Abstract
Objective
Fat talk—negative communication about weight—is common in the media, peer groups, and families. Little is known about parental fat talk directed at oneself or others. This study examined associations between different forms of parental fat talk and child disordered eating behaviors and weight, and differences by child sex and age.
Methods
Parents of pre-adolescents or adolescents (N=581) reported fat talk about themselves (self-fat talk), others (obesity-fat talk) and their child (child-fat talk).
Results
76.0% of parents reported regular self-fat talk in front of children, 51.5% reported obesity-fat talk and 43.6% reported child-fat talk. Fat talk did not differ significantly between parents of pre-adolescents and adolescents but was more common with sons than daughters. Of the three forms of fat talk, only child-fat talk was associated with all child eating and weight variables (binge eating, overeating, secretive eating, and overweight/obesity); associations were strongest for adolescent girls. Child sex was associated with secretive eating and overweight/obesity.
Conclusions
Parents reported using different forms of fat talk frequently. Parent self- and obesity-fat talk were reported more frequently, but child-fat talk was the most strongly associated with children’s eating and weight. Because of associations with disordered eating behaviors, intervening to reduce fat talk might contribute to improving pediatric disordered eating and weight-related interventions.
Keywords: adolescent, pediatric, obesity, parenting, fat talk, binge eating
Pediatric obesity is a public health concern that affects 17% of children and adolescents in the United States and can have adverse consequences for physical and psychosocial development (1). There is evidence linking childhood obesity with adult obesity (2) and disordered eating behaviors such as binge eating (3), which makes childhood obesity costly to public health. Parents are key stakeholders in and greatly influence their children’s health by controlling the foods that are available to them, setting daily schedules, and providing access to healthcare (4, 5). Parents can create healthy environments for their children at home and model eating and body image attitudes (6), thereby encouraging children’s development of healthy eating behaviors and body image. One way that parents may be able to improve the home environment is to alter the extent to which they engage in “fat talk” around their children, but this has received minimal research attention.
“Fat talk” is defined as disparaging comments about body image and weight (7), and can include comments about weight, eating and exercise habits, fear of overweight, appearance and behavior comparisons, or strategies to change appearance (8). Fat talk is associated with body dissatisfaction, yet individuals who use fat talk paradoxically seek to alleviate weight-related guilt (e.g., by seeking reassurance that eating high-calorie foods is not abnormal), increase social conformity (e.g., joining appearance-focused conversations), and decrease body-image dissatisfaction (e.g., seeking affirmation from peers about body image) (7, 9–11). Fat talk is pervasive in Western culture, and can be found in the media, within peer groups, and within families (7, 8, 12). Fat talk can have detrimental effects on body image, self-confidence, and eating behaviors (9, 10, 13). Descriptive studies suggest that fat talk such as weight teasing increases risk for excess weight gain and body dissatisfaction (13, 14), as well as eating-disorder behaviors such as fasting and vomiting (15). Experimental studies have also shown an association between hearing fat talk and heightened body dissatisfaction (10, 16).
Fat talk has been studied primarily among college-aged and young adult women (9, 10), yet the parent-child relationship is an important area of study because negative weight-related comments from parents can reinforce sociocultural norms about body image and eating (17). Fat talk can include direct comments that focus on the child’s weight—such as teasing, blame, or criticism—and can also include indirect comments that focus on the individual’s own weight or on the weight of others and not on the weight of the person hearing the fat talk (18). Some research has found that parental weight-related teasing (19) and maternal comments about their own weight (20, 21) are both associated with children’s body dissatisfaction and disordered eating, and fat talk may have a role in the onset of eating disorders (22).
The current study aimed to investigate associations between fat talk in parent-child interactions and children’s eating behaviors and weight. The aim of the study was (a) to examine parent-reported fat talk (directed toward self, obesity, and child); (b) to examine associations of parental fat talk with child disordered eating behaviors and weight; and (c) to compare parental fat talk by child age (pre-adolescents and adolescents) and sex (boys and girls). We hypothesized that parental fat talk would be associated with more child disordered eating behaviors (overeating, binge eating, and secretive eating) and with child overweight/obesity. We further hypothesized that this association would be strongest when parental fat talk was about the child (i.e., rather than about the parent or about another person). Finally, because past research has shown more fat talk amongst adolescents and girls than children and boys (10), and has shown associations between eating-disorder psychopathology and fat talk (9), we hypothesized a similar pattern would emerge for parental fat talk.
