Abstract
Objective
To characterize associations of snacking frequency with weight status among US children aged 1 to 5 years.
Methods
Participants were children (n = 4,669) aged 1 to 5 years in the 2005 to 2014 National Health and Nutrition Examination Survey (NHANES). Snacking was assessed by two 24‐hour dietary recalls using definitions that considered “snack” occasions as well as other foods/beverages consumed between meals. Overweight/obesity (OW/OB) was defined using percentile cutoffs: ≥ 97.7th weight‐for‐length (< 2 years) cutoff and the ≥ 85th BMI‐for‐age (≥ 2 years) cutoff. Linear/logistic regressions evaluated snacking based on daily occasions and relative to current recommendations (two to three snacks per day).
Results
During 2005 to 2014, US children aged 1 to 5 years consumed, on average, two to three snacks daily. Children with normal weight in both age groups tended to snack less frequently than children with OW/OB when considering all foods/beverages eaten between meals (P < 0.01‐0.12). Across most snacking definitions, children < 2 years who snacked more frequently than recommended had greater odds of having OW/OB (P < 0.01‐0.12) and consumed greater daily snack energy than those who snacked within recommendations (all P < 0.01). Recommendations did not clearly delineate weight status among children aged 2 to 5 years.
Conclusions
Snacking frequency and weight are positively associated among US children 1 to 5 years old, with most consistent associations seen among children < 2 years old and when considering all foods/beverages consumed between meals.
Introduction
Snacking (i.e., eating in between meals) is nearly universal among young children 1, 2. The American Academy of Pediatrics (AAP) recommends two to three small snacks daily for toddlers and two snacks daily for preschool‐aged children as part of its Healthy Active Living for Families obesity prevention–oriented guidance 3. Despite the fact that snacking is pervasive 1, 2, the association of snacking with overweight/obesity (OW/OB) is unclear, particularly for young children for whom snacks are believed to be most nutritionally important 4. Concerns about snacking 5 have arisen in response to secular increases in the number and portion size of snacks consumed by US children since the late 1970s 2. Furthermore, the top snack foods consumed by US children (2 to 18 years of age) are desserts, sweetened beverages, and salty snacks that tend to be high in energy, saturated fat, and added sugars 6. Surprisingly, there have been no studies of snacking and weight outcomes focused on toddlers and preschoolers, particularly at the national level.
Measurement issues, including the lack of a standard definition, are often cited as a fundamental barrier to understanding associations of snacking with obesity and other health outcomes 7. Snacking tends to be participant defined in epidemiological studies; this is potentially problematic for understanding weight outcomes among children, given qualitative findings that parents offer young children foods and beverages outside of meals that they do not consider to be “snacks” 8, 9. Analytical definitions of snacking have similarly differed as to whether all food and beverage occasions between meals are considered to be snacks 1, 6, 10, 11, 12, as opposed to only those occasions identified by caregivers as snacks being included 13, 14, and whether occasions involving trivial energy intake (e.g., water) are included 1, 11, 13, 14 or excluded 6, 10, 12. As noted by Murakami and Livingstone 12, much of the research on this topic has also failed to account for reporting bias that may attenuate the relationship between snacking and weight 15.
The purpose of this analysis was to evaluate, for the first time (to our knowledge), the association of daily snacking occasions with weight status among US children aged 1 to 5 years, using 2005 to 2014 National Health and Nutrition Examination Survey (NHANES) data. A secondary aim was to characterize associations of snacking occasions with the patterning of energy intake. AAP guidance on snacking was used to contextualize associations of snacking with weight and energy intake 3. Associations were evaluated across several occasion‐based analytical definitions of snacking to address gaps in knowledge around measurement. Models were adjusted for dietary reporting accuracy to account for potential reporting bias as well as for mean snack size and snack energy density to consider other snacking dimensions that might explain associations with weight. Data from children 1 to 2 years of age were analyzed separately from those of older children in the interest of: (1) generating population‐representative evidence to support the development of dietary guidelines for children under 2 years of age 16 and (2) reflecting age‐related differences in assessment and definition of OW/OB (17).
Methods
Design and participants
Participants were US children aged 1 to 5 years (12 to 71.9 months) in the 2005 to 2014 NHANES. NHANES is a continuous, cross‐sectional, nationally representive study of the nutritional and health status of the civilian noninstitutionalized US population 18, 19. NHANES uses a complex, multistage, probability sampling design with county as the primary sampling unit, within which clusters of households are selected, followed by the selection of participants. Data are released in 2‐year cycles; five consecutive cycles from 2005 to 2014 were examined. NHANES included an in‐home interview during which demographic data were collected. Dietary and anthropometric data were collected during a second visit to a mobile examination center; dietary data were also collected during a follow‐up telephone call. Response rates across data cycles evaluated in this research ranged from 68.5% to 77.3% (median = 75.4%). Written consent for children's participation was provided by the parent/legal guardian as approved by the National Center for Health Statistics Research Ethics Review Board.
Children between the ages of 12 and 71.9 months were included in the analysis. Exclusion criteria for the present analysis included the use of medications known to affect appetite and/or weight (e.g., prednisolone, levothyroxine, n = 90), the presence of diabetes (n = 1), having < 1 day of dietary data (n = 598), and missing weight and/or length or height data (n = 227). Cases that included eating occasions labeled as “infant feeding” were also excluded (n = 512), as many of these instances involved solely milk feedings (e.g., human milk, formula; data not shown). The final analytic sample included 4,669 children.
Measures
Demographics
Data on age, sex, and race/ethnicity were collected for the participating child and head of the household (HH) via computer‐assisted software at an in‐home interview. Data on marital status, level of education, and income were collected about the HH. The ratio of income to poverty (RIP) was estimated to express family income relative to the poverty threshold, with adjustments for geographic location and family size 20.
