Abstract
Despite the increasing recognition of household food insecurity as a policy issue, there is currently no routine measurement of food insecurity in the UK. There is nothing to suggest that Government will address this in the near future for all parts of the UK. In which case, policy makers and campaigners might instead seek out consistent and robust measures of the population-level factors which are known to contribute to food insecurity. However, no systematic measures exist, meaning that resources may not be targeted at those areas most in need. This paper presents the first objective estimate of high population-level risk of household food insecurity in English neighbourhoods (4.09% of the population, 95%CI 4.08-4.10) using public data. Estimated geographic distribution of factors contributing to household food insecurity is customisable to local pressures and is adaptable to settings outside of England.
Keywords: food insecurity, secondary data analysis, GIS, population estimation
1. Introduction
Those experiencing food insecurity contend with the inability to acquire or consume an adequate quality or sufficient quantity of food in socially acceptable ways, and/or the uncertainty that they will be able to do so [1]. Within the UK the very real problem of people not being able to access sufficient food has become increasingly apparent [2]. A history of welfare diversification over the last 20 years, combined with ongoing restructuring, severe public spending cuts and recession have meant a rise in both food insecurity and charitable sector responses to it [3–5].
Private sector management styles have developed in welfare alongside welfare-to-work and labour-centred benefit reforms. The outcomes have been increasing concerns over widening social inequality and inequity, and the expansion of the third sector to deal with the shortcomings in provision and coverage that these changes entail [6]. One key example is benefits sanctions, the stoppage of welfare payments to recipients. This has been identified as an immediate and severe pathway into poverty, and therefore also into food insecurity. There has been a spectacular growth of these harsh penalties for non-compliance in recent years, especially in relation to the ongoing welfare-to-work focus of post 2010-policy. At their peak, benefit sanctions in the UK exceeded the number of fines imposed by the criminal courts. The severity and potential injustice of this has become an area of debate for causing disproportionate hardship [7].
However, the growing policy problem of food insecurity in the UK is currently ill-informed due to a lack of systematically collected data on who is experiencing food insecurity, where and for how long. All nations in the UK do not routinely measure food insecurity among their populations, nor is there an established and robust measure of the population-level factors which contribute to food insecurity which might be utilised in place. This seems unlikely to change soon because of the challenges in harmonising data collection across the UK, though there are increasing calls for such data collection [8].
This paper considers how to best estimate the household conditions which contribute to food insecurity in England at a time when no widespread information on this situation is collected regularly, and offers a new tool that may be adapted by local councils or charitable groups seeking to identify areas where such conditions may be occurring more frequently. As one option, this method of estimation is described to assist in establishing a national measure of risk of household food insecurity.
1.1. The challenge of measuring food insecurity in the UK
While there are no routinely collected data on food security, one indication of the increasing incidence of food insecurity in the UK is the proliferation of food banks since 2010, highlighted in the All-party parliamentary group (APPG) on hunger and food poverty’s final report [9]. The prevalence and location of food banks – Trussell Trust food banks (the largest network of food banks in the UK, organised as a franchise) – could be used as a proxy measure for levels and distribution of food poverty or insecurity. One recent study showed that Trussell Trust food banks are more likely to open in local authorities characterised by cuts to central welfare, higher rates of unemployment and higher rates of benefit sanctions. [10] However, to rely on food bank location data to identify areas of food poverty or insecurity is extremely problematic (and indeed, not the intention of the aforementioned study). The third sector / franchise nature of food bank set ups means that the opening and location of food banks is based on community resources and local social networks – not an objective measure of need or population characteristics. In the UK, barriers to accessing food banks may include stigma associated with receiving food aid[11], awareness of local food banks and the presence of a ‘gatekeeper’ who may provide the required voucher such as a GP. In fact, research in Canada suggests that only around 20% of people who are food insecure use food banks [12]. Given the increasing importance of food insecurity as a public health issue, this approximation/lack of measurement cannot continue.
1.2. Calls for measurement solutions
A 2016 report by the Food Research Collaboration (FRC) in the UK [5] echoed the call for a formal measure of food insecurity in the UK, based on survey questions from Canada or the EU (European Union’s Survey on Income and Living Conditions [EU-SILC]). [13] The selected EU-SILC questions used in Wales and Northern Ireland reflect different aspects of food insecurity, asking about specific components of diet and meal skipping in recent weeks; this does not address changes in diet due to insufficient funds and only includes the immediate past [8].
There are validated measures of material and social deprivation for the UK that may identify areas where food insecurity is more likely to occur. The most common indicator of local deprivation in England, the Index of Multiple Deprivation (IMD), is a comprehensive measure of social and material deprivation. Some of the domains which inform local scores could be useful in identifying areas where households are likely to be at a higher risk of food insecurity, such as unemployment and benefits claimants, however, the data used in each IMD is based on older data; for example the 2015 IMD is informed by data from 2012 and 2013 [14]. It would be beneficial to include the most recent data on benefits as they are available each quarter [15]. Additionally, the IMD uses the entire population when devising a deprivation score, and we see different risk factors depending on age, household composition from the qualitative work [16] which allow for more precise measurement.
There is scope to devise a risk indicator specific to household food insecurity, as requested by the government [9] and the recent FRC report [8]. Although the IMD or other deprivation measures (such as Carstairs [17]) may be used to predict food insecurity based on population profiles, there is a precedent to develop bespoke indicators for specific health concerns. One example is the MEDclass and MediX environmental classification system to provide a score for the local physical environment as it may impact on the health of local populations [18, 19].These environmental classifications offer greater specificity to health risks/benefits posed by the physical environment that overlaps with and compliments the Living Environment domain of the IMD score [14].
Measurement of food insecurity risk by locality in the UK is now a priority, as indicated by the convening of the all-party parliamentary inquiry into food poverty and hunger which addresses this lack of information in its first term of reference: “to understand the extent and geographical spread of hunger and food poverty in this country” [9]. In the absence of a full or partial population measure a tool has been devised here to estimate household food insecurity in local areas (Middle Super Output Areas [MSOA]) across England. This tool may be adapted for use in other countries of the UK and in similar settings, such as Australia, where household food insecurity survey data are unavailable.
2. Materials and Methods
This model is created to estimate risk of household food insecurity in two broad population groups, working age including children and pensionable age. Two influential factors in identifying risk include demographic traits of the households and whether benefits are claimed. The model provides options to combine data on these factors (described here as ‘domains’) to allow end users to customise the outputs to best suit their focus; this was developed with input from potential users and stakeholders at a seminar in xxx xxx (blinded for peer review) which refined the methods and choice of presentation. [20] Please see the data appendix for detail regarding geographic scale and benefits categories for both UK and international readers.
