Abstract
Objective
This study documents the prevalence and impact of anxiety and depression in US children based on the parent report of health care provider diagnosis.
Methods
National Survey of Children's Health data from 2003, 2007, and 2011–2012 were analyzed to estimate the prevalence of anxiety or depression among children aged 6 to 17 years. Estimates were based on the parent report of being told by a health care provider that their child had the specified condition. Sociodemographic characteristics, co-occurrence of other conditions, health care use, school measures, and parenting aggravation were estimated using 2011–2012 data.
Results
Based on the parent report, lifetime diagnosis of anxiety or depression among children aged 6 to 17 years increased from 5.4% in 2003 to 8.4% in 2011–2012. Current anxiety or depression increased from 4.7% in 2007 to 5.3% in 2011–2012; current anxiety increased significantly, whereas current depression did not change. Anxiety and depression were associated with increased risk of co-occurring conditions, health care use, school problems, and having parents with high parenting aggravation. Children with anxiety or depression with effective care coordination or a medical home were less likely to have unmet health care needs or parents with high parenting aggravation.
Conclusion
By parent report, more than 1 in 20 US children had current anxiety or depression in 2011–2012. Both were associated with significant comorbidity and impact on children and families. These findings may inform efforts to improve the health and well-being of children with internalizing disorders. Future research is needed to determine why child anxiety diagnoses seem to have increased from 2007 to 2012.
Anxiety and depression are internalizing mental disorders that often start during childhood.1,2 Anxiety encompasses a heterogeneous group of conditions, characterized by excessive fear or worry, whereas depression is characterized by persistent sad or irritable mood.2 Childhood anxiety tends to have an earlier onset and may confer an increased risk of depression.1,3 Anxiety and depression frequently co-occur with each other and neurobehavioral disorders1,2 and health conditions.2,4 Alone and in combination, these conditions have been associated with school, social, and family problems; health risk behaviors; and the significant individual, family, and community costs.3,5 In 2013, anxiety and depression were 2 of the top 20 conditions with the highest health care costs among US children.6 Anxiety and depression frequently persist into adulthood and are associated with ongoing risk of co-occurring conditions, lower income, and earlier mortality.7 Because of an increased need for specialty care8 and the co-occurrence of mental and other chronic health conditions, effective care coordination may be particularly important for children with anxiety or depression. One such approach, the medical home, provides accessible, comprehensive care, including effective coordination of primary and specialist care.9
Monitoring childhood mental disorders is important for defining impact, informing public health strategies, and documenting the potential service needs of this population. In a 2004 review of community-based studies, anxiety and depression were among the most common mental disorders in children (anxiety: 1.9%–23.8%; major depressive disorder: 0.2%–12.9%).10 Lifetime anxiety (31.9%) and depression (11.7%) were also the most common mental disorders identified in the 2001 to 2004 National Comorbidity Survey Replication Adolescent Supplement (NCS-A).1 Studies using direct assessment of children allow for the identification of both previously diagnosed and undiagnosed children. However, direct assessment requires significant resources, and studies using direct assessment typically do not allow for examination of trends over time, are rarely nationally representative, and may still misclassify children.11 National surveillance shows wide-ranging estimates of depression but few estimates of anxiety.12 Parent-reported data from the 2007 National Health Interview Survey showed 3% of children aged 4 to 17 years were depressed and 2.6% had phobias or fears.12 Approximately 12.5% of adolescents reported symptoms meeting criteria for a major depressive episode based on the 2015 National Survey of Drug Use and Health (NSDUH); this estimate was higher than estimates from 2004 to 2014.13
The National Survey of Children's Health (NSCH) is the only national data source to evaluate the presence of anxiety and depression on a regular basis. The NSCH was conducted in 2003, 2007, and 2011–2012; in each survey, parents reported whether a health care provider ever told them that their child had anxiety or depression, allowing for estimates over time. In addition, parents reported about other conditions, allowing for estimates of co-occurrence and comparison with published prevalence estimates. Co-occurring conditions included autism spectrum disorder, attention-deficit/hyperactivity disorder, and other disorders.14,15 Reliance on reported diagnoses excludes undiagnosed cases from estimates but provides insights into the number of families affected by these conditions who come to the attention of a health care provider.11 Furthermore, these surveys have large sample sizes and consider a broad range of measures of health and well-being. These characteristics allow for an assessment of both prevalence over time and impact of mental disorders among US children.
This study used parent-reported NSCH data to (1) estimate the 2011–2012 prevalence of diagnosed anxiety and depression among US children, (2) determine whether the diagnosed prevalence had changed over time, (3) describe characteristics of children with anxiety and depression, and (4) assess the association between medical home access and selected measures of impact among children with depression and anxiety.
Methods
Sample
The National Survey of Children's Health is a cross-sectional random digit dial telephone survey of parents and guardians (2003, n = 102,353; 2007, n = 91,642; and 2011–2012, n = 95,677).16 The 2003 and 2007 surveys used landlines only; a sample of cell phone numbers was added in 2011–2012. In 2011–2012, the proportion of households known to include children whose parents completed the interview, known as the interview completion rate, was 54.1% and 41.2% for landline and cell phone samples, respectively. The overall response rate was 23% in 2011–2012, 46.7% in 2007, and 55.3% in 2003. 16–18 The analyses were restricted to children aged 6 to 17 years with valid data on sex and anxiety and depression questions (n = 65,411 of 65,680 in 2011–2012; n = 63,874 of 64,076 in 2007; and n = 68,786 of 69,031 in 2003).
