Abstract
Objective
To describe trends in income disparities in dental caries among U.S. children and adolescents during two decades of fluctuating economic growth.
Methods
Data were from National Health and Nutrition Examination Surveys conducted in 1988–1994, 1999–2004 and 2011–2014. The number of tooth surfaces with dental caries experience per child was computed for three age groups: 2–5, 6–11 and 12–17 years. Absolute and relative measures of inequality compared caries experience in families below the poverty level with families where income was at least three times the poverty threshold.
Results
Conspicuous, inverse income gradients in dental caries were observed at each time period and in each age group. However, there was no consistent trend or statistically significant change in the degree of inequality between survey periods.
Conclusions
Persisting income disparities in dental caries among U.S. children and adolescents challenge public health dentistry to redouble efforts to redress the inequity.
Keywords: Dental caries, Child, Health status disparities, Poverty, Health surveys, United States
Introduction
The U.S. Surgeon General’s landmark 2000 report Oral Health in America (1) highlighted the inherent unfairness by which the greatest burden of oral disease disproportionately affects those groups with fewest resources. To redress these and other disparities, the Healthy People initiative set an overarching goal to eliminate health disparities by 2010. As the decade closed with disparities persisting, Healthy People 2020 expanded the goals to include attainment of health equity and improvements in the health of all groups.
Many determinants contribute to income disparities in population health, ranging from macro-level national economic indicators to more proximal factors in the delivery of health care. After sustained economic growth during the 1990s, the percentage of children living in poverty declined to 16% by 2000, before increasing to 22% by 2010 following a deep recession early in the 21st century. A previous study(2) described income-associated trends in caries prevalence among U.S. children between 1999–2004 and 2011–2014, but did not report measures of inequality and did not report extent of caries experience (i.e., mean dfs or mean DMFS per child). The aim of this study was to describe temporal patterns in measures of income-associated inequality in extent of dental caries experience among U.S. children and adolescents from 1988–94 to 2011–14.
Methods
Study Design, Setting, and Periods
Cross-sectional interview and dental examination data for three periods (1988–1994, 1999–2004, 2011–2014) were obtained from the National Health Nutrition and Examination Survey (NHANES). In each period, NHANES selected a stratified random sample representative of the U.S. civilian, non-institutionalized population. Interviews conducted with a reference adult householder obtained information about demographic characteristics of the sampled child/adolescent, the household and family income.
Dental Caries Examinations
Trained dental examiners recorded the status of each tooth surface in the primary and permanent dentitions. Dental decay was classified at the threshold of cavitation and a surface was classified as filled if the restoration had been placed to treat dental caries. Permanent teeth missing due to decay were also recorded. The standardized NHANES dental examination protocol has rigorous quality control procedures and dental examiners exhibit high levels of inter-examiner reliability.(3)
Age-Specific Indices of Dental Caries Experience
Outcome measures computed for each individual were the number of decayed or filled primary teeth surfaces (dfs) and number of decayed, missing or filled permanent tooth surfaces (DMFS). Three age groups relevant to stages of dental development were analyzed: dfs in 2–5 year olds; dfs and DMFS in 6–11 year olds; and DMFS in 6–17 year olds. In each survey period, tooth-surface-specific variables were used to compute the caries indices yielding data from 9,975 subjects in 1988–1994 (NHANES-III), 10,655 subjects in 1999–2004, and 6,234 subjects in 2011–2014.
Absolute and Relative Measures of Inequality
The income-to-poverty ratio is derived by dividing family income by the poverty guidelines specified by Department of Health and Human Services for any given year, taking account of family size, and state of residence. This continuous variable was grouped into four categories: below poverty threshold, up to twice the poverty threshold (i.e., 100% to <200%); up to three times the poverty threshold (i.e., 200% to <300%) and at least three times the poverty threshold (i.e. ≥300%).