This method is developed based on profiles identified by qualitative research rather than an income-based cut-off (e.g., households falling below a certain level of income are at risk of food insecurity [21]). Drawing on research conducted in England to inform our method is the most reliable option in the absence of a clear working hypothesis in a relatively new area of study, and it allows for the acknowledgement that in some areas of the country or personal situations income will stretch further, influenced by other living costs. We further discussed this measure with other researchers on the topic and local community groups to refine our process at a seminar in July 2015 [20]. Thus, our measure is focused on economic characteristics, as identified in the qualitative studies, however, we avoid a definitive numeric income level to characterise households at highest risk.
Choice and development of domains is informed by recent qualitative studies into food insecurity in England. The first domain identifies types (demographic profiles) of households at greatest risk of food insecurity from the 2011 Census: pensioners living alone, low-income households with dependent children, low-income lone parent households [16]. At a time when there is still little detailed information, certainly no systematic data apart from that collected by food banks about the causes or influences of food insecurity in England, the best option was to explore the literature on food insecurity that is growing in the UK. A team of researchers conducted a study based around Trussell Trust food banks, funded by the Department for Environment, Food and Rural Affairs (DEFRA) and identified the above types of households as being at highest risk of experiencing food insecurity [16]. While this area of research is developing, this was the optimal starting point to create a more detailed profile of populations at risk.
The second domain provides a range of data on benefits claimants by MSOA for a sample of recent data (Sept-Nov 2015) on the counts of people claiming benefits, here we specified Job Seekers Allowance (JSA) or Employment and Support Allowance (ESA) in Lower Super Output Areas (LSOA) [15] and the counts of people who claim JSA or ESA and were sanctioned (had benefit payments stopped) over the same time [22]. These two categories of benefit claimants are the groups for which data on sanctions were available, so became the focus of our analysis for the working age population. Data were collated providing counts of pensioners who claim Pension Credit (PC) by LSOA (then aggregated to MSOA level), an income-related benefit for pensioners [23].
When discussing this measure with local community groups, their interest was very much about prioritising areas with the highest proportion of benefit claimants [20]. Therefore the focus of the second domain is to calculate the proportion of the population claiming benefits, however, recent research has illustrated the potential connection between benefit sanctions and food insecurity [10, 24], which is explored briefly as another option for estimating higher risk of food insecurity.
The data on benefit sanctions are available for MSOA level by month, and we collated the data, which matches temporally with the number of benefit claimants, Sep-Nov 2015. Here we have opted to use data provided on the count of individuals with an adverse sanction decision (benefits are stopped) rather than a total count of benefit sanctions to avoid double-counting people with more than one sanction in the time period. Although we recognise that the impact of multiple sanctions is likely very detrimental to food security for an individual, the intention is to compile a population risk profile. Notably, the number of benefit sanctions has declined [25] since the publication of Loopstra et al, [10] therefore the example selected to illustrate population-level influences of food insecurity risk is based on the distribution of benefit claimants rather than sanctions.
The model was developed to provide an index of food insecurity risk for two population groups: working age & children (0–64 years) and pensionable age (65+). This used data at the MSOA level, where there are 6791 such areas in England. The two domains may be used independently to either estimate food insecurity risk based on household composition, to explore the distribution or changes in benefit claimants by small area, or to combine the two domains. Table 1 describes the domains that make up the Index of Food Insecurity (IFI) and the data which underpins them. This model is developed to be comparable to the 2015 Indices of Deprivation for England [14], which is comprised of seven sub-domains (Income, Employment, Living Environment, etc) that can be used together or individually. With the two population groups and two domains in the IFI users may select the appropriate domains to answer specific queries such as “Where is the estimated prevalence of food insecurity greatest for pensioners?” (Household type pensionable population, Incidence of PC claimants)
Table 1.
Domains of household food insecurity risk for areas. Both domains are calculated for working age groups including children (0–64 years) and pensioners (65+ years)
| Domain | Source | Date | Data | Description |
|---|---|---|---|---|
| Household type | Census of Population | 2011 | Household composition1 Occupation of Household Reference Person2 Population age 0-64 years3 Population aged 65+ years1 |
Quintiles of prevalence based on household characteristics by MSOA |
| Benefit profile | Department for Work & Pensions Office for National Statistics (annual population estimates for MSOAs) |
June 2015-May 2016 Mid-2015 estimates |
Count of people claiming JSA, ESA, PC benefits by LSOA, MOSA (age 16-64, 65+) Count of JSA or ESA benefit sanctions by MSOA |
Classification of MSOA by incidence of claimants: quintiles, 2 SD above the mean Classification by MSOA by incidence of sanctions |
Table DC1109EW
Table QS608EW
Table KS102EW
Data were combined from the 2011 Census of population [26] as domain one (household type), and data from the Department for Work and Pensions (DWP) collated to represent the proportion of a local population receiving benefits including JSA, ESA or PC (domain 2, benefit claimants). The data can be expressed as the proportion of the population who meet the risk profile for one or both of these domains, with quintiles or similar area classifications calculated for each of the domains. There are also different recommendations on addressing household food insecurity in these two broad age groups from a recently submitted report to the Inquiry [27].
2.1. Domain one: Household type
In an optimal situation, data would be available to show the number of households in an area which are at risk of food insecurity due to household structure and occupational status (for example, low income households with dependent children; low income single parent households with dependent children). However, these data are not available so a joint probability was calculated. This was feasible as the probability of a household to have dependent children is statistically independent of the occupational group of the Household Representative Person (HRP) (akin to head of household). Calculation of joint probabilities of household types at greatest risk of food insecurity is described below (Table 2).
Table 2.
Calculation of household type domain (Domain 1)
| Working age population at highest risk of food poverty: |
| p (Ch,LI) = probability of a person in an MSOA to be in a household with dependent children (Ch) from Census table DC1109EW and on a low income (LI) as defined by the occupation class Routine, Semi-routine or long term unemployed of the HRP |
| p (LP,LI) = probability of a person in an MSOA to be in a lone parent household (LP) with dependent children and on a low income as defined by the occupation of the HRP (LI, as above) |
| LowInc with Child = p (LP,LI) x p (Ch,LI) x total population under age 65 |
| Pensionable age population at highest risk of food poverty: |
| SingPenCt= count of a person in an MSOA in a household made up of a single pensioner |
The resulting probabilities, joint or single, were applied to the age-appropriate 2011 base population to provide the proportion of people at greatest risk of food poverty based on household type.