Dietary intake
Daily snacking occasions were assessed as part of the What We Eat in America interview 21 using two 24‐hour dietary recalls. The first recall occurred in person in the mobile examination center and a second recall occurred by telephone. The Automated Multiple‐Pass Method was used to collect the data, including a quick list recall, forgotten foods, eating time and frequency, detail cycle, and final probe. A proxy respondent (e.g., a parent or caregiver from the home) completed dietary recalls on behalf of children. Data were processed using the US Department of Agriculture Food and Nutrient Database for Dietary Studies (versions 3.0, 4.1, 5.0, 2010‐2011, 2013‐2014). Mean 2‐day values were calculated for each individual and used with dietary weights developed for use with 2 days of recall data that adjust sample weights for dietary nonresponse and day of the week 22. Nutrient intakes from supplements were not included in this analysis, given the focus on eating behavior and food intake.
Eating occasions were participant defined (i.e., by proxy) from a predetermined list. Consistent with previous studies, all food and beverages reported at the same clock time were considered a single eating occasion 12. Following previous research, two main occasion‐based definitions of snacking were employed (including Spanish equivalents): (1) only those occasions identified by the caregiver as a snack 13, 14 and (2) snack occasions plus all other foods/beverages consumed between meals as given by “beverage” and “extended consumption” occasion labels 1, 6, 10, 11, 12. Each of these definitions was evaluated with 1, 11, 13, 14 and without occasions 6, 10, 12 at which trivial energy (< 5 kcal) was consumed (e.g., water). Of all eating occasions reported between meals, 39,905 were labeled as snacks, whereas 7,955 were labeled as beverages and 3,125 were labeled as extended consumption. Removal of occasions involving trivial energy intake (< 5 kcal) excluded 4,319 snack, 2,879 beverage, and 2,210 extended consumption occasions.
Descriptive data on the types of foods and beverages consumed between meal eating occasions were generated using What We Eat in America food group classifications 21: (1) milk and milk products; (2) meat, poultry, fish, and mixtures; (3) eggs; (4) beans, legumes, nuts, and seeds; (5) grain products (e.g., bread, cake, cookies); (6) fruits (e.g., whole fruit, 100% fruit juice); (7) vegetables; (8) fats, oils, and salad dressings; or (9) sugars, sweets, and beverages (e.g., candies, sugar‐sweetened beverages).
Other snacking variables
Mean snack size (kilocalories) per occasion, daily snack energy (kilocalories), daily meal energy (kilocalories), total daily energy (kilocalories), and the percentage of total daily energy from snacks were used to characterize snacking influences on the patterning of energy intake.
Dietary reporting accuracy
Dietary reporting accuracy was estimated using the ratio of reported energy intake to estimated energy requirements (EI/EER) 12. Estimated energy requirements were calculated using Dietary Reference Intake equations based on age, sex, weight, and physical activity level 23. A “low active” level of physical activity (≥ 1.4 to < 1.6) was assumed for all children based on accelerometer data from NHANES 2003 to 2006 24. Following the methods of Murakami and Livingstone 12, the EI/EER ratio was used as a covariate in analyses, as this approach has been shown to yield similar results to excluding implausible cases, without biasing sample selection 12, 25).
Weight status
Child weight and recumbent length (children < 2 years) or standing height (children ≥ 2 years) were measured by trained professionals at the mobile examination center. OW/OB was defined following Centers for Disease Control and Prevention age‐specific recommendations 17. Among children < 2 years, overweight was defined as weight for length ≥ 97.7th percentile, based on World Health Organization growth standards 27. Among children ≥ 2 years, OW/OB was defined as BMI for age ≥ 85th percentile 28, based on Centers for Disease Control and Prevention reference data 29.
Analyses
Analyses were performed in Stata/SE (version 14.2; StataCorp, College Station, Texas). Descriptive statistics and measures of variability were generated for all variables; data are shown as the mean (SE) unless otherwise indicated. Data from children < 2 years of age (12 to 23 months; n = 809) were analyzed separately from those of older children aged 2 to 5 years (24 to 71 months; n = 3,860) to reflect substantive interests in building the evidence base for dietary guidelines for children under 2 years of age 16 and methodological issues related to the assessment of OW/OB 17. Analyses were conducted across four analytical definitions of snacking. Multiple linear regression was used to evaluate differences in the number of daily snacking occasions between children with normal weight versus those with OW/OB. To evaluate snacking relative to AAP guidance (two to three snacks for children < 2 years, two snacks for children ≥ 2 years (3)), the reference group was defined as two to three daily snacking occasions, against which less and more frequent snacking was compared. Logistic regression was used to evaluate prevalence of OW/OB, and multiple linear regression was used to evaluate the patterning of energy intake, relative to snacking recommendations.
Weights created specifically for 2 days of dietary data were used 22; these further adjust 1‐day sample weights for dietary nonresponse and day of the week. Poisson regression using backward elimination using P > 0.10 was used to evaluate the following potential covariates in models predicting daily snack occasions and weight status: child sex, age, race, EI/EER ratio, HH age, marital status, education, RIP, and survey cycle. Child race, EI/EER, HH age, marital status, education, RIP, and survey cycle year were retained in the model and included as covariates in all analyses for which daily snacking occasions was the predictor of interest. Mean snack size (kilocalories) was included as a precision variable in models evaluating the association of snacking occasions with weight status. The mean snack energy density (kilocalories per gram) of all foods and beverages consumed per snacking occasion 30 was also included in the aforementioned models as an indicator of snack quality in sensitivity analyses; substantive conclusions were equivalent. The distributions of daily energy and energy from snacks were not normally distributed. Square root transformation toward normality as suggested via Tukey's ladder of powers did not affect the substantive results. For this reason, the more interpretable, untransformed energy (kilocalorie) metric is presented. Statistical significance was inferred by P < 0.05.
