Abstract
Objective
To evaluate the efficacy and safety of intratympanic and systemic steroid therapies in the initial treatment of Sudden Sensorineural Hearing Loss (SSNHL) patients.
Methods
A comprehensive search of PubMed, Wanfang database and CNKI (China National Knowledge Infrastructure) was performed covering the period from January 1990 to July 2014. A meta-analysis was conducted after filtering by the criteria of Cochrane Collaboration. Three hundred fifty six subjects in nine studies allocated to the group of intratympanic steroid therapies and 343 controls receiving systemic steroid therapies met the criteria for meta-analysis. The data were extracted and analyzed using the RevMan 5.3 meta-analysis software.
Results
The total effectiveness rate in SSNHL patients receiving intratympanic steroid therapies did not differ statistically from patients receiving systemic therapies (RR = 1.08, 95%CI = 0.99–1.99, P = 0.10), although the rate of full hearing recovery in this group differed significantly from patients receiving systemic therapies (RR = 1.29, 95%CI = 1.00–1.66, P = 0.05).
Conclusion
Local steroid therapy appears to generate higher rate of complete hearing recovery than systemic steroid treatment as an initial treatment for SSNHL, which may be especially useful for patients in whom systemic steroids are contraindicated.
Keywords: Sudden sensorineural hearing loss, Intratympanic steroids, Systemic steroid, Meta-analysis
1. Introduction
Sudden Sensorineural Hearing Loss (SSNHL), first reported by De Kleyn (Seggas et al., 2010) in 1944, is an otologic event that needs urgent intervention. SSNHL is commonly defined as hearing loss greater than 30 dB and involving at least 3 consecutive audiometric frequencies, occurring within 3 days without any identifiable cause (Seggas et al., 2010, Arastou et al., 2013). Although a number of theories regarding the cause have been suggested, the etiologies and pathogenesis of SSNHL are still unclear. The overall incidence of diagnosed SSNHL ranges from 5 to 20 per 100,000 persons per year (Seggas et al., 2010, Arslan et al., 2011, Battaglia et al., 2008). The rate of spontaneous recovery without treatment ranges 32–65% (Seggas et al., 2010, Arastou et al., 2013, Battaglia et al., 2008), and the rate of full recovery in treated patients ranges 49–79% (Arastou et al., 2013, Battaglia et al., 2008).
The cause of SSNHL has been the subject of debate for many years and has been widely studied. The suggested theories include vascular compromise, viral infection, and immune-mediated reactions (Seggas et al., 2010, Arslan et al., 2011). The condition may well have a multifactorial etiology and each of the above mentioned mechanisms may be responsible for a proportion of the total number of observed cases.
A number of treatments have been reported, such as vasoactive substances, hyperbaric oxygen, antivirals and vitamins (Crane et al., 2014, Koltsidopoulos et al., 2013). Each approach has, however, been debated with no standard protocol universally accepted until the introduction of steroid therapy. Administration of steroids, systemically or intratympanally, alone or in combination, is considered to be the mainstay of treatment for SSNHL (Arslan et al., 2011, Battaglia et al., 2008, Crane et al., 2014). Systemic steroid therapy, however, has serious adverse effects and contraindications and therefore local use of steroids has attracted popularity among otology centers during the last decade (Koltsidopoulos et al., 2013).
In the present study we performed a review of randomized controlled trials (RCTs) involving the use of intratympanic steroid therapy (IST) or systemic steroid therapy (SST) for initial treatment in SSNHL patients. The aim of the meta-analysis was to evaluate the efficacy and safety of IST and determine whether this treatment is more effective as a primary treatment for SSNHL than SST.
2. Materials and methods
2.1. Strategy and criteria
Literature search was performed using a combination of the keywords “sudden hearing loss”, “hearing loss”, ‘‘steroid’’, “transtympanic” and ‘‘intratympanic’’. PubMed, Wanfang database and CNKI were searched to yield all possible relevant results. Articles limited to human subjects and published in the English or Chinese languages between January 1990 and July 2014 were included. All RCTs based on the use of steroids and the efficacies of intratympanic and systemic steroid treatments in patients with SSNHL were assessed. Two authors collected and extracted the data independently. Disagreements were solved through discussion. RCTs fulfilling the following criteria were included: (1) the RCT was designed to study the efficacy and safety of SST and IST as initial treatment of SSNHL; (2) SSNHL was reliably diagnosed, excluding other causes, and the RCT presented with a control arm (systemic steroid treatment) and a treatment arm (intratympanic steroids), as well as a clear description of the steroid treatment regimen; (3) the age and sex in the treatment and control groups were not limited, but with no significant difference at baseline.
