Abstract
Objective
Individuals seeking weight loss treatment have diverse pretreatment weight trajectories, and once enrolled, individuals’ response to weight loss treatments also varies greatly and may be influenced by the presence of binge-eating disorder (BED). Reported average weight losses may obscure these considerable differences. This study examined whether BED status and different weight-related change variables are associated with successful weight loss treatment outcomes in a controlled treatment study.
Method
Participants (N=89) with overweight/obesity, with and without BED, participated in a 3-month weight loss trial in primary care with 3- and 12-month follow-ups. We tested the prognostic significance of four weight-related change variables (The Last Supper, Early Weight Loss, Pretreatment Weight Trajectory, Weight Suppression) on outcomes (Weight Loss-Overall, Weight Loss-“Subsequent,” weight loss during second half of treatment).
Results
Early Weight Loss was positively associated with Weight Loss-Overall at post-treatment, and at 3-month and 12-month follow-up. Early Weight Loss was positively associated with Weight Loss-Subsequent at post-treatment only. No other weight-related variables were significantly associated with weight loss. Models including BED status and treatment condition were not significant.
Discussion
Participants with Early Weight Loss were more likely to continue losing weight, regardless of BED status or treatment condition. The results highlight the importance of early dedication to weight loss treatment to increase the likelihood of positive outcomes.
Keywords: binge-eating disorder, obesity, primary care, treatment, weight loss, outcomes research
Introduction
Individuals seeking weight loss treatment have broadly divergent pretreatment weight trajectories, with some seeking to enroll after recently gaining or losing a great deal of weight (Ivezaj, Kalebjian, Grilo, & Barnes, 2014). Once enrolled, individuals’ response to weight loss treatments also varies widely, with reported average weight losses obscuring considerable differences (Look Ahead Research Group, 2007). Determining how or if such variables are related to successful weight loss treatment outcomes may help to refine future weight loss interventions and to identify individuals early on who may need more intensive treatment via a stepped-care approach. Examples of these weight-related change variables, which may be related to weight loss treatment outcomes, include The Last Supper, Early Weight Loss, Pretreatment Weight Trajectory, and Weight Suppression. As reviewed below, the relevant existing literature on these factors is varied with equivocal empirical support.
“The Last Supper” is used to describe individuals overeating prior to initiating a diet (Eldredge, Agras, & Arnow, 1994; West, Harvey-Berino, Krukowski, & Skelly, 2011). Researchers examined participants’ weight change between intake assessment and their first treatment session (i.e., The Last Supper) to determine if fluctuation may be related to weight loss treatment outcomes (West et al., 2011). Individuals who lost weight during The Last Supper time period lost significantly more weight during treatment compared to participants who either gained weight or had no weight change between intake assessment and their first treatment session (West et al., 2011). Recently, another weight loss trial utilizing similar methods found no weight loss treatment response differences among participants who gained, lost, or maintained weight between intake and first treatment appointments (Kerrigan et al., 2016). Thus, it is unclear whether The Last Supper is related to weight loss treatment outcomes.
“Early Weight Loss,” or participants’ initial weight loss in treatment, may be predictive of weight loss treatment outcomes (Carels, Cacciapaglia, Douglass, Rydin, & O’Brien, 2003; Nackers, Ross, & Perri, 2010) as far as one (Fujioka et al., 2016; Waring et al., 2014) to two (Feig & Lowe, 2017) years and up to four and eight years (Unick et al., 2015) following treatment. Studies of Early Weight Loss suggest that participants who lose more weight initially during treatment will continue to lose significantly more weight compared to individuals who do not. The significance of Early Weight Loss compared to the other individual weight-related change variables is unknown.
“Pretreatment Weight Trajectory,” or participants’ weight change in the months directly preceding treatment has gained attention recently (Barnes, Blomquist, & Grilo, 2011; Blomquist et al., 2011; Ivezaj et al., 2014). Weight-loss treatment seeking individuals reported extreme ranges of weight changes prior to treatment, ranging from losing 78 to gaining 99 pounds in the year directly preceding treatment (Ivezaj et al., 2014). Research on Pretreatment Weight Trajectory suggests a possible link between weight change prior to treatment start and weight-related behaviors such as overeating (Ivezaj et al., 2014). The relationship between Pretreatment Weight Trajectory and weight-loss treatment outcomes, however, has not yet been examined.