Diagnosed Prevalence Over Time
To compare the prevalence of diagnosed anxiety or depression over time for children aged 6 to 17 years, parent-reported data from the 3 survey years were analyzed. In 2003, parents responded to a single question: “Has a doctor or health care provider ever told you that [CHILD] has depression or anxiety?” In 2007 and 2011–2012, anxiety and depression were asked about independently. Parents were asked the following questions: “Has a doctor or other health care provider ever told you that [CHILD] had anxiety problems?” and “Has a doctor or other health care provider ever told you that [CHILD] had depression?” If yes, parents were asked, “Does [CHILD] currently have anxiety problems” and “Does [CHILD] currently have depression?” Parents were asked to rate current anxiety or depression as mild, moderate, or severe.
Characteristics of Children with Anxiety or Depression (2011–2012)
Sociodemographic characteristics included child's sex, age, race, Hispanic ethnicity, household income relative to the federal poverty level, parental educational attainment, region, and health insurance status and type (Table 1).
Table 1. Parent-Reported Anxiety or Depression by Sociodemographic Characteristics Among US Children Aged 6 to 17 Years, 2011–2012.
| Characteristic | Current Depression | Current Anxiety | Current Anxiety or Depression | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| % (95% CI) | PR (95% CI) | % (95% CI) | PR (95% CI) | % (95% CI) | PR (95% CI) | |
| Total | 2.7 (2.5–3.1) | — | 4.1 (3.8–4.5) | — | 5.3 (5.0–5.7) | — |
| Age (yr) | ||||||
| 6–11 | 1.5 (1.2–1.8) | Referent | 3.5 (3.1–3.9) | Referent | 4.1 (3.7–4.6) | Referent |
| 12–17 | 4.0 (3.5–4.5) | 2.7 (2.1–3.5) | 4.7 (4.3–5.3) | 1.4 (1.2–1.6) | 6.5 (6.0–7.2) | 1.6 (1.4–1.8) |
| Sex | ||||||
| Male | 2.9 (2.5–3.4) | 1.1 (0.9–1.4) | 4.4 (4.0–4.9) | 1.2 (1.0–1.4) | 5.7 (5.2–6.3) | 1.1 (1.0–1.3) |
| Female | 2.6 (2.2–3.0) | Referent | 3.8 (3.4–4.3) | Referent | 5.0 (4.5–5.5) | Referent |
| Race/ethnicity | ||||||
| White non-Hispanic | 2.9 (2.6–3.4) | Referent | 5.3 (4.9–5.8) | Referent | 6.5 (5.9–7.0) | Referent |
| Black non-Hispanic | 2.7 (2.1–3.6) | 0.9 (0.7–1.2) | 2.8 (2.2–3.7) | 0.5 (0.4–0.7) | 4.1 (3.3–5.1) | 0.6 (0.5–0.8) |
| Hispanic | 2.3 (1.7–3.2) | 0.8 (0.5–1.1) | 2.5 (1.9–3.2) | 0.5 (0.4–0.6) | 3.8 (3.0–4.8) | 0.6 (0.5–0.8) |
| Highest household education | ||||||
| High school diploma or less | 3.0 (2.6–3.5) | 1.3 (1.1–1.7) | 4.1 (3.6–4.6) | 0.9 (0.8–1.1) | 5.4 (4.9–6.0) | 1.0 (0.9–1.2) |
| At least some college or technical school | 2.2 (1.9–2.7) | Referent | 4.4 (3.9–4.9) | Referent | 5.3 (4.8–5.9) | Referent |
| Household income | ||||||
| ≤200% of federal poverty level | 3.9 (3.4–4.4) | 2.0 (1.6–2.5) | 4.6 (4.1–5.2) | 1.2 (1.1–1.5) | 6.4 (5.8–7.1) | 1.4 (1.2–1.6) |
| >200% of federal poverty level | 1.9 (1.6–2.3) | Referent | 3.8 (3.4–4.2) | Referent | 4.5 (4.1–5.0) | Referent |
| Region | ||||||
| Northeast | 2.6 (2.0–3.4) | Referent | 5.2 (4.5–6.2) | Referent | 6.5 (5.6–7.5) | Referent |
| Midwest | 3.1 (2.7–3.7) | 1.2 (0.9–1.6) | 4.3 (3.8–4.9) | 0.8 (0.7–1.0) | 5.6 (5.0–6.2) | 0.9 (0.7–1.0) |
| South | 2.9 (2.4–3.5) | 1.1 (0.8–1.5) | 4.1 (3.5–4.7) | 0.8 (0.6–1.0) | 5.4 (4.7–6.0) | 0.8 (0.7–1.0) |
| West | 2.2 (1.6–3.0) | 0.8 (0.5–1.2) | 3.3 (2.7–3.9) | 0.6 (0.5–0.8) | 4.3 (3.6–5.2) | 0.7 (0.5–0.8) |
| Health care coverage | ||||||
| No health care coverage | 2.3 (1.2–4.1) | 1.3 (0.7–2.5) | 2.3 (1.4–3.6) | 0.6 (0.4–1.0)a | 3.5 (2.3–5.3) | 0.8 (0.5–1.2) |
| Medicaid | 4.7 (4.1–5.4) | 2.8 (2.2–3.6) | 5.3 (4.7–5.9) | 1.5 (1.2–1.7) | 7.5 (6.8–8.3) | 1.7 (1.5–2.0) |
| Non-Medicaid | 1.7 (1.4–2.0) | Referent | 3.7 (3.3–4.1) | Referent | 4.3 (3.9–4.8) | Referent |
Data source: CDC/NCHS, National Survey of Children's Health, 2011–2012.
, p < 0.05 compared with referents. CDC, Centers for Disease Control and Prevention; CI, confidence interval; NCHS, National Center for Health Statistics; PR, prevalence ratio.
