use them, and can recognize wounds requiring tourniquets.
Conclusions
Brief, Web‐based training, combined with JiT education, may help as many as 75% of laypeople properly apply a tourniquet. These findings suggest that this approach may help teach the public to Stop the Bleed.
Background
“Stop the Bleed” is a nationwide campaign designed to empower and educate laypeople to stop life‐threatening hemorrhage before professional help arrives.1, 2 It is based on years of U.S. military experience in Iraq and Afghanistan, where swift application of extremity tourniquets, often applied by non–medically trained soldiers, saved an estimated 1,000 to 2,000 American lives.3 The program is endorsed by several federal agencies, the American College of Surgeons, and expert groups like the Hartford Consensus.4, 5
Importance
Although the benefits of rapid hemorrhage control with tourniquets are well established, the optimal approach to teaching laypeople these techniques is not known. Stop the Bleed lists “just‐in‐time” (JiT) bystander education as one of its five objectives.2 We have previously shown that providing laypeople simple JiT written instructions on a card boosts successful tourniquet application from 20% of attempts to 44%.6, 7 This JiT education compares favorably to other types of layperson medical training, such as bystander cardiopulmonary resuscitation training, that has documented successful performance rates as low as 30% following in‐person training.8
Goals of This Investigation
In this study, we tested whether exposure to brief, Web‐based instruction several weeks prior to tourniquet application improves layperson success compared to utilizing JiT instructions alone. Findings from this work could influence emerging nationwide Stop the Bleed education programs.
Methods
Study Design
This study is a prospective, randomized trial of two approaches to layperson education. Since it involved minimal risk to participants and did not collect personal health information, the Uniformed Services University Institutional Review Board approved it as an exempt educational protocol (MEM‐91‐3987). The primary outcome of interest was the proportion of subjects that successfully applied a tourniquet to a simulated amputation. Secondary outcomes included mean time to application, mean placement position, volunteer's ability to distinguish bleeding requiring a tourniquet from bleeding requiring direct pressure only, and self‐reported comfort and willingness to apply a tourniquet in a rescue scenario. A separate subgroup analysis sought to assess whether adding audio instructions to written JiT instructions boosts rates of successful tourniquet application. The education materials were developed by the National Center for Disaster Medicine and Public Health, with input from military and civilian experts. The model website used for preexposure education can be accessed at stopthebleed.usuhs.edu.
Study Setting and Population
Non–medically trained laypeople were recruited via electronic postings and information sheets. Volunteers came from Washington, DC, area businesses, nonprofit foundations, faith‐based institutions, universities, and government offices (Figure 1). Exclusion criteria included age less than 18 or greater than 65, being a health care provider, prior training in tourniquet use, and inability to return for assessment. Participants were not compensated for their time.
Figure 1.
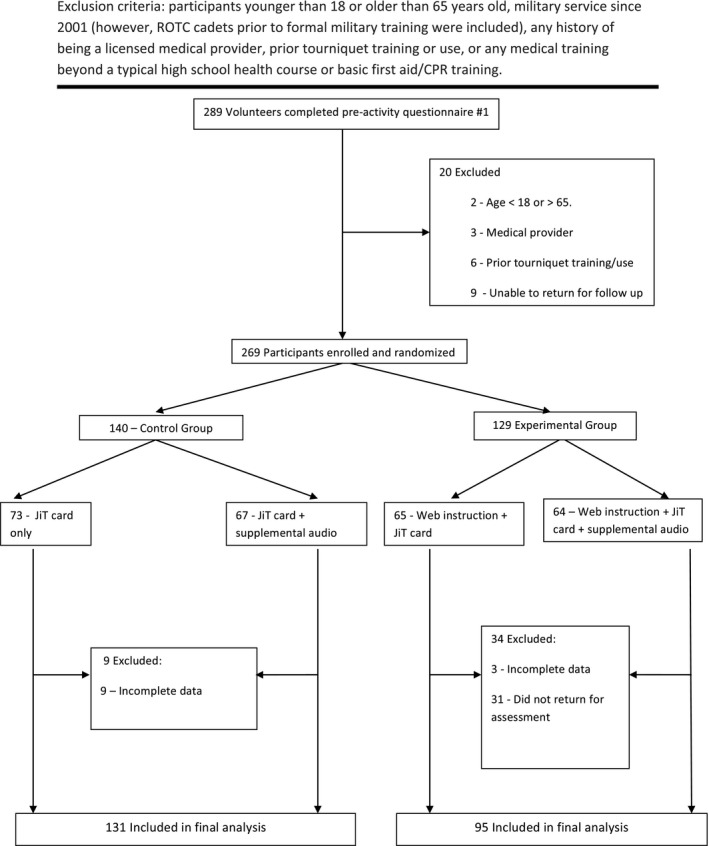
Participant enrollment.