Data fulfilling the following criteria were excluded: (i) articles that were reviews, expert commentaries, case reports or other non-clinical research literature, (ii) trials that had incomplete reporting of pre- and post-treatment PTA results, (iii) trials that did not evaluate steroids as a primary treatment of SSNHL, and did not evaluate systemic steroids alone or intratympanic steroids alone as the primary treatment.
Nine studies met the criteria and were included for analysis (Table 1). The following information was extracted from each article: sample size of each study arm, type and dose of steroids, methods of steroid administration, duration of therapy, outcomes, major complications and follow-up time.
Table 1.
Characteristics of the included research.
| Included literature (author, published time) | Intratympanic therapy |
Systemic therapy |
Follow-up time | ||||
|---|---|---|---|---|---|---|---|
| Drug | Usage and dosage | Time | Drug | Usage and dosage | Time | ||
| Lim et al. (2013) | Dexamethasone | Intratympanic injection, 1.5–2 mg | 2w | Prednisone | Oral, 60 mg/d | 10d | 3w |
| Rauch et al. (2011) | Methylprednisolone | Intratympanic injection, 40 mg | 2w | Prednisone | Oral, 60 mg/d | 19d | 6m |
| Dispenza et al. (2011) | Dexamethasone | Intratympanic injection, 4 mg | 4w | Prednisone | Oral, 6 mg/d | 14d | 6m |
| Zhou et al. (2006) | Dexamethasone | Intratympanic injection, 2.5 mg | 8d | Prednisone | Oral, 30 mg/d | 8d | 20d |
| Peng et al. (2008) | Dexamethasone | Intratympanic injection, 5 mg | 10d | Dexamethasone | Intravenous, 10 mg | 10d | 20d |
| Deng (2011) | Dexamethasone | Intratympanic injection, 1 mg | 10d | Dexamethasone | Intravenous, 10 mg | 10d | 30d |
| Yi et al. (2011) | Dexamethasone | Auditory tube injection, 5 mg | 10d | Dexamethasone | Intravenous,10 mg | 7d | 30d |
| You et al. (2008) | Dexamethasone | Intratympanic injection, 1–1.5 mg | 10d | Dexamethasone | Intravenous, 10 mg | 10d | 15d |
| Mao et al. (2005) | Methylprednisolone | Auditory tube injection, 5 mg | 10d | Methylprednisolone | Intravenous, 40 mg | 7d | 20d |
After identifying the reports, the abstract and full text were carefully read and the publication's quality was screened and evaluated according to the Handbook of System Quality Evaluation of Cochrane criteria. Pre- and post-treatment pure-tone audiometry (PTA) results were noted. Treatment efficacy was determined in accordance to the sudden deafness diagnosis and treatment standards by the Chinese Medical Association Otolaryngology Head and Neck Surgery Branch, Ji'nan, 2005. A change of hearing thresholds within the 250–4000 Hz frequency range back to within normal range, or to the level of the healthy ear, or back to the level before SSNHL was considered to represent a full recovery (cured); and a threshold recovery of 15 dB or greater was considered to indicate significant improvement (Spear and Schwartz, 2011). The rates of full recovery and significant improvements were calculated.
2.2. Statistical analysis
Data analysis was performed with the RevMan5.3 software. Tests of heterogeneity were conducted with the chi-square test, as an x2 variate. Between-study heterogeneity was assessed using the I2, as the percentage of variability among effect estimates beyond that expected by chance (Ng et al., 2014). As a reference, I2 values of 25% were considered low, 50% as moderate, and 75% as high (Ng et al., 2014). If the result did not show heterogeneity (i.e. I2 < 50%, P > 0.10), the fixed-effect model was used for calculation. If a clinical heterogeneity existed, the random-effects mode was used. The Mantel–Haenszel method was used to summarize the results, by calculation of the combined Risk Ratio (RR) and 95% confidence intervals (95% CI), and forest plots were generated.
