Abstract
Verification and validation are objective and subjective measurements of hearing aid function. Many studies have provided rationales for performing these measurements as necessary for hearing aid practitioners to provide the highest level of care. Several researchers have suggested that completing these measurements as part of routine clinical care will reduce the number of return visits, reduce the number of aids returned for credit, and increase patient satisfaction. The purpose of this review article is to provide background, method and rationale for practitioners to use these measurements to improve their practice of hearing healthcare.
Keywords: Hearing aids, Verification, Real-ear measurements, Probe-microphone measurements, Satisfaction
1. Background
Verifying and validating hearing aids confirms the value of the practitioner and the device. Verification of a hearing aid fitting is an objective measure (often referred to as real-ear measurements or probe-microphone measurements) that ensures the hearing aid is operating appropriately by analyzing the device using a hearing aid analyzer or through probe microphone measurements. Validation is a subjective measure that captures the hearing aid user's perceived benefit, satisfaction, and handicap reduction by the use of hearing aids (ASHA, 1998). Many studies have pointed to the rationales for performing these measurements in terms of providing the highest level of service to the patients in terms of their communication needs. In addition, verification provides the clinician with confidence that they provide a quality product and is promoting greater satisfaction and benefit to their patients. This article will focus on how to implement appropriate verification and validation measurements into daily clinic and the benefits of doing so.
For most patients, the goal is adequate access to acoustic information for appropriate speech communication. To ensure appropriate access to the auditory signal, audibility needs to be confirmed. Currently, probe microphone measurements are the only way to ensure an audible signal of a hearing assistive device. Ensuring an audible signal is not only a method of verifying the device, but it is also verifying that our job of providing quality products to our patients is completed as well.
Audiology best practices guidelines state that probe microphone measurements should be completed to ensure that hearing aid gain and output meet prescribed targets for each individual. Several international organizations [e.g. American Academy of Audiology; American Speech Language Association; Hearing Instrument Association (ASHA, 2006, IHS, ND; Valente, 2006; Valente et al., 2006)] have provided guidance to those who dispense hearing aids. They recommend that “prescribed gain from a validated prescriptive method should be verified using a probe microphone approach” (Valente et al., 2006). In contrast to these recommendations, several studies have suggested that more than half of hearing aid providers are not conducting these measurements on a routine basis (Bamford et al., 2001, Mueller and Picou, 2010). In a survey of dispensers, 57% of respondents reported owning the equipment; however, only 34% of all respondents reported that they consistently used the equipment (Kirkwood, 2006). In all of these surveys respondents to these surveys have reported lack of time, financial difficulties or space constraints as to why these measurements are not completed. However, none of these challenges are a valid argument for not providing the highest quality care to our patients.
Some hearing aid providers report other means of verification. Some report using aided speech testing. However, this type of testing is likely not able to provide reliable information (Thornton and Raffin, 1978). While aided speech testing can be a very useful tool, this method is more validating that the aids is working for the patient and providing the patient with validation of the aids' worth. Some practitioners report relying on manufacturer first-fit formulas to provide accurate fitting gains. Indeed the most compelling reason to complete real-ear measurements is that several studies have confirmed that the manufacturer's first-fit algorithm is inadequate in providing appropriate gain (Aarts and Cafee, 2005, Aazh and Moore, 2007, Hawkins and Cook, 2003). Therefore, verification of gain relative to audiometric thresholds is absolutely necessary and should be part of routine patient care.
2. Verification
Prior to real-ear measurements, a hearing aid practitioner must first ensure that the aids are appropriate for the patient (e.g. appropriate hearing aid style, mold, tubing, venting, etc.) and that the correct device was selected for the patient. In recent years, open fit hearing aids have ben come more popular. Patients and clinicians enjoy the lack of occlusion and fitting options. Several styles of open fit aids are available including receiver in the aid (RITA) devices connected to a thin tube and an open dome as well as receiver in the canal (RIC) devices connected to an open dome. For the purposes of this discussion, open fit devices are open regardless of the location of the receiver. There are reasons to use a RIC or RITA that are beyond the scope of this paper and would warrant an entire publication alone (some information may be found in Mueller (2009)).