Randomization
To determine their eligibility, volunteers completed a preactivity questionnaire. Those found to be eligible were randomized into one of two arms: 1) an experimental group that received preexposure education using the prototype Stop the Bleed website and 2) a control group that did not receive preexposure education. A post hoc analysis found that participants were well matched with regard to demographic characteristics (Table 1). At the time of assessment, all study groups received a written card that provided JiT instructions on tourniquet use (Figure 2). This is a card similar to the ones used successfully in our earlier studies.6, 7
Table 1.
Demographic Data of Study Participants
| Variable | No Preexposure (n = 131) | Preexposure (n = 95) | p‐value |
|---|---|---|---|
| Male, No. (%) | 48 (36.6) | 30 (31.6) | 0.44 |
| Race or ethnic group, No. (%) | 0.11 | ||
| White | 69 (52.7) | 46 (48.4) | — |
| Black | 32 (24.4) | 17 (17.9) | — |
| Asian | 14 (10.7) | 21 (22.1) | — |
| Hispanic | 12 (9.2) | 12 (12.6) | — |
| Age (years), mean (±SD) | 33 (±14.5) | 32 (±11.4) | 0.7 |
| Age category (years), No. (%) | 0.09 | ||
| 18–29 | 69 (52.7) | 48 (50.5) | — |
| 30–39 | 21 (16) | 23 (24.2) | — |
| 40–49 | 15 (11.5) | 10 (10.5) | — |
| 50–59 | 10 (7.6) | 11 (11.6) | — |
| 60–65 | 10 (7.6) | 1 (1.1) | — |
| Education, No. (%) | 0.63 | ||
| Some high school | 0 | 0 | — |
| High school | 4 (3.1) | 1 (1.1) | — |
| Some college or current college student | 41 (31.3) | 27 (28.4) | — |
| College graduate | 60 (45.8) | 45 (47.4) | — |
| Master's degree | 15 (11.5) | 17 (17.9) | — |
| Doctoral degree | 7 (5.3) | 5 (5.3) | — |
| Income, No. (%) | 0.7 | ||
| <$24,999 | 6 (4.6) | 7 (7.4) | — |
| $25,000–$49,999 | 20 (15.3) | 12 (12.6) | — |
| $50,000–$74,999 | 26 (19.8) | 17 (17.9) | — |
| $75,000–$99,999 | 15 (11.5) | 13 (13.7) | — |
| $100,000–$149,999 | 35 (26.7) | 23 (24.2) | — |
| $150,000–$199,999 | 8 (6.1) | 11 (11.6) | — |
| $200,000–$249,999 | 9 (6.8) | 4 (4.2) | — |
| >$250,000 | 4 (3.1) | 5 (5.3) | — |
Figure 2.
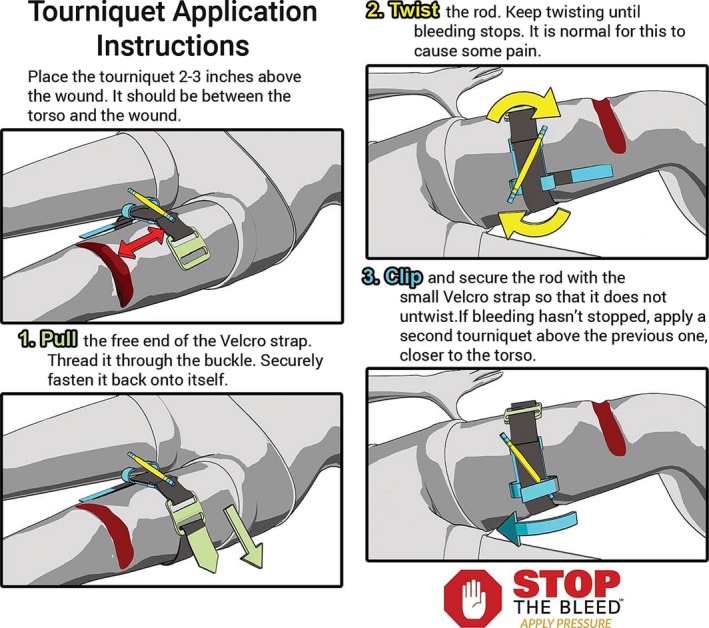
Just‐in‐time instruction card.
