Abstract
Study Design
Single-blinded randomized controlled trial.
Purpose
To evaluate the effects of a multi-step core stability exercise program in nurses with chronic low back pain (CLBP).
Overview of Literature
CLBP is a common disorder among nurses. Considering that patient-handling activities predispose nurses to CLBP, core stability exercises suggested for managing CLBP in the general population may also be helpful in nurses. However, sufficient evidence is not available on whether a multi-step core stability exercise program affects pain, disability, quality of life, and the diameter of lateral abdominal muscles in nurses with CLBP.
Methods
In this single-blinded randomized controlled trial, 36 female nurses with CLBP were recruited. The sample was divided into two groups of 18 patients (intervention and control). Nurses in the intervention group performed core stability exercises for 8 weeks, based on a progressive pattern over time. Roland–Morris Disability Questionnaire (RDQ), quality of life (36-item Short Form Health Survey [SF-36]), ultrasound assessment of the diameter of lateral abdominal muscles, and Visual Analog Scale (VAS) score for pain were evaluated in the participants before and after the trial. Sixteen nurses (eight from each group) dropped out of the study, and analysis of covariance was used to compare outcomes for the remaining nurses in the intervention (10 nurses) and control (10 nurses) groups.
Results
The results after the trial showed significant improvements in RDQ, SF-36, and VAS score in the intervention group compared with that in the control group (p <0.005). Furthermore, the ultrasound data showed a significant increase in the left and right muscle diameter of all three abdominal muscles during the abdominal drawing-in maneuver in the intervention group compared with that in the control group (p <0.05).
Conclusions
This study showed that a multi-step core stability exercise program is a helpful treatment option for improving quality of life and reducing disability and pain in female nurses with CLBP.
Keywords: Nurses, Low back pain, Exercise therapy, Quality of life
Introduction
Low back pain (LBP) is the most common musculoskeletal disorder affecting the adult population [1,2]. It has been recognized as one of the leading debilitating conditions worldwide and in 2010, was found to have the highest rate of disability among other musculoskeletal diseases [3]. Furthermore, high economic costs due to productivity losses caused by early retirement or low quality of work are other consequences of LBP [4]. Most people experience LBP in their lives. For approximately one-half of them, the pain is self-limiting, but in about 10%–50% of patients, LBP lasts more than 3 months, which is considered as chronic low back pain (CLBP) [5,6]. The prevalence of LBP is high in healthcare workers, with an annual prevalence of 50%–77% and with the highest overall incidence reported in nurses [7]. Patient-handling activities are considered to be the most significant risk factor for LBP among healthcare workers (odds ratio, 1.6) [8].
Core stability exercises that improve lumbopelvic stability may be included as a part of prevention and clinical rehabilitation for patients with LBP. Core stability exercises include a range of exercise programs with different approaches, having the common goal of improving lumbopelvic and abdominal control. These exercises are designed to enhance the ability of the neuromuscular and motor control systems to prevent spinal injury [9].
A recent meta-analysis demonstrated that in contrast with general exercises, core stability exercises are more effective in short-term pain reduction and physical function improvement in patients with CLBP [10]. Kliziene et al. [11] revealed that core stability exercises increase the cross-sectional area of the lumbar multifidus (LM) in both healthy women and women with CLBP. In addition, Leonard et al. [12] found that lumbopelvic core stability exercises significantly increase the thickness of transversus abdominis (TrA) in patients with CLBP during rest and contraction. However, they did not describe other clinical outcomes, such as quality of life and disability.
Different core stability programs are widely studied as an effective treatment for LBP. Clinicians mainly use two rehabilitation approaches: (1) a motor control approach with exercises affecting local muscles (lumbar and lateral abdominal muscles) and (2) a general exercise approach with exercises for global body muscles [13]. Applying yoga techniques, using a Swiss ball, and exercising in water are some of the many techniques used in core stability exercises [14-16]. An effective approach for performing core stability exercises is a progressive multi-step core stability exercise program. In this program, normal muscle mobility and length are first restored to correct any existing musculoskeletal imbalances. Next, the activation of central core muscles, namely lateral abdominal muscles and LM, is initiated, and advanced exercises on a mat and with a physioball is added based on the tolerance of the patient. Finally, transition to standing position and functional movements completes the protocol, thereby achieving the goal of coordination, strength, and stabilization of the trunk movements instead of strengthening individual muscles [17]. Multi-step core stability exercise programs can be helpful for treating nurses with CLBP; however, to the best of our knowledge, no study has revealed whether such a systematic exercise program can affect the disability, quality of life, and the diameter of the muscles involved in occupations at risk of LBP, such as nursing. Therefore, we implemented a single-blinded randomized controlled trial to study the effects of a multi-step core stability exercise program in nurses with CLBP.
Materials and Methods
1. Participants
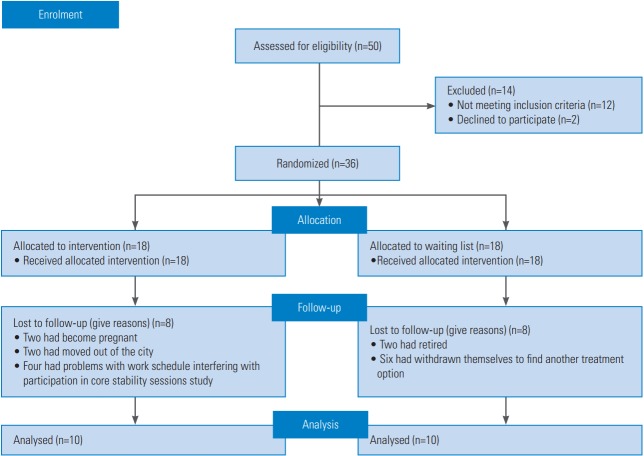
In this single-blinded randomized controlled trial, 36 female nurses with non-specific CLBP who worked in four university hospitals were recruited as volunteers. This sample was divided into two groups of 18 (intervention and control) by computer-generated random lists. The number of participants in each stage and the number of dropouts are provided in study flow diagram (Fig. 1).
Fig. 1.