Methods
Participants
Participants were parents (N=581) of pre-adolescents (ages 9–11; n=278) or adolescents (12–15; n=301). Participants were recruited from the Mechanical Turk website to complete a one-time online survey on parents’ opinions about weight and eating. Mechanical Turk provides high-quality and convenient data; comparisons indicate the psychometric properties of measures completed by participants recruited from Mechanical Turk do not differ in reliability or validity from participants recruited using traditional sources (23). Mechanical Turk yields samples with greater diversity in geography and demographic characteristics than undergraduate samples (23–25), and has been used in psychological and psychiatric research (26) including eating (27) and weight bias research (28). To be eligible to complete the survey, parents had to be primary caregivers (i.e., their child lived in their household more than half the time).
Participants were mothers (n=387, 66.7%) and fathers (n=193, 33.2%; n=1 gender not reported), most of whom were biological parents (n=504, 86.7%). Parents self-identified as White (n=467, 80.4%), Black (n=43, 7.4%), Hispanic (n=25, 4.3%), Asian (n=14, 2.4%), or Other (n=34, 5.5%). On average, parents were 38.66 (SD=7.97) years old and had BMIs of 29.60 kg/m2 (SD=7.83). In the survey, parents were asked to answer items about one child. Responses pertained to daughters (n=289, 49.7%) and sons (n=292, 50.3%). On average, children’s BMI z-scores (age- and sex-specific) were in the 66.60th percentiles (SD=31.57; BMI z-score M=0.59, SD=1.38). This study was reviewed and approved by our university’s institutional review board; all participants provided informed consent electronically.
Measures
Body Mass Index (BMI)
Parents reported their child’s age, height and weight, which were used to calculate child BMI z-score and child BMI percentile. Parents also reported their own height and weight, which were used to calculate BMI.
Fat Talk Questionnaire (FTQ)
This 16-item measure of negative conversations about weight (“fat talk”) (29) was adapted to assess how parents talk in front of their child about themselves, people with obesity, and their child. For example, “When I’m with my child, I comment that my arms are too flabby”; “When I’m with my child and see an obese person, I comment that the obese person’s arms are too flabby”; “When I notice that my child has gained weight, I comment that his/her arms are too flabby.” Items are scored on a five-point scale (i.e., never, rarely, sometimes, often, always). The FTQ had excellent internal consistency in the original FTQ study (α=.93) (29) and in the current study (self α=.96, obesity α=.97, child α=.96).
Eating Disorder Examination Questionnaire (EDE-Q)
The EDE-Q assesses eating-disorder psychopathology over the past 28 days on seven-point scales (30); the current study used a brief empirically-supported version of the full scale, which has been shown to demonstrate superior psychometric properties in nonclinical (31) and clinical (32) studies compared with the psychometric properties of the original measure. Subscales (Restraint, Overvaluation, Body Dissatisfaction) were internally consistent in earlier work, α=.89–.91 (31), and in the current study α=.90–.94. Additionally, we adapted the behavioral items (overeating, binge-eating episodes, secretive eating) for parents to report about their child.
Statistical analyses
Frequencies of individual FTQ statements were used to calculate the percentages of parents who indicated that they “always,” “often,” or “sometimes” said individual fat talk statements in front of their child. ANOVAs compared fat talk by child sex and age. Post-hoc tests using a Tukey correction for multiple comparisons evaluated pairwise differences. Chi-square tests compared eating behaviors and weight across the four sex/age groups. Correlations evaluated associations between fat talk and eating-disorder psychopathology. Multivariate logistic regressions evaluated whether child sex, child age group, self-fat talk, fat talk about people with obesity, and child-fat talk significantly predicted child eating behaviors and weight status. Additional logistic regressions by child sex/age group evaluated whether child age group, self-fat talk, fat talk about people with obesity, and child-fat talk significantly predicted child eating behaviors and weight status.
Results
Child Weight and Eating Behaviors
Chi-square tests compared child weight and eating behaviors across the four sex/age groups. Regular eating behaviors were dichotomized as weekly or greater (presence) or less than weekly (absence); weight was dichotomized as overweight/obesity or healthy-weight. More parents reported the presence of overeating for adolescent boys, χ2(3) = 10.28, p = 0.016, than any other group. Weight status also differed by group, χ2(3) = 14.08, p = 0.003: more pre-adolescent boys (51.1%) had overweight/obesity than pre-adolescent girls (37.1%) and more adolescent boys (48.4%) had overweight/obesity than adolescent girls (32.4%). Child binge eating, χ2(3) = 3.41, p = 0.33, and secretive eating, χ2(3) = 5.68, p = 0.13, did not significantly differ among the four groups.
