Abstract
Reproductive decision making is complex and personal. Having a child with undiagnosed developmental delay can further complicate these decisions, as recurrence risks are unknown. This qualitative study is an exploration of the experiences of parents who have a child with an undiagnosed developmental disorder, focusing on their reproductive decisions. The aims of the research were to explore the reproductive decision making process and examine the factors that influence these decisions. Data were collected from in-depth semi-structured interviews with five mothers of children without a diagnosis. Transcripts were analysed using an interpretative phenomenological analysis. Analysis identified five factors that were considered by participants when contemplating reproductive decisions: future uncertainty, perceptions of risk, the potential impact a child would have on their current children, expectations of a family and the desire for another child. Being aware of the factors that influence reproductive decisions for these mothers and being sensitive to them can enable genetic counsellors to carry out their role more effectively, as they are aware of the factors that need to be discussed and explored before a decision is made.
Keywords: Developmental delay, Reproductive decisions, Diagnosis, Undiagnosed, Genetic counselling
Introduction
Even with the most recent advances in genetic technologies, a large proportion of children with developmental delay do not have a molecular diagnosis (Lionel et al. 2017). Whilst clinical diagnoses may be given to the individual symptoms, the lack of identification of a genetic mutation means that there is no causal explanation for the child’s condition, no recurrence risk for future pregnancies and no prediction for what the future may hold for the child’s health. The experience of living without a diagnosis has been explored previously (Graungaard and Skov 2006; Lewis et al. 2010; Makela et al. 2009; McLaughlin et al. 2011; Rosenthal et al. 2001) and a recurring issue that these studies have raised is that without a diagnosis reproductive choices are restricted. There is a risk that future children may also have the same condition; however, this risk cannot be given in terms of probability because the genetic mutation has not been identified. Therefore, it is not possible to predict whether this mutation has been inherited from one or both of the parents, or whether it occurred in the child during fertilisation (this is known as a de novo mutation). Without a genetic diagnosis, reproductive options are limited, as genetic testing cannot be offered.
Literature review
Living without a diagnosis
A diagnosis is thought to help with coping, after the birth of a disabled child. Graungaard and Skov (2006) found that the search for a diagnosis and thus a prognosis is driven by a need to know what the future may hold for their child. There is a hope that a diagnosis will provide further treatment options so that parents can actively help their child and being able to help greatly reduced the emotional stress related to having a child with disabilities. Parents can find it difficult to accept that their child’s coexisting symptoms suggest a permanent condition when their child does not have a diagnosis (Graungaard and Skov 2006). Future uncertainty can leave parents feeling out of control of their situation, unable to plan for their future and feeling unprepared to handle what it may bring. This can lead to emotional issues that persist over time particularly relating to the uncertainty of the future for their child and the recurrence risk in future pregnancies (Lewis et al. 2010). High levels of anxiety and stress in parents were reported in a study by McLaughlin et al. (2011) due to the lack of options to inform and support the decisions made in regard to their undiagnosed child, their siblings and future reproductive choices. However, a diagnosis is not seen as a positive for all parents. For some parents, a sense of guilt and responsibility is felt as they come to terms with the inheritance (Kay and Kingston 2002; McLaughlin et al. 2011).
Social reasons for wanting a diagnosis have also been identified (Lewis et al. 2010; McLaughlin et al. 2011; Rosenthal et al. 2001). A diagnosis provides validation and acceptance of the condition and criticism of bad parenting can be dismissed when an etiological cause for challenging behavioural issues is given, providing parents with some emotional relief (Makela et al. 2009). Access to help and support is more readily available when a diagnosis is recognised with some services withholding support until a diagnosis is made (Rosenthal et al. 2001). Parents report feeling isolated and alone, as their child does not fit into a known support group (Lewis et al. 2012).
Reproductive decision making
The reproductive decisions that people make in circumstances of genetic risk are complex and emotional. Many couples do not ever reach a firm decision, and the decisions that are made may change over time. Factors that influence these decisions include risk information and perceived risk (Lee et al. 2013), social context (Decruyenaere et al. 2007), personal experiences of the genetic condition (Donnelly et al. 2013; Peters et al. 2002) and the uncontrollable desire for a child (Decruyenaere et al. 2007; Myring et al. 2011).
Risk is one of the main deciding factors, cited as influencing the reproductive decisions of those at genetic risk. However, it is not just the risk itself but the individual’s perception of the risk. Lee et al. (2013) found that of a group of women with a diagnosis of epilepsy, 25% decided to have fewer children and this decision was found to be associated with an amplified perception of the risk of their child developing the condition. When a diagnosis is unknown, a risk figure of recurrence cannot be given.
Personal experience of a disorder has also been shown to influence reproductive decisions, as shown in a study carried out by Peters et al. (2002), in which participants that had a family history of Marfan syndrome or had suffered an aortic dissection due to the disorder were less likely to have children. Similar results were obtained from a study by Donnelly et al. (2013), in which women who had a positive test result for a BRCA1 or BRCA2 mutation used their values and personal experiences of the disease to weigh up the negative aspects of the cancer predisposition versus the positive motives of having a child. Some used the future uncertainty due to the incomplete penetrance of the BRCA mutation to validate having children. The difficulty of the decision was also associated with the impact that cancer had on their lives; if this impact had been manageable, these decisions were reported as less problematic than if the cancer had a large negative impact.
