Abstract
Background
Inability to resume employment after acute myocardial infarction (MI) has important implications for patients. We sought to assess the prevalence of and outcomes associated with adverse change in employment after MI in a national US cohort.
Methods and Results
The TRANSLATE-ACS study assessed employment status at baseline and 1 year among 9,319 MI patients (mean age 60.8 years, standard deviation [SD] 11.3; 27.3% female) enrolled at 233 US hospitals. We defined adverse change in employment as patients working at baseline but working less or not working at 1 year post-MI. In multivariable models, we assessed factors associated with adverse change in employment and its association with patient-reported depression, health status, persistence to evidence-based medications prescribed at discharge and financial hardship affording medications. Half of patients (51%, n=4,730) were employed at the time of MI. By 1 year, 10% (n=492) of these reported an adverse change in employment, with 3% (n=143) working less and 7% (n=349) no longer working (only 27 of 349 reported retirement). Factors significantly associated with adverse change in employment included number of unplanned readmissions, post-discharge bleeding complications, hypertension, and smoking. At 1 year, patients with an adverse change in employment were more likely to report depression (Patient Health Questionnaire-2 score >3: 27.4% vs. 16.7%), lower health status (mean EuroQoL visual analogue scale: 73 [SD 17.8] vs. 78 [SD 14.8]) and moderate-extreme financial hardship with medication costs (41.0% vs. 28.4%) (all p<0.001). There was no difference in persistence to evidence-based medications prescribed at discharge.
Conclusions
Patients who experienced an adverse change in employment after MI reported lower quality of life, increased depression and more difficulty affording medications. These results underscore the need for interventions to address this patient-centered outcome and its health impact.
Clinical Trial Registration
ClinicalTrials.gov; Unique Identifier: NCT01088503
Keywords: acute myocardial infarction, job Loss, depression, quality of life, medication adherence, financial hardship
Cardiovascular disease is the leading cause of morbidity and mortality in the United States1 and acute myocardial infarction (MI) accounts for a significant proportion of the disease burden of cardiovascular disease. Advances in prevention and treatment strategies have led to significant improvement in clinical outcomes and age-adjusted mortality from MI.2 It remains unclear, though, if similar progress has been achieved in outcomes that are particularly patient-centric, such as the ability to maintain or return to employment.
Social determinants of health are strongly linked to the risk of human disease, with employment, or the lack thereof, being one of the most significant. 3 The risk of MI increases linearly with each cumulative job loss.3 Single center studies performed in the early percutaneous coronary intervention (PCI) era have shown that more than a third of MI patients are unable to return to work by 1 year.4, 5 Job loss significantly interacts with other psychosocial factors such as depression and health status; for example, depression can be both a cause and a consequence of an adverse change in employment.6 Employment status may also influence medication-taking behavior and affordability.7 However, the prevalence of adverse change in employment after MI, as well as the association between post-MI job changes and psychosocial outcomes and medication-taking behavior, have not been well investigated in a large representative US cohort.
Using data from the Treatment with Adenosine Diphosphate Receptor Inhibitors: Longitudinal Assessment of Treatment Patterns and Events after Acute Coronary Syndrome (TRANSLATE-ACS) registry8, we assessed the prevalence of adverse change in employment between baseline and 1 year post-MI in a national US cohort. We compared patient-reported depression, quality of life, medication adherence, and financial hardship affording medications between patients who experienced an adverse change in employment and those who remained working at 1 year without an adverse change.
Methods
Study Population
TRANSLATE-ACS (http://clinicaltrials.gov: NCT01088503) is a longitudinal, observational registry of patients treated for acute MI at 2333 US hospitals between April 2010 and October 2012. Details of the design and conduct of the TRANSLATE-ACS study have been previously published.8 Patients were included in the registry if they were ≥18 years of age presenting with STEMI or NSTEMI, treated with percutaneous coronary intervention (PCI) and a P2Y12 inhibitor, were not enrolled in another research study, and were able to provide written consent for longitudinal telephonic follow-up and data collection. Study enrollment received institutional review board approval at each participating hospital. Of the total 12,365 patients enrolled in 233 US hospitals, we excluded patients who died in-hospital (n=14), did not have baseline (n=98) and 1 year employment status recorded (n=2,934), resulting in a final study population of 9,319 patients for this analysis.
Data Collection and Definitions
Detailed demographic, clinical, and angiographic characteristics, in-hospital laboratory values, and adverse outcomes (as shown in Table 1) were collected for all patients using a standardized set of data elements and definitions in accordance with those used by the National Cardiovascular Data Registry CathPCI Registry.9 Centralized telephone follow-up was conducted by trained Duke Clinical Research Institute personnel for all enrolled patients at 6 weeks, and 6, 12 and 15 months after discharge. At each interview, standardized questionnaires collected interval medication changes and patient-reported outcomes using validated instruments, as described in the Outcomes section below. 10, 11
Table 1.