2.2. Domain two: Benefits claims and sanctions
The second domain relating to benefits profiles was created by collating data on benefits claimants by LSOA in Sep-Nov 2015. Data aggregation via a look up table was required as the counts of benefits claimants were available by 2001 Lower Super Output Area (LSOA) boundaries, which fit within MSOA 2011 boundaries.
Values for this domain may be expressed as incidence of benefits claimants by MSOA, ranked into quintiles or the distribution of MSOAs around the mean incidence of the population claiming benefits each year. The incidence was calculated using the Office for National Statistics (ONS) mid-year population estimates for 2015 at the MSOA level as the denominator [28] (see Table 1 for details). Downloaded claimant data from DWP are rounded to the nearest five count of the population so an error term was incorporated as recommended by the ONS [29]. The mean proportion of the populations claiming benefits and standard deviation (SD) was calculated, with areas having incidence above two SD over the mean identified as having significantly higher than expected rates of claimants. The same calculations for benefit sanctions were completed, totalling four choices for domain 2.
2.3. Combining the domains
Two examples of how the domains may be combined are shown below, as calculated using Microsoft Excel.
First, we identified the MSOAs which are in the highest quintile for Domain 1 (both age groups) AND have a significantly high number of benefit claimants (>2 SD above the mean), and mapped the results. For validation purposes we tested one further combination. To create a numeric value from both domains, we summed the ranks of each MSOA for both domains, with a higher weighting on the household profile domain (75%) than the benefits claimants (25%). This addressed any potential double-counting of benefits claimants (Domain 2) who are included in households on low income in the Census (Domain 1).
2.4. Validation of the estimates and comparison with food bank locations, area deprivation
The difficulty with assessing reliability of a measure where we are estimating outcomes that are unknown is that no outcome data are available at the same scale. This is typically a challenge in small-area estimation methods, and can be addressed by either aggregating small area estimates up to a geography where the data area known [30], or to assess model fit against a related outcome. In the case of type 2 diabetes authors have used the rate of diabetic amputations to validate estimates of population prevalence [31]. Here, we compare the spatial distribution of estimated risk of population-level food insecurity against the locations of franchised food banks (Trussell Trust), the 2015 IMD score, and the prevalence of childhood obesity which is measured using the National Child Measurement Programme (NCMP).
Modelled estimates of household food insecurity risk are validated against the prevalence of children in reception and/or year 6 who are classified as obese from the NCMP data, which includes children who have a BMI greater than or equal to the 95th centile of the 1990 British growth reference. The estimates of food insecurity risk are validated using the 2011-14 pooled data at the MSOA level. Over 99% of the records in the dataset included valid postcodes for each of the three years [32].
This outcome was selected as a validation because children are more often protected from food insecurity (parents not eating to feed children), so the impact of food insecurity may be most visible in this population [33, 34]. Episodic food insecurity can lead to overweight [35, 36] and the Faculty of Public Health indicates that overweight/obese is associated with food insecurity [35, 37].
The distribution of Trussell Trust food banks (August 2016) was compared to both the 2015 IMD score and the food insecurity domains, to identify any correlation between locations of food banks and areas where more of the population is at higher risk. The hypothesis was that food bank locations may not be correlated to areas of either high food insecurity risk or deprivation as measured by the IMD, as food banks are a charitable sector response which are therefore limited to locations with sufficient volunteers and storage available. A comparison of the results from the model with childhood obesity and the 2015 IMD score was completed using Spearman’s rank correlation. Quintiles of MSOAs for each domain and a combined risk score were compared with quintiles of childhood obesity by MSOA using a χ2 test. All analyses were conducted in SPSS v 22.
3. Results
The resulting estimates are shown below for each of the domains, with maps of the two populations and the combined estimated level of risk. The combined risk is calculated as described above and mapped, and then the results (domain estimates, combined estimates) are compared with the distribution of childhood obesity, and finally at the Local Authority District (n=326) level against the IMD score and food bank density due to small numbers of food banks in MSOAs.
3.1. Domain one: Household type
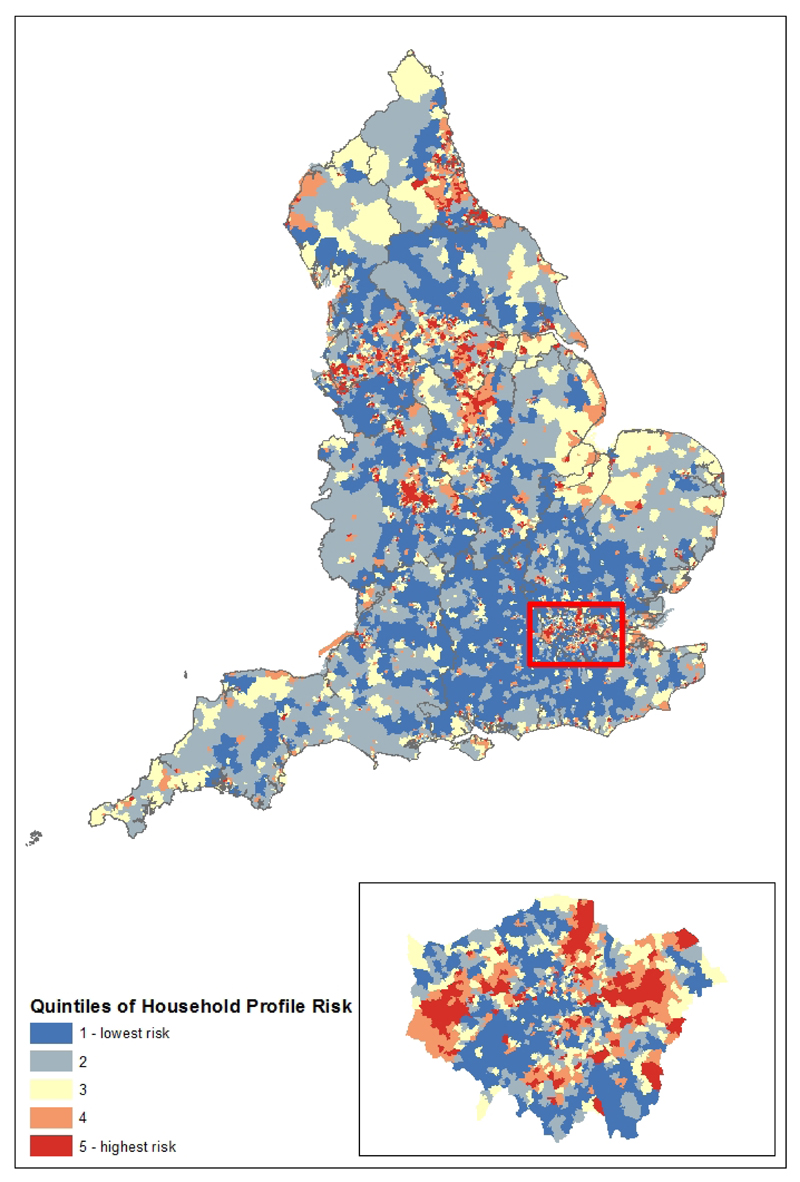
The total population at highest risk of household food insecurity from the 2011 Census was estimated to be 9,074,700 or 17.4% of the total population (95% CI: 17.2-17.5). This includes 6,349,103 (14.5%; 95% CI: 13.7-14.3) of the children and working age population and 2,725,596 (32.4%) of the over-65 population (95% CI: 32.2-32.5). The total counts of household types at greatest risk were converted to proportions of the population at risk of food insecurity by MSOA (range 0.90%–44.0%; mean 17.3%, standard deviation 6.9%). These proportions were used to calculate quintiles of risk for all MSOAs in England where Quintile 1 has the lowest risk and Quintile 5 the highest (Figure 1).
