Abstract
1 Background
Suicide in low- and middle-income countries (LMICs) accounts for 75% of the world’s burden of suicide mortality and is the leading single cause of death among Nepali reproductive age women. To advance treatment for suicidal behaviors in LMICs, a single-case experimental design (SCED) was conducted of a culturally adapted Dialectical Behavior Therapy skills intervention for Nepali populations (DBT-N).
2 Method
Ten Nepali women with histories of suicidality participated in the 10-session intervention. Outcomes of emotion regulation, suicidal ideation, depression, anxiety, resilience, and coping skills use were measured at multiple time points pre-intervention, during, and at follow-up. Qualitative interviewing assessed DBT-N’s feasibility and acceptability.
3 Results
Participants showed improvements in emotion regulation over the course of treatment, which were associated with increased skills use. Rapid, sustained reductions in suicidal ideation and improvements in resilience were observed after DBT-N initiation.
4 Conclusion
This SCED supports conducting further evaluation of DBT-N through controlled trials with emotion regulation as a target mechanism of action for reducing suicidal behaviors in LMICs.
Suicide accounts for 800,000 deaths annually (World Health Organization, 2014). Globally, 75% of suicide deaths occur in low- and middle-income countries (LMICs), and for every incident of completed suicide, an estimated 20 attempts occur. LMICs in South and East Asia account for the greatest burden of suicide deaths (39%) and have the highest average regional rates (17.7 per 100,000). Nepal exemplifies this regional public health crisis: among women of childbearing age, suicide is the leading single cause of mortality, accounting for over 16% of deaths, with a rate of 28/100,000 (Suvedi et al., 2009).
The World Health Organization (WHO) has drawn attention to the dearth of evidence-based initiatives addressing suicide and nonsuicidal self-injury (NSSI) in LMICs (WHO, 2014). One treatment with strong potential for cultural adaptation and dissemination in resource-strained global mental health contexts is dialectical behavior therapy (DBT; Linehan, 1993a), a skills-based cognitive behavioral therapy with robust empirical support for reducing suicide risk in individuals with complex diagnoses. DBT’s underlying theory posits that suicidal behaviors (e.g., suicidal ideation, NSSI, and suicide attempts) result from difficulties regulating emotions or are themselves maladaptive emotion regulation strategies for reducing chronic and intense negative affect. Though the majority of controlled trials using DBT have examined changes in suicidal behaviors in individuals with borderline personality disorder (BPD) or BPD traits (e.g., Carter, Wilcox, Lewin, Conrad, & Bendit, 2010; Harned, Korslund, & Linehan, 2014; Koons et al., 2001; Linehan et al., 1991, 1999, 2006, 2015; McMain et al., 2009; Pistorello, Fruzzetti, MacLane, Gallop, & Iverson, 2012), a number of recent trials have demonstrated the efficacy of standard or skills-only DBT in addressing a wider range of psychopathology (e.g., depression, anxiety, eating disorders) with hypothesized roots in maladaptive emotion regulation (e.g., Goldstein et al., 2015; Hill, Craighead, & Safer, 2011; Neacsiu, Eberle, Kramer, Wiesmann, & Linehan, 2014; Telch, Agras, & Linehan, 2001).
DBT is unique in its potential for cross-cultural application in LMIC settings like Nepal. First, DBT is rooted in Eastern spiritual traditions that align with South and East Asian religious beliefs (Robins & Chapman, 2004). Buddhist practices, such as mindfulness, acceptance, and dialectical truth—foundations for DBT’s theoretical development—overlap with Nepali ethnopsychological1 divisions of the mind, body, and self (Kohrt & Harper, 2008). Second, DBT offers a flexible, contextual, and principle-driven view of behavior that incorporates tailoring of treatment components to clients’ unique life circumstances (Hayes, Villatte, Levin, & Hildebrandt, 2011), rendering it amendable to cultural adaptation. Third, DBT’s origins in a skills-deficit model and its resulting emphasis on modular skills training via a group setting may encourage delivery of treatment components by paraprofessionals, thereby increasing its ability to be scaled up in resource-poor contexts where poor access to mental health services remains chronic and severe (Singla et al., 2017). Further, DBT’s emphasis on treating core, transdiagnostic processes of emotion dysregulation has added value in allowing clinicians to address psychopathology crossing DSM-defined diagnostic boundaries (e.g., Murray et al., 2014).
Despite this potential, the overwhelming majority of DBT trials have been conducted in western, educated, industrialized, rich, and democratic (WEIRD) settings with limited inclusion of culturally diverse samples. Despite cross-cultural adaptations of DBT with Native American and Latino populations (e.g., Beckstead, Lambert, DuBose, & Linehan, 2015; Germán et al., 2015), these trials were restricted to the United States and lack extensive empirical evaluation. Outside of the United States, virtually no published trials have evaluated the treatment’s performance in resource-strained LMIC settings. Further, to the authors’ knowledge, no published studies have examined intra-individual changes in programs addressing suicidal behaviors in order to identify potential mechanisms of action. Single-case experimental designs (SCEDs) are one alternative to group-comparison, cross-sectional designs, and may provide a powerful means of identifying these idiographic differences in treatment response (Kazdin, 2003).
The objective of this study was to contribute to the growing call for person-centered psychology (Barlow & Nock, 2009) by evaluating the idiographic performance of a culturally adapted DBT skills training intervention in a low-resource, rural Nepali context. The primary aim was to provide an initial evaluation of culturally adapted DBT skills for Nepali populations (DBT-N; Ramaiya, Fiorillo, Regmi, Robins, & Kohrt, 2017) in reducing psychological distress in low-literacy women with prior histories of suicidality. A SCED was used to identify intra- as well as inter-individual changes in psychological functioning across domains associated with emotion dysregulation, our theorized and target mechanism of change. We hypothesized that DBT-N would result in improvements in individual emotion regulation, and that increases in emotion regulation would predict increases in DBT skills use over time. A secondary aim was to use client semi-structured interviews to provide broader insight into DBT-N’s feasibility and acceptability. To the authors’ knowledge, this study is the first SCED of a cultural modification of DBT skills training in a non-WEIRD, LMIC setting.
1 METHODS
1.1 Setting
The study was conducted in Jumla, a mountainous and semi-isolated district in northwestern Nepal. Rural Nepal is characterized by poor access to physical health care, high rates of poverty and illiteracy, and negligible mental health services and infrastructure (United Nations Development Programme, 2004). With a population of over 100,000, Jumla has nine health posts and one hospital with five doctors. In 2007–08, following a decade-long civil war, rates of depression and anxiety in Jumla were 40.6% and 47.7%, respectively (Kohrt et al., 2012).
1.2 Design
The present study employed a mixed-methods SCED series following a classic AB design with repeated follow-up. Quantitative measures were assessed at each of the following timepoints: baseline measurements were taken during a wait-list period (A; two weekly time points), followed by weekly measurement following treatment initiation (B; nine weekly time points), and a follow-up period to assess for sustained trends following termination (one- and four-week time points).
1.3 Intervention
A tri-phasic, iterative approach was employed to culturally modify the standard DBT regimen to develop DBT-N (Ramaiya et al., 2017). DBT-N development was heavily guided by grounded theory methodology and was thus specifically designed for use in Nepal and similar resource-strained, South Asian settings. All intervention content, teaching strategies, and curriculum materials were designed for delivery by lay providers with no prior or formal mental health training, in order to enhance the intervention’s dissemination and implementation potential in these contexts. (See Ramaiya et al., 2017 for a comprehensive description of treatment modifications and their underlying rationale.)