The parent report of 11 other specified neurobehavioral disorders and 9 specified chronic health conditions (Table 2) used the same question structure as that for anxiety and depression (i.e., whether a doctor or other health care providers ever told them their child had [condition], and if yes, if their child currently had the condition). Body mass index (BMI) was calculated using parent-reported height and weight; a BMI in the 95th percentile or higher was considered obese.19 BMI data for children younger than 10 years were not available because of concerns about the validity of the height data; thus, BMI was excluded from Table 2 and as a control variable.
Table 2. Parent-Reported Co-occurring Neurobehavioral and Other Chronic Health Conditions Among US Children Aged 6 to 17 Years with and Without Parent-Reported Anxiety or Depression, 2011–2012.
| Characteristic | Current Depression | Current Anxiety | Current Anxiety or Depression | No Current Anxiety or Depression | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||
| % (95% CI) | aPR (95% CI) | % (95% CI) | aPR (95% CI) | % (95% CI) | aPR (95% CI) | % (95% CI) | |
| Any neurobehavioral condition other than depression and anxiety | 77.0 (71.9–81.3) | 3.2 (3.0–3.5) | 76.6 (73.1–79.8) | 3.3 (3.1–3.5) | 75.6 (72.4–78.6) | 3.4 (3.2–3.6) | 20.9 (20.3–21.6) |
| Attention-deficit/hyperactivity disorder | 57.3 (51.7–62.7) | 4.6 (4.1–5.2) | 54.1 (50.2–58.0) | 4.6 (4.2–5.1) | 53.3 (49.7–56.9) | 4.8 (4.3–5.2) | 10.0 (9.4–10.5) |
| Behavioral problems | 43.6 (38.2–49.2) | 10.9 (9.2–13.0) | 39.3 (35.4–43.2) | 11.2 (9.6–13.1) | 38.5 (34.9–42.2) | 12.7 (10.9–14.8) | 3.0 (2.7–3.3) |
| Tourette syndrome | 1.0 (0.6–1.8) | 3.2 (1.5–6.7) | 2.4 (1.7–3.5) | 10.4 (6.2–17.5) | 1.9 (1.3–2.7) | 8.4 (5.0–13.9) | 0.2 (0.1–0.2) |
| Autism spectrum disorder | 12.2 (8.7–16.7) | 5.8 (4.0–8.5) | 21.2 (18.3–24.4) | 11.7 (9.6–14.3) | 18.0 (15.3–21.0) | 11.0 (8.8–13.7) | 1.6 (1.4–1.8) |
| Developmental delay | 21.5 (17.6–26.1) | 3.9 (3.1–5.0) | 32.3 (28.8–36.0) | 6.6 (5.7–7.7) | 27.8 (24.8–31.0) | 5.8 (5.0–6.8) | 4.5 (4.2–4.8) |
| Intellectual disability | 7.0 (4.8–10.2) | 4.6 (2.8–7.6) | 9.4 (7.3–12.0) | 8.5 (6.0–11.9) | 7.7 (6.1–9.8) | 6.9 (5.0–9.7) | 1.1 (0.9–1.3) |
| Speech/language problems | 26.9 (21.8–32.6) | 3.2 (2.5–4.0) | 28.3 (25.0–31.8) | 3.2 (2.8–3.7) | 28.1 (24.8–31.6) | 3.3 (2.9–3.9) | 7.8 (7.4–8.3) |
| Learning disability | 46.5 (41.0–52.1) | 3.8 (3.2–4.4) | 47.9 (44.0–51.8) | 4.3 (3.9–4.8) | 46.2 (42.5–49.8) | 4.3 (3.8–4.7) | 10.1 (9.6–10.7) |
| Other chronic health conditions | 47.3 (41.8–52.8) | 1.7 (1.5–2.0) | 49.0 (45.1–52.9) | 1.9 (1.7–2.1) | 46.6 (43.0–50.3) | 1.8 (1.6–2.0) | 24.7 (24.0–25.5) |
| Hearing or vision problems | 10.5 (8.3–13.2) | 1.8 (1.4–2.3) | 12.9 (10.7–15.5) | 2.3 (1.8–2.8) | 11.7 (9.8–13.9) | 2.1 (1.7–2.6) | 5.2 (4.8–5.6) |
| Hearing problems | 7.3 (5.5–9.7) | 1.9 (1.4–2.6) | 10.0 (8.0–12.6) | 2.7 (2.1–3.6) | 8.7 (7.0–10.8) | 2.5 (1.9–3.2) | 3.2 (2.9–3.5) |
| Vision problems | 4.5 (3.2–6.5) | 2.1 (1.4–3.2) | 4.4 (3.3–5.7) | 2.0 (1.5–2.8) | 4.2 (3.3–5.4) | 2.0 (1.5–2.8) | 2.1 (1.9–2.4) |
| Asthma | 32.1 (27.4–37.2) | 1.7 (1.4–2.1) | 30.4 (27.0–34.0) | 1.7 (1.5–2.0) | 29.8 (26.7–33.1) | 1.7 (1.5–1.9) | 16.8 (16.2–17.5) |
| Epilepsy or seizure disorder | 3.4 (2.2–5.2) | 2.4 (1.4–4.1) | 4.9 (3.6–6.6) | 3.9 (2.6–5.8) | 3.9 (2.9–5.3) | 3.1 (2.1–4.6) | 1.3 (1.1–1.5) |
| Diabetes | 2.2 (1.2–4.1) | 3.5 (1.7–7.5) | 1.5 (0.8–2.7) | 2.4 (1.1–5.3) | 1.6 (1.0–2.6) | 2.7 (1.4–5.2) | 0.5 (0.4–0.6) |
| Cerebral palsy | 0.5 (0.3–0.9) | 1.4 (0.6–3.3) | 0.8 (0.5–1.4) | 3.4 (1.7–7.0) | 0.6 (0.4–1.1) | 2.5 (1.2–5.2) | 0.2 (0.2–0.3) |
| Bone, joint, or muscle problems | 14.7 (11.2–19.2) | 3.4 (2.4–4.7) | 14.6 (11.8–18.1) | 3.9 (3.0–5.1) | 14.0 (11.4–17.0) | 3.8 (2.9–4.9) | 3.3 (3.0–3.6) |
| Brain injury/concussion | 7.7 (5.5–10.8) | 1.9 (1.3–2.9) | 8.5 (6.8–10.8) | 2.2 (1.6–2.9) | 7.7 (6.2–9.6) | 2.0 (1.5–2.6) | 3.1 (2.8–3.4) |
The aPR was adjusted for the following factors categorized as they are shown in Table 1, except race/ethnicity: age, sex, race/ethnicity (white non-Hispanic vs all others), highest household education, and household income. Data source: CDC/NCHS, National Survey of Children's Health, 2011–2012. aPR, adjusted prevalence ratio; CDC, Centers for Disease Control and Prevention; CI, confidence interval; NCHS, National Center for Health Statistics.
