Abstract
Short bowel syndrome is a major cause of morbidity and mortality in children. Despite decades of experience in the management of short bowel syndrome, current therapy is primarily supportive. Definitive treatment often requires intestinal transplantation, which is associated with significant morbidity and mortality. In order to develop novel approaches to the treatment of short bowel syndrome, we and others have focused on the development of an artificial intestine, by placing intestinal stem cells on a bioscaffold that has an absorptive surface resembling native intestine, and taking advantage of neovascularization to develop a blood supply. This review will explore recent advances in biomaterials, vascularization, and progress towards development of a functional epithelium and mesenchymal niche, highlighting both success and ongoing challenges in the field.
Introduction
The clinical problem of short bowel syndrome
Short bowel syndrome (SBS) refers to the condition in which limited intestinal mucosa cannot meet the nutritional needs of the patient via enteral absorption (1,2). The diagnosis of SBS relies on an assessment of the loss of intestinal length (1–3), in combination with poor enteral absorption (4), dependence on total parenteral nutrition (TPN) (5–7), or some combination of these factors. (1,2,8). The epidemiology of SBS remains difficult to define due to variation in diagnostic criteria, study population (pediatric versus adult), and the length of the follow-up period among studies. In one of the largest population-based studies of SBS (3), the overall incidence was found to be 0.02% of all live births, and 2.2% of neonatal intensive care unit (NICU) admissions. Notably, the incidence among premature infants (<37 weeks gestational age) was 100× higher than among infants >37 weeks. Further, there is an increased incidence associated with low birth weight (0.7 in very low birth weight, and 1.1% in extremely low birth weight) babies (1).
Causes of short bowel syndrome and the need for innovative therapies
Among the pediatric population, leading causes of SBS include necrotizing enterocolitis (NEC), intestinal atresia, gastroschisis, and malrotation with volvulus (2,7,9,10), with NEC representing about 96% of cases in the low birth weight NICU population (1). Complications of SBS are many, and include cholestasis resulting in liver failure, bowel dilation resulting in bacterial overgrowth, and sepsis with its related complications, which may arise both from central-line associated bacterial infection [CLABSI] and bacterial overgrowth. (2,5,7,10–12). The overall mortality of SBS is estimated at 27.5% to 37.5% over a follow up period of 2–5 years (1,2,7,8,13), with leading causes of death being hepatic failure and sepsis (2,7,9,11,13). Given that the inability to achieve enteral autonomy is one of the leading predictors of mortality (2,7,9), current therapy for SBS aims to restore enteral autonomy. Present treatment options focus on either increasing absorption (via adaptation and intestinal reversal procedures) or restoring intestinal length (via intestinal lengthening procedures and transplant.). Despite decades of experience with TPN supplementation and optimization of surgical techniques and transplantation, half of all patients with SBS will never attain enteral autonomy. The annual mortality in SBS is 15–30% (3,8,12.) Given the limited success and high morbidity of current therapy, novel treatment approaches are clearly needed. As will be reviewed in the following sections, the development of an artificial intestine derived from the patient’s own intestinal stem cells and incorporated into a novel bioscaffold that recruits an endogenous blood supply may represent an attractive option for the treatment of children with SBS.
Strategies for the development of an artificial intestine
The goals of developing an artificial intestine include the provision of appropriate absorptive epithelium, barrier and immune functions, and motility. In addition, the artificial intestine would be autologous in order to achieve enteral independence without the need for immunosuppressive drugs. In support of the success of this approach, the modern era of tissue engineering began in 1988 with Joseph Vacanti and Robert Langer demonstrating growth of pancreatic and intestinal tissue on a bioabsorbable scaffold implanted into the omentum of rats (14). Since this early finding, there has been a large body of research focused on the development of a tissue engineered intestine. The basic requirements for an engineered intestine include a source of stem cells with the capacity to grow and differentiate into a mature and absorptive mucosal surface (Figure 1), a bioscaffold capable of supporting cellular growth (Figure 2–4), a niche for engraftment and growth of the tissue, and vascularization of the new tissue. Additional challenges include meeting the large surface area needed for enteral autonomy and optimization of gastrointestinal motility. Each of these challenges will be discussed with a focus on successes and opportunities which lie ahead.
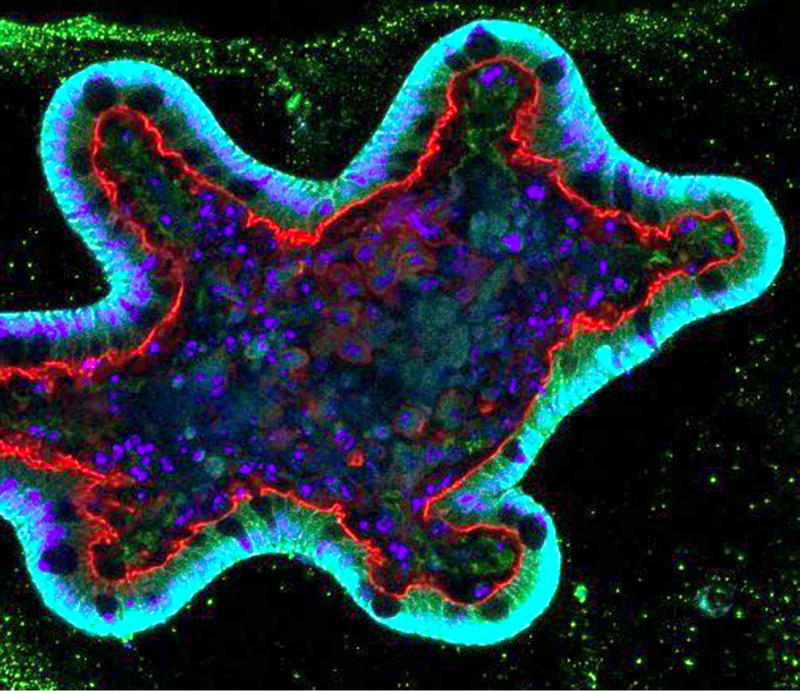
Figure 1.
Confocal micrograph revealing the growth of a mini-gut (enteroid) in culture as a precursor to the development of an artificial intestine. Green - ki67, cyan – e-cadherin, red – phalloidin, blue – DAPI.
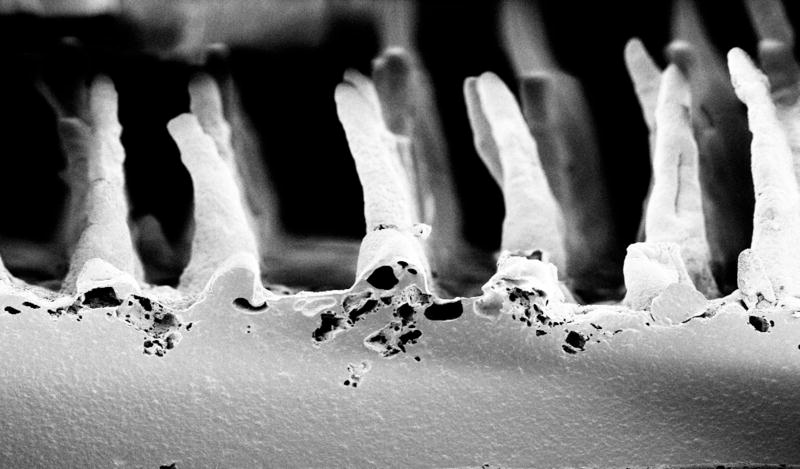
Figure 2.