The resulting intervention, DBT-N, is a modularized, 10-session group intervention largely derived from the skills training component of standard DBT. Treatment structure was informed by a truncated DBT skills group program developed for survivors of domestic violence in the United States (Iverson, Shenk, & Fruzzetti, 2009). The primary objective of the intervention is to reduce deficits in emotion regulation via increasing acquisition and generalization of skills. Each group session, lasting approximately 180 minutes, parallels standard DBT skills training procedures (See Table 1 for an overview of the curriculum). All sessions begin with a group mindfulness exercise, followed by a behavioral chain analysis in order to identify problem behaviors appropriate for skills training. Chain analysis is then followed by homework review. The remainder of each session focuses on skill-specific didactics and in-vivo behavioral rehearsal of skills from one of the five DBT-N modules (i.e., Mindfulness, Distress Tolerance, Self-Validation, Emotion Regulation, and Interpersonal Effectiveness). Sessions conclude with a homework assignment and skills generalization strategies (e.g., anticipation of internal and external states in which clients use skills, repeated behavioral rehearsal across real-world contexts, involvement of family members in homework completion). A 30-minute lunch break is also provided.
Table 1.
Dialectical Behavior Therapy skills for Nepali populations (DBT-N) schedule
| Session | Topics covered | Allocated time (min) |
|---|---|---|
| Orientation & Pretreatment | Diary card | 30 |
| Contact Information | 15 | |
| Treatment Overview | 45 | |
| Break | 30 | |
| Group Guidelines | 20 | |
| Homework: Weekly Diary Card | 10 | |
| Session Two | Homework Review | 15 |
| Mindfulness* | ||
| Wise mind | 45 | |
| “What” skills | 45 | |
| Break | 30 | |
| Chain Analysis | 25 | |
| Establish Treatment Targets | 15 | |
| Homework: Using Breath to Find Wise Mind | 5 | |
| Session Three | Chain Analysis | 25 |
| Homework Review | 15 | |
| Mindfulness | ||
| Wise mind | 45 | |
| Break | 30, | |
| Mindfulness | ||
| “How” skills | 60 | |
| Homework: Practicing “How” Skills | 5 | |
| Session Four | Chain Analysis | 25 |
| Homework Review | 15 | |
| Distress Tolerance* | ||
| Wise Mind ACCEPTS Skills | 45 | |
| Break | 30 | |
| Distress Tolerance | ||
| Self-Soothe Skills | 60 | |
| Homework: Practicing ACCEPTS & Self-Soothe Skills | 5 | |
| Session Five | Chain Analysis | 25 |
| Homework Review | 15 | |
| Distress Tolerance | ||
| Radical Acceptance | 45 | |
| Break | 30 | |
| Distress Tolerance | ||
| Radical Acceptance | 45 | |
| Homework: Practicing Radical Acceptance | 5 | |
| Session Six | Chain Analysis | 25 |
| Homework Review | 15 | |
| Distress Tolerance | ||
| Radical Acceptance | 15 | |
| Break | 30 | |
| Self-Validation | ||
| Step 1: Awareness of Emotion | 45 | |
| Step 2: Normalizing of Emotion | 45 | |
| Homework: Noticing Validation Towards Self & Others | 5 | |
| Session Seven | Chain Analysis | 25 |
| Homework Review | 15 | |
| Self-Validation | ||
| Step 3: Self-Forgiveness | 45 | |
| Step 4: Self-Encouragement | 30 | |
| Break | 30 | |
| Emotion Regulation* | ||
| Model for Describing Emotions | 30 | |
| Homework: Noticing and Responding to Invalidation | 5 | |
| Session Eight | Chain Analysis | 25 |
| Homework Review | 15 | |
| Emotion Regulation | ||
| Mindfulness of Positive Emotion | 25 | |
| Reducing Vulnerabilities | 25 | |
| Break | 30 | |
| Emotion Regulation | ||
| Nepali Pleasant Activities | 25 | |
| Opposite Action | 30 | |
| Homework: Practicing Opposite Action | 5 | |
| Session Nine | Chain Analysis | 25 |
| Homework Review | 15 | |
| Interpersonal Effectiveness* | ||
| Relationship Effectiveness | 60 | |
| Break | 30 | |
| Safety Plan Development | 45 | |
| Homework: Balancing Priorities in Interpersonal Relationships | 5 | |
| Session Ten | Chain Analysis | 25 |
| Homework Review | 15 | |
| Interpersonal Effectiveness | ||
| Objectives Effectiveness Skills | 60 | |
| Break | 30 | |
| Program Recap and Review | 30 | |
| Closing | 20 |
Module derived from first-edition Skills Training Manual (Linehan, 1993b)
The intervention was delivered in Nepali by two lay providers: one U.S. masters-level student with 20 hours of didactic training in comprehensive DBT but no direct clinical experience, and a local Nepali counselor trained in DBT-N over a five-day period. A U.S. trained psychologist of Nepali origin with DBT expertise provided weekly, remote supervision.
1.4 Procedure
Ten women with current or past histories of suicidal and/or NSSI behaviors were recruited for the study using community-based referrals. All participants were native citizens of the rural Jumla district, were treatment-naïve (i.e., had never received formal inpatient or outpatient mental health services), and met the following inclusion criteria: female between the ages of 18–50 years; a suicide or self-harming attempt within the last two years OR a score of 2+ on Item #9 Nepali version of the Beck Depression Inventory (endorsing that either “I would like to kill myself” or “I would kill myself if I had the chance”) (Kohrt, Kunz, Koirala, Sharma, & Nepal, 2002). Exclusion criteria included comorbidity of psychosis, one or more developmental disorders, and current alcohol or substance dependence.
Outcome baseline measurements were obtained at two- and one-week prior to the intervention. The intervention period consisted of 10 weekly meetings, with measurements taken 3–4 days following the conclusion of each group for sessions 2–10. Follow-up measurements were taken 1- and 4-weeks post-intervention. Due to the high rate of illiteracy, all measurements were taken using interviewer-administered questionnaires conducted by a local research assistant. The trained research assistant was a native Nepali speaker and blind to all treatment content. The same research assistant also conducted individual semi-structured interviews (averaging 60 minutes in length) for qualitative analysis two-weeks post-intervention.
The intervention was provided at no financial cost, and no monetary compensation was provided. Approval for the study was obtained by both the Duke University Institutional Review Board (Pro00052917) and the Nepal Health Research Council, the national body providing ethical oversight for clinical research in Nepal.
1.5 Self-report measurement
All instruments required transcultural adaptation and were modified using a five-step procedure commonly used in LMIC cross-cultural research settings (van Ommeren et al., 1999).
1.5.1 Suicide and self-injurious behaviors
Frequency and severity of suicide attempts and NSSI episodes were measured at baseline using an adapted version of the Suicide Attempt Self-Injury Interview (SASII; Linehan, Comtois, Brown, Heard, & Wagner, 2006). This semi-structured assessment has been used in numerous outcome studies of DBT (e.g., Linehan et al., 1991, 2006, 2015; Pistorello et al., 2012). At follow-up, rates of suicidal and self-injurious behaviors were determined via clinical interviewing rather than standardized measurement. Suicidal ideation was assessed via Item #9 of the Nepali version of the Beck Depression Inventory (BDI; Kohrt et al., 2002).
1.5.2 Emotion regulation
An adapted version of the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) was used to assess multiple areas of emotion regulation, including difficulties in emotion recognition and awareness, lack of emotional clarity, non-acceptance of emotion, difficulties engaging in goal-directed behavior, impulse control difficulties, and limited access to emotion regulation strategies. The 26-item Nepali version was adapted in order to target multiple domains of measurement equivalence and includes 26-items spanning the original six domains. Higher scores indicate greater difficulties with emotion regulation. In this sample, Cronbach’s alpha (α) = 0.95.
1.5.3 Coping skills
Changes in skills use were measured using an adapted version of the Dialectical Behavior Therapy Ways of Coping Checklist (DBT-WCCL; Neacsiu, Rizvi, Vitaliano, Lynch, & Linehan, 2010). The Nepali version contains 25 items that can be scored as two subscales that measure the frequency of DBT skills use and dysfunctional coping over the previous week. On the skills use subscale, higher scores indicate greater use of coping skills. This subscale was used for all analyses in this study. Internal reliability of the Nepali version is good (α = 0.86).