The final variable of interest is “Weight Suppression,” or the difference between individuals’ highest adult weight and current weight (Lowe, 1984). Higher weight suppression was related to more weight gain during women’s first year of college and severe weight cycling among a community sample of individuals with overweight/obesity (de Zwaan, Engeli, & Müller, 2015). Weight suppression also is thought to maintain bulimia nervosa symptoms and chronic dieting behaviors, such that individuals suppressing more weight are more symptomatic (Bodell, Brown, & Keel, 2017; Linardon, Piedad Garcia, & Brennan, 2017). Although Weight Suppression may be related to weight loss treatment outcomes, research to date has been limited to individuals with overweight/obesity and co-existing binge-eating disorder (BED, (Zunker et al., 2011)).
How BED may impact the relationship between these four variables and weight loss treatment outcomes is unknown. BED, a psychological disorder included in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), includes frequently consuming unusually large amounts of food without the regular compensatory behaviors observed in bulimia nervosa, paired with a subjective sense of loss of control (American Psychiatric Association, 2013). BED is common among individuals seeking weight loss treatment (Barnes, White, Martino, & Grilo, 2014) and may impair individuals’ weight-loss treatment response (Blaine & Rodman, 2007; Grilo & White, 2013). Among individuals with overweight/obesity and binge-eating disorder (BED), Weight Suppression failed to predict weight change or binge-eating abstinence in a study of cognitive-behavioral therapy (CBT) for BED (Zunker et al., 2011). CBT for BED, however, typically focuses on binge eating reduction and not weight loss, resulting in small average weight losses (Grilo, 2017), including in the one study of Weight Suppression (Zunker et al., 2011). Higher Weight Suppression was, however, related to more frequent dieting among individuals seeking treatment for obesity and BED (Roehrig, Masheb, White, & Grilo, 2009). Further, Pretreatment Weight Trajectory may be differentially related to eating behaviors based on BED status (Ivezaj et al., 2014). The Last Supper was even first characterized among individuals with BED and overweight/obesity (Eldredge et al., 1994), yet neither outcome paper examined the potential impact of a BED diagnosis (Kerrigan et al., 2016; West et al., 2011), nor did the literature testing the relationship between Early Weight Loss and treatment outcomes (Carels et al., 2003; Feig & Lowe, 2017; Fujioka et al., 2016; Unick et al., 2015; Waring et al., 2014).
In summary, there is an emerging, albeit mixed, literature regarding the potential relevance of four weight-related changes variables, The Last Supper, Early Weight Loss, Pretreatment Weight Trajectory, and Weight Suppression, that may or may not be related to weight-loss treatment success. The current study examined whether different weight-related change variables were associated with successful weight loss treatment outcomes in a controlled treatment study. Refining our understanding of the nature of these weight-related variables may help us identify individuals, prior to or early into weight loss treatment, who may benefit from different or more intensive treatment (e.g., stepped-care approach, weight loss medications). Based on the existing literature, we hypothesized that Early Weight Loss would be most predictive of weight-loss treatment success and that results would differ based on BED status.
Methods
Participants
Participants were 89 consecutively evaluated adult participants with overweight and obesity (body mass index (BMI) between 25 and 55) who participated in a weight loss trial (Barnes et al., 2014; Barnes, Ivezaj, Martino, Pittman, & Grilo, 2017). Participants were recruited through referrals from primary care physicians and flyers placed in waiting/patient rooms for a weight loss treatment study being performed in an urban primary care setting. Notable exclusion criteria included BMI ≥ 55, over 65 years of age, select severe psychiatric (e.g., schizophrenia, bipolar disorder) or medical problems (e.g., cardiac disease), pregnancy/breastfeeding, and uncontrolled liver disease, hypertension, thyroid disease, or diabetes.