Figure 1.
Household food insecurity risk by household type for England by 2011 MSOA
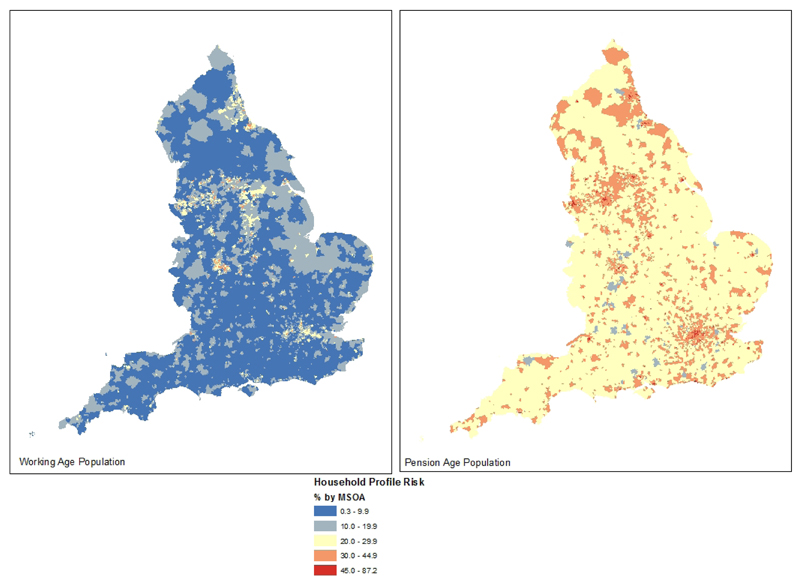
The distribution of areas where more households are deemed at risk based on this profile varies between the working age with children population (0.3-44.8% of households within a MSOA) and the pension age population (14.4-87.2%) (Figure 2). The working age population households are concentrated in urban areas, however it is worth noting the difference in proportions between the two populations (pensioners: mean 32.8, SD 7.0; working age: mean 14.2, SD 7.9). The pensioner population has a greater influence on the overall household risk shown in Figure 1.
Figure 2.
Domain 1 shown by age-specific population
3.2. Domain two: Benefits Claimants
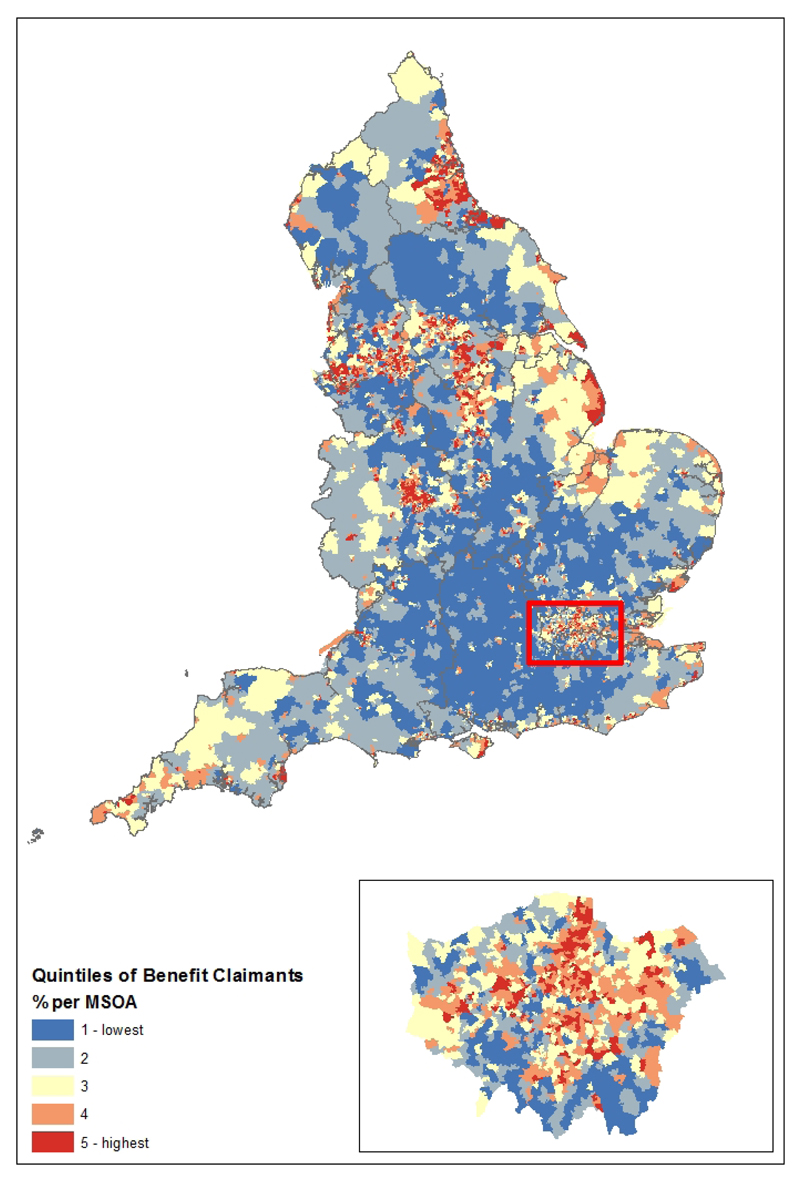
The populations in MSOAs claiming benefits were calculated with a focus on the proportion of the working age population claiming either JSA or ESA and the proportion of the pensionable age population claiming PC. The overall total of the population in each area claiming one of these three benefits is shown in Figure 3, again expressed as quintiles. Children age under 16 years are excluded from this population altogether as they are not eligible to claim any of these benefits.