Results
Demographics
The analytic sample was approximately 54% non‐Hispanic white, 16% Mexican American, 14% non‐Hispanic Black, 8% other race, and 8% other Hispanic (Table 1). Approximately 7% of children < 2 years old had overweight and 22% of children 2 to 5 years old had OW/OB. On average, HH age was 35 years, with more than half (56.9%) reporting education beyond high school and most (81.2%) either married or partnered. The RIP, on average, was 230%.
Table 1.
Demographic characteristics of US children aged 1‐5 y
| Total (n = 4,669) | < 2 y (n = 809) | ≥ 2 y (n = 3,860) | P | |
|---|---|---|---|---|
| % | % | % | ||
| Child | ||||
| Race | 0.62 | |||
| Non‐Hispanic White | 54.4 | 56.2 | 54.1 | — |
| Mexican American | 15.8 | 14.8 | 15.9 | 0.45 |
| Non‐Hispanic Black | 14.3 | 15.2 | 14.2 | 0.78 |
| Other race | 7.8 | 6.3 | 8.1 | 0.20 |
| Other Hispanic | 7.7 | 7.5 | 7.7 | 0.78 |
| Gender | 0.99 | |||
| Male | 51.6 | 51.0 | 51.7 | — |
| Female | 48.4 | 49.0 | 48.3 | 0.81 |
| Weight status a | ||||
| Normal weight | — | 93.5 | 77.7 | — |
| Overweight | — | 6.5 | 12.5 | — |
| Obesity | — | — | 9.8 | — |
| Caregiver | ||||
| Age, mean (SE) | 35.3 (0.3) | 34.3 (0.6) | 35.5 (0.3) | 0.08 |
| RIP, mean (SE) b | 2.3 (0.1) | 2.4 (0.1) | 2.3 (0.1) | 0.44 |
| Education | ||||
| High school or less | 43.1 | 41.5 | 43.3 | — |
| More than high school | 56.9 | 58.5 | 56.7 | 0.59 |
| Marital status | ||||
| Partnered | 81.2 | 80.6 | 81.3 | — |
| Not partnered | 18.8 | 19.4 | 18.7 | 0.77 |
Overweight among children < 2 y = weight for length ≥ 97.7th percentile 17, 27; overweight among children ≥ 2 y = BMI for age ≥ 85th percentile; obesity among children ≥ 2 y = BMI for age ≥ 95th percentile 28, 29.
Calculated by dividing family income by US Health and Human Services poverty guidelines, specific to family size, as well as year and state.
RIP, ratio of income to poverty; —, not applicable.
Snacking occasions
In the full sample, 77.2% of eating occasions between meals were labeled as snacks, whereas 16.5% were labeled as beverages and 6.3% were labeled as extended consumption. As shown in Figure 1, grains and milk or milk products were consumed most frequently at snack occasions among children < 2 years (29.0% and 21.0%, respectively), whereas grains and sugars/sweets were consumed most frequently among older children (27.8% and 25.8%, respectively). Of beverage occasions, milk or milk products were consumed most frequently by children < 2 years of age (58.0%), whereas sugars/sweets (i.e., sugar‐sweetened beverages) were most frequently consumed among older children (54.0%). Finally, sugars/sweets dominated extended consumption occasions in both age groups (61.7% among children < 2 years, 82.6% in children ≥ 2 years).
Figure 1.
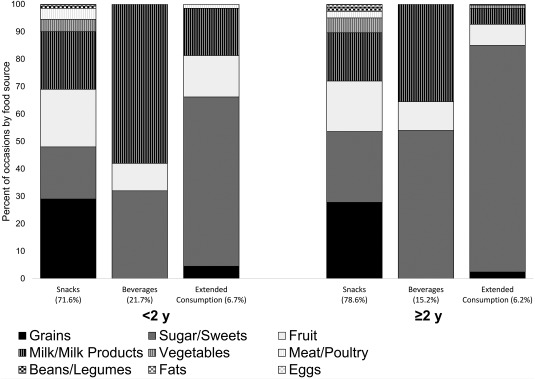
Food groups consumed outside of meal eating occasions.
The number of daily snack occasions (excluding < 5‐kcal occasions) was 2.3 (0.1) and 2.2 (0.03) among children < 2 years of age and children ≥ 2 years of age, respectively. When all eating occasions between meals (i.e., snacks, beverages, and extended consumption) were included in the definition (excluding < 5‐kcal occasions), daily snacking occasions increased to 3.1 (0.1) and 2.6 (0.03) among younger and older children, respectively. Mean snack size and energy density across snack definitions ranged from 117.3 (3.0) to 133.2 (3.4) kcal per occasion and 0.7 (0.02) to 1.5 (0.1) kcal/g among children < 2 years and 139.0 (1.8) to 170.4 (2.4) kcal per occasion and 0.8 (0.01) to 1.7 (0.03) kcal/g among older children, respectively.
As illustrated in Figure 2, the percentage of children meeting AAP recommendations varied with the snacking definition employed. Based on occasions labeled as snacks (< 5‐kcal occasions excluded), close to 57% of children were within AAP recommendations (i.e., two to three times daily), with approximately 8% of children snacking more frequently. When considering all energy‐containing eating occasions between meals (< 5‐kcal occasions excluded), close to a third of children < 2 years and approximately 17% of older children snacked more frequently than recommended.
Figure 2.
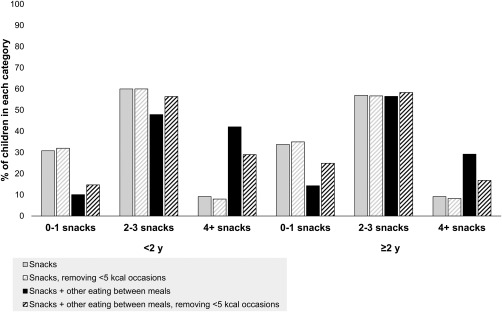
Distribution of snack consumption by age and snacking definition.