Differences in Characteristics and Outcomes Between Patients Working and Not Working at Baseline
| Not Working (n=4589) | Working (n=4730) | P value | |
|---|---|---|---|
| Demographics | |||
| Age, mean (years) | 65.9 (11.0) | 55.8 (9.2) | <0.001 |
| Male gender | 65.0 (2,984) | 80.3 (3796) | <0.001 |
| White race | 87.5 (4013) | 90.3 (4269) | <0.001 |
| Black race | 9.7 (446) | 6.5 (308) | <0.001 |
| Hispanic race | 3.0 (139) | 3.3 (156) | 0.46 |
| Uninsured | 12.3 (566) | 13.7 (647) | 0.063 |
| High School or beyond | 84.2 (3862) | 93.0 (4397) | <0.001 |
| Married | 60.9 (2795) | 70.3 (3327) | <0.001 |
| Clinical Characteristics | |||
| Prior MI | 23.9 (1095) | 14.5 (684) | <0.001 |
| Prior PCI | 26.4 (1211) | 16.0 (757) | <0.001 |
| Prior CABG | 13.5 (618) | 4.9 (233) | <0.001 |
| Prior CVA/TIA | 8.0 (369) | 2.5 (118) | <0.001 |
| Peripheral artery disease | 9.1 (417) | 2.8 (130) | <0.001 |
| Prior heart failure | 8.1 (372) | 1.9 (89) | <0.001 |
| AFIB/flutter | 7.0 (322) | 2.3 (107) | <0.001 |
| Diabetes | 30.4 (1394) | 19.9 (942) | <0.001 |
| Hypertension | 74.7 (3428) | 58.7 (2777) | <0.001 |
| Chronic lung disease | 13.3 (610) | 4.7 (222) | <0.001 |
| Current/recent smoker | 31.9 (1462) | 38.7 (1828) | <0.001 |
| In-hospital Characteristics | |||
| ST-Elevation MI | 46.9 (2151) | 57.2 (2705) | <0.001 |
| Cardiac arrest during admission | 2.6 (120) | 3.8 (178) | 0.002 |
| Cardiogenic shock during admission | 1. 8 (83) | 2.1 (101) | 0.287 |
| Multivessel disease | 53.7 (2463) | 44.9 (2125) | <0.001 |
| Body mass index, mean | 29.9 (6.7) | 30.5 (6.2) | <0.001 |
| Creatinine clearance, mean | 65.8 (28.7) | 82.47 (24.6) | <0.001 |
| Ejection Fraction, mean | 50.5 (11.3) | 51.4 (10.8) | <0.001 |
| Length of stay, mean | 3.2 (2.3) | 2.9 (1.8) | <0.001 |
| 1-Year Post-Discharge Course | |||
| Recurrent MI | 5.5 (252) | 2.5 (120) | <0.001 |
| Unplanned Revascularization | 10.9 (502) | 8.5 (401) | <0.001 |
| Stroke | 1.0 (44) | 0.3 (15) | <0.001 |
| BARC 2+ bleed | 22.8 (1046) | 18.3 (865) | <0.001 |
| # of All-cause unplanned hospitalizations, mean | 0.0 (1.2) | 0.4 (0.8) | <0.001 |
Values presented as %(n) or mean (standard deviation) where indicated. Abbreviations: AFIB – atrial fibrillation, CABG – coronary artery bypass grafting, CVA – cerebrovascular accident, MI – myocardial infarction, PCI – percutaneous coronary intervention, PHQ - patient health questionnaire, TIA – transient ischemic attack
Patients were asked about their work status at the 1-year interview. Those who reported working “full-time” or “part-time” were defined as working. We defined an “adverse change in employment” as patients who reported working immediately before the index MI hospitalization, but were either no longer working or working less hours 1 year later. Patients no longer working at 1 year included those who reporting being laid off, disabled, on sick leave, retired or unemployed for other or non-specified reasons.
Hospital bills were collected for all subsequent hospital visits involving at least one overnight stay, including inpatient or observation status admission.12 Medical records were collected to permit independent physician adjudication of recurrent MI, coronary revascularization procedures, stroke, and bleeding events occurring within 1 year post-MI. Unplanned readmissions were defined as any bill-confirmed hospital visit involving at least 1 overnight stay except for hospitalizations involving an adjudicated, planned coronary revascularization within 60 days of the index PCI.
Outcomes
Outcomes of interest included depression, self-rated health status, evidence based medication (EBM) persistence13, patient-reported medication adherence14, and financial hardship associated with medication costs12. Depression and self-rated health status at baseline, 6 weeks, 6 months and 1 year post-MI were compared between patients with and without adverse change in employment. Depression was defined as a Patient Health Questionnaire score-2 score >315, and health status was measured using the EuroQoL-5 Dimensions (EQ5D) visual analog scale 11. As previously described, “persistence” was defined as percentage of patients still taking the EBMs prescribed at discharge at the 1-year interview.13 These EBMs included aspirin, P2Y12 inhibitors, statins, beta blockers, and angiotensin-converting enzyme inhibitors/angiotensin-receptor blockers (ACE/ARB). Consistent with prior work, patient-reported medication adherence was a summed score based on 3 questions asked during the 1 year interview14; the score ranged from 0 to 3 where 0 indicates optimal adherence: 1) Do you sometimes forget heart medications? Yes = 1, No = 0; 2) How often do you have difficulty remembering to take all your heart medications? Never = 0, all other answers = 1; 3) Do you know what to do if you run out of medication? Yes = 0, No =1. Patients were asked to rank on a scale of 1 to 5 the financial hardship of their monthly medication cost (1=no hardship, 2=minimal hardship, 3=moderate hardship, 4=much hardship, 5=extreme hardship). Financial hardship was defined as a score >2.
Statistical Analysis
We compared patient characteristics between patients working at baseline and not working at baseline, and then among those working at baseline, those with and without an adverse change in employment by 1 year. Categorical variables were presented as frequencies (percentages) and differences between the groups were assessed using the Chi-Square test. Continuous variables are presented as mean with standard deviation (SD) and were compared using the Wilcoxon rank-sum test. Changes in depression and EQ5D VAS over time were compared among patients who experienced adverse change in employment, patients who retained employment, and patients who were not employed or retired at baseline. We calculated p trends for changes in EQ5D VAS and PHQ2 >3 over time from baseline to 6 months to 1 year post-MI.