Figure 3.
Household food insecurity risk by benefit claimants for England by 2011 MSOA
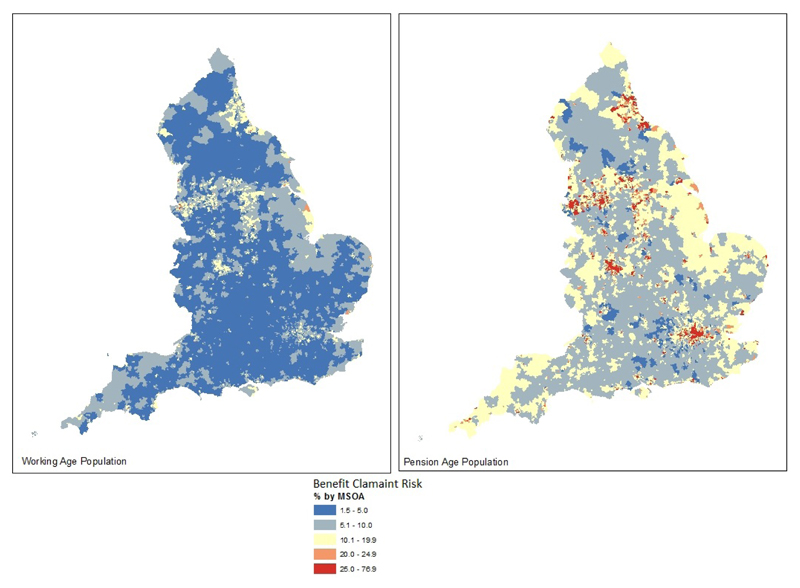
The difference between the distributions of the two population groups is illustrated in Figure 4. The proportion of working age population claimants in MSOAs range between 0.1 to 31.8%, mean 7.3 and SD 4.2. For the population claiming PC, the values range from 1.5 to 76.9%, mean 17.4 and SD 10.6. Again, the combined measure of benefits claimants is driven by higher rates of pensioners claiming PC.
Figure 4.
Domain 2 shown by age-specific population
An alternative way to explore the data on benefits claimants is to identify the areas where benefit sanctions on JSA or ESA are most frequent. Analysis of the most recent data (Sept-Nov 2015) shows that most (63.8%) MSOAs had no sanctions, while there was a maximum of 96 sanctions in any one MSOA. The mean number of sanctions per MSOA over this time was 4.58 with a SD of 8.06. Looking at the data as proportions of the populations in each area claiming either JSA or ESA, again the range is from 0 to 78.9%, with a mean value of 1.94% and SD of 4.42. We identified the areas with significantly more sanctions (>2 SD above the mean); 326 MSOAs reported this many sanctions in the time period. Only two of these MSOAs were also identified as being in the highest risk quintile for domain 1, and the data were heavily skewed by a large number of MSOAs with no sanctions over this time.
3.3. Combining the risk domains
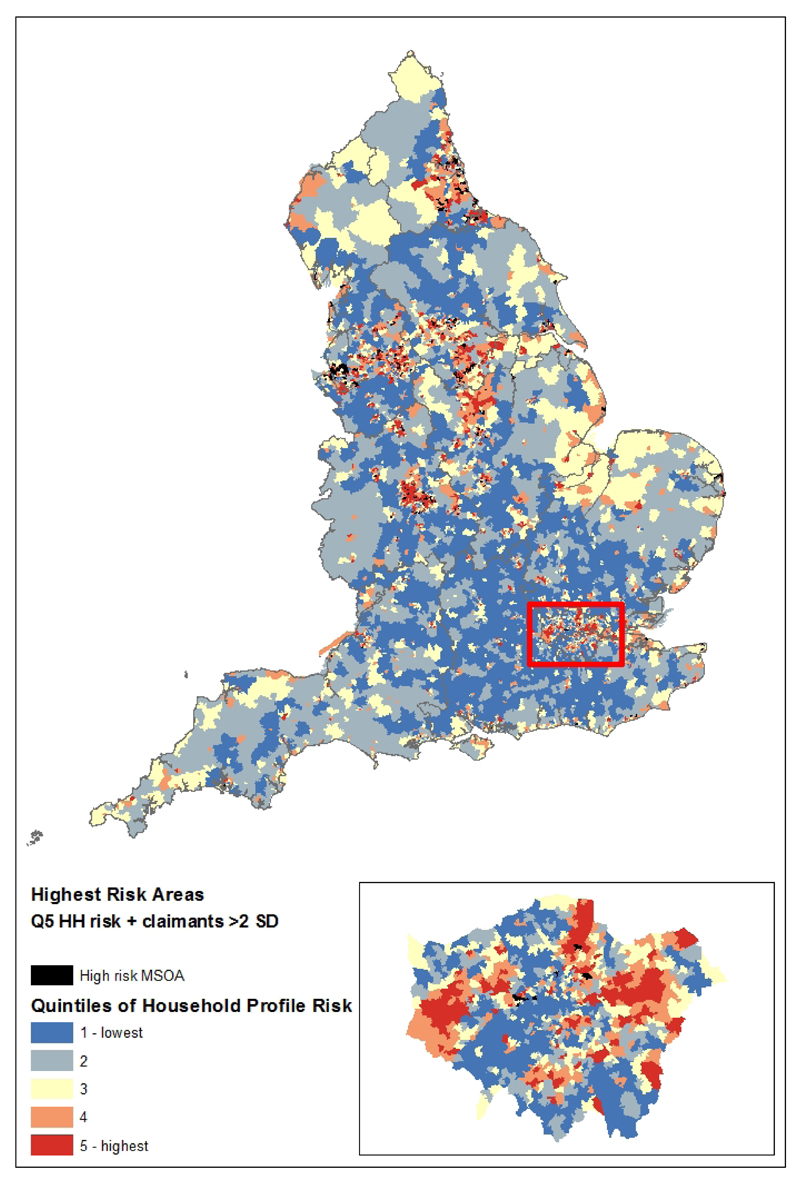
The two domains were combined to map the MSOAs where the risk of household food insecurity is highest based on household type (Quintile 5, n=1358) and a significantly high number of benefits claimants, the mean percentage of claimants plus two SD of the population claiming JSA, ESA or PC (n=326). Figure 5 highlights in black the MSOAs where both conditions are true (n=301, 4.43% of MSOAs representing 4.09% of the population [95%CI: 4.08-4.1%]). The figures are very similar to data from Oxfam, estimating about 2 million people in the UK are malnourished, and in total 3 million are at risk of malnourishment. [38] These MSOAs are concentrated in several northern cities and part of London (Figure 5).