Once received, the aid function should be confirmed and all of the features within the aid should be checked to ensure appropriate function. This includes validating that the aids can connect to the programming software, are able to accept programming changes, and minimal necessary gain can be achieved. Further, any features that are ordered such as directional microphones should be verified. Directional microphone verification can be completed in a hearing aid analyzer test-box by testing the gain of a hearing aid in the directional setting checking the gain with the aids facing the speaker and at 90° (front-side measurement) (for further description on this see Wu and Bentler (2012)). Additional features, such as frequency lowering and tinnitus management should have a functional assessment. All hearing aid features that are ordered for the patient should have their confirmed; if the feature is ordered, functionality should be ensured for patient success confirmed to ensure they are functioning as intended.
Once the patient arrives, appropriate patient expectations have been set and otoscopy has ensured clear ear canals; the real-ear verification process can begin. The purpose of real-ear measurements are to ensure that appropriate gain is provided to a person with hearing loss. Therefore, accurate hearing thresholds are converted from the audiogram measurement (dB HL) to the measurement of hearing aid output (dB SPL). For the most accurate conversion of dB HL to dB SPL, real-ear-to-coupler difference (RECD) needs to be measured. This measurement is conducted with a probe tube microphone in the ear and either an insert earphone or the hearing aid earmold. The goal of this measurement is to accurately convert the dB HL measurements of the audiometric testing to hearing aid output measurement of dB SPL. Without this measurement, the average dB HL to dB SPL conversion is used which could over or under-estimate the size of the person's ear. The most accurate conversion of dB HL to dB SPL requires an RECD measurement. It is highly recommended that this measurement be conducted as these converted thresholds are how a target gain is calculated; the more accurate the conversion, the more accurate the target gains.
Once thresholds are converted, a target prescription should be selected. Currently, the most commonly used prescriptive targets are from two labs (NAL and DSL). There are many differences between the two formulas. However, the premise of NAL is to restore normal loudness perception thus ensuring signal clarity; while DSL's primary goal is to ensure an audible signal thus improving access to the sounds for signal clarity. There are many reasons to select one of the prescriptive targets as compared to the other (for a more thorough review and comparisons of the most recent NAL and DSL formulas see Johnson (2012) and Johnson and Dillon (2011)); however, in general either method will provide an audible and clear signal thus ensuring quality access to sounds and improve communication clarity.
It is suggested that prior to starting on ear verification measures, depending on the hearing aid manufacturer, a feedback assessment should be completed. This is because feedback manager, depending on the hearing aid manufacturer, may reduce the gain of the aid in specific channels. If gain is reduced to rid the aid of feedback, changes in gain output made during verification may be significantly reduced. Therefore, it is suggested that this measurement be conducted prior to the fitting of the aid. If feedback manager significantly reduces gain output, the physical characteristics (e.g. venting, fit of the mold/aid) should be assessed to determine if a tighter fit of the aid can be achieved.
3. Real-ear (probe-microphone) measurements
With the hearing aid and probe tube microphone in the ear, the next step is to compare the hearing aid output to the selected targets. A soft, moderate and loud signal should be presented. There are many signals available to analyze the hearing aid gain. However, gains obtained for real-world signals may be very different than pure tones or composite signals. Therefore, it is recommended to complete this measurement using speech signals. One such signal created for this purpose is the International Speech Test Signal (ISTS; Holube et al., 2010) which is an internationally recognized test signal. It was created on the need for a standardized test signal that includes all relevant properties of speech. It is based on natural recordings of speech in six languages based on long term average speech spectrum (LTASS) standards. While this signal was created for the purposes of real-ear measurements, any standardized speech signal would be recommended over composite noise or pure tones.