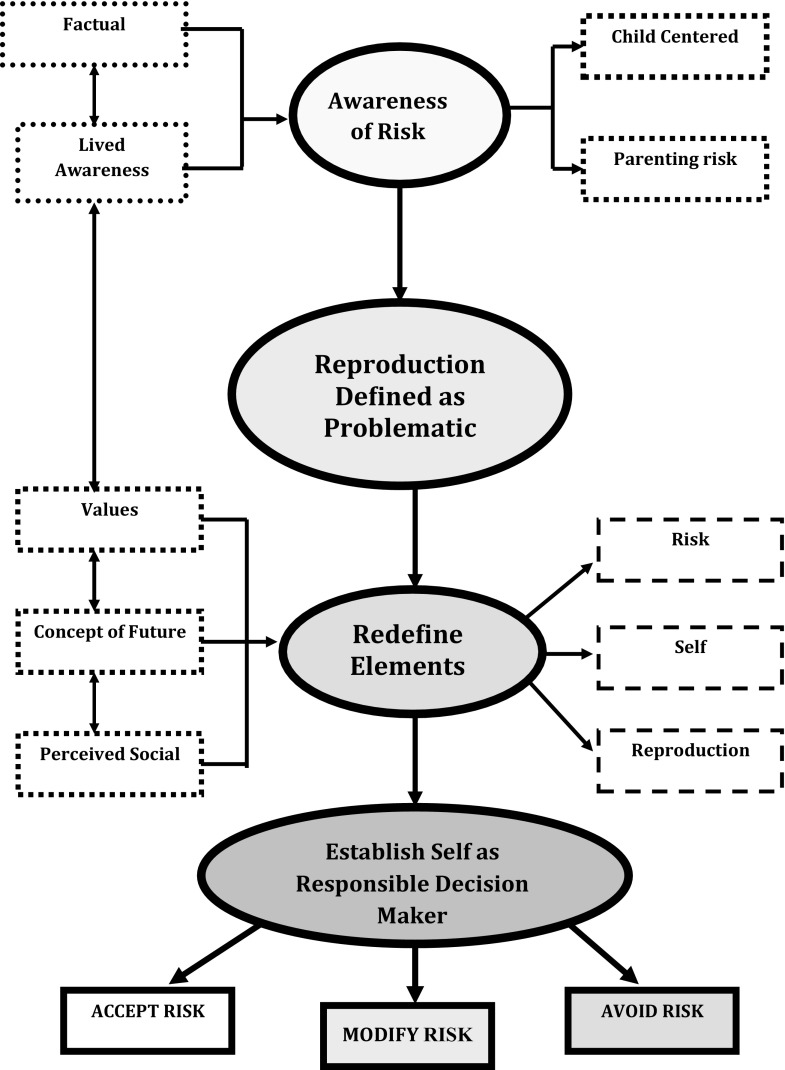
The notion of responsibility is one that stands out in the research and accounts of reproductive decision making (Boardman 2014; Donnelly et al. 2013; Kay and Kingston 2002; McLaughlin et al. 2011). A theoretical model of responsibility proposed by Downing (2002), depicted in Fig. 1, was designed to summarise how those at risk of Huntington disease and their partners confront reproductive decisions. The initial basis is the awareness of the risk, which identifies reproduction as problematic. This increasing awareness forces people to reconsider their specific situation, such as the nature of the risks, their fertility and their relationships. These elements are then redefined to their personal situation. This occurs by actively or cognitively rearranging the elements to create a different story and is influenced by these factors as well as the personal values the individual or the couple hold, how they perceive the future and the support available to them. Redefining allows people to tell different stories when consequently accepting, modifying or avoiding the risks. Downing (2005) found that the value of responsibility dominated participants’ stories and therefore this was classified as the core concept for the model. Although the risks facing those at risk of Huntington disease differ from those of parents of a child without a diagnosis, this model appears to fit with other accounts of reproductive decisions and will provide a theoretical framework for comparison with the results of the current study.
Fig. 1.
The model of responsibility as proposed by Downing (2002)
Reproductive decision making has been explored in the context of several different genetic disorders which illustrate the complexity of these decisions and the number of factors that influence the outcome. Exploration of parents’ experiences of living without a diagnosis confirms that one of the main reasons for wanting a diagnosis is to provide information for future reproductive decisions. Despite this lack of information, couples in this situation still make reproductive decisions, whether they choose not to have any more children or whether they take the risk and conceive again. Yet there is no available research that explores how these decisions are made and the factors that influence them. The purpose of the current study was to explore reproductive decision making in a sample of parents who have a child without a diagnosis. Gaining a better understanding of the reproductive decision making process for this population sample may help genetic counsellors to facilitate decision making more effectively. The major research question investigated in this study was ‘What factors do parents consider when making reproductive decisions, after having a child with an undiagnosed developmental disorder?’
Methods
In this study, qualitative research techniques were used to gather the experiences of parents who have a child with an undiagnosed developmental disorder, to understand their view points, thoughts and feelings and not predetermine their answers in a quantitative approach.
Procedures
Ethical approval was obtained for this study from the Cardiff University Research Ethics Committee. The respondents in the study were recruited with help from the charity SWAN UK, who posted an advert for the research onto their website and links to this were posted on their Facebook page and Twitter. The advert was also printed in the SWAN UK January newsletter. The advert advised that individuals who were interested in participating could contact the researcher by email or post. Interested participants who contacted the researcher were sent a consent form and information sheet, which provided details about the research and interview process, as well as their rights in terms of withdrawal from the study. This information was clarified again verbally at the start of the interview. Consent forms were returned to the researcher before the interview took place. Telephone interviews were carried out by the first author. An interview guide was developed and used as a loose structure aimed at eliciting data relevant to the research question and aims. Open-ended questions were used to encourage the participant to lead the content and direction of the interviews, whilst also not limiting the responses of the participant. Additional questions were asked in order to clarify or prompt further detail. Participants were interviewed via telephone, and the interviews varied in length from 27 to 56 min.