Overall, participants had a mean age of 47.9 years (SD=10.5, range 22–65) and a mean BMI of 35.3 kg/m2 (SD = 7.0). Participants were primarily female (76.4%, n=68), and 25.8% (n=23) of individuals met DSM-5 BED criteria (American Psychiatric Association, 2013). The sample was relatively diverse, with 65.2% of participants identifying as White, not Hispanic (n=58), 4.5% as White, Hispanic (n=4), 20.2% as African American (n=18), 5.6% as More Than One Race, not Hispanic (n=5), and 4.5% as More Than One Race, Hispanic (n=4).
Procedures
The study had full Yale IRB review and approval and all participants provided written informed consent. Participants were assessed by independent master or doctoral level psychology clinicians trained in eating and weight disorders who were blinded to treatment randomization. BED diagnosis was based on the Eating Disorder Examination (Fairburn, Wilson, & Schleimer, 1993) and the Structured Clinical Interview for DSM-IV Axis I Disorders edited for DSM-5 BED criteria (First, Gibbon, Spitzer, & Williams, 1996). Participants were randomly assigned to one of three conditions and randomization was stratified by the presence or absence of DSM-5 BED diagnosis. These treatment conditions included Motivational Interviewing and Internet Condition, Nutrition Psychoeducation and Internet Condition, or Usual Care provided by medical assistants (Barnes et al., 2014; Barnes et al., 2017). Height was measured at baseline-only using a wall measure, weight was measured using a large capacity digital scale at pretreatment assessment, baseline (first treatment session), mid-treatment (6 weeks), post-treatment (12 weeks), 3-month follow-up assessment (24 weeks), and 12-month follow-up assessment (64 weeks). Participants randomized to Usual Care (n=30) were not included in the 12-month follow-up assessment because they were offered compassionate care treatment following the 3-month follow-up assessment; therefore, 59 of the originally randomized participants were eligible to participate in the 12-month follow-up.
To provide context for the current analyses the following information is provided from the previously published RCT (Barnes et al., 2014; Barnes et al., 2017). At post-treatment and 3-month follow-up, participants randomized to Nutrition Psychoeducation (post: M = −4.9 pounds, SD = 6.1; 3-month follow-up: M = −5.7 pounds, SD = 9.0) lost significantly more weight than participants randomized to Usual Care (post: M = −0.4 pounds, SD = 6.2; 3-month follow-up: M = +0.4 pounds, SD = 7.2). There were no significant differences between Motivational Interviewing (post: M = −3.3 pounds, SD = 6.5; 3-month follow-up: M = −2.6 pounds, SD = 8.7) and Nutritional Psychoeducation or Usual Care at either time point. By 12-month follow-up, there were no significant differences between participants randomized to Nutrition Psychoeducation (M = −3.1 pounds, SD = 9.2) and Motivational Interviewing (M = +3.3 pounds, SD = 12.9). There were no significant weight loss differences at any time point based on BED status.
In addition to measuring participants’ weight at the assessment points, at pretreatment assessment, participants were asked to provide their best estimate of self-reported weight (non-pregnancy) for their highest adult weight (≥ 18 years old) and their weight 3-, 6-, and 12-months prior to their pretreatment assessment.
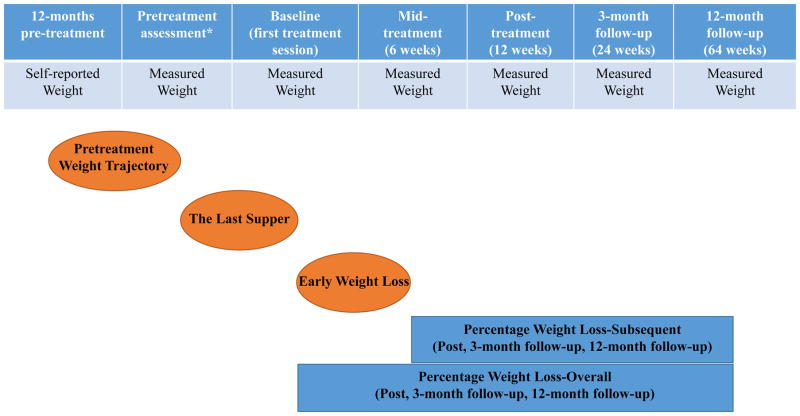
Predictor and Outcome Variables (Negative values denote weight loss; see Figure 1 for a visual depiction)
Figure 1.
