Abstract
To date structure-activity relationship (SAR) studies of the dynorphins (Dyn), endogenous peptides for kappa opioid receptors (KOR), have focused almost exclusively on Dyn A with minimal studies on Dyn B. While both Dyn A and Dyn B have identical N-terminal sequences, their C-terminal sequences differ which could result in differences in pharmacological activity. We performed an alanine scan of the non-glycine residues up through residue 11 of Dyn B amide to explore the role of these side chains in the activity of Dyn B. The analogs were synthesized by fluorenylmethyloxycarbonyl (Fmoc)-based solid phase peptide synthesis and evaluated for their opioid receptor affinities and opioid potency and efficacy at KOR. Similar to Dyn A the N-terminal Tyr1 and Phe4 residues of Dyn B amide are critical for opioid receptor affinity and KOR agonist potency. The basic residues Arg6 and Arg7 contribute to the KOR affinity and agonist potency of Dyn B amide, while Lys10 contributes to the opioid receptor affinity, but not KOR agonist potency, of this peptide. Comparison to the Ala analogs of Dyn A(1-13) suggests that the basic residues in the C-terminus of both peptides contribute to KOR binding, but differences in their relative positions may contribute to the different pharmacological profiles of Dyn A and Dyn B. The other unique C-terminal residues in Dyn B amide also appear to influence the relative affinity of this peptide for KOR. This SAR information may be applied in the design of new Dyn B analogs that could be useful pharmacological tools.
Phrases for indexing: Dynorphin B, alanine scan, kappa opioid receptor, structure-activity relationships, C-terminal basic residues
Graphical abstract

Introduction
The dynorphins, like the other mammalian opioid endogenous peptides, are obtained by enzymatic cleavage from a precursor protein, prodynorphin.1 Prodynorphin is primarily cleaved into four larger opioid peptides, dynorphin (Dyn) A, leumorphin, and α and β-neoendorphin,2 and leumorphin is further cleaved to yield Dyn B (Figure 1). Dyn A and Dyn B were both initially isolated from porcine pituitary by Fischli and Goldstein.3-5 These prodynorphin-derived peptides, which are most abundant in the neural lobe of the rat pituitary and in the posterior pituitary, are differentially processed in various parts of the brain.2
Figure 1.
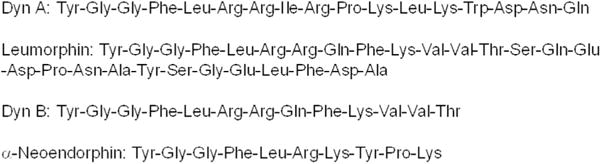
Dynorphins and related peptides derived from prodynorphin1
These prodynorphin peptides preferentially interact with kappa opioid receptors (KOR). In radioligand binding assays both peptides exhibit subnanomolar to low nanomolar affinity for KOR, with Dyn A exhibiting higher KOR affinity than Dyn B (4.7-fold higher in mouse brain preparations6 and 46-fold higher for cloned human KOR7). In mouse brain preparations, both Dyn A and Dyn B exhibited 9-fold selectivity for KOR vs. mu opioid receptors (MOR).6 In the cloned human opioid receptors, Dyn B exhibited 3-fold selectivity for KOR vs. MOR compared to Dyn A which exhibited 261-fold selectivity.7 Both peptides exhibit subnanomolar to low nanomolar agonist potency in the guinea pig ileum assay,8,9 and low nanomolar potency in the GTPγS assay at cloned human KOR.7
In contrast, the reported non-opioid effects of the two peptides are markedly different. Dyn A produces non-opioid effects10-12 such as hind limb paralysis13,14 and nociceptive behavior15 in rodents, effects that are resistant to naloxone but blocked by administration of an N-methyl-D-aspartate (NMDA) antagonist.16 Additionally, Dyn A has been reported to produce long lasting allodynia17,18 and hypothermia19 in rats. (Induction of hypothermia is thought to be due to a mixture of opioid and non-opioid effects of dynorphins.19) In addition, Dyn A causes cytotoxicity in non-neuronal as well as neuronal cells through a mechanism resistant to naloxone.20,21 In contrast, Dyn B did not produce nociceptive behavior15 or hypothermia19 in rats. Also unlike Dyn A, Dyn B did not produce cytotoxic effects in neuronal and non-neuronal cells in vitro.20
Differences have also been reported for membrane interactions of Dyn A and Dyn B in model systems such as phospholipid large unilamellar vesicles (LUVs)22 and in live mammalian cells.23 In phospholipid LUVs Dyn A produced membrane perturbations and induced calcein leakage, possibly by causing transient pore formation. In contrast, Dyn B did not cause membrane perturbation or calcein leakage.22 Studies of the membrane interactions of Dyn A and Dyn B with phospholipid bicelles by NMR and saturation transfer difference (STD) experiments24 showed that the N-terminus of Dyn A was inserted in the hydrophobic lipid bilayer region, as evident by changes in the NMR, while the C-terminal residues were loosely attached to the bicelle surface. In contrast, Dyn B was bound to the bilayer but did not insert into the lipid bilayer, and the NMR of the N-terminus did not change in the presence of the bicelles.24 Using fluorescence imaging, correlation spectroscopy and patch clamp techniques it was recently shown that Dyn A accumulates in the plasma membrane of live mammalian cells and causes pore formation, whereas Dyn B does not.23 These results from pharmacological and biophysical studies suggest that the non-opioid cytotoxic effects produced by Dyn A but not by Dyn B may be due in part to either transient pore formation and/or membrane perturbations.