Selected indicators of impact included the following: whether the child had “special health care needs” (CSHCN; defined as having a chronic condition resulting in functional limitations or service use or need beyond that generally required by children of the same age, assessed with a validated screener) 20; whether their child had any kind of emotional, developmental, or behavioral problem for which he/she needs treatment or counseling; parenting aggravation (high/low; past month, calculated from the parent report of how often they felt angry with their child, that it was harder to care for their child than for other children of the same age, and that their child did things that really bothered them)21; and if the child had repeated a grade other than kindergarten. Indicators for the past 12 months included whether the parent was contacted about school problems and whether the child had received preventive medical care; received treatment or counseling from a mental health professional; taken medication because of difficulties with emotions, concentration, or behavior; saw a specialist other than a mental health professional; had a medical home, based on a series of 19 questions assessing medical home criteria22; received needed care coordination, 1 component of the medical home9; and had unmet health care needs, including medical and/or mental health services. Access to a medical home required the child to have a personal doctor or nurse, a usual source of care, family-centered care, and receive referrals and care coordination, if needed. Care coordination was based on parent responses about whether they received help, if needed, arranging or coordinating the child's care among doctors or services.
Statistical Analysis
SAS-callable SUDAAN (version 11.0.0, RTI International, Cary, NC) was used to account for the complex sampling design. Weighted prevalence estimates and 95% confidence intervals were calculated to determine the prevalence of parent-reported diagnosed anxiety and depression.
Using 2011–2012 data, prevalence ratios (PRs) were calculated using logistic regression to compare the prevalence of parent-reported anxiety and depression among children aged 6 to 17 years across demographic subgroups and the prevalence of co-occurring conditions relative to children without anxiety or depression. Adjusted PRs controlled for child's sex, age (6–11 vs 12–17 years), race and ethnicity (white non-Hispanic vs other), household education, and household income. To clarify the specific relationship between anxiety and depression (as opposed to other conditions) with indicators of impact, these models were further adjusted for co-occurring conditions. When considering the relationship between having a medical home or effective care coordination and impact, the models were further adjusted for whether the child had severe depression or anxiety. Household income was imputed for those (9.3%) without valid income data; this variable was provided in the public use data set. All estimates are generalizable to the population of noninstitutionalized US children aged 6 to 17 years.
Results
Parent Report of Health Care Provider Diagnosis of Anxiety and Depression over Time
Among children aged 6 to 17 years, the prevalence of ever being diagnosed with anxiety or depression increased from 5.4% (confidence interval [CI]: 5.1–5.7) in 2003 to 7.8% (CI: 7.3–8.4) in 2007 and to 8.4% (CI: 8.0–8.9) in 2011–2012; this is a 56% increase in diagnosed prevalence from 2003 to 2011–2012. Similarly, current anxiety or depression increased 13% from 4.7% (CI: 4.3–5.1) in 2007 and to 5.3% in 2011–2012 (p < 0.05). Separate estimates for individual diagnoses were as follows: current anxiety increased 19% from 3.5% (95% CI: 3.2–3.9) in 2007 to 4.1% in 2011–2012 (p < 0.01); ever-diagnosed anxiety increased 17% from 5.5% (CI: 5.1–6.0) to 6.4% (p < 0.01); current depression did not change significantly from 2007 (2.5%, CI: 2.2–2.8) to 2011–2012 (2.7%, p = 0.18, p > 0.05); and ever-diagnosed depression did not change significantly from 4.7% (CI: 4.3–5.2) in 2007 to 4.9% (CI: 4.5–5.3) in 2011–2012 (p > 0.05). These estimates correspond with approximately 2 million children aged 6 to 17 years in 2011–2012 with current anxiety, 1.4 million children with current depression, 2.6 million with current anxiety or depression, and 760,000 children with both.
Characteristics of Children with the Parent Report of Health Care Provider–Diagnosed Anxiety or Depression
Anxiety and depression among children aged 6 to 17 years varied by sociodemographic characteristics (Table 1). Current depression and current anxiety were more common among older children and those living in households with lower income. Current depression was more common among children living in households with lower parental education. Current anxiety and either anxiety or depression were more common among white non-Hispanic children and less common among children without health care coverage and children living in the West compared with the Northeast. The sociodemographic patterns were similar for ever-diagnosed depression or anxiety with 1 exception; higher parental education was associated with ever-diagnosed anxiety ( , p < 0.05).