We used logistic regression to assess factors associated with adverse change in employment status at 1 year post-discharge. The variable list, adapted from prior research based on clinical judgment 4, 16–18 included the following variables: Age, sex, race, Hispanic ethnicity, insurance status, education level, marital status, diabetes, hypertension, smoking, body mass index, prior MI, prior PCI, prior coronary artery bypass graft surgery, prior stroke/transient ischemic attack, peripheral arterial disease, atrial fibrillation/flutter, chronic lung disease, STEMI, multivessel disease, multivessel PCI, creatinine clearance, ejection fraction ≤40%, length of index stay, presentation or in-hospital development of heart failure signs/symptoms, cardiac arrest, cardiogenic shock, baseline PHQ2>3, baseline EQ5D VAS, post-discharge events within 1 year (recurrent MI, unplanned revascularization, stroke, Bleeding Academic Research Consortium [BARC] 2+ bleeding), and number of all-cause unplanned rehospitalizations. We used generalized estimating equations with exchangeable correlation structure to account for within-hospital clustering. We calculated a C-index to assess how well this model discriminated between patients with and without an adverse change in employment.
We used a similar methodology to assess the association of adverse change in employment with 1-year depression, EBM persistence, medication adherence, and financial hardship affording medications. Each model adjusted for the following variables: age, sex, race, body mass index, STEMI, prior MI, diabetes, hypertension, smoker, number of unplanned rehospitalizations in first year, BARC 2+ bleeding in first year, number of meds reported at 1 year (of aspirin, P2Y12 inhibitor, statin, beta-blocker, ACE/ARB), baseline EQ5D VAS, and baseline PHQ2. Adjusting for these same variables, we assessed the association of adverse change in employment with 1-year EQ5D VAS using linear regression with GEE.
Variables inputted into the model were missing <5%. To account for missing data, categorical variables were imputed to the mode, creatinine clearance, and ejection fraction were imputed using medians and body mass index was imputed using gender and STEMI vs. NSTEMI specific medians. We did not impute clinical outcomes. In all instances, p<0.05 was considered statistically significant. All analyses were performed with SAS version 9.2 (Cary, NC).
Results
In the final study population of 9,319 patients, the mean age was 55.8 years (SD 9.2) and 27.3% were female; more than half (n=4,730, 51%) were working at the time of their index MI. (Figure 1) Patients not working at baseline were more likely to be older, black, female, unmarried and not have graduated high school. (Table 1) They were more likely to have medical comorbidities than patients who were working. Most patients not working at baseline were retired (n=3355, 73%). Patients working at baseline were more likely to smoke and to present with STEMI or have a cardiac arrest during the index MI hospitalization.
Figure 1.
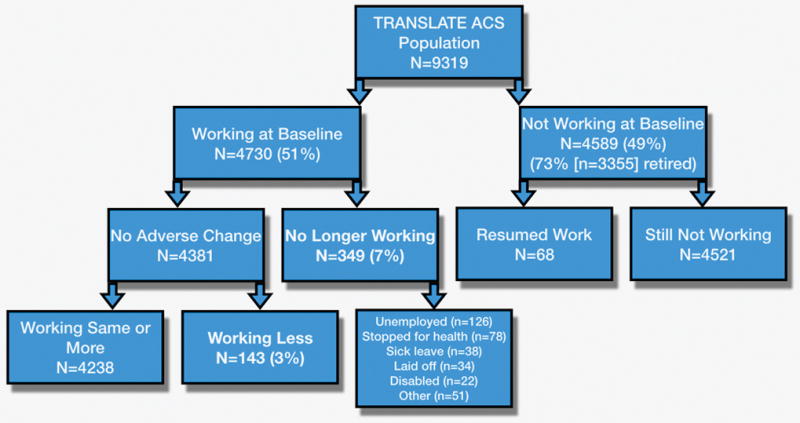
Distribution of Patients by Baseline Employment Status and Change After MI.
Changes in Work Status
Among patients working at baseline, 10% (n=492) reported an adverse change in employment 1 year later, with 7% (n=349) no longer working while 3% (n=143) reported working less. (Figure 1) Only 27 of those with an adverse change in employment reported retirement; 172 patients (49% of patients no longer working) reported involuntary job loss such as being laid off or no longer working due to their health and disability.
Patients who experienced an adverse change in employment post-MI were more likely to be female, have diabetes, hypertension, tobacco use and were less likely to have a drug eluting stent placed than patients who continued working as before. (Table 2) Patients with an adverse change in employment were more likely to have recurrent MI, unplanned revascularization, stroke and BARC2+ bleeding than patients who were still working. (Table 2)
Table 2.
Differences in Characteristics and Outcomes Between Patients With or Without Adverse Change in Employment within 1 Year post-discharge.