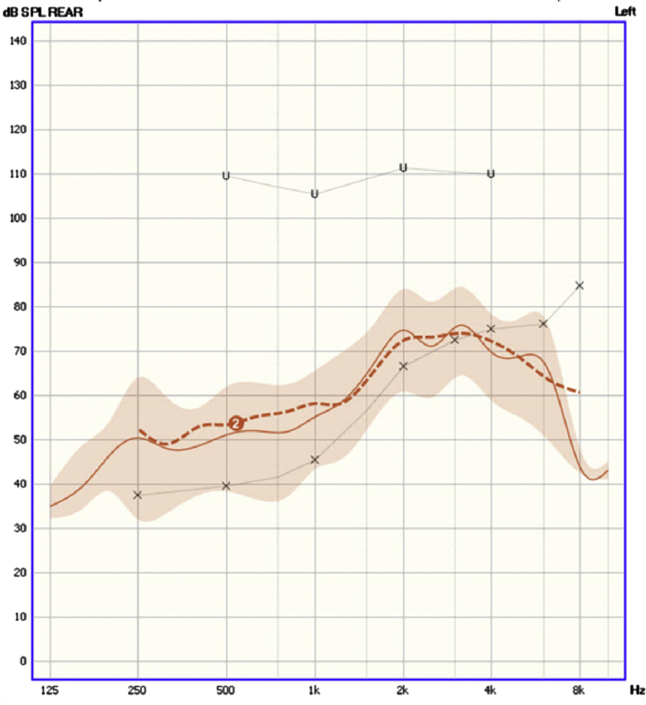
Real-ear aided response (REAR) or real-ear insertion gain (REIG) responses are the most common method of viewing hearing aid gain compared with targets based on individual thresholds (For a review of REAR and REIG, see Galster (2011)). REAR responses allow for comparison of hearing aid response to the patient dynamic range, so for the purposes of this article, the REAR is the preferred method of measuring hearing aid output. The REAR permits the hearing aid provider to ensure audibility while comparing the output to the dynamic range. Because of the comparison to the dynamic range, REAR allows the practitioner to ensure that the signals are audible across the frequency spectrum. While target prescriptive formulas are important, it is also important to know where the output is compared with thresholds and Uncomfortable Loudness Levels (UCL). In Fig. 1, the “x” represents the threshold, the “u” represent the UCL. The area between these would be the patient's dynamic range. The goal of appropriate fitting would be to ensure that as much of the signal is possible within the dynamic range while also attempting to get the hearing aid gain to match the target gain prescription.
Fig. 1.
REAR.
In the example Fig. 1, the targets (represented by darker dashed lines) are NAL-NL2 targets (Keidser et al., 2011) based on thresholds. These targets are a mathematical calculation that provides target gain output at differing inputs. In this example, the dashed lines labeled “2” are NAL-NL2 (Keidser et al., 2011) for a moderate 65 dB SPL input. The outputs are measured in the ear, with a probe tube and the hearing aid in the ear. It should be noted that additional steps may be necessary if an open fit (or large vent) is used in the aid (for additional information on open-fitting REAR, see Aazh et al. (2012)) The ISTS signal is played out of the speaker, is amplified by the hearing aid, and is measured by the probe microphone in the patient's ear. This is the most accurate measurement of the sounds passing through the hearing aid into the patient's ear. Without this measurement, depending on the manufacturer's first-fit or patient reports alone will not provide accurate information (Abrams et al., 2013, Leavitt and Flexer, 2012, Sanders et al., 2015). The output of the hearing aids is compared with the targets at each of these levels. As speech is variable, the shaded area represents the speech modulation around that frequency. However, the long-term average speech spectrum (LTASS), the solid line in the middle of the shaded area, is compared with the targets. As you can tell in Fig. 1, the hearing aids are meeting the target output through nearly all of the frequencies. However; most of the signal above 4000 Hz is inaudible to the patient. This process should be repeated for soft and loud input. Beyond matching targets, one should be aware of the audibility of the signal; however, this is a topic outside the scope of this paper. Once the gains are changed and appropriate output is reached, the maximum power output of the hearing aid (MPO) should be measured and compared to the patient's UCL (marked “u” on Fig. 1). This is to ensure that the loudest the hearing aid could output does not cause pain for the patient. If UCL measurements were obtained, accurate MPO measurements can be obtained. If they were not, watch the patient for signs of discomfort.
4. Validation
Once verification of hearing aid output has been completed, validate that the hearing aids are working for the patient. Validation includes asking the patient about sound quality, ear balance and comfort of the devices. Adjustments can be made to the devices so that the patient is comfortable with the devices. However, it is also important to not turn down the devices at the initial fitting. The adjustment period for new devices may be up to 4–6 months. Conversely, it is important to keep in mind that the verification targets are averages. This means that some people desire the sounds to be louder while others desire them to be softer. It is this balance between managing patient desires while ensuring audible signals that make an excellent hearing aid provider.