Flow diagram of the progress through the phases of the study.
The inclusion criteria were as follows: age of 18–55 years; at least 1 year in the nursing profession; nonspecific CLBP for at least 3 months in the past 6 months; pain between the last rib and lower gluteal fold; no history of spinal trauma or spinal or abdominal surgery; no history of systemic disease (e.g., systemic scleroderma or muscular dystrophy), spinal deformity (e.g., scoliosis and kyphosis), or abdominal wall hernia; and no history of participation in core stability exercises in the past 6 months. Exclusion criteria were any signs of serious spinal cord involvement (such as urine or fecal incontinence, numbness, or limb paralysis) and pregnancy. Nurses were assessed by a sports medicine specialist at the Sports Medicine Research Center. Allocations to each group were prepared before the study: the group names were written and concealed in similar-looking packets; at the beginning of the study, each patient was asked to randomly select a packet and was assigned to the specified group. This study was approved by the Ethics Committee of the Tehran University of Medical Sciences (RCT registration no., IRCT138903314231N1), and all participants received written and verbal information about the study and provided written consent.
2. Multi-step core stability exercise protocol
The main goal in this exercise protocol was to restore and maintain the stability of the spine by retraining the main stabilizing muscles of the trunk through multi-step progressive stages. Nurses in the intervention group visited the Sports Medicine Research Centre weekly to learn and perform their specific exercises for the week ahead at home. In each session, participants performed the specific exercises under supervision of a physiotherapist and a written pamphlet with illustrations was provided. Because the Swiss ball plays a substantial role in the activation of trunk muscles [15,18,19], for the 8 weeks of training, two floor exercises and two exercises with a Swiss ball were included in each week.
During the first session, the intervention group was educated about the muscles involved in core stability, their influence on LBP, and the effect of core stability exercises in reducing LBP symptoms and recurrence. In addition, the intervention group was taught movements that emphasized on the activation of central core stability muscles. Participants learned the abdominal drawing-in maneuver (ADiM) and activation of lumbar paraspinal muscles (especially LM), as well as how to maintain them in static (supine and quadruped) positions. In subsequent sessions, muscle activation was combined with other functional movements, and participants learned how to retain the maneuver in dynamic positions (while sitting and moving the limbs in a controlled and slow motion on the floor or on a Swiss ball) and in normal physical actions during the day. Each exercise was performed for three sets (morning, mid-day, and night) with ten repetitions and a ten-second holding position in each repetition. Notably, the exercise protocol (number of repetitions and contraction time) was quite flexible based on the physical ability of each nurse. In addition, the core stability movements had a progressive pattern over time, and new and more complicated movements based on the retention of balance and stability were added in each session. The intensity of exercises was increased based on participants’ tolerance, and movements were avoided if they caused pain. The movements performed in the eight sessions are demonstrated in Appendix 1. Throughout the study, the physiotherapist contacted the participants in the middle of each week and encouraged them to complete their exercises; the phone number of the trial’s administrator was given to the participants for contacting in case of any problems. Meanwhile, the control group was kept on a waiting list and did not receive any instruction about an exercise program for their LBP.
3. Measurements
The demographic characteristics of all participants were collected at the beginning of the study. The Farsi version of Roland–Morris Disability Questionnaire (RDQ) was used to measure disability in all participants at the beginning of the study and 8 weeks later. The questionnaire comprised 24 questions on daily activities, with scores of 0–24 points reported as total score, and was valid and reliable in patients with LBP. Quality of life was estimated before and after the 8 weeks of the trial using the Farsi version of 36-item Short Form Health Survey (SF-36), which contained 36 items classified into eight domains (including physical function, physical role, bodily pain, general health, vitality, social function, emotional role, and mental health). The score of each question was variable from zero (worse state) to one hundred (ideal state). All eight subscales of SF-36 were used for analysis.
The diameters of lateral abdominal muscles, including external oblique (EO), internal oblique (IO), and TrA, were measured on both sides of participants at rest and during ADiM at the beginning of the study and 8 weeks later. While participants laid in a hook-lying position (hips flexed to almost 30°), a point 25 mm antero-medial to the midpoint between the inferior rib and the iliac crest on the mid-axillary line was set for the linear transducer position [20]. Before taking the muscle diameter measurements, participants were trained to perform the ADiM while their contractions were observed using ultrasound biofeedback [21]. The ultrasound assessor had more than three years of experience in the field of musculoskeletal ultrasound assessment and was unaware of study group allocation.
The thickness of lateral abdominal muscles was measured in B-mode format using a Sonosite Miramaxx (Sonosite Inc., Bothell, WA, USA) ultrasound machine. The linear transducer (6–13 MHz) was transversely positioned at the assessment point, which is described above. In addition, to eliminate the confounding effect of food consumption on the thickness of lateral abdominal muscles, all measurements were performed 4 hours after eating [22,23]. Visual Analog Scale (VAS) was used to evaluate the intensity of pain felt by the participants. In this study, VAS was a 100-mm solid horizontal line, with zero at one end considered as no pain and 100 at the other end considered as the most intense pain. RDQ, SF-36, and VAS were completed by all participants before and after the trial.
4. Sample size calculation
The sample size of 18 subjects per group was helpful in detecting a 20-point difference in the VAS between groups, assuming a standard deviation of 11.8, an α level of 0.05, a power of 80%, and a dropout rate of 40% [24,25].
5. Statistics
Descriptive data was presented as mean±standard deviation and number (percentage). The paired sample t-test was used to compare the results after 8 weeks in each group, and analysis of covariance (ANCOVA) was used to compare the results between the groups. Analysis was adjusted for age, weight, and baseline value of each variable. The significance level of this study was set at p<0.05, and IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. Lastly, our statistician was blinded to the study groups.
Results
During the trial, 16 (eight in each group) participants were excluded because they did not attend the training sessions (Fig. 1). Of the eight participants from the intervention group who left the study, two had become pregnant, two had moved out of the city, and four had problems with work schedule interfering with participation in core stability sessions. Of the eight participants from the control group who left the study, two had retired and six had withdrawn themselves to find another treatment option. The basic and demographic data of the participants in each group are presented in Table 1. When using ANCOVA, baseline data was considered as the independent factor and the data after intervention was considered as the dependent factor. The data were adjusted by age, weight, and baseline values.