Parental Fat Talk
Parental reports of regularly using fat talk in the presence of their children were common: 76.0% of parents reported sometimes (or more often) saying at least one fat talk statement about themselves in front of their child, 51.5% of parents reported saying at least one fat talk statement about people with obesity in front of their child, and 43.6% of parents reported saying at least one fat talk statement about the child in front of the child. Table 1 shows the percentages of parents who indicated that they “always,” “often,” or “sometimes” endorse individual fat talk statements about themselves, about people with obesity, and about their child. Notably, one-third of parents reported that they complain that they are fat in front of their children. About one-quarter of parents report regularly remarking that a person with obesity is out of shape in the presence of their children. Parents also reported fat talk about their child, with 18.3% of parents reporting they comment that their child has gained weight, and 18.5% of parents report telling their child that they should not be eating fattening foods.
Table 1.
Parental Fat Talk
| Statement | Self | Obesity | Child |
|---|---|---|---|
| When I’m with my child, I complain that my arms are too flabby. | 19.8% | 10.2% | 5.4% |
| When I’m with my child, I complain that my stomach is fat. | 36.6% | 13.5% | 9.3% |
| When I’m with my child, I criticize my body compared to thin models in magazines. | 14.5% | 8.6% | 5.2% |
| When I’m with my child, I complain that my body is out of proportion. | 15.9% | 14.1% | 6.7% |
| When I’m with my child, I complain that I hate my whole body. | 13.6% | 8.6% | 5.5% |
| When I’m with my child, I complain that I am fat. | 34.7% | 19.8% | 6.1% |
| When I’m with my child, I complain that I should not be eating fattening foods. | 41.4% | 19.8% | 18.5% |
| When I’m with my child, I complain that I’ve gained weight. | 34.6% | n/a | 18.3% |
| When I’m with my child, I complain that my clothes are too tight. | 26.6% | 17.6% | 15.4% |
| When I’m with my child, I complain that I need to stop eating so much. | 31.2% | 20.0% | 14.4% |
| When I’m with my child, I criticize my body compared to my friends’ bodies. | 11.1% | 12.6% | 5.9% |
| When I’m with my child, I complain that I feel pressure to be thin. | 11.4% | 9.7% | 6.6% |
| When I’m with my child, I complain that my body is disgusting. | 11.6% | 11.9% | 5.3% |
| When I’m with my child, I complain that I’m not in shape. | 42.8% | 22.7% | 11.9% |
Note. Percentages reflect the proportion of parents from the full sample who reported regularly (“sometimes,” “often,” or “always”) using the fat talk statement when they were with their child. 76.0% of parents reported regular self-fat talk in front of children, 51.5% reported obesity-fat talk and 43.6% reported child-fat talk.
Fat Talk Sex/Age Differences
Parents’ self-fat talk did not differ between sons and daughters, t(572)=0.20, p=0.85, d=0.016, nor did fat talk about people with obesity, t(573)=0.98, p=0.33, d=0.082. However, parents reported more child-fat talk directed towards sons (M=1.35, SD=0.70) than daughters (M=1.24, SD=0.54), t(539.19)=2.11, p=0.035, d=0.176.
No forms of fat talk significantly differed by child age: parental self-fat talk, t(572)=1.51, p=0.13, d=0.126, fat talk about people with obesity, t(573)=1.31, p=0.19, d=0.110, and child-fat talk, t(575)=1.21, p=0.23, d=0.101.
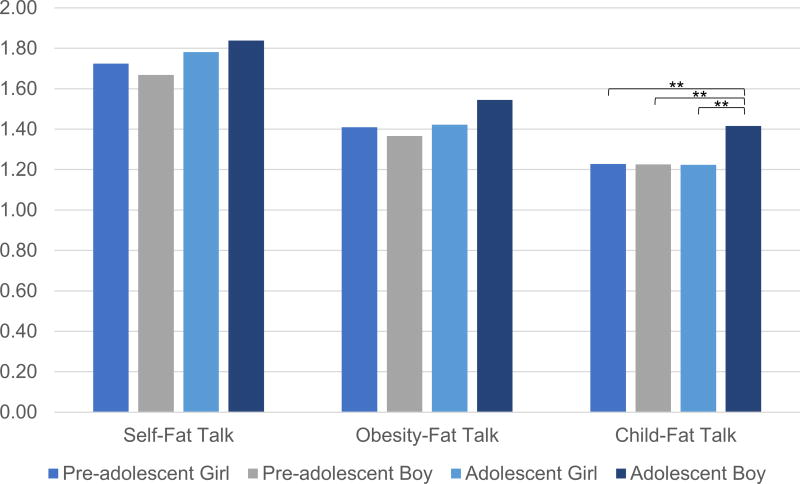
ANOVAs included four child groups (pre-adolescent girls, pre-adolescent boys, adolescent girls, and adolescent boys) to examine whether parent-reported child characteristics were associated with the amount of parental fat talk. Means are depicted in Figure 1. Parents’ self-fat talk, F(3,568)=1.06, p=0.36, ηp2=.006, and fat talk about people with obesity, F(3,568)=1.56, p=0.20, ηp2=.008, did not significantly differ among the four groups. However, there were significant differences in child-fat talk, F(3,568)=3.97, p=0.008, ηp2=0.021, such that parents of adolescent boys (M=1.42, SD=0.76) reported significantly more child-fat talk than parents of pre-adolescent boys (M=1.23, SD=0.51, p=0.006), pre-adolescent girls (M=1.23, SD=0.52, p=0.006), and adolescent girls (M=1.22, SD=0.51, p=0.004). An additional ANCOVA that included child BMI z-score as a covariate showed the same pattern of findings. Even with BMI z-score included in the model, age/sex groups were significantly different, F(3,568)=3.17, p=0.02, ηp2=0.017, such that parents of adolescent boys reported more child-fat talk than parents of pre-adolescent boys (p=0.013), pre-adolescent girls (p=0.013), and adolescent girls (p=0.013).
