Abstract
Background
Increased relationship continuity in primary care is associated with better health outcomes, greater patient satisfaction, and fewer hospital admissions. Greater socioeconomic deprivation is associated with lower levels of continuity, as well as poorer health outcomes.
Aim
To investigate whether deprivation scores predicted variations in the decline over time of patient-perceived relationship continuity of care, after adjustment for practice organisational and population factors.
Design and setting
An observational study in 6243 primary care practices with more than one GP, in England, using a longitudinal multilevel linear model, 2012–2017 inclusive.
Method
Patient-perceived relationship continuity was calculated using two questions from the GP Patient Survey. The effect of deprivation on the linear slope of continuity over time was modelled, adjusting for nine confounding variables (practice population and organisational factors). Clustering of measurements within general practices was adjusted for by using a random intercepts and random slopes model. Descriptive statistics and univariable analyses were also undertaken.
Results
Relationship continuity declined by 27.5% between 2012 and 2017, and at all deprivation levels. Deprivation scores from 2012 did not predict variations in the decline of relationship continuity at practice level, after accounting for the effects of organisational and population confounding variables, which themselves did not predict, or weakly predicted with very small effect sizes, the decline of continuity. Cross-sectionally, continuity and deprivation were negatively correlated within each year.
Conclusion
The decline in relationship continuity of care has been marked and widespread. Measures to maximise continuity will need to be feasible for individual practices with diverse population and organisational characteristics.
Keywords: continuity of patient care, primary health care, socioeconomic factors
INTRODUCTION
Halting the persistent and widespread decline of continuity of care is a challenge for English general practices.1 Continuity of care is generally regarded as a key feature and probable strength of primary care globally.2 Though researchers recognise several different types of continuity, it has two complementary essential elements: the ongoing relationship between an individual and a clinician (known as ‘relationship’ continuity), and the coordinated clinical care that progresses smoothly as the individual moves between different parts of the healthcare system (known as ‘management’ continuity).3 Relationship continuity is generally valued both by clinicians4 and by patients,5 especially those who are older or who have complex or worrying health problems.6,7
The benefits of increased relationship continuity include a more holistic approach to care,8 better recognition of some health problems,9 better concordance with medication regimens,10 better uptake of preventive services,11 and more cost-effective use of healthcare resources,12–14 including reduced hospital admission rates.15 However, the potential harms of continuity include increased staff costs to deliver,2 potential collusion with less adherence to professional standards and guidelines,16,17 and a lack of a fresh perspective8 that may cause diagnostic delay.18,19
Aiming largely to reduce hospital admissions, the General Medical Services Contract was amended in 2014–2015, requiring all patients aged ≥75 years to be provided with a named accountable GP, working with other professionals to ‘deliver a multidisciplinary care package’ and to ensure access to health checks. As of 2015–2016, all patients were required to have a named accountable GP to take ‘lead responsibility for the coordination of all services required under the contract’.20 In the first 9 months after these requirements were introduced there was no improvement in continuity.21
Socioeconomic deprivation measures the disadvantage of an individual or group relative to the local community or wider society,22 and, thus, is an indicator of socioeconomic position. Across the world, those who are disadvantaged in this way suffer higher rates of adverse health problems, such as suicide, heart disease, lung disease, obesity, and diabetes, and are more likely to have shorter lives.23
The Royal College of General Practitioners (RCGP) has compared continuity of care between clinical commissioning groups (CCGs).24 In CCGs with higher levels of deprivation, patients are less likely to have a preferred GP; the RCGP also found a weak negative correlation between being able to see a preferred GP (if the patient had one) and deprivation. However, some patients are more successful at obtaining continuity than others.25
How this fits in
Benefits of increased relationship continuity are associated with better health outcomes, and greater socioeconomic deprivation is associated with less continuity and poorer health outcomes. In this longitudinal observational study, deprivation scores did not predict variations in the decline of relationship continuity of care (as measured by the GP Patient Survey 2012–2017) at practice level after accounting for the effects of confounding variables. These confounders did not predict, or only weakly predicted, decline in continuity with very small effects. Continuity declined slightly more in practices with higher percentages of those aged ≥75 years or of those with chronic illness. This decline coincides with lengthening waiting times for routine GP appointments and increasing non-elective hospital admissions. The contractual return to a named doctor has, so far, not led to improved continuity.