Data analysis
Data were collected using semi-structured interviews which were audio recorded and transcribed verbatim by the researcher. Pseudonyms are used for participants in order to protect their confidentiality. The transcripts were analysed by the first author using interpretative phenomenological analysis (IPA) following the guidelines laid out by Smith and Osborn (2008). The interview transcripts were read repeatedly and keywords and phrases were highlighted. Notes were made alongside the transcript on emerging themes. Emergent themes were identified and labelled with a word or phrase to represent them. Frequent and significant themes were then clustered together into superordinate themes that appeared to describe the connections between them. Although the themes emerged from the data, an attempt to see the world as the participant perceives it was made by the researcher; therefore, the analysis necessarily involved an element of interpretation by the researcher. In order to reduce single researcher bias, the first author practised reflexivity, which is the process of self-reflection that allows one to develop an understanding of how their own background, experiences and beliefs impact the research process (Finlay and Gough 2003). This allowed identification of one’s own assumptions which can shape and influence the study design and analysis of the data (Roulston 2010; Haynes 2012). Each transcript was first analysed in isolation, then similarities and differences in themes across all interviews were identified. The second author reviewed the coding and themes generated in order to highlight inclinations for certain types of interpretations and explanations and suggest alternatives to help reduce bias and increase the rigour of analysis.
Participants
The five participants were all female and had one child with an undiagnosed condition. Two of the participants also had an older child and another participant had adopted a child after the birth of her son. One of the participants received a genetic diagnosis for her child between expressing an interest in the study and the date of interview. This participant was included in the study, but questions during the interview focused on her experience of reproductive decision making before the recent diagnosis. Any quotes used relating to decisions and experiences after receiving a diagnosis are clearly reported. For more information on participants, see Box 1.
Box 1.
Additional participant information
| Melanie’s son, Ned, was born after five miscarriages. Ned is 7 years old and looks relatively well, but Melanie knew that something was not right from birth. She struggled to get anyone to acknowledge the problems that Ned was having for the first few years of his life. Melanie and her husband have decided not to have any other children. Lucy has two daughters. Her youngest daughter, Daisy, is 19 months old and has an undiagnosed disorder. Lucy knew that something was wrong during the pregnancy as Daisy stopped moving. Lucy’s partner is keen for another child, but she has decided not to have any more children. Judy’s son, Callum, was conceived via IVF. She noticed that Callum was delayed in comparison to his peers at approximately 4 months old and had been searching for a diagnosis ever since. Although Judy and her husband decided not to have any more children at first, they started to consider having another child as Callum’s health was improving. A diagnosis for Callum was recently identified. Fiona was told that her son, Nathan, would not survive and was advised to terminate the pregnancy. Fiona decided to continue the pregnancy and Nathan is now 10 years old, exceeding all expectations. Fiona decided not to have any more biological children but did however adopt a child with Down syndrome in order to expand her family. Shelly has two sons. Her youngest son, Rory, is 5 years old and has a range of health problems but no overall diagnosis. Shelly is no longer with her sons’ father but has a new partner. Shelly would like to have another child. |
Results
Factors that influence reproductive decision making
Reproductive options are limited for families without a diagnosis. Without a known mutation, genetic testing is not available for future pregnancies. The only options available are taking the risk of having another affected child, adoption or not having other children. Of the five participants, three decided not to have more biological children and two hoped to have another child in the future. Three of the participants had considered adoption when making reproductive decisions: one had adopted a child before the interviews took place, another had considered adoption but has since decided against it and the third participant was still considering adoption as a future option. Factors that were found to impact the reproductive decision were ‘future uncertainty’, ‘perceptions of risk’, ‘impact on the child’, ‘expectations of a family’ and ‘desire for another child’. Themes are presented with quotations from the interviews.
Future uncertainty
A diagnosis provides a family with more information about their child’s condition; they can look at other people’s experiences of the condition and are often given information on signs and symptoms to be aware of, life expectancy, management and what the child is likely to achieve. Without a diagnosis, the majority of participants found it difficult to plan for the future, as the future is so uncertain:
Shelly: It’s horrible, absolutely horrible, because you don’t know what you can plan for the future…I mean I’ve put my son’s DLA money away which I’ve been told is wrong and I keep getting told off for it, that I should be using it for him for like now, but I’m like I’m not exactly loaded I don’t have a lot of money so I want him to have something when he gets older when I’m not about.
Shelly is trying to plan for an unknown future. She does not know what life holds for her son but also does not want him to suffer because of a lack of preparation. The practical challenges of not having a diagnosis were often cited as frustrations for parents:
Fiona: Not having a diagnosis is a right royal pain in the shirt. You fill in a form and you have to write a list of something…With the symptoms if you write them all down, takes two, two pages of A4. Umm, so it’s a nightmare…umm…so in that respect not having a diagnosis, not having any kind of prognosis, are we expecting him to live until he is a teenager? And is something going to happen?...because you don’t know, you live everyday as if it’s the last, because you don’t know.
Melanie and Lucy both describe the uncertainty as a physical pain that has the power to hurt them and their family:
Melanie: And you don’t know what’s coming, that’s the worst of it, you have no idea what’s about to come round and hit you.
Lucy: I think my partner would cope a lot better if he can know sort of know where…Daisy’s life is sort of going…I mean I, I’ve faced fact that we might never know…and I think that, that’s going to hurt him more than knowing is not knowing and my parents, I think my parents would cope a lot better saying this is the reason for why she is the way she is…rather than going we just don’t know.