Figure 1.
Fat Talk by Sex and Age groups
Figure 1 shows mean levels of three different forms of parental fat talk across pre-adolescent girls, pre-adolescent boys, adolescent girls, and adolescent boys. **p<0.01.
Fat Talk and Weight and Eating Behaviors
Table 2 summarizes the multivariate logistic regression analyses evaluating whether child sex, child age group, and the three types of parent fat talk were significantly associated with child disordered eating behaviors and weight. Child-fat talk was significantly associated with binge eating, overeating, secretive eating, and overweight/obesity. Child sex was significantly associated with secretive eating and overweight/obesity, but not binge eating or overeating. Child age group, self-fat talk, and obesity-fat talk were not significantly associated with overweight/obesity or disordered eating behaviors.
Table 2.
Logistic regression associations of different forms of parental fat talk with child disordered eating and weight.
| χ2 | df | p | Nagelkerke R2 |
Child Sex Odds Ratio (95% CI) |
Child Age Odds Ratio (95% CI) |
Self-Fat talk Odds Ratio (95% CI) |
Obesity-Fat Talk Odds Ratio (95% CI) |
Child-Fat talk Odds Ratio (95% CI) |
|
|---|---|---|---|---|---|---|---|---|---|
| Binge Eating | 67.41 | 5 | <.001 | .168 | 1.22 (0.80–1.85) | 1.11 (0.73–1.68) | 1.39 (0.76– 2.55) | 1.19 (0.75–1.88) | 4.86*** (3.03–7.78) |
| Overeating | 51.88 | 5 | <.001 | .116 | 0.89 (0.63–1.27) | 1.21 (0.85–1.73) | 1.02 (0.65–1.60) | 1.36 (0.93–1.98) | 2.93*** (2.02–4.27) |
| Secretive Eating | 66.63 | 5 | <.001 | .160 | 1.58* (1.06–2.37) | 1.10 (0.74–1.65) | 1.26 (0.72– 2.20) | 1.46 (0.95–2.27) | 4.04*** (2.60– 6.26) |
| Overweight/Obesity | 55.79 | 5 | <.001 | .124 | 0.57** (0.40–0.81) | 0.78 (0.55–1.11) | 0.91 (0.59–1.42) | 0.68 (0.47–1.00) | 3.40*** (2.31–5.01) |
Note.
p<.05,
p<.01,
p<.001.
Child sex was coded 0=male, 1=female; child age was coded 0=pre-adolescent, 1=adolescent.
Table 3 summarizes a series of exploratory parallel analyses conducted to evaluate whether the three types of parent fat talk were significantly associated with child disordered eating behaviors and weight, in each of the child age/sex groups. Results paralleled overall analyses: child-fat talk was significantly associated with binge eating, overeating, secretive eating, and overweight/obesity across child age/sex groups, except that child-fat talk was not associated with binge eating among pre-adolescent girls, or overeating among pre-adolescent boys. Odds ratios for child-fat talk were largest among adolescent girls. Self-fat talk was not associated with any child disordered eating behaviors or weight across child age/sex groups. Obesity-fat talk was not associated with any child disordered eating behaviors or weight, except for secretive eating among adolescent girls.
Table 3.