Practices based in more deprived areas appear to have higher workloads than those in more affluent areas.26 For busier practices, providing adequate access to services could have an adverse impact on relationship continuity. Thus, this study aimed to explore the possible longitudinal association between deprivation and continuity. The research question was: do deprivation scores predict variations in the slopes over time of patient-perceived relationship continuity of care, after adjustment for organisational and other population factors at practice level?
METHOD
Existing data were published as spreadsheets by Public Health England (PHE), NHS England, NHS Digital, and the Department of Health.1 These were combined using the common unique practice identification code, into a single database for analysis of practices in England.
Dependent variable
This study used practice-level data. Data were extracted from weighted reports by the GP Patient Survey (GPPS)1 for the business years 2011–2012 to 2016–2017 inclusive, to calculate the study variable, patient-perceived relationship continuity, in other words, having both a preferred GP and being able to see that GP. As used by Freeman,2 this was calculated for each practice by multiplying the percentages of:
‘Yes’ responses to the Question 8 (Q8) ‘Have a preferred GP to see or speak to’; and
the sum of ‘Always or almost always’ and ‘A lot of the time’ (Q8); and responses to Q9 ‘Frequency of seeing preferred GP’ in those with a preferred GP. (The GPPS has validated this combination as representing higher access by presenting confidence intervals [CI] in their weighted reports.)1,28
Unlike some other questions in the GPPS, these questions have been present and unaltered in all years of the present study.
Independent variables
Though the research question in this study focused on the relationship between continuity and deprivation, the authors recognised that other factors might act as confounders in this relationship, and, thus, needed to be included in the analysis. Practice population and organisational characteristics may alter both workload and the practice’s capacity to address this.
A previous conceptual framework devised by the authors (Figure 1)27 was based on the postulation of a network, at the centre of which is an illness pathway with three groups of variables, containing an illness pathway starting with health determinants (the interactions between patient-related and disease-related factors), which give rise to health needs (based on a broad model of illness), which, in turn, predict and lead to health outcomes. Two groups of modifying factors, the context of population characteristics (a range of non-medical factors, including socioeconomic, cultural, policy-related, and physical environment) and healthcare interventions, may affect trajectories along illness pathways at various stages, whether by altering modifiable health determinants or the interactions between diseases and populations that generate health needs, or by reducing the risk of adverse health outcomes resulting from these health needs. Conceptually, healthcare interventions can be subdivided into structures — describing the organisation of healthcare systems — and processes — describing the range of actions undertaken by healthcare systems.
Figure 1.
Configuration of the population health framework showing the main variable domains and groups.27
Based on plausibility guided by the conceptual framework described above, and on data availability at practice level, the following variables were included as confounders, subdivided into:
population related: practice Indices of Multiple Deprivation (IMD) scores, percentages of the practice population aged ≥75 years,29 black or South Asian ethnicity (including mixed ethnicity), current smokers, report having a long-term condition, claim disability benefit (having permanent disability);1 and
organisation related: practice list size,30 location of the practice in England (subdivided into the North, Midlands, or the South, including London).31
Performance-related factors, such as Quality and Outcomes Framework (QOF) achievement, were not included in the study model, as these were not directly relevant to the present research question.
The GPPS question ‘Overall experience of GP surgery’ reflects the patient’s overall assessment of a practice. The sum of the ‘Very good’ and ‘Fairly good’ responses (other options were ‘Neither good nor poor’ and ‘Fairly poor’) was used for a subsidiary univariable analysis.
Missing data
A full set of values for all of the variables in each year studied was not obtained. However, because the proportion of missing values never exceeded 6% (Table 1), the authors decided not to undertake multiple imputation.
Table 1.