Associations of snacking occasions with child weight status
As shown in Table 2, when considering only occasions labeled as snacks (both with and without < 5‐kcal occasions), daily snacking occasions did not differ between children with normal weight and children with OW/OB in either age group. However, when expanding the definition to include all occasions between meals, children with normal weight consumed fewer snacks daily than children with OW/OB in both age groups. Daily snacking occasions were 3.2 (0.1) versus 3.7 (0.2) occasions per day among children with normal weight and OW/OB who were < 2 years and were 3.2 (0.04) versus 3.3 (0.1) occasions per day among children 2 to 5 years of age (all P < 0.05). Among children < 2 years but not older children, differences in daily snacking occasions by weight status remained significant when < 5‐kcal occasions were removed. In both age groups, children with normal weight also consumed less total daily energy from snacks as well as from meals in comparison to children with OW/OB (P < 0.01‐0.05; Supporting Information Table S1).
Table 2.
Mean snack occasions among US children 1‐5 y with normal weight and overweight
| < 2 y (n = 809)a | ≥ 2 y (n = 3,860)b | |||||
|---|---|---|---|---|---|---|
| Snack occasions | Snack occasions | |||||
| Mean | SE | P | Mean | SE | P | |
| Snacks c | ||||||
| Normal weight | 2.0 | 0.1 | — | 2.3 | 0.03 | — |
| Overweight/obesity | 2.4 | 0.2 | 0.10 | 2.4 | 0.1 | 0.29 |
| Snacks, removing < 5‐kcal occasions | ||||||
| Normal weight | 1.9 | 0.1 | — | 2.3 | 0.03 | — |
| Overweight/obesity | 2.4 | 0.2 | 0.07 | 2.3 | 0.1 | 0.33 |
| Snacks + other eating between meals d | ||||||
| Normal weight | 3.2 | 0.1 | — | 3.2 | 0.04 | — |
| Overweight/obesity | 3.7 | 0.2 | 0.02 | 3.3 | 0.1 | 0.02 |
| Snacks + other eating between meals, removing < 5‐kcal occasions | ||||||
| Normal weight | 2.6 | 0.1 | — | 2.7 | 0.04 | — |
| Overweight/obesity | 3.2 | 0.2 | < 0.01 | 2.8 | 0.1 | 0.12 |
Adjusted for dietary weights, survey cycle year, child race, HH age, HH marital status, HH level of education, RIP, EI/EER ratio, mean snack size, mean snack energy density.
Snacks = eating occasions identified by caregivers as snacks.
Other eating between meals = eating occasions identified by caregivers as beverages and extended consumption.
EI/EER, reported energy intake to estimated energy requirements; HH, head of household; RIP, ratio of income to poverty; —, not applicable.
Among children < 2 years of age, snacking more frequently than recommended by AAP was associated with increased odds of OW/OB for three of the four snacking definitions considered (Table 3). Odds of OW/OB among children < 2 years consuming four or more snacks per day ranged from 1.8 (not significant) to 14.4 (P < 0.01) times that of children who snacked within recommendations, and the predicted probability of OW/OB ranged from 18.7% (not significant) to 52.8% (P < 0.01). However, among children 2 to 5 years old, odds of OW/OB did not differ between children who snacked within recommendations versus more frequently than recommended, regardless of the snacking definition employed. When taking into account all eating occasions between meals (including < 5‐kcal occasions), children 2 to 5 years old who snacked infrequently (0‐1 times daily) were less likely to have OW/OB compared with children who snacked within recommendations (P < 0.05).
Table 3.
Odds of overweight/obesity by number of daily snacks among US children 1‐5 y
| Daily occasionsa | n | OR | 95% CI | Predicted probability (%) | P | |
|---|---|---|---|---|---|---|
| Snacks b | ||||||
| < 2 y c | ||||||
| 0‐1 snacks | 278 | 1.4 | 0.4 | 4.6 | 13.9 | 0.55 |
| 2‐3 snacks | 440 | ref | — | — | 10.4 | — |
| 4 + snacks | 91 | 10.2 | 2.7 | 37.9 | 46.3 | < 0.01 |
| ≥ 2 y d | ||||||
| 0‐1 snacks | 1,371 | 0.9 | 0.6 | 1.2 | 20.1 | 0.35 |
| 2‐3 snacks | 2,060 | ref | — | — | 22.7 | — |
| 4 + snacks | 429 | 1.1 | 0.6 | 1.7 | 23.7 | 0.83 |
| Snacks, removing < 5‐kcal occasions | ||||||
| < 2 y | ||||||
| 0‐1 snacks | 284 | 1.4 | 0.4 | 4.5 | 13.6 | 0.56 |
| 2‐3 snacks | 442 | ref | — | — | 10.4 | — |
| 4 + snacks | 83 | 14.4 | 3.6 | 57.2 | 52.8 | < 0.01 |
| ≥ 2 y | ||||||
| 0‐1 snacks | 1,410 | 0.9 | 0.6 | 1.2 | 20.3 | 0.42 |
| 2‐3 snacks | 2,044 | ref | — | — | 22.3 | — |
| 4 + snacks | 406 | 1.1 | 0.7 | 1.9 | 24.4 | 0.62 |
| Snacks + other eating between meals e | ||||||
| < 2 y | ||||||
| 0‐1 snacks | 86 | 0.3 | 0.1 | 1.2 | 4.5 | 0.09 |
| 2‐3 snacks | 373 | ref | — | — | 12.0 | — |
| 4 + snacks | 350 | 1.8 | 0.8 | 4.0 | 18.7 | 0.12 |
| ≥ 2 y | ||||||
| 0‐1 snacks | 609 | 0.7 | 0.5 | 1.0 | 16.2 | 0.03 |
| 2‐3 snacks | 2,001 | ref | — | — | 22.2 | — |
| 4 + snacks | 1,250 | 1.1 | 0.8 | 1.4 | 23.6 | 0.55 |
| Snacks + other eating between meals, removing < 5‐kcal occasions | ||||||
| < 2 y | ||||||
| 0‐1 snacks | 123 | 1.2 | 0.2 | 8.0 | 12.6 | 0.82 |
| 2‐3 snacks | 417 | ref | — | — | 10.7 | — |
| 4 + snacks | 269 | 3.0 | 1.3 | 6.7 | 23.8 | < 0.01 |
| ≥ 2 y | ||||||
| 0‐1 snacks | 976 | 0.9 | 0.6 | 1.3 | 20.0 | 0.57 |
| 2‐3 snacks | 2,088 | ref | — | — | 21.5 | — |
| 4 + snacks | 796 | 1.2 | 0.9 | 1.7 | 24.9 | 0.25 |
Adjusted for dietary weights, survey cycle year, child race, HH age, HH marital status, HH level of education, RIP, EI/EER ratio, mean snack size, mean snack energy density.