Logistic regressions by age and sex group.
| Pre-Adolescent Girl (n=140) | Pre-Adolescent Boy (n=137) | Adolescent Girl (n=148) | Adolescent Boy (n=155) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Self-Fat talk Odds Ratio (95% CI) |
Obesity- Fat Talk Odds Ratio (95% CI) |
Child- Fat talk Odds Ratio (95% CI) |
Self-Fat talk Odds Ratio (95% CI) |
Obesity- Fat Talk Odds Ratio (95% CI) |
Child- Fat talk Odds Ratio (95% CI) |
Self-Fat talk Odds Ratio (95% CI) |
Obesity- Fat Talk Odds Ratio (95% CI) |
Child- Fat talk Odds Ratio (95% CI) |
Self-Fat talk Odds Ratio (95% CI) |
Obesity- Fat Talk Odds Ratio (95% CI) |
Child- Fat talk Odds Ratio (95% CI) |
|
| Binge Eating | 2.66 (0.71–9.95) | 1.85 (0.77–4.44) | 2.32 (0.97–5.51) | 1.95 (0.50–7.59) | 0.62 (0.22–1.76) | 4.88** (1.67–14.26) | 0.88 (0.24–3.28) | 1.35 (0.47–3.84) | 17.95*** (5.60–57.53) | 1.07 (0.36–3.18) | 1.12 (0.49–2.57) | 3.77** (1.56–9.12) |
| Overeating | 0.82 (0.33–2.05) | 2.09 (0.98–4.44) | 2.73* (1.25–5.97) | 0.86 (0.35–2.13) | 1.37 (0.61–3.05) | 2.14 (0.96–4.77) | 1.34 (0.49–3.65) | 1.23 (0.54-–2.81) | 6.00*** (2.74–13.14) | 1.32 (0.56–3.09) | 0.94 (0.47–1.90) | 2.16* (1.08–4.35) |
| Secretive Eating | 1.41 (0.49–4.06) | 1.17 (0.52–2.66) | 3.95** (1.72–9.09) | 1.59 (0.40–6.38) | 0.87 (0.30–2.52) | 7.33** (2.32–23.23) | 1.69 (0.49–5.83) | 3.01* (1.19–7.60) | 4.67*** (2.00–10.91) | 0.81 (0.30–2.20) | 1.23 (0.55–2.73) | 2.70* (1.18–6.19) |
| Overweight/ Obesity | 0.73 (0.30–1.79) | 0.59 (0.27–1.30) | 4.24** (1.86–9.65) | 0.81 (0.35–1.87) | 0.71 (0.33–1.54) | 2.81** (1.27–6.18) | 0.78 (0.31–1.99) | 0.84 (0.37–1.91) | 4.53** (2.06–9.96) | 1.49 (0.62–3.60) | 0.63 (0.31–1.29) | 2.52* (1.22–5.17) |
Note.
p<.05,
p<.01,
p<.001.
Fat Talk and Parents’ Eating-Disorder Psychopathology
Parents’ fat talk about themselves was significantly correlated with their personal dietary restraint (r=0.234, p<.001), body dissatisfaction (r=.348, p<.001), and overvaluation of weight/shape (r=.366, p<.001). Parents’ obesity-fat talk and child-fat talk were not significantly associated with any of the EDE-Q scales (all p>.05).
Discussion
This study examined associations between different forms of parental fat talk (i.e., self, other, or child fat talk in front of their children), and youth disordered eating behaviors and weight status. This study found that parents reported engaging in different forms of fat talk, and that certain forms of fat talk were especially associated with problematic child eating behaviors. Importantly, our findings highlight the specific significance of child-fat talk – that is, parents’ direct fat talk about their child to their child – which appeared to be uniquely associated with child disordered eating behaviors and weight. Indeed, it was significantly associated with all child disordered eating behavior variables (binge eating, overeating, secretive eating) and child weight status (overweight/obesity).
Parents generally reported saying fat talk statements about themselves the most, and statements about their child the least. Parents’ self-fat talk was associated with their personal dietary restraint, body dissatisfaction, and overvaluation of weight/shape, but child-fat talk and obesity-fat talk were not significant associated with parents’ personal eating-disorder psychopathology. Future research should investigate whether parental fat talk is also associated with children’s own dietary restraint, body dissatisfaction, and overvaluation of weight/shape. Although child-fat talk was the least frequently reported, it presented the strongest association with child disordered eating behaviors. Previous research using the same data source found an association between child weight status and parental child-fat talk, but no significant association of child weight status with parental self-fat talk or parental fat talk about people with obesity (33). Our study expands upon this research, as it addresses child disordered eating behaviors along with child weight in the context of pre-adolescent and adolescent child age groups. Parents who reported child-fat talk were about five times more likely to report that their children engaged in binge eating, about three times more likely to report child overeating, about four times more likely to report that their child ate in secret, and about 3.5 times more likely to report that their child’s height and weight placed them in the overweight/obesity weight category. These likelihoods were even stronger for adolescent girls. Taken together, associations of eating-disorder psychopathology and disordered eating behaviors with fat talk suggest a need for prospective clinical research on the function of fat talk in parent-child relationships and the development of eating disorders (e.g., as an antecedent, consequence, or mediator of eating-disorder psychopathology). For this reason, it is also crucial to test whether intervening with parents to reduce child-fat talk ameliorates these disordered eating behaviors in a prevention or treatment framework.