Descriptive statistics of variables
| Variable | Year | |||||
|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| Normally distributed | Mean (SD); % missing | Mean (SD); % missing | Mean (SD); % missing | Mean (SD); % missing | Mean (SD); % missing | Mean (SD); % missing |
| Continuity,a % | 37.5 (13.4); 1.50 | 35.9 (13.6); 1.10 | 34.3 (13.5); 0.97 | 32.1 (13.4); 1.40 | 30.1 (13.1); 1.40 | 27.2 (13.1); 3.40 |
| Has preferred GP, % (GPPS Q8) | 56.2 (11.6); 0.11 | 55.8 (11.5); 0.02 | 55.0 (11.4); 0.00 | 52.1 (12.0); 0.00 | 49.7 (11.8); 0.00 | 46.9 (11.9); 1.70 |
| Able to see GP always, almost always, or a lot of the time, % (GPPS Q9) | 65.2 (15.6); 1.20 | 62.8 (16.2); 0.80 | 61.0 (16.8); 0.66 | 59.8 (16.7); 1.10 | 58.4 (16.9); 1.10 | 55.5 (17.8); 3.10 |
| Good overall appointment experience, % (GPPS Q18) | 88.5 (7.4); 0.11 | 87.1 (8.1); 0.02 | 86.1 (8.6); 0.00 | 85.3 (9.3); 0.00 | 85.6 (9.0); 0.00 | 85.3 (9.4); 1.70 |
| Practice list aged ≥75 years, % (PHE) | 7.6 (3.1); 0.00 | 7.7 (3.1); 0.00 | 7.8 (3.1); 0.00 | 7.8 (3.2); 0.00 | 7.8 (3.2); 0.01 | 7.9 (3.3); 1.90 |
| Self-reported long-term condition, % (GPPS Q31) | 53.1 (7.4); 0.11 | 53.5 (7.7); 0.02 | 53.9 (7.7); 0.0 | 54.0 (7.9); 0.0 | 53.3 (7.8); 0.00 | 53.7 (7.8); 1.70 |
| Skewed distribution | Median (IQR); % missing | Median (IQR); % missing | Median (IQR); % missing | Median (IQR); % missing | Median (IQR); % missing | Median (IQR); % missing |
| List size, n (QOF) | 7060 (4685 to 10 136); 0.08 | 7141 (4750 to 10 228); 0.08 | 7212 (4808 to 10 312); 0.21 | 7321 (4898 to 10 453); 0.10 | 7454 (5038 to 10 677); 0.0 | 7718 (5211 to 10 959); 1.90 |
| Black ethnicity, % (GPPS Q52) | 0.0 (0.0 to 2.8); 5.60 | 0.0 (0.0 to 2.7); 5.70 | 0.0 (0.0 to 2.7); 4.10 | 0.0 (0.0 to 2.9); 4.10 | 0.6 (0.0 to 3.1); 1.90 | 0.6 (0.0 to 3.4); 4.30 |
| South Asian ethnicity, % (GPPS Q52) | 1.0 (0.0 to 4.1); 4.90 | 0.9 (0.0 to 4.1); 4.90 | 0.9 (0.0 to 4.3); 3.40 | 0.9 (0.0 to 4.3); 3.60 | 1.1 (0.0 to 5.1); 2.30 | 1.2 (0.0 to 5.0); 4.10 |
| Permanently sick or disabled, % (GPPS Q53) | 4.2 (2.5 to 6.6); 1.00 | 4.0 (2.3 to 6.4); 0.62 | 3.9 (2.1 to 6.2); 0.70 | 3.7 (2.1 to 6.1); 0.88 | 3.7 (1.9 to 5.9); 0.30 | 3.6 (1.9 to 5.8); 2.20 |
| Self-reported smokers, % (GPPS Q59) | 18.2 (14.1 to 23.0); 0.14 | 17.2 (13.1 to 21.8); 0.11 | 16.6 (12.6 to 21.5); 0.08 | 15.8 (11.9 to 20.6); 0.24 | 16.0 (12.1 to 20.5); 0.03 | 15.1 (11.1 to 19.7); 1.70 |
Continuity was calculated by multiplying the scores of specified responses to two questions in the GPPS: Q8, ‘Have a preferred GP to see or speak to’ (‘Yes’ answer), and Q9, ‘Frequency of seeing preferred GP’ (higher level of access: the sum of ‘Always or almost always’ and ‘A lot of the time’ answers). The GPPS responses are weighted and in the data presentation, a 95% confidence interval is given for each practice of the combined estimates of the two options. GPPS = GP Patient Survey. IQR = interquartile range. PHE = Public Health England. QOF = Quality and Outcomes Framework. SD = standard deviation.
Statistical analysis plan
Descriptive statistics of variables was undertaken, univariable analyses of the relationships between pairs of variables, and finally multivariable analyses.
A random intercepts and random slopes model was fitted to adjust for the clustering of measurements within practices. The a priori rationale for selecting this type of model was that it could not be assumed that the intercepts or slopes for all practices’ levels of continuity over time would be similar. The linear effect of each independent variable on continuity over time was modelled by fitting interaction terms, formed as the product of each independent variable with year. The significance of the interaction term between deprivation and year would indicate whether or not deprivation independently predicted the slope of continuity over time. Statistical significance was set at 5%. Post-estimation statistics were used to generate random effects values, predicted values for continuity, and to check intraclass correlations. STATA version 14 was used for all analyses.