Figure 5.
Combined risk, with the MSOAs at highest estimated risk identified
3.4. Validation of the method and comparison with IMD score food bank locations
Three datasets are compared to the spatial distribution of estimated risk of population-level food poverty against the 2015 IMD score, locations of franchised food banks (Trussell Trust) and the prevalence of childhood obesity using NCMP data.
The Spearman correlation between the 2015 overall IMD score (population-weighted averages for MSOAs, as the IMD is calculated for LSOAs) and the risk of food poverty estimated as a combined risk from both domains (ranks for Domain 1 added to the rank for Domain 2, weighted at 3:1) is 0.929, where p<0.01. This is a highly significant correlation, which is expected given the data used to calculate the household risk of food poverty is collinear with data used in the calculation of the IMD scores: individuals on low incomes and/or claiming benefits. The 2015 IMD score is derived from seven domains, with 44.5% of the overall score based on low income (Income domain) or excluded from work (Employment domain). [14] There were significant and positive correlations between the domains and specific population domains and the IMD and NCMP data (Table 3). Only benefit sanctions were negatively correlated with all other variables; this may be due to the time period of the data used and the distribution of the data. Childhood obesity, labelled in the table as NCMP, is positively correlated with both domains individually and the combination of the two (Ranks Combined).
Table 3.
Correlations between domains, variables and NCMP and IMD data at MSOA level. ** indicates the relationship is significant at p<0.01, two tailed
| Domain 1 | Domain 2 | Domain 1: Working age | Domain 1: Pensioner | % JSA/ESA Claimants | % PC Claimants | IMD 2015 | % Sanction | Ranks Combined | NCMP | |
|---|---|---|---|---|---|---|---|---|---|---|
| Domain 1 | 1.000 | .876** | .970** | .469** | .866** | .759** | .830** | -.070** | .928** | .694** |
| Domain 2 | .876** | 1.000 | .838** | .614** | .986** | .898** | .933** | -.097** | .992** | .693** |
| % JSA/ESA Claimants | .866** | .986** | .832** | .590** | 1.000 | .848** | .922** | -.098** | .979** | .678** |
| % PC Claimants | .759** | .898** | .763** | .697** | .848** | 1.000 | .911** | -.106** | .884** | .697** |
| Domain 1: Working Age | .970** | .838** | 1.000 | .393** | .832** | .763** | .827** | -.068** | .892** | .724** |
| Domain 2: Pensioner | .469** | .614** | .393** | 1.000 | .590** | .697** | .594** | -.090** | .592** | .352** |
| IMD 2015 | .830** | .933** | .827** | .594** | .922** | .911** | 1.000 | -.102** | .929** | .730** |
| % Sanction | -.070** | -.097** | -.068** | -.090** | -.098** | -.106** | -.102** | 1.000 | -.093** | -.080** |
| Ranks Combined | .928** | .992** | .892** | .592** | .979** | .884** | .929** | -.093** | 1.000 | .710** |
| NCMP | .694** | .693** | .724** | .352** | .678** | .697** | .730** | -.080** | .710** | 1.000 |
Quintiles based on the two domains were compared with quintiles of childhood obesity using a cross-classification table. In both cases there was a significant result for the test of association (Domain 1 x Obesity χ2 = 3548, p < 0.001; Domain 2 x Obesity χ2 = 3402, p < 0.001). The quintiles of combined ranks were also significantly associated with quintiles of obesity (χ2 = 3583, p < 0.001). Each table included only MSOAs with valid data for obesity (n=6578).
Another consideration is to compare the IFI estimates with food bank location data. A total of 318 Trussell Trust food banks were open in England in August 2016 when the data were accessed, of which 313 were successfully geocoded. The locations of food banks (number per local authority [LA], n=326) ranged from zero to 10, with an average of one per LA. Over a third of the LAs had no food bank (n= 113, 34.7%) and nearly half (46.3%) had only one. Repeating the correlation analysis at the LA level with food banks included as the number per 1000 residents, there were no significant relationships between food bank density and any of the other variables.
4. Discussion
This paper has presented a method of estimating household food insecurity risk in small areas of England, which has the option to be updated quarterly as new data on benefit claimants and sanctions are made available. Users may choose to focus on either the working age including children or pensionable age population, and may alter the weight of benefits to household profiles to customise the measure for local situations. The results and data inputs may be shared with interested parties and mapped in free software such as Google Fusion Tables to allow for ease of use. In a setting where food insecurity is not measured in any systematic process, this method offers a much-needed means of estimating population-level risk.
Food insecurity is increasing at a population level. This is evident in the data collected by Trussell Trust [39], research by academics in varied settings across England [21, 40] and from other charities who address food insecurity [41]; Oxfam provides similar estimates of malnourishment across the UK to predictions reported here [38]. Until we have a more accurate way of measuring local-level population experience of food insecurity a risk score allows local authorities and charities a way to assess local risk and plan appropriate interventions. This was one key message from the APPG on food poverty and hunger which we have addressed, to assess the extent of food poverty spatially.
4.1. Limitations
There are some limitations to the model. The model does not include housing or council tax benefit claimants as there were no data on sanctions for these types of benefits. Household type may inadvertently double-count people claiming benefits due to unemployment or having children. The data informing household type is by necessity from the 2011 Census so would benefit from more informed local surveys to update this domain. The benefits data are complicated; looking at counts of claimants does not address the number of people unable to claim. Finally, as with any area-based estimate we must acknowledge the ecological fallacy; not all people living in areas classified as highest risk will experience food insecurity, just as many people living in areas classified as lower risk may experience food insecurity.
4.2. Alternative measures
Trussell Trust are devising a similar measure of food insecurity risk based on the profiles of clients who visit their food banks [42]. This is indeed a useful tool as it will help to identify areas where there are similar populations, however, this will not identify the populations who experience food insecurity but do not seek help from a food bank. By using qualitative data from work on food insecurity rather than food bank clients we offer an alternative that will identify a wider profile of populations at risk of food insecurity. The use of data from the Census and DWP provides access to our measure to a variety of organisations, and a methodology for use in other countries where food insecurity is of increasing concern but presently unmeasured such as Scotland and Australia.