Parents may not be aware of the potentially detrimental influence of parental fat talk on their children. Research on fat talk among young adult women suggests that negative weight-related conversations can be seen as normative (7, 10, 11). Clinicians working in the context of eating-disorder prevention or treatment settings may seek to observe how parents and children talk about weight, and offer parents psychoeducation and training to encourage supportive weight-related conversations and help parents promote positive health behaviors. As has been demonstrated in earlier research, parents want to promote healthy body image and eating in their children and are open to parent-training interventions that focus on being a positive role model and improving parent-child communication skills (e.g., 34).
Although the external pressures that girls and young women experience regarding fat talk and body image have been increasingly investigated (9, 10), very little research has addressed whether these pressures affect boys and young men as well. Our study found that parents of boys report more child-fat talk than parents of girls, although associations of disordered eating behaviors with child-fat talk were strongest for adolescent girls. Out of the four groups studied (pre-adolescent boys, pre-adolescent girls, adolescent boys, and adolescent girls), parents of adolescent boys reported significantly more child-fat talk than parents of pre-adolescent girls and adolescent girls, but not pre-adolescent boys. This is an important new and surprising finding, as it suggests that young boys may experience more weight stigma in their families than young girls. It is possible that parents are more aware that fat talk is potentially detrimental to their daughters than their sons, perhaps because eating disorders are more readily associated with young women than men, and parents may benefit from education about weight-related communication for both sons and daughters.
This study expands upon previous research on fat talk in several important ways, as it included both boys and girls and examined pre-adolescent and adolescent age groups. Most previous research has investigated fat talk among young adults; our study included a younger age range to explore whether these relationships emerge in pre-adolescents as well. One of the main strengths of this study is that this study aimed to focus on the child, rather than investigating parent behaviors and characteristics. The child-focus of this study enabled us to explore associations among parent-reported fat talk, eating behaviors, and weight when child characteristics varied.
In terms of limitations, this study was correlational and cross-sectional. Thus, we cannot infer any causal or temporal relationships about fat talk and disordered eating and weight. While it is clear that the two are associated, it is not known whether fat talk caused disordered eating behaviors or overweight/obesity in youth; indeed, previous research has suggested a bi-directional relationship (9). It may be the case that child-fat talk in the home leads to greater weight stigma and therefore, causes youth disordered eating behaviors. It is also possible that parents of children who engage in disordered eating behaviors or have excess weight are more likely to make derogatory comments about their child’s weight. Additionally, data were reported by parents about themselves and about their children. In psychometric studies of binge-eating assessment, parent-reported binge-eating episodes have acceptable agreement with child-reported and interview measures of binge-eating episodes (35–37). Yet, it is important to note that parents were better at knowing when binge eating was not occurring than when it was occurring (35–37). Parents also reported height and weight for themselves and their child. Earlier work has shown that discrepancies between self-reported and measured weights were unrelated to eating-disorder psychopathology (38, 39), but associations of discrepancies between parent-reported and measured child weights have not been studied. Future research could clarify these potential areas of bias. Finally, our sample was limited to parents of children between 9 and 15 years old, and participants had limited racial/ethnic diversity, with the majority well-educated and biological parents. Future research should examine whether our results generalize to the important groups of parents not well-represented in our sample.
With the study’s strengths and limitations in mind, our study has implications to guide healthcare providers in advising parents how to address weight and body image with their children. While disordered eating behaviors may not be associated with self-fat talk and fat talk about people with obesity that parents use around their children, these negative conversations may still establish a weight-stigmatizing environment in the home. Overall, parents, clinicians, and clinical-researchers should consider how parents communicate with their children (boys and girls across age groups) about weight. It is important to note that parents’ reasons for using fat talk are unknown. Parents may attempt to use fat talk to create empathy or to model self-awareness, or to motivate children to be healthy. Nonetheless, it is also important to note that the fat talk measured by the FTQ is strongly negative, using words such as “criticize,” “hate” and “disgusting.” Further research on parental fat talk may explore whether positive weight-related conversations in the home are associated with the absence of disordered eating behaviors and overweight/obesity in youth; this could guide the development of an intervention for parents about how to communicate with their children about weight, eating, and body image. Testing these parent interventions may help inform treatment and prevention efforts for pediatric obesity and eating disorders. Yet, for now, child psychologists and pediatricians should carefully consider the role of fat talk and parent-child communication about weight in their efforts to reduce disordered eating behaviors and overweight/obesity in youth.