Per AAP guidance: 2‐3 snacks per day reference for both age groups.
Snacks = eating occasions identified by caregivers as snacks.
Other eating between meals = eating occasions identified by caregivers as beverages and extended consumption.
AAP, American Academy of Pediatrics; EI/EER, reported energy intake to estimated energy requirements; HH, head of household; OR, odds ratio; ref, reference value; RIP, ratio of income to poverty; —, not applicable.
Associations of snacking occasions with patterning of energy intake
As shown in Table 4, total daily energy intake of children who snacked within recommendations did not differ from those who snacked less or more frequently. Regardless of the snacking definition employed, children who snacked more frequently than recommended by the AAP tended to consume greater total daily energy from snacks and a greater percentage of total daily energy from snacks than those children who snacked within recommendations (all P < 0.001). Conversely, children who snacked less frequently consumed less daily energy from snacks and a lower percentage of their total daily energy from snacks (all P < 0.001). The mean snack size of children who snacked more frequently than recommended was smaller than that of children who snacked within recommendations (all P < 0.01), regardless of the definition used. With few exceptions, the mean snack size among children who snacked less frequently did not differ from that of children who snacked within recommendations.
Table 4.
Associations between number of daily snacks and patterning of energy intake among US children 1‐5 y
| Daily occasionsa | Mean snack size (kcal) | Daily snack energy (kcal) | Total daily energy (kcal) | % of daily energy from snacks | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | P | Mean | SE | P | Mean | SE | P | Mean | SE | P | |
| Snacks only b | ||||||||||||
| < 2 y a | ||||||||||||
| 0‐1 snacks | 119.9 | 7.6 | 0.3 | 121.7 | 7.4 | < 0.01 | 1,094.9 | 15.9 | 0.8 | 12.2 | 0.6 | < 0.01 |
| 2‐3 snacks | 110.5 | 3.5 | ref | 286.4 | 8.1 | ref | 1,090.2 | 13.4 | ref | 26.1 | 0.7 | ref |
| 4 + snacks | 82.6 | 6.8 | < 0.01 | 439.4 | 25.8 | < 0.01 | 1,080.0 | 45.6 | 0.8 | 37.9 | 1.7 | < 0.01 |
| ≥ 2 y b | ||||||||||||
| 0‐1 snacks | 191.4 | 4.9 | < 0.01 | 231.0 | 6.8 | < 0.01 | 1,566.5 | 13.8 | 0.8 | 13.7 | 0.4 | < 0.01 |
| 2‐3 snacks | 165.2 | 2.6 | ref | 415.6 | 6.4 | ref | 1,570.1 | 8.2 | ref | 26.5 | 0.3 | ref |
| 4 + snacks | 129.9 | 4.2 | < 0.01 | 580.4 | 20.1 | < 0.01 | 1,566.9 | 18.6 | 0.9 | 36.4 | 0.9 | < 0.01 |
| Snacks only, removing < 5‐kcal occasions | ||||||||||||
| < 2 y | ||||||||||||
| 0‐1 snacks | 122.5 | 7.4 | 0.2 | 124.6 | 7.2 | < 0.01 | 1,094.5 | 15.6 | 0.8 | 12.5 | 0.6 | < 0.01 |
| 2‐3 snacks | 111.1 | 3.3 | ref | 288.3 | 8.0 | ref | 1,089.6 | 13.1 | ref | 26.2 | 0.7 | ref |
| 4 + snacks | 87.8 | 6.5 | 0.01 | 458.0 | 21.2 | < 0.01 | 1,085.7 | 48.7 | 0.9 | 39.2 | 1.4 | < 0.01 |
| ≥ 2 y | ||||||||||||
| 0‐1 snacks | 197.1 | 6.2 | < 0.01 | 233.8 | 7.2 | < 0.01 | 1,564.0 | 13.7 | 0.6 | 14.0 | 0.5 | < 0.01 |
| 2‐3 snacks | 166.3 | 2.6 | ref | 417.5 | 6.3 | ref | 1,571.6 | 7.9 | ref | 26.6 | 0.4 | ref |
| 4 + snacks | 133.5 | 4.8 | < 0.01 | 595.5 | 21.7 | < 0.01 | 1,566.1 | 19.7 | 0.8 | 37.3 | 0.9 | < 0.01 |
| Snacks + other eating between meals c | ||||||||||||
| < 2 y | ||||||||||||
| 0‐1 snacks | 137.3 | 15.5 | 0.06 | 147.2 | 20.5 | < 0.01 | 1,086.7 | 36.7 | 0.8 | 15.1 | 1.3 | < 0.01 |
| 2‐3 snacks | 107.3 | 4.2 | ref | 293.8 | 11.3 | ref | 1,074.6 | 13.5 | ref | 28.4 | 1.0 | ref |
| 4 + snacks | 93.9 | 3.2 | 0.02 | 457.4 | 12.7 | < 0.01 | 1,111.0 | 20.1 | 0.1 | 40.9 | 1.0 | < 0.01 |
| ≥ 2 y | ||||||||||||
| 0‐1 snacks | 163.1 | 7.0 | 0.05 | 230.4 | 12.2 | < 0.01 | 1,562.9 | 16.7 | 0.3 | 12.9 | 0.8 | < 0.01 |
| 2‐3 snacks | 148.4 | 2.6 | ref | 410.5 | 7.7 | ref | 1,580.1 | 9.1 | ref | 25.9 | 0.5 | ref |
| 4 + snacks | 119.9 | 2.6 | < 0.01 | 574.5 | 11.9 | < 0.01 | 1,549.6 | 13.3 | 0.1 | 36.8 | 0.6 | < 0.01 |
| Snacks + other eating between meals, removing < 5‐kcal occasions | ||||||||||||
| < 2 y | ||||||||||||
| 0‐1 snacks | 143.7 | 13.2 | 0.2 | 147.5 | 14.3 | < 0.01 | 1,062.8 | 27.5 | 0.3 | 15.5 | 1.0 | < 0.01 |
| 2‐3 snacks | 125.2 | 3.9 | ref | 339.0 | 11.0 | ref | 1,095.6 | 13.8 | ref | 31.9 | 1.0 | ref |
| 4 + snacks | 99.4 | 3.6 | < 0.01 | 489.7 | 17.2 | < 0.01 | 1,100.2 | 25.6 | 0.9 | 43.5 | 1.0 | < 0.01 |
| ≥ 2 y | ||||||||||||
| 0‐1 snacks | 196.1 | 8.4 | < 0.01 | 243.6 | 8.7 | < 0.01 | 1,575.3 | 17.3 | 0.9 | 14.0 | 0.6 | < 0.01 |
| 2‐3 snacks | 170.1 | 2.4 | ref | 446.7 | 6.2 | ref | 1,573.0 | 6.5 | ref | 28.5 | 0.4 | ref |
| 4 + snacks | 137.2 | 2.9 | < 0.01 | 656.3 | 15.1 | < 0.01 | 1,554.7 | 15.8 | 0.1 | 41.9 | 0.6 | < 0.01 |
Adjusted for dietary weights, survey cycle year, child race, HH age, HH marital status, HH level of education, RIP, EI/EER ratio, mean snack size, mean snack energy density.
Per AAP guidance: 2‐3 snacks per day reference for both age groups.
Snacks = eating occasions identified by caregivers as snacks.
Other eating between meals = eating occasions identified by caregivers as beverages and extended consumption.