Table 1.
Basic and demographic data of participants at the study onset
| Characteristic | Intervention group (N=10) | Control group (N=10) | p-value |
|---|---|---|---|
| Age (yr) | 43.3±7.5 | 41.3±6.4 | 0.68 |
| Weight (kg) | 63.3±4.7 | 63.5±5.8 | 0.34 |
| Height (cm) | 162.5±6.9 | 161.5±3.7 | 0.30 |
| Body mass index (kg/m2) | 24.0±1.7 | 24.3±2.1 | 0.54 |
| Pain duration (mo) | 18.2±6.4 | 16.4±5.9 | 0.94 |
Values are presented as mean±standard deviation.
The results showed that the RDQ score decreased significantly in the intervention group compared with that in the control group (p<0.001) (Table 2), indicating that the intervention led to an increase in the functional ability of the nurses. Furthermore, core stability exercises significantly increased the SF-36 questionnaire score in all subcategories (p<0.001), except for emotional role (p=0.405), in the intervention group compared with that in the control group (Table 2). The results of the ultrasound muscle assessment (Table 3) revealed a significant increase in the left and right muscle diameter of all three abdominal muscles during ADiM in the intervention group compared with that in the control group (p<0.05). Lastly, VAS score decreased significantly in the intervention group after the trial (approximately 30 points) (p<0.001), whereas no difference in VAS score was observed in the control group after the trial (Table 2).
Table 2.
Measured variables at the baseline and after the study in each group and comparison within and between groups
| Variable | Intervention group (N=10) |
Control group (N=10) |
Between-group comparisonb) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before study | After study | Within-group comparisona) |
Before study | After study | Within-group comparisona) |
|||||
| CI | p-value | CI | p-value | CI | p-value | |||||
| Current VAS score | 38.4±21.7 | 4.0±5.4 | 19.6 to 49.4 | 0.001* | 36.2±27.2 | 25.2±17.7 | −1.4 to 23.4 | 0.08 | −32.8 to −12.9 | <0.001* |
| VAS score during previous week | 51.8±24.1 | 12.4±13.5 | 22.6 to 56.2 | <0.001* | 44.2±26.5 | 39.4±20.9 | −10.3 to 19.8 | 0.49 | −45.7 to −15.6 | 0.001* |
| RDQ score | 7.8±3.4 | 1.7±2.4 | 3.3 to 8.9 | 0.001* | 9.5±4.9 | 7.9±3.3 | −1.3 to 4.5 | 0.24 | −8.8 to −3.6 | <0.001* |
| Health domain scales of SF-36 | ||||||||||
| Physical functioning | 68.5±14.3 | 86.0±11.5 | −30.5 to −4.5 | 0.014* | 68.0±19.6 | 65.5±19.9 | −5.8 to 10.8 | 0.51 | 9.1 to 33.9 | 0.002* |
| Role-physical | 40.0±29.3 | 95.0±10.5 | −73.5 to −36.5 | <0.001* | 50.0±42.5 | 65.0±41.2 | −40.6 to 10.6 | 0.22 | 11.3 to 60.5 | 0.007* |
| Bodily pain | 52.8±16.4 | 85.6±15.8 | −44.9 to −20.1 | <0.001* | 55.0±23.3 | 59.0±15.0 | −18.0 to 10.0 | 0.54 | 16.6 to 41.1 | <0.001* |
| General health | 69.5±14.6 | 83.0±6.7 | −25.9 to −1.8 | 0.028* | 54.5±25.1 | 57.5±22.7 | −15.4 to 9.4 | 0.59 | 8.1 to 30.9 | 0.002* |
| Vitality | 45.5±13.2 | 72.5±13.6 | −41.4 to −12.6 | 0.002* | 49.8±14.7 | 51.5±21.2 | −18.2 to 14.7 | 0.82 | 4.9 to 40.8 | 0.016* |
| Social functioning | 56.3±13.5 | 82.5±21.4 | −42.8 to −9.7 | 0.006* | 68.8±20.6 | 62.5±22.0 | −10.2 to 22.7 | 0.41 | 2.8 to 48.9 | 0.03* |
| Role-emotional | 40.0±40.9 | 66.7±47.1 | −68.4 to 15.1 | 0.18 | 83.3±28.3 | 60.0±40.9 | −6.5 to 53.2 | 0.11 | −32.1 to 75.3 | 0.41 |
| Mental health | 66.4±16.6 | 80.4±15.7 | −24.2 to −3.8 | 0.013* | 68.4±15.6 | 64.4±11.8 | −4.2 to 12.2 | 0.30 | 9.8 to 28.2 | 0.001* |
Values are presented as mean±standard deviation or CI, unless otherwise stated.
CI, confidence interval; VAS, Visual Analog Scale; RDQ, Roland–Morris Disability Questionnaire; SF-36, 36-item Short Form Health Survey.
p<0.05 (statistically significant).
Paired sample t-test for comparing data obtained before and after the study in each group.
Analysis of covariance of each variable, which is adjusted for age, weight, and its baseline value.
Table 3.