Income disparities were quantified using two measures of health inequality (4):
An absolute measure of inequality was computed as mean caries experience in the lowest income category minus mean caries experience in the highest income category (null value = 0);
A relative measures of inequality was computed as the ratio of absolute inequality divided by mean caries experience in the highest income category and multiplied by 100 (null value = 0).
Subjects with missing income data were excluded from calculations of inequality. For descriptive purposes, Table 1 reports all available data from examined children in the NHANES datasets, quantifying the extent of missing income information. The data were analyzed separately for each period using SAS survey estimation procedures to account for sampling characteristics and weights applicable to each period. Estimates therefore were generalizable to the U.S. population in this age range and in the respective survey period.
Table 1.
Number of children examined and population distribution of family income and dental caries experience among US children and adolescents in three periods of National Health and Nutrition Examination Surveys, 1988 to 2014
| Age group (years) | |||||
|---|---|---|---|---|---|
| Period | Statistic | 2–5 | 6–11 | 12–17 | All 2–17 |
| 1988–1994 | Number of children | ||||
| Unweighted number examined | 4,301 | 3,237 | 2,437 | 9,975 | |
| Family income: % of population (se) | Weighted population estimates
|
||||
| Below poverty threshold | 26.4 (1.5) | 24.3 (1.8) | 20.8 (1.7) | 23.5 (1.2) | |
| 100-<200% of poverty threshold | 24.1 (1.1) | 23.2 (1.5) | 23.2 (1.7) | 23.4 (1.1) | |
| 200-<300% of poverty threshold | 20.5 (1.2) | 22.3 (1.5) | 22.4 (2.1) | 21.9 (1.2) | |
| ≥ 300% of poverty threshold | 23.5 (1.4) | 26.2 (1.7) | 27.3 (2.4) | 25.9 (1.4) | |
| Missing | 5.5 (0.4) | 4.1 (0.5) | 6.3 (1.0) | 5.2 (0.5) | |
| Dental caries: population mean (s.e.) * | |||||
| dfs† per child | 2.1 (0.2) | 3.5 (0.2) | |||
| DMFS‡ per child | 0.9 (0.1) | 4.4 (0.3) | |||
| Dental caries: population prevalence (s.e.) | |||||
| % of children with dfs>0 | 23.9 (1.3) | 44.3 (1.6) | |||
| % of children with DMFS>0 | 26.0 (1.7) | 64.0 (2.1) | |||
| 1999–2004 | Number of children | ||||
| Unweighted number examined | 2,379 | 3,171 | 5,105 | 10,655 | |
| Family income: % of population (se) | Weighted population estimates
|
||||
| Below poverty threshold | 25.8 (1.2) | 22.2 (1.3) | 19.6 (0.8) | 22.1 (0.8) | |
| 100-<200% of poverty threshold | 24.6 (1.5) | 25.1 (1.7) | 21.1 (1.0) | 23.4 (1.2) | |
| 200-<300% of poverty threshold | 14.9 (1.2) | 16.8 (1.2) | 15.5 (0.9) | 15.9 (0.9) | |
| ≥ 300% of poverty threshold | 28.6 (1.8) | 30.2 (1.9) | 37.6 (1.5) | 32.6 (1.5) | |
| Missing | 6.3 (0.7) | 5.6 (0.8) | 6.2 (0.6) | 6.0 (0.5) | |
| Dental caries: population mean (s.e.) | |||||
| dfs per child | 2.6 (0.2) | 4.0 (0.2) | |||
| DMFS per child | 0.7 (0.0) | 3.5 (0.1) | |||
| Dental caries: population prevalence (s.e.) | |||||
| % of children with dfs>0 | 28.0 (1.4) | 46.3 (1.9) | |||
| % of children with DMFS>0 | 20.8 (1.1) | 55.4 (1.0) | |||
| Age group | |||||
| Period | Statistic | 2–5 yrs | 6–11 yrs | 12–17 yrs | All 2–17 yrs |
| 2011–2014 | Number of children | ||||
| Unweighted number examined | 1,773 | 2,523 | 1,938 | 6,234 | |
| Family income: % of population (se) | Weighted population estimates
|
||||
| Below poverty threshold | 29.7 (2.4) | 25.6 (2.0) | 20.7 (2.2) | 24.8 (1.9) | |