While Dyn A and Dyn B have identical N-terminal sequences, their C-terminal sequences differ. Hence, differences in their lipid membrane interactions and non-opioid cytotoxic effects must be due to differences in their C-terminal sequences.
To date, studies involving structure-activity relationships (SAR) of dynorphins at opioid receptors have focused almost exclusively on Dyn A (see refs.25,26 for reviews). These have included novel cyclization approaches (N-terminal cyclization27,28 and ring-closing metathesis29) and antagonist analogs containing modifications in the N-terminal “message”30 sequence,27,31-36 along with some exploration of the SAR of the C-terminal sequence in these analogs.37-40 However, there has been minimal SAR evaluation of Dyn B analogs. Schiller and coworkers synthesized the Mdp1 (Mdp = (2S)-2-methyl-3-(2,6-dimethyl-4-hydroxyphenyl)propanoic acid) analog of Dyn B41 as well as of Dyn A-(1-11) amide.33 The Dyn A analog dynantin was 180-fold more potent as a KOR antagonist in the guinea pig ileum (GPI) assay than the Dyn B analog, indicating the importance of the C-terminal sequence to the potency of dynantin. This study raises questions concerning the contributions of the C-terminal residues in Dyn B vs. Dyn A to the opioid receptor affinities and opioid activity of the two peptides.
We hypothesized that unique residue(s) in the C-terminus of Dyn B interact with opioid receptors and contribute to the peptide’s opioid activity. To test this hypothesis all of the non-glycine residues up through residue 11 of Dyn B amide were substituted with Ala (Figure 2) in order to explore the contributions of these side chains to the pharmacological activity profile of Dyn B.
Figure 2.
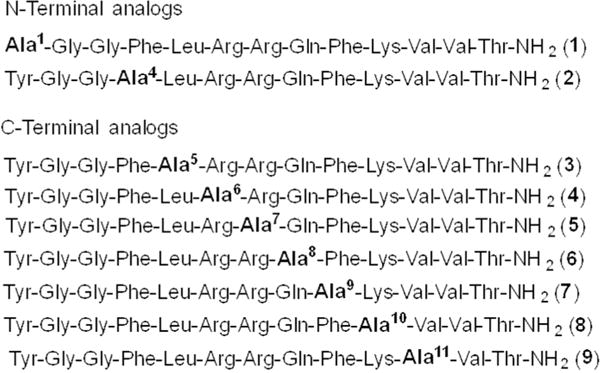
Alanine analogs of Dyn B amide
Materials and Methods
Materials
The reagents and solvents used for peptide synthesis were obtained from the sources previously reported.40
Peptide synthesis
The peptides were prepared by solid phase peptide synthesis performed on an automated CS Bio 336 peptide synthesizer. The peptides were assembled on the PAL-PEG-PS resin (0.19 mmol/g, 200 mg) using standard Fmoc synthetic strategy. The resin was swollen with 5 mL of DMF (2 × 10 min). The Fmoc group on the resin was removed using 20% piperidine in DMF (5 mL, 2 × 10 min), and the resin washed with DCM/DMF (1:1, 10 × 30 sec). The desired Fmoc-protected amino acids (4 equiv) were coupled to the resin with PyBOP, HOBt (4 equiv each) and DIEA (10 equiv) in DMF (2 mL) for 2 h. The side chains of Lys, Gln, Arg and Tyr were protected with Boc, trityl (Trt), Pbf and tert-butyl, respectively. The Fmoc deprotection of the N-terminal amino acid on the resin was repeated followed by the next coupling cycle. The deprotection-coupling cycle was repeated until the desired peptide was assembled on the resin.
The peptide resins were treated with Reagent B42 (88% TFA, 5% phenol, 5% water, and 2% TIS, 5 mL) for 2 h with occasional shaking. Subsequently, the resins were filtered and the TFA was evaporated in vacuo. Water (20 mL) was added to the residues, and the solutions lyophilized to give the crude peptides.
Purification and analysis of the peptides
The crude peptides were purified by preparative reversed phase HPLC using an LC-AD liquid chromatograph (Shimadzu) equipped with an SPD-10A VP system controller and SPD-10A VP UV-Vis detector and a Vydac C18 column (10 μ, 300 Å, 22 mm × 250 mm) equipped with a Vydac C18 guard cartridge. For purification, the crude peptides (20–30 mg) were dissolved in 75–85% MeOH in water (total volume ~1.5 mL). A linear gradient of 15–50% aqueous MeCN containing 0.1% TFA over 45 min, at a flow rate of 18 mL/min, was used except as noted, and the purifications monitored at 214 nm. Peptide 3 was purified using a linear gradient of 30–50% aqueous MeOH containing 0.1% TFA over 40 min. Peptide 8 was purified using a linear gradient of 5–40% aqueous MeCN containing 0.1% TFA over 70 min with a flow rate of 15 mL/min. The purity of the final peptides was verified on a Vydac 218-TP column (5 μ, 300 Å, 4.6 mm × 50 mm) equipped with a Vydac guard cartridge on an LC-10AT VP analytical HPLC (Shimadzu) equipped with an SCL-10A VP system controller and SPD-10A VP UV-visible detector or on an Agilent 1200 series liquid chromatograph system equipped with a multiple wavelength UV-visible detector. Two systems were used for the analyses: a linear gradient of 5–50% solvent B (solvent A = aqueous 0.1% TFA and solvent B = MeCN containing 0.1% TFA) over 45 min, at a flow rate of 1 mL/min (system 1), and a linear gradient of 15–0% solvent B (solvent A = aqueous 0.1% TFA and solvent B = MeOH containing 0.1% TFA) over 45 min, also at a flow rate of 1.0 mL/min (system 2). The final purity of all peptides by both analytical systems was ≥ 98%, except for peptides 3 and 8 (see Table 1). Molecular weights of the compounds were determined by ESI-MS using a Waters-time of flight (TOF) mass spectrometer (LCT premier, Waters, Milford, MA).