Overall, sex was not significantly associated with anxiety or depression. Age-stratified post hoc analyses were conducted to identify more specific relationships between sex and internalizing disorders, given previously documented associations.12 Boys aged 6 to 11 years were more likely than girls of the same age to have depression ( , p < 0.01), anxiety ( , p < 0.01), or either ( , p < 0.001); no differences were noted for children aged 12 to 17 years. Among children 15 to 17 years, current anxiety or depression was more common among girls (8.6% vs 6.7%; p < 0.05); there were no sex differences for either individual condition.
Children with anxiety or depression were more likely than those without either condition to have co-occurring conditions; this difference was significant for each individual condition (Table 2). Children with current anxiety or depression were more likely than those without anxiety or depression to be obese ( , p < 0.01, 21.2% vs 15.3%). Specifically, 25.4% of children with current depression were obese (adjusted PR [aPR] 5 1.7, CI: 1.3–2.2), whereas 20.5% of children with current anxiety were obese (aPR = 1.4, CI: 1.1–1.7).
After adjusting for sociodemographic factors, anxiety or depression was associated with indicators of impact with 1 exception: receiving preventive medical care (data not shown). After further adjusting for co-occurring conditions (Table 3), the findings remained significant, except for the associations between depression and seeing a specialist and having an unmet health care needs including mental health services, between anxiety and unmet medical care needs, and between either anxiety or depression and repeating a grade. Considering children with anxiety or depression, 25% did not receive mental health treatment or counseling; this decreased to 19% when including medication for emotion, concentration, or behavior. Children with anxiety or depression were less likely than those with other chronic health conditions to have a medical home (aPR = 0.7, CI: 0.6–0.8) or effective care coordination (aPR = 0.7, CI: 0.6–0.8).
Table 3. Selected Indicators of Impact Among US Children Aged 6-17 Years with and Without Parent-Reported Anxiety or Depression, Adjusting for the Presence of Other Neurobehavioral and Chronic Health Conditions, 2011–2012.
| Indicators of Health Care Use and Impact | Current Depression | Current Anxiety | Current Anxiety or Depression | No Current Anxiety or Depression | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||
| % (95% CI) | aPRa (95% CI) | % (95% CI) | aPRa (95% CI) | % (95% CI) | aPRa (95% CI) | % (95% CI) | |
| Meets criteria for children with special health care needs (CSHCN) | 84.3 (78.6–88.7) | 1.9 (1.5–2.4) | 85.6 (82.5–88.2) | 2.5 (2.2–2.8) | 83.9 (80.7–86.6) | 2.7 (2.5–3.0) | 20.4 (19.7–21.1) |
| Has condition that requires treatment or counseling | 84.8 (79.9–88.6) | 4.2 (3.1–5.8) | 77.4 (74.0–80.4) | 4.0 (3.3–4.9) | 77.7 (74.7–80.5) | 6.4 (5.6–7.4) | 7.2 (6.7–7.7) |
| High parenting aggravation (past month) | 36.2 (31.0–41.7) | 1.8 (1.3–2.4) | 32.8 (29.1–36.7) | 2.5 (1.9–3.2) | 32.1 (28.6–35.8) | 3.0 (2.5–3.6) | 6.5 (6.1–7.0) |
| Repeated a grade in school other than kindergarten | 20.4 (16.4–25.0) | 1.2 (0.8–1.7) | 13.7 (11.4–16.4) | 1.0 (0.7–1.3) | 16.0 (13.6–18.7) | 1.2 (0.9–1.5) | 6.2 (5.7–6.7) |
| Parent contacted about a school problemb | 70.8 (64.9–76.0) | 1.4 (1.2–1.6) | 69.7 (66.0–73.2) | 1.6 (1.4–1.8) | 68.6 (65.0–72.0) | 1.7 (1.6–1.9) | 29.5 (28.7–30.4) |
| Received preventive medical careb | 95.5 (92.2–97.4) | 1.0 (1.0–1.0) | 93.7 (90.7–95.8) | 1.0 (0.9–1.0) | 94.4 (91.9–96.1) | 1.0 (1.0–1.0) | 94.6 (94.2–95.0) |
| Received treatment or counseling from a mental health professionalb | 81.6 (77.1–85.3) | 4.7 (3.7–6.0) | 74.1 (70.7–77.3) | 4.2 (3.6–5.0) | 74.8 (71.7–77.7) | 6.6 (5.9–7.4) | 7.7 (7.2–8.2) |
| Taken medication for emotion, concentration, or behaviorb | 48.7 (41.7–55.8) | 6.4 (4.4–9.4) | 38.5 (33.8–43.4) | 4.6 (3.2–6.7) | 37.9 (33.7–42.4) | 11.7 (8.7–15.7) | 1.6 (1.4–1.9) |
| Either of the 2 treatments above (mental health professional or medication)b | 86.9 (82.5–90.3) | 4.7 (3.7–6.1) | 81.1 (77.7–84.0) | 4.3 (3.6–5.0) | 81.4 (78.4–84.0) | 6.2 (5.5–7.0) | 8.7 (8.2–9.3) |
| Seen a specialist (other than mental health)b | 37.6 (32.6–42.9) | 1.1 (0.9–1.3) | 42.8 (39.0–46.7) | 1.4 (1.2–1.6) | 39.8 (36.4–43.3) | 1.4 (1.2–1.6) | 22.7 (22.0–23.4) |
| Receives effective care coordination | 40.7 (35.3–46.4) | 0.8 (0.7–0.9) | 44.7 (40.7–48.7) | 0.8 (0.7–0.9) | 43.2 (39.5–47.0) | 0.7 (0.6–0.8) | 68.3 (67.0–69.6) |
| Has a medical home | 30.0 (25.1–35.4) | 0.8 (0.7–1.0) | 34.7 (31.0–38.5) | 0.8 (0.7–0.9) | 33.0 (29.7–36.4) | 0.7 (0.6–0.8) | 53.7 (52.7–54.6) |
| Has an unmet health care needb | 23.8 (19.8–28.4) | 1.3 (0.9–1.8) | 22.8 (19.9–26.0) | 2.3 (1.8–2.9) | 21.8 (19.1–24.7) | 2.3 (1.9–2.8) | 6.6 (6.2–7.1) |
| Unmet medical care needb | 11.4 (8.5–15.1) | 2.2 (1.4–3.5) | 8.0 (6.3–10.2) | 1.4 (1.0–2.1) | 8.1 (6.5–10.2) | 2.1 (1.5–2.8) | 3.1 (2.8–3.4) |
| Unmet mental health service needb | 11.0 (8.2–14.5) | 1.7 (0.9–2.9) | 11.6 (9.4–14.2) | 7.2 (4.2–12.4) | 10.7 (8.8–13.1) | 9.5 (6.4–14.1) | 0.6 (0.5–0.7) |
Data source: CDC/NCHS, National Survey of Children's Health, 2011–2012.