1.5.4 Depression symptoms
Depressive symptomatology was measured using a validated Nepali version of the Beck Depression Inventory (BDI; Kohrt et al., 2002). The 21-item scale assesses depression symptoms over the prior 2 weeks and has high discriminant validity (AUC = 0.919; 95% CI 0.878—0.960) and internal reliability (α = 0.90; Kohrt et al., 2012). A score of 20 or greater indicates the presence of moderate depression (Kohrt et al., 2012).
1.5.5 Anxiety
Anxiety symptomatology was measured using a validated Nepali version of the Beck Anxiety Inventory (BAI; Kohrt, Kunz, & Koirala, 2003). The 21-item scale assesses anxiety symptoms over the prior 2 weeks and has high discriminant validity (AUC = 0.847; 95% CI 0.789—0.906) and internal reliability (α = 0.90; Kohrt et al., 2012). A score of 17 or greater indicates the presence of moderate anxiety (Kohrt et al., 2012).
1.5.6 Post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) symptoms were measured using a Nepali version (Thapa & Hauff, 2005) of the PTSD Checklist, Civilian Version (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993). The 17-item scale corresponds with the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revised (American Psychiatric Association, 2000) PTSD diagnostic criteria. A score of 50 or greater indicates need for clinical intervention (Thapa & Hauff, 2005).
1.5.7 Resilience
A 9-item Nepali version of the Resilience Scale (RES; Wagnild & Young, 1993) has been adapted for use in Nepal (Kohrt et al., 2016). The scale identifies the degree to which an individual is able to cope with and respond successfully to life stressors. Higher scores reflect higher individual resiliency. The scale has good internal reliability (α = 0.83; Kohrt et al., 2016).
1.6 Analyses
1.6.1 SCED protocol
A tri-phasic approach was used to analyze data in accordance with standard SCED assessment procedures (Barlow, Nock, & Hersen, 2009; Kazdin, 2003). In phase 1, the first and second authors independently performed case-by-case, visual inspection of performance on all outcome variables. Visual inspection was used to complement linear regressions by identifying trends (e.g., sudden within-case variability, similarities in multi-indicator trends) that may be concealed by statistical methods. Visual inspection followed guidelines proposed by (Barlow et al., 2009; Manolov & Moeyaert, 2017). These include assessment of specific trends both within and between each phase of the AB design: (a) change in trend or symptom level across phases A, B, and follow-up; (b) the degree of change (slope of the graph) between phases; and (c) changes in variability of the data that capture stability of symptom change within phases. Interrater reliability for visual inspection (κ = 0.981) indicated a high level of agreement. Similar procedures have been utilized in evaluations of novel interventions in resource-strained, global mental health settings (e.g., Jordans et al., 2012; Jordans, Komproe, Tol, Nsereko, & De Jong, 2013).
In phase 2, linear regressions were conducted in SPSS (release 24) to examine stability of observed trends in changes per outcome variable, per case. Standardized beta coefficients were estimated using a multiple linear regression model using ordinary least-squares regression. Significant β values (established a cut-off of α < 0.05) represented trend stability within cases in either positive or negative directions, and were used to corroborate visual inspection analyses.
In phase 3, group data were aggregated across outcome indicators, and Wilcoxon signed rank tests and effect sizes (r) were calculated for all outcomes. To probe improvements, results from phases 1 and 2 were used to cluster individuals into treatment response subgroups: positive change (26–75%) and no improvement (1–25%). Change was thus defined as significant improvement or deterioration when similar trends are confirmed across all indicators.
1.6.2 Qualitative analysis
Semi-structured interviews with DBT-N participants were used to explore the intervention’s feasibility and acceptability. Nine post-intervention interviews were conducted. One participant was not available for qualitative interviewing due to work-related travel. Following Nepali transcription and English translation, interviews were analyzed using a comparative method (Guest, 2012). This method consisted of reading transcripts for content and open-coding transcripts for key themes related to intervention feasibility and acceptability. This iterative process was applied to remaining transcripts until a final set of themes emerged. Qualitative commercial software (NVIVO 9) was used for data management and analyses.
2 RESULTS
2.1 Client characteristics
Demographic information, clinical characteristics, and suicidal behaviors are summarized in Table 2. The sample consisted of 10 women (age 19–47), all of whom were Hindu agriculturalists and primary contributors to their household income. 70% were illiterate. At baseline, all participants were above Nepali clinical cut-offs for anxiety, depression, and PTSD caseness. The average number of lifetime suicide attempts was 2.1.
Table 2.
Baseline characteristics and treatment completion (N = 10)
| Participants | |
|---|---|
| Age, mean (SD, range) | 30.8 (8.78,19–47) |
| Female, no. (%) | 10 (100) |
| Married, no. (%) | 9 (90) |
| No. of children, mean (SD, range) | 2.2 (1.08, 0–4) |
| Caste, no. (%) | |
| Brahman | 2 (20) |
| Chhetri | 3 (30) |
| Dalit | 5 (50) |
| Highest education level completed (%) | 5 (50) |
| None | 3 (30) |
| Primary school | 2 (20) |
| School leaving certificate a | |
| No. of sessions attended, mean (range) | 7.9 (3–10) |
| 10 sessions, no. (%) | 3 (30) |
| 9 sessions, no. (%) | 2 (20) |
| 8 sessions, no. (%) | 1 (10) |
| 7 sessions, no. (%) | 2 (20) |
| 6 sessions, no. (%) | 1 (10) |
| 3 sessions, no. (%) | 1 (10) |
| Current Axis I Disorders | |
| Depression, no. (%) | 10 (100) |
| Anxiety, no. (%) | 10 (100) |
| Posttraumatic stress disorder, no. (%) | 10 (100) |
| Lifetime suicide attempts, mean (SD) | 2.1 (1.4) |
The national exam required for admission to upper secondary school in Nepal. Examination occurs at the end of 10th grade.
2.2 Attrition
DBT-N participants had an overall completion rate of 82%, with completion defined as attendance in over 50% of sessions. The attrition rate mirrored Linehan and colleagues’ (1991) initial randomized clinical trial of comprehensive DBT, where treatment dropout (defined as missing four or more consecutive individual or skills group sessions) was 16.7%. One participant withdrew from the study after Session 3 due to family concerns regarding stigma related to participation in an intervention addressing suicidality. No participants received additional psychiatric or psychological treatment over the course of the study.
2.3 Outcome analyses
There were no deaths by suicide or documented suicide attempts or self-harming events over the course of the study.
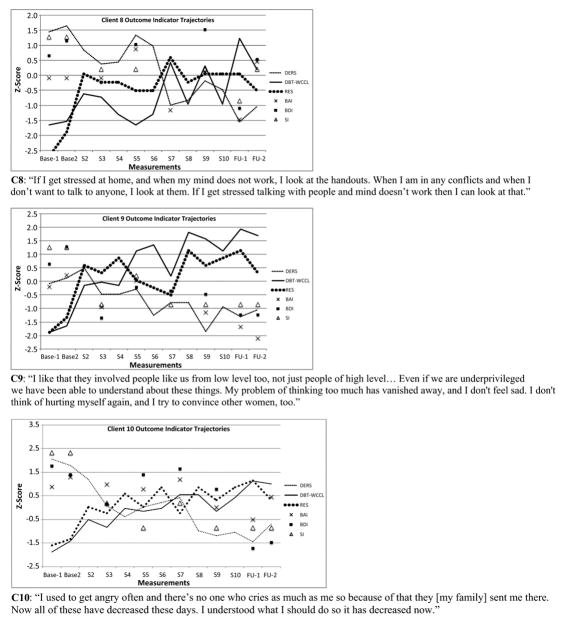
Within- and between-case patterns emerged from visual analyses of individual trajectories (See Figure 1). At baseline, suicidal ideation scores had pre-intervention stability across cases (clients 1, 5, 6, 8, 9, 10), with resilience scores showing similar stability patterns (clients 2, 6, 7). For other indicators, baseline stability was more variable. The same observation held in the follow-up phase.