Table 1.
Analytical data for the Dyn B amide analogs
| Compound | HPLC system tR (min)a | ESI-MS (m/z)b | ||
|---|---|---|---|---|
| System 1c | System 2d | Calculated | Observed | |
| 1 | 19.1 | 29.1 | 739.4 | 739.4 |
| 2 | 20.7 | 24.6 | 747.4 | 747.4 |
| 3 | 21.7e | 23.9f | 764.4 | 764.4 |
| 4 | 22.2 | 34.5 | 742.9 | 742.9 |
| 5 | 23.8 | 33.3 | 742.9 | 742.9 |
| 6 | 29.9 | 39.8 | 756.9 | 756.9 |
| 7 | 16.6 | 23.2 | 747.4 | 747.4 |
| 8 | 20.3g | 31.1 | 756.9 | 756.9 |
| 9 | 20.1 | 30.0 | 771.4 | 771.4 |
| Dyn B amide | 18.6 | 31.9 | 785.4 | 785.4 |
The purities of the peptides were ≥98% except where noted.
[M + 2H]2+
Aqueous MeCN containing 0.1% TFA.
Aqueous MeOH containing 0.1% TFA. See the Experimental section for gradient details.
97.9% purity.
Peptide 3: tR = 18.4 min and 96.2% purity using a gradient of 25–45% aqueous MeOH containing 0.1% TFA over 40 min.
95.5% purity
Pharmacological assays
Radioligand binding assays
Radioligand binding assays were performed as previously described40,43 using cloned rat KOR and MOR, and mouse DOR stably expressed separately on CHO cells and [3H]diprenorphine, [3H]DAMGO ([D-Ala2,N-MePhe4,Gly-ol]enkephalin) and [3H]DPDPE (cyclo[D-Pen2,D-Pen5]enkephalin), respectively, as radioligands. Incubations were carried out in triplicate with varying concentrations of peptides (0.1-10,000 nM) for 90 min at RT in the presence of peptidase inhibitors and 3 mM Mg2+. Nonspecific binding was determined in the presence of 10 μM unlabeled Dyn A-(1-13)NH2, DAMGO and DPDPE for KOR, MOR and DOR, respectively.
[35S]GTPγS assay
The binding of the GTP analog [35S]GTPγS to CHO cell membranes expressing cloned KOR was assayed as described previously.40,44 Incubations were carried out in triplicate with varying concentrations of peptides (0.1-10,000 nM) for 90 min at RT in the presence of peptidase inhibitors and 1 μM GDP.
IC50 values and EC50 values from the radioligand binding and [35S]GTPγS assays, respectively, were determined by nonlinear regression analysis fit to a logistic equation using Prism software (GraphPad Software Co., San Diego, CA). For the radioligand binding assays Ki values were calculated from the IC50 values using the Cheng and Prusoff equation.45
Results and Discussion
Chemistry
The peptides were synthesized by the Fmoc (9-fluorenylmethoxycarbonyl) solid phase synthetic strategy. The Dyn B amide sequences were assembled on a polyethylene glycol-polystyrene (PEG-PS) resin containing the PAL [peptide amide linker, 5-(4-Fmoc-aminomethyl-3,5-dimethoxyphenoxy)valeric acid] linker using 7-benzotriazol-1-yl-oxytripyrrolidinophosphonium hexafluorophosphate (PyBOP) and 1-hydroxy-7-benzotriazole (HOBt) as the coupling agents and N,N-diisopropylethylamine (DIEA) as the base. The side chains of Lys, Gln, Arg and Tyr were protected with tert-butyloxycarbonyl (Boc), trityl (Trt), 2,2,4,6,7-pentamethyldihydrobenzofuran-5-sulfonyl (Pbf) and tert-butyl (tBu) groups, respectively. The peptides were assembled using cycles consisting of Fmoc deprotection and Fmoc-amino acid coupling. The crude peptides were cleaved from the resin using Reagent B42 (trifluoroacetic acid (TFA) in the presence of scavengers).
The peptides were isolated following TFA cleavage and purified according to standard procedures (see the Experimental section). The Dyn B amide analogs are hydrophobic and required organic solvent for solubilization of the peptides prior to purification by reversed phase high performance liquid chromatography (RP-HPLC). MeOH, which is a weaker solvent for RP-HPLC than MeCN, was used to assist in peptide dissolution while minimizing the impact on the chromatography.