Predictor and Outcome Variables
*Weight Suppression was calculated using self-reported life-time highest adult weight collected at pretreatment assessment.
Weight-Related Predictor Variables
The Last Supper percentage weight change was calculated by subtracting participants’ pretreatment assessment measured weight from their baseline session measured weight (first treatment session), dividing by pretreatment assessment measured weight, and multiplying by 100. This variable was calculated continuously to allow for more direct comparisons with other predictor variables examined, as opposed to the previous literature that categorized participants into lost, gained, or maintained categories.
Early Weight Loss percentage weight change was calculated by subtracting participants’ baseline session measured weight (first treatment session) from their mid-treatment measured weight (6 weeks), dividing by baseline session measured weight, and multiplying by 100.
Pretreatment Weight Trajectory percentage weight change was calculated by estimating a slope for weight measured across 12-, 6-, 3-months prior to pretreatment for each subject based on participants’ pretreatment assessment measured weight and their self-reported weight 12-, 6-, and 3-months prior to starting treatment.
Weight Suppression percentage weight change was calculated by subtracting participants’ self-reported highest adult weight from their pretreatment assessment measured weight, dividing by their self-reported highest adult weight, and multiplying by 100. Using percentage Weight Suppression appears to measure the same construct as the traditional measurement (i.e., kilogram or pounds difference) while controlling for potentially confounding data (Schaumberg et al., 2016). Negative values denoted participants suppressing weight at pretreatment assessment from their highest self-reported adult weight. A value of 0 indicated participants were assessed for treatment at their highest adult weight.
Treatment Outcome Weight Variables
Weight Loss-Overall (Carels et al., 2003; Fujioka et al., 2016; Unick et al., 2015; Waring et al., 2014) was calculated for post-treatment, 3-month follow-up and 12-month follow-up assessments by subtracting participants’ baseline measured weight (first treatment session) from their measured weight at each time point, dividing by their baseline measured weight, and multiplying by 100. Despite the obvious overlap between this variable Early Weight loss and Weight Loss-Overall, we chose to provide these descriptive analyses for context and to replicate previous literature (Carels et al., 2003; Fujioka et al., 2016; Unick et al., 2015; Waring et al., 2014). While our primary analysis is described in the following paragraph (i.e., predicting subsequent weight loss), it is clinically informative for clinicians to grasp the total magnitude of weight loss as context.
Weight Loss-Subsequent (Feig & Lowe, 2017) was calculated using weight measured at mid-treatment (6 weeks) as the baseline to avoid overlap with the Early Weight Loss predictor variable. Specifically, this outcome was calculated by subtracting participants’ mid-treatment measured weight from their measured weight at post-treatment (and subsequent time points), dividing by their mid-treatment measured weight, and multiplying by 100.
Statistical Analyses
For each outcome, separate linear mixed models were developed for each predictor. These models included each predictor as a continuous variable and time (post, 3-month follow-up, 12-month follow-up) as a within-subjects factor. Inclusion of the predictor by time interaction, whether significant or not, allowed for a priori estimation of slopes to assess the association between each predictor and each outcome at the three time points. The best-fitting variance-covariance structure was evaluated using information criteria. To test whether any associations uncovered in the above models differed by BED status or treatment assignment, we tested all 2- and 3-way interactions with these variables in separate models. No interactions were observed, and BED status and treatment assignment were dropped from the model. Because of differences in weight loss between treatments observed in the original RCT, treatment assignment was also considered as a covariate in the above models. All results were substantively and statistically similar with or without treatment assignment; thus, treatment assignment was dropped for parsimony. Similar results were also found with and without BED status included as a covariate. All analyses were conducted using SAS, version 9.4 (Cary, NC).
Results
See Table 1 for means and standard deviations for weight-related change predictor and weight loss treatment outcome variables.
Table 1.