Figure 1.
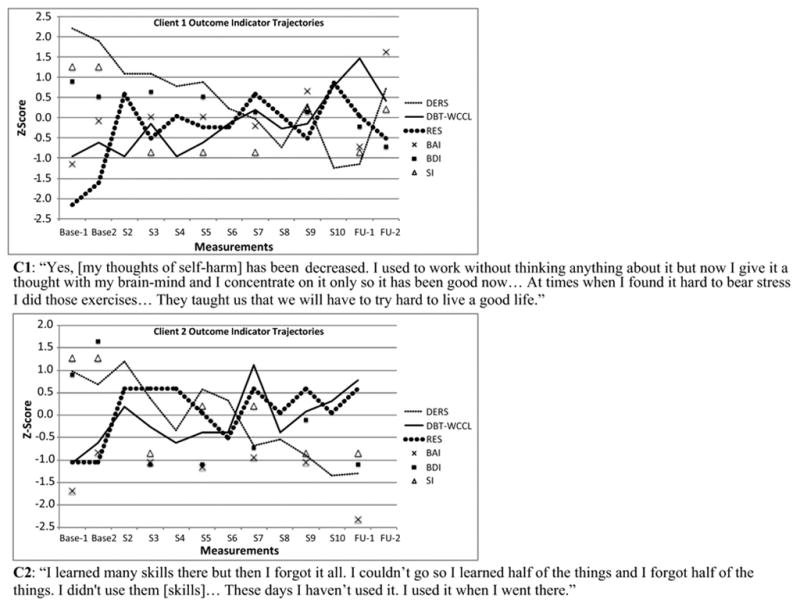
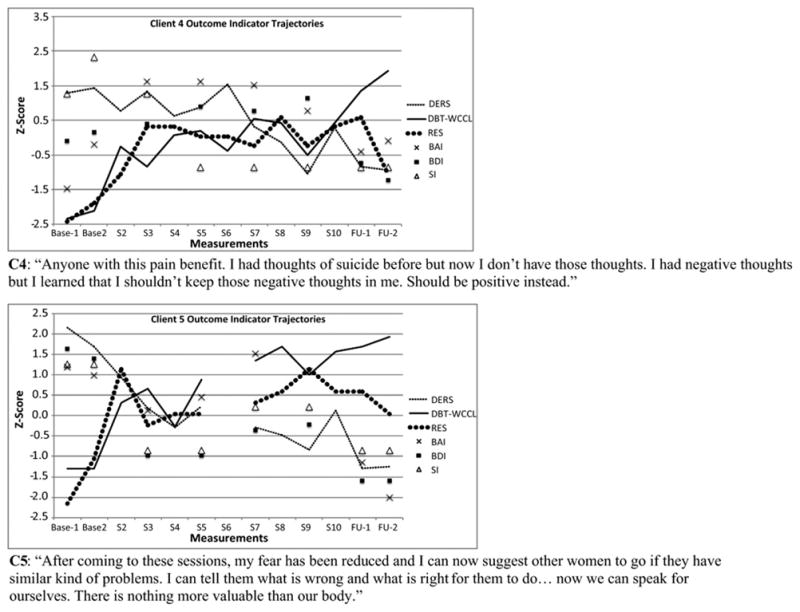
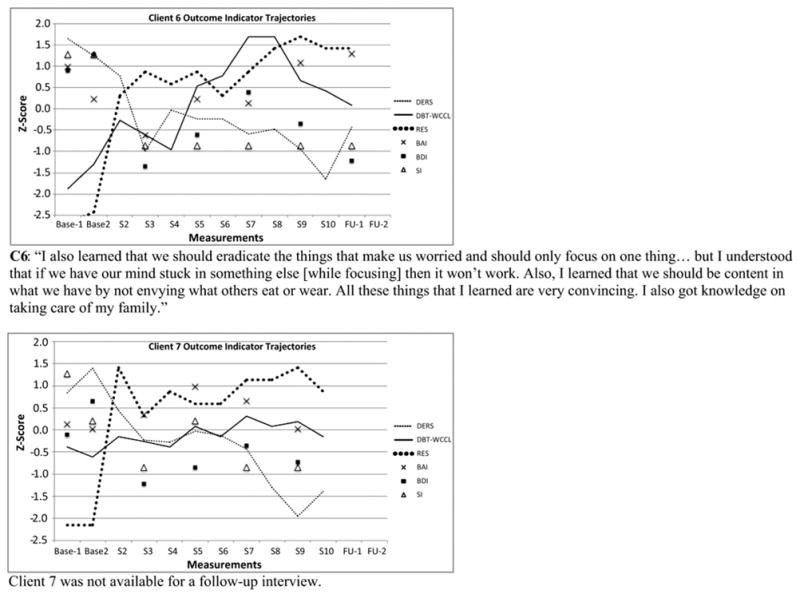
Individual change profiles (standardized scores)
Note. All instrument total scores were standardized using Z-transformation to allow for visual comparison across individuals.
DERS = Difficulties in emotion regulation scale; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; RES = Resilience Scale; DBT-WCCL = DBT Ways of Coping Checklist, skills use subscale; SI = Suicidal Ideation, Beck Depression Inventory Item #9
Visual inspection results of note include: (a) gradual, coinciding improvement on the DERS and DBT-WCCL scores during the intervention phase for a majority of clients (with the exception of clients 2 and 7), with DBT-WCCL scores demonstrating greater variability over time; (b) sharp level changes in resilience scores between baseline and intervention for all clients except 10 (who experienced more gradual gains), with gains stabilizing across all cases except 2, 9, and 6, the last of whom continued experiencing rapid gains throughout the intervention phase; and (c) lack of improvement trends on BDI and BAI across all cases, with the exception of clients 2 and 9 (who experienced gains in one or both indicators). Further, any gains in coping and emotion regulation over the course of treatment were sustained at follow-up, with the exception of client 2, whose DERS scores diminished.
For each case, standardized regression coefficients were calculated for each outcome indicator (Table 3). Based on combined regression analysis with all outcomes, the following subgroups emerged: those demonstrating positive change (clients 1, 4, 5, 6, 9, 10) and no change (clients 2, 7, 8). If outcomes were restricted to emotion regulation, coping skills use, and suicidal ideation, all clients experienced positive change.
Table 3.