Each arm of the study was further divided into two subgroups (Figure 1). At the time of testing, half of participants in each arm received supplemental audio instructions that reinforce the JiT cards. The other half of both groups received only the JiT cards. After being randomly assigned to a study group, participants completed a second, preassessment questionnaire to report their attitudes about using a tourniquet.
The Primary Intervention
Participants randomized to the experimental group (preexposure education) were allowed up to 15 minutes to explore an instructional website using a Samsung SM‐T350 tablet and headphones. This program included a 5‐minute video on how to determine life‐threatening bleeding and apply a tourniquet, images that correspond to the JiT instruction card, a short quiz, a looping gif video depicting tourniquet application, and other resources. No directions were provided to participants on how to interact with the website. Following this brief review, participants could not return to the website because it was not publicly available. After completing preexposure education, these participants were dismissed and asked to return for assessment 4 to 8 weeks later. Control group participants did not receive any preexposure education on tourniquet use.
Measurements
To assess participants randomized to both the experimental and the control groups, an observer read a standardized scenario aloud and then directed each participant to apply a tourniquet to a lifelike silicone leg designed to simulate a fresh, above‐the‐knee amputation due to trauma. As the assessment began, all participants in each group received a JiT instruction card that explains the steps of tourniquet application. For this exercise, all participants used a specially modified combat application tourniquet with key components colored to match images depicted on the JiT card (Figure 2). This color‐coded tourniquet is the same one validated in our previous study.7 Half of participants in each study arm also received prerecorded, minute‐long, looping audio instructions intended to reinforce the guidance provided on the JiT card (Figure 1). An observer timed participants and documented their performance of critical actions, but did not interact with them in any way. Timing continued until the participant finished or seven minutes elapsed, whichever came first.
Outcomes
The main outcome measure was successful application of a tourniquet. Criteria for successful application included placement of the tourniquet proximal to the wound; application time less than 7 minutes; completion of all steps including securing the windlass rod in place; and adequate pressure applied. Observers considered tourniquet pressure adequate if they observed tourniquet indentation into the mannequin and were unable to slide a finger under the tightened band. After a primary observer completed each assessment, a second observer independently confirmed proper tourniquet placement and pressure and also documented any reason(s) for failure. If disagreement occurred, the study site supervisor cast the deciding vote. To preserve participant confidentiality, participant names were not linked to outcomes.
After completing the exercise, all participants reported their demographic data, both comfort and willingness to use a tourniquet (both quantified on 5‐point Likert scales) and a quiz consisting of five images of various extremity wounds prepared by a medical illustrator. After each image, participants were asked to identify whether or not the wound requires treatment with a tourniquet: three did, two did not.
Data Analysis
Group differences were explored using the chi‐square test. Continuous measurements, such as the seconds to completion, were evaluated using the t test. Changes in knowledge and attitudes before and after the activity were tested using the Stewart Maxwell test for marginal homogeneity. Demographic differences were assessed by either chi‐square test or Fisher's test, where appropriate. All analysis was conducted in the statistical software R. The study was powered to detect an improvement in main outcome measure (successful tourniquet placement) from 50% in the control group to 75% in the intervention group.
Results
A total of 226 participants completed the study: 95 in the experimental group (preexposure education + JiT card) arm and 131 in the control group (JiT card only; Table 1). Three‐fourths of participants (n = 71) in the intervention group successfully applied a tourniquet compared to half (n = 66) in the control group (risk ratio [RR] = 1.48, 95% confidence interval [CI] = 1.21–1.82).
Mean time for tourniquet application was 100 seconds in the intervention group and 108.5 seconds in the control group (NS). Both groups placed the tourniquet approximately 4 inches proximate to the wound (NS). Ninety percent of participants in both groups got either four or all five questions correct on the five‐question quiz to identify wounds that require a tourniquet.
Table 2 depicts reasons for failure and Table 3 characterizes participants’ pre‐ and postassessment attitudes about tourniquet use. The most common reason for incorrect tourniquet application was insufficient tightening. Compared to their preparticipation scores, both groups’ overall self‐reported willingness to use a tourniquet increased significantly, from 60% preparticipation to 79% following study participation. In addition, self‐reported confidence rose from 22% of participants describing themselves as “comfortable” or “very comfortable” with tourniquet use prior to participation to 47% postparticipation (Table 3)
Table 2.