| No Adverse Change (n=4238) | Adverse Change (n=492) | P Value | |
|---|---|---|---|
| Demographics | |||
| Age, mean (years) | 55.8 (9.3) | 56.05.7 (8.7) | 0.940 |
| Male gender | 80.9 (3427) | 75.0 (369) | 0.002 |
| White race | 90.4 (3832) | 88.8 (437) | 0.189 |
| Black race | 6.4 (269) | 7.9 (39) | 0.183 |
| Hispanic race | 3.3 (141) | 3.1 (15) | 0.735 |
| Uninsured | 13.5 (571) | 15.5 (76) | 0.258 |
| High School or beyond | 92.3 (3935) | 93.9 (462) | 0.870 |
| Married | 70.8 (2999) | 66.7 (328) | 0.057 |
| Clinical Characteristics | |||
| Prior MI | 14.4 (608) | 15.5 (76) | 0.511 |
| Prior PCI | 15.9 (672) | 17.3 (85) | 0.416 |
| Prior CABG | 4.9 (206) | 5.5 (27) | 0.543 |
| Prior CVA/TIA | 2.4 (103) | 3.1 (15) | 0.402 |
| Peripheral artery disease | 2.7 (113) | 3.5 (17) | 0.311 |
| Prior heart failure | 1.8 (76) | 2.6 (13) | 0.190 |
| AFIB/flutter | 2.3 (99) | 1.6 (8) | 0.318 |
| Diabetes | 19.4 (823) | 24.2 (119) | 0.012 |
| Hypertension | 57.8 (2451) | 66.3 (326) | 0.0003 |
| Chronic lung disease | 4.7 (200) | 4.5 (22) | 0.806 |
| Current/recent smoker | 38.1 (1615) | 43.3 (213) | 0.025 |
| In-Hospital Characteristics | |||
| ST-Elevation MI | 57.0 (2417) | 58.5 (288) | 0.523 |
| Cardiac arrest on admission | 3.8 (162) | 3.3 (16) | 0.510 |
| Cardiogenic shock | 2.2 (92) | 1.8 (9) | 0.604 |
| Multivessel disease | 44.8 (1900) | 45.7 (225) | 0.831 |
| Multivessel PCI | 9.8 (414) | 9.2 (45) | 0.652 |
| Drug eluting stent used | 75.1 (3184) | 69.9 (344) | 0.010 |
| Body mass index, mean | 30.4 (6.0) | 31.1 (7.1) | 0.084 |
| Creatinine clearance, mean | 82.6 (24.5) | 81.8 (25.8) | 0.315 |
| Ejection Fraction, mean | 51.4 (10.7) | 50.9 (11.5) | 0.652 |
| Length of stay, mean (days) | 2.9 (1.8) | 3.0 (1.7) | 0.114 |
| EQ5D VAS Score, mean | 73.5 (17.5) | 70.7 (19.7) | 0.013 |
| PHQ2 >3 | 4.5 (189) | 6.5 (32) | 0.042 |
| 1-Year Post-Discharge Course | |||
| Recurrent MI w/in 1 year | 2.2 (91) | 5.9 (29) | <0.001 |
| Unplanned Revas w/in 1 year | 7.9 (333) | 13.8 (68) | <0.001 |
| Stroke w/in 1 year | 0.3 (11) | 0.8 (4) | 0.039 |
| BARC 2+ bleed w/in 1 year | 17.6 (745) | 24.4 (120) | <0.001 |
| # of unplanned hospitalizations, mean | 0.4 (0.8) | 0.6 (1.1) | <0.001 |
Values presented as %(n) or mean (standard deviation) where indicated. Abbreviations: AFIB – atrial fibrillation, CABG – coronary artery bypass grafting, CVA – cerebrovascular accident, MI – myocardial infarction, PCI – percutaneous coronary intervention, PHQ - patient health questionnaire, TIA – transient ischemic attack
In multivariable analysis, the strongest factor associated with adverse change in employment in the 1 year after discharge was the number of readmissions within the first year (OR 1.20, 95% CI 1.09–1.32 per event). Other factors significantly associated with adverse change in employment include baseline smoking status, hypertension, and post-discharge bleeding (Table 3). Notably, factors, such as sex, baseline health status, and recurrent MI were significant in unadjusted comparisons, but did not remain significantly associated with adverse change in employment in the multivariable model.
Table 3.
Factors associated with adverse change in employment status at 1 year
| Adjusted | |||
|---|---|---|---|
| Parameter | OR (95% CI) | Wald Chi-Square Test Statistic | P-value |
| # of Unplanned Readmissions per 1 increase | 1.20 (1.09, 1.32) | 13.20 | 0.0003 |
| BARC 2+ bleed w/in 1 year | 1.39 (1.13, 1.72) | 9.34 | 0.0022 |
| Hypertension | 1.33 (1.08, 1.65) | 7.12 | 0.0076 |
| Smoker | 1.28 (1.04, 1.57) | 5.28 | 0.0215 |
| Recurrent MI w/in 1 year | 1.64 (0.99, 2.71) | 3.64 | 0.0563 |
| Female vs. Male | 1.23 (0.98, 1.56) | 3.15 | 0.0757 |
| BMI per 5 increase | 1.07 (0.99, 1.16) | 3.07 | 0.0798 |
| Baseline EQ5D VAS per 10 unit decrease | 1.04 (0.99, 1.10) | 2.83 | 0.0927 |
| Unplanned Revascularization w/in 1 year | 1.30 (0.95, 1.79) | 2.65 | 0.1038 |
Factors with p≤0.1 shown. Additional nonsignificant parameters included stroke within 1 year, EF <40%, insurance status, chronic lung disease, atrial fibrillation, STEMI vs. NSTEMI, cardiac arrest, ethnicity, education, creatinine clearance, age, diabetes, marital status, cardiogenic shock, prior CABG, multivessel PCI, prior stroke/transient ischemic attack, any heart failure, peripheral arterial disease, prior MI, multivessel disease, length of stay and prior PCI. Adjusted model c-index = 0.63. Abbreviations: BMI – body mass index, CABG – coronary artery bypass grafting, CI – confidence interval, EF – ejection fraction, OR – odds ratio, PCI – percutaneous coronary intervention, VAS – visual analog scale