Respondent change indicators from combined visual inspection and regression analyses (n = 9)
| Case | DERS | BAI | BDI | RES | DBT-WCCL | SI | |
|---|---|---|---|---|---|---|---|
| 1 | Visual a | + | − | + | + | + | + |
| Regression b | −.835 (.735); .001* | .825 (.322); .043 | −.945 (.166); .004* | .414 (.246); .205 | .838 (.304); .001* | −.300 (.102); .563 | |
| 2 | Visual a | + | + | + | + | + | + |
| Regression b | −.780 (.608); .005* | −.530 (.549); .280 | −.514 (.930); .297 | .299 (.194); .372 | .582 (.423); .060 | −.655 (.082); .158 | |
| 4 | Visual a | + | − | + | + | + | + |
| Regression b | −.527 (.867); .096 | .013 (1.325); .980 | −.365 (.755); .476 | .530 (.242); .094 | .750 (.560); .008* | −.843 (.084); .035* | |
| 5 | Visual a | + | + | + | + | + | + |
| Regression b | −.796 (.556); .006* | −.452 (1.241); .368 | −.613 (.995); .196 | .521 (.248); .123 | .848 (.454); .002* | −.393 (.100); .441 | |
| 6 | Visual a | + | − | + | + | + | + |
| Regression b | −.674 (1.076); .023* | .648 (.668); .164 | −.461 (.970); .358 | .736 (.288); .010* | .626 (.700); .039* | −.655 (.082); .158 | |
| 7 | Visual a | + | No change | + | + | + | + |
| Regression b | −.416 (1.441; .232 | .083 (.692); .894 | −.378 (.849); .530 | .567 (.364); .087 | .652 (.197); .041* | −.671 (.096); .215 | |
| 8 | Visual a | + | No change | No change | + | + | + |
| Regression b | −.760 (.667); .007* | −.279 (.811); .592 | −.148 (.922); .813 | .510 (.227); .109 | .584 (.586); .059 | −.814 (.044); .093 | |
| 9 | Visual a | + | + | + | + | + | + |
| Regression b | −.743 (.513); .009* | −.808 (.618); .098 | −.567 (.815); .241 | .516 (.249); .104 | .838 (.526); .001* | −.703 (.080); .119 | |
| 10 | Visual a | + | + | + | + | + | + |
| Regression b | −.772 (.956); .005* | −.794 (.413); .059 | −.646 (1.076); .166 | .692 (.186); .018* | .856 (.336); .001* | −.777 (.098); .069 |
Visual inspection of improving post-intervention trend compared to pre-intervention trend. A + indicates an improving trend.
Regression analyses, collapsing pre- and post-time points, after start of the intervention.
Regression coefficient significant and positive result of visual inspection.
Note. DERS = Difficulties in Emotion Regulation Scale; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; RES = Resilience Scale; DBT-WCCL = DBT Ways of Coping Checklist, skills use subscale; SI = Suicidal Ideation, Beck Depression Inventory Item #9
2.4 Clinically significant change
Clinically significant change for the BDI, BAI, and PCL was determined by a combined assessment of (a) sufficient improvements in individual post- compared to pre-treatment functioning and/or compared to a normative sample (Jacobson, Follette, & Revenstorf, 1984); and (b) a reliable change index (Jacobson & Truax, 1991). All participants began DBT-N above the criterion necessary for change on all three measures. For the BDI and BAI, clinically significant change was calculated using criterion “c” with comparison to a normed, non-clinical group of Nepalis (Kohrt et al., 2012). For the BDI, eight individuals were classified as recovered and one as improved (client 6). For the BAI, three recovered (clients 2, 5, 9), one improved (client 10), two were unchanged (clients 7, 8), and three deteriorated (clients 1, 4, 7). For the PCL, clinically significant change was calculated using criterion “a” due to the absence of a normed, non-clinical sample for comparison (Thapa et al., 2005). Under these criteria, at post-treatment, six recovered, one improved (client 4), one deteriorated (client 5), and one (client 7) was not classified due to missing data.
Based on clinical cut-offs, at post-treatment, 66.7% of participants no longer scored above the BDI clinical cut-off, 33.3% were below the clinical cut-off on the BAI, and 75.0% of cases fell below the PCL cut-off.
2.5 Aggregated (group-level) treatment effects
To probe treatment effects, Wilcoxon ranked tests were conducted on all outcome measures (See Table 4). There were significant improvements between pre- to post-intervention for five of six outcome measures, with large effect sizes for the DERS, BDI, Resilience, DBT-WCCL, and suicidal ideation. Changes on the BAI also showed a moderate effect size, though improvements were not statistically significant. Longitudinal analyses using generalized estimating equations (GEE) indicated that changes in DERS scores were predicted by time-lagged DBT-WCCL scores, controlling for pre-lag time point DERS scores, over the course of the study (β = .355, SE = .133, p = .008). Group figures charting progress across all outcomes were also included to supplement findings (See Figure 2). Visual inspection of these data indicates that gains in emotion regulation and coping skills use were gradual and sustained over the course of the study (mirroring GEE results), while improvements in suicidal ideation and resilience were most rapid between baseline and treatment initiation.
Table 4.
Aggregated outcomes pre- and post- dialectical behavior therapy skills group intervention (n = 9)
| Measure | Time point | M | SD | Za | Asymp. sig. | Effect size (r) |
|---|---|---|---|---|---|---|
| DERS | Pre | 113.33 | 12.63 | −2.668 | .008 | .889 |
| Post | 72.22 | 15.48 | ||||
| BAI | Pre | 31.06 | 7.74 | −1.244 | .214 | .415 |
| Post | 25.67 | 11.04 | ||||
| BDI | Pre | 35.00 | 4.76 | −2.666 | .008 | .889 |
| Post | 18.39 | 5.35 | ||||
| RES | Pre | 6.06 | 1.72 | −2.670 | .008 | .890 |
| Post | 14.50 | 2.11 | ||||
| DBT-WCCL | Pre | 24.50 | 4.80 | −2.666 | .008 | .889 |
| Post | 44.67 | 6.14 | ||||
| SI | Pre | 2.06 | 0.46 | −2.680 | .007 | .893 |
| Post | 0.22 | 0.36 |
Note. DERS = Difficulties in Emotion Regulation Scale; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; RES = Resilience Scale; DBT-WCCL = DBT Ways of Coping Checklist, skills use subscale; SI = Suicidal Ideation, Beck Depression Inventory Item #9.
Figure 2.
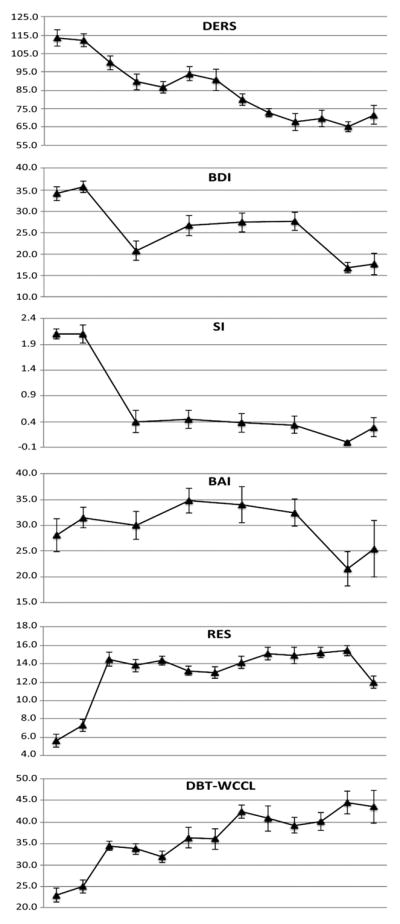
Group change profiles (raw scores)
*Clinical cut-off scores for caseness validated in Nepal. Beck Depression Inventory (BDI) depression caseness ≥ 20 total score (Kohrt et al., 2002). Beck Anxiety Inventory (BAI) anxiety caseness ≥ 17 total score (Kohrt et al., 2003).
Note. DERS = Difficulties in Emotion Regulation Scale; BDI = Beck Depression Inventory; SI = Suicidal Ideation (Beck Depression Inventory Item #9); BAI = Beck Anxiety Inventory; RES = Resilience Scale; DBT-WCCL = DBT Ways of Coping Checklist
2.6 Qualitative findings
2.6.1 Feasibility
All 10 clients reported generally favorable impressions of the intervention (See individual client quotes in Figure 1). A majority cited group bonding and cohesion as main reasons for continuing treatment, indicating that sessions provided an enjoyable and interactive reprieve from clients’ regular and often solitary work as agriculturalists.
Interviewer (I): What did you like most about group?
Client (C) 2: I miss everyone. I miss the group leaders when we don’t mingle around with them. Yes, if I could go there again I could have learned other things with them, too. I miss being around everyone.
C9: It was very interesting. I enjoyed it. I understood different things and we danced too. I found it good for my heart-mind. My heart-mind was never unhappy with them, when we were together. I wish we women can gather together and talk and share our things and do those activities together again.