Factors Observed During Tourniquet Application
| Outcome | No Preexposure (n = 131) | Preexposure (n = 95) | RR (95% CI) | p‐value | ||||
|---|---|---|---|---|---|---|---|---|
| Total | Instruction Card | Instruction Card and Audio | Total | Instruction Card and Mobile app | Instruction Card and Mobile App + Audio | |||
| Successful application, n (%) | 66 (50) | 30 | 36 | 71 (75) | 35 | 36 | 1.48 (1.21–1.82) | <0.05 |
| Seconds to successfully apply tourniquet, median (IQR) | 107 (68–147) | 91.5 | 110 | 100 (73–128) | 90 | 101 | — | 0.17 |
| Reason for failure (% of failures) | ||||||||
| Total number of failures | 65 (50) | 35 | 30 | 24 (39) | 11 | 13 | 0.51 (0.35–0.75) | <0.05 |
| Incorrect position | 6 (5) | 3 | 3 | 3 (3) | 2 | 1 | 0.65 | |
| Device too loose | 61 (47) | 34 | 27 | 21 (22) | 10 | 11 | 0.33 | |
| No all steps completed | 31 (24) | 18 | 13 | 14 (15) | 7 | 7 | 0.38 | |
| Subject requested to stop early | 3 (2) | 3 | 0 | 1 (1) | 0 | 1 | 0.93 | |
| Time (>7 minutes) | 2 (2) | 1 | 1 | 0 | 0 | 0 | — | — |
| Multiple reasons (any combination) | 31 (24) | 19 | 12 | 11 (12) | 6 | 5 | 0.78 | |
IQR = interquartile range; RR = risk ratio.
Table 3.
Participant Opinions
| Preactivity | Postactivity | OR (CI) | p‐value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total n (%) | No Preexposure | Preexposure | Total n (%) | No Preexposure | Preexposure | No Preexposure | Preexposure | No Preexposure | Preexposure | |
| Would you use a tourniquet in real life? | ||||||||||
| Yes | 136 (60) | 82 | 54 | 174 (79) | 104 | 70 | 3.5 (1.7–7.9) | 2.89 (1.3–7.0) | <0.05 | <0.05 |
| No or unsure | 89 (40) | 49 | 50 | 47 (21) | 23 | 24 | <0.05 | <0.05 | ||
| Comfort level of having to use a tourniquet in real life? | ||||||||||
| Very uncomfortable, uncomfortable, or neutral | 171 (78) | 96 | 75 | 115 (53) | 60 | 55 | 8.2 (3.2–26.6) | 2.54 (1.3–5.3) | <0.05 | <0.05 |
| Comfortable or very comfortable | 48 (22) | 29 | 19 | 104 (47) | 65 | 39 | <0.05 | <0.05 | ||
In retrospect, the provision of supplemental audio instructions to half of participants in both the experimental and the control groups was not adequately powered to detect meaningful improvement over provision of the JiT instruction cards alone. In general both subgroups in the experimental and control groups achieved comparable rates of success.
Discussion
Laypeople may be the first rescuers to encounter victims with life‐threatening extremity hemorrhage. For this reason, multiple groups have recommended teaching laypeople how to properly control life‐threatening bleeding.1, 2, 4, 5 Our study suggests that the addition of brief, easily disseminated Web‐based educational program paired with JiT training using a simple instruction card can achieve high rates of success.
This approach differs from previous layperson education efforts, such as bystander cardiopulmonary resuscitation training, that typically require learners to attend an in‐person class to obtain a certification card. Numerous groups have found that this strategy achieves retention rates as low as 30% 2 months after training.8, 9, 10, 11, 12 Recent modifications to CPR training, such as video self‐instruction, “hands‐only” CPR, and even cell phone CPR, have produced higher rates of success.8, 13, 14, 15, 16, 17, 18 This is consistent with modern education theory, which notes that adult learners benefit from immediate application of learning.19
In two previous studies, we found that previously untrained laypeople given JiT instructions on how to apply a tourniquet can successfully do so in roughly half of attempts—a higher success rate than traditional CPR training.6, 7
In this study, we found that the addition of a brief (<15 minutes), Web‐based training program can boost rates of tourniquet application as high as 75% 4 to 8 weeks after training. This is a better result than teaching laypeople to respond to other types of medical emergencies.8, 9, 10, 11, 12 The mean time to tourniquet application in the experimental and control arms of the study (100 and 108.5 seconds, respectively) is consistent with prior research and is acceptable to stop life‐threatening hemorrhage prior to arrival of emergency medical services.6, 7
In addition to demonstrating acceptable skill in tourniquet placement, the vast majority of participants with and without Web‐based instruction properly selected wounds that require a tourniquet. This indicates the fear that lay rescuers will select the wrong patients for tourniquets may be misplaced. Additionally, the laypeople in our study expressed a strong willingness to respond to life‐threatening bleeding and increased their confidence following brief educational exposure—both are key predictors of responding during a crisis.20, 21
Our study offers important insights into why some laypeople fail to properly apply a tourniquet. The most common reason—insufficient pressure—is consistent with prior studies.6, 7 This information may prompt product designers to devise a self‐tightening tourniquet or adjuncts that provide visual feedback when proper tightness is achieved.