RESULTS
Number of practices used in analysis
Of the 8160 practices with data, 1297 were single-handed practices either in 2013, 2014, or 2016 (the years for which these data were available). These were removed owing to being irrelevant to the research question of this study (practices with one GP are unlikely to offer discontinuity), leaving 6863 practices in the initial dataset. However, not all practices had complete datasets throughout the entire study period. Practices were excluded if either there were no continuity scores for any of the years studied, or the deprivation score was unavailable. Thus, 620 practices (9.0%) were excluded, leaving 6243 for the analysis.
Variables excluded from analysis
Though data were available for other variables, these were excluded from the analysis: the percentage of unemployed patients1 was highly correlated with IMD scores and had contributed to the calculation of IMD; number of GPs and nurses;32,33 and payments per registered patient34–36 as data for these variables were available for only 3 years, and across these years values were not highly correlated, meaning that imputation would be tenuous, with over half of the values requiring to be imputed.
Practice IMD scores were available for only 2012 and 2015, but these were very highly correlated (r = 0.98). As 2012 had more complete data, it was used to represent IMD for all years.
Years used in analysis
Originally, data were collated for 8 consecutive years, from 2009–2010 to the first quarter of 2017. However, in the first 2 years, 2009–2010 and 2010–2011, data for many of the independent variables were unavailable. In a multivariate analysis, the number of practices analysed would have been reduced, due to missing data, or a very large proportion of missing values would have had to have been multiply imputed. These 2 years were excluded from the multivariate analysis, leaving unimputed data for the 6 most recent (consecutive) years.
Descriptive statistics
Table 1 provides the distribution of values and the percentage of missing values in each year for all of the variables included in the analysis. Some variables, for example, continuity, had a normal distribution. Other independent variables had a skewed distribution, for example, ethnicity.
Univariable analyses
Although the mean of patient-perceived relationship continuity declined by 27.5% between 2012 and 2017, the standard deviation was fairly constant. The coefficient of variation, calculated by dividing the standard deviation by the mean, increased steadily and substantially over the years 2012–2017 (Table 2), indicating increased relative variability.
Table 2.
Variability of relationship continuity of care in England 2012–2017
| Year | Coefficient of variation (SD/mean) |
|---|---|
| 2012 | 0.36 |
| 2013 | 0.38 |
| 2014 | 0.39 |
| 2015 | 0.42 |
| 2016 | 0.44 |
| 2017 | 0.48 |
SD = standard deviation.
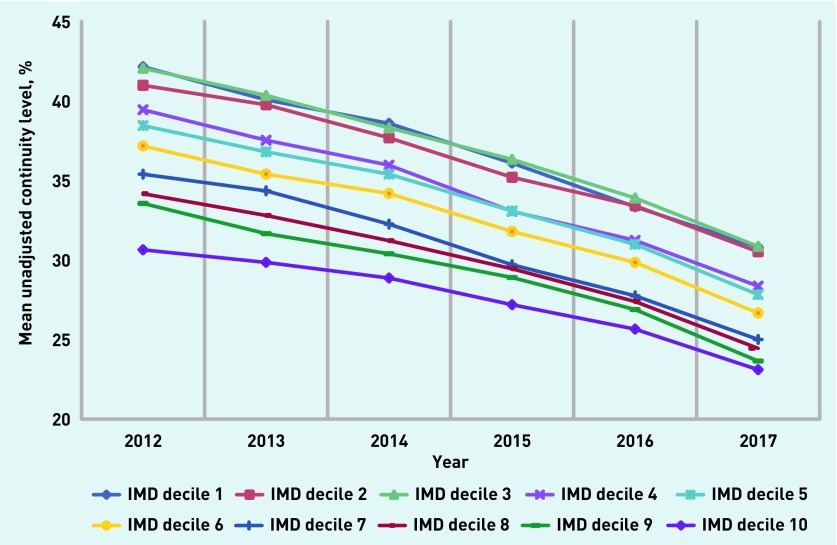
Practices were divided into deciles after ranking IMD scores. Mean unadjusted continuity levels for each deprivation decile declined similarly over the years 2012–2017 (Figure 2), although the cross-sectional correlation between continuity and IMD was negative in all years.
Figure 2.
Mean unadjusted continuity in English practices by IMD decile 2012–2017.