Outcomes
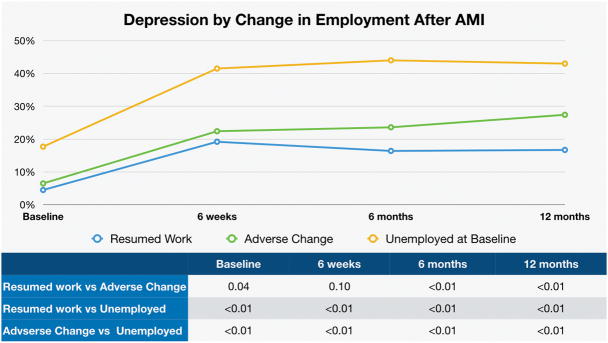
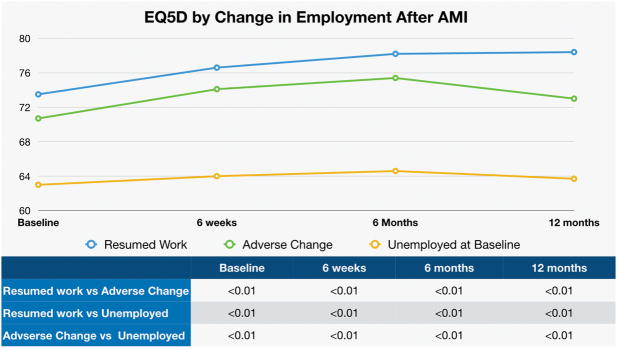
Patients experiencing an adverse change in employment were more likely to have depression at baseline compared with those experiencing no change (6.5% vs. 4.5%, p=0.04); these differences widened at 6 weeks (22.4% vs. 19.2%, p=0.1), 6 months (23.6% vs. 16.4%, p<0.001) and 1 year (27.4% vs. 16.7%, p<0.001, Figure 2A) in part due to observed improvement among patients who resumed work. The difference in depression over time was significant between patients who experienced an adverse change in employment and those who resumed work: p<0.001. Patients not working at baseline, not retired and who did not resume working at 1 year had significantly higher rates of depression throughout study period. Patients with an adverse change in employment also had lower self-rated health status (EQ5D VAS) than those not experiencing any adverse change (70.7 [SD 19.7] vs. 73.5 [17.5] at baseline, 74.1 [SD 16.2] vs. 76.7 [SD 15.3] at 6 weeks, 75.4 [SD 15.8] vs. 78.2 [SD 15.0] at 6 months, 73.0 [SD 17.8] vs. 78.4 [SD 14.8] at 1 year, all p≤0.01, Figure 2B). Patients not working at baseline, not retired and who did not resume working at 1 year had significantly poorer EQ5D VAS scores throughout the study period. Change in EQ5D VAS score over time was significant only for patients working at baseline with no adverse change within the next year (p<0.001); these patients experienced improvement in quality of life over time.
Figure 2.
Change in (A) depression (PHQ2>3) and (B) self-rated health status (EQ5D VAS) after MI amongst patients by employment status change. P values show significance of differences in PHQ2>3 amongst patient groups at baseline and followup.
At 1 year, patients with adverse changes in employment were more likely to have PHQ2 score>3 suggestive of depression and lower EQ5D VAS scores suggestive of lower quality of life in both unadjusted and adjusted comparisons (Table 4). No difference was noted in patient-reported medication adherence or in persistence of EBMs prescribed at discharge. However, more patients who had adverse change in employment reported moderate-extreme financial hardship with out of pocket medication costs than those without change in work status after adjustment for clinical and sociodemographic characteristics (Table 4).
Table 4.
Outcomes at 1 year.
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Adverse employment change (n=492) | No adverse change (n=4238) | P value | HR (95% CI) | |
| PHQ2 depression score >3 | 27.4% | 16.7% | <0.001 | 1.60 (1.27, 2.02) |
| EQ5D Visual Analog Scale | 73 (17.8) | 78 (14.8) | <0.001 | −3.23 (−4.73, −1.74)* |
| Medication adherence | 68.0% | 70.6% | 0.226 | 1.15 (0.93, 1.41) |
| Medication persistence | ||||
| • P2Y12 inhibitors | 86.1% | 88.2% | 0.185 | 0.88 (0.68, 1.14) |
| • Aspirin | 95.3% | 96.3% | 0.239 | 0.86 (0.53, 1.40) |
| • Statins | 86.1% | 88.3% | 0.178 | 0.87 (0.67, 1.13) |
| • Beta-blockers | 86.0% | 87.0% | 0.565 | 0.91 (0.70, 1.17) |
| • ACEi/ARB | 78.0 | 81.4% | 0.116 | 0.80 (0.63, 1.02) |
| Moderate/extreme financial hardship with medication costs | 41.0% | 28.4% | <0.001 | 1.57 (1.33, 1.87) |
Continuous variables expressed as mean (standard deviation). Adjusted for age, sex, race, BMI, MI type, prior MI, diabetes, hypertension, smoking, unplanned rehospitalizations in first year, BARC 2+ bleeding in first year, number of medications reported at 1 year, baseline EQ5D VAS, baseline PHQ2. *Linear regression results expressed as estimate (95% CI)
Abbreviations: ACEi – angiotensin converting enzymes inhibitor, ARB – angiotensin receptor blocker, CI – confidence interval, HR – hazard ratio
Discussion
This study sheds novel insights into patients’ ability to return to work after MI. We found that 1 in 10 patients working at baseline had an adverse change in employment at 1 year; 7% were unable to return to work and 3% worked less. Almost half of job losses were described by the patient as involuntary. An adverse change in employment was associated with increased risk of depression, lower self-rated health status and increased financial hardship associated with affording medications. These findings have important implications for patient-centered care for MI patients.