Means (M) and standard deviations (SD) for predictor and outcome variables in percentage pounds.
| N (%) | M | SD | |
|---|---|---|---|
| Outcome Variablesa | |||
| Weight Loss-Overallb | |||
| Post Treatment | 84 (94%) | −1.30 | 2.94 |
| 3-month follow-up | 83 (93%) | −1.39 | 4.18 |
| 12-month follow-upc | 44 (75%) | −0.23 | 5.21 |
| Weight Loss-Subsequentd | |||
| Post Treatment | 76 (85%) | −0.26 | 1.58 |
| 3-month follow-up | 75 (84%) | −0.26 | 3.17 |
| 12-month follow-upc | 40 (68%) | 1.72 | 3.93 |
| Predictor Variablesa | |||
| The Last Supper | 88 (99%) | 0.05 | 1.58 |
| Early Weight Loss | 78 (88%) | −1.15 | 2.25 |
| Pretreatment Weight Trajectory | 81 (91%) | 0.58 | 1.43 |
| Weight Suppression | 87 (98%) | −4.19 | 5.39 |
Note.
Negative values=weight loss.
Percentage weight change from first session.
Usual Care participants were not included in the 12-month follow-up as they were provided compassionate care after the 3-month follow-up.
Percentage weight change from mid-treatment (week 6).
Correlations Among Predictor Variables
The Last Supper and Early Weight Loss were not significantly correlated with any other predictor variables. Pretreatment Weight Trajectory was significantly correlated with Weight Suppression (r(79) = 0.48, p < 0.0001).
Weight Loss-Overall
Estimated slopes indicated that Early Weight Loss was positively associated with Weight Loss-Overall at post-treatment (b = 1.18±.08, r = .87, p = .0001), and at 3-month (b = 1.22±.16, r = .68, p = .0001) and 12-month (b = 1.15±.24, r = .56, p = .0001) follow-up. There was no significant interaction, however, between Early Weight Loss and Time (F(2, 110) = .20, p = .82). The Last Supper, Pretreatment Weight Trajectory, and Weight Suppression predictor variables were not significantly associated with Weight Loss-Overall. There were no significant main or interaction effects when adding BED status or treatment condition into the models.
Weight Loss-Subsequent
Slopes estimated from the mixed model indicated that Early Weight Loss was positively associated with Weight Loss-Subsequent at post-treatment, (b = 0.18±.08, r = .26, p = .018), but not at 3-month (b = 0.24±.16, r = .17, p = .14) or 12-month (b = 0.10±.25, r = .07, p = .68) follow-up. The estimated slopes, however, at each time point did not significantly differ (Early Weight Loss by time interaction: F(2, 110) = .25, p = .78). The Last Supper, Pretreatment Weight Trajectory, and Weight Suppression predictor variables were not significantly associated with Weight Loss-Subsequent. There were no significant main or interaction effects when adding BED status or treatment condition into the models.
Discussion
This is the first direct comparison of four weight-related change variables identified in the literature, their relationship to weight loss treatment outcomes, and the impact of BED on those relationships. Participants’ Early Weight Loss was the only predictor variable significantly related to weight loss treatment outcomes, regardless of BED status or treatment assignment. The Last Supper, Pretreatment Weight Trajectory, and Weight Suppression were unrelated to weight loss treatment outcomes.
BED status was unrelated both to weight loss in the original RCT (Barnes et al., 2014; Barnes et al., 2017) and to the relationship between Early Weight Loss and weight loss outcomes in the current analyses. These results are noteworthy given the previous mixed literature showing that BED may (Blaine & Rodman, 2007; Grilo & White, 2013) or may not (Barnes et al., 2014; Barnes et al., 2017; Barnes et al., 2018) moderate individuals’ response to weight loss treatment. Further, individuals with BED previously were found to gain significantly more weight in the year prior to initiating weight loss treatment when compared to their counterparts without BED (Ivezaj et al., 2014). The current findings may be particularly encouraging for those with BED seeking weight loss treatment, although replication with larger BED samples is warranted.