Ultrasound measurements at the baseline and after the study in each group and comparison within and between groups
| Muscles | Side of muscle | Intervention group (N=10) |
Control group (N=10) |
Between-group comparisonb) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before study | After study | Within group comparisona) |
Before study | After study | Within group comparisona) |
||||||
| CI | p-value | CI | p-value | CI | p-value | ||||||
| During rest | |||||||||||
| EO (mm) | Right | 4.3±1.3 | 4.4±1.3 | −0.1 to 0.03 | 0.18 | 4.4±1.4 | 4.4±1.3 | −0.1 to 0.2 | 0.93 | −0.05 to 0.18 | 0.26 |
| Left | 4.4±1.3 | 4.4±1.4 | −0.1 to 0.2 | 0.70 | 4.4±1.3 | 4.4±1.3 | −0.2 to 0.07 | 0.44 | −0.25 to 0.15 | 0.59 | |
| IO (mm) | Right | 4.9±1.5 | 4.9±1.5 | −0.08 to 0.1 | 0.81 | 4.9±1.6 | 4.9±1.7 | −0.1 to 0.04 | 0.24 | −0.19 to 0.07 | 0.30 |
| Left | 4.8±1.6 | 4.8±1.5 | −0.2 to 0.1 | 0.57 | 4.8±1.5 | 4.9±1.7 | −0.2 to 0.08 | 0.34 | −0.25 to 0.19 | 0.78 | |
| TrA (mm) | Right | 2.4±0.8 | 2.4±0.8 | −0.2 to 0.16 | 0.89 | 2.3±0.8 | 2.2±0.8 | −0.02 to 0.2 | 0.09 | −0.07 to 0.29 | 0.23 |
| Left | 2.4±0.9 | 2.3±0.8 | −0.05 to 0.3 | 0.12 | 2.3±0.7 | 2.3±0.8 | −0.09 to 0.08 | 0.95 | −0.33 to 0.04 | 0.12 | |
| During ADiM | |||||||||||
| EO (mm) | Right | 5.1±1.5 | 5.9±1.7 | −1.1 to −0.5 | <0.001* | 5.1±1.7 | 5.1±1.6 | −0.09 to 0.08 | 0.96 | 0.57 to 01.06 | <0.001* |
| Left | 5.1±1.6 | 6.0±1.8 | −1.0 to −0.6 | <0.001* | 5.0±1.6 | 5.1±1.5 | −0.17 to 0.001 | 0.07 | 0.47 to 1.02 | <0.001* | |
| IO (mm) | Right | 5.7±1.6 | 6.2±1.5 | −0.8 to −0.2 | 0.002* | 5.9±1.8 | 5.9±1.7 | −0.07 to 0.06 | 0.94 | 0.22 to 0.72 | 0.001* |
| Left | 5.7±1.5 | 6.3±1.4 | −0.9 to −0.3 | 0.003* | 5.8±1.7 | 5.8±1.8 | −0.18 to 0.002 | 0.06 | 0.13 to 0.75 | 0.009* | |
| TrA (mm) | Right | 2.9±0.7 | 3.5±0.9 | −0.7 to −0.4 | <0.001* | 2.9±0.8 | 3.0±0.8 | −0.05 to 0.1 | 0.43 | 0.39 to 0.82 | <0.001* |
| Left | 3.0±0.7 | 3.5±0.8 | −0.8 to −0.4 | <0.001* | 3.1±0.8 | 3.1±0.7 | −0.12 to 0.1 | 0.97 | 0.35 to 0.81 | <0.001* | |
Values are presented as mean±standard deviation or CI, unless otherwise stated.
CI, confidence interval; EO, external oblique; IO, internal oblique; TrA, transversus abdominis; ADiM, abdominal drawing-in maneuver.
p<0.05 (statistically significant).
Paired sample t-test for comparing data obtained before and after the study in each group.
Analysis of covariance analysis of each variable, which is adjusted for age, weight, and its baseline value.
Discussion
Findings of this study revealed that core stability exercises can be effective in managing CLBP in female nurses. Over the 8 weeks of training, functional ability, quality of life, and VAS score improved in the intervention group compared with those in the control group. Furthermore, the ultrasound muscle assessment confirmed the improvement of muscle function by demonstrating a significant increase in muscle diameter during ADiM in the intervention group compared with that in the control group. However, limitations of the study should be considered during interpretation and generalization of results.
Patient-handling activities and lack of appropriate exercises in the routine schedule are suggested as risk factors for LBP in nurses [26]. The main proposed mechanism of exercise therapy in the management of LBP involves the improvement of neuromuscular function and augmentation of the muscles that control and support the spine and pelvis [9]. Moreover, specific exercises, such as core stability exercises, could be effective in retraining the trunk muscles, which have a vital role in the stabilization, coordination, and control of the spine [9].
1. Exercise protocol
In this study, we assessed the effectiveness of a multi-step core stability protocol based on three goals: (1) learning how to activate central core stability muscles and coactivating these muscles during other movements, (2) increasing the intensity of exercises based on tolerance and ability of each patient, and (3) integrating exercises into functional movements, dynamic positions, unstable surfaces, and daily physical motions. In the study by Koumantakis et al. [27], patients with recurrent LBP underwent 8 weeks of trunk muscle stabilization training. Similarly, their protocol included the activation of local stabilizing muscles and integration of this activation with dynamic functional movements. However, the study protocol was not as comprehensive as ours in terms of the application to unstable surfaces, verity, and volume of training. In another study by Norris and Matthews [24], patients with CLBP underwent a 6-week integrated back stability program consisting of optimizing posture, back fitness, and functional exercises. Although their protocol was comprehensive, they did not provide any information regarding application to unstable surfaces or illustration of exact movements. Other studies have also not provided details of exercise protocols or the utilization of unstable surfaces and have conducted only supervised sessions without home exercises [11,28-33]. Variations between these exercise protocols could be an explanation for different results.
2. Disability
The average RDQ score showed that the disability index decreased significantly in the intervention group compared with that in the control group. In addition, the change in RDQ scores (6.1) in the intervention group was >5, which is considered as the minimum clinically important difference (MCID) [25]. Koumantakis et al. [27] found improvement of approximately 4.65 units in RDQ scores in patients with recurrent LBP who performed 20 weeks of stabilization-enhanced exercise. In a separate study, Shaughnessy and Caulfield [31] provided a 10-week core stability exercise program to 41 volunteers with CLBP who had been referred to an orthopedic clinic. In the intervention group, the RDQ score decreased by 5 scores, which was significant. In addition, Bayraktar et al. [16] revealed that patients with CLBP who participated in land- and water-based core stability exercises reported improvement of 5 and 4.5 units in RDQ scores, respectively. As discussed above, most studies have demonstrated the effectiveness of core stability exercises in the amelioration of disability. The possible explanations for these findings are improvement of trunk muscles activity and an increase in the lumbar range of motion, which lead to reduced disability and functional recovery. However, it seems that the discrepancy between levels of improvement could be related to different exercises protocols.