Scanning electron micrograph showing a synthetic (Poly(glycerol) sebacate (PGS) scaffold with an architecture that mimics the native intestinal crypt-villus architecture in cross section.
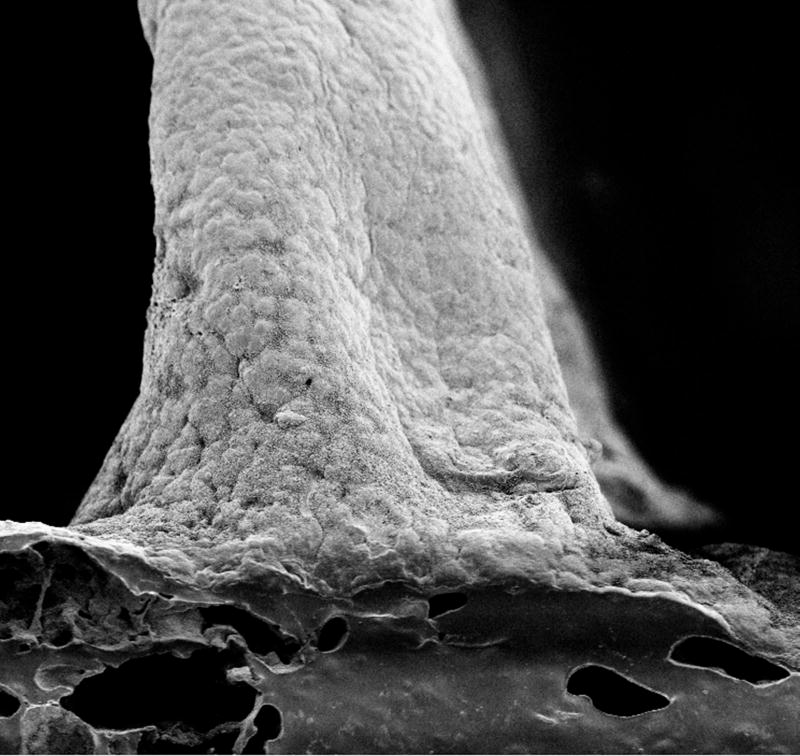
Figure 4.
Scanning electron micrograph showing the intestinal stem cells covering a synthetic villous at the villus base.
a. PGS scaffold supports growth of intestinal epithelium
Biomaterials for the development of an artificial intestine
The production of an effective and biocompatible scaffold on which cells can grow and be transplanted as a graft is a critical step in the development of artificial intestine. A successful bioscaffold will require the following features: a material capable of supporting stem cell attachment, proliferation, and differentiation; support of angiogenesis and vascular ingrowth; approximation of mechanical and electrical properties of the intestine so as to facilitate operative insertion, and incorporation without an excessive acute inflammatory or chronic immune response. Available scaffolds fall into one of three categories: decellularized organs, biological materials, and synthetic polymers.
i. decellularized tissue
Decellularized scaffolds have been used for a variety of tissue engineering applications (15–20), and decelullarized intestine has garnered attention as a potential scaffold for engineered intestine(21–23). Totonelli et al. demonstrated the adherence of intestinal epithelial cells, preservation of extracellular components, and angiogenic properties of a seeded decellularized intestinal scaffold. Nowocin et al. demonstrated the ability to implant seeded decellularized pig intestine scaffolds into rats without evidence of an inflammatory response. Other decellularized tissues such as acellular dermal matrix (ADM) and small intestinal submucosa have also been demonstrated to support intestinal mucosal ingrowth when anastomosed with native intestine (24–26). With all decellularized scaffolds, tissue source is a consideration. Additionally, some recent evidence (27) suggests that human embryonic stem cells (hESCs) do not grow on decellularized porcine tissue, and human intestinal organoids (HIOs) lose their intestinal phenotype on decellularized porcine tissue in vivo.
ii. biologically based scaffolds
Biologically-based scaffolds are typically created from components of tissue, such as collagen, or other naturally occurring materials like silk or chitosan hydrogel (28–33). Small intestinal submucosal components and collagen carry the advantage of maintaining some components of the naturally occurring extracellular matrix, but allow more customization of the design of the final construct. Chitosan has been used with favorable biocompatibility, degradation, and abundant reactive groups useful for pharmaceuticals. Recent publications have reported successful creation of polarized epithelium and supportive mesenchyme in an in vitro model with silk scaffolds (29). Potential advantages of silk include low immunogenicity and the ability to tune its degradation and mechanical properties.
iii. synthetic scaffolds
The most widely-reported class of scaffold in the current literature is synthetic scaffolds. Specifically, polyglycolic acid (PGA), polylactic acid (PLA), poly-ε-caprolactone (PCL), polylactic-co-glycolic acid (PLGA), and other combinations are frequently used, often coated with a second polymer or matrix protein such as collagen, fibronectin, or matrigel (34–43) (Figure 2–4). The primary advantage of synthetic polymers is the ability to synthesize nearly unlimited quantities and tune mechanical, structural, and degradation properties based upon rational polymer design. Disadvantages include the potential for chronic inflammation and complement activation, which is seen particularly in the polyesters. Recently, in collaboration with the March lab, we have created novel intestinal scaffolds using synthetic PLGA that mimics the microarchitecture of the intestinal villus, and demonstrated effective growth of enteroids and macrophages, as well as recreation of the crypt-villus architecture (43). We further demonstrated that these scaffolds were capable of regenerating the anorectal mucosa following mucosectomy in dogs. Additionally, PLGA has been shown to support growth of human enteroids, with successful transplantation into immunocompromised murine hosts (43–45). Recently, we have begun investigating the use of poly(glylcerol sebacate) (PGS) synthetic scaffolds, which have been shown to support the growth of murine and porcine intestinal epithelium. (Figure 1)
Vascularization of the implanted scaffold
Vascularization is a critical step in the production of an artificial intestine. Implantation of artificial intestine into a recipient relies on cellular nourishment via diffusion until a vascular supply is achieved. In a series of experiments with autotransplantation of intestinal organoid units, (34,38,40,46), Vacanti’s group reported successful vascularization of artificial intestine with production of neomucosa on PLGA scaffolds in P7 rat omentum after 3 weeks. We have corroborated these findings in our studies in dogs (43). Sites of engraftment in which vascularization can be successfully achieved include the omentum (34–37,43) or renal capsule (27,29,47). However, vascularization sufficient for surgical anastomosis of an isolated segment of artificial intestine in either the omentum or renal capsule remains a challenge. Gardner-Thorpe (34) et al. investigated angiogenesis in a rat model of omental vascularization and determined that while the mucosa and submucosa of artificial intestine increased in size, vascularity was limited to capillary growth without evidence of formation of the larger vessels present in native intestine. Further, they found that various growth factors, including vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) were higher in native compared to artificial intestine. In a subsequent study (48), Rocha et al. found that PGA scaffolds seeded with VEGF microspheres and implanted into the omentum of rats resulted in higher VEGF levels, increased proliferation, and increased capillary density compared to empty constructs. Similarly, Minardi et al. (49) found improved vascularization and epithelial growth of tissue when scaffolds incorporated with slow-release platelet-derived growth factor were used. Another approach to vascularizing tissue engineered constructs is pre-vascularization. Pre-vascularization has demonstrated some success in cardiac and other muscular tissue engineering, but in spite of more robust capillary network formation, such tissues still lack adequate vascular architecture for surgical anastomoses with the native circulatory system. Thus, these systems rely instead on vascular budding and ingrowth to survive, which is explained in part from our finding that endothelial stem cells are recruited to the site of graft implantation (43). Ju, et al., recently published a method of prevascularization using scaffolds pre-seeded with autologous endothelial cells and smooth muscle. Using this technique, they demonstrated fully cellularized vascular constructs capable of contractility. Their grafts demonstrated high degree of patency and structural integrity and minimal immune reaction in host tissue (50). Future directions may thus employ artificial intestinal constructs in which autologous endothelial stem cells are pre-woven into the graft (50,51).