The JiT and website instructions used in this study followed the military's recommendation that a tourniquet should be placed 2 to 3 inches proximal to the wound.22 However, there is variation in in the civilian trauma community (2–3 inches proximal to the wound vs. “as proximal as possible”). Based on the military's experience with blast‐related amputations and gunshot wounds, an average tourniquet placement 4 inches proximal to the wound should be sufficient to control bleeding.
Limitations
Participants were tested on a static leg model without the visual, auditory and emotional stress that is typically associated with treating one or more trauma victims with life‐threatening injuries. Further evaluations of Web‐based and JiT training in more stressful simulated environments or observation of volunteer performance and clinical outcomes in real‐world situations is warranted to confirm the value of this educational approach. It is possible, if not likely, that the volunteers who participated in our study are more highly motivated to help than average community members. And, individuals in some populations may be less likely to be present at the government, business, or church buildings we utilized. The fact that 24% of subjects randomized to preexposure Web‐based training did not return for follow‐up testing may have introduced a degree of selection bias. Finally, observers were not blinded to the training status of volunteers. However, the study outcomes, most notably proper placement of a tourniquet, were easily determined and quantified. There is little reason to expect that this was differentially expressed in the treatment groups.
Conclusion
In summary, brief, Web‐based training, combined with provision of just‐in‐time education, may help as many as 75% of laypeople properly apply a tourniquet. Participants in both arms of the study were able to identify wounds that require application of a tourniquet. These findings suggest that this low‐cost, readily scalable approach could teach the lay public to “Stop the Bleed.”
The authors thank Dr. Andrew Branting and Dr. Erin Mack for their help in creating the simulators and arranging data collection, Elizabeth Weissbrod and Eric Wilson for assistance with project artwork and simulators, and all the volunteer study observers and site coordinators.
AEM Education and Training 2018;2:154–161
This study was funded by a U.S. Department of Defense grant to the National Center for Disaster Medicine & Public Health, titled “Core Support—National Center for Disaster Medicine and Public Health (NCDMPH),” grant HT9404‐12‐1‐0032, Craig Goolsby, MD, MEd, principal investigator.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Uniformed Services University, Department of the Army, Department of Defense, or the U.S. Government.
CAG has a patent filed (Number 62/152,174) entitled, “Tourniquet and Method of Use.” The patent's contents are not directly related to this paper.
Author contributions: CAG, KSR, KG, and VK developed the study concept and design; KSR, VK, KG, LR, and CG acquired data; CAG, LR, and SR analyzed data; CAG, KSR, and TK drafted manuscript; SR provided statistical expertise; CAG, AK, and TK provided critical revisions of the manuscript; CAG and KSR acquired funding.
References
- 1. Rasmussen TE, Baer DG, Goolsby C. The giving back: battlefield lesson to national preparedness. J Trauma Acute Care Surg 2016;80:166–7. [DOI] [PubMed] [Google Scholar]
- 2. What the White House's Stop the Bleed Campaign Means for EMS. 2017. Available at: http://www.jems.com/articles/print/volume-41/issue-40/special-focus-gearing-up-for-active-shooter-tactical-high-threat-incidents/what-the-white-house-s-stop-the-bleed-campaign-means-for-ems.html. Accessed Jun 3, 2017.