AAP, American Academy of Pediatrics; EI/EER, reported energy intake to estimated energy requirements; HH, head of household; ref, reference value; RIP, ratio of income to poverty; —, not applicable.
Discussion
Understanding modifiable practices that influence weight status among young children is critical to public health efforts to address obesity. To our knowledge, this research is the first to evaluate the association of daily snacking occasions with child weight status in a large nationally representative sample of US children aged 1 to 5 years. Results revealed that the associations varied with child age and the definition of snacking employed. Positive associations of snacking with weight status were seen most consistently among children under 2 years of age and when employing snacking definitions that took into account snacks and other occasions between meals, which were primarily occasions labeled beverages. That children with OW/OB in both age groups consumed greater daily energy from snacks than children with normal weight generally corroborates these findings. Collectively, the findings support the notion that snacking frequency is relevant for weight status, particularly among young children.
A causal role for snacking in the development of obesity is controversial, and evidence is mixed. Studies of older children or adolescents have observed negative associations of snacking 31 or eating frequency (a distinct but related construct) 32, 33, 34, 35 with weight status, whereas others have found no relationship 10 or a positive association 12, 35, 36. The present findings provide evidence that daily snacking occasions are positively associated with weight status (particularly for children < 2 years). The cross‐sectional nature of the data, however, precludes causal inferences. The present findings are inconsistent with a large meta‐analysis of 11 cross‐sectional studies involving 18,849 children 2 to 19 years of age that revealed a modest but negative association of daily eating frequency with weight status 37. However, it is important to note that many of the studies in the meta‐analysis involved less rigorous dietary assessment methods than those used in NHANES and did not take into account dietary reporting accuracy. A recent NHANES analysis of snacking and weight status among older children 6 to 11 years old revealed findings similar to those reported here when adjusting for dietary reporting accuracy, based on the EI/EER ratio 12. Observed differences in snacking between children with normal weight and children with OW/OB seen in the present study were relatively modest. At the same time, these findings raise the possibility that small differences in snacking may accumulate over time to influence OW/OB among young children.
Although the influence of snacking on weight status is of primary interest, it not possible to rule out reverse causality where children with higher weight may simply be prone to more frequent snacking. Indeed, children with higher weight have been observed to have higher levels of appetitive traits that favor excessive intake, including greater food responsiveness, reinforcing value of food 38, and intake of energy‐dense snacks in the absence of hunger 39. These traits may make some children more susceptible to potentially obesogenic aspects of the current dietary environment than others. For instance, an observational study of 5‐ to 6‐year‐old non‐Hispanic Black children (n = 100) found that those reported by their parents to have lower satiety responsiveness showed greater increases in energy intake across meals at which food portion sizes were systematically increased 40. Similarly, a study of 187 low‐income Hispanic preschoolers revealed that greater enjoyment of food was associated with more frequent snacking and greater daily energy intake from snacks among children with OW/OB, whereas the opposite was true of children with normal weight 41. Clearly, experimental and longitudinal designs are required to evaluate temporality and causality in associations of snacking with child appetite and weight outcomes.
The optimal frequency of snacking for promoting healthy growth in early childhood is unknown. This research used anticipatory guidance from AAP as a reference 3. The results provide strong support for AAP snacking guidance for toddlers; the odds of OW/OB among children < 2 years of age who snacked more frequently than AAP recommendations (two to three times daily) was 3‐ to 14‐fold greater than those children who were within recommendations. Children < 2 years who snacked within recommendations consumed roughly 26% to 32% of daily energy from snacks, whereas those who snacked more frequently consumed as much as 38% to 44% of daily energy from snacks, across definitions. In contrast, AAP guidance on snacking did not clearly delineate weight status among children 2 to 5 years old. The reasons for this are unclear. Additional research is needed to understand whether other dimensions (e.g., quality, time of day) or patterns of snacking are more relevant for weight status than number alone during the preschool years when rapid socialization of eating occurs.