| 100-<200% of poverty threshold | 24.7 (1.7) | 22.7 (1.4) | 22.1 (1.9) | 23.0 (1.1) | |
| 200-<300% of poverty threshold | 11.7 (1.5) | 14.5 (1.2) | 14.6 (1.4) | 13.8 (1.0) | |
| ≥ 300% of poverty threshold | 28.2 (3.1) | 32.3 (2.8) | 36.9 (3.2) | 33.0 (2.6) | |
| Missing | 5.7 (0.7) | 5.0 (0.7) | 5.7 (0.8) | 5.4 (0.6) | |
| Dental caries: population mean (s.e.) | |||||
| dfs per child | 2.6 (0.3) | 4.8 (0.3) | |||
| DMFS per child | 0.7 (0.1) | 3.5 (0.2) | |||
| Dental caries: population prevalence (s.e.) | |||||
| % of children with dfs>0 | 23.4 (1.4) | 45.4 (1.8) | |||
| % of children with DMFS>0 | 18.0 (1.1) | 52.6 (1.8) | |||
s.e. standard error
dfs = number of primary tooth surfaces decayed or filled due to dental decay
DMFS = number of permanent tooth surfaces decayed, missing due to dental decay or filled due to dental decay
This study was reviewed by the UNC Office of Human Research Ethics, and deemed exempt from IRB review (study #15-2225).
Results
Population estimates of income and caries experience in each period are presented in Table 1. In 1988–1994, 2–17 year olds were distributed in approximate quartiles across the four income categories, although by 2011–2014, about one third was in the highest income category. Within each period, the percentage of children below the poverty threshold tended to be greater in younger age groups. In each period and each age group, approximately 5% had missing data for the income-poverty ratio (Table 1). Dental caries experience in the primary dentition increased between 1988–1994 and 2011–2014, whereas it decreased somewhat in the permanent dentition.
All periods and all age groups, were characterized by conspicuous, inverse gradients in caries experience according to income-to-poverty ratio (Figure 1). The gradient was monotonic in most instances, signifying greater caries experience across successively lower income categories. Absolute and relative inequalities were statistically significantly different from the null value in all but one instance (6–11 year-old DMFS in 1988–1994, Fig 1C). Inequality was greatest in 2–5 year olds (Fig 1A): absolute inequality ranged from 2.4 to 4.0 across periods, while relative inequality ranged from 199 to 446. In contrast, among 12–17 year olds (Fig 1D), the ranges were 1.3 to 2.9 and 38 to 137, respectively.
Figure 1.
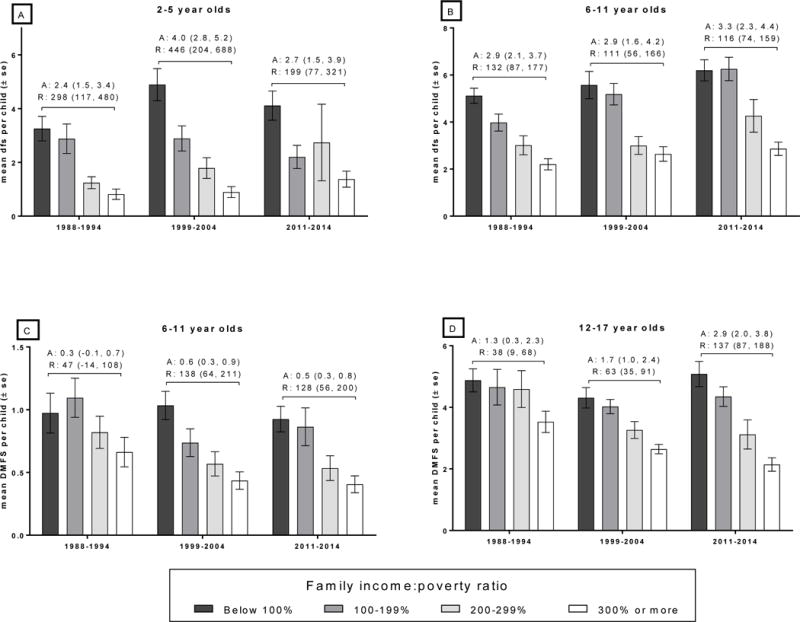
Data are from children dentally examined in the U.S. National Health Nutrition and Examination Survey during the periods indicated. Income-to-poverty ratio is the quotient of family income divided by the poverty guidelines specified by Department of Health and Human Services for a given year, taking account of family size, and state of residence. Vertical bars represent means and whiskers indicate standard errors of the mean for population estimates of number of decayed or filled primary teeth surfaces (dfs) per person and decayed, missing or filled permanent tooth surfaces (DMFS) per person. Numbers above bars represent two measures of inequality in caries experience and their 95% confidence intervals: A = absolute measure of inequality, computed as mean caries experience in the lowest income category minus mean caries experience in the highest income category; R = relative measures of inequality, computed as the ratio of absolute inequality divided by mean caries experience in the highest income category and multiplied by 100 (null value = 0).