3. Quality of life
The overall quality of life (SF-36 score) in participants in the intervention group improved significantly compared with that in the control group. Based on the consideration of 30% improvement as a threshold for MCID, most of the SF-36 domain scores meet this threshold. In agreement with our results, Bayraktar et al. [16] showed that healthrelated quality of life, which was measured by Nottingham Health Profile, improved in patients with CLBP due to lumbar disc herniation in both water- and land-based core stability exercise groups. Further, Ota et al. [32] reported improvement in quality of life, based on Japanese Orthopedic Association Back Pain Evaluation Questionnaire, after 3 and 6 months of lumbar stabilization exercises in patients with CLBP. The only factor that was not affected by core stability exercises in the present study was the emotional role. Emotional disorders have mainly multifactorial roots, and in nurses, working factors, such as job stress, health behavior, and work environment, may affect emotional status more than physical complications. However, Shaughnessy and Caulfield [31] and Ota et al. [32] illustrated that core stability exercises improve the emotional aspect of quality of life in patients with CLBP; these findings could be due to a longer study duration and more interactions between patients and their exercise instructors.
4. Pain
The amelioration of LBP was indicated by a significant decrease in the VAS score in the intervention group after the trial, whereas no such difference was observed in the control group. In addition, the VAS mean difference in the intervention group (approximately 30 points from 100) meets the criteria for MCID (15 points) [25]. Koumantakis et al. [27] revealed that in their patients, after 8 weeks of core stability training, mean pain intensity over the past week and past month decreased by approximately 18 points (from 100) and 28 points (from 100), respectively. In addition, Norris et al. demonstrated a 39-point (from 100) reduction in the VAS score, based on McGill pain questionnaire, after 6 weeks of integrated back stability program [24]. Zhang et al. [33] used a randomized controlled trial to evaluate the combination of Chinese massage and core stability exercises in patients with nonspecific LBP and obtained similar results. Their results showed that after eight weeks of intervention, the VAS score significantly decreased (approximately 6 points from 10) in the intervention group compared with that in the control group (approximately 4.5 points from 10). Most of these studies met the criteria for MCID in showing that stabilization exercises could diminish pain intensity. The increase in tissue blood flow during lumbar stabilization exercise in patients with chronic non-specific LBP [34] could be suggested as an integrated mechanism for releasing spasm, improving blood flow, and decreasing the inflammation of local tissues in the lumbar spine, which in return reduced pain.
5. Thickness of lateral abdominal muscles
Another focus of our study was the trunk muscles involved in CLBP. The ultrasound data showed that the thickness of the lateral abdominal muscles (EO, IO, and TrA) in ADiM increased significantly in the intervention group compared with that in the control group. Previous studies have shown an alteration in lateral abdominal muscle activity, particularly TrA activity, in patients with CLBP [9,35]. Because the deep abdominal muscles are used in postural control and lumbopelvic coordination, anticipating their role in the clinical outcomes of LBP seems logical. However, the inconsistency among the findings of previous studies may be related to the multifactorial aspects of etiology of and treatments for LBP [36]. Vasseljen and Fladmark [37] showed no significant changes in resting thickness of lateral abdominal muscles and their contraction thickness ratio during ADiM after 8 weeks of ADiM exercises and their implementation in daily living activities in patients with CLBP. However, Kim et al. [38] demonstrated that increasing the intensity during graded stabilization exercises also significantly increases the activity of the related lumbar stabilizing muscles (including EO), which could be considered for future graded core stability protocols. As they suggested, our exercise protocol intensity progressively increased to match the ability of our participants. In addition, Mannion et al. [20] demonstrated that after 9 weeks of spinal segmental stabilization exercises in patients with CLBP, the voluntarily activation of the TrA increased significantly, but its contraction ratio or recruitment showed no significant relationship with disability scores (clinical outcomes). Lastly, Ferreira et al. [39] demonstrated that patients with CLBP who received 8 weeks of exercise to improve the control of lumbopelvic movements and stability showed a greater improvement in the recruitment of the TrA [39]; this finding is consistent with our study results. In our study, the lack of change in muscle thickness at rest was anticipated due to the short length of the intervention; however, improvement in muscle performance during ADiM was observed after eight weeks of exercise.
6. Strengths and limitations
There are some clinical implications for the current findings. The multi-step core stability exercise program could be applied to all healthcare workers, especially those with nursing responsibilities in hospitals, clinics, schools, and institutions. Furthermore, nursing students could be educated to use these exercises to prevent LBP during their career.
Several limitations for the present study should be addressed, including the small sample size, notable loss to follow-up, and the short duration of the intervention, any of which may have influenced the results. All study participants in our study were females, which limits the generalization of the results to male nurses. The ultrasonography assessment was only conducted in the hooklying position, although it could have shown significant improvement in functional positions. Lastly, the control group in our study received no intervention and was on a waiting list. Some of them left the waiting list and could not be contacted; however, we considered intention-totreat analysis for who had remained on the list, and they received the multi-step core stability exercise program immediately after the completion of the study.
Conclusions
This study showed that a multi-step core stability exercise program can improve the quality of life and reduce disability and pain in female nurses with CLBP. However, study limitations should be considered during interpretation and generalization of the results. For future research, long-term studies with larger sample sizes can be planned to examine the effectiveness of our approach in various study groups at risk of LBP. Using assessment techniques other than ultrasonography, such as electromyography, may give more precise results. Moreover, the benefits of multi-step core stability exercises should be compared with those of other treatment interventions in future studies.
Acknowledgments
This research was supported by Tehran University of Medical Sciences & Health Services grant (88-03-30-9316). The authors thank Dr. Mahboubeh Ghayour Najafabadi (Department of Physical Education and Sport Sciences, University of Tehran) for her competent assistance during the study.