Achieving an intact epithelial lining within the artificial intestine
The most important goal in the development of an artificial intestine is restoration of enteral autonomy. In order to achieve this, a functional mucosa capable of absorption must be developed. A large body of work has been performed showing that intestinal crypt stem cells can differentiate into the four types of differentiated intestinal mucosa: goblet cells, enteroendocrine cells, paneth cells, and columnar mucosal cells (52,53). Perhaps the largest advance occurred through work of Hans Clever et al., who first identified a reliable intestinal epithelial stem cell marker, LGR5, and demonstrated that crypt-villus units can be generated from a single LGR5+ stem cell (54,55). We now understand that LGR5 is a co-receptor for the canonical Wnt pathway, which is activated through binding of R-spondin proteins (56–60). Many investigators, including our group (35,36,43,45,61–63), have reported successful generation of intestinal tissue using an intestinal source of stem cells (Figure 2). While Clever et al. demonstrated that crypt-villus units can be generated from a single LGR5+ stem cell (enteroids), many methods of intestinal generation involve the isolation of multicellular units derived from the intestinal crypt, termed organoids, using the method of Evans et al. (64), rather than individual stem cells (Figure 1). The primary distinction between enteroids and organoids is the inclusion of mesenchymal cellular components in organoids, whereas enteroids consist of primarily intestinal epithelial cells.
Mesenchymal components required for generation of an artificial crypt-villus axis
The mesenchymal elements of the intestine have been found to play a critical role in creation and maintenance of the epithelial niche. This niche is maintained by intestinal subepithelial mesenchymal cells (ISEMCs), whose functions include the maintenance of the basement membrane and regulation of epithelial cell function via signaling pathways involving VEGF, Wnt, R-spondin, and stem cell factor. Multiple studies have suggested that the presence of myofibroblasts, macrophages, and smooth muscle cells enhance the growth and differentiation of artificial intestinal epithelium (56,57,67–69). Various authors have addressed the issue of mesenchymal support by utilizing native mesenchyme. In a series of papers from 1999–2000, Vacanti’s group reported production of neomucosa with autotransplantation of intestinal organoid units on PLGA scaffolds in P7 rat omentum after 3 weeks (38,40,46). In additional studies, Grikscheit et al. have demonstrated neomucosa in rat pups with good crypt-villus architecture, collagen-rich submucosa and basement membrane, actin-positive muscle fibers in the muscularis propria, and microarchitecture including microvilli (34,39). Multiple experiments by Vacanti’s group suggested that, following a period of growth in the omentum, anastomosis with native intestine enhanced growth of artificial intestine. When compared to artificial intestine that remained in the omentum without anastomosis, the anastomosed artificial intestine demonstrated superior villus height, crypt depth, and proliferation (38,46,70). It is unclear the degree to which this improved growth is attributable to lateral ingrowth of native intestinal mucosal and mesenchymal components versus restoration of the mesenchymal niche resulting in improved growth of transplanted cells. Other groups have recreated the mesenchymal niche by adding back specific growth factors, such as Wnt, Noggin, R-spondin, and epidermal growth factor (EGF) and demonstrated the ability to grow and expand enteroids in vitro for extended periods of time (55,71–73). Our group has focused on a combinatorial approach to establish the intestinal niche in epithelial cell culture utilizing a combination of Wnt, Noggin, R-spondin, EGF, macrophages, myofibroblasts, and commensal bacterial cultures resulting in a more robust epithelialization and vascularization of artificial intestine grafts (43).
Enteric Nervous System and Motility
In order for an artificial intestine to function as an autonomous, nutrient absorbing apparatus, it must attain some degree of innate peristaltic activity. To achieve this, various labs have focused on the ability to develop a functional enteric nervous system (ENS) (69,74–76). Pachnis’ group identified (RET+) cells serving as multipotent progenitors capable of inducing colonization of aganglionic bowel with neurons and glia (77), and Schafer et al. published a technique for isolation of neurospheres from the ENS (78). When isolated and transplanted into aganglionic mice, these neurospheres differentiated into neurons and glia with evidence of synapse formation which were capable of contraction (79,80). In artificial intestine, multiple groups have demonstrated evidence of neuronal components after patch graft with collagen-based (33,67) or PLGA-based constructs (37).
More recently, neuronal components have been successfully harvested from humans (74, 76, 81.) Wieck et al demonstrated successful engraftment of human and murine neurospheres into tissue engineered colonic tissue with successful differentiation of neuronal and glial components (74). These findings suggest that co-culture of organoids with neurospheres may re-create functional neuronal networks and achieve intestinal motility as recently described by Workman et al. (82).
Putting it all together: manufacturing an artificial intestine
Several laboratories have integrated many of the above findings in order to manufacture an artificial intestine which appears to histologically resemble the native intestine. Grickscheit’s group has shown that intestinal-derived organoid units can produce a histologically normal appearing epithelium, mesenchymal components, and neuronal components in models using omental implantation (44,45). Sala et al. reported one of the first large animal models with successful production of artificial intestine from autologous intestinal cells (37). In this model, autologous jejunal cells from 6 week old Yorkshire swine were seeded onto PLGA scaffolds and vascularized in the omentum. At 7 weeks, they were found to have crypt-villus architecture similar to native intestine. They also identified enterocytes, goblet cells, and enteroendocrine cells. They found ganglion cells between longitudinal and circular muscle layers and in the submucosa. One potential limitation to the organoid unit is its requirement for derivation from full-thickness intestine, raising the question as to whether a partial thickness biopsy could re-create all layers of the intestine or whether mesenchymal and neuronal components would need to be added back individually. Additionally, it is unclear whether the neuronal component is preserved after multiple expansions (72) and cryopreservation (44). Given these challenges, several groups have turned to a second potential source for intestinal tissue, namely HIOs, which may be generated from hESCs or induced pluripotent stem cells (iPSCs). Multiple groups have described a system in which hESCs and iPSCs can be differentiated into three-dimensional intestinal tissue with epithelium and mesenchyme (27,83–86).
Recent publications (27,84) have implanted HIOs into the mouse kidney capsule and demonstrated evidence of epithelial and mesenchymal tissue formation in vivo. After implantation for 6 weeks, these HIOs produced crypt-villus architecture with central capillary networks, demonstrated the presence of all epithelial cell types in addition to multiple mesenchymal cell types, specifically ISEMFs, fibroblasts, and smooth muscle cells (84). Notably, when using HIOs alone, Finkbeiner et al. found an absence of S100b+ and NeuN+ cells. They were able to reproduce these cells by adding organoid units (27). This suggests that current methods of HIO differentiation may not be able to reproduce functional neuronal networks and may require the addition of organoid units or neurospheres. Workman et al. (2016) recently published methods to combine HIOs and iPSC-derived neural crest cells (NCCs) with the achievement of a functional enteric nervous system in mice (82).