IMD = Indices of Multiple Deprivation.
The Pearson correlation (r) between continuity and good overall experience was moderately positive and consistent (0.49 to 0.51), over the years 2012–2017 (Table 3). Good experience was more positively correlated with being able to see a preferred GP (0.57 to 0.58) than with having a preferred GP (the coefficient increasing from 0.21 in 2012 to 0.29 in 2017).
Table 3.
Pearson correlation coefficient between satisfaction (good overall experience) and other variables
| Year | Continuity coefficient, r | Has preferred GP coefficient, r | Able to see preferred GP coefficient, r | IMD 2012 coefficient, r |
|---|---|---|---|---|
| 2012 | 0.49 | 0.21 | 0.57 | −0.27 |
| 2013 | 0.49 | 0.21 | 0.57 | −0.27 |
| 2014 | 0.50 | 0.21 | 0.57 | −0.25 |
| 2015 | 0.50 | 0.25 | 0.58 | −0.28 |
| 2016 | 0.49 | 0.27 | 0.57 | −0.30 |
| 2017 | 0.51 | 0.29 | 0.58 | −0.28 |
IMD = Indices of Multiple Deprivation.
Supplementary analyses
Though the research question in this study was focused on whether deprivation predicted variations in a specific metric of continuity, in other words, its slope over time, other associations between continuity and deprivation are possible and worth examining. In cross-sectional regressions, deprivation, as well as most of the independent variables used as confounders in the present model, predicted, with small effect sizes, variations in continuity for all 6 years, 2012–2017. Increases in deprivation score, list size, black, and South Asian ethnicities, and, in some years, smokers, predicted lower levels of continuity, but increases in those aged ≥75 years, and in some years, having a long-term condition and claiming disability, predicted higher levels of continuity (data not shown; available from authors on request).
Mixed effects multi-level regression
When the model was run for 2012–2017 (Table 4), the practice IMD score did not predict variations in the slope of relationship continuity at practice level, after accounting for the effects of organisational and population confounding variables. Of these confounding variables, five (using their interactions with year) predicted variations in the slope of relationship continuity either positively (less decline with higher values) for black ethnicity and South Asian ethnicity, or negatively (greater decline with higher values) for list size, those aged ≥75 years, and those having a self-reported long-term condition. As the effect sizes were small, significance may be partly due to the large sample size: for each 1% increase in the percentage of those aged ≥75 years or in those with long-term conditions, continuity slopes were, respectively, 0.059% and 0.013% steeper per year; for each 1% increase in the percentages of black and South Asian ethnicity, continuity slopes were, respectively, 0.025% and 0.010% less per year. The remaining three confounder variables were not significant: smokers, those with permanent disability, and geographical location of the practice.
Table 4.
Results of mixed-effects multi-level regression with dependent variable = continuity (product of ‘has preferred GP’ and ‘sees preferred GP’) from 6243 GP practices and 33 933 observations
| Independent variable (interaction with year) | Effect size of significant coefficient | 95% CI | P-value | Predictors,a % |
|---|---|---|---|---|
| IMD decile | 0.011 | −0.015 to 0.037 | 0.40 | |
| List sizeb | −0.000036 | −0.000047 to −0.000025 | <0.001 | −0.036 per 1000 patients |
| Black ethnicityb | 0.025 | 0.015 to 0.034 | <0.001 | 0.025 |
| South Asian ethnicityb | 0.0099 | 0.0051 to 0.015 | <0.001 | 0.010 |
| Aged ≥75 yearsb | −0.059 | −0.080 to −0.038 | <0.001 | −0.059 |
| Smokers | 0.0025 | −0.0058 to 0.011 | 0.56 | |
| Claiming disability | 0.0091 | −0.0077 to 0.026 | 0.29 | |
| Long-term conditionb | −0.013 | −0.021 to −0.0063 | <0.001 | −0.013 |
| Sub-regionc | 0.014 | −0.051 to 0.078 | 0.68 |
Change in slope of continuity for each year if variable increases by 1%, unless otherwise specified.
Significant predictors.
North sub region taken as reference. CI = confidence interval. IMD = Indices of Multiple Deprivation.
The intraclass correlation within the study model measured the proportion of the variation in continuity at the practice level. This was 0.804 (80.4%), justifying the use of a multi-level model.