Overall, the current data suggest that irrespective of individuals’ weight changes prior to their first treatment session, it is important for them to “get off to a good start” immediately upon treatment commencement. Participants with more Early Weight Loss were more likely to continue losing weight, regardless of the treatment received. Further, Early Weight Loss was strongly predictive of weight loss outcomes even in the context of a weight loss intervention designed to be scalable and low-burden to increase generalizability to other primary care centers (i.e., 2.5 hours over 12 weeks (Barnes et al., 2014; Barnes et al., 2017). While the average weight loss was relatively small, effect sizes for both intervention conditions were medium to medium-large and there was much variability, with approximately 25% of participants receiving treatment reaching a clinically meaningful weight loss of 5% or more by 3-month follow-up (Barnes et al., 2014). The current data support previously published trials examining Early Weight Loss (Carels et al., 2003; Feig & Lowe, 2017; Fujioka et al., 2016; Nackers et al., 2010; Unick et al., 2015; Waring et al., 2014) and extend them to individuals diagnosed with BED. The findings maintained through post-treatment regardless of how weight loss outcomes were calculated. We note, however, that to our knowledge, this is only the second paper to examine “subsequent” weight loss (i.e., calculated currently as “Weight Loss-Subsequent”(Feig & Lowe, 2017), and that the remaining research reports did not specify whether or not there was overlap between the calculation of Early Weight Loss and weight loss outcome variables (i.e., calculated currently as “Weight Loss-Overall”; (Carels et al., 2003; Fujioka et al., 2016; Nackers et al., 2010; Unick et al., 2015; Waring et al., 2014)).
Future research examining Early Weight Loss will need to address the potential overlap between the predictor (Early Weight Loss) and outcome (overall versus subsequent weight loss) variables. Closer examination of factors related to Early Weight Loss also will be important for future research. Based on previous studies, variables of interest include a more consistent pattern of initial weight loss (Feig & Lowe, 2017) and treatment adherence (Nackers et al., 2010; Unick et al., 2015). Even very early treatment nonadherence may be a signal for changing weight loss treatment approach (Unick et al., 2015). Perhaps individual variables such as stress, life events, or motivation impact treatment attendence and adherence, and therefore Early Weight Loss. While preliminary, we do know from the current data that Early Weight Loss was unrelated to any pretreatment weight change (The Last Supper, Pretreatment Weight Trajectory, Weight Suppression), further highlighting the significance of this critical time period at treatment start.
In contrast to an initial report (West et al., 2011), this is the second study to report no significant relationship between The Last Supper and weight loss outcomes (Kerrigan et al., 2016). The current data, in combination with the previous two Last Supper studies (West et al., 2011), highlight the importance of obtaining a true pre-treatment weight at the first treatment appointment as individuals’ weight can change dramatically between their initial screening/assessment appointment and when they actually start treatment (Kerrigan et al., 2016). Similarly, despite current participants reporting a wide range of Weight Suppression (0 to −92 pounds) and Pretreatment Weight Trajectories (from 37 pounds lost to 99 pounds gained in the year preceding treatment), neither variable was related to weight loss outcomes. These results are similar to those of Zunker and colleagues (Zunker et al., 2011) who examined Weight Suppression and weight loss within a BED only sample and was the first to examine Pretreatment Weight Trajectories and treatment outcomes. While beyond the scope of the current study, future research should examine if any of these pretreatment weight-related variables are associated with weight regain following treatment.
It is important to consider the limitations of the current study. First, the sample size was relatively small, particularly for the subgroup of individuals with BED and at 12-month follow-up assessment as participants randomized to Usual Care were provided compassionate care and not included in this final assessment. Future research should include a larger sample of participants, both with and without BED. Second, the average weight losses in this scalable primary care intervention were relatively small, restricted range could account for the null results. Similarly, the results may not generalize to individuals seeking weight loss treatment in specialty care clinics. Third, some of the predictor variables (Pretreatment Weight Trajectory, Weight Suppression), relied on participants’ self-reported weights. The literature suggests, however, that similar patient groups tend to be reasonably accurate when providing self-report weight (Ivezaj et al., 2014). Fourth, the Early Weight Loss data was collected halfway through treatment. It is likely that even earlier weight loss may be predictive of treatment outcomes.
In summary, the current results replicate and extend the previous literature by highlighting the importance of Early Weight Loss during weight loss treatment, regardless of BED status or the type of weight loss treatment received. Other pretreatment weight-related change variables, including The Last Supper, Pretreatment Weight Trajectory, and Weight Suppression were not significantly related to weight loss. It may be helpful for clinicians to highlight these findings when working with individuals both with and without BED seeking weight loss as they can consider the beginning of treatment a critical period for swift action. Similarly, it may be important for clinicians to consider a stepped-care or different treatment approach for individuals who do not respond initially to weight loss treatment.