There are multiple options for the interpretation of the risk estimates, with examples provided in this paper. Here we highlighted MSOAs where there were very high numbers of benefits claimants and people in high-risk household profiles, however, in some areas there may be more important stressors, such as housing benefit charges such as the bedroom tax/spare room subsidy [41]. Given the flexibility of this model each user may specify the combination of domains to customise the outputs. What we are able to do is disaggregate the estimates by population age to illustrate the spatial patterns of risk factors, such as single pensioners or families with low incomes and dependent children. This information will be useful for considering the type of intervention: perhaps more community meals in areas where there are more pensioners at risk, or more summer holiday lunch clubs where there are more families with children at risk.
The IMD is one option to identify areas where risk is higher, however, our method offers a measure which can be updated regularly and customised to address locality-specific stressors as well as population subgroups. As discussed, food bank density is not an appropriate proxy measure for food insecurity and in fact there was no significant relationship between food bank density and either the risk estimates or IMD score; this may be due to the greater capacity for volunteers in less deprived areas. Childhood obesity prevalence was used to validate these estimates as the best available proxy indicator of food insecurity.
4.3. Possible applications
We offer suggestions of alternative means of collecting data on food insecurity alongside the use of our risk estimation tool to gather a comprehensive picture of household food insecurity. A recent review of food insecurity studies across the UK identified a range of approaches from eleven studies dating from 2000, but there was no consistent means of measurement [43]. Similar lack of consistent measurement was described in the recent compilation by the Food Research Collaboration [8].
The use of a food insecurity measurement tool based on the HFSS Core Module from the US, following research to validate its use in the UK, is recommended for consistent use in research and national data collection. This survey is the most extensive measure found, both in the various dimensions (e.g. anxiety, coping behaviours) and the levels (e.g. household, adult and child) of food insecurity. It is likely that this survey would be valid for use in the UK because of the similarities between these countries and the US, and could be incorporated into the regular national health surveys of England and Scotland to gather more consistent data on the extent of food insecurity in these settings. The incorporation of this measure, or the HFSS subset for convenience, into samples of Accident & Emergency A&E/ER attendance data or a primary care setting would allow for monitoring of more vulnerable groups who are not captured in national household-based surveys. In the absence of extended data collection, a tool such as this model offers a strong alternative approach to estimating household food insecurity in the UK.
A set of known risk factors for food insecurity, similar to screening GP databases to compile risk scores for type 2 diabetes [44], could identify local populations more likely to experience food insecurity. This information could then be shared with local medical and social care professionals. GPs, midwives or district nurses may then be more prepared to sensitively assess the situation with patients.
5. Conclusion
Household food insecurity is a very real challenge in England, however, we lack consistent data on the extent and spatial distribution of the problem. Building on the terms agreed by the parliamentary inquiry to define and implement the means to regularly measure population-level food insecurity, one option is presented here with suggestions for improved data collection as seen in other countries that are also attempting to tackle food insecurity in a wealthy context. On a pragmatic level, the necessity of estimating food insecurity locally and identifying at-risk populations and areas is evident; just over 4% of the population is estimated to be at high risk at any one time (95% CI 4.08-4.10 of the population), but the geography of the populations (working age and pensioners) vary dramatically. This global model will allow for more effective local responses targeting higher-risk groups in each area, and is the first neighbourhood-level model of food insecurity risk for England.
On a more political level, we would argue that by failing to measure household food insecurity we are failing to acknowledge it as a serious problem in terms of both social policy and public health. The WHO identifies food as a basic human right; the UK is failing to provide this through formal sectors, with implications for public health already becoming apparent. [4, 5, 45] Country-wide measurement of household food insecurity, as described here, is necessary both to enable primary care providers to address the problem at the local level and to reframe it as a national issue.
Acknowledgements
We would like to thank XXX XXXX for comments on an earlier draft, and the reviewers for their suggestions. We are grateful to participants from a <blinded> seminar for their comments on combining the domains and domain specification.
Funding: none.
Appendix
| Middle Super Output Area (MSOA) | The main geographic unit used in this analysis, a statistical unit from the 2011 Census with a mean population of 7000. |
| Lower Super Output Area (LSOA) | A smaller geographic unit from the 2011 Census with a mean population of 1500. |
| Job Seekers Allowance (JSA) | Financial unemployment benefit paid while seeking work. In this paper it refers to either the income- or contribution-based JSA. Income-based is based on eligibility rules around hours worked and savings. Contribution-based JSA is available to individuals who had paid sufficient National Insurance contributions prior to claiming JSA. |
| Employment and Support Allowance (ESA) | Financial benefit paid to people who are ill or disabled and it affects their work. As with JSA there are income- and contribution-based versions of ESA. Contribution based ESA is payable up to a year for people in some work, and may be payable alongside income-based ESA |
| Pension Credit (PC) | Financial income-related benefit for people of pensionable age. There are two parts, a Guarantee Credit which ensures a weekly income for single people or couples and a Savings Credit for people who have already saved money toward a pension. |
Footnotes
Author contribution: blinded for peer review
Competing interests: None declared.
Data sharing: All data included in the analysis are freely available from the 2011 Census, Office for National Statistics and the Department for Work & Pensions.
References
- 1.Riches G. Hunger and the welfare state: comparative perspectives. In: Riches G, editor. First World Hunger: Food Security and Welfare Politics. Macmillan Press; Basingstoke: 1997. [Google Scholar]
- 2.Alkon AH, et al. Foodways of the urban poor. Geoforum. 2013;48:126–135. [Google Scholar]
- 3.Lambie-Mumford H. 'Every Town Should Have One': Emergency Food Banking in the UK. Journal of Social Policy. 2013;42(1):73–89. [Google Scholar]
- 4.Ashton JR, Middleton J, Lang T. Open letter to Prime Minister David Cameron on food poverty in the UK. The Lancet. 2014 doi: 10.1016/S0140-6736(14)60536-5. [DOI] [PubMed] [Google Scholar]
- 5.Taylor-Robinson D, et al. The rise of food poverty in the UK. BMJ. 2013;347 doi: 10.1136/bmj.f7157. [DOI] [PubMed] [Google Scholar]
- 6.Heins E, Bennett H. ‘Best of Both Worlds’? A Comparison of Third Sector Providers in Health Care and Welfare-to-Work Markets in Britain. Social Policy & Administration. 2016;50:39–58. [Google Scholar]
- 7.Adler M. A New Leviathan: Benefit Sanctions in the Twenty-first Century. Journal of Law and Society. 2016;43(2):195–227. [Google Scholar]
- 8.Food Research Collaboration. Time to count the hungry: the case for a standard measure of household food insecurity in the UK. 2016 [Google Scholar]
- 9.All party parlimentary group on hunger & food poverty. Feeding Britain: A strategy for zero hunger in England, Wales, Scotland and Northern Ireland. London: 2014. [Google Scholar]
- 10.Loopstra R, et al. Austerity, sanctions, and the rise of food banks in the UK. BMJ. 2015;350 doi: 10.1136/bmj.h1775. [DOI] [PubMed] [Google Scholar]
- 11.Lambie-Mumford H, et al. Household food security in the UK: a review of food aid. Department for Environment, Food and Rural Affairs; London: 2014. [Google Scholar]
- 12.Loopstra R, Tarasuk V. Food bank usage is a poor indicator of food insecurity: Insights from Canada. Social Policy & Society. 2015;14(3):443–455. [Google Scholar]
- 13.Arora VS, et al. Data Resource Profile: The European Union Statistics on Income and Living Conditions (EU-SILC) International Journal of Epidemiology. 2015;44(2):451–461. doi: 10.1093/ije/dyv069. [DOI] [PubMed] [Google Scholar]
- 14.Department for Communities and Local Government. The English Indices of Deprivation 2015 Statistical Release. 2015 [Google Scholar]
- 15.Department for Work and Pensions. Neighbourhood Statistics Data. 2016 Available from: http://tabulation-tool.dwp.gov.uk/NESS/page1.htm.