A number of clients indicated that being in a group setting encouraged their sense of mastery in interpersonal contexts.
C8: We went there once in a week and I wanted to listen to the good things they taught and I learned that it is good to enjoy and feel good… So I felt good about all these things when we were together. I used to get afraid to speak but after going to training I learned to speak, and now I don’t feel scared anymore.
Despite the facilitative role of groups, barriers to attendance also were mentioned by half of clients. Attendance barriers included competing religious events and time needed to travel long distances on a daily basis to collect firewood.
I: Was it easy for you to participate?
C6: Sometimes it was difficult like in days of work, or in holiday season from the months of September through November. But I tried to manage. Sometimes we had work… we had to collect firewood so we couldn’t attend. There’s no one to do it but us. Women are always worried about their household chores, wherever they go.
2.6.2 Acceptability
Clients endorsed mixed views of family and community perceptions of their participation in the program. Some families were supportive. Others, however, reported concerns that participation in a program that addressed suicidality would endanger family reputations in their small communities. One client’s husband forced her to terminate treatment after the third session. Others shared that community members assumed they were receiving financial compensation for participation, and that future participants would expect financial incentives.
I: Did any other people know about you participating in the training?
C8: Yes, they knew about it. At the beginning they were happy about my sessions but later they asked me if I was getting something for going to the sessions as I had to leave all my works to go there. At first they didn’t say anything but later they said what does that organization give you, because I went there leaving the household works.
I: Will you suggest that other women and family members to participate in this group?
C4: They won’t listen even if I suggest it… they don’t understand. They won’t listen.
2.6.3 Skills use
Clients shared a range of skills they found particularly helpful throughout the intervention. They enjoyed and recalled mindfulness skills. Many also continued to implement DBT skills consistent with religious activities.
I: Do you still practice any of the skills?
C9: Yes, like watching the flowers blooming and enjoying it. And letting the leaves flow in stream, putting all our worries in leaf of letting it all flow and sail. I understood about that… I still do that and I still want to learn about it. There were small streams and we would let leaf flow in that. When I do these activities, my worries… go away and my mind just focuses. I also worship in the morning and the evening.
C1: We learned different skills like observing, explaining, mindfulness. They showed us some pictures, which helped us realize that everyone goes through pain and sadness. Those parts helped a lot.
C5: First, to concentrate on one thing at a time. If we divert our mind elsewhere then if we cook rice it won’t be good and sometimes we might put salt twice in our meal or put chili powder instead of salt. So after attending those sessions I have been able to concentrate well.
C6: I liked the activity we did about looking to God and the activity of practicing wise mind to convince our hearts. And… we learned that we should do one thing at a time rather than doing everything at once.
Barriers to generalizing skills also emerged, and a few clients reported difficulties remembering skills. Others indicated that they were unable to apply skills after the intervention.
C2: I learned many skills there but then I forgot it all. I couldn’t go so I learned half of the things and I forgot half of the things.
I: Do you ever use any of the skills?
C2: I didn’t use them… These days I haven’t used it. I used it when I went there.
2.6.4 Areas for improvement
Despite participating in a DBT orientation session explaining the nature of the treatment, some clients believed the intervention would have a stronger biomedical focus. They felt somatic complaints had not been sufficiently reduced. As a result, many suggested providing supplementary medical treatment for physical symptoms as a means of improving the program.
C2: It would have been good if they had provided some treatment for my heart. I get worried thinking what will happen if my heartbeat stops.
I: If something bad will happen, you mean?
C2: Yes… Sometimes my chest pains a lot and my heart beats fast and my chest pains. When my mother was ill, I could not take care of her because I was sick too, my chest pained a lot during those days.
C7: I have different problems like having cold hands and feet, my head become hot, my body becomes weary and dizzy, my vision becomes unclear, so it would have been good if they could have provided some medical treatment for this. Out children are small and we are poor. What to do?
3 DISCUSSION
This results from this pilot study suggest that a modified DBT skills intervention for low-literacy Nepali women may be helpful in increasing adaptive emotion regulation through use of DBT skills, with potential for reduction of suicidal behaviors. Over the course of treatment, there were no documented suicide attempts or NSSI incidents. This study represents the first systematic evaluation of culturally adapted DBT skills training in a non-WEIRD, LMIC context, and is to our knowledge the first SCED series of DBT skills training as a stand-alone treatment for emotion dysregulation in an illiterate population with a history of suicidality.
The quantitative pattern of results is consistent with expectations that treatment initiation would correspond to reductions in emotion dysregulation and distress-related psychopathology. For all nine treatment completers, gradual improvements in DERS scores were observed both descriptively and statistically over the course of treatment. As hypothesized, these improvements were predicted by increases in skills use over time. Further, any improvements in DBT-WCCL and DERS scores over the course of treatment were sustained at follow-up, with the exception of client 2, whose improvements in DERS scores diminished. Regression analyses indicated more conservative gains in BDI and BAI scores, with the exception of significant, stable improvements in depression symptoms for one participant (client 1).
Despite this lack of intra-individual improvement in BAI scores, however, pooled data revealed statistically significant improvements in anxiety symptoms. However, DBT-N’s effect size for improvements in BAI scores were lower than those reported in trials for various anxiety disorders in WEIRD settings (Dimidjian et al., 2006; Neacsiu et al., 2014; Westbrook & Kirk, 2005). This may be attributed to the somatic nature of BAI items, raising the potential that high BAI scores reflect comorbid medical problems such as under- or untreated diabetes, anemia and micronutrient deficiencies, cardiovascular disease, and infections (Kohrt, Tol, & Harper, 2007). Qualitative data mirrored these quantitative findings. Despite our comparatively high completion rate relative to other trials (e.g., Soler et al., 2009) and high client satisfaction, many clients complained of physical symptoms after treatment. Participants suggested that their somatic concerns (e.g., dizziness, blurry vision, a racing heart, chest pain, overheating, and feeling cold) would be best managed with medical treatment. Referrals for medical evaluation at the time of screening would also be a useful means of eliminating any existence of cooccurring physiological disorder.
Though combined regression analyses for all outcomes grouped a majority of clients into a “positive change” subgroup, three clients (2, 7, 8) fell into the “no change” subgroup. For client 2, this appears to be due to her trending DBT-WCCL change profile (p = .060) and the lack of sustained DBT-WCCL gains at 4-week follow-up. Qualitative results supported these results, with client 2 reporting difficulties using skills outside of the session context. Client 8′s DBT-WCCL change profile also trended (p = .059) and gains were also not sustained at follow-up. For client 7, all follow-up data were missing.
Though SCED designs often boast high degrees of internal validity (in this case, demonstrating the causal effect of DBT-N), rival explanations for our findings remain. Although results suggest a contributing role of DBT-N skills, it is possible that observed treatment effects resulted from “common” or non-specific factors (e.g., time and attention from group leaders and other DBT-N participants). This view is buttressed by qualitative findings, which indicated that a supportive group environment provided a majority of clients with a source of meaningful social interaction outside of their isolated profession as agriculturalists. Another interpretation is that these non-specific factors were necessary in exerting an initial effect, but not sufficient in maintaining one. It is plausible that, for instance, non-specific factors were responsible for the initial, immediate gains in suicidal ideation and resilience, but that maintenance of gains was facilitated by skills use over time. Use of validated instruments for rigorously measuring non-specific factors in psychological interventions may provide one opportunity for disentangling these competing effects. Such measures have already been developed and implemented in Nepal (e.g., Kohrt et al., 2015) and should be utilized in future evaluations of DBT-N.