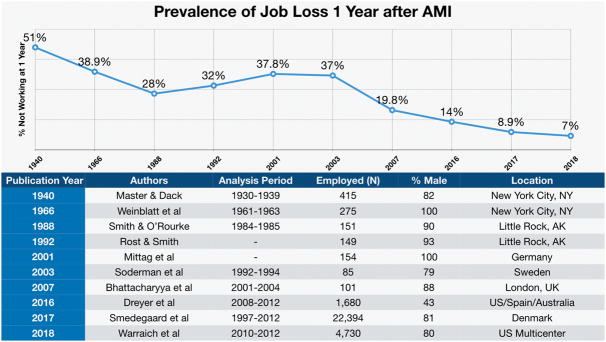
A key finding of this analysis is the very low rate of adverse change in employment after MI. Improvements in treatments for MI, in addition to causing dramatic reductions in total and age-adjusted mortality after MI, have also resulted in significant improvements in patient functionality after MI. We hypothesize that advances in MI care have also resulted in improvement in patients’ ability to resume employment. In comparison with prior literature, we now observe a substantially lower rate of job loss within 1 year after MI.4, 5, 16–22 In fact, our study demonstrates the lowest rate of adverse change in employment at 1 year amongst MI patients to date (Figure 3). These findings thus represent commendable translation of clinical outcomes into patient-centered measures, representing additional crucial protection for patients from the financial hardship associated with medical care. However, this progress must not deter efforts to target patients who are at high risk for job loss with psychosocial and occupational interventions during the initial episode of care for MI. In our study, factors that were associated with the greatest chance of work loss were unplanned hospitalizations, bleeding, hypertension and smoking status. Finally, similar to prior studies, we demonstrate that patients unemployed at baseline are at risk for poorer outcomes after MI.3
Figure 3.
Prevalence of job loss at 1 year after MI. Authors review of historical literature that reported prevalence of job loss at 12 months after acute MI.4, 5, 16–22
Depression occurs commonly after MI and our data suggests that an adverse change in employment is associated with higher rates of depression. Rates of depression increase after MI for all patient groups, however, patients able to resume work actually demonstrate a reduction in rates of depression while those who are unable to resume work see a continuously rising trend in prevalence of depression. Rates of depression in patients unable to resume work begin to approach those who are unemployed and not retired at baseline by 1 year.3 Furthermore, patients with depression remain at high risk for losing employment even after they return to work. In a recently published nationwide study from Denmark analyzing factors associated with inability to maintain work after despite resumption of work within a 1 year post-MI, depression was the strongest predictor of subsequent detachment from work.22 In our analysis, however, while depression was slightly higher at baseline amongst patients who experienced adverse change in employment (6.5% vs. 4.5%, p=0.04), depression was not a significant predictor of adverse change in our adjusted model.
Patients who experience an adverse change in employment also experience poorer quality of life. Self-rated health, in addition to reflecting a poor sense of physical and emotional well being, is also a sensitive marker of adverse clinical outcomes, and is associated with increased mortality.23 While self-rated health improved steadily for patients who resumed work (p trend <0.001), it did not do so for patients unemployed at baseline or who were unable to resume work (p trend non-significant). These outcomes become increasingly important given their importance to patients and improvements in clinical outcomes such as mortality.
These associations underscore the importance of this patient-centered outcome and raise several questions. Can we predict or prevent adverse changes in employment? Our data suggests that the factor most strongly associated with job loss was unplanned readmissions. Prevention of post-MI readmission has been the focus of national quality improvement initiatives in recent years.24 Patients who experienced a bleeding complication also had a higher likelihood of experiencing adverse change in employment. Risk scores to identify patients at high risk of bleeding have been proposed to assist in antiplatelet medication selection and long-term management.25, 26 Treating depression in patients post-MI has been known to lower depression and improve quality of life, but not cardiovascular outcomes, it remains unknown if behavioral or pharmacotherapeutic interventions result in an improved ability to return to work.27
Unemployment is known to reduce medication adherence,28 another important factor affecting outcomes in patients after MI.29 In our study, we examined medication-taking in 2 ways: persistence assesses both clinician and patient continuation of evidence-based medications, whereas adherence describes the patient’s medication-taking behavior. While adverse change in employment did not result in a significant difference in medication persistence or adherence in our study, we did find increased financial hardship reported amongst those whose work status was adversely affected. Financial hardship associated with medications has been shown in prior studies to lead to reduced long-term adherence and worse medical outcomes amongst post-MI patients.30
Our study has several limitations. The precise timing of work loss/reduction could not be analyzed. Unmeasured factors may contribute to adverse change in employment. Medication adherence was patient self-reported based on a questionnaire, and may be overestimated. While financial hardship was assessed, specific impact of adverse change in employment on household income could not be examined as ~43% of patients declined to provide information about income level. Income levels are poorly reported in many observational studies and can be weighted towards both patients with high or low socioeconomic status.31 Given the observational nature of this study, we cannot make inferences regarding causality when examining outcomes. Lastly, we included patients who retired (n=27) into those experiencing as adverse change in employment given that health shocks such as MI are associated with early retirement decisions.32, 33
In conclusion, our study shows that the lowest levels of job loss in the context of prior studies of MI patients. However, almost half of job losses were involuntary. Patients who experience an adverse change in employment are at increased risk of depression, lower quality of life, and increased financial hardship with medication costs compared to those who continue working. Unplanned rehospitalizations and post-MI bleeding are the strongest predictors of adverse change in employment, increasing the impetus to reduce the incidence of these adverse outcomes. These results underscore the need for interventions to address this patient-centered outcome and its health impact.