DISCUSSION
Summary
Relationship continuity of care declined by 27.5% over the period 2012–2017, whereas relative variations in continuity increased between practices. In this study deprivation scores did not predict variations in the decline of relationship continuity at practice level, after accounting for the effects of organisational and population confounding variables, which themselves did not predict, or weakly predicted with very small effect sizes, the decline of continuity.
Strengths and limitations
This study’s strengths are the longitudinal analysis (unlike previous studies) using a robust statistical model, and the large sample size (all English practices with more than one GP), including recent (2017) data with low levels of missing values. For this study variable, an appropriate metric at practice level was chosen.2
However, there are limitations: only perceived relationship continuity was investigated, and this is difficult to measure. The GPPSs have had low response rates, largely addressed by a sophisticated weighting system.37 The GPPS-derived variables used were subjective measurements with no independent objective confirmation. Other unknown or unmeasured variables (possibly related to factors listed below) that might predict continuity or affect the adjusted slope were not available. By not using patient-level data, the authors were unable to establish relationships between deprivation and the slope of continuity at the individual level.
Comparison with existing literature
Factors other than deprivation may be implicated in the decline of continuity. Workload has steadily increased owing to: an ageing population with more morbidity, QOF incentivising proactive care,38 and work shifting from secondary care. Primary care services have become more fragmented owing to contract changes that allow alternative providers,38 and an increasing proportion of part-time or locum clinicians in the workforce.32,33 The proportion of total NHS spending allocated to primary care has declined.39 Policies extending opening hours and 7-day working will lead to prioritising rapid access over continuity, especially if practices cannot find sufficient capacity to cope with growing demands.
The analysis in the present study shows that, in the first 3 years after introducing the requirement for named GPs, continuity declined more in practices with higher percentages of those aged ≥75 years or of those with chronic illness. However, it may be too soon to fully evaluate the effectiveness of this new policy.
The decline in continuity coincides with reports of lengthening waiting times for routine GP appointments40 and an increase in non-elective hospital admissions in England of 11.5% between 2011–2012 and 2016–2017.41 Though there is an association between continuity and admission rates,15 this study is unable to conclude whether and to what extent the decline in continuity was a factor in the rise of admissions.
This study found that continuity and good overall experience were moderately correlated. Continuity is associated with higher satisfaction and with greater patient trust;42 however, if declining continuity were to result in lower satisfaction, then this might influence, in the longer term, how patients use services, such as more emergency department and private GP usage, or drive policy changes, such as further re-organisations of primary care.
Implications for research and practice
Greater relationship continuity of care is one mechanism for delivering safe, efficient, and coordinated care to increasingly complex patients. The authors hope to raise awareness of the extent and nature of the decline in continuity.
How much decline is due to workload, part-time doctors, or other factors? More detailed work within practices would be useful. This might include quantifying how many professionals are seen by individual patients, describing the characteristics of those patients who consult with numerous professionals, examining pathways (structures and processes, including appointment systems, telephones, reception configuration, teams), and reviewing policies, for example, priority groups of patients in larger practices using smaller teams.
The RCGP Toolkit43 will help practice teams to better measure continuity, undertake appropriate interventions, and audit the changes.
The contractual return to a named doctor is unlikely to improve continuity unless the causes of its decline are found and addressed. Measures to maximise continuity need to be evidence based, feasible for individual practices without detriment to overall service delivery, and lead to improved health outcomes.
Acknowledgments
The authors wish to acknowledge George Freeman, Imperial College London, for his helpful comments about the manuscript.
Funding
This work had no dedicated funding. No funding organisations had a role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Ethical approval
Ethical approval was not required, as the study used only published data without identified individuals.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.NHS England GP patient survey: surveys and reports: 2012–2017. https://gp-patient.co.uk/SurveysAndReports (accessed 1 May 2018).