These extracts vividly illustrate how difficult it can be to live without knowing what to expect from their child’s condition; living in fear that every day may be the last they have with their child. Not knowing what to expect can mean that the pain and shock, if something bad happens, is elevated. Without a diagnosis, there is no indication as to how the disorder may progress or what signs and symptoms to expect. In contrast, Judy focused less on the future and more on the present moment:
Judy: [I]n a way we had become full of hope…because, every test would come back negative, so after such long lists of tests coming back negative, we started thinking and getting used to the idea of perhaps, you know, we would never find out for sure, but that our son was progressing… every doctor that sees him sees that he is getting better, as they don’t know what kind of, umm, milestones he is ever going to achieve…but they are very encouraging, the fact that he is going forward ...very quickly instead of going backwards or just, you know, plateauing…you know.
Judy appears to view a diagnosis in a negative frame. As more and more tests did not confirm a genetic condition, she began to gain hope that a condition would not be identified. She focused on how her son was progressing and this allowed her to enjoy the present moment rather than fear the uncertain future ahead.
Not having a diagnosis left parents feeling isolated and frustrated. Having to explain lists of symptoms rather than give a name for their child’s disorder and not knowing what to expect, meant that they were continuously searching for an explanation. The future uncertainty not only changed the way families lived their lives but also added a new level of complexity to reproductive decisions.
Perceptions of risk
Not knowing the cause of a condition means that health professionals are unable to predict the likelihood of the condition affecting another pregnancy. This probability is called the recurrence risk. Having no recurrence risk figure was the biggest concern for all participants. The lack of a probability made the risk too big for most and this was a gamble they were not willing to take:
Fiona: Well we were actually biologically not going to have any more because the risk was so big…there was no numbers on it, no nothing, no indication at all. The uncertainty, too big.
Fiona quantifies the uncertainty in an attempt to visualise the risk. This lack of a probability is viewed as a large risk for Fiona who is not only considering the recurrence risk of having another child with the same condition but also the risk of doing so without having a risk figure or probability. Whilst some participants focused on the lack of risk figures, Lucy wanted complete certainty if she were to consider having another child:
Lucy: [T]here’s no guarantee that you’re not going to get another child like Daisy…if I could get given guarantees then…I might think about it eventually, but…no, I, I think I’ve pretty much firm on the no.
Needing a guarantee is not something that can be given in any pregnancy, but the need for this demonstrates the fear that uncertainty can cause. For Shelly, the worry is still present even though she is with a different partner:
Shelly: [I]t’s just kind of like a constant…worrying and obviously I do want another child, and it’s like y’know how do you know whether or not it will happen again and especially with it being a different dad as I think some things link to him and obviously because we don’t know which side this has come from, it’s like y’know who knows if this could happen again.
Shelly recognises that being with a new partner may reduce the chances of recurrence, but this is not certain. Being in a different situation did allow Shelly to think more about having another child and she was one of the two participants who still planned on having another child.
Before receiving a diagnosis for her son, Judy mentioned that she had become ‘full of hope’ because the genetic tests were negative and her son was progressing. She started to focus less on the recurrence risk and this allowed her to start thinking about having another child:
Judy: [S]o, with that frame of mind, we were thinking, we were, we were of two minds, we were, okay if we have another child, we’ve got no risk figure of the same condition could, you know, come out in the second child. We were thinking it was a bit scary, umm, but at the same time, because we, we were, at that moment, kind of fairly happy with how things were going…we were also, we were getting a little bit careless, to be honest, with contraception and like well if it happens it happens.
Judy weighs up the risks against her own happiness and she leaves the future to fate. The recurrence risk appears to hold less fear for Judy than for the other four participants, which enables her to consider having another child.
Of interest, Judy speaks of her upcoming genetic counselling appointment where she plans to find out what reproductive technologies are available to her, now that a cause for Callum’s condition has been identified. At the point of interview, she had not been informed on the inheritance of her son’s condition:
Judy: I suppose I want to know about possibilities for having another baby…and I want to know about the techniques of selecting embryos without the mutation…the chances of success…you know…when using that selection technique. And if they say that the chances of success are like 1…I don’t know, 1 in 10,000 or something I’m not even going to try!
In the above quote, Judy has moved away from weighing up the possible risks to considering the chances of success of reproductive technologies, demonstrating that even with a diagnosis, there are still probabilities to consider.
Impact on child
In their interviews, the parents made it clear that although their desire for another child was strong their current child/children were the most important factor of all. Needing to be emotionally and physically capable to care for the children was a top priority. Participants’ views on how another child may impact their current child/children differed, and they framed these to justify the decision made:
Lucy: I didn’t want to run the risk of potentially having another child…that is the way that Daisy is…when I can put all my focus on the two that I’ve already got rather than, for that ease of words, feel like I’ve let them down, like it’s not like, ignoring them or anything like that, to deal with another child that could, potentially have bigger health problems or could just be normal, you don’t know, I wouldn’t want to run the risk of doing that again…I don’t think it would be fair.
Melanie had previously considered the option of adoption but felt that this was no longer an option for her family:
Melanie: No not an option now, it wouldn’t be fair on Ned, at so many levels it just wouldn’t be fair, umm you know when I thought that a younger, because it would be you know they would place a younger child with us, but watching a younger child develop normally and zip past him...it…we couldn’t do that to him and also it wouldn’t be fair on the child because Ned needs so much stuff sorting…you know, when I look at our diaries it’s just packed with Ned appointments and I just don’t think it would be fair on another child you know that has come through a system already and have had that time, I just don’t think we could give that time to them.
Previous bad experience during pregnancy and the need to be able to look after their child with disabilities during this time further complicated the decision for Judy, who wanted to have another child but was concerned about the impact this would have on her own health as well as her child’s care:
Judy: I had diabetes…gestational diabetes. And the, the whole IVF, they tell you that by stimulating the ovaries they are increasing the chances of you developing ovarian cancer in the future. So all those things, they are making me very, very scared. And I had a C-section and I, I would most likely have another C-section. Which it’s okay, I’m not that afraid of surgery. But the one thing is the recovery period would be much longer than it was and we need to take care of the children when I am recovering…all those things…my health is going to be okay. To take care of the children, especially one that has so many…extra needs of therapy and appointments and all that.