Within the youngest age group, the degree of inequality was somewhat greater in 1999–2004 than either the earlier or later period, although 95% confidence intervals overlapped considerably between periods, signifying no statistically significant difference in inequality over time. Overall, there was no clear temporal pattern of change in the degree of inequality as signified by marked overlap of 95% confidence intervals for estimates.
The time-series depicts two birth cohorts. The earliest cohort, born around 1987, was aged 2–5 years in the 1988–94 period and most were aged 12–17 years in the 1999–2004 period: both absolute and relative inequalities reduced as that cohort aged. The later cohort, born around 1997, was aged 2–5 years in the 1999– 2004 period, and most were aged 12–17 years in the 2011–2004 survey: absolute and relative inequalities likewise reduced as that cohort aged, and the extent of inequality at a given age was greater in the later cohort than in the cohort born earlier.
Discussion
Pronounced income-related disparities in caries experience in the U.S. population of children and adolescents persisted over the two decades studied here. During this period of economic growth and recession, the extent of inequality did not change appreciably, suggesting that macro-economic forces bore little influence on income disparities in dental health. Analysis of the two birth cohorts raises the possibility that income inequality in dental caries is greater among children born around 1997 than among the cohort born a decade earlier. However, analysis of future survey data is needed to verify this possibility. Overall, findings corroborate previous studies showing no real progress in eliminating disparities in other oral health indicators, including income-related disparities in untreated dental caries (despite concomitant increases in dental sealant provision) (5) and negligible changes in use of dental services across income groups (despite expansion of Medicaid and related health insurance programs).(6)
While discouraging, this conclusion does not mean that oral health disparities are insurmountable. For example, in Australia(7) and the United Kingdom,(8) socio-economic inequalities in children’s caries were less pronounced in areas with community water fluoridation compared to non-fluoridated places. Given that coverage of fluoridation in the U.S. expanded during the period studied, reduced inequalities in dental caries might be expected. However, fluoridation’s potential impact on inequalities in dental caries has not been investigated in the U.S. Also, there have been other noteworthy changes during the period that may have exacerbated disparities in dental caries, such as the increased prevalence of obesity, greater consumption of bottled water and increasing public mistrust in the safety of tap water.
In principle, efforts to reduce inequalities are most likely to be successful if they target determinants of health operating at multiple levels, ranging from upstream policies targeting poverty itself, to downstream interventions in healthcare.(9) One strategy is interprofessional collaboration between oral healthcare providers and nondental health professionals to educate and learn from fellow-health professionals and jointly provide services targeting disadvantaged groups.(10) By their nature, such interventions are likely to operate at local- or state-levels. Yet, even the successful ones may fail to alter national caries levels, as studied here.