- 16.Kneafsey M, et al. Consumers and food security: Uncertain or empowered? Journal of Rural Studies. 2012;29:101–112. [Google Scholar]
- 17.Carstairs V. Deprivation indices: their interpretation and use in relation to health. J Epidemiol Community Health. 1995;49 doi: 10.1136/jech.49.suppl_2.s3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richardson EA, et al. Developing Summary Measures of Health-Related Multiple Physical Environmental Deprivation for Epidemiological Research. Environment and Planning A. 2010;42(7):1650–1668. [Google Scholar]
- 19.Richardson EA, et al. Evidence-based selection of environmental factors and datasets for measuring multiple environmental deprivation in epidemiological research. Environmental Health. 2009;8(1):1–8. doi: 10.1186/1476-069X-8-S1-S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thompson C, Smith D, Shelton N. Exploring the health challenges and inequalities of the new food aid system: a half-day symposium on working with and within foodbanks. Wellcome Trust; 2015. [Google Scholar]
- 21.Niamh OC, Karim F, Richard B. What is food poverty? A conceptual framework. British Food Journal. 2016;118(2):429–449. [Google Scholar]
- 22.Department for Work and Pensions. Jobseeker’s Allowance and Employment and Support Allowance sanctions statistics. 2016 Available from: https://www.gov.uk/government/collections/jobseekers-allowance-sanctions.
- 23.Department for Work and Pensions. Pension Credit. 2016 Available from: http://tabulation-tool.dwp.gov.uk/NESS/BEN/pc.htm.
- 24.Garratt E. Please sir, I want some more: an exploration of repeat foodbank use. BMC Public Health. 2017;17(1):828. doi: 10.1186/s12889-017-4847-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Webster D. Briefing: The DWP’s JSA/ESA sanctions statistics release. 2015 [Google Scholar]
- 26.Office for National Statistics. 2011 Census of Population. 2012 [Google Scholar]
- 27.Tywcross F. Inquiry into Food Poverty and Hunger in Britain. 2014 [Google Scholar]
- 28.Office for National Statistics. Middle Super Output Area Mid-year population estimates. 2014 [Google Scholar]
- 29.Office for National Statistics. Analysing change over time for small areas: a strategy. 2013 [Google Scholar]
- 30.Riva M, Smith D. Generating small-area prevalence of psychological distress and alcohol consumption: validation of a spatial microsimulation method. Social Psychiatry and Psychiatric Epidemiology. 2012;47(5):745–755. doi: 10.1007/s00127-011-0376-6. [DOI] [PubMed] [Google Scholar]
- 31.Congdon P. Estimating diabetes prevalence by small area in England. Journal of Public Health. 2006;29(1):71–81. doi: 10.1093/pubmed/fdi068. [DOI] [PubMed] [Google Scholar]
- 32.Public Health England, editor. Data tables: Electoral Ward and MSOA NCMP child obesity prevalence. 2015.
- 33.Bruening M, Lucio J. Parent-child relationships between food insecurity and eating behaviors. The FASEB Journal. 2015;29(1 Supplement) [Google Scholar]
- 34.Coleman-Jensen A, McFall W, Nord M. Food Insecurity in Households With Children Prevalence, Severity, and Household Characteristics, 2010-11. Economic Research Service/USDA; 2013. [Google Scholar]
- 35.Eisenmann JC, et al. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obesity Reviews. 2011;12(5):e73–e83. doi: 10.1111/j.1467-789X.2010.00820.x. [DOI] [PubMed] [Google Scholar]
- 36.Metallinos-Katsaras E, Must A, Gorman K. A longitudinal study of food insecurity on obesity in preschool children. J Acad Nutr Diet. 2012;112(12):1949–58. doi: 10.1016/j.jand.2012.08.031. [DOI] [PubMed] [Google Scholar]
- 37.Faculty of Public Health. Food Poverty & Health: Briefing Statement. 2004 [Google Scholar]
- 38.Oxfam. Food Poverty in the UK. 2016 Available from: http://policy-practice.oxfam.org.uk/our-work/poverty-in-the-uk/food-poverty#contentprimary_0_ctl00_FirstTab.
- 39.Trussell Trust. Latest Stats. 2016 Available from: https://www.trusselltrust.org/news-and-blog/latest-stats/S.
- 40.Dowler EA, et al. Thinking about 'food security': engaging with UK consumers. Critical Public Health. 2011;21(4):403–416. [Google Scholar]
- 41.Cooper N, Purcell S, Jackson R. Below the Breadline: the relentless rise of food poverty in Britain. Church Action on Poverty; 2014. [Google Scholar]
- 42.AAM Associates. Trussell Trust data visualisation platform overview. 16 Jun 16; Available from: https://vimeo.com/164281583.
- 43.Parker S. Measures of Food Poverty in the United Kingdom: A Review. CPCPH; Queen Mary University of London; 2013. [Google Scholar]
- 44.Noble D, et al. Feasibility study of geospatial mapping of chronic disease risk to inform public health commissioning. BMJ Open. 2012;2(1) doi: 10.1136/bmjopen-2011-000711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O'Dowd A. Half a million people using food banks in UK as food poverty grows. BMJ. 2013;346 doi: 10.1136/bmj.f3578. [DOI] [PubMed] [Google Scholar]