Determining the functional capacity of artificial intestine
While multiple studies have demonstrated the ability to form artificial intestine that histologically resembles native intestine, the question remains, does it work? Several studies have evaluated the functionality of artificial intestine constructs. Specifically, in one study, rats underwent a colectomy with end ileostomy with the addition of an implantation of artificial intestine via an anastomosis in a side-to-side fashion proximal to the end ileostomy. The rats that received artificial constructs showed attenuated weight loss, slowed stool transit times, and increase in serum bile acids compared to controls (39). Another study reported that engineered intestine implantation resulted in improved recovery after massive small bowel resection with implanted rats regaining more of their preoperative weight (98%) than controls (76%). In addition, rats receiving engineered constructs had increased stool transit times (35). Avansino et al. also demonstrated improvement of bile acid malabsorption using ileal stem cell transplantation onto jejunal scaffolds after mucosectomy (87). Follow-up studies by Dr. Grikscheit’s lab showed engineered intestine could be developed using human tissue as an organoid source when seeded onto PLGA scaffolds and implanted into the omenta of irradiated NOD/SCID mice. At four weeks, tissue evaluation revealed the presence of all four small intestinal epithelial cell types. Additionally, they noted presence of fibroblasts and neuromuscular elements. Immunostaining for the human istotype of β2 microglobulin confirmed that these identified components were from the human cell source (45). In a subsequent study, using human organoid units, Grant et al. demonstrated the presence of sodium chloride secretory transporters in the basolateral membrane of the intestinal epithelium, as well as sodium glucose transport proteins (SGLT-1), suggesting that absorption theoretically could occur (62). Watson et al. (84) recently demonstrated successful engraftment of collagen-embedded HIOs into the kidney capsule of SCID mice. At six weeks, they demonstrated all intestinal cell lineages with normal architecture, proliferation, and differentiation along the crypt-villus axis. They further noted the presence of lamina propria, muscularis mucosa, submucosa, and smooth muscle layers after engraftment. They observed the presence of brush border enzymes such as alkaline phosphatase, lactase, glucose transporter 2 (GLUT2), and sucrose-isomaltase. Recent work by Workman et al. (82) presented novel methods of differentiating NCCs from human iPSCs. They presented an experimental model combining HIOs and neural crest cells derived from iPSC-neural crest cells (iPSC-NCCs) into spheroid aggregates, which were cultured under three-dimensional growth conditions for 28 days and then engrafted into mice for 6–10 weeks. Using this method, they produced not only mature vascularized intestinal tissue with submucosal and myenteric layers of smooth muscle fibers, but also found evidence of organized neuronal ganglia located in close proximity to the submucosal and myenteric layers of smooth muscle. Functional tests of this tissue in vitro revealed coordinated calcium efflux in the ENS cells in response to potassium chloride and organized, ENS-dependent contractile waves in response to electrical stimulus. While investigation is ongoing into the ability to create a fully mature and functional enteric neuromuscular system, this study shows promise for the future development of a fully-functional artificial intestine.
Strategies towards clinical usage of the artificial intestine
With multiple successes in functional animal models, the field has begun to turn an eye towards clinical applicability. The ultimate goal in human treatment would be to obtain a human source of tissue, either full thickness intestine at the time of initial NEC resection or in a second surgery, biopsied intestinal tissue at a later date, or from iPSCs. To limit the amount of starting material required, several labs have described reliable methods for expansion of intestinal epithelial cells in culture (88). This would allow repopulation of an entire graft with a small amount of starting tissue. Besner and colleagues recently reported successful artificial intestine production using expanded enteroids from murine intestinal biopsies, confirming that small amounts of starting material can be used to generate enough cells for an entire graft (72). In a further bridge to clinical applicability, Spurrier et al. (44) have reported methods of successfully cryopreserving organoid units, suggesting that intestinal organoid units could be harvested and preserved until needed. It is unclear whether the neuronal component was preserved in these experiments. Recent work by Dr. Helmrath’s group (82) holds promise for the potential to add in the neural component prior to implantation.
As noted above, an absorptive epithelium requires the development of an intact blood supply in order to transport nutrients from the gut lumen to the blood stream. This may be achieved in part through either recruitment of endogenous endothelial stem cells (48,89,90) or the use of a combination of pre-vascularization and prefabricated constructs with the artery/arteriole/capillary vascular hierarchical structure already present (50,51,91). For development of motility, barriers to overcome include the development of an independently functioning neuromuscular plexus, for which iPSC-NCCs hold promise (82). An alternative approach might be the use of battery powered implantable pumps to re-create peristaltic movement. Finally, while recent successes with human tissue in small animal models have been promising, large animal models are still needed. While various investigators, including our own group, have utilized swine and dogs, such studies are expensive, time intensive, and more prone to the development of significant inflammation after transplantation compared to rodent studies. Ongoing large animal trials are necessary to confirm the applicability of previous work in a model more similar to the human child and to ultimately gain Food and Drug Administration (FDA) approval for use.
Design of clinical trials using the artificial intestine
Once successful products are proven in animals, human trials will still face significant challenges. The FDA regulatory process will require that all fabrication and manufacturing processes are safe. It will also be important to define which population may be expected to benefit most from implantation of an artificial intestine. Initial studies should focus on those in whom medical management has failed and in whom intestinal transplantation is not an option, for instance due to an anatomic or genetic barrier. In the ideal workflow setting, autologous stem cells would be obtained as described above, expanded in vitro on an appropriate scaffold, re-implanted into the host, and then connected to the native gut to allow for enteric absorption. Following the exciting work in human usage of vascular (92) and bladder (93) grafts, it is reasonable to have optimism that such success may also one day be seen for the artificial intestine.
Conclusions
Based upon studies performed over the past several decades, that which was once thought to be science fiction i.e. the generation of a functional artificial intestine – may finally be be inching closer to reality. With recent advances in our ability to isolate, grow, and differentiate intestinal stem cells from the host, an increased understanding of the intestinal niche required to maintain the artificial intestinal mucosa, and novel techniques for the generation of an intact blood supply, it appears that the major elements for a functional absorptive intestine are achievable. With ongoing investigation into machine driven motility and endogenous neural elements, there is additional optimism that peristalsis may also be achieved. Taken together, through the work of many labs around the world, it is reasonable to believe that an artificial intestine may one day be developed for children with SBS, thus alleviating suffering and providing hope to these fragile patients.
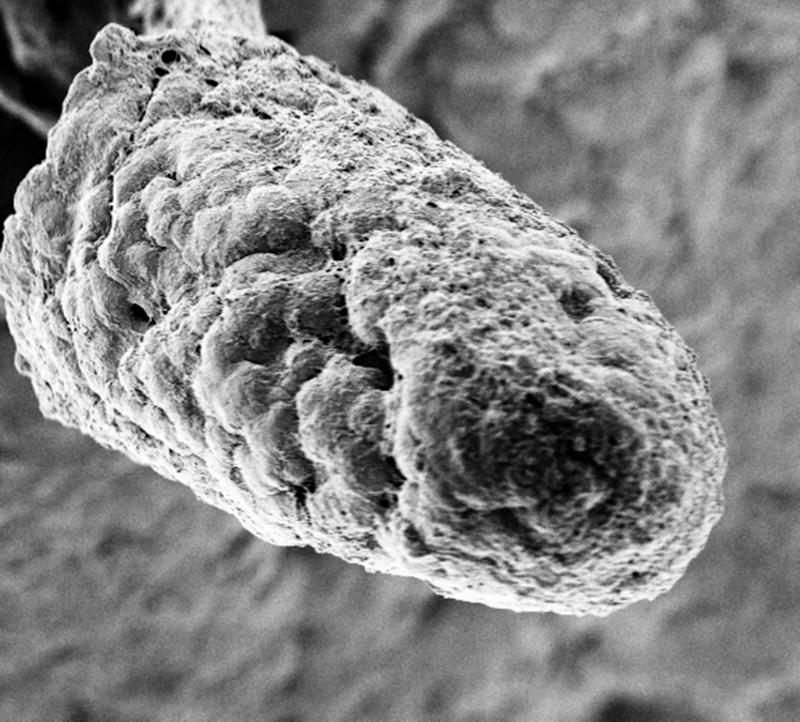
Figure 3.