Pharmacological activity
The opioid receptor binding affinities of the alanine substituted analogs of Dyn B amide were determined in Chinese hamster ovary (CHO) cell membranes expressing cloned rat MOR and KOR and mouse delta opioid receptors (DOR) (Table 2). As expected, the aromatic residues in positions 1 and 4 in the N-terminal sequence of Dyn B amide are critical for its opioid receptor affinities. Substitution of Ala in position 1 caused a 141-fold decrease, while substitution in position 4 caused a 240-fold decrease in the KOR binding affinity compared to Dyn B amide. The Ala1 and Ala4 analogs also exhibited 81- and 129-fold decreases, respectively, in MOR binding affinity and showed minimal affinity for DOR, indicating that these two residues are critical for binding to all three receptors.
Table 2.
Opioid binding affinities of Dyn B amide alanine analogs.
| Tyr1-Gly-Gly-Phe4-Leu5-Arg6-Arg7-Gln8-Phe9-Lys10-Val11-Val-Thr-NH2 | ||||
|---|---|---|---|---|
|
| ||||
| Compound | Ki (nM ± SEM)a | |||
| KOR | MOR | DOR | KOR/MOR/DOR | |
| N-Terminal alanine substituted analogs | ||||
| 1 [Ala1] | 886 ± 123 | 651 ± 70 | >10,000 | 1/0.7/>11 |
| 2 [Ala4] | 1510 ± 221 | 1040 ± 100 | >10,000 | 1/0.7/>6 |
| C-Terminal alanine substituted analogs | ||||
| 3 [Ala5] | 12.1 ± 5.2 | 20.3 ± 3.1 | 265 ± 43 | 1/2/22 |
| 4 [Ala6] | 43.1 ± 2.8 | 14.1 ± 3.0 | 25.7 ± 1.6 | 1/0.3/0.6 |
| 5 [Ala7] | 82.4 ± 9.3 | 16.7 ± 5.1 | 67.5 ± 8.3 | 1/0.2/0.8 |
| 6 [Ala8] | 13.0 ± 0.96 | 4.32 ± 0.10 | 54.0 ± 6.9 | 1/0.3/4 |
| 7 [Ala9] | 11.3 ± 1.7 | 3.76 ± 0.22 | 42.1 ± 2.5 | 1/0.3/4 |
| 8 [Ala10] | 31.6 ± 6.0 | 40.5 ± 3.9 | 119 ± 16 | 1/0.8/4 |
| 9 [Ala11] | 12.4 ± 1.6 | 7.45 ± 2.69 | 58.8 ± 3.4 | 1/0.6/5 |
| Dyn B amide | 6.30 ± 1.68 | 8.05 ± 2.87 | 43.2 ± 1.6 | 1/1.3/7 |
Values are mean ± SEM for n ≥ 3.
The basic residues in the C-terminal sequence all appeared to contribute to the KOR affinity of Dyn B amide. Substitutions of Ala for Arg6 and Arg7 caused 7- and 13-fold decreases in KOR binding affinity, respectively. Substitution of the C-terminal Lys10 residue by Ala caused a 5-fold decrease, suggesting that Lys10 also contributed to KOR binding. In contrast, the non-charged residues Leu5, Gln8, Phe9 and Val11 appeared to make minimal contributions to KOR affinity; substitution of any of these residues by Ala caused only about a 2-fold decrease in KOR affinity.
None of the residues in the C-terminus except Lys10 appeared to significantly contribute to the MOR affinity of Dyn B amide. The analogs with Ala substitution in position 6 or 7 displayed similar (within approximately 2-fold) MOR affinity to Dyn B amide, in contrast to the larger decreases observed in the KOR affinities of these analogs. The analogs with Ala substitution in place of the nonbasic residues in positions 5, 8, 9 or 11 also displayed similar MOR affinities to the parent peptide, with substitution of residue 8 or 9 resulting in the highest MOR affinity, 2-fold higher than Dyn B amide. Because of the direction and magnitude of the changes of the MOR and KOR affinities, the selectivity of analogs with Ala substitution in positions 6 to 9 switched to a small preference for MOR over KOR. Interestingly, the analog with substitution of the Lys residue in position 10 showed a 5-fold decrease in MOR affinity, suggesting that this residue made a contribution to the MOR affinity of Dyn B amide.
Most of the residues in the C-terminus, except those in positions 5 and 10, did not appear to contribute to the DOR affinity of Dyn B amide. Substitution of Leu5 and Lys10 by Ala decreased DOR affinity by 6- and 3-fold, respectively, while the DOR affinities of the other analogs with an Ala substitution in the C-terminus were within 2-fold of the parent peptide. The Ala6 analog exhibited the highest DOR affinity of any of the peptides examined, although its DOR affinity was within 2-fold that of the parent peptide.