Shelly wanted another child to help out with the responsibility of looking after their sibling when their parents were no longer around:
Shelly: Yeah, because obviously I would prefer maybe Scott to have another sibling so that they can, y’know-I know it sounds horrible, but basically so they can help look after Rory when he gets older.
But she was concerned about how a pregnancy may impact on her own health and ability to care for her child:
Shelly: It’s always a worry thinking, he’s going to need me when I’m older to be active and I don’t want a pregnancy that’s gonna…knock me for six, which is why I have a kinda cut-off age.
Reproductive decisions are complicated. Having to balance desires for a child against many other factors such as age and physical capabilities of the mother, time, finances and work commitments can be very challenging. Having a child with complex needs means that they need more time and care and having another child can impact on this, particularly if there is a risk that another child may have similar needs. By creating a cut-off age, Shelly managed to find a balance between the supports another child would provide in the family and the physical strain a pregnancy may cause on her own health. Participants could not always find a balance between their own desires and their responsibility to their child/children, but they always put their children first, even if that meant not fulfilling their own desire to have another child.
Expectations of a family
Participants’ expectations of their own future played a role in influencing their reproductive decisions. These expectations could have been shaped by previous family experience, experiences during pregnancy or views toward adoption. Past experience, views and values were clearly of importance to participants and influenced the decision making process. The number of children that participants had expected or hoped to have, which was often shaped by their own experiences of growing up in a certain family size, was an important identifier for two of the participants for how they viewed their future:
Shelly: I don’t know I just always wanted to have three kids to be honest—I was bought up as like three, umm there was me, my sister and my younger brother.
Melanie: I think we’d always assumed, I mean Edward is one of four, five, umm I’m a scout leader, umm you know we’ve always been surrounded by children umm you know we’ve both got multiple godchildren…umm, we just assumed we would have children.
Listing the ways in which they have been ‘surrounded’ by children is given as reasoning for why they should have more children and justifies why they expected this. Having to readjust expectations as well as suppress the desire for another child was a challenge and something that could not always be fully accomplished. Fiona had never planned on having a certain number of children but was ‘starting with one’. This allowed acceptance of her situation:
Fiona: I didn’t ever grieve for the child I should have had, because Nathan is the child I should have had. I was surrounded by people, a lot of my friends couldn’t have children. People who had a great difficulty getting pregnant, but I wasn’t ever of the opinion where I had this God given right, to decide I was going to have a baby, to get pregnant and have this wee perfect bundle at the end of it.
Relinquishing control to the concept of fate allowed Fiona to adjust to her situation and reach a relatively firm decision. The thought that there was a higher control that determined their course allowed Fiona to accept their situation and not grieve after the birth of her son. She expressed less of a desire to have another child after the birth of her son, but she did adopt a second child.
Lucy had never expected to have children but now has two daughters. Both pregnancies were difficult, particularly her second which resulted in the birth of her daughter Daisy, who has an undiagnosed condition. Although her partner is keen to have another child, Lucy states that the experience of pregnancy has also played a role in her decision:
Lucy: Umm, I know he would like to have another one, I know he wants to have a boy eventually, but I, I can’t do it, I mean I, with both pregnancies, both of them were really bad, they were both born prematurely…I, I wouldn’t want to put myself through the heartache again…of constantly being worried…and like listening, feeling for every move—no I just couldn’t do it again.
The molecular diagnosis of a mitochondrial condition for Judy’s son Callum also brought with it the devastating news that his condition was life-limiting. This sparked new discussions about having another child, as the thought of being childless did not appear to fit with Judy and her family:
Judy: Life shortening conditions…like this…mean, mean that we are now, that we won’t have a child in [Inaudible] years. So we are starting again to consider…having another child…my mother…she was always saying that we shouldn’t have anymore, at my age…She was always saying…you have enough on your plate…you don’t know how much a pregnancy at your age is going to affect your health….but immediately when she heard about the diagnosis immediately she said, umm, what are the chances of having the same thing or condition if you decide to have a second child. So immediately, when she heard about the possible life shortening possibility, she immediately changed her mind.
Desire for another child
Throughout the interviews, participants constantly weighed up factors for and against having another child (biologically or adopting). Even when a firm decision had been made, participants were continuously reassessing their decision and justifying the reasons. Parents recognised that their desire for a child is not something that can be controlled, even when a final firm decision had been made:
Melanie: but then at my darkest point which was about 11 months…I suddenly had this amazing urge to have another baby… and umm, you know it was, it was like a hunger you know it was, it was the most, it was the, suddenly I understood what women were talking about, this craving to have a baby and umm, my body was just going for god’s sake just get pregnant breed, breed, breed and my brain was going what the fuck are you thinking of?!
Melanie speaks of her mind and her body as separate entities in this extract. She had decided not to have any more children and was not in a mental state to do so, yet her body craved a baby. This intense desire was out of her control, and although she could reason with why not to have another child, her body continued to long a pregnancy. All the justification, reasoning and knowledge with what one ought to do does not lessen the desire for a child and the need that people felt.
For those that decided not to have any more children, there was a sense that even though they had made the decision themselves, that the decision was never really theirs to make. They made the decision based on what they ought to do rather than their own desires:
Fiona: Yes, umm, and it wasn’t really a discussion about having other children because we were both quite clear we couldn’t do it. Umm, and it was more and I felt, more than I would have ever have expected to feel—cheated. Well I wasn’t out there planning to have lots and lots of children, having one child was absolutely fine for me, but when that choice is removed it just feels different and although there wasn’t anyone to say you shouldn’t have any more children, we imposed that on ourselves, we couldn’t do this again. That was quite hard.