Scanning electron micrograph showing attached cells on a synthetic villus prior to implantation into the host omentum.
Acknowledgments
Statement of financial support: DJH is supported by R01GM078238 and R01DK083752 from the National Institutes of Health. LYM and MRL are supported by T32—from the national institues of health.
Footnotes
Disclosure statement: there are no conflicts of interest with respect to the current work.
References
- 1.Cole CR, Hansen NI, Higgins RD, Ziegler TR, Stoll BJ. Very Low Birth Weight Preterm Infants With Surgical Short Bowel Syndrome: Incidence, Morbidity and Mortality, and Growth Outcomes at 18 to 22 Months. Pediatrics [Internet] 2008;122:e573–82. doi: 10.1542/peds.2007-3449. Available from: http://pediatrics.aappublications.org/cgi/doi/10.1542/peds.2007-3449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spencer AU, Neaga A, West B, Safran J. Pediatric Short Bowel Syndrome. 2005;242:403–12. doi: 10.1097/01.sla.0000179647.24046.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wales PW, De Silva N, Kim J, Lecce L, To T, Moore A. Neonatal Short Bowel Syndrome: Population-Based Estimates of Incidence and Mortality Rates. J Pediatr Surg. 2004;39:690–5. doi: 10.1016/j.jpedsurg.2004.01.036. [DOI] [PubMed] [Google Scholar]
- 4.Fitzgibbons S, Ching YA, Valim C, et al. Relationship between serum citrulline levels and progression to parenteral nutrition independence in children with short bowel syndrome. J Pediatr Surg. 2009;44:928–32. doi: 10.1016/j.jpedsurg.2009.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andorsky DJ, Lund DP, Lillehei CW, et al. Nutritional and other postoperative management of neonates with short bowel syndrome correlates with clinical outcomes. J Pediatr. 2001;139:27–33. doi: 10.1067/mpd.2001.114481. [DOI] [PubMed] [Google Scholar]
- 6.Duro D, Kalish LA, Johnston P, et al. Risk factors for intestinal failure in infants with necrotizing enterocolitis: A glaser pediatric research network study. J Pediatr [Internet] 2010;157:203–208.e1. doi: 10.1016/j.jpeds.2010.02.023. Available from: http://www.scopus.com/inward/record.url?eid=2-s2.0-77955298545&partnerID=40&md5=9cd14788cf482d6e019e35760c98026b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nucci A, Cartland Burns R, Armah T, et al. Interdisciplinary management of pediatric intestinal failure: A 10-year review of rehabilitation and transplantation. J Gastrointest Surg. 2008;12:429–36. doi: 10.1007/s11605-007-0444-0. [DOI] [PubMed] [Google Scholar]
- 8.Diamond IR, de Silva N, Pencharz PB, Kim JH, Wales PW. Neonatal short bowel syndrome outcomes after the establishment of the first Canadian multidisciplinary intestinal rehabilitation program: preliminary experience. J Pediatr Surg. 2007;42:806–11. doi: 10.1016/j.jpedsurg.2006.12.033. [DOI] [PubMed] [Google Scholar]
- 9.Modi BP, Langer M, Ching YA, et al. Improved survival in a multidisciplinary short bowel syndrome program. J Pediatr Surg. 2008;43:20–4. doi: 10.1016/j.jpedsurg.2007.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fitzgibbons SC, Ching Y, Yu D, et al. Mortality of necrotizing enterocolitis expressed by birth weight categories. J Pediatr Surg. 2009;44:1072–6. doi: 10.1016/j.jpedsurg.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Yang CJ, Lee M, Valim C, et al. HHS Public Access. 2015;44:1084–8. [Google Scholar]
- 12.Squires RH, Duggan C, Teitelbaum DH, et al. Natural history of pediatric intestinal failure: Initial report from the pediatric intestinal failure consortium. J Pediatr. 2012:161. doi: 10.1016/j.jpeds.2012.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wales PW, Christison-Lagay ER. Short bowel syndrome: epidemiology and etiology. Semin Pediatr Surg. 2010;19:3–9. doi: 10.1053/j.sempedsurg.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Vacanti JP, Morse MA, Saltzman WM, Domb AJ, Perez-Atayde A, Langer R. Selective cell transplantation using bioabsorbable artificial polymers as matrices. J Pediatr Surg. 1988;23:3–9. doi: 10.1016/s0022-3468(88)80529-3. [DOI] [PubMed] [Google Scholar]
- 15.Verstegen M, Willemse J, van den Hoek S, et al. Decellularization of whole human liver grafts using controlled perfusion for transplantable organ bioscaffolds. Stem Cells Dev [Internet] 2017 doi: 10.1089/scd.2017.0095. scd.2017.0095. Available from: http://online.liebertpub.com/doi/10.1089/scd.2017.0095. [DOI] [PubMed]
- 16.Campo H, Baptista PM, López-Pérez N, Faus A, Cervelló I, Simón C. De- and recellularization of the pig uterus: a bioengineering pilot study. Biol Reprod [Internet] 2017;96:34–45. doi: 10.1095/biolreprod.116.143396. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28395322. [DOI] [PubMed] [Google Scholar]
- 17.Granados M, Morticelli L, Andriopoulou S, et al. Development and Characterization of a Porcine Mitral Valve Scaffold for Tissue Engineering. J Cardiovasc Transl Res [Internet] 2017:1–17. doi: 10.1007/s12265-017-9747-z. Available from: http://link.springer.com/10.1007/s12265-017-9747-z. [DOI] [PubMed]
- 18.Tillman BW, Yazdani SK, Neff LP, et al. Bioengineered vascular access maintains structural integrity in response to arteriovenous flow and repeated needle puncture. J Vasc Surg [Internet] 2012;56:783–93. doi: 10.1016/j.jvs.2012.02.030. Available from: http://dx.doi.org/10.1016/j.jvs.2012.02.030. [DOI] [PubMed] [Google Scholar]
- 19.Chirco KR, Worthington KS, Flamme-Wiese MJ, et al. Preparation and evaluation of human choroid extracellular matrix scaffolds for the study of cell replacement strategies. Acta Biomater [Internet] 2017;57:293–303. doi: 10.1016/j.actbio.2017.05.011. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1742706117302945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baert Y, Goossens E. Preparation of Scaffolds from Decellularized Testicular Matrix. Methods Mol Biol [Internet] 2017:257–84. doi: 10.1007/7651_2017_29. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28456952. [DOI] [PubMed]
- 21.Totonelli G, Maghsoudlou P, Garriboli M, et al. Biomaterials A rat decellularized small bowel scaffold that preserves villus-crypt architecture for intestinal regeneration. Biomaterials [Internet] 2012;33:3401–10. doi: 10.1016/j.biomaterials.2012.01.012. Available from: http://dx.doi.org/10.1016/j.biomaterials.2012.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nowocin AK, Southgate A, Shurey S, Sibbons P, Gabe SM, Ansari T. The development and implantation of a biologically derived allograft scaffold. 2016:140–8. doi: 10.1002/term.1722. [DOI] [PubMed] [Google Scholar]