Contemporary hearing rehabilitation of adults with acquired hearing loss is patient-centered and outcome-driven. Ultimately, outcomes are significantly influenced by the initial part of the individual's journey on how they opted to seek hearing healthcare. The motivation for treatment and expectations greatly influence outcomes. Treatment planning, involving the individual, family members and/or communication partners, must reflect on how the individual got to the point where they initiated obtaining hearing aids in order to plan for successful outcomes. Ignoring this part of the journey belies the expectations, attitudes, experiences and other factors that can undermine the process.
Using a comprehensive case history and self-report tools are essential to working with all individuals who seek hearing healthcare services. Addressing their personal needs using self-report tools that assess multiple domains provides extensive, valuable information about the individual's activity and participation restrictions as well as the social and emotional effects of hearing loss unique to this patient. A unique self-assessment questionnaire developed by Saunders et al. (2012) uses the stages-of-change model to quantify perceived severity, susceptibility, and patient movement toward action. Individuals in the initial stages of change and motivation will need counseling focused on the psychological, social, emotional and occupational effects of hearing loss. They may benefit from discussions about the benefits of amplification and rehabilitation and setting realistic expectations as well as addressing his/her personal goals. The hearing care provider can play a critical role is arming the individual with the information needed for him/her to move towards making an action plan. Indeed, the hearing care provider's goal is to guide the individual's movement towards action and acceptance of hearing assistive technology. Further, psychosocial health declines with hearing loss (Nachtegaal et al., 2009). These individuals, in conjunction with family and/or communication partners, will need individualized plans focused on coping and communication strategies, amplification and bi-sensory communication in addition to the psychosocial counseling and development of realistic expectations. Self-assessment tools, patient education materials and counseling will be essential for individuals who live with hearing loss.
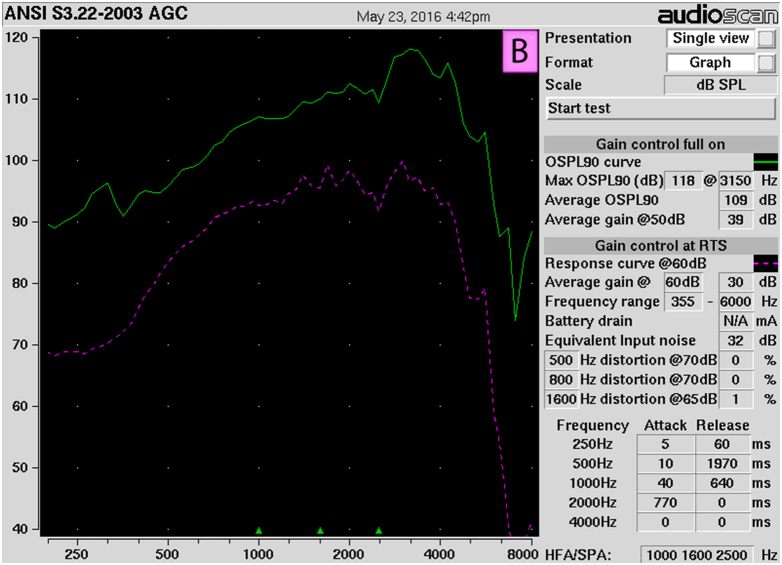
After the ideal fitting has been achieved, a frequency response curve should be obtained. This measurement is completed in a test box chamber with the aid connected to the coupler and is completed using the ANSI measurement signals (for set up see Fig. 2; ANSI (2003)). As seen in Fig. 3, a 90 dB SPL signal (solid line) followed by a 50 dB SPL (hashed line) is played and output of the aid is recorded. This is not a true ANSI curve as the output of the aid is not changed per the ANSI protocol, but uses the standardized ANSI test signals to obtain a frequency response curve at user settings. This frequency response curve can be printed for future comparison. If a patient returns to the clinic and reports that the aid is non-functional or under-performing, an ANSI curve can be compared to the initial fitting curve at their user setting. This ANSI curve can also be used to document the output of the hearing aid; the example in Fig. 3 has a highest maximum output of 118 dB SPL. The aid will not output any signals louder than 118 dB SPL; this is necessary to document for purposes of ensuring the output of the aid will not cause damage to the auditory system of the wearer. Running the ANSI curve is the final step in verification of the function of the aid, but is not the last step in appropriate and ethical fitting of hearing aids.