- 2.Freeman G, Hughes J. Continuity of care and the patient experience. London: King’s Fund; 2010. [Google Scholar]
- 3.Hill AP, Freeman GK. Promoting continuity of care in general practice. London: RCGP; 2011. [Google Scholar]
- 4.Ridd M, Shaw A, Salisbury C. ‘Two sides of the coin’ — the value of personal continuity to GPs: a qualitative interview study. Fam Pract. 2006;23(4):461–468. doi: 10.1093/fampra/cml010. [DOI] [PubMed] [Google Scholar]
- 5.Saultz JW, Albedaiwi W. lnterpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med. 2004;2(5):445–451. doi: 10.1370/afm.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker R, Boulton M, Windridge K, et al. Interpersonal continuity of care: a cross-sectional survey of primary care patients’ preferences and their experiences. Br J Gen Pract. 2007;57(537):283–290. [PMC free article] [PubMed] [Google Scholar]
- 7.Turner D, Tarrant C, Windridge K, et al. Do patients value continuity of care in general practice? An investigation using stated preference discrete choice experiments. J Health Serv Res Policy. 2007;12(3):132–137. doi: 10.1258/135581907781543021. [DOI] [PubMed] [Google Scholar]
- 8.Rhodes P, Sanders C, Campbell S. Relationship continuity: when and why do primary care patients think it is safer? . Br J Gen Pract. 2014 doi: 10.3399/bjgp14X682825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koopman R, Mainous AG, 3rd, Baker R, et al. Continuity of care and recognition of diabetes, hypertension, and hypercholesterolaemia. Arch Int Med. 2003;163(11):1357–1361. doi: 10.1001/archinte.163.11.1357. [DOI] [PubMed] [Google Scholar]
- 10.Stevenson FA, Cox K, Britten N, Dundar Y. A systematic review of the research on communication between patients and health care professionals about medicines: the consequences for concordance. Health Expect. 2004;7(3):235–245. doi: 10.1111/j.1369-7625.2004.00281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flocke SA, Stange K, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(Suppl 8):AS21–AS30. doi: 10.1097/00005650-199808001-00004. [DOI] [PubMed] [Google Scholar]
- 12.Wasson JH, Sauvigne AE, Mogielnicki RP, et al. Continuity of outpatient medical care in elderly men. A randomized trial. JAMA. 1984;252(17):2413–2417. [PubMed] [Google Scholar]
- 13.Gill JM, Mainous AG., 3rd The role of provider continuity in preventing hospitalizations. Arch Fam Med. 1998;7(4):352–357. doi: 10.1001/archfami.7.4.352. [DOI] [PubMed] [Google Scholar]
- 14.Gill JM, Mainous AG, 3rd, Nsereko M. The effect of continuity of care on emergency department use. Arch Fam Med. 2000;9(4):333–338. doi: 10.1001/archfami.9.4.333. [DOI] [PubMed] [Google Scholar]
- 15.Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: cross sectional study of routinely collected, person level data. BMJ. 2017;356:j84. doi: 10.1136/bmj.j84. [DOI] [PubMed] [Google Scholar]
- 16.Hjortdahl P, Borchgrevink CF. Continuity of care: influence of general practitioners’ knowledge about their patients on use of resources in consultations. BMJ. 1991;303(6811):1181–1184. doi: 10.1136/bmj.303.6811.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Summerskill WS, Pope C. ‘I saw the panic rise in her eyes, and evidence-based medicine went out of the door.’ An exploratory qualitative study of the barriers to secondary prevention in the management of coronary heart disease. Fam Pract. 2002;19(6):605–160. doi: 10.1093/fampra/19.6.605. [DOI] [PubMed] [Google Scholar]
- 18.Broom DH. Familiarity breeds neglect? Unanticipated benefits of discontinuous primary care. Fam Pract. 2003;20(5):503–507. doi: 10.1093/fampra/cmg501. [DOI] [PubMed] [Google Scholar]
- 19.Rogers S, Gildea C, Meechan D, Baker R. Access, continuity of care and consultation quality: which best predicts urgent cancer referrals from general practice? J Public Health (Oxf) 2014;36(4):658–666. doi: 10.1093/pubmed/fdt127. [DOI] [PubMed] [Google Scholar]
- 20.NHS Employers 2015/16 General Medical Services (GMS) contract: guidance for GMS contract 2015/16. 2015. http://www.nhsemployers.org/~/media/Employers/Documents/Primary%20care%20contracts/GMS/GMS%20guidance%202010-present/2015-16/201516%20GMS%20Guidance.pdf (accessed 28 Jan 2018).