3. Results
Nine studies met the inclusion criteria and revealed rates of significant improvement and full recovery. The nine studies were published from 2005 to 2013. For intratympanic therapies, dexamethasone (Lim et al., 2013, Dispenza et al., 2011, Zhou et al., 2006, Peng et al., 2008, Deng, 2011, Yi et al., 2011, You et al., 2008) and methylprednisolone (Rauch et al., 2011, Mao et al., 2005) were used, either through the tympanic membrane (Lim et al., 2013, Rauch et al., 2011, Dispenza et al., 2011, Zhou et al., 2006, Peng et al., 2008, Deng, 2011, You et al., 2008) or via the auditory tube (Yi et al., 2011, Mao et al., 2005). The drugs administered systemically were prednisone (Lim et al., 2013, Rauch et al., 2011, Dispenza et al., 2011, Zhou et al., 2006), dexamethasone (Peng et al., 2008, Deng, 2011, Yi et al., 2011, You et al., 2008) and methylprednisolone (Mao et al., 2005), via oral (Lim et al., 2013, Rauch et al., 2011, Dispenza et al., 2011, Zhou et al., 2006) or intravenous (Peng et al., 2008, Deng, 2011, Yi et al., 2011, You et al., 2008, Mao et al., 2005) routes. Data from the nine studies were pooled for meta-analysis.
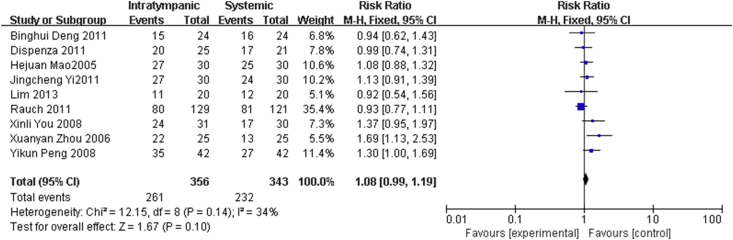
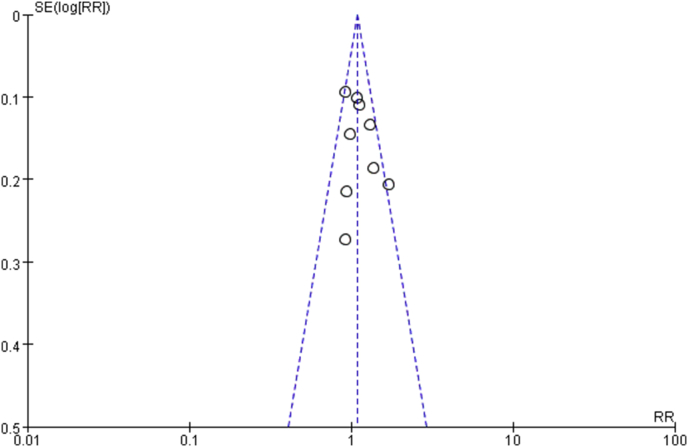
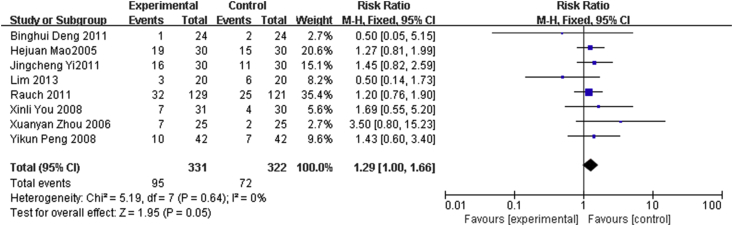
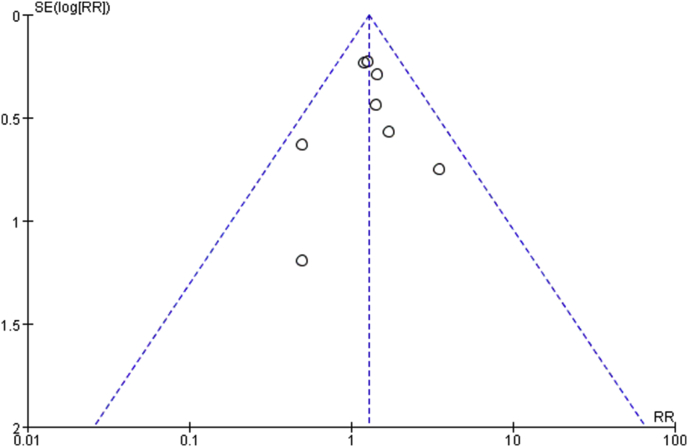
A forest plot was created to depict the results of individual studies along with the summary results derived from the meta-analyses. Results showed that patients who received intratympanic steroids therapies demonstrated a statistically significant improvement in the hearing threshold as compared to those receiving systemic steroids therapies, reflecting that local steroids treatments for SSNHL was more effective than systemic therapies. Fig. 1 presents the rate of total effectiveness for local steroids treatments in comparison to systemic steroids treatments. The forest plot results are: x2 = 12.15, p = 0.14, I2 = 34%. As