Several strengths and limitations merit consideration. The use of NHANES data provides population‐representative “signals” on snacking and weight in a relatively large sample of US toddlers and preschoolers. Evaluating these associations across multiple snacking definitions is another strength. At the same time, multiple‐pass 24‐hour dietary recalls are considered the gold standard method of dietary assessment in epidemiological studies, but it is well acknowledged that this method underestimates true energy intake 42, particularly for individuals with higher weight 15. If present, however, this type of bias would likely attenuate associations of snacking with weight. This analysis defined snacking based on occasions rather than energy intake to minimize this type of bias. Related, data on snack and daily energy intake were primarily presented for descriptive purposes using group means, which are more robust than analyses estimating individual deviations in observed or predicted values. Finally, the EI/EER ratio was also included in analyses to account for reporting bias.
Conclusion
These findings provide new evidence of a positive association between the number of daily snacking occasions and OW/OB among US children aged 1 to 5 years, with most consistent associations seen among children < 2 years of age and when defining snacking based on all foods and beverages consumed between meals. These analyses are the first, to our knowledge, to specifically focus on children < 2 years of age for whom evidence‐based dietary guidance is critically needed (16). Additional research is needed to consider other facets of snacking that may influence OW/OB among young children, including the quality, timing, and portion sizes of snacks offered.
Supporting information
Supporting Information
Funding agencies: This study was funded by the National Institutes of Health, National Institute of Child Health and Development grant R21HD085137.
Disclosure: The authors declared no conflict of interest.
Author contributions: AK conducted the analyses and participated in drafting the manuscript. AD conceptualized the analytic approach, supervised the analyses, and provided critical review of the manuscript. RLB provided critical review of analyses and the manuscript. JOF conceptualized the research, provided critical direction for and review of analyses, and drafted the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- 1. Dunford E, Popkin B. 37 year snacking trends for US children 1977‐2014. Pediatr Obes 2018;13:247‐255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ziegler P, Hanson C, Ponza M, Novak T, Hendricks K. Feeding Infants and Toddlers Study: meal and snack intakes of Hispanic and non‐Hispanic infants and toddlers. J Am Diet Assoc 2006;106(1 Suppl 1):S107‐S123. [DOI] [PubMed] [Google Scholar]
- 3. American Academy of Pediatrics . HALF Implementation Guide: age specific content. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/HALF-Implementation-Guide/Age-Specific-Content/Pages/Age-Specific-Content.aspx. Published 2016. Accessed January 1, 2017.
- 4. Casazza K, Fontaine KR, Astrup A, et al. Myths, presumptions, and facts about obesity. N Engl J Med 2013;368:446‐454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hess J, Slavin J. Snacking for a cause: nutritional insufficiencies and excesses of U.S. children, a critical review of food consumption patterns and macronutrient and micronutrient intake of U.S. children. Nutrients 2014;6:4750‐4759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Piernas C, Popkin BM. Trends in snacking among U.S. children. Health Aff (Millwood) 2010;29:398‐404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gregori D, Foltran F, Ghidina M, Berchialla P. Understanding the influence of the snack definition on the association between snacking and obesity: a review. Int J Food Sci Nutr 2011;62:270‐275. [DOI] [PubMed] [Google Scholar]
- 8. Fisher J, Wright G, Herman A, et al. “Snacks are not food”. Low‐income, urban mothers' perceptions of feeding snacks to their preschool‐aged children. Appetite 2015;84:61‐67. [DOI] [PubMed] [Google Scholar]
- 9. Blake CE, Younginer N, Fisher JO, et al. Child snacking contexts and purposes and their associated nutritional quality among low‐income caregivers of preschoolers. Poster presented at: International Society of Behavioral Nutrition and Physical Activity 2014 Annual Meeting; May 21‐24, 2014; San Diego, California.
- 10. Murakami K, Livingstone BE. Decreasing the number of small eating occasions (< 15% of total energy intake) regardless of the time of day may be important to improve diet quality but not adiposity: a cross‐sectional study in British children and adolescents. Br J Nutr 2015;115:332‐341. [DOI] [PubMed] [Google Scholar]
- 11. US Department of Agriculture Agriculture Research Service; Food Surveys Research Group . WWEIA data tables (2013‐2014). https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/wweia-data-tables/. Updated June 9, 2017. Accessed January 1, 2017.
- 12. Murakami K, Livingstone MBE. Associations between meal and snack frequency and overweight and abdominal obesity in US children and adolescents from National Health and Nutrition Examination Survey (NHANES) 2003‐2012. Br J Nutr 2016;115:1819‐1829. [DOI] [PubMed] [Google Scholar]
- 13. Shriver LH, Marriage BJ, Bloch TD, et al. Contribution of snacks to dietary intakes of young children in the United States. Matern Child Nutr 2018;14:e12454. doi:10.1111/mcn.12454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang D, van der Horst K, Jacquier E, Eldridge AL. Snacking among US children: patterns differ by time of day. J Nutr Educ Behav 2016;48:369‐375.e1. [DOI] [PubMed] [Google Scholar]
- 15. Fisher JO, Johnson RK, Lindquist C, Birch LL, Goran MI. Influence of body composition on the accuracy of reported energy intake in children. Obes Res 2000;8:597‐603. [DOI] [PubMed] [Google Scholar]
- 16. Raiten DJ, Raghavan R, Porter A, Obbagy JE, Spahn JM. Executive summary: evaluating the evidence base to support the inclusion of infants and children from birth to 24 mo of age in the Dietary Guidelines for Americans—“the B‐24 Project.” Am J Clin Nutr 2014;99:663S‐691S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Grummer‐Strawn LM, Reinold C, Krebs NF; Centers for Disease Control and Prevention . Use of World Health Organization and CDC growth charts for children aged 0‐59 months in the United States. MMWR Recomm Rep 2010;59(No. RR‐9):1‐15. [PubMed] [Google Scholar]
- 18. Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National Health and Nutrition Examination Survey: sample design, 2011‐2014. Vital and Health Statistics, series 2, no. 162. DHHS Publication No. 2014‐1362. Hyattsville, MD: National Center for Health Statistics; 2014. [PubMed]
- 19. Johnson CL, Paulose‐Ram R, Ogden CL, et al. National Health and Nutrition Examination Survey: analytic guidelines, 1999‐2010. Vital and Health Statistics, series 2, no. 161. DHHS Publication No. 2013‐1361. Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed]
- 20. US Department of Health and Human Services . Annual update of the HHS poverty guidelines. Fed Regist 2017;82:8831‐8832. [Google Scholar]
- 21. US Department of Agriculture Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics . What We Eat in America. http://www.ars.usda.gov/Services/docs.htm?docid=13793. Accessed June 26, 2015.