Turcotte et al. performed the Ala scan of Dyn A(1-13)46 (Table 3). Within the N-terminal sequence of this peptide Ala1 and Ala4 substitutions caused dramatic decreases in the opioid receptor binding affinity, indicating that the Tyr1 and Phe4 residues were critical for the opioid receptor affinity of this peptide.46 Among the analogs modified outside of the N-terminal tetrapeptide sequence, the Ala5 analog displayed the largest decrease (17-fold) in opioid receptor affinity, while the Ala6 and Ala7 analogs showed 7- and 4-fold decreases, respectively, in the opioid receptor affinities, suggesting that Leu5, Arg6 and Arg7 in the C-terminus contributed to opioid receptor interactions. Ala6 and Ala7 analogs of the Dyn A-(1-11) amide KOR antagonist derivatives arodyn (Ac[Phe1-3,Arg4,D-Ala8]Dyn A-(1-11)NH2)38 and zyklophin (N-benzyl-Tyr1,cyclo[D-Asp5,Dap8]Dyn A-(1-11)NH240 showed comparable decreases (3- to 18-fold) in KOR affinity. Ala9 and Ala11 analogs of Dyn A-(1–13) also showed small decreases (3-fold) in opioid receptor affinities, suggesting that the basic residues in these positions make minor contributions to opioid receptor interactions. The agonist potencies of the analogs containing Ala substitutions in positions 1 and 4 showed a similar trend in the GPI assay as found in the radioligand binding assay.46 Similarly, among the C-terminal residues positions 5, 6 and 7 contributed the most, while residues 9 and 11 also made contributions, to maintaining the agonist potency of Dyn A (1–13) at opioid receptors in the GPI assay.46
Table 3.
Opioid receptor affinities and agonist potencies of alanine analogs of Dyn A(1–13)28
| Tyr1-Gly2-Gly3-Phe4-Leu5-Arg6-Arg7-Ile8-Arg9-Pro10-Lys11-Leu-Lys | ||||
|---|---|---|---|---|
|
| ||||
| Peptide | Affinity | Agonist potency | ||
| IC50 (nM)a | Fold decreaseb | IC50 (nM)c | Fold decreaseb | |
| [Ala1] Dyn A(1-13) | 1400 ± 210 | 519 | 750 ± 30 | 1070 |
| [Ala2]- ″ | 13.5 ± 0.4 | 5 | 104 ± 32 | 149 |
| [Ala3]- ″ | 21.5 ± 3.7 | 8 | 2.0 ± 0.3 | 3 |
| [Ala4]- ″ | 750 ± 35 | 278 | 700 ± 20 | 1000 |
| [Ala5]- ″ | 45.0 ± 1.1 | 17 | 14 ± 4 | 20 |
| [Ala6]- ″ | 19.2 ± 0.8 | 7 | 23 ± 6 | 33 |
| [Ala7]- ″ | 10.0 ± 1.2 | 4 | 19 ± 5 | 27 |
| [Ala8]- ″ | 0.3 ± 0.0 | – | 1.4 ± 0.1 | 2 |
| [Ala9]- ″ | 7.4 ± 0.8 | 3 | 5.5 ± 0.8 | 8 |
| [Ala10]- ″ | 3.8 ± 0.5 | 1.5 | 3.3 ± 0.7 | 5 |
| [Ala11]- ″ | 8.7 ± 0.9 | 3 | 7.6 ± 0.4 | 11 |
| Dyn A(1-13) | 2.7 ± 0.3 | – | 0.7 ± 0.1 | – |
IC50 obtained from radioligand binding assays using[3H]etorphine in rat brain homogenates.
Compared to Dyn A(1-13).
IC50 obtained from the GPI assay.
A comparison of the results obtained from the alanine substituted analogs of Dyn A(1–13) and Dyn B amide indicates expected similarities between the two peptides, but also some subtle differences. As expected, the aromatic residues in positions 1 and 4 of both Dyn A(1–13) and Dyn B amide are critical for opioid receptor binding. While the Leu residue in position 5 is important for opioid receptor binding in the case of Dyn A(1–13), it does not make a major contribution to either the KOR or MOR affinity of Dyn B amide, although it does appear to make a contribution to the peptide’s DOR affinity. The common basic residues in positions 6 and 7 appear to contribute to both the opioid receptor binding of Dyn A(1–13) and the KOR binding of Dyn B amide. Among the C-terminal residues of both peptides, these basic residues appear to make larger contributions to receptor affinities (opioid receptor affinity in the case of Dyn A(1–13) and KOR affinity in the case of Dyn B amide) than other residues. The unique basic residues in these peptides (Arg9 and Lys11 in Dyn A(1–13) and Lys10 in Dyn B amide) also appear to contribute to the opioid receptor affinities of their respective parent peptide. The differences in the relative positions of the unique basic residues may be one reason for subtle differences in the pharmacological profiles exhibited by the two peptides.
It should be noted that there are several differences in the radioligand binding assays used to evaluate the Ala analogs of the two peptides. In the study of Dyn A analogs, the results represent a weighted average of the affinities at multiple opioid receptors in rat brain (which has relatively low expression of KOR)47 since the radiolabeled opioid agonist used, [3H]etorphine, exhibits low selectivity for KOR (KOR/MOR/DOR 1/4/2).48 In the case of the Dyn B amide analogs, the opioid affinities were determined using cell membranes expressing individual cloned opioid receptors that permitted the different effects of residue substitution on KOR affinity vs. MOR and DOR affinity to be assessed. Hence, the comparisons of the affinities of the Ala substituted analogs from the two peptides should be made with some caution.