Fig. 2.
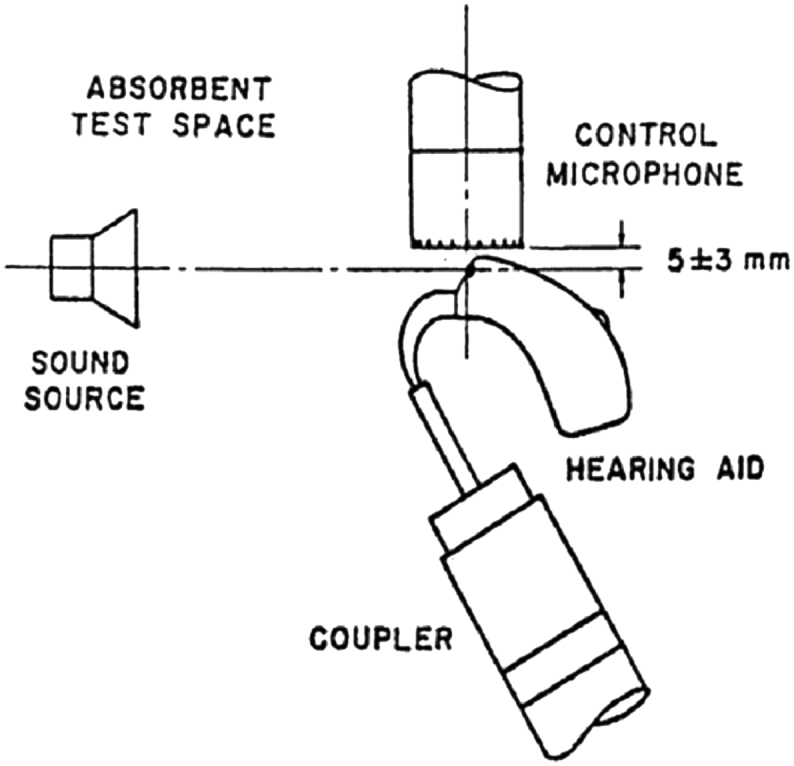
ANSI test box set up (ANSI, 2003).
Fig. 3.
ANSI output curve.
Most ideal protocols will include validating that the patient's treatment with hearing aids has been effective by comparing pre- and-post measures. This includes measurements of speech or sentence comprehension in noise and quiet and using real-world performance metrics; these can be done by using questionnaires or in the test booth. Remember, however, that these are validation measurements, not verification. The only way to know the information that the patient is receiving is via real-ear measurements. Providing counseling and aural rehabilitative services relative to the patient's specific needs is necessary for patient to use this hearing aid. These counseling services include the care and maintenance of the hearing aid, instruction on hearing aid features, such as how to appropriately place themselves in noisy situations so as to get the most out of directional microphones.
5. Discussion
According to Christensen and Groth (2008) the primary mistake was non-use of probe-microphone real-ear measurement to objectively quantify the acoustic output or gain of the hearing aids in the patient's ear canal. The real-ear measurement is an objective and accurate measurement of hearing and output; it offers a more meaningful metric than measures of functional gain. Accurate measurements are critical for assessing audibility, appropriate output for different input levels, and verification of appropriately selected prescriptive algorithms. Indeed, a most compelling reason for completing real-ear measurements is that several studies (e.g. Aarts and Cafee, 2005, Aazh and Moore, 2007, Hawkins and Cook, 2003) have reported that manufacturer's initial-fit algorithm is an inadequate amplification prescription and often provides less gain that is necessary. Despite dissent that report that real-ear verification is unnecessary as changes less than 10 dB SPL have not shown to improve a person's performance with the aid (Cunningham et al., 2001), this difference between verified targets and manufacturer first-fit has been suggested to be as much as 20 dB SPL particularly in the high frequencies. These reported differences are further evidence that verification real-ear measurements are necessary to provide appropriate gain, particularly for those with high frequency hearing loss.