The seeming intractability of income disparities in dental caries at a national level casts doubt on the wisdom of goals aiming to reduce or even eliminate them.(1) We disagree, although there might be merit in promulgating less ambitious targets, such as improvements in population health that at least do not worsen health disparities. Instead, we believe it is essential to document them. The information should encourage new efforts and sustain existing programs that seek to redress the inequity.
Acknowledgments
Research reported in this publication was supported by the National Institute of Dental & Craniofacial Research of the National Institutes of Health under Award Number UH2DE025494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest statement
The authors declare no financial conflicts of interest.
Contributor Information
Gary Douglas Slade, University of North Carolina at Chapel Hill School of Dentistry, Chapel Hill, United States.
Dr Anne Sanders, University of North Carolina at Chapel Hill School of Dentistry, Department of Dental Ecology, Koury Oral Health Sciences Building, Chapel Hill, United States.
References
- 1.United States. Public Health Service. Office of the Surgeon General., National Institute of Dental and Craniofacial Research (U.S.) Oral health in America: a report of the Surgeon General. Bethesda, Md.: National Institute of Dental and Craniofacial Research: U.S. Public Health Service, Dept. of Health and Human Service; 2000. [Google Scholar]
- 2.Dye BA, Mitnik GL, Iafolla TJ, Vargas CM. Trends in dental caries in children and adolescents according to poverty status in the United States from 1999 through 2004 and from 2011 through 2014. J Am Dent Assoc. 2017 Jun 13; doi: 10.1016/j.adaj.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 3.Dye BA, Li X, Lewis BG, Iafolla T, Beltran-Aguilar ED, Eke PI. Overview and quality assurance for the oral health component of the National Health and Nutrition Examination Survey (NHANES), 2009–2010. J Public Health Dent. 2014 Summer;74(3):248–56. doi: 10.1111/jphd.12056. [DOI] [PubMed] [Google Scholar]
- 4.Cheng NF, Han PZ, Gansky SA. Methods and software for estimating health disparities: the case of children’s oral health. Am J Epidemiol. 2008 Oct 15;168(8):906–14. doi: 10.1093/aje/kwn207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Capurro DA, Iafolla T, Kingman A, Chattopadhyay A, Garcia I. Trends in income-related inequality in untreated caries among children in the United States: findings from NHANES I, NHANES III, and NHANES 1999–2004. Community Dent Oral Epidemiol. 2015 Dec;43(6):500–10. doi: 10.1111/cdoe.12174. [DOI] [PubMed] [Google Scholar]
- 6.Akinkugbe A, Lucas-Perry E. Trends in Dental Visits among the Us Non-Institutionalized Civilian Population: Findings from Brfss 1995 – 2008. J Theory Pract Dent Public Health. 2013;1(2):32–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Slade GD, Spencer AJ, Davies MJ, Stewart JF. Influence of exposure to fluoridated water on socioeconomic inequalities in children’s caries experience. Community Dent Oral Epidemiol. 1996 Apr;24(2):89–100. doi: 10.1111/j.1600-0528.1996.tb00822.x. [DOI] [PubMed] [Google Scholar]
- 8.Riley JC, Lennon MA, Ellwood RP. The effect of water fluoridation and social inequalities on dental caries in 5-year-old children. Int J Epidemiol. 1999 Apr;28(2):300–5. doi: 10.1093/ije/28.2.300. [DOI] [PubMed] [Google Scholar]
- 9.Borrell LN. Oral Health Inequities: An AJPH Supplement to Help Close the Gap. Am J Public Health. 2017 May;107(S1):S6–S7. doi: 10.2105/AJPH.2017.303959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harper HJ, Conicella ML, Cranston NC, Edmonds JC, Matthews CO. The Aetna-NDA Partnership for Achieving Racial and Ethnic Health Equity. Am J Public Health. 2017 May;107(S1):S10–S1. doi: 10.2105/AJPH.2017.303944. [DOI] [PMC free article] [PubMed] [Google Scholar]