Taken together, our pattern of results warrants further evaluation of DBT-N as a transdiagnostic mental health treatment in Nepali settings. In addition to a demonstrated history of suicidal and self-injurious behaviors, our group experienced high levels of comorbidity at baseline, with all completers meeting criteria for a clinical diagnosis of anxiety, depression, and PTSD. These findings echo data from WEIRD populations, which show that clients with emotion regulation related deficits also exhibit high levels of psychiatric comorbidity (e.g., Neacsiu et al., 2014). At posttreatment, two-thirds of participants no longer scored above the BDI clinical cut-off, one-third were below the clinical cut-off on the BAI, and three-quarters of cases fell below the PCL cut-off.
While results from this small-scale pilot offer promising preliminary support of DBT-N, the findings are not without limitations. Use of a standard design lacking controlled or more rigorous SCED components (e.g., multiple baseline and follow-up measurement, randomization at baseline, use of an alternating treatment group) limit the potential strength of inferences drawn from the current study. Our small sample size also merits cautious interpretation of statistical findings and weakens their validity and generalizability. Our measurement of suicide and NSSI at baseline and over treatment is an additional limitation of note: changes in suicidal ideation were assessed using a single item, and a combination of scheduling difficulties and lack of available clinical interviewers at follow-up restricted structured measurement of suicide attempts and NSSI episodes to baseline only. These barriers limit possible conclusions about DBT-N’s efficacy in targeting suicidal behaviors specifically and should be addressed in future trials.
Due to lack of a standardized fidelity or rating tool for DBT-N, treatment adherence and fidelity were not evaluated in this SCED evaluation, leading to potential concerns surrounding the validity of reported inferences. Behavioral measures of clinical competence are increasing in global mental health settings including Nepal (e.g., Kohrt et al., 2015) and could provide a basis for developing a DBT-N fidelity tool. Further, a limited number of therapists conducted the intervention in the sample, one of whom was a U.S.-based graduate researcher with limited didactic DBT training. As the empirical recommendation is the use of paraprofessionals to deliver psychological treatments in LMIC, additional research is needed to assess the generalizability of the intervention across multiple therapists with more limited mental health training.
4 CONCLUSION
This pilot study suggests that DBT-N may be useful as a transdiagnostic treatment among low-literacy Nepali women with histories of suicidality. Participants demonstrated improvements in emotion regulation across the course of treatment, and these benefits were associated with increased use of DBT-N skills over time. Rapid and sustained reductions in suicidal ideation and improvements in resilience were observed for a majority of cases after treatment initiation. The intervention was also feasible and acceptable, demonstrated by both a high retention rate and favorable treatment impressions. Future studies should investigate the extent to which DBT-N skills mediate observed gains in emotion regulation using both multiple single-case as well as group-comparison designs.
Acknowledgments
Funding information
This research was supported by grants from Duke Global Health Institute and Duke University Center for International Studies (to MKR). BAK receives salary support from the National Institute of Mental Health (K01MH104310). The authors thank the participating clients and their families, and especially acknowledge the research and clinical staff at Transcultural Psychosocial Organization Nepal for their ongoing support. Special thanks to Nandaraj Acharya for his clinical support in delivering the intervention. The authors also thank the Nepal Health Research Council for providing ethical approval for the study.
Glossary
- BAI
Beck Anxiety Inventory
- BDI
Beck Depression Inventory
- DBT
Dialectical behavior therapy
- DBT-N
Dialectical Behavior Therapy skills for Nepali populations
- DERS
Difficulties in Emotion Regulation Scale
- HIC
High-income country
- LMIC
Low- and middle-income country
- PCL
PTSD Checklist
- RES
Resilience Scale
- SCED
Single-case experimental design
- SI
Suicidal ideation
- WEIRD
Western, educated, industrialized, rich and democratic
Footnotes
Ethnopsychology is the study of cultural or “folk” models of psychological subjectivity, and is one salient means of uncovering a culture’s own understanding and experience of the self, emotions, physical body, and connections to the social world (Kohrt & Harper, 2008).
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4 2000. [Google Scholar]
- Barlow DH, Nock MK. Why can’t we be more idiographic in our research? Perspectives on Psychological Science. 2009;4(1):19–21. doi: 10.1111/j.1745-6924.2009.01088.x. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Nock M, Hersen M. Single-Case Experimental Designs. 3. Boston, MA: Pearson Education; 2009. [Google Scholar]
- Beckstead DJ, Lambert MJ, DuBose AP, Linehan M. Dialectical behavior therapy with American Indian/Alaska Native adolescents diagnosed with substance use disorders: Combining an evidence based treatment with cultural, traditional, and spiritual beliefs. Addictive Behaviors. 2015;51:84–87. doi: 10.1016/j.addbeh.2015.07.018. [DOI] [PubMed] [Google Scholar]
- Carter GL, Willcox CH, Lewin TJ, Conrad AM, Bendit N. Hunter DBT project: Randomized controlled trial of dialectical behaviour therapy in women with borderline personality disorder. Australian and New Zealand Journal of Psychiatry. 2010;44(2):162–173. doi: 10.3109/00048670903393621. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, … Jacobson NS. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74:658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Feather JS, Ronan KR. Trauma-focused cognitive behavioural therapy for abused children with posttraumatic stress disorder: A pilot study. New Zealand Journal of Psychology. 2006;35(3):132–145. [Google Scholar]
- Germán M, Smith HL, Rivera-Morales C, González G, Haliczer LA, Haaz C, Miller AL. Dialectical behavior therapy for suicidal Latina adolescents: Supplemental dialectical corollaries and treatment targets. American Journal of Psychotherapy. 2015;69(2):179–197. doi: 10.1176/appi.psychotherapy.2015.69.2.179. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Fersch-Podrat RK, Rivera M, Axelson DA, Merranko J, Yu H, … Birmaher B. Dialectical behavior therapy for adolescents with bipolar disorder: results from a pilot randomized trial. Journal of Child and Adolescent Psychopharmacology. 2015;25(2):140–149. doi: 10.1089/cap.2013.0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis. Sage Publications; 2012. [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of Dialectical Behavior Therapy with and without the Dialectical Behavior Therapy Prolonged Exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behaviour Research and Therapy. 2014;55:7–17. doi: 10.1016/j.brat.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Villatte M, Levin M, Hildebrandt M. Open, aware, and active: Contextual approaches as an emerging trend in the behavioral and cognitive therapies. Annual Review of Clinical Psychology. 2011;7:141–168. doi: 10.1146/annurev-clinpsy-032210-104449. [DOI] [PubMed] [Google Scholar]
- Hill DM, Craighead LW, Safer DL. Appetite-focused dialectical behavior therapy for the treatment of binge eating with purging: A preliminary trial. International Journal of Eating Disorders. 2011;44(3):249–261. doi: 10.1002/eat.20812. [DOI] [PubMed] [Google Scholar]
- Iverson KM, Shenk C, Fruzzetti AE. Dialectical behavior therapy for women victims of domestic abuse: A pilot study. Professional Psychology: Research and Practice. 2009;40(3):242. [Google Scholar]
- Jacobson NS, Follette WC, Revenstorf D. Psychotherapy outcome research: Methods for reporting variability and evaluating clinical significance. Behavior Therapy. 1984;15(4):336–352. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jordans MJ, Komproe IH, Smallegange E, Ntamatumba P, Tol WA, De Jong JT. Potential treatment mechanisms of counseling for children in Burundi: A series of n = 1 studies. American Journal of Orthopsychiatry. 2012;82(3):338–348. doi: 10.1111/j.1939-0025.2012.01171.x. [DOI] [PubMed] [Google Scholar]