Acknowledgments
Funding: This study was supported by NIH career development awards, K23-DK092279 for RDB and K24-DK070052 for CMG.
Footnotes
Conflicts of Interest: RDB, VI, and BPP have no conflicts of interest. CMG reports no relevant conflicts of interest but notes that he has received honoraria from professional and scientific conferences and from CME institutes for lectures and presentations, and book royalties from Guilford Press and Taylor and Francis for academic books.
References
- Association, A. P. Diagnostic and statistical manual of mental disorders (DSM-5®) American Psychiatric Pub; 2013. [DOI] [PubMed] [Google Scholar]
- Barnes RD, Blomquist KK, Grilo CM. Exploring pretreatment weight trajectories in obese patients with binge eating disorder. Comprehensive Psychiatry. 2011;52(3):312–318. doi: 10.1016/j.comppsych.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes RD, Ivezaj V, Martino S, Pittman BP, Grilo CM. Back to Basics? No Weight Loss from Motivational Interviewing Compared to Nutrition Psychoeducation at One-Year Follow-Up. Obesity. 2017;25(12):2074–2078. doi: 10.1002/oby.21972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes RD, Ivezaj V, Martino S, Pittman BP, Paris M, Grilo CM. Examining motivational interviewing plus nutrition psychoeducation for weight loss in primary care. Journal of Psychosomatic Research. 2018;104:101–107. doi: 10.1016/j.jpsychores.2017.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes RD, White MA, Martino S, Grilo CM. A randomized controlled trial comparing scalable weight loss treatments in primary care. Obesity. 2014;22(12):2508–2516. doi: 10.1002/oby.20889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaine B, Rodman J. Responses to weight loss treatment among obese individuals with and without BED: a matched-study meta-analysis. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2007;12(2):54–60. doi: 10.1007/BF03327579. [DOI] [PubMed] [Google Scholar]
- Blomquist KK, Barnes RD, White MA, Masheb RM, Morgan PT, Grilo CM. Exploring weight gain in year before treatment for binge eating disorder: a different context for interpreting limited weight losses in treatment studies. International Journal of Eating Disorders. 2011;44(5):435–439. doi: 10.1002/eat.20836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodell LP, Brown TA, Keel PK. Weight suppression predicts bulimic symptoms at 20-year follow-up: The mediating role of drive for thinness. Journal of Abnormal Psychology. 2017;126(1):32. doi: 10.1037/abn0000217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carels RA, Cacciapaglia HM, Douglass OM, Rydin S, O’Brien WH. The early identification of poor treatment outcome in a women’s weight loss program. Eating Behaviors. 2003;4(3):265–282. doi: 10.1016/S1471-0153(03)00029-1. doi: https://doi.org/10.1016/S1471-0153(03)00029-1. [DOI] [PubMed] [Google Scholar]
- de Zwaan M, Engeli S, Müller A. Temperamental factors in severe weight cycling. A cross-sectional study. Appetite. 2015;91:336–342. doi: 10.1016/j.appet.2015.04.064. [DOI] [PubMed] [Google Scholar]
- Eldredge KL, Agras WS, Arnow B. The last supper: emotional determinants of pretreatment weight fluctuation in obese binge eaters. International Journal of Eating Disorders. 1994;16(1):83–88. doi: 10.1002/1098-108x(199407)16:1<83::aid-eat2260160109>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Wilson GT, Schleimer K. Binge eating: Nature, assessment, and treatment. Guilford Press; New York: 1993. [Google Scholar]
- Feig EH, Lowe MR. Variability in Weight Change Early in Behavioral Weight Loss Treatment: Theoretical and Clinical Implications. Obesity. 2017;25(9):1509–1515. doi: 10.1002/oby.21925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JB. User’s guide for the structured clinical interview for DSM-IV axis I Disorders—Research version. New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Fujioka K, O’Neil PM, Davies M, Greenway F, Lau CWD, Claudius BPH, … Wilding J. Early Weight Loss with Liraglutide 3.0 mg Predicts 1-Year Weight Loss and is Associated with Improvements in Clinical Markers. Obesity. 2016;24(11):2278–2288. doi: 10.1002/oby.21629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM. Psychological and Behavioral Treatments for Binge-Eating Disorder. The Journal of Clinical Psychiatry. 2017;78:20–24. doi: 10.4088/JCP.sh16003su1c.04. [DOI] [PubMed] [Google Scholar]