The efficacies and potencies of the Ala substituted analogs of Dyn B amide were determined at KOR using the [35S]GTPγS assay (Table 4). All of the analogs displayed comparable efficacy to the reference agonist Dyn A(1-13)NH2, indicating that none of the residue side chains were required for the KOR efficacy of Dyn B amide. As expected from the KOR affinities, the Ala1 and Ala4 analogs exhibited very low potency, and the Ala6 and Ala7 analogs displayed substantial decreases (13-and 88-fold, respectively) in potency compared to Dyn B amide in this assay. The Ala5 analog was 10-fold less potent than the parent peptide in this functional assay, even though the KOR affinity was only 2-fold lower than Dyn B amide. Similar decreases in potency were observed in the GPI assay for the corresponding Dyn A(1–13) analogs.46 In contrast, the Ala10 analog did not exhibit lower potency in the KOR [35S]GTPγS assay, in spite of its 5-fold decrease in KOR affinity. Ala substitution of the non-basic amino acids in positions 8, 9 and 11 of Dyn B amide also had minimal effect on the analogs’ potencies in the [35S]GTPγS assay, as expected based on their KOR affinities; similarly, substitution of the non-basic residues in the C-terminus of Dyn A(-1-13) also had minimum effects on potency in the GPI assay.46
Table 4.
Potencies and efficacies of the Dyn B amide alanine analogs at KOR in the GTPγS assay
| Peptide | EC50 (nM ± SEM)a,b |
|---|---|
| N-Terminal alanine substituted analogs | |
| 1 [Ala1] | 2650 ± 890 |
| 2 [Ala4] | 1180 ± 330 |
| C-Terminal alanine substituted analogs | |
| 3 [Ala5] | 109 ± 34 |
| 4 [Ala6] | 116 ± 21 |
| 5 [Ala7] | 802 ± 290 |
| 6 [Ala8] | 20.2 ± 10.8 |
| 7 [Ala9] | 14.8 ± 2.6 |
| 8 [Ala10] | 6.36 ± 1.70 |
| 9 [Ala11] | 8.79 ± 2.20 |
| Dyn B NH2 | 9.14 ± 1.96 |
Values are for n ≥ 2.
All analogs exhibited ≥90% efficacy as compared to Dyn A(1-13)NH2 (efficacy = 100%) except for Ala10 (86 ± 3% efficacy).
Conclusions
The results of the alanine scan of Dyn B amide revealed similarities for contributions to opioid receptor affinities and agonist potency for residues shared in common with Dyn A(1–13). As expected, the aromatic residues in positions 1 and 4 in the N-terminal “message” sequence30 of both peptides are critical for their opioid receptor binding and agonist potency. The basic Arg6 and Arg7 residues in the C-terminal “address” sequence30 also contribute substantially to the opioid receptor affinity and agonist potency of Dyn A(1–13) and the KOR affinity and agonist potency of Dyn B amide. Interestingly, substitution of Leu5 by Ala substantially decreased agonist potency in both Dyn A(1–13) and Dyn B amide, although the substitution had a much larger impact on the opioid receptor affinity of the Dyn A(1–13) analog than it did on the KOR affinity of the Dyn B amide analog.
The binding affinities at MOR and DOR for the alanine analogs of Dyn B amide indicate differences in the contributions of some of these residues to interaction of the parent peptide with different opioid receptors. As expected, the N-terminal aromatic residues were important for the peptide’s affinity for all three opioid receptors. In contrast, and consistent with the “message-address” concept,30 Arg6 and Arg7 contributed to Dyn B amide’s affinity for KOR, but not appreciably to MOR or DOR affinity. Interestingly, while substitution of Leu5 had a small impact on KOR or MOR affinity (≤2.5-fold decrease relative to Dyn B amide), it caused a larger decrease (6-fold) in DOR affinity, enhancing the selectivity of this analog for KOR over DOR.
The pharmacological evaluation of the alanine analogs of Dyn B amide also reveal contributions of the unique residues in the C-terminal sequence to the pharmacological profile of the parent peptide. With the exception of the effect of Lys10 substitution on KOR affinity, the impact of Ala substitution of one of these residues on KOR affinity or agonist potency was minimal (≤2-fold decrease). Interestingly, the results of Ala substitution for Lys10 indicate that this unique C-terminal basic residue enhances affinity for all three opioid receptors, although it does not appear to contribute to KOR agonist potency. In Dyn A(1–13) the basic residues Arg9 and Lys11 both make significant contributions to agonist potency as well as smaller contributions to opioid receptor affinity.46 The different relative positions of these basic residues in the two peptides likely contribute to these differences, although there could also be differences in the effects of Arg9 or Lys11 substitution in Dyn A(1–13) on interactions with different opioid receptors that could not be determined in the assays performed in tissues containing multiple receptors. In contrast to Ala substitution in other positions, replacement of either Gln8 or Phe9 of Dyn B amide by Ala slightly increased MOR affinity (by 2-fold), resulting in the highest affinities for this receptor and a small preference for MOR over KOR. In contrast to substitution of the other unique residues, replacement of Val11 by Ala had a minimal effect (≤2-fold difference) on the affinities at any of the receptors or potency in the KOR functional assay.
Differences in the sequences of Dyn A and B, however, can result in significant differences in the KOR interactions of derivatives of these peptides, as evident from the large differences in the relative potencies of the antagonist analogs of these two peptides containing Mdp at the N-termini.41 The pharmacological data obtained for the C-terminal Dyn B amide analogs support our hypothesis that a unique residue in the C-terminus of Dyn B, Lys10, likely interacts with opioid receptors and contributes to the parent peptide’s opioid receptor affinities. Other unique residues in the C-terminus of Dyn B amide appear to influence the relative affinity of this Dyn for KOR. However, to more fully understand how the C-terminal differences in Dyn B affect structure-activity relationships, the preparation and evaluation of additional analogs of this peptide are needed; such studies could also result in the identification of new useful pharmacological tools.