- 23.Maghsoudlou P, Totonelli G, Loukogeorgakis SP, Eaton S, De Coppi P. A Decellularization Methodology for the Production of a Natural Acellular Intestinal Matrix. J Vis Exp [Internet] 2013 doi: 10.3791/50658. Available from: http://www.jove.com/video/50658/a-decellularization-methodology-for-production-natural-acellular. [DOI] [PMC free article] [PubMed]
- 24.Pahari MP, Raman A, Bloomenthal A, et al. A Novel Approach for Intestinal Elongation Using Acellular Dermal Matrix: An Experimental Study in Rats. 2006:1849–50. doi: 10.1016/j.transproceed.2006.05.052. [DOI] [PubMed] [Google Scholar]
- 25.Ansaloni L, Bonasoni P, Cambrini P, et al. Experimental Evaluation of Surgisis as Scaffold for Neointestine Regeneration in a Rat Model. 2006;1848:1844–8. doi: 10.1016/j.transproceed.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 26.Cicalese L, Corsello T, Stevenson HL, et al. Evidence of Absorptive Function in vivo in a Neo-Formed Bio-Artificial Intestinal Segment Using a Rodent Model. 2016:34–42. doi: 10.1007/s11605-015-2974-1. [DOI] [PubMed] [Google Scholar]
- 27.Finkbeiner SR, Freeman JJ, Wieck MM, et al. Generation of tissue-engineered small intestine using embryonic stem cell-derived human intestinal organoids. Biol Open [Internet] 2015;4:1462–72. doi: 10.1242/bio.013235. Available from: http://bio.biologists.org/cgi/doi/10.1242/bio.013235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Franck D, Chung YG, Coburn J, David L, Jr, Mauney CREJR. In vitro evaluation of bi-layer silk fibroin scaffolds for gastrointestinal tissue engineering. 2014 doi: 10.1177/2041731414556849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Y, Lin Y, Davis KM, et al. Robust bioengineered 3D functional human intestinal epithelium. Sci Rep [Internet] 2015;5:13708. doi: 10.1038/srep13708. Available from: http://www.nature.com/articles/srep13708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang Y, Gunasekara DB, Reed MI, et al. Biomaterials A microengineered collagen scaffold for generating a polarized crypt- villus architecture of human small intestinal epithelium. Biomaterials [Internet] 2017;128:44–55. doi: 10.1016/j.biomaterials.2017.03.005. Available from: http://dx.doi.org/10.1016/j.biomaterials.2017.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Denost Q, Adam J, Pontallier A, Lyon D. Colorectal tissue engineering : A comparative study between porcine small intestinal submucosa (SIS) and chitosan hydrogel patches. Surgery [Internet] 158:1714–23. doi: 10.1016/j.surg.2015.06.040. Available from: http://dx.doi.org/10.1016/j.surg.2015.06.040. [DOI] [PubMed] [Google Scholar]
- 32.Yu J, Peng S, Luo D, March JC. E DITORS ‘ C HOICE In Vitro 3D Human Small Intestinal Villous Model for Drug Permeability Determination. 2012;109:2173–8. doi: 10.1002/bit.24518. [DOI] [PubMed] [Google Scholar]
- 33.Nakase Y, Hagiwara A, Nakamura T, et al. Tissue Engineering of Small Intestinal Tissue Using Collagen Sponge Scaffolds Seeded with Smooth Muscle Cells. Tissue Eng [Internet] 2006;12:403–12. doi: 10.1089/ten.2006.12.403. Available from: http://www.liebertonline.com/doi/abs/10.1089/ten.2006.12.403. [DOI] [PubMed] [Google Scholar]
- 34.Gardner-Thorpe J, Grikscheit TC, Ito H, et al. Angiogenesis in Tissue-Engineered Small Intestine. Tissue Eng [Internet] 2003;9:1255–61. doi: 10.1089/10763270360728161. Available from: http://www.liebertonline.com/doi/abs/10.1089/10763270360728161. [DOI] [PubMed] [Google Scholar]
- 35.Grikscheit TC, Siddique A, Ochoa ER, et al. Tissue-Engineered Small Intestine Improves Recovery After Massive Small Bowel Resection. Ann Surg [Internet] 2004;240:748–54. doi: 10.1097/01.sla.0000143246.07277.73. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00000658-200411000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grikscheit TC, Ochoa ER, Ramsanahie A, et al. Tissue-engineered large intestine resembles native colon with appropriate in vitro physiology and architecture. Ann Surg [Internet] 2003;238:35–41. doi: 10.1097/01.SLA.0000074964.77367.4a. Available from: /pmc/articles/PMC1422658/?report=abstract%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1422658&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sala FG, Kunisaki SM, Ochoa ER, Vacanti J, Grikscheit TC. Tissue-Engineered Small Intestine and Stomach Form from Autologous Tissue in a Preclinical Large Animal Model. J Surg Res. 2009;156:205–12. doi: 10.1016/j.jss.2009.03.062. [DOI] [PubMed] [Google Scholar]
- 38.Kim SS, Kaihara S, Benvenuto MS, et al. Effects of anastomosis of tissue-engineered neointestine to native small bowel. J Surg Res. 1999;87:6–13. doi: 10.1006/jsre.1999.5743. [DOI] [PubMed] [Google Scholar]
- 39.Grikscheit TC, Ogilvie JB, Ochoa ER, Alsberg E, Mooney D, Vacanti JP. Tissue-engineered colon exhibits function in vivo. Surgery. 2002;132:200–4. doi: 10.1067/msy.2002.125310. [DOI] [PubMed] [Google Scholar]
- 40.Choi RS, Vacanti JP. Preliminary studies of tissue-engineered intestine using isolated epithelial organoid units on tubular synthetic biodegradable scaffolds. Transplant Proc. 1997;29:848–51. doi: 10.1016/s0041-1345(96)00164-9. [DOI] [PubMed] [Google Scholar]
- 41.Spurrier RG, Grikscheit TC. Tissue engineering the small intestine. Clin Gastroenterol Hepatol [Internet] 2013;11:354–8. doi: 10.1016/j.cgh.2013.01.028. Available from: http://dx.doi.org/10.1016/j.cgh.2013.01.028. [DOI] [PubMed] [Google Scholar]
- 42.Costello CM, Sorna RM, Goh Y, Cengic I, Jain NK, March JC. 3 D Intestinal Sca ff olds for Evaluating the Therapeutic Potential of Probiotics. 2014 doi: 10.1021/mp5001422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shaffiey SA, Jia H, Keane T, Costello C. Intestinal stem cell growth and differentiation on a tubular scaffold with evaluation in small and large animals. Regenerative [Internet] 2016;11:45–61. doi: 10.2217/rme.15.70. Available from: https://www.futuremedicine.com/doi/full/10.2217/rme.15.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spurrier RG, Grant CN, Levin DE, Speer AL, Grikscheit TC. Vitrification preserves murine and human donor cells for delayed generation of tissue-engineered small intestine. J Surg Res [Internet] 2014;186:646–7. doi: 10.1016/j.jss.2014.04.041. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L71304520%5Cnhttp://dx.doi.org/10.1016/j.jss.2013.11.677%5Cnhttp://library.deakin.edu.au/ress://dx.doi.org/10.1016/j.jss.2013.11.677%5Cnhttp://library.deakin.edu.au/ress://library.deakin.edu.au/resserv?sid=EMBASE&issn=00224804&id=doi:10.1016%2Fj.jss.2013.11.677&atitle=Vitrification+pres. [DOI] [PubMed] [Google Scholar]