Acknowledgments
Funding Source: This research was supported, in part, by National Institutes of Health grant K24DK070052 (Dr. Grilo)
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315:2292–9. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herpertz-Dahlmann B, Dempfle A, Konrad K, Klasen F, Ravens-Sieberer U group Bs. Eating disorder symptoms do not just disappear: the implications of adolescent eating-disordered behaviour for body weight and mental health in young adulthood. Eur Child Adolesc Psychiatry. 2015;24:675–84. doi: 10.1007/s00787-014-0610-3. [DOI] [PubMed] [Google Scholar]
- 3.Reed ZE, Micali N, Bulik CM, Davey Smith G, Wade KH. Assessing the causal role of adiposity on disordered eating in childhood, adolescence, and adulthood: a Mendelian randomization analysis. Am J Clin Nutr. 2017;106:764–72. doi: 10.3945/ajcn.117.154104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arroyo A, Segrin C. Family interactions and disordered eating atittudes: The mediating roles of social competence and psychological distress. Commun Mongr. 2013;80:399–424. [Google Scholar]
- 5.Cooley E, Toray T, Wang MC, Valdez NN. Maternal effects on daughters' eating pathology and body image. Eat Behav. 2008;9:52–61. doi: 10.1016/j.eatbeh.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Mazzeo SE, Kelly NR, Stern M, Gow RW, Serdar K, Evans RK, et al. Nourishing Our Understanding of Role Modeling to Improve Support and Health (NOURISH): design and methods. Contemp Clin Trials. 2012;33:515–22. doi: 10.1016/j.cct.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nichter M, Vuckovic N. Fat talk: Body image among adolescent girls. Many Mirrors: Body Image and Social Relations. 1994:109–31. [Google Scholar]
- 8.Ousley L, Cordero ED, White S. Fat talk among college students: how undergraduates communicate regarding food and body weight, shape & appearance. Eat Disord. 2008;16:73–84. doi: 10.1080/10640260701773546. [DOI] [PubMed] [Google Scholar]
- 9.Mills J, Fuller-Tyszkiewicz M. Fat talk and its relationship with body image disturbance. Body Image. 2016;18:61–4. doi: 10.1016/j.bodyim.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 10.Sharpe H, Naumann U, Treasure J, Schmidt U. Is fat talking a causal risk factor for body dissatisfaction? A systematic review and meta-analysis. Int J Eat Disord. 2013;46:643–52. doi: 10.1002/eat.22151. [DOI] [PubMed] [Google Scholar]
- 11.Salk RH, Engeln-Maddox R. “If you’re fat, then I’m humongous!” Frequency, content, and impact of fat talk among college women. Psychol Women Q. 2011;35:18–28. [Google Scholar]
- 12.Shannon A, Mills JS. Correlates, causes, and consequences of fat talk: A review. Body Image. 2015;15:158–72. doi: 10.1016/j.bodyim.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Arroyo A, Segrin C, Andersen KK. Intergenerational transmission of disordered eating: Direct and indirect maternal communication among grandmothers, mothers, and daughters. Body Image. 2017;20:107–15. doi: 10.1016/j.bodyim.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Haines J, Neumark-Sztainer D, Eisenberg ME, Hannan PJ. Weight teasing and disordered eating behaviors in adolescents: longitudinal findings from Project EAT (Eating Among Teens) Pediatrics. 2006;117:e209–15. doi: 10.1542/peds.2005-1242. [DOI] [PubMed] [Google Scholar]
- 15.Madowitz J, Knatz S, Maginot T, Crow SJ, Boutelle KN. Teasing, depression and unhealthy weight control behaviour in obese children. Pediatric obesity. 2012;7:446–52. doi: 10.1111/j.2047-6310.2012.00078.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cruwys T, Leverington CT, Sheldon AM. An experimental investigation of the consequences and social functions of fat talk in friendship groups. Int J Eat Disord. 2016;49:84–91. doi: 10.1002/eat.22446. [DOI] [PubMed] [Google Scholar]
- 17.Bauer KW, Bucchianeri MM, Neumark-Sztainer D. Mother-reported parental weight talk and adolescent girls' emotional health, weight control attempts, and disordered eating behaviors. J Eat Disord. 2013;1:45. doi: 10.1186/2050-2974-1-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abraczinskas M, Fisak B, Jr, Barnes RD. The relation between parental influence, body image, and eating behaviors in a nonclinical female sample. Body Image. 2012;9:93–100. doi: 10.1016/j.bodyim.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 19.Phares V, Steinberg AR, Thompson JK. Gender differences in peer and parental influences: Body image disturbance, self-worth, and psychological functioning in preadolescent children. J Youth Adolescence. 2004;33:421–9. [Google Scholar]