The aPR was adjusted for the following factors categorized as they are shown in Table 1, except race/ethnicity: age, sex, race/ethnicity (white non-Hispanic vs others), highest household education, household income (percent of federal poverty level), and presence of any other neurobehavioral or other chronic health conditions (Table 2). Depression models were also adjusted for anxiety; anxiety models were also adjusted for depression.
Parent reported on “past 12 months.” aPR, adjusted prevalence ratio; CDC, Centers for Disease Control and Prevention; CI, confidence interval; NCHS, National Center for Health Statistics.
Among children aged 6 to 17 years, parents described current depression as mild for 53.5%, moderate for 35.7%, and severe for 10.7%; current anxiety was mild for 48.0%, moderate for 36.8%, and severe for 15.2%. There was no association between depression severity and having a medical home; however, children with a medical home or effective care coordination were more likely to have mild anxiety, rather than moderate or severe (data not shown). After adjusting for the severity of both conditions, children with anxiety or depression, and without effective care coordination and a medical home, were more likely than those with a medical home or effective care coordination to have parents with high parenting aggravation and unmet health care needs, including mental health services (Fig. 1). Findings were similar when considering effective care coordination and medical home separately.
Figure 1.
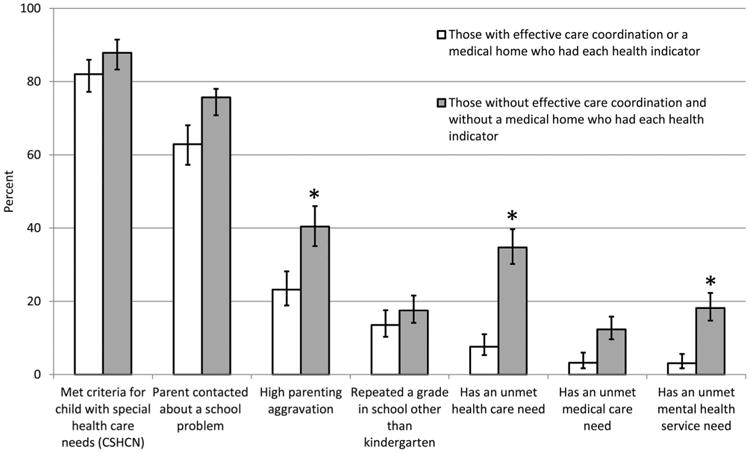
Selected indicators of impact among US children aged 6 to 17 years with parent-reported anxiety or depression with and without effective care coordination or a medical home, 2011–2012. Adjusted prevalence ratios and 95% confidence intervals comparing children with effective care coordination or a medical home to those without either were calculated, adjusting for the following factors categorized as they are shown in Table 1, except as noted: age, sex, race/ethnicity (white non-Hispanic vs others), highest household education, household income (percent of federal poverty level), insurance status (yes/no), and whether the child had severe depression or severe anxiety. *p < 0.001. Data source: CDC/NCHS, National Survey of Children's Health, 2011–2012. CDC, Centers for Disease Control and Prevention; NCHS, National Center for Health Statistics.
Discussion
This study presents national estimates of parent-reported, health care provider–diagnosed anxiety and depression over time and characterizes the impact of these disorders on children and families in 2011–2012. In 2011–2012, 5.3% of US children aged 6 to 17 years had current anxiety or depression, representing more than 2.6 million children. From 2007 to 2011–2012, the parent report of current anxiety diagnoses increased 19%; depression did not change.