- 45.Levin DE, Barthel ER, Speer AL, et al. Human tissue-engineered small intestine forms from postnatal progenitor cells. J Pediatr Surg. 2013;48:129–37. doi: 10.1016/j.jpedsurg.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 46.Kaihara S, Kim SS, Benvenuto M, et al. Anastomosis between tissue-engineered intestine and native small bowel. Transplant Proc. 1999;31:661–2. doi: 10.1016/s0041-1345(98)01738-2. [DOI] [PubMed] [Google Scholar]
- 47.Raghavan S, Gilmont RR, Miyasaka EA, et al. Successful implantation of bioengineered, intrinsically innervated, human internal anal sphincter. Gastroenterology. 2011;141:310–9. doi: 10.1053/j.gastro.2011.03.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rocha FG, Sundback CA, Krebs NJ, et al. The effect of sustained delivery of vascular endothelial growth factor on angiogenesis in tissue-engineered intestine. Biomaterials. 2008;29:2884–90. doi: 10.1016/j.biomaterials.2008.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Minardi S, Pandolfi L, Taraballi F, et al. Enhancing Vascularization through the Controlled Release of Platelet-Derived Growth Factor-BB. ACS Appl Mater Interfaces [Internet] 2017;9:14566–75. doi: 10.1021/acsami.6b13760. Available from: http://pubs.acs.org/doi/abs/10.1021/acsami.6b13760. [DOI] [PubMed] [Google Scholar]
- 50.Ju YM, Ahn H, Arenas-Herrera J, et al. Electrospun vascular scaffold for cellularized small diameter blood vessels: A preclinical large animal study. Acta Biomater [Internet] 2017 doi: 10.1016/j.actbio.2017.06.027. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1742706117304063. [DOI] [PubMed]
- 51.Chiu LLY, Montgomery M, Liang Y, Liu H, Radisic M. Perfusable branching microvessel bed for vascularization of engineered tissues. 2012:109. doi: 10.1073/pnas.1210580109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cheng H, Leblond CP. Origin, differentiation and renewal of 4 main epithelial cell types in mouse small intestine. 5 Unitarian theory of origin of 4 epithelial cell types. Am J Anat. 1974;141:537–561. doi: 10.1002/aja.1001410407. [DOI] [PubMed] [Google Scholar]
- 53.Bjerknes M, Cheng H. Clonal analysis of mouse intestinal epithelial progenitors. Gastroenterology [Internet] 1999;116:7–14. doi: 10.1016/s0016-5085(99)70222-2. Available from: http://www.sciencedirect.com/science/article/pii/S0016508599702222. [DOI] [PubMed] [Google Scholar]
- 54.Barker N, van Es JH, Kuipers J, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature [Internet] 2007;449:1003–7. doi: 10.1038/nature06196. Available from: http://www.nature.com/doifinder/10.1038/nature06196. [DOI] [PubMed] [Google Scholar]
- 55.Sato T, Vries RG, Snippert HJ, et al. Single Lgr5 stem cells build crypt{&}{#}150;villus structures in vitro without a mesenchymal niche. Nature [Internet] 2009;459:262–5. doi: 10.1038/nature07935. Available from: http://www.nature.com/doifinder/10.1038/nature07935. [DOI] [PubMed] [Google Scholar]
- 56.Lahar N, Lei NY, Wang J, et al. Intestinal subepithelial myofibroblasts support in vitro and in vivo growth of human small intestinal epithelium. PLoS One. 2011;6:1–9. doi: 10.1371/journal.pone.0026898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lei NY, Jabaji Z, Wang J, et al. Intestinal subepithelial myofibroblasts support the growth of intestinal epithelial stem cells. PLoS One. 2014:9. doi: 10.1371/journal.pone.0084651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kuhnert F, Davis CR, Wang H-T, et al. Essential requirement for Wnt signaling in proliferation of adult small intestine and colon revealed by adenoviral expression of Dickkopf-1. Proc Natl Acad Sci [Internet] 2004;101:266–71. doi: 10.1073/pnas.2536800100. Available from: http://www.pnas.org/cgi/doi/10.1073/pnas.2536800100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pinto D, Gregorieff A, Begthel H, Clevers H. Canonical Wnt signals are essential for homeostasis of the intestinal epithelium service Canonical Wnt signals are essential for homeostasis of the intestinal epithelium. 2003:1709–13. doi: 10.1101/gad.267103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yen TH, Wright NA. The gastrointestinal tract stem cell niche. Stem Cell Rev. 2006;2:203–12. doi: 10.1007/s12015-006-0048-1. [DOI] [PubMed] [Google Scholar]
- 61.Sala FG, Kunisaki SM, Ochoa ER, Vacanti J, Grikscheit TC. Tissue-Engineered Small Intestine and Stomach Form from Autologous Tissue in a Preclinical Large Animal Model. J Surg Res. 2009;156:205–12. doi: 10.1016/j.jss.2009.03.062. [DOI] [PubMed] [Google Scholar]
- 62.Grant CN, Mojica SG, Sala FG, et al. Human and mouse tissue-engineered small intestine both demonstrate digestive and absorptive function. Am J Physiol - Gastrointest Liver Physiol [Internet] 2015;308:G664–77. doi: 10.1152/ajpgi.00111.2014. Available from: http://ajpgi.physiology.org/lookup/doi/10.1152/ajpgi.00111.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu Y, Rager T, Johnson J, Enmark J, Besner GE. Enriched Intestinal Stem Cell Seeding Improves the Architecture of Tissue-Engineered Intestine. Tissue Eng Part C Methods [Internet] 2015;21:816–24. doi: 10.1089/ten.TEC.2014.0389. Available from: http://online.liebertpub.com/doi/10.1089/ten.tec.2014.0389. [DOI] [PubMed] [Google Scholar]
- 64.Evans GS, Flint N, Somers aS, Eyden B, Potten CS. The development of a method for the preparation of rat intestinal epithelial cell primary cultures. J Cell Sci. 1992;101(Pt 1):219–31. doi: 10.1242/jcs.101.1.219. [DOI] [PubMed] [Google Scholar]
- 65.Powell DW, Pinchuk V, Saada JI, Xin Chen RCM. Mesenchymal Cells of the Intestinal Lamina Propria. Annu Rev Physiol. 2013:213–37. doi: 10.1146/annurev.physiol.70.113006.100646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Andoh A, Bamba S, Brittan M, Fujiyama Y, Wright NA. Role of intestinal subepithelial myofibroblasts in inflammation and regenerative response in the gut. Pharmacol Ther. 2007;114:94–106. doi: 10.1016/j.pharmthera.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 67.Nakase Y, Nakamura T, Kin S, et al. Endocrine Cell and Nerve Regeneration in Autologous In Situ Tissue-Engineered Small Intestine. J Surg Res. 2007;137:61–8. doi: 10.1016/j.jss.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 68.Shaffiey SA, Jia H, Keane T, et al. Intestinal stem cell growth and differentiation on a tubular scaffold with evaluation in small and large animals. Regen Med [Internet] 2016;11:45–61. doi: 10.2217/rme.15.70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26395928%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4891976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Graham HK, Maina I, Goldstein AM, Nagy N. Intestinal smooth muscle is required for patterning the enteric nervous system. J Anat. 2017;230:567–74. doi: 10.1111/joa.12583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tavakkolizadeh A, Berger UV, Stephen AE, et al. Tissue-engineered neomucosa: morphology, enterocyte dynamics, and SGLT1 expression topography1. Transplantation [Internet] 2003;75:181–5. doi: 10.1097/01.TP.0000044101.03656.9F. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00007890-200301270-00003. [DOI] [PubMed] [Google Scholar]