Appendix 1. Multi-step core stability exercise protocol
| Session 1 (first week): | |||
|---|---|---|---|
| 1 | A: | Lie on your back while your knees are bent. |  |
| B: | Hold drawing-in maneuver for 10 seconds. | ||
| C: | Rest. | ||
| D: | Repeat 10 times. | ||
| 2 | A: | Stay on your hands and knees. |  |
| B: | Hold drawing-in maneuver for 10 seconds while keeping the natural posture of your back and contracting lumbar paraspinal muscles. | ||
| C: | Loosen your muscles. | ||
| D: | Repeat 10 times. | ||
| 3 | A: | Sit on the Swiss ball. |  |
| B: | Try to keep your balance. | ||
| C: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction for 10 seconds while keeping your back straight. | ||
| C: | Loosen your muscles. | ||
| D: | Repeat 10 times. | ||
| 4 | A: | Sit on the Swiss ball while your knees are bent and your back is straight and your arms are away from your body sides. |  |
| B: | Bring one leg up and hold it up for 10 seconds while performing drawing-in maneuver and contracting lumbar paraspinal muscles. | ||
| C: | Bring your leg down and repeat with the other leg. | ||
| D: | Repeat 10 times. | ||
| Session 2 (second week): | |||
| 1 | A: | Stand. |  |
| B: | Hold drawing-in maneuver and contract lumbar paraspinal muscles during walking. | ||
| C: | Walk 20 minutes per day. | ||
| D: | If you can after a few minutes, perform jogging. | ||
| 2 | A: | Hold drawing-in maneuver and contract lumbar paraspinal muscles during daily activities. | Daily activities |
| 3 | A: | Sit on the Swiss ball. |  |
| B: | Try to keep your balance. | ||
| C: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction for 10 seconds while keeping your back straight. Then lift one of your arms. Hold it for 10 second. | ||
| C: | Loosen your muscles. | ||
| D: | Repeat 10 times. | ||
| E: | Repeat for the other side. | ||
| 4 | A: | Sit on the Swiss ball. |  |
| B: | Try to keep your balance. | ||
| C: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction for 10 seconds while keeping your back straight. Then lift both of your arms. Hold it for 10 second. | ||
| C: | Loosen your muscles. | ||
| D: | Repeat 10 times. | ||
| Session 3 (third week): | |||
| 1 | A: | lie on your back while your knees are bent. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while lifting your buttocks off the floor. Hold it for 10 seconds. | ||
| C: | Rest. | ||
| D: | Repeat 10 times. | ||
| 2 | A: | lie on your back while your knees are bent. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while lifting your buttocks off the floor. Then extend one of your knees. Hold it for 10 seconds. | ||
| C: | Rest. Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| 3 | A: | Sit on the Swiss ball while your knees are bent and your back is straight. |  |
| B: | Bring left leg and right arm up. Hold it up for 10 seconds while performing drawing-in maneuver and contracting lumbar paraspinal muscles. | ||
| C: | Bring your leg and arm down and repeat with the other side. | ||
| D: | Repeat 10 times. | ||
| 4 | A: | Sit on the Swiss ball while your knees are bent and your back is straight. |  |
| B: | Bring left leg and left arm up. Hold it up for 10 seconds while performing drawing-in maneuver and contracting lumbar paraspinal muscles. | ||
| C: | Bring your leg and arm down and repeat with the other side. | ||
| D: | Repeat 10 times. | ||
| Session 4 (forth week): | |||
| 1 | A: | Stay on your hands and knees. |  |
| B: | Hold drawing-in maneuver for 10 seconds while keeping the natural posture of your back and contracting lumbar paraspinal muscles. | ||
| C: | Extend your left leg and right arm. Hold it for 10 second. | ||
| D: | Rest. Repeat it for the other side. E: Repeat 10 times. | ||
| 2 | A: | lie on your side while your knees are extended. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while raising your buttocks off the floor until trunk, back, and knees become in a line. Hold it for 10 seconds. | ||
| C: | Rest. Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| 3 | A: | Sit on the Swiss ball while your knees are bent and your back is straight. |  |
| B: | Tilt your pelvis side to side and rotate it clockwise and counterclockwise while performing drawing-in maneuver and contracting lumbar paraspinal muscles. | ||
| C: | Back to the start position. | ||
| D: | Repeat 10 times. | ||
| 4 | A: | Sit on the Swiss ball while your knees are bent and your back is straight. |  |
| B: | Tilt your pelvis front to the back and vice versa while performing drawing-in maneuver and contracting lumbar paraspinal muscles. | ||
| C: | Back to the start position. | ||
| D: | Repeat 10 times. | ||
| Session 5 (fifth week): | |||
| 1 | A: | lie on your back while your knees are bent. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while lifting your left arm and right leg off the floor. Hold it for 10 seconds. | ||
| C: | Rest. Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| 2 | A: | lie on your back while your knees are 90–90 and your arms are over the head. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while moving right elbow to left knee and straightening right knee. | ||
| C: | Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| 3 | A: | Sit on the Swiss ball while your knees are bent and your back is straight. |  |
| B: | Walk forward until leaning on ball and your body become straight and parallel to the floor, while performing drawing-in maneuver and contracting lumbar paraspinal muscles. Hold it up for 10 seconds. | ||
| C: | Back to the start position. | ||
| D: | Repeat 10 times. | ||
| 4 | A: | Sit on the Swiss ball while your knees are bent and your back is straight. |  |
| B: | Walk forward until leaning on ball and your body become straight and parallel to the floor, while performing drawing-in maneuver and contracting lumbar paraspinal muscles. Then lift your arms over the head and rock side to side on the ball. | ||
| C: | Back to the start position. | ||
| D: | Repeat 10 times. | ||
| Session 6 (sixth week): | |||
| 1 | A: | lie on your belly while your body is straight. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while lifting your head and legs off the floor. Hold it for 10 seconds. | ||
| C: | Rest. | ||
| D: | Repeat 10 times. | ||