Consistent with previous research,23 children with depression or anxiety were at increased risk of co-occurring neurobehavioral and chronic health conditions and obesity. Children with co-occurring neurobehavioral disorders are more likely than those without to have associated functional impairment and to use more services.10 Even after adjusting for co-occurring conditions, anxiety or depression was associated with greater health service use, school problems, and parenting aggravation. The identification and treatment of child anxiety or depression might improve overall health and well-being.24
Despite significant health care needs, nearly 20% of children with anxiety or depression did not receive mental health treatment in the past year; approximately 75% received “treatment or counseling from a mental health professional,” and nearly 38% had “taken medication for emotion, concentration, or behavior.” These estimates of mental health treatment are higher than those reported from the 2007 National Survey of Children's Health (NSCH)25 but align with observed increases in mental health service use during overlapping time periods.6,26 About one-third of children with anxiety or depression had a medical home, and less than half had effective care coordination. These findings extend 2007 NSCH results, showing that children with neurobehavioral disorders were less likely than those with other chronic health conditions to have a medical home or effective care coordination, both of which were associated with better family and health measures for children with anxiety and depression.22,27
The increase in diagnosed anxiety occurred alongside increases in diagnosed attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) 14,15 and other chronic health conditions28 among children. Children with multiple diagnoses may be more likely to be identified; increased awareness and development of evidence-based treatments for certain conditions may increase the identification of co-occurring conditions. An increase in ADHD and ASD specifically may increase the identification of anxiety either as a co-occurring condition or an alternate diagnosis. Notably, the prevalence of anxiety was higher in boys, reflecting the sex differences observed for both ADHD and ASD.14,15
The increases in parent-reported diagnosed anxiety do not necessarily reflect an increase in anxiety symptoms but may reflect improved identification of anxiety, increased diagnosis of mild anxiety, or increased mental health service use over the same time period.6,26 The reason for this increase cannot be determined from these data. Despite the increase in diagnosed anxiety, the estimates reported here are lower than community-based studies,1,10 suggesting that child anxiety may be underdiagnosed. By contrast, ADHD estimates from community-based studies and parent-reported surveys are similar, possibly reflecting better identification.29 Pediatric ADHD treatment guidelines30 may contribute to the increased comfort level of pediatricians diagnosing ADHD relative to anxiety or depression. Furthermore, because of the externalizing nature of ADHD symptoms, ADHD may be more likely to cause school impairment and may therefore come to the attention of teachers and parents.
Findings should be interpreted considering certain limitations. Child anxiety and depression relied on the parent report of being told by a health care provider that their child had the specified condition. This requires the child have health care access, that a child is appropriately assessed for a condition, that the health care provider clearly communicates this to the parent, that the parent recalls the diagnosis at the time of the interview, and that the parent is comfortable sharing potentially sensitive information. Parents were asked about “anxiety problems”; although reporting on “problems” rather than a “disorder” might lead to increased estimates, requiring that the parent heard this from a health care provider may result in decreased estimates. A related limitation is the lack of data on specific anxiety disorders. The cross-sectional nature of the data does not allow for interpretations about causality. The NSCH methodology differed across waves in ways that may have introduced bias on reported estimates (e.g., parents responded to a single question about anxiety or depression in 2003, but the conditions were separated in subsequent waves). Second, the number of cell-only households increased during the study period31; only the 2011–2012 sample included cell-only households. Third, overall response rates declined over time. Sample weights included adjustments to account for possible coverage and non-response biases.16 In analyses of nonresponse bias, the bias across multiple key variables in the NSCH was determined to be smaller than the potential sampling error.16
In conclusion, more than 1 in 20 US children aged 6 to 17 years had diagnosed current anxiety or depression in 2011–2012 by the parent report. The high degree of comorbidity of anxiety and depression, significant impact beginning during childhood, and increasing prevalence of diagnosed anxiety collectively demonstrate the public health impact of these disorders. Early intervention and prevention efforts can improve health outcomes among children with these conditions.3 The integration of mental health and primary care may improve outcomes for children with anxiety and depression.32 Consistent with professional guidelines, assessing for anxiety and depression among children with other neurobehavioral and chronic health conditions may be beneficial.3 Research is needed to identify factors associated with an increased prevalence of diagnosed anxiety and how systems and practice-level interventions, such as care coordination, brief pediatrician-delivered interventions,33 and online parent support interventions,34 can be leveraged to improve the health and well-being of children with anxiety and depression.
Acknowledgments
Disclosure: J. Walkup has received free drug/placebo from the following pharmaceutical companies for National Institute of Mental Health-funded studies: Eli Lilly (2003), Pfizer (2007), and Abbott (2005). J. Walkup is a paid speaker of the Tourette Association of America—Centers for Disease Control and Prevention outreach educational programs, the American Academy of Child and Adolescent Psychiatry, and the American Psychiatric Association. J. Walkup also receives grant funding from the Hartwell Foundation and the Tourette Association of America. J. Walkup receives royalties for books on Tourette syndrome from Guilford Press and Oxford Press and for educational materials from Wolters Kluwer. He is also an unpaid advisor to the Anxiety Disorders Association of America, the Trichotillomania Learning Center, and the American Foundation of Suicide Prevention. There was no funding for these analyses or writing of the manuscript.
Footnotes
The remaining authors declare no conflicts of interest.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Health Resources and Services Administration.
References
- 1.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the national comorbidity survey replication–adolescent supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 5th. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 3.Birmaher B, Brent D, AACAP Work Group on Quality Issues et al. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46:1503–1526. doi: 10.1097/chi.0b013e318145ae1c. [DOI] [PubMed] [Google Scholar]
- 4.Pinquart M, Shen Y. Depressive symptoms in children and adolescents with chronic physical illness: an updated meta-analysis. J Pediatr Psychol. 2011;36:375–384. doi: 10.1093/jpepsy/jsq104. [DOI] [PubMed] [Google Scholar]
- 5.Smith JP, Smith GC. Long-term economic costs of psychological problems during childhood. Soc Sci Med. 2010;71:110–115. doi: 10.1016/j.socscimed.2010.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bui AL, Dieleman JL, Hamavid H, et al. Spending on children's personal health care in the United States, 1996-2013. JAMA Pediatr. 2017;171:181–189. doi: 10.1001/jamapediatrics.2016.4086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jonsson U, Bohman H, von Knorring L, et al. Mental health outcome of long-term and episodic adolescent depression: 15-year follow-up of a community sample. J Affect Disord. 2011;130:395–404. doi: 10.1016/j.jad.2010.10.046. [DOI] [PubMed] [Google Scholar]
- 8.Sheldrick RC, Perrin EC. Medical home services for children with behavioral health conditions. J Dev Behav Pediatr. 2010;31:92–99. doi: 10.1097/DBP.0b013e3181cdabda. [DOI] [PubMed] [Google Scholar]
- 9.American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP) et al. Joint principles of the patient centered medical home. [Accessed Novemer 3, 2017];2007 Available at: http://www.pcpcc.net/content/joint-principles-patient-centered-medical-home.