- 22. Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr 2016;7:121‐134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Institute of Medicine, Food and Nutrition Board . Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: National Academy Press; 2002. [DOI] [PubMed] [Google Scholar]
- 24. Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou CP, Spruijt‐Metz D. Physical activity in US youth: effect of race/ethnicity, age, gender, and weight status. Med Sci Sports Exerc 2010;42:2211‐2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jessri M, Lou WY, L'Abbe MR. Evaluation of different methods to handle misreporting in obesity research: evidence from the Canadian national nutrition survey. Br J Nutr 2016;115:147‐159. [DOI] [PubMed] [Google Scholar]
- 26. Centers for Disease Control and Prevention . National Health and Nutrition Examination Survey (NHANES): Anthropometry Procedures Manual. Atlanta, GA: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 27. World Health Organization, Multicentre Growth Reference Study Group . WHO Child Growth Standards: Length/Height‐for‐Age, Weight‐for‐Age, Weight‐for‐Length, Weight‐for‐Height and Body Mass Index‐for‐Age: Methods and Development. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 28. Flegal KM, Tabak CJ, Ogden CL. Overweight in children: definitions and interpretation. Health Educ Res 2006;21:755‐760. [DOI] [PubMed] [Google Scholar]
- 29. Kuczmarski RJ, Ogden CL, Grummer‐Strawn LM, et al. CDC Growth charts: United States. Advance Data, no. 314. Hyattsville, MD: National Center for Health Statistics; 2000. [PubMed]
- 30. Ledikwe JH, Blanck HM, Khan LK, et al. Dietary energy density determined by eight calculation methods in a nationally representative United States population. J Nutr 2005;135:273‐278. [DOI] [PubMed] [Google Scholar]
- 31. Keast DR, Nicklas TA, O'Neil CE. Snacking is associated with reduced risk of overweight and reduced abdominal obesity in adolescents: National Health and Nutrition Examination Survey (NHANES) 1999‐2004. Am J Clin Nutr 2010;92:428‐435. [DOI] [PubMed] [Google Scholar]
- 32. Lioret S, Touvier M, Lafay L, Volatier JL, Maire B. Are eating occasions and their energy content related to child overweight and socioeconomic status? Obesity (Silver Spring) 2008;16:2518‐2523. [DOI] [PubMed] [Google Scholar]
- 33. Zerva A, Nassis GP, Krekoukia M, Psarra G, Sidossis LS. Effect of eating frequency on body composition in 9‐11 year‐old children. Int J Sports Med 2007;28:265‐270. [DOI] [PubMed] [Google Scholar]
- 34. Barba G, Troiano E, Russo P, Siani A. Total fat, fat distribution and blood pressure according to eating frequency in children living in southern Italy: the ARCA project. Int J Obes (Lond) 2006;30:1166‐1169. [DOI] [PubMed] [Google Scholar]
- 35. Jennings A, Cassidy A, van Sluijs EM, Griffin SJ, Welch AA. Associations between eating frequency, adiposity, diet, and activity in 9‐10 year old healthy‐weight and centrally obese children. Obesity (Silver Spring) 2012;20:1462‐1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rodriguez‐Ramirez S, Mundo‐Rosas V, Garcia‐Guerra A, Shamah‐Levy T. Dietary patterns are associated with overweight and obesity in Mexican school‐age children. Arch Latinoam Nutr. 2011;61:270‐278. [PubMed] [Google Scholar]
- 37. Kaisari P, Yannakoulia M, Panagiotakos DB. Eating frequency and overweight and obesity in children and adolescents: a meta‐analysis. Pediatrics 2013;131:958‐967. [DOI] [PubMed] [Google Scholar]
- 38. Temple JL, Legierski CM, Giacomelli AM, Salvy SJ, Epstein LH. Overweight children find food more reinforcing and consume more energy than do nonoverweight children. Am J Clin Nutr 2008;87:1121‐1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Asta K, Miller AL, Retzloff L, Rosenblum K, Kaciroti NA, Lumeng JC. Eating in the absence of hunger and weight gain in low‐income toddlers. Pediatrics 2016;137:e20153786. doi:10.1542/peds.2015-3786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mooreville M, Davey A, Orloski A, et al. Individual differences in susceptibility to large portion sizes among obese and normal‐weight children. Obesity (Silver Spring) 2015;23:808‐814. [DOI] [PubMed] [Google Scholar]
- 41. Rudy E, Bauer KW, Hughes SO, et al. Interrelationships of child appetite, weight and snacking among Hispanic preschoolers. Pediatr Obes 2016;13:38‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Subar AF, Freedman LS, Tooze JA, et al. Addressing current criticism regarding the value of self‐report dietary data. J Nutr 2015;145:2639‐2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