- 3. Blackbourne LH, Baer DG, Eastridge BJ, et al. Military medical revolution: prehospital combat casualty care. J Trauma Acute Care Surg 2012;73:S372–7. [DOI] [PubMed] [Google Scholar]
- 4. Jacobs LM, Wade D, McSwain NE, et al. Hartford Consensus: a call to action for THREAT, a medical disaster preparedness concept. J Am Col Surg 2014;218:467–75. [DOI] [PubMed] [Google Scholar]
- 5. Jacobs LM Jr. The Hartford Consensus III: implementation of bleeding control‐if you see something do something. Bull Am Coll Surgeons 2015;100:20–6. [PubMed] [Google Scholar]
- 6. Goolsby C, Branting A, Chen E, Mack E, Olsen C. Just‐in‐time to save lives: a pilot study of layperson tourniquet application. Acad Emerg Med 2015;22:1113–7. [DOI] [PubMed] [Google Scholar]
- 7. Goolsby C, Chen E, Branting A, et al. Analysis of layperson tourniquet application using a novel color‐coded device. Disast Med Public Health Prep 2016;10:274–80. [DOI] [PubMed] [Google Scholar]
- 8. Einspruch EL, Lynch B, Aufderheide TP, Nichol G, Becker L. Retention of CPR skills learned in a traditional AHA Heartsaver course versus 30‐min video self‐training: a controlled randomized study. Resuscitation 2007;74:476–86. [DOI] [PubMed] [Google Scholar]
- 9. Smith KK, Gilcreast D, Pierce K. Evaluation of staff's retention of ACLS and BLS skills. Resuscitation 2008;78:59–65. [DOI] [PubMed] [Google Scholar]
- 10. Chalkias A, Antoniou P, Xanthos T. Education in resuscitation: the need for a new teaching method. Am J Emerg Med 2017;35:370–1. [DOI] [PubMed] [Google Scholar]
- 11. Mahony PH, Griffiths RF, Larsen P, Powell D. Retention of knowledge and skills in first aid and resuscitation by airline cabin crew. Resuscitation 2008;76:413–8. [DOI] [PubMed] [Google Scholar]
- 12. Anderson GS, Gaetz M, Masse J. First aid skill retention of first responders within the workplace. Scand J Trauma, Resusc Emerg Med 2011;19:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Benoit JL, Vogele J, Hart KW, Lindsell CJ, McMullan JT. Passive ultra‐brief video training improves performance of compression‐only cardiopulmonary resuscitation. Resuscitation 2017;115:116–9. [DOI] [PubMed] [Google Scholar]
- 14. Todd KH, Heron SL, Thompson M, Dennis R, O'Connor J, Kellermann AL. Simple CPR: a randomized, controlled trial of video self‐instructional cardiopulmonary resuscitation training in an African American church congregation. Ann Emerg Med 1999;34:730–7. [DOI] [PubMed] [Google Scholar]
- 15. Merchant RM, Abella BS, Abotsi EJ, et al. Cell phone cardiopulmonary resuscitation: audio instructions when needed by lay rescuers: a randomized, controlled trial. Ann Emerg Med 2010;55(538–43):e1. [DOI] [PubMed] [Google Scholar]
- 16. Chang MP, Gent LM, Sweet M, Potts J, Ahtone J, Idris AH. A novel educational outreach approach to teach hands‐only cardiopulmonary resuscitation to the public. Resuscitation 2017;116:22–6. [DOI] [PubMed] [Google Scholar]
- 17. Del Rios M, Aldeen A, Campbell T, et al. Save‐a‐life at the ballpark: 10‐min spectator training achieves proficiency in cardiac arrest response. Resuscitation 2015;87:21–5. [DOI] [PubMed] [Google Scholar]
- 18. Panchal AR, Meziab O, Stolz U, et al. The impact of ultra‐brief chest compression‐only CPR video training on responsiveness, compression rate, and hands‐off time interval among bystanders in a shopping mall. Resuscitation 2014;85:1287–90. [DOI] [PubMed] [Google Scholar]
- 19. Knowles MS, Holton EF III, Swanson RA. Part 3: advancements in adult learning In: The Adult Learner: The definitive classic in adult education and human resource development. 8th ed Abingdon, Oxon/New York, NY: Routledge, 2015. pp. 369–70. [Google Scholar]
- 20. Qureshi K, Gershon RR, Sherman MF, et al. Health care workers’ ability and willingness to report to duty during catastrophic disasters. J Urban Health 2005;82:378–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Barnett DJ, Balicer RD, Thompson CB, et al. Assessment of local public health workers’ willingness to respond to pandemic influenza through application of the extended parallel process model. PLoS One 2009;4:e6365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Montgomery HR, Butler FK, Kerr W, et al. TCCC Guidelines Comprehensive Review and Update: TCCC Guidelines Change 16‐03. J Special Oper Med 2017;17:21–38. [DOI] [PubMed] [Google Scholar]


