Endoscopic submucosal dissection (ESD) is a minimally invasive endoscopic treatment that provides 1-piece resection of early GI neoplasms. ESD requires high endoscopic skill because it is a “1-hand” surgical procedure, meaning that it is performed without any traction except for gravity. Surgeons usually use both hands to obtain adequate traction when they use an electrosurgical knife. In the past, several traction methods have been reported.1, 2, 3 The dental floss clip (DFC) method is a newly developed traction method. Previous reports have demonstrated the effectiveness of the DFC method for gastric lesions.4, 5 In addition, dental floss is a reasonable and easy-to-purchase device. We herein report a case of recurrent cecal tumor that was successfully treated with ESD and the use of a modified DFC method.
A 71-year-old woman underwent colonoscopy for the diagnosis of laterally spreading tumor, nongranular type (LST-NG) in the cecum (Fig. 1A). The tumor showed a tubular pit pattern (IIIL and IIIS, Kudo classification). Initial endoscopic treatment was performed by piecemeal endoscopic mucosal resection (p-EMR) and argon plasma coagulation (APC) (Figs. 1B and C). The resected specimen showed intramucosal cancer. After the initial treatment, closed endoscopic follow-up was planned. The initial follow-up examination revealed no recurrent tumor on the previous p-EMR scar. However, 11 months after the initial treatment, the tumor recurred (Figs. 2A and B). The recurrent tumor demonstrated remarkable converging folds, suggesting passivity of submucosal invasion and severe fibrosis in the submucosal layer. Salvage EMR was considered technically difficult because of the severe submucosal fibrosis caused by the initial p-EMR. Diagnostic ESD was therefore planned before surgical intervention. A mixture of hyaluronic acid, glycerol, and indigo carmine was used for submucosal injection. The electrosurgical generator (VIO 300D, ERBE Elektromedizin GmbH, Tubingen, Germany) was set at endocut I (effect 2, duration 2, interval 2) for mucosal incision and swift coagulation and at (effect 2, 35 W) for submucosal dissection. Hemostasis was performed with the use of soft coagulation (effect 6, 70 W). A circumferential mucosal incision was conducted with a 1.5-mm dual knife (KD-650U, Olympus Medical Systems). A submucosal dissection was performed with a dual knife and an ITknife nano (KD-612U, Olympus, Tokyo, Japan). A mucosal incision was performed away from the fibrotic area to obtain adequate mucosal lift and avoid perforation (Fig. 3A). The submucosal fibrosis was severe and widespread in the post–p-EMR area. The DFC method was then attempted to unfold the mucosal flap and confirm the submucosal layer directly. However, adequate traction could not be obtained with the conventional DFC method. Therefore, additional clipping was performed at the opposite colon wall to obtain a pulley-like effect (Figs. 3B, C, and D; Video 1, available online at www.VideoGIE.org). Finally, the submucosal dissection was completed without adverse events (Fig. 3E). Histologic examination revealed deep submucosal invasion with negative vertical and horizontal margins (Fig. 4). An additional surgical resection with lymph node dissection was performed because of the possibility of lymph node metastasis. The surgical specimen showed no residual tumor and no lymph node metastasis.
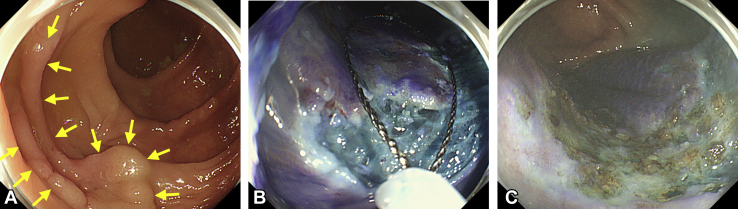
Figure 1.
Laterally spreading tumor in the cecum. A, Conventional endoscopic image showing widespread tumor, approximately 4 cm in diameter. The yellow arrows indicate the edge of the lesion. B, C, Endoscopic piecemeal resection and argon plasma coagulation performed after endoscopic image was magnified by crystal violet staining.
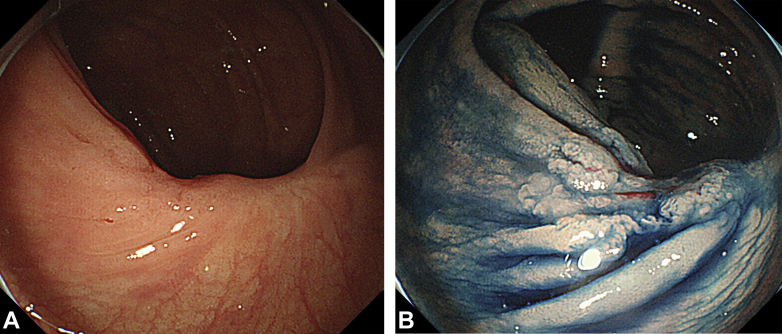
Figure 2.
Recurrent tumor on the endoscopic piecemeal mucosal resection scar 11 months later. A, Follow-up colonoscopic image showing shallow depressed lesion with a slightly reddish change. B, Dye-sprayed endoscopic image clearly shows margin of recurrent tumor.