Acknowledgments
This research was supported by grant R01 DA018832 from the National Institute on Drug Abuse. The authors thank Stacey Sigmon and Bridget Sefranek for performing the pharmacological assays.
References
- 1.Aldrich JV, Vigil-Cruz SC. In: Burger’s Medicinal Chemistry & Drug Discovery. 6th. Abraham DJ, editor. John Wiley and Sons; New York: 2003. pp. 329–481. [Google Scholar]
- 2.Hollt V. Annu Rev Pharmacol Toxicol. 1986;26:59–77. doi: 10.1146/annurev.pa.26.040186.000423. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein A, Fischli W, Lowney LI, Hunkapiller M, Hood L. Proc Natl Acad Sci U S A. 1981;78:7219–7223. doi: 10.1073/pnas.78.11.7219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldstein A, Tachibana S, Lowney LI, Hunkapiller M, Hood L. Proc Natl Acad Sci U S A. 1979;76:6666–6670. doi: 10.1073/pnas.76.12.6666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fischli W, Goldstein A, Hunkapiller MW, Hood LE. Proc Natl Acad Sci U S A. 1982;79:5435–5437. doi: 10.1073/pnas.79.17.5435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garzon J, Sanchez-Blazquez P, Hollt V, Lee NM, Loh HH. Life Sci. 1983;33(Suppl 1):291–294. doi: 10.1016/0024-3205(83)90500-3. [DOI] [PubMed] [Google Scholar]
- 7.Merg F, Filliol D, Usynin I, Bazov I, Bark N, Hurd YL, Yakovleva T, Kieffer BL, Bakalkin G. J Neurochem. 2006;97:292–301. doi: 10.1111/j.1471-4159.2006.03732.x. [DOI] [PubMed] [Google Scholar]
- 8.Suda M, Nakao K, Yoshimasa T, Ikeda Y, Sakamoto M, Yanaihara C, Yanaihara N, Numa S, Imura H. Life Sci. 1983;33(Suppl 1):275–278. doi: 10.1016/0024-3205(83)90496-4. [DOI] [PubMed] [Google Scholar]
- 9.James IF, Fischli W, Goldstein A. J Pharmacol Exp Ther. 1984;228:88–93. [PubMed] [Google Scholar]
- 10.Faden AI. Ann Neurol. 1990;27:67–74. doi: 10.1002/ana.410270111. [DOI] [PubMed] [Google Scholar]
- 11.Shukla VK, Lemaire S. Trends Pharmacol Sci. 1994;15:420–424. doi: 10.1016/0165-6147(94)90091-4. [DOI] [PubMed] [Google Scholar]
- 12.Walker JM, Moises HC, Coy DH, Baldrighi G, Akil H. Science. 1982;218:1136–1138. doi: 10.1126/science.6128791. [DOI] [PubMed] [Google Scholar]
- 13.Long JB, Rigamonti DD, de Costa B, Rice KC, Martinez-Arizala A. Brain Res. 1989;497:155–162. doi: 10.1016/0006-8993(89)90982-7. [DOI] [PubMed] [Google Scholar]
- 14.Herman BH, Goldstein A. J Pharmacol Exp Ther. 1985;232:27–32. [PubMed] [Google Scholar]
- 15.Tan-No K, Esashi A, Nakagawasai O, Niijima F, Tadano T, Sakurada C, Sakurada T, Bakalkin G, Terenius L, Kisara K. Brain Res. 2002;952:7–14. doi: 10.1016/s0006-8993(02)03180-3. [DOI] [PubMed] [Google Scholar]
- 16.Isaac L, Van Zandt O’Malley T, Ristic H, Stewart P. Brain Res. 1990;531:83–87. doi: 10.1016/0006-8993(90)90760-9. [DOI] [PubMed] [Google Scholar]
- 17.Laughlin TM, Vanderah TW, Lashbrook J, Nichols ML, Ossipov M, Porreca F, Wilcox GL. Pain. 1997;72:253–260. doi: 10.1016/s0304-3959(97)00046-8. [DOI] [PubMed] [Google Scholar]
- 18.Vanderah TW, Laughlin T, Lashbrook JM, Nichols ML, Wilcox GL, Ossipov MH, Malan TP, Jr, Porreca F. Pain. 1996;68:275–281. doi: 10.1016/s0304-3959(96)03225-3. [DOI] [PubMed] [Google Scholar]
- 19.Cavicchini E, Candeletti S, Spampinato S, Ferri S. Neuropeptides. 1989;14:45–50. doi: 10.1016/0143-4179(89)90033-4. [DOI] [PubMed] [Google Scholar]
- 20.Tan-No K, Cebers G, Yakovleva T, Hoon Goh B, Gileva I, Reznikov K, Aguilar-Santelises M, Hauser KF, Terenius L, Bakalkin G. Exp Cell Res. 2001;269:54–63. doi: 10.1006/excr.2001.5309. [DOI] [PubMed] [Google Scholar]
- 21.Hauser KF, Knapp PE, Turbek CS. Exp Neurol. 2001;168:78–87. doi: 10.1006/exnr.2000.7580. [DOI] [PubMed] [Google Scholar]
- 22.Hugonin L, Vukojevic V, Bakalkin G, Graslund A. FEBS Lett. 2006;580:3201–3205. doi: 10.1016/j.febslet.2006.04.078. [DOI] [PubMed] [Google Scholar]