- 21.Barker I, Lloyd T, Steventon A. Effect of a national requirement to introduce named accountable general practitioners for patients aged 75 or older in England: regression discontinuity analysis of general practice utilisation and continuity of care. BMJ Open. 2016;6(9):e011422. doi: 10.1136/bmjopen-2016-011422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Townsend P. Deprivation. J Soc Policy. 1987;16(2):125–146. [Google Scholar]
- 23.Marmot M. The health gap: the challenge of an unequal world. London: Bloomsbury; 2015. [DOI] [PubMed] [Google Scholar]
- 24.Baker M, Jeffers H. Continuity of care in modern day general practice. London: RCGP; 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boulton M, Tarrant C, Windridge K, et al. How are different types of continuity achieved? A mixed methods longitudinal study. Br J Gen Pract. 2006;56(531):749–755. [PMC free article] [PubMed] [Google Scholar]
- 26.Boomla K, Hull S, Robson J. GP funding formula masks major inequalities for practices in deprived areas. BMJ. 2014;349:g7648. doi: 10.1136/bmj.g7648. [DOI] [PubMed] [Google Scholar]
- 27.Levene LS, Baker R, Bankart MJG, et al. How healthcare may modify the effects of health determinants on population outcomes: a conceptual framework for primary care. BJGP Open. (in press). [DOI] [PMC free article] [PubMed]
- 28.Campbell J, Smith P, Nissen S, et al. The GP Patient Survey for use in primary care in the National Health Service in the UK — development and psychometric characteristics. BMC Fam Pract. 2009;10:57. doi: 10.1186/1471-2296-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Public Health England National general practice profiles Practice summary downloads. https://fingertips.phe.org.uk/profile/general-practice (accessed 26 Apr 2018). [Google Scholar]
- 30.NHS Digital Number of patients registered at a GP practice: 2012–2017. https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice (accessed 27 Apr 2017).
- 31.NHS Digital Quality and Outcomes Framework 2012–13 to 2016–17. http://content.digital.nhs.uk/qof (accessed 20 Apr 2018).
- 32.NHS Digital NHS workforce statistics — December 2014 provisional statistics. http://content.digital.nhs.uk/catalogue/PUB16922 (accessed 20 Apr 2018).
- 33.NHS Digital Healthcare workforce statistics, September 2016, provisional experimental. http://www.content.digital.nhs.uk/catalogue/PUB23540 (accessed 20 Apr 2018).
- 34.NHS Digital NHS payments to general practice, England, 2015–16. http://www.digital.nhs.uk/catalogue/PUB21318 (accessed 20 Apr 2018). [Google Scholar]
- 35.NHS Digital NHS payments to general practice, England, 2014–15. https://digital.nhs.uk/catalogue/PUB18468 (accessed 20 Apr 2018). [Google Scholar]
- 36.NHS Digital NHS payments to general practice, England, 2013–14: experimental statistics. http://content.digital.nhs.uk/catalogue/PUB16847 (accessed 20 Apr 2018).
- 37.Ipsos MORI Social Research Institute GP Patient Survey — national summary report. [updated 7 January 2016; cited 19 August 2017. https://www.ipsos.com/ipsos-mori/en-uk/latest-gp-patient-survey-results-released-3 (accessed 20 Apr 2018).
- 38.NHS Employers . GMS contract changes 2003/04. NHS; 2014. http://www.nhsemployers.org/your-workforce/primary-care-contacts/general-medical-services/gms-contract-changes/contract-changes-2003-04 (accessed 20 Apr 2018). [Google Scholar]
- 39.NHS Digital, Health and Social Care Information Centre Investment in general practice 2009/10 to 2013/14 England, Wales, Northern Ireland and Scotland. http://content.digital.nhs.uk/catalogue/PUB14900/inve-gene-prac-eng-wal-ni-scot-09-14-rep.pdf (accessed 20 Apr 2018).
- 40.Kaffash J. Average waiting time for GP appointment increases 30% in a year. Pulse. 2016 Jun;10 http://www.pulsetoday.co.uk/your-practice/access/average-waiting-time-for-gp-appointment-increases-30-in-a-year/20032025.article (accessed 20 Apr 2018). [Google Scholar]
- 41.NHS England Monthly hospital activity data Hospital activity time-series 2012–2017. https://www.england.nhs.uk/statistics/statistical-work-areas/hospital-activity/monthly-hospital-activity/mar-data/ (accessed 20 Apr 2018). [Google Scholar]
- 42.Baker R, Mainous AG, 3rd, Gray DP, Love MM. Exploration of the relationship between continuity, trust in regular doctors, and patient satisfaction with consultations with family doctors. Scand J Prim Health Care. 2003;21(1):27–32. doi: 10.1080/0283430310000528. [DOI] [PubMed] [Google Scholar]
- 43.Freeman G, Anwar S, Dalal A, et al. RCGP continuity of care toolkit: helping clinicians and practices maximise relationship continuity. London: RCGP; 2013. [Google Scholar]