- 20.Arroyo A, Andersen KK. Appearance-related communication and body image outcomes: Fat talk and old talk among mothers and daughters. J of Fam Commun. 2016;16:95–110. [Google Scholar]
- 21.Neumark-Sztainer D, Bauer KW, Friend S, Hannan PJ, Story M, Berge JM. Family weight talk and dieting: How much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? J Adolesc Health. 2010;47:270–6. doi: 10.1016/j.jadohealth.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loth KA, Neumark-Sztainer D, Croll JK. Informing family approaches to eating disorder prevention: perspectives of those who have been there. Int J Eat Disord. 2009;42:146–52. doi: 10.1002/eat.20586. [DOI] [PubMed] [Google Scholar]
- 23.Behrend TS, Sharek DJ, Meade AW, Wiebe EN. The viability of crowdsourcing for survey research. Behav Res Methods. 2011;43:800–13. doi: 10.3758/s13428-011-0081-0. [DOI] [PubMed] [Google Scholar]
- 24.Buhrmester M, Kwang T, Gosling SD. Amazon's Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspect Psychol Sci. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- 25.Hauser DJ, Schwarz N. Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behav Res Methods. 2016;48:400–7. doi: 10.3758/s13428-015-0578-z. [DOI] [PubMed] [Google Scholar]
- 26.Chandler J, Shapiro D. Conducting Clinical Research Using Crowdsourced Convenience Samples. Annu Rev Clin Psychol. 2016;12:53–81. doi: 10.1146/annurev-clinpsy-021815-093623. [DOI] [PubMed] [Google Scholar]
- 27.Powell EM, Frankel LA, Umemura T, Hazen N. The relationship between adult attachment orientation and child self-regulation in eating: The mediating role of persuasive-controlling feeding practices. Eat Behav. 2017;26:121–8. doi: 10.1016/j.eatbeh.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 28.Puhl RM, Himmelstein MS, Quinn DM. Internalizing Weight Stigma: Prevalence and Sociodemographic Considerations in US Adults. Obesity. 2017 doi: 10.1002/oby.22029. [DOI] [PubMed] [Google Scholar]
- 29.Royal S, MacDonald DE, Dionne MM. Development and validation of the Fat Talk Questionnaire. Body Image. 2013;10:62–9. doi: 10.1016/j.bodyim.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 30.Fairburn CG, Beglin S. Assessment of eating disorders: Interview or self-report questionnaire? Int J Eat Disord. 1994;16:363–70. [PubMed] [Google Scholar]
- 31.Grilo CM, Reas DL, Hopwood CJ, Crosby RD. Factor structure and construct validity of the Eating Disorder Examination-Questionnaire in college students: Further support for a modified brief version. Int J Eat Disord. 2015;48:284–9. doi: 10.1002/eat.22358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grilo CM, Crosby RD, Peterson CB, Masheb RM, White MA, Crow SJ, et al. Factor structure of the eating disorder examination interview in patients with binge-eating disorder. Obesity. 2010;18:977–81. doi: 10.1038/oby.2009.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lydecker JA, Grilo CM. The apple of their eye: Attitudinal and behavioral correlates of parents' perceptions of child obesity. Obesity. 2016;24:1124–31. doi: 10.1002/oby.21439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Runfola CD, Zucker NL, Von Holle A, Mazzeo S, Hodges EA, Perrin EM, et al. NURTURE: development and pilot testing of a novel parenting intervention for mothers with histories of an eating disorder. Int J Eat Disord. 2014;47:1–12. doi: 10.1002/eat.22178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Elliott CA, Tanofsky-Kraff M, Mirza NM. Parent report of binge eating in Hispanic, African American and Caucasian youth. Eat Behav. 2013;14(1):1–6. doi: 10.1016/j.eatbeh.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tanofsky-Kraff M, Yanovski SZ, Yanovski JA. Comparison of child interview and parent reports of children's eating disordered behaviors. Eat Behav. 2005;6:95–9. doi: 10.1016/j.eatbeh.2004.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johnson WG, Grieve FG, Adams CD, Sandy J. Measuring binge eating in adolescents: Adolescent and parent versions of the questionnaire of eating and weight patterns. Int J Eat Disord. 1999;26:301–14. doi: 10.1002/(sici)1098-108x(199911)26:3<301::aid-eat8>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 38.White MA, Masheb RM, Grilo CM. Accuracy of self-reported weight and height in binge eating disorder: Misreport is not related to psychological factors. Obesity. 2010;18(6):1266–9. doi: 10.1038/oby.2009.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gay J, Monsma EV, Torres-McGehee T. Give or take a few? Comparing measured and self-reported height and weight as correlates of social physique anxiety. Res Q Exerc Sport. 2009;80(3):656–62. doi: 10.1080/02701367.2009.10599605. [DOI] [PubMed] [Google Scholar]