In 2010, MarkeTrak focused on the impact of the hearing healthcare profession on hearing aid user success (Kochkin et al., 2010). This survey reported that there are several factors which can improve patient's success with hearing technology. The top five include: physical fit, number of required visits (lower being better), hearing healthcare professional attributes, use of real-ear measurements, and subjective benefit. It is clear that the use of real-ear measurements can impact several of these factors including number of required visits, use of real-ear measurements has been suggested to reduce return visits; professional attributes, the use of verification demonstrates high level of knowledge; and, obviously, the use of real-ear measurements. However, this survey reported that there are still a high percentage of people who are highly dissatisfied with hearing aids. It is possible, and likely, that these people are under-fit or under-counselled on appropriate expectations. Beck (2010) reported an 18% increase in satisfaction when real-ear measurements were completed as compared to those for whom hearing aid gain was verified. Additionally, Mueller (2005) in conjunction with Kochkin et al. (2010), suggested that by completing these measurements there was a reduction in patient complaints, thus decreasing repeat appointments and return-for-credit aids; they attributed this to the patient's access to an audible signal. Completing real-ear measurements can be seen as an opportunity to improve patient care and provider satisfaction or obstacle as it is something that has to be done. However, these measurements define the hearing aid provider as an expert. By providing patients with aids that are specifically fit to their needs using verification and validation measurements, the hearing aid provider is confirming the value of the aid and the practitioner.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
References
- Aarts N., Cafee C. Manufacturer predicted and measured REAR values in adult hearing aid fitting: accuracy and clinical usefulness. Int. J. Audiol. 2005;44:293–301. doi: 10.1080/14992020500057830. [DOI] [PubMed] [Google Scholar]
- Aazh H., Moore B.C. The value of routine real ear measurement of the gain of digital hearing aids. J. Am. Acad. Audiol. 2007;18:653–664. doi: 10.3766/jaaa.18.8.3. [DOI] [PubMed] [Google Scholar]
- Aazh H., Moore B.C., Prasher D. The accuracy of matching target insertion gains with open-fit hearing aids. Am. J. Audiol. 2012;21(2):175–180. doi: 10.1044/1059-0889(2012/11-0008). [DOI] [PubMed] [Google Scholar]
- American Speech Language Hearing Association (ASHA) 2006. Preferred Practice Patterns for the Profession of Audiology.http://www.asha.org/uploadedFiles/PP2006-00274.pdf Available at: [PubMed] [Google Scholar]
- Abrams H.B., Chisolm T.H., McManus M., McArdle R. Initial-fit approach versus verified prescription: comparing self-perceived hearing aid benefit. J. Am. Acad. Audiol. 2013;23(10):768–778. doi: 10.3766/jaaa.23.10.3. [DOI] [PubMed] [Google Scholar]
- ANSI . 2003. American National Standards Standard 3.22-2003 – a Revision of ANSI 3.22-1996.https://law.resource.org/pub/us/cfr/ibr/002/ansi.s3.22.2003.html Available at: [Google Scholar]
- American Speech-Language-Hearing Association . 1998. Guidelines for Hearing Aid Fitting for Adults [Guidelines]www.asha.org/policy Available from: [Google Scholar]
- Beck DL. Do real-ear measurements make a real difference to patient outcomes? Available at: www.audiology.org/news/interviews/Pages/20090119a.aspx. (accessed 09.03.10.)
- Bamford J., Beresford D., Mencher G. Provision and fitting of new technology hearing aids: implications from a survey of some “good practice services” in UK and USA. In: Seewald R.C., Gravel J.S., editors. A Sound Foundation through Early Amplification: Proceedings of an International Conference. Phonak AG; Stafa, Switzerland: 2001. pp. 213–219. [Google Scholar]
- Christensen L., Groth J. Seminar Presented at: American Academy of Audiology. 2008. Top ten clinician mistakes in geriatric hearing aid fitting. [Google Scholar]
- Cunningham D.R., Williams K.J., Goldstein L.J. Effects of providing and withholding post-fitting fine-tuning adjustments on outcome measures in novice hearing aid users: a pilot study. Am J Audiol. 2001;10:51–65. doi: 10.1044/1059-0889(2001/001). [DOI] [PubMed] [Google Scholar]
- Galster J. Staying on target. Audiol. Today. 2011 March/April: 26–30. [Google Scholar]
- Hawkins D., Cook J. Hearing aid software predictive gain values: how accurate are they? Hear. J. 2003;56(7):26–34. [Google Scholar]
- Holube I., Fredelake S., Vlaming M., Kollmeier B. Development and analysis of an international speech test signal (ISTS) Int. J. Audiol. 2010;49(12):891–903. doi: 10.3109/14992027.2010.506889. [DOI] [PubMed] [Google Scholar]
- International Hearing Society (IHS) (ND) A Professional Practice Profile for Hearing Health Professionals. Available at: http://ihsinfo.org/IhsV2/Communities_Members/Professional_Practice_Profile.cfm.