can be seen from the figure, I2 = 34% < 50%, P = 0.14 > 0.10, indicates no heterogeneity and justification for using the fixed-effect model. The Mantel–Haenszel method was used to summarize the results. The total Risk Ratio (RR) was 1.08 and the 95% confidence intervals (95% CI) was 0.99–1.19. The overall effect, Z = 1.67, P = 0.10 > 0.05, did not indicate statistically significant difference between the rates of total effectiveness for local and systemic steroids therapies. Fig. 2 presents the funnel plots of local and systemic steroids treatments. In the funnel plot, each point is distributed symmetrically, indicating low publication bias. Fig. 3 compares the rates of full recovery for local and systemic steroids treatments. The forest plot results are x2 = 5.19, p = 0.64, I2 = 0%. The figure shows I2 = 0% < 50%, P = 0.64 > 0.10, again indicating no heterogeneity and justification for using the fixed-effect model. The Mantel–Haenszel method showed that the total RR was 1.29 and the 95% CI was 1.00–1.66. The overall effect, Z = 1.95, P = 0.05 = 0.05, showed a statistically significant difference. Fig. 4 presents a funnel plot of the number of patients with full recovery. Each point in the funnel plot is distributed symmetrically, indicating low publication bias.
Fig. 1.
Meta-analysis forest map of the rate of significant improvement for local and systemic glucocorticoid treatments for SSNHL.
Fig. 2.
Meta-analysis funnel plot of local and systemic glucocorticoid treatment for SSNHL.
Fig. 3.
Meta-analysis forest map of the rate of full recovery for local and systemic glucocorticoid treatments for SSNHL.
Fig. 4.
Meta-analysis funnel plot of articles of local and systemic glucocorticoid treatments for SSNHL depicting the number of patients with full recovery.
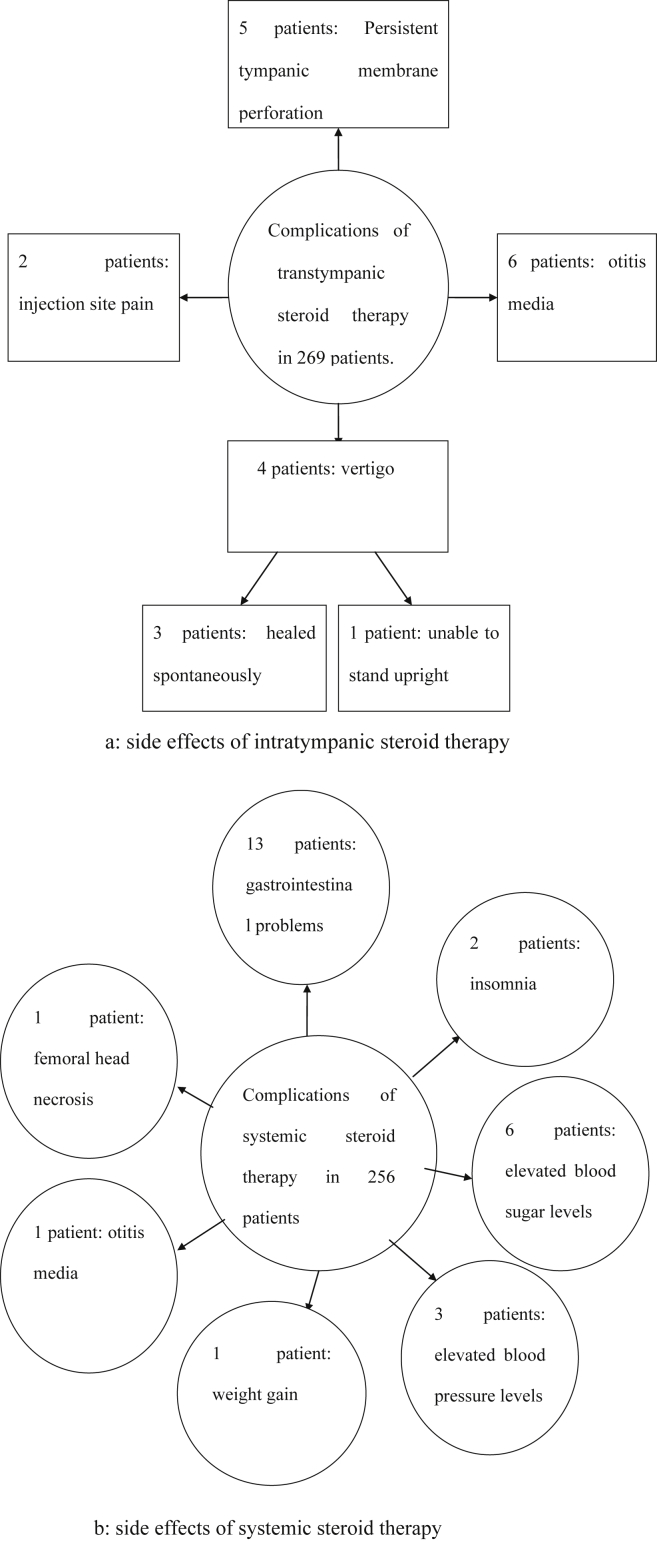