- 71.Neal MD, Jia H, Eyer B, et al. Discovery and validation of a new class of small molecule Toll-like receptor 4 (TLR4) inhibitors. PLoS One [Internet] 2013;8:e65779. doi: 10.1371/journal.pone.0065779. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23776545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cromeens BP, Liu Y, Stathopoulos J, Wang Y, Johnson J, Besner GE. ScienceDirect Association for Academic Surgery Production of tissue-engineered intestine from expanded enteroids. J Surg Res [Internet] 2016;204:164–75. doi: 10.1016/j.jss.2016.02.030. Available from: http://dx.doi.org/10.1016/j.jss.2016.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Matthews Ja, Sala FG, Speer AL, Warburton D, Grikscheit TC. VEGF optimizes the formation of tissue-engineered small intestine. Regen Med. 2011;6:559–67. doi: 10.2217/rme.11.49. [DOI] [PubMed] [Google Scholar]
- 74.Wieck MM, El-Nachef WN, Hou X, et al. Human and Murine Tissue-Engineered Colon Exhibit Diverse Neuronal Subtypes and Can Be Populated by Enteric Nervous System Progenitor Cells When Donor Colon Is Aganglionic. Tissue Eng Part A [Internet] 2016;22:53–64. doi: 10.1089/ten.tea.2015.0120. Available from: http://online.liebertpub.com/doi/10.1089/ten.tea.2015.0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cheng LS, Hotta R, Graham HK, Belkind-Gerson J, Nagy N, Goldstein AM. Postnatal human enteric neuronal progenitors can migrate, differentiate, and proliferate in embryonic and postnatal aganglionic gut environments. Pediatr Res [Internet] 2017:81. doi: 10.1038/pr.2017.4. Available from: http://www.nature.com/doifinder/10.1038/pr.2017.4. [DOI] [PMC free article] [PubMed]
- 76.Cheng LS, Graham HK, Pan WH, et al. Optimizing neurogenic potential of enteric neurospheres for treatment of neurointestinal diseases. J Surg Res. 2016;206:451–9. doi: 10.1016/j.jss.2016.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Natarajan D, Grigoriou M, Marcos-Gutierrez CV, Atkins C, Pachnis V. Multipotential progenitors of the mammalian enteric nervous system capable of colonising aganglionic bowel in organ culture. Development. 1999;126:157–68. doi: 10.1242/dev.126.1.157. [DOI] [PubMed] [Google Scholar]
- 78.Schäfer KH, Hagl CI, Rauch U. Differentiation of neurospheres from the enteric nervous system. Pediatr Surg Int. 2003;19:340–4. doi: 10.1007/s00383-003-1007-4. [DOI] [PubMed] [Google Scholar]
- 79.Almond S, Lindley RM, Kenny SE, Connell MG, Edgar DH. Characterisation and transplantation of enteric nervous system progenitor cells. Gut [Internet] 2007;56:489–96. doi: 10.1136/gut.2006.094565. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1856871%7B&%7Dtool=pmcentrez%7B&%7Drendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lindley RM, Hawcutt DB, Connell MG, et al. Human and Mouse Enteric Nervous System Neurosphere Transplants Regulate the Function of Aganglionic Embryonic Distal Colon. Gastroenterology. 2008;135:205–16. doi: 10.1053/j.gastro.2008.03.035. [DOI] [PubMed] [Google Scholar]
- 81.Binder E, Natarajan D, Cooper J, et al. Enteric neurospheres are not specific to neural crest cultures: Implications for neural stem cell therapies. PLoS One. 2015;10:1–18. doi: 10.1371/journal.pone.0119467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Workman MJ, Mahe MM, Trisno S, et al. Engineered human pluripotent-stem-cell-derived intestinal tissues with a functional enteric nervous system. Nat Publ Gr [Internet] 2016;23:49–61. doi: 10.1038/nm.4233. Available from: http://dx.doi.org/10.1038/nm.4233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chen Y, Lin Y, Davis KM, et al. Robust bioengineered 3D functional human intestinal epithelium. Nat Publ Gr [Internet] 2015:1–11. doi: 10.1038/srep13708. Available from: http://dx.doi.org/10.1038/srep13708. [DOI] [PMC free article] [PubMed]
- 84.Watson CL, Mahe MM, Múnera J, et al. An in vivo model of human small intestine using pluripotent stem cells. Nat Med [Internet] 2014;20:1310–4. doi: 10.1038/nm.3737. Available from: http://www.nature.com/doifinder/10.1038/nm.3737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mccracken KW, Howell JC, Wells JM, et al. NIH Public Access. 2014;6:1920–8. [Google Scholar]
- 86.Spence JR, Mayhew CN, Rankin SA, et al. Directed differentiation of human pluripotent stem cells into intestinal tissue in vitro. Nature [Internet] 2011;470:105–9. doi: 10.1038/nature09691. Available from: http://www.nature.com/doifinder/10.1038/nature09691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Avansino JR, Chen DC, Hoagland VD, Woolman JD, Haigh WG, Stelzner M. Treatment of bile acid malabsorption using ileal stem cell transplantation. J Am Coll Surg. 2005;201:710–20. doi: 10.1016/j.jamcollsurg.2005.06.270. [DOI] [PubMed] [Google Scholar]
- 88.Fuller MK, Faulk DM, Sundaram N, Shroyer NF, Henning SJ, Helmrath MA. Intestinal crypts reproducibly expand in culture. J Surg Res. 2012;178:48–54. doi: 10.1016/j.jss.2012.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Shaffiey S, Jia H, Keane T, Costello C. Intestinal stem cell growth and differentiation on a tubular scaffold with evaluation in small and large animals. Regenerative [Internet] 2016;11:45–61. doi: 10.2217/rme.15.70. Available from: https://www.futuremedicine.com/doi/full/10.2217/rme.15.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gardner-Thorpe J, Grikscheit TC, Ito H, et al. Angiogenesis in Tissue-Engineered Small Intestine. [[cited 2017 May 18]];Tissue Eng [Internet] 2003 9:1255–61. doi: 10.1089/10763270360728161. Available from: http://online.liebertpub.com/doi/pdf/10.1089/10763270360728161. [DOI] [PubMed] [Google Scholar]
- 91.Rouwkema J, Khademhosseini A. Vascularization and Angiogenesis in Tissue Engineering: Beyond Creating Static Networks. Trends Biotechnol. 2016;34:733–45. doi: 10.1016/j.tibtech.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 92.Hibino N, McGillicuddy E, Matsumara G, et al. Late term results of tissue-engineered vascular grafs in human. J Thorac Cardiovasc Surg. 2010;139(2):431–6. doi: 10.1016/j.jtcvs.2009.09.057. [DOI] [PubMed] [Google Scholar]
- 93.Atala A, Bauer S, Soker S, et al. Tissue-engineered autologous bladders for patients needing cystoplasty. Lancet. 2006;367(9518):1241–6. doi: 10.1016/S0140-6736(06)68438-9. [DOI] [PubMed] [Google Scholar]