The above extract demonstrates the pain experienced by the loss of control felt over a decision that an individual should have the right to make. Fiona recognises that the choice was always her own, but she felt cheated; although presented as a choice, it was never really her choice to make. She was forced to make the decision not to have any more children. This underlying desire and hope that the choice to have another child still remained was apparent in the narratives of participants who had decided not to have another child:
Lucy: I find it hard to talk to my partner about this sort of stuff than I do anyone else…I think…saying it out loud seems quite final [laughs]…but I think, I think I’ve known for a while that I wouldn’t be able to do it again, that I wouldn’t be able to go…and have another baby.
Melanie: I can’t get rid of Ned’s baby stuff…it’s in the loft…all of his clothes from about 3 years old onwards I’ve merrily passed on to friends and family, but there is something that- even then I’m too old to breed now umm, but there’s, I just couldn’t get rid of the baby stuff there was just that sort of something in the back of my mind, you know…could we, could we have another one, but…realistically, you know.
Lucy and Melanie were both firm about their decision not to have another child. Both had listed reasons why they would not have another: Melanie had experienced a difficult pregnancy and labour, and she felt that having another child would be unfair to her son. Lucy was content with two children and did not want another even if she was told that the child would be healthy. Saying the decision aloud and clearing out baby things were a step too far for these participants, suggesting that the hope of the possibility of having another child was always present.
Fiona adopted a child with Down syndrome, following the birth of her son who does not have a diagnosis:
Fiona: [M]edically he is very well, doesn’t have any of the associated health issues, but umm, so that has been very good and it’s allowed us to extend the family without taking that huge risk. And although Thomas has a disability, we were well aware of that disability, and knowing what that potentially entails. Umm, so we could make that choice.
Adoption of a child with disabilities, but also with a diagnosis, eliminated the future uncertainty experienced by not having a diagnosis. Deciding to adopt a boy with Down syndrome was a choice that Fiona made, allowing her to take back control of the situation, providing herself with another option for extending the family.
Judy had started trying for a baby in her late 30s and her son was conceived via IVF. As the process had been so difficult, she did not plan on having any more children, but soon the desire for another child outweighed the negative aspects of this difficult experience:
Judy: [W]e thought it would be crazy to try again; we got what we’d hoped for. It wasn’t easy the first time, when I was 40, so…I guess it will not going to be easy for this one.
Judy recognises that her age and past difficulties are likely to make conception difficult; however, her desire for another child outweighs this bad experience.
Discussion
This study was used to explore the experience of reproductive decision making for parents of a child without a diagnosis. Not having a diagnosis had a large impact on the reproductive decisions that participants made and analysis identified five factors that played a major role in these decisions: future uncertainty, perceptions of risk, the potential impact a child would have on their current children, expectations of a family and the desire for another child.
The lack of future certainty was a constant worry for participants. Although a diagnosis does not necessarily give future certainty, this population group does not have any prognosis or inclination to what the future holds for their child and this was what parents strived for. In the search for a diagnosis, participants held a great expectation of what a diagnosis will provide and this has been reported in other studies (Graungaard and Skov 2006; McLaughlin et al. 2011) where the meaning parents attached to a diagnosis was not always realistic in a medical sense, as there was an assumption that a known diagnosis would give future predictability and a possibility to gain some control over the situation. Yet many parents find that this is not the case, particularly for those that receive a diagnosis for a very rare condition. Identification of the genetic cause is helpful in terms of predicting the recurrence risk to future pregnancies and for the availability of options using reproductive technologies. Participants in this study wanted a diagnosis in order to inform reproductive decisions and this has been described by many parents of a child without a diagnosis (Lenhard et al. 2005; Lewis et al. 2010; Makela et al. 2009; Rosenthal et al. 2001).
Reproductive decisions are complex decisions made by weighing up various factors. For some participants, the ‘right’ option was clear to them and the decision was made quickly. There was often a sense of what one ought to do, but this was often in conflict with the desires of the individual. The lack of recurrence risk information had a huge influence on the decisions that the women made, as their perceptions of the risk were high. Not having any risk figures caused participants to focus on the possible worse-case scenario of having another affected child. This style of thought has been described in other studies (Kay and Kingston 2002; Lippman-Hand and Fraser 1979). Similar to the findings of Lee et al. (2013), this perception of high risk was often a barrier to further reproduction and the majority of participants (3/5) decided against having another child. For the two participants that did want another child, other factors outweighed the risk; both women had a more negative view of a diagnosis, as they feared the prognosis that may accompany this. Judy viewed a lack of a diagnosis as good news, focusing on how her son was progressing, possibly indicating that she had not fully accepted that her son’s symptoms suggested a permanent condition; similar findings have been reported by Graungaard and Skov (2006). Shelly was in a new relationship, which could possibly change the recurrence risk.
The impact that another sibling would have on their current child/children was often stated by participants with concerns relating to the amount of time and attention that their child needed as they did not want to jeopardise the care of any of their children. These worries have been reported in studies of cystic fibrosis carriers (Myring et al. 2011).
As previously shown, past experiences also influenced the reproductive decisions (Donnelly et al. 2013; Peters et al. 2002). These experiences included reflecting on their own childhood and their expectations of a family. Past experience of the condition and the parents’ ability to cope with the challenges it presented appeared to also influence the decisions. Participants that decided not to have any more children spoke in detail about their child’s problems, the difficulties they experienced in pregnancy and during birth and they also spoke more vividly about their search for a diagnosis. These stories were recalled as negative experiences that participants did not want to endure again.