Side effects of intratympanic and systemic steroid therapies were reported in six (Rauch et al., 2011, Dispenza et al., 2011, Deng, 2011, Yi et al., 2011, You et al., 2008, Mao et al., 2005) of the nine studies. Complications of transtympanic steroid therapy included vertigo, otalgia, nystagmus, otitis media, tinnitus, injection site pain, and persistent tympanic membrane perforations. Of the 269 patients in these studies, 4 developed vertigo (Deng, 2011), of whom 3 resolved spontaneously, one was unable to stand upright and discontinued the treatment. Persistent tympanic membrane perforation was seen in 5 patients (Rauch et al., 2011), and 6 patients suffered from otitis media (Rauch et al., 2011). Two patients in the intratympanic treatment group withdrew consent due to injection site pain (Rauch et al., 2011). No infectious complications occurred. Adverse reactions of systemic steroids use were cardiovascular, gastrointestinal, neurologic, and endocrine problems. Of the 256 patients in these studies, 13 developed gastrointestinal problems (Deng, 2011, Yi et al., 2011, Mao et al., 2005), 2 had insomnia (You et al., 2008), 6 had elevated blood sugar levels (Deng, 2011, Yi et al., 2011), 3 showed elevated blood pressure levels (Deng, 2011, Yi et al., 2011), and 1 developed weight gain (You et al., 2008). Otitis media occurred in 1 patient (Rauch et al., 2011) and 1 patient suffered right femoral head necrosis (Mao et al., 2005), the latter being the most serious complication showed in Fig. 5). No other serious complications occurred in the two groups.
Fig. 5.
Side effects from intratympanic and systemic steroid therapies.
4. Discussion
Treatment strategies for SSNHL vary widely and remain a challenge for otologists. Since 1980, administration of cortico-steroids (systemic and/or intratympanic) has been the mainstay therapy for SSNHL (Battaglia et al., 2008, Koltsidopoulos et al., 2013, Stachler, 2012). However, there is a limited amount of clinical data and the efficacy and safety of steroids for treatment in SSNHL remain controversial.