| 2 | A: | lie on your back while your knees are 90–90. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while rotating legs from right to left. | ||
| C: | Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| 3 | A: | Put your belly on the Swiss ball while your knees are bent and your toes touch the wall. |  |
| B: | Straighten your body by straightening knees and arms over the head, while performing drawing-in maneuver and contracting lumbar paraspinal muscles. Hold it up for 10 seconds. | ||
| C: | Back to the start position. | ||
| D: | Repeat 10 times. | ||
| 4 | A: | Put your belly on the Swiss ball while your knees are bent and your hands touch the floor. |  |
| B: | Raise the right leg and the left arm, while performing drawing-in maneuver and contracting lumbar paraspinal muscles. Hold it up for 10 seconds. | ||
| C: | Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| Session 7 (seventh week): | |||
| 1 | A: | Stand on your legs while your body is straight. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while lifting one of your legs off the floor. Hold it for 10 seconds. | ||
| C: | Rest. | ||
| D: | Repeat 10 times. | ||
| 2 | A: | Stand on your legs while your body is straight. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while lifting your right leg off the floor. Then bend the left knee slightly and reach your right arm in front of your body. Hold it for 10 seconds. | ||
| C: | Rest. Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| 3 | A: | Stand on your legs while your body is straight and a ball is between your back and wall. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while slowly bending knees. Hold it for 10 seconds. | ||
| C: | Rest. | ||
| D: | Repeat 10 times. | ||
| 4 | A: | Lie on your back while putting your legs on the Swiss ball. |  |
| B: | Lift your buttocks off the floor, while performing drawing-in maneuver and contracting lumbar paraspinal muscles. Hold it up for 10 seconds. | ||
| C: | Back to the start position. | ||
| D: | Repeat 10 times. | ||
| Session 8 (eighth week): | |||
| 1 | A: | Stand on your legs while your body is straight. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while stepping backward with left leg into the lunge position. Hold it for 10 seconds. | ||
| C: | Rest. Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| 2 | A: | Stand on your legs while your body is straight. |  |
| B: | Hold drawing-in maneuver and lumbar paraspinal muscles contraction while stepping backward with left leg into the lunge position. Then lift your left leg off the floor and reach your arms in front of your body. Hold it for 10 seconds. | ||
| C: | Rest. Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| 3 | A: | Put your side on the Swiss ball while your upper body is supported on the. |  |
| B: | Straighten your body by lifting buttock upward and straightening knees, while performing drawing-in maneuver and contracting lumbar paraspinal muscles. Hold it up for 10 seconds. Back to the start position. | ||
| C: | Repeat it for the other side. | ||
| D: | Repeat 10 times. | ||
| 4 | A: | Put your legs on the Swiss ball while your hands are on the floor. |  |
| B: | Keep your body straight and do push up, while performing drawing-in maneuver and contracting lumbar paraspinal muscles. | ||
| C: | Back to the start position. | ||
| D: | Repeat 10 times. | ||
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24:769–81. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Noormohammadpour P, Mansournia MA, Asadi-Lari M, Nourian R, Rostami M, Kordi R. A subtle threat to urban populations in developing countries: low back pain and its related risk factors. Spine (Phila Pa 1976) 2016;41:618–27. doi: 10.1097/BRS.0000000000001269. [DOI] [PubMed] [Google Scholar]
- 3.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–96. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8:8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Itz CJ, Geurts JW, van Kleef M, Nelemans P. Clinical course of non-specific low back pain: a systematic review of prospective cohort studies set in primary care. Eur J Pain. 2013;17:5–15. doi: 10.1002/j.1532-2149.2012.00170.x. [DOI] [PubMed] [Google Scholar]
- 6.Noormohammadpour P, Mansournia MA, Koohpayehzadeh J, et al. Prevalence of chronic neck pain, low back pain, and knee pain and their related factors in community-dwelling adults in Iran: a population-based national study. Clin J Pain. 2017;33:181–7. doi: 10.1097/AJP.0000000000000396. [DOI] [PubMed] [Google Scholar]
- 7.Karahan A, Kav S, Abbasoglu A, Dogan N. Low back pain: prevalence and associated risk factors among hospital staff. J Adv Nurs. 2009;65:516–24. doi: 10.1111/j.1365-2648.2008.04905.x. [DOI] [PubMed] [Google Scholar]
- 8.Holtermann A, Clausen T, Jorgensen MB, Burdorf A, Andersen LL. Patient handling and risk for developing persistent low-back pain among female healthcare workers. Scand J Work Environ Health. 2013;39:164–9. doi: 10.5271/sjweh.3329. [DOI] [PubMed] [Google Scholar]
- 9.Hodges PW. Core stability exercise in chronic low back pain. Orthop Clin North Am. 2003;34:245–54. doi: 10.1016/s0030-5898(03)00003-8. [DOI] [PubMed] [Google Scholar]
- 10.Wang XQ, Zheng JJ, Yu ZW, et al. A meta-analysis of core stability exercise versus general exercise for chronic low back pain. PLoS One. 2012;7:e52082. doi: 10.1371/journal.pone.0052082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kliziene I, Sipaviciene S, Klizas S, Imbrasiene D. Effects of core stability exercises on multifidus muscles in healthy women and women with chronic low-back pain. J Back Musculoskelet Rehabil. 2015;28:841–7. doi: 10.3233/BMR-150596. [DOI] [PubMed] [Google Scholar]
- 12.Leonard JH, Paungmali A, Sitilertpisan P, Pirunsan U, Uthaikhup S. Changes in transversus abdominis muscle thickness after lumbo-pelvic core stabilization training among chronic low back pain individuals. Clin Ter. 2015;166:e312–6. doi: 10.7417/T.2015.1884. [DOI] [PubMed] [Google Scholar]