The desire for a child was often the main factor drawing participants to consider another pregnancy. Narratives suggested that the desire for a child was not something that participants can control, whether it was the desire for a healthy child, desire to have a child with a new partner or the desire for a certain family size. This desire was also apparent for couples at risk of having a child with cystic fibrosis, as studied by Myring et al. (2011). However, in contrast to Myring et al. (2011), participants with an affected child in this study did not seem to believe that the odds will be in their favour for the next pregnancy; the difference here could be due to the ambiguity surrounding the risk for those without a diagnosis. The desire for a child was particularly apparent throughout the transcripts of those that decided against having another child. The definite decision that was expressed was undermined by their feelings of longing and holding onto the possibility of having another child. This finding agrees with the findings by Frets et al. (1991) that couples who decided not to have another child tended to have unresolved doubts about the decision. All participants in this study expressed that the decision made about their reproductive plans was final. However, one participant spoke of how she had become a bit careless with contraception. This tactic has been previously described by Lippman-Hand and Fraser (1979) and was termed ‘reproductive roulette’ in which leaving conception to fate removes personal responsibility, thereby removing the decision or making a ‘non-decision’.
The factors found in this study to influence reproductive decisions have also been found to influence the decisions in the context of known genetic diagnoses, but not having a diagnosis adds an extra layer of complexity to the decision. Downing’s (2005) model of responsibility shows a schematic of reproductive decision making that focuses on responsibility as a major defining theme. The data from the current study fits within this model to a certain extent: Awareness of the risk (or lack of a risk figure) was discussed by all participants and this leads to identification of reproduction as problematic. This awareness of the complications makes people reconsider their specific situation. In this study, the specific situation took into account the future uncertainty, perceived risk, the impact on their current children, their expectations of a family and their desire for another child. These elements were redefined in the participants’ narratives to represent their personal situation by creating a story influenced by their personal values and experiences. As Downing (2005) describes, this allowed people to tell different stories when consequently accepting, modifying or avoiding the risks. On the other hand, the model is a flow diagram suggesting that parents moved from one stage to the next, without revisiting stages. The current study suggests that even when a decision is made, it is not always satisfactory to the parents and they are constantly weighing up the factors and revisiting the ‘redefine elements’ stage.
Study limitations
This research is a qualitative and exploratory study and it is therefore not possible to generalise the findings to the population of interest but is intended to provide an insight into individual’s experiences. Recruitment was aided by a support group and although membership to this group was not a requirement for participation, awareness was made to the research by accessing the support group website or social media. Therefore, it cannot be determined whether individuals who agreed to participate differ in significant ways from those that did not participate. Analyses of data were completed using IPA. IPA requires a smaller sample size than other qualitative analysis techniques (Smith and Osborn 2008). Although the present study had a sufficient number of participants for this type of analysis, more participants would have further enriched the data and may have allowed further themes to be identified.
Practice implications
The findings from this study may help genetic counsellors to better understand the complexity of the reproductive decision making process for this group of mothers. Increasing genetic counsellors’ knowledge of the influencing factors will enable them to be more sensitive to these issues and explore the perspectives of the individual. In turn, this may help to increase the sense of empowerment and choice for parents of a child without a diagnosis. Although these decisions are hugely complicated, that does not mean that there are no options available to them. Talking through how parents’ perceive the risks, and what other factors are influencing their decisions, will help them to see their options more clearly. Signposting parents to other services for fostering and adoption may also be of benefit.
Research recommendations
Further research is needed in this area to compare results, as at the time of the research this is the only study focusing on the topic of reproductive decision making for parents without a diagnosis. Possible areas to research for further understanding would be to include the father’s perspective in order to compare the experience of reproductive decision making between mothers and fathers of children without a diagnosis. Some studies have suggested that the more options available to couples, such as prenatal testing and preimplantation genetic diagnosis, the more complex the decision (Frets et al. 1991; Shiloh et al. 2006). A comparison of reproductive decisions made by those with a diagnosis compared to those without a diagnosis would help with the understanding of the decision making process and identify unifying factors as well as factors unique to both groups. All participants in this study had made a definite decision; however, these decisions change over time and therefore a long-term follow-up study that follows the decision making process and ‘definite’ decisions made over time would provide further insight into this experience.
Compliance with ethical standards
Conflict of interest
Emily Pond and Rebecca Dimond declare that they have no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5).