- Jordans MJD, Komproe IH, Tol WA, Nsereko J, De Jong JTVM. Treatment processes of counseling for children in South Sudan: A multiple n = 1 design. Community Mental Health Journal. 2013;49(3):354–367. doi: 10.1007/s10597-013-9591-9. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Research Design in Clinical Psychology. 4. Boston, MA: Allyn & Bacon; 2003. [Google Scholar]
- Kohrt BA, Harper I. Navigating diagnoses: Understanding mind–body relations, mental health, and stigma in Nepal. Culture, Medicine, and Psychiatry. 2008;32(4):462. doi: 10.1007/s11013-008-9110-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Hruschka DJ, Worthman CM, Kunz RD, Baldwin JL, Upadhaya N, Jordans MJ. Political violence and mental health in Nepal: Prospective study. The British Journal of Psychiatry. 2012;201(4):268–275. doi: 10.1192/bjp.bp.111.096222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJ, Rai S, Shrestha P, Luitel NP, Ramaiya MK, Patel V. Therapist competence in global mental health: Development of the ENhancing Assessment of Common Therapeutic factors (ENACT) rating scale. Behaviour Research & Therapy. 2015;69:11–21. doi: 10.1016/j.brat.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Kunz RD, Koirala NR. Validation of the Nepali version of Beck Anxiety Inventory. Journal of Institute of Medicine. 2007;26(3) [Google Scholar]
- Kohrt BA, Kunz RD, Koirala NR, Sharma VD, Nepal MK. Validation of a Nepali version of the Beck Depression Inventory. Nepalese Journal of Psychiatry. 2002;2(4):123–130. [Google Scholar]
- Kohrt BA, Tol WA, Harper I. Reconsidering somatic presentation of generalized anxiety disorder in Nepal. Journal of Nervous and Mental Disease. 2007;195(6):544. doi: 10.1097/NMD.0b013e318064e7eb. [DOI] [PubMed] [Google Scholar]
- Kohrt BA, Worthman CM, Adhikari RP, Luitel NP, Arevalo JM, Ma J, Cole SW. Psychological resilience and the gene regulatory impact of posttraumatic stress in Nepali child soldiers. Proceedings of the National Academy of Sciences. 2016;113(29):8156–8161. doi: 10.1073/pnas.1601301113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koons CR, Robins CJ, Tweed JL, Lynch TR, Gonzalez AM, Morse JQ, Bastian LA. Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behavior Therapy. 2001;32(2):371–390. [Google Scholar]
- Linehan M. Cognitive-Behavioral Treatment for Borderline Personality Disorder. New York, NY: Guilford Press; 1993a. [Google Scholar]
- Linehan M. Skills Training Manual for Treating Borderline Personality Disorder. New York, NY: Guilford Press; 1993b. [Google Scholar]
- Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of General Psychiatry. 1991;48(12):1060–1064. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Brown MZ, Heard HL, Wagner A. Suicide Attempt Self-Injury Interview (SASII): Development, reliability, and validity of a scale to assess suicide attempts and intentional self-injury. Psychological Assessment. 2006;18(3):303. doi: 10.1037/1040-3590.18.3.303. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006;63(7):757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Heard HL, Armstrong HE. Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Archives of General Psychiatry. 1993;50(12):971–974. doi: 10.1001/archpsyc.1993.01820240055007. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, … Murray-Gregory AM. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: a randomized clinical trial and component analysis. JAMA Psychiatry. 2015;72(5):475–482. doi: 10.1001/jamapsychiatry.2014.3039. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Schmidt H, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. The American Journal on Addictions. 1999;8(4):279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Manolov R, Moeyaert M. Recommendations for choosing single-case data analytical techniques. Behavior Therapy. 2017;48(1):97–114. doi: 10.1016/j.beth.2016.04.008. [DOI] [PubMed] [Google Scholar]
- McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, Streiner DL. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. American Journal of Psychiatry. 2009;166(12):1365–1374. doi: 10.1176/appi.ajp.2009.09010039. [DOI] [PubMed] [Google Scholar]
- Murray LK, Dorsey S, Haroz E, Lee C, Alsiary MM, Haydary A, Bolton P. A common elements treatment approach for adult mental health problems in low-and middle-income countries. Cognitive and Behavioral Practice. 2014;21(2):111–123. doi: 10.1016/j.cbpra.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neacsiu AD, Rizvi SL, Vitaliano PP, Lynch TR, Linehan MM. The dialectical behavior therapy ways of coping checklist: Development and psychometric properties. Journal of Clinical Psychology. 2010;66(6):563–582. doi: 10.1002/jclp.20685. [DOI] [PubMed] [Google Scholar]
- Neacsiu AD, Eberle JW, Kramer R, Wiesmann T, Linehan MM. Dialectical behavior therapy skills for transdiagnostic emotion dysregulation: A pilot randomized controlled trial. Behaviour Research & Therapy. 2014;59:40–51. doi: 10.1016/j.brat.2014.05.005. [DOI] [PubMed] [Google Scholar]
- O’Hearn A, Pollard RQ. Modifying dialectical behavior therapy for deaf individuals. Cognitive and Behavioral Practice. 2008;15(4):400–414. [Google Scholar]
- Pistorello J, Fruzzetti AE, MacLane C, Gallop R, Iverson KM. Dialectical behavior therapy (DBT) applied to college students: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2012;80(6):982. doi: 10.1037/a0029096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaiya MK, Fiorillo D, Regmi U, Robins CJ, Kohrt BA. A cultural adaptation of dialectical behavior therapy in Nepal. Cognitive and Behavioral Practice. 2017;24(4):428–444. doi: 10.1016/j.cbpra.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins CJ, Chapman AL. Dialectical behavior therapy: Current status, recent developments, and future directions. Journal of Personality Disorders. 2004;18(1):73–89. doi: 10.1521/pedi.18.1.73.32771. [DOI] [PubMed] [Google Scholar]
- Singla DR, Kohrt B, Murray LK, Anand A, Chorpita BF, Patel V. Psychological treatments for the world: Lessons from low-and middle-income countries. Annual Review of Clinical Psychology. 2017;13(1):149–181. doi: 10.1146/annurev-clinpsy-032816-045217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soler J, Pascual JC, Tiana T, Cebria A, Barrachina J, Campins MJ, et al. Dialectical behaviour therapy skills training compared to standard group therapy in borderline personality disorder: A 3-month randomized controlled clinical trial. Behavior Research & Therapy. 2009;47:353–358. doi: 10.1016/j.brat.2009.01.013. [DOI] [PubMed] [Google Scholar]
- Suvedi BK, Pradhan A, Barnett S, Puri M, Chitrakar SR, Poudel P, … Hulton L. Nepal maternal mortality and morbidity study 2008/2009: Summary of preliminary findings. Kathmandu, Nepal: 2009. [Google Scholar]
- Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69(6):1061. doi: 10.1037//0022-006x.69.6.1061. [DOI] [PubMed] [Google Scholar]
- Thapa SB, Hauff E. Psychological distress among displaced persons during an armed conflict in Nepal. Social Psychiatry and Psychiatric Epidemiology. 2005;40(8):672–679. doi: 10.1007/s00127-005-0943-9. [DOI] [PubMed] [Google Scholar]
- United Nations Development Programme. Nepal Human Development Report. Kathmandu, Nepal: United Nations Development Programme; 2004. [Google Scholar]
- van Ommeren M, Sharma B, Thapa S, Makaju R, Prasain D, Bhattarai R, de Jong J. Preparing instruments for transcultural research: Use of the translation monitoring form with Nepali-speaking Bhutanese refugees. Transcultural Psychiatry. 1999;36(3):285–301. [Google Scholar]
- Wagnild G, Young H. Development and psychometric evaluation of the Resilience Scale. Journal of Nursing Measurement. 1993;1(2):165–178. [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. Annual Convention of the International Society for Traumatic Stress Studies. San Antonio: International Society for Traumatic Stress Studies; 1993. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. [Google Scholar]
- Westbrook D, Kirk J. The clinical effectiveness of cognitive behaviour therapy: Outcome for a large sample of adults treated in routine practice. Behaviour Research & Therapy. 2005;43:1243–1261. doi: 10.1016/j.brat.2004.09.006. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Preventing suicide: A global imperative. World Health Organization; 2014. [Google Scholar]