In the nine randomized controlled trials, the total effectiveness of local steroids in treating SSNHL was similar to that of systemic steroid therapies. In contrast, the rate of full recovery in local steroid treatment was higher than that in systemic therapies. Systemic steroids may increase the risks of important adverse effects, such as femoral head necrosis, gastrointestinal and endocrine problems, and weight gain. In the systemic steroid group, a total of 29 patients suffered side effects. By comparison, 17 people had side effects in the local glucocorticoid group. Systemic administration of steroids may have broad effects on body functions, including numerous adverse reactions, especially in long-term use. Due to side effects from systemic administration of steroids, intratympanic administration of steroids has been utilized (Kakehata et al., 2006, Hong et al., 2009). Local administration of steroids via the middle ear cavity may act directly on the inner ear at a higher concentration, without risks of systemic complications or cochlear dysfunctions – advantages that may make it an ideal choice for SSNHL in certain patient groups. Intratympanic steroid treatment has been used in patients in whom systemic steroids are contraindicated; i.e., in patients with immunocompromising disturbances, diabetes, hypertension, peptic ulcer, and tuberculosis.
The number of clinical trials, meta-analyses and reviews concerning steroid therapy for SSNHL is large world-wide with no consistent conclusions. Studies on SSNHL patients have shown efficacy for intratympanic steroids as an initial treatment and as a salvage therapy for refractory patients (Hong et al., 2009, Koltsidopoulos et al., 2013, Lee et al., 2011, Wu et al., 2011), and when combined with systemic steroids (Arastou et al., 2013, Arslan et al., 2011, Gundogan et al., 2013, Kakehata et al., 2011). Seggas et al. (2010) carried out a study to seek the most effective technique and optimal administration schedule by examining the published literature regarding the therapeutic value of each method of treatment. They concluded that topical steroids can be a valuable solution for SSNHL patients who either cannot tolerate systemic steroid therapy or are refractory to it. Ding et al. (2013) stated, in studies on SSNHL patients with diabetes, that local steroids should be the first treatment of choice. Thus, local steroid treatment has been assumed to be a suitable alternative when there are medical contraindications to oral prednisone administration. In another study, Arastou et al. (2013) evaluated the efficacy of combined intratympanic and systemic steroid therapies compared with systemic steroid therapy alone in SSNHL patients with poor prognostic factors (age greater than 40 years, hearing loss of more than 70 dB, and a greater than 2-week delay between the onset of hearing loss and initiation of therapy). It was concluded that combined intratympanic and systemic steroid therapy showed a higher efficacy than systemic prednisolone alone in the treatment of SSNHL patients with poor prognosis. So SSNHL patients with poor prognostic factors can consider choosing combined intratympanic and systemic steroid therapies. Ng et al. (2014) conducted a meta-analysis to evaluate the efficacy of intratympanic steroids as a salvage treatment for patients who have initial treatment failure with systemic steroids. They showed salvage intratympanic steroids to be superior to no further treatment in patients who have failed systemic steroids.
In the present meta-analysis, we systematically scrutinized English and Chinese literature on systemic and local administration of corticosteroids in SSNHL patients. The systemic corticosteroids administered in all trials by oral or intravenous routes were prednisone, dexamethasone, and methylprednisolone at a dose of 30–60 mg/d (oral) or 10 mg/d (intravenous) for 7–10 days. Intratympanic administration of steroids was performed about four times during a 1 month treatment period, at a dose of 1–40 mg/injection (dexamethasone) or 5 mg/injection (methylprednisolone). Our meta-analysis showed that the dose in intratympanic steroid treatment was considerably lower compared to that in systemic administration.
The purpose of our meta-analysis was to evaluate the efficacy and safety of intratympanic and systemic steroid therapies in the initial treatment for patients with SSNHL. The study showed that the two different treatment protocols, systemic and local steroids, resulted in similar rates of hearing improvement but were different in the rate of complete recovery. Moreover, local steroids carried lower risks of side effects as compared to systemic treatments. We therefore recommend transtympanic steroid administration as an initial treatment for those in whom initial systemic steroid treatment has failed.