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- Boardman F. Experiential knowledge of disability, impairment and illness: the reproductive decisions of families genetically at risk. Health. 2014;18(5):476–492. doi: 10.1177/1363459313507588. [DOI] [PubMed] [Google Scholar]
- Decruyenaere M, Evers-Kiebooms G, Boogaerts A, Philippe K, Demyttenaere K, Dom R, Vandenberghe W, Fryns JP. The complexity of reproductive decision-making in asymptomatic carriers of the Huntington mutation. Eur J Hum Genet. 2007;15(4):453–462. doi: 10.1038/sj.ejhg.5201774. [DOI] [PubMed] [Google Scholar]
- Donnelly LS, Watson M, Moynihan C, Bancroft E, Evans DGR, Eeles R, Lavery S, Ormondroyd E. Reproductive decision-making in young female carriers of a BRCA mutation. Hum Reprod. 2013;28(4):1006–1012. doi: 10.1093/humrep/des441. [DOI] [PubMed] [Google Scholar]
- Downing C (2002). Reproductive decision-making in families at risk for Huntington’s disease: perceptions of responsibility. An unpublished dissertation submitted to the University of Cambridge for the Degree of Doctor of Philosophy
- Downing C. Negotiating responsibility: case studies of reproductive decision-making and prenatal genetic testing in families facing Huntington disease. J Genet Couns. 2005;14(3):219–234. doi: 10.1007/s10897-005-0619-3. [DOI] [PubMed] [Google Scholar]
- Finlay L, Gough B. Reflexivity: a practical guide for researchers in health and social sciences. 1. Oxford: Blackwell Science; 2003. [Google Scholar]
- Frets PG, Duivenvoorden HJ, Verhage F, Peters-Romeyn BMT, Niermeijer MF. Analysis of problems in making the reproductive decision after genetic counselling. J Med Genet. 1991;28(3):194–200. doi: 10.1136/jmg.28.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graungaard AH, Skov L. Why do we need a diagnosis? A qualitative study of parents’ experiences, coping and needs, when the newborn child is severely disabled. Child Care Health Dev. 2006;33(3):296–307. doi: 10.1111/j.1365-2214.2006.00666.x. [DOI] [PubMed] [Google Scholar]
- Haynes K. Chapter 5: reflexivity in qualitative research. In: Symon G, Cassell C, editors. Qualitative organizational research: core methods and current challenges. London: Sage Publications; 2012. pp. 72–89. [Google Scholar]
- Kay E, Kingston H. Feelings associated with being a carrier and characteristics of reproductive decision making in women known to be carriers of X-linked conditions. J Health Psychol. 2002;7(2):169–181. doi: 10.1177/1359105302007002456. [DOI] [PubMed] [Google Scholar]
- Lee SM, Nam HW, Kim EN, Shin DW, Moon HJ, Jeong JY, Kim SA, Kim BJ, Lee SK, Jun JK. Pregnancy-related knowledge, risk perception, and reproductive decision making of women with epilepsy in Korea. Seizure. 2013;22(10):834–839. doi: 10.1016/j.seizure.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Lenhard W, Breitenbach E, Ebert H, Schindelhauer-Deutscher HJ, Hen W. Psychological benefit of diagnostic certainty for mothers of children with disabilities: Lessons from down syndrome. Am J Med Genet. 2005;133A:170–175. doi: 10.1002/ajmg.a.30571. [DOI] [PubMed] [Google Scholar]
- Lewis C, Skirton H, Jones R. Living without a diagnosis: the parental experience. Genet Test Mol Biomarkers. 2010;14(6):807–815. doi: 10.1089/gtmb.2010.0061. [DOI] [PubMed] [Google Scholar]
- Lewis C, Skirton H, Jones R. Development of an evidence-based information booklet to support parents of children without a diagnosis. J Genet Couns. 2012;21:854–861. doi: 10.1007/s10897-012-9501-2. [DOI] [PubMed] [Google Scholar]
- Lionel AC,Costain G, Monfared N, Walker S, Reuter MS, Hosseini SM et al (2017) Improved diagnostic yield compared with targeted gene sequencing panels suggests a role for whole-genome sequencing as a first-tier genetic test. Genet Med [Online]. Available at: http://www.nature.com/gim/journal/vaop/ncurrent/full/gim2017119a.html [accessed: 29th October 2017] [DOI] [PMC free article] [PubMed]
- Lippman-Hand A, Fraser FC. Genetic counseling—the postcounseling period: II. Making reproductive choices. Am J Med Genet. 1979;4:73–87. doi: 10.1002/ajmg.1320040109. [DOI] [PubMed] [Google Scholar]
- Makela NL, Birch PH, Friedman JM, Marra CA. Parental perceived value of a diagnosis for intellectual disability (ID): a qualitative comparison of families with and without a diagnosis for their child’s ID. Am J Med Genet A. 2009;149A:2393–2402. doi: 10.1002/ajmg.a.33050. [DOI] [PubMed] [Google Scholar]
- McLaughlin J, Clavering E, Haimes E, and Wright M (2011) Genetic journeys: key findings from a study of the experiences of families referred to paediatric genetics. Policy, Ethics and Life Sciences Research Centre, Newcastle University. Available at: http://www.ncl.ac.uk/peals/assets/publications/Peals-ResearchReportA5spreads.pdf [Accessed 3/07/2015]
- Myring J, Beckett W, Jassi R, Roberts T, Sayers R, Scotcher D, McAllister M. Shock, adjust, decide: reproductive decision making in cystic fibrosis (CF) carrier couples—a qualitative study. J Genet Couns. 2011;20(4):404–417. doi: 10.1007/s10897-011-9363-z. [DOI] [PubMed] [Google Scholar]
- Peters KF, Kong K, Hanslo M, Biesecker BB. Living with Marfan syndrome III. Quality of life and reproductive planning. Clin Genet. 2002;62(2):110–120. doi: 10.1034/j.1399-0004.2002.620203.x. [DOI] [PubMed] [Google Scholar]
- Rosenthal ET, Biesecker LG, Biesecker BB. Parental attitudes toward a diagnosis in children with unidentified multiple congenital anomaly syndromes. Am J Med Genet. 2001;103(2):106–114. doi: 10.1002/ajmg.1527. [DOI] [PubMed] [Google Scholar]
- Roulston K. Reflective interviewing: a guide to theory and practice. London: Sage Publications; 2010. [Google Scholar]
- Shiloh S, Gerad L, Goldman B. The facilitating role of information provided in genetic counseling for counselees’ decisions. Genetics in Medicine. 2006;8(2):116–124. doi: 10.1097/01.gim.0000196823.50502.a4. [DOI] [PubMed] [Google Scholar]
- Smith JA, Osborn M. Interpretative phenomenological analysis. In: Smith J, editor. Qualitative psychology: a practical guide to research methods. 2. London: Sage; 2008. pp. 53–80. [Google Scholar]