- 13.Brumitt J, Matheson JW, Meira EP. Core stabilization exercise prescription, part I: current concepts in assessment and intervention. Sports Health. 2013;5:504–9. doi: 10.1177/1941738113502451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Omkar SN, Vishwas S, Tech B. Yoga techniques as a means of core stability training. J Bodyw Mov Ther. 2009;13:98–103. doi: 10.1016/j.jbmt.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 15.Marshall PW, Murphy BA. Core stability exercises on and off a Swiss ball. Arch Phys Med Rehabil. 2005;86:242–9. doi: 10.1016/j.apmr.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 16.Bayraktar D, Guclu-Gunduz A, Lambeck J, Yazici G, Aykol S, Demirci H. A comparison of water-based and land-based core stability exercises in patients with lumbar disc herniation: a pilot study. Disabil Rehabil. 2016;38:1163–71. doi: 10.3109/09638288.2015.1075608. [DOI] [PubMed] [Google Scholar]
- 17.Akuthota V, Ferreiro A, Moore T, Fredericson M. Core stability exercise principles. Curr Sports Med Rep. 2008;7:39–44. doi: 10.1097/01.CSMR.0000308663.13278.69. [DOI] [PubMed] [Google Scholar]
- 18.Czaprowski D, Afeltowicz A, Gebicka A, et al. Abdominal muscle EMG-activity during bridge exercises on stable and unstable surfaces. Phys Ther Sport. 2014;15:162–8. doi: 10.1016/j.ptsp.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Wilk BR, Stenback JT, Gonzalez C, Jagessar C, Nau S, Muniz A. Core muscle activation during Swiss ball and traditional abdominal exercises. J Orthop Sports Phys Ther. 2010;40:538–9. [PubMed] [Google Scholar]
- 20.Mannion AF, Pulkovski N, Toma V, Sprott H. Abdominal muscle size and symmetry at rest and during abdominal hollowing exercises in healthy control subjects. J Anat. 2008;213:173–82. doi: 10.1111/j.1469-7580.2008.00946.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rostami M, Noormohammadpour P, Sadeghian AH, Mansournia MA, Kordi R. The effect of lumbar support on the ultrasound measurements of trunk muscles: a single-blinded randomized controlled trial. PM R. 2014;6:302–8. doi: 10.1016/j.pmrj.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 22.Kordi R, Rostami M, Noormohammadpour P, Mansournia MA. The effect of food consumption on the thickness of abdominal muscles, employing ultrasound measurements. Eur Spine J. 2011;20:1312–7. doi: 10.1007/s00586-011-1708-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noormohammadpour P, Ansari M, Mansournia MA, Rostami M, Nourian R, Kordi R. Reversal time of postprandial changes of the thickness of abdominal muscles employing ultrasound measurements. Man Ther. 2015;20:194–9. doi: 10.1016/j.math.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 24.Norris C, Matthews M. The role of an integrated back stability program in patients with chronic low back pain. Complement Ther Clin Pract. 2008;14:255–63. doi: 10.1016/j.ctcp.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 25.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976) 2008;33:90–4. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 26.Sopajareeya C, Viwatwongkasem C, Lapvongwatana P, Hong O, Kalampakorn S. Prevalence and risk factors of low back pain among nurses in a Thai public hospital. J Med Assoc Thai. 2009;92 Suppl 7:S93–9. [PubMed] [Google Scholar]
- 27.Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. 2005;85:209–25. [PubMed] [Google Scholar]
- 28.Franca FR, Burke TN, Caffaro RR, Ramos LA, Marques AP. Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. J Manipulative Physiol Ther. 2012;35:279–85. doi: 10.1016/j.jmpt.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 29.Rhee HS, Kim YH, Sung PS. A randomized controlled trial to determine the effect of spinal stabilization exercise intervention based on pain level and standing balance differences in patients with low back pain. Med Sci Monit. 2012;18:CR174–81. doi: 10.12659/MSM.882522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andrusaitis SF, Brech GC, Vitale GF, Greve JM. Trunk stabilization among women with chronic lower back pain: a randomized, controlled, and blinded pilot study. Clinics (Sao Paulo) 2011;66:1645–50. doi: 10.1590/S1807-59322011000900024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shaughnessy M, Caulfield B. A pilot study to investigate the effect of lumbar stabilisation exercise training on functional ability and quality of life in patients with chronic low back pain. Int J Rehabil Res. 2004;27:297–301. doi: 10.1097/00004356-200412000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Ota M, Kaneoka K, Hangai M, Koizumi K, Muramatsu T. Effectiveness of lumbar stabilization exercises for reducing chronic low back pain and improving quality-of-life. J Phys Ther Sci. 2011;23:679–81. [Google Scholar]
- 33.Zhang Y, Tang S, Chen G, Liu Y. Chinese massage combined with core stability exercises for nonspecific low back pain: a randomized controlled trial. Complement Ther Med. 2015;23:1–6. doi: 10.1016/j.ctim.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Paungmali A, Henry LJ, Sitilertpisan P, Pirunsan U, Uthaikhup S. Improvements in tissue blood flow and lumbopelvic stability after lumbopelvic core stabilization training in patients with chronic non-specific low back pain. J Phys Ther Sci. 2016;28:635–40. doi: 10.1589/jpts.28.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferreira PH, Ferreira ML, Hodges PW. Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine (Phila Pa 1976) 2004;29:2560–6. doi: 10.1097/01.brs.0000144410.89182.f9. [DOI] [PubMed] [Google Scholar]
- 36.Wong AY, Parent EC, Funabashi M, Kawchuk GN. Do changes in transversus abdominis and lumbar multifidus during conservative treatment explain changes in clinical outcomes related to nonspecific low back pain?: a systematic review. J Pain. 2014;15:377. doi: 10.1016/j.jpain.2013.10.008. e1-35. [DOI] [PubMed] [Google Scholar]
- 37.Vasseljen O, Fladmark AM. Abdominal muscle contraction thickness and function after specific and general exercises: a randomized controlled trial in chronic low back pain patients. Man Ther. 2010;15:482–9. doi: 10.1016/j.math.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 38.Kim CR, Park DK, Lee ST, Ryu JS. Electromyographic changes in trunk muscles during graded lumbar stabilization exercises. PM R. 2016;8:979–89. doi: 10.1016/j.pmrj.2016.05.017. [DOI] [PubMed] [Google Scholar]
- 39.Ferreira PH, Ferreira ML, Maher CG, Refshauge K, Herbert RD, Hodges PW. Changes in recruitment of transversus abdominis correlate with disability in people with chronic low back pain. Br J Sports Med Please add. 2010;44:1166–72. doi: 10.1136/bjsm.2009.061515. [DOI] [PubMed] [Google Scholar]