- 23.Maximyuk O, Khmyz V, Lindskog CJ, Vukojevic V, Ivanova T, Bazov I, Hauser KF, Bakalkin G, Krishtal O. Cell Death Dis. 2015;6:e1683. doi: 10.1038/cddis.2015.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lind J, Graslund A, Maler L. Biochemistry. 2006;45:15931–15940. doi: 10.1021/bi061199g. [DOI] [PubMed] [Google Scholar]
- 25.Naqvi T, Haq W, Mathur KB. Peptides. 1998;19:1277–1292. doi: 10.1016/s0196-9781(98)00042-4. [DOI] [PubMed] [Google Scholar]
- 26.Hall SM, LeBaron L, Ramos-Colon C, Qu C, Xie JY, Porreca F, Lai J, Lee YS, Hruby VJ. ACS Chem Neurosci. 2016;7:1746–1752. doi: 10.1021/acschemneuro.6b00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vig BS, Murray TF, Aldrich JV. J Med Chem. 2003;46:1279–1282. doi: 10.1021/jm0256023. [DOI] [PubMed] [Google Scholar]
- 28.Vig BS, Murray TF, Aldrich JV. Biopolymers (Pept Sci) 2003;71:620–637. doi: 10.1002/bip.10591. [DOI] [PubMed] [Google Scholar]
- 29.Fang WJ, Cui Y, Murray TF, Aldrich JV. J Med Chem. 2009;52:5619–5625. doi: 10.1021/jm900577k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chavkin C, Goldstein A. Proc Natl Acad Sci U S A. 1981;78:6543–6547. doi: 10.1073/pnas.78.10.6543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wan Q, Murray TF, Aldrich JV. J Med Chem. 1999;42:3011–3013. doi: 10.1021/jm9901071. [DOI] [PubMed] [Google Scholar]
- 32.Schlechtingen G, Zhang L, Maycock A, DeHaven RN, Daubert JD, Cassel J, Chung NN, Schiller PW, Goodman M. J Med Chem. 2000;43:2698–2702. doi: 10.1021/jm990442p. [DOI] [PubMed] [Google Scholar]
- 33.Lu Y, Nguyen TM, Weltrowska G, Berezowska I, Lemieux C, Chung NN, Schiller PW. J Med Chem. 2001;44:3048–3053. doi: 10.1021/jm0101186. [DOI] [PubMed] [Google Scholar]
- 34.Bennett MA, Murray TF, Aldrich JV. J Med Chem. 2002;45:5617–5619. doi: 10.1021/jm025575g. [DOI] [PubMed] [Google Scholar]
- 35.Patkar KA, Yan X, Murray TF, Aldrich JV. J Med Chem. 2005;48:4500–4503. doi: 10.1021/jm050105i. [DOI] [PubMed] [Google Scholar]
- 36.Fang WJ, Bennett MA, Murray TF, Aldrich JV. Biopolymers (Pept Sci) 2011;96:103–110. doi: 10.1002/bip.21495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schlechtingen G, DeHaven RN, Daubert JD, Cassel JA, Chung NN, Schiller PW, Taulane JP, Goodman M. J Med Chem. 2003;46:2104–2109. doi: 10.1021/jm020125+. [DOI] [PubMed] [Google Scholar]
- 38.Bennett MA, Murray TF, Aldrich JV. J Pept Res. 2005;65:322–332. doi: 10.1111/j.1399-3011.2005.00216.x. [DOI] [PubMed] [Google Scholar]
- 39.Patkar KA, Murray TF, Aldrich JV. J Med Chem. 2009;52:6814–6821. doi: 10.1021/jm900715m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Joshi AA, Murray TF, Aldrich JV. J Med Chem. 2015;58:8783–8795. doi: 10.1021/jm501827k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schiller PW, Weltrowska G, Nguyen TM, Lemieux C, Chung NN, Lu Y. Life Sci. 2003;73:691–698. doi: 10.1016/s0024-3205(03)00389-8. [DOI] [PubMed] [Google Scholar]
- 42.Sole NA, Barany G. J Org Chem. 1992;57:5399–5403. [Google Scholar]
- 43.Arttamangkul S, Ishmael JE, Murray TF, Grandy DK, DeLander GE, Kieffer BL, Aldrich JV. J Med Chem. 1997;40:1211–1218. doi: 10.1021/jm960753p. [DOI] [PubMed] [Google Scholar]
- 44.Ross NC, Reilley KJ, Murray TF, Aldrich JV, McLaughlin JP. Br J Pharmacol. 2012;165:1097–1108. doi: 10.1111/j.1476-5381.2011.01544.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cheng Y, Prusoff WH. Biochem Pharmacol. 1973;22:3099–3108. doi: 10.1016/0006-2952(73)90196-2. [DOI] [PubMed] [Google Scholar]
- 46.Turcotte A, Lalonde JM, St-Pierre S, Lemaire S. Int J Pept Protein Res. 1984;23:361–367. [PubMed] [Google Scholar]
- 47.Gillan MG, Kosterlitz HW. Br J Pharmacol. 1982;77:461–469. doi: 10.1111/j.1476-5381.1982.tb09319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Magnan J, Paterson SJ, Tavani A, Kosterlitz HW. Naunyn Schmiedebergs Arch Pharmacol. 1982;319:197–205. doi: 10.1007/BF00495865. [DOI] [PubMed] [Google Scholar]