Our meta-analysis has limitations. The type of steroids used varied as well as the duration and dose of treatment (Table 1). For example, dexamethasone was used in 8 studies and methylprednisolone in the remaining study. The dose of dexamethasone ranged from 1 to 5 mg, and the administration schedule varied from once a week for 4 consecutive weeks to daily administration for 8 or 10 consecutive days. Because of the limited number of trials and the variability regarding duration and dose, subgroup analyses, such as comparisons between dexamethasone and methylprednisolone or between transtympanic injections and administration via the auditory tube, could not be performed.
Some trials contained a small number of patients. Despite that most of these studies showed a statistically significant benefit, it cannot be excluded that studies with a similar sample size but with negative results did not reach enough priority for publication. Furthermore, publication bias cannot be completely ruled out, although the funnel plots showed a low publication bias. However, larger RCTs are required to definitely confirm this conclusion.
The present study showed a statistically significant difference between intratympanic and systemic steroid treatments for SSNHL. Intratympanic steroid treatment is an effective procedure that allows focused treatment of the ear of the affected side only, a factor which can reduce pharmacological interactions. Despite the risks for adverse effects such as infection, residual tympanic perforation and vertigo, complications are less frequent than with systemic treatment.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
References
- Arastou S., Tajedini A., Borghei P. Combined intratympanic and systemic steroid therapy for poor-prognosis sudden sensorineural hearing loss. Iran. J. Otorhinolaryngol. 2013;1(25):23–28. [PMC free article] [PubMed] [Google Scholar]
- Arslan N., Oğuz H., Bakanligi S. Combined intratympanic and systemic use of steroids for idiopathic sudden sensorineural hearing loss. Otol. Neurotol. 2011;32(3):393–397. doi: 10.1097/MAO.0b013e318206fdfa. [DOI] [PubMed] [Google Scholar]
- Battaglia A., Burchette R., Cueva R. Combination therapy (intratympanic dexamethasone + high-dose prednisone taper) for the treatment of idiopathic sudden sensorineural hearing loss. Otol. Neurotol. 2008;29(4):453–460. doi: 10.1097/MAO.0b013e318168da7a. [DOI] [PubMed] [Google Scholar]
- Crane R.A., Camilon M., Nguyen S., et al. Steroids for treatment of sudden sensorineural hearing loss: a meta-analysis of randomized controlled trials. Laryngoscope. 2014 Jul 21. http://dx.doi.org/10.1002/lary.24834. (Epub ahead of print). [DOI] [PubMed]
- Deng B.H. Single use of hormone to treat sudden sensorineural hearing loss and comparison of two different administration ways. J. Clin. Med. Eng. 2011;18(8):1238–1239. [Google Scholar]
- Ding X.Y., Cui T.T., Feng G.D. Intratympanie versus systemic steroid treatment for idiopathic sudden hearing loss: a meta-analysis. China J. Otorhinolaryngol. Head Neck Surg. 2013;48(5):412–416. [PubMed] [Google Scholar]
- Dispenza F., Amodio E., De Stefano A. Treatment of sudden sensorineural hearing loss with transtympanic injection of steroids as single therapy: a randomized clinical study. Eur. Arch. Otorhinolaryngol. 2011;268(9):1273–1278. doi: 10.1007/s00405-011-1523-0. [DOI] [PubMed] [Google Scholar]
- Gundogan O., Pinar E., Imre A. Therapeutic efficacy of the combination of intratympanic methylprednisolone and oral steroid for idiopathic sudden deafness. Otolaryngol. Head Neck Surg. 2013;149(5):753–758. doi: 10.1177/0194599813500754. [DOI] [PubMed] [Google Scholar]