Supplementary Material
What Is Known
Clinical outcomes of acute myocardial infarction have experienced sustained improvement over the past several decades.
Acute myocardial infarction, historically, has had a profoundly adverse experience on patients’ ability to resume full employment.
What This Study Adds
In a more contemporary national US population, adverse change in employment only affects one in ten patients after acute myocardial infarction.
Bleeding after cardiac catheterization and unplanned rehospitalization are the factors most strongly associated with adverse change in employment after acute myocardial infarction.
Patients who experience adverse change in employment have worse health status, depression and hardship affording medications than patients who do not experience adverse change in employment.
Acknowledgments
Sources of Funding: The TRANSLATE-ACS (NCT01088503) registry was sponsored by Daiichi Sankyo, Inc. and Lilly USA. The Duke Clinical Research Institute is the coordinating center for this study, which represents a collaborative effort with the American College of Cardiology. This analysis was funded in part by a U01HL107023 grant from the National Heart, Lung, and Blood Institute.
none.
Footnotes
Disclosures: Dr Warraich and Ms Kaltenbach have no disclosures. Dr Fonarow reports being a consultant to Eli Lilly, Novartis, and Janssen. Dr Peterson reports grant support from American College of Cardiology, American Heart Association, and Janssen; and consulting from Bayer, Boehringer Ingelheim, Merck, Valeant, Sanofi, Astra Zeneca, Janssen, Regeneron, and Genentech. Dr Wang reports research funding from AstraZeneca, Gilead, Lilly, The Medicines Company, NIH and Canyon Pharmaceuticals (all significant); educational activities or lectures (generates money for Duke) for AstraZeneca (modest); consulting (including CME) for Medco (modest); and American College of Cardiology (significant).
References
- 1.Writing Group M; Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB American Heart Association Statistics C, Stroke Statistics S. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38–60. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. The New England journal of medicine. 2010;362:2155–65. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 3.Dupre ME, George LK, Liu G, Peterson ED. The cumulative effect of unemployment on risks for acute myocardial infarction. Archives of internal medicine. 2012;172:1731–7. doi: 10.1001/2013.jamainternmed.447. [DOI] [PubMed] [Google Scholar]
- 4.Mittag O, Kolenda KD, Nordman KJ, Bernien J, Maurischat C. Return to work after myocardial infarction/coronary artery bypass grafting: patients’ and physicians’ initial viewpoints and outcome 12 months later. Soc Sci Med. 2001;52:1441–50. doi: 10.1016/s0277-9536(00)00250-1. [DOI] [PubMed] [Google Scholar]
- 5.Soderman E, Lisspers J, Sundin O. Depression as a predictor of return to work in patients with coronary artery disease. Soc Sci Med. 2003;56:193–202. doi: 10.1016/s0277-9536(02)00024-2. [DOI] [PubMed] [Google Scholar]
- 6.Andreeva E, Hanson LLM, Westerlund H, Theorell T, Brenner MH. Depressive symptoms as a cause and effect of job loss in men and women: evidence in the context of organisational downsizing from the Swedish Longitudinal Occupational Survey of Health. Bmc Public Health. 2015:15. doi: 10.1186/s12889-015-2377-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kronish IM, Rieckmann N, Burg MM, Alcantara C, Davidson KW. The Psychosocial Context Impacts Medication Adherence After Acute Coronary Syndrome. Ann Behav Med. 2014;47:158–164. doi: 10.1007/s12160-013-9544-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chin CT, Wang TY, Anstrom KJ, Zhu B, Maa JF, Messenger JC, Ryan KA, Davidson-Ray L, Zettler M, Effron MB, Mark DB, Peterson ED. Treatment with adenosine diphosphate receptor inhibitors-longitudinal assessment of treatment patterns and events after acute coronary syndrome (TRANSLATE-ACS) study design: expanding the paradigm of longitudinal observational research. Am Heart J. 2011;162:844–51. doi: 10.1016/j.ahj.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 9.Moussa I, Hermann A, Messenger JC, Dehmer GJ, Weaver WD, Rumsfeld JS, Masoudi FA. The NCDR CathPCI Registry: a US national perspective on care and outcomes for percutaneous coronary intervention. Heart. 2013;99:297–303. doi: 10.1136/heartjnl-2012-303379. [DOI] [PubMed] [Google Scholar]
- 10.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10:348–54. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Ellis JJ, Eagle KA, Kline-Rogers EM, Erickson SR. Validation of the EQ-5D in patients with a history of acute coronary syndrome. Curr Med Res Opin. 2005;21:1209–16. doi: 10.1185/030079905X56349. [DOI] [PubMed] [Google Scholar]
- 12.Hess CN, Wang TY, McCoy LA, Messenger JC, Effron MB, Zettler ME, Henry TD, Peterson ED, Fonarow GC. Unplanned Inpatient and Observation Rehospitalizations After Acute Myocardial Infarction: Insights From the Treatment With Adenosine Diphosphate Receptor Inhibitors: Longitudinal Assessment of Treatment Patterns and Events After Acute Coronary Syndrome (TRANSLATE-ACS) Study. Circulation. 2016;133:493–501. doi: 10.1161/CIRCULATIONAHA.115.017001. [DOI] [PubMed] [Google Scholar]