- Grilo CM, White MA. Orlistat with behavioral weight loss for obesity with versus without binge eating disorder: Randomized placebo-controlled trial at a community mental health center serving educationally and economically disadvantaged Latino/as. Behaviour Research and Therapy. 2013;51(3):167–175. doi: 10.1016/j.brat.2013.01.002. doi: https://doi.org/10.1016/j.brat.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivezaj V, Kalebjian R, Grilo CM, Barnes RD. Comparing weight gain in the year prior to treatment for overweight and obese patients with and without binge eating disorder in primary care. Journal of Psychosomatic Research. 2014;77(2):151–154. doi: 10.1016/j.jpsychores.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerrigan SG, Schaumberg K, Kase C, Gaspar M, Forman E, Butryn ML. From last supper to self-initiated weight loss: Pretreatment weight change may be more important than previously thought. Obesity. 2016;24(4):843–849. doi: 10.1002/oby.21423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon J, Piedad Garcia X, Brennan L. Predictors, moderators, and mediators of treatment outcome following manualised cognitive-behavioural therapy for eating disorders: A systematic review. European Eating Disorders Review. 2017;25(1):3–12. doi: 10.1002/erv.2492. [DOI] [PubMed] [Google Scholar]
- Look Ahead Research Group. Reduction in Weight and Cardiovascular Disease Risk Factors in Individuals With Type 2 Diabetes: One-Year Results of the Look AHEAD Trial. Diabetes Care. 2007;30(6):1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe MR. Dietary concern, weight fluctuation and weight status: Further explorations of the Restraint Scale. Behaviour Research and Therapy. 1984;22(3):243–248. doi: 10.1016/0005-7967(84)90004-4. [DOI] [PubMed] [Google Scholar]
- Nackers LM, Ross KM, Perri MG. The association between rate of initial weight loss and long-term success in obesity treatment: does slow and steady win the race? International Journal of Behavioral Medicine. 2010;17(3):161–167. doi: 10.1007/s12529-010-9092-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roehrig M, Masheb RM, White MA, Grilo CM. Dieting frequency in obese patients with binge eating disorder: behavioral and metabolic correlates. Obesity. 2009;17(4):689–697. doi: 10.1038/oby.2008.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaumberg K, Anderson LM, Reilly EE, Gorrell S, Anderson DA, Earleywine M. Considering alternative calculations of weight suppression. Eating Behaviors. 2016;20:57–63. doi: 10.1016/j.eatbeh.2015.11.003. [DOI] [PubMed] [Google Scholar]
- Unick JL, Neiberg RH, Hogan PE, Cheskin LJ, Dutton GR, Jeffery R, … Wing RR. Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later. Obesity. 2015;23(7):1353–1356. doi: 10.1002/oby.21112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waring ME, Schneider KL, Appelhans BM, Busch AM, Whited MC, Rodrigues S, … Pagoto SL. Early-treatment weight loss predicts 6-month weight loss in women with obesity and depression: Implications for stepped care. Journal of Psychosomatic Research. 2014;76(5):394–399. doi: 10.1016/j.jpsychores.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West DS, Harvey-Berino J, Krukowski RA, Skelly JM. Pretreatment weight change is associated with obesity treatment outcomes. Obesity. 2011;19(9):1791–1795. doi: 10.1038/oby.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zunker C, Crosby RD, Mitchell JE, Wonderlich SA, Peterson CB, Crow SJ. Weight suppression as a predictor variable in treatment trials of bulimia nervosa and binge eating disorder. International Journal of Eating Disorders. 2011;44(8):727–730. doi: 10.1002/eat.20859. [DOI] [PMC free article] [PubMed] [Google Scholar]