- Hong S.M., Park C.H., Lee J.H. Hearing outcomes of daily intratympanic dexamethasone alone as a primary treatment modality for ISSHL. Otolaryngol. Head Neck. 2009;141(5):579–583. doi: 10.1016/j.otohns.2009.08.009. [DOI] [PubMed] [Google Scholar]
- Kakehata S., Sasaki A., Oji K. Comparison of intratympanic and intravenous dexamethasone treatment on sudden sensorineural hearing loss with diabetes. Otol. Neurotol. 2006;27(5):604–608. doi: 10.1097/01.mao.0000224092.79635.ee. [DOI] [PubMed] [Google Scholar]
- Kakehata S., Sasaki A., Futai K. Daily short-term intratympanic dexamethasone treatment alone as an initial or salvage treatment for idiopathic sudden sensorineural hearing loss. Audiol. Neurootol. 2011;16(3):191–197. doi: 10.1159/000320269. [DOI] [PubMed] [Google Scholar]
- Koltsidopoulos P., Bibas A., Sismanis A. Intratympanic and systemic steroids for sudden hearing loss. Otol. Neurotol. 2013;34(4):771–776. doi: 10.1097/MAO.0b013e31828bb567. [DOI] [PubMed] [Google Scholar]
- Lee J.B., Choi S.J., Park K. The efficiencyof intratympanic dexamethasone injection as a sequential treatment after initial systemic steroid therapy for sudden sensorineural hearing loss. Eur. Arch. Otorhinolaryngol. 2011;268(6):833–839. doi: 10.1007/s00405-010-1476-8. [DOI] [PubMed] [Google Scholar]
- Lim H.J., Kim Y.T., Choi S.J. Efficacy of 3 different steroid treatments for sudden sensorineural hearing loss: a prospective, randomized trial. Otolaryngol.–Head Neck Surg. 2013;148(1):121–127. doi: 10.1177/0194599812464475. [DOI] [PubMed] [Google Scholar]
- Mao H.J., Lu Z.M., Zhang R.H. Comparison of the effects of two different administration routes with hormone on sudden hearing loss. Chin. J. Misdiagnostics. 2005;5(12):2203–2204. [Google Scholar]
- Ng JH, Ho RC, Cheong CS, et al. Intratympanic steroids as a salvage treatment for sudden sensorineural hearing loss? A meta-analysis. Eur. Arch. Otorhinolaryngol..2014 Sep 13. (Epub ahead of print). [DOI] [PubMed]
- Peng Y.K., Xiong S.Z., Cheng Y.H. Clinical investigation of different routes of administration of dexamethasone on sudden deafness. J. Clin. Otorhinolaryngol. Head Neck Surg. (China) 2008;22(10):442–445. [PubMed] [Google Scholar]
- Rauch S.D., Halpin C.F., Antonelli P.J. Oral vs intratympanie cortieosteroid therapy for idiopathic sadden sensorineural heating loss: a randomized trial. JAMA. 2011;305(20):2071–2079. doi: 10.1001/jama.2011.679. [DOI] [PubMed] [Google Scholar]
- Seggas I., Koltsidopoulos P., Bibas A. Intratympanic steroid therapy for sudden hearing loss: a review of literature. Otol. Neurotol. 2010;32(1):29–35. doi: 10.1097/mao.0b013e3181f7aba3. [DOI] [PubMed] [Google Scholar]
- Spear Samuel A., Schwartz Seth R. Intratympanic steroids for sudden sensorineural hearing loss: a systematic review. Otolaryngol.–Head Neck Surg. 2011;145(4):534–543. doi: 10.1177/0194599811419466. [DOI] [PubMed] [Google Scholar]
- Stachler R.J. Clinical practice guideline. Otolaryngol. Head Neck Surg. 2012;146(1S):S1–S35. doi: 10.1177/0194599812436449. [DOI] [PubMed] [Google Scholar]
- Wu H.P., Chou Y.F., Yu S.H. Intratympanic steroid injections as a salvage treatment for sudden sensorineural hearing loss: a randomized, double-blind, placebo-controlled study. Otol. Neurotol. 2011;32(5):774–779. doi: 10.1097/MAO.0b013e31821fbdd1. [DOI] [PubMed] [Google Scholar]
- Yi J.C., Chen S., Huang C.Y. Observation on the therapeutic effect of eustachian tubeinjection of dexamethasone in treatment of sudden deafness. Guangxi Med. J. 2011;33(2):179–180. [Google Scholar]
- You X.L., Lin X., Zhu B.C. Local and systemic glucocorticoid treatment for sudden hearing loss. China Prac. Med. 2008;3(28):125–127. [Google Scholar]
- Zhou X.Y., Tao Q., Lv L.Y. The treatment for sudden deafness with intratympanic dexamethasone injection. Chin. J. Otorhinolaryngol. -Skull Base Surg. 2006;12(1):47–48. [Google Scholar]