- 10.Costello JE, Mustillo S, Keeler G, et al. Prevalence of psychiatric disorders in childhood and adolescence. In: Levin BL, Petrila J, Hennessy KD, editors. Mental Health Services: A Public Health Perspective. 2nd. New York, NY: Oxford University Press; 2004. [Google Scholar]
- 11.Holbrook JR, Bitsko RH, Danielson ML, et al. Interpreting the prevalence of mental disorders in children: tribulation and triangulation. Health Promot Pract. 2017;18:5–7. doi: 10.1177/1524839916677730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perou R, Bitsko RH, Blumberg SJ, et al. Mental health surveillance among children–United States, 2005-2011. MMWR Suppl. 2013;62:1–35. [PubMed] [Google Scholar]
- 13.Center for Behavioral Health Statistics and Quality. Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. Rockville, MD: HHS, SAMHSA; 2016. [Google Scholar]
- 14.Blumberg SJ, Bramlett MD, Kogan MD, et al. Changes in prevalence of parent-reported autism spectrum disorder in school-aged U.S. children: 2007 to 2011–2012. Natl Health Stat Report. 2013:1–11. [PubMed] [Google Scholar]
- 15.Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry. 2014;53:34–46.e32. doi: 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bramlett MD, Blumberg SJ, Zablotsky B, et al. Design and operation of the national survey of Children's health, 2011–2012. Vital Health Stat 1. 2017:1–256. [PubMed] [Google Scholar]
- 17.Blumberg SJ, Foster EB, Frasier AM, et al. Design and operation of the national survey of Children's health, 2007. Vital Health Stat 1. 2012:1–149. [PubMed] [Google Scholar]
- 18.Blumberg SJ, Olson L, Frankel MR, et al. Design and operation of the national survey of Children's health, 2003. Vital Health Stat 1. 2005:1–131. [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. About BMI for children and teens. [Accessed October 30, 2017];2011 Available at: http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html.
- 20.Bethell CD, Read D, Stein RE, et al. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr. 2002;2:38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 21.Robinson LR, Bitsko RH, Schieve LA, et al. Tourette syndrome, parenting aggravation, and the contribution of co-occurring conditions among a nationally representative sample. Disabil Health J. 2013;6:26–35. doi: 10.1016/j.dhjo.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adams SH, Newacheck PW, Park MJ, et al. Medical home for adolescents: low attainment rates for those with mental health problems and other vulnerable groups. Acad Pediatr. 2013;13:113–121. doi: 10.1016/j.acap.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Kendall PC, Compton SN, Walkup JT, et al. Clinical characteristics of anxiety disordered youth. J Anxiety Disord. 2010;24:360–365. doi: 10.1016/j.janxdis.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keeton CP, Ginsburg GS, Drake KL, et al. Benefits of child-focused anxiety treatments for parents and family functioning. Depress Anxiety. 2013;30:865–872. doi: 10.1002/da.22055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghandour RM, Kogan MD, Blumberg SJ, et al. Mental health conditions among school-aged children: geographic and sociodemographic patterns in prevalence and treatment. J Dev Behav Pediatr. 2011;33:42–54. doi: 10.1097/DBP.0b013e31823e18fd. [DOI] [PubMed] [Google Scholar]
- 26.Ghandour RM, Perry DF, Kogan MD, et al. The medical home as a mediator of the relation between mental health symptoms and family burden among children with special health care needs. Acad Pediatr. 2011;11:161–169. doi: 10.1016/j.acap.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 27.Health Care Cost Institute. Washington, DC: 2012. [Accessed November 3, 2017]. Children's Health Care Spending Report: 2007—2010. Available at: http://www.healthcostinstitute.org/files/HCCI_CHCSR20072010.pdf. [Google Scholar]
- 28.Bloomgarden ZT. Type 2 diabetes in the young: the evolving epidemic. Diabetes Care. 2004;27:998–1010. doi: 10.2337/diacare.27.4.998. [DOI] [PubMed] [Google Scholar]
- 29.Walkup JT, Stossel L, Rendleman R. Beyond rising rates: personalized medicine and public health approaches to the diagnosis and treatment of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2014;53:14–16. doi: 10.1016/j.jaac.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 30.American Academy of Pediatrics. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blumberg SJ, Luke JV. National Center for Health Statistics; 2013. [Accessed November 3, 2017]. Wireless Substitution: Early Release of Estimates from the National Health Interview Survey, July–December 2012. Available at: http://www.cdc.gov/nchs/nhis.htm. [Google Scholar]
- 32.Asarnow JR, Rozenman M, Wiblin J, et al. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: a meta-analysis. JAMA Pediatr. 2015;169:929–937. doi: 10.1001/jamapediatrics.2015.1141. [DOI] [PubMed] [Google Scholar]
- 33.Ginsburg GS, Drake K, Winegrad H, et al. An open trial of the anxiety action plan (AxAP): a brief pediatrician-delivered intervention for anxious youth. Child Youth Care Forum. 2016;45:19–32. doi: 10.1007/s10566-015-9320-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yap MB, Lawrence KA, Rapee RM, et al. Partners in parenting: a multi-level web-based approach to support parents in prevention and early intervention for adolescent depression and anxiety. JMIR Ment Health. 2017;4:e59. doi: 10.2196/mental.8492. [DOI] [PMC free article] [PubMed] [Google Scholar]