- 13.Mathews R, Wang TY, Honeycutt E, Henry TD, Zettler M, Chang M, Fonarow GC, Peterson ED Investigators T-AS. Persistence with secondary prevention medications after acute myocardial infarction: Insights from the TRANSLATE-ACS study. Am Heart J. 2015;170:62–9. doi: 10.1016/j.ahj.2015.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rymer J, McCoy L, Anstrom K, Fonarow G, Erskine N, Peterson E, Wang T. Hospital Evaluation of Health Literacy and Associated Outcomes in Patients After Acute Myocardial Infarction. Am Heart J. 2017 doi: 10.1016/j.ahj.2017.08.024. https://doi.org/10.1016/j.ahj.2017.08.024. [DOI] [PubMed]
- 15.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 16.Bhattacharyya MR, Perkins-Porras L, Whitehead DL, Steptoe A. Psychological and clinical predictors of return to work after acute coronary syndrome. Eur Heart J. 2007;28:160–5. doi: 10.1093/eurheartj/ehl440. [DOI] [PubMed] [Google Scholar]
- 17.Dreyer RP, Xu X, Zhang W, Du X, Strait KM, Bierlein M, Bucholz EM, Geda M, Fox J, D’Onofrio G, Lichtman JH, Bueno H, Spertus JA, Krumholz HM. Return to Work After Acute Myocardial Infarction: Comparison Between Young Women and Men. Circulation Cardiovascular quality and outcomes. 2016;9:S45–52. doi: 10.1161/CIRCOUTCOMES.115.002611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinblatt E, Shapiro S, Frank CW, Sager RV. Return to work and work status following first myocardial infarction. Am J Public Health Nations Health. 1966;56:169–85. doi: 10.2105/ajph.56.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Master AM, Dack S. Rehabilitation Following Acute Coronary Artery Occlusion. JAMA. 1940;115:828–832. [Google Scholar]
- 20.Smith GR, Jr, O’Rourke DF. Return to work after a first myocardial infarction. A test of multiple hypotheses. JAMA. 1988;259:1673–7. [PubMed] [Google Scholar]
- 21.Rost K, Smith GR. Return to work after an initial myocardial infarction and subsequent emotional distress. Archives of internal medicine. 1992;152:381–5. [PubMed] [Google Scholar]
- 22.Smedegaard L, Nume AK, Charlot M, Kragholm K, Gislason G, Hansen PR. Return to Work and Risk of Subsequent Detachment From Employment After Myocardial Infarction: Insights From Danish Nationwide Registries. Journal of the American Heart Association. 2017;6:e006486. doi: 10.1161/JAHA.117.006486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol. 1997;50:517–28. doi: 10.1016/s0895-4356(97)00045-0. [DOI] [PubMed] [Google Scholar]
- 24.United States Department of Health and Human Services. [Accessed March 2018];Centers for Medicare and Medicaid Services Readmissions Reduction Program. Published 2017: https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html.
- 25.Mathews R, Peterson ED, Chen AY, Wang TY, Chin CT, Fonarow GC, Cannon CP, Rumsfeld JS, Roe MT, Alexander KP. In-hospital major bleeding during ST-elevation and non-ST-elevation myocardial infarction care: derivation and validation of a model from the ACTION Registry(R)-GWTG. Am J Cardiol. 2011;107:1136–43. doi: 10.1016/j.amjcard.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 26.Yeh RW, Secemsky EA, Kereiakes DJ, Normand SL, Gershlick AH, Cohen DJ, Spertus JA, Steg PG, Cutlip DE, Rinaldi MJ, Camenzind E, Wijns W, Apruzzese PK, Song Y, Massaro JM, Mauri L Investigators DS. Development and Validation of a Prediction Rule for Benefit and Harm of Dual Antiplatelet Therapy Beyond 1 Year After Percutaneous Coronary Intervention. JAMA. 2016;315:1735–49. doi: 10.1001/jama.2016.3775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen BE, Edmondson D, Kronish IM. State of the Art Review: Depression, Stress, Anxiety, and Cardiovascular Disease. Am J Hypertens. 2015;28:1295–302. doi: 10.1093/ajh/hpv047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PloS one. 2013;8:e62775. doi: 10.1371/journal.pone.0062775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bansilal S, Castellano JM, Garrido E, Wei HG, Freeman A, Spettell C, Garcia-Alonso F, Lizano I, Arnold RJ, Rajda J, Steinberg G, Fuster V. Assessing the Impact of Medication Adherence on Long-Term Cardiovascular Outcomes. Journal of the American College of Cardiology. 2016;68:789–801. doi: 10.1016/j.jacc.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 30.Choudhry NK, Avorn J, Glynn RJ, Antman EM, Schneeweiss S, Toscano M, Reisman L, Fernandes J, Spettell C, Lee JL, Levin R, Brennan T, Shrank WH Post-Myocardial Infarction Free Rx E, Economic Evaluation T. Full coverage for preventive medications after myocardial infarction. The New England journal of medicine. 2011;365:2088–97. doi: 10.1056/NEJMsa1107913. [DOI] [PubMed] [Google Scholar]
- 31.Kim S, Egerter S, Cubbin C, Takahashi ER, Braveman P. Potential implications of missing income data in population-based surveys: an example from a postpartum survey in California. Public Health Rep. 2007;122:753–63. doi: 10.1177/003335490712200607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Topa G, Depolo M, Alcover CM. Early Retirement: A Meta-Analysis of Its Antecedent and Subsequent Correlates. Front Psychol. 2017;8:2157. doi: 10.3389/fpsyg.2017.02157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Rijn RM, Robroek SJ, Brouwer S, Burdorf A. Influence of poor health on exit from paid employment: a systematic review. Occup Environ Med. 2014;71:295–301. doi: 10.1136/oemed-2013-101591. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.