- Johnson E. 2012. 20Q: Same or Different – Comparing the Latest NAL and DSL Prescriptive Targets.http://www.audiologyonline.com/articles/20q-same-or-different-comparing-769 Audiology Online. Available at: [Google Scholar]
- Johnson E.E., Dillon H. A comparison of gain for adults from generic hearing aid prescriptive methods: impacts on predicted loudness, frequency bandwidth, and speech intelligibility. J. Am. Acad. Audiol. 2011;22(7):441–459. doi: 10.3766/jaaa.22.7.5. [DOI] [PubMed] [Google Scholar]
- Keidser G., Dillon H., Flax M., Ching T., Brewer S. The NAL-NL2 prescription procedure. Audiol. Res. 2011;1:88–90. doi: 10.4081/audiores.2011.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkwood D. Survey: dispensers fitted more hearing aids in 2005 at higher prices. Hear. J. 2006;59(4):40–50. [Google Scholar]
- Kochkin S., Beck D., Christensen L., Compton-Conley C., Fligro B., …, Turner R. MarkeTrak VIII: the impact of the hearing healthcare professional on hearing aid user success. Hear. Rev. 2010;17(4):12–34. [Google Scholar]
- Leavitt R.J., Flexer C. The importance of audibility in successful amplification of hearing loss. Hear. Rev. 2012;19(13):20–23. [Google Scholar]
- Mueller H.G. A candid round table discussion on open-canal hearing aid fittings. Hear. J. 2009;62(4):19–26. [Google Scholar]
- Mueller H.G. Probe-mic measures: hearing aid fitting's most neglected element. Hear. J. 2005;28(10):21–30. [Google Scholar]
- Mueller H.G., Picou E.M. Survey examines popularity of real-ear probe-microphone measures. Hear. J. 2010;63(5):27–28. [Google Scholar]
- Nachtegaal J., Smit J., Smits C., Bezemer P., van Beek J., Festen J., Kramer S. The Association between Hearing Status and Psychosocial Health before the Age of 70 Years: results from an Internet-Based National Survey on Hearing. Ear & Hearing. 2009;30(3):302–312. doi: 10.1097/AUD.0b013e31819c6e01. [DOI] [PubMed] [Google Scholar]
- Sanders J., Stoody T., Weber J., Mueller H.G. Manufacturers' NAL-NL2 fittings fail real-ear verification. Hear. Rev. 2015;21(3):24. [Google Scholar]
- Saunders G.H., Chisolm T.H., Wallhagen M.I. Older adults and hearing help-seeking behaviors. Am. J. Audiol. 2012;21(2):331–337. doi: 10.1044/1059-0889(2012/12-0028). [DOI] [PubMed] [Google Scholar]
- Thornton A., Raffin M. Speech-discrimination scores modeled as a binomial variable. J. Speech Hear. Res. 1978;21(3):507–518. doi: 10.1044/jshr.2103.507. [DOI] [PubMed] [Google Scholar]
- Valente M., 2006. Guideline for Audiologic Management of the Adult Patient. Available at: www.audiologyonline.com/articles/article_detail.asp?article_id=1716.
- Valente M. Audiological management of adult hearing impairment. Audiol. Today. 2006;18(5):32–36. [Google Scholar]
- Wu Y., Bentler R. Clinical measures of hearing aid directivity: assumption, accuracy and reliability. Ear Hear. 2012;33(1):L 44–56. doi: 10.1097/AUD.0b013e3182292107. [DOI] [PubMed] [Google Scholar]