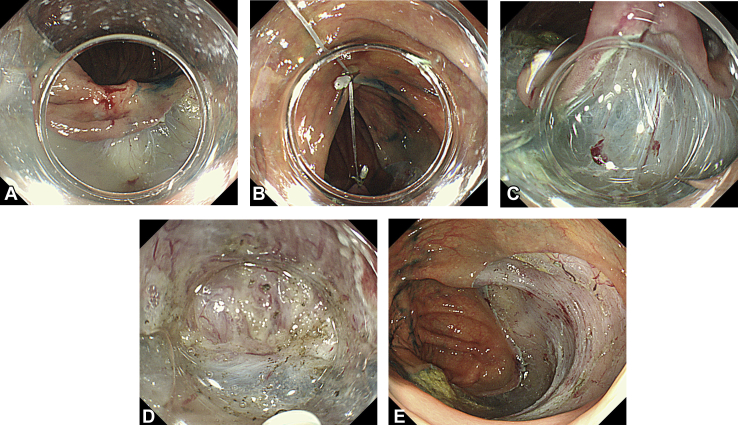
Figure 3.
Salvage endoscopic submucosal dissection for recurrent tumor. A, Mucosal incision around recurrent tumor. B, Dental floss clip attached to edge of mucosal flap, additional clipping applied on the opposite colon wall. Pulley-like effect obtained, and dental floss clip method used to unfold the mucosal flap. C, Direct confirmation of submucosal layer. D, Severely fibrotic area dissected without perforation. E, Complete resection achieved.
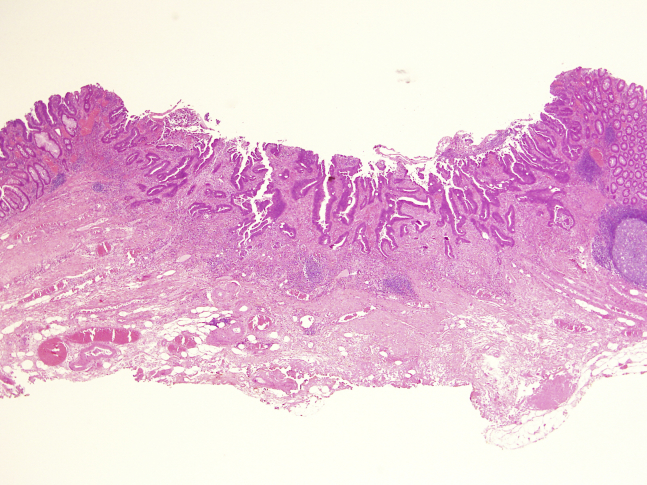
Figure 4.
Pathologic view showing deep submucosal invasion with negative vertical margin (H&E, orig. mag. × 40).
In this decade, ESD has been widely accepted, and many supportive devices have been developed. ESD for lesions of the cecum is technically difficult because the endoscope is placed perpendicular to the cecal wall. Moreover, breathing movements are an obstacle to the procedure and make stabilization of the endoscopic view difficult. In this case, the previous p-EMR area showed severe fibrosis, and unexpected submucosal invasion of the recurrent tumor complicated the submucosal dissection. Our experience showed that the conventional DFC method was not useful for the cecum. In this case, an additional clip modification was successfully applied, the recurrent tumor was finally removed with a negative vertical margin, and adequate pathologic assessment was possible. Additional surgical intervention with lymph node dissection is recommended.
The advantages of this DFC method include the convenience in procuring the device and its relatively inexpensive cost. However, its disadvantages include the necessity of withdrawing and reinserting the endoscope. If reinsertion is difficult (eg, because of a long colon or adhesions), the DFC method should not be used, especially in the cecum and ascending colon.
Generally, the majority of recurrent tumors after p-EMR occur as tiny lesions. Nevertheless, in this case, the recurrent tumor invaded the submucosal layer within a short time (11 months). Pathologic assessment was not performed in the APC-treated area because EMR could not be accomplished. It is possible that submucosal invasion already existed in the APC-treated area during the initial treatment. Uraoka et al6 reported that an LST-NG invades the submucosa multifocally and recommended that an LST-NG should be removed as an en bloc specimen.
In conclusion, ESD with the pulley-like DFC method described herein is a promising approach to remove neoplasms in the cecum.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Modified dental floss method for recurrent tumor.
References
- 1.Sakamoto N., Osada T., Shibuya T. Endoscopic submucosal dissection of large colorectal tumors by using a novel spring-action S-O clip for traction (with video) Gastrointest Endosc. 2009;69:1370–1374. doi: 10.1016/j.gie.2008.12.245. [DOI] [PubMed] [Google Scholar]
- 2.Saito Y., Emura F., Matsuda T. A new sinker-assisted endoscopic submucosal dissection for colorectal cancer. Gastrointest Endosc. 2005;62:297–301. doi: 10.1016/s0016-5107(05)00546-8. [DOI] [PubMed] [Google Scholar]
- 3.Gotoda T., Oda I., Tamakawa K. Prospective clinical trial of magnetic-anchor-guided endoscopic submucosal dissection for large early gastric cancer (with videos) Gastrointest Endosc. 2009;69:10–15. doi: 10.1016/j.gie.2008.03.1127. [DOI] [PubMed] [Google Scholar]
- 4.Suzuki S., Gotoda T., Kobayashi Y. Usefulness of a traction method using dental floss and a hemoclip for gastric endoscopic submucosal dissection: a propensity score matching analysis (with videos) Gastrointest Endosc. 2016;83:337–346. doi: 10.1016/j.gie.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Yoshida M., Takizawa K., Ono H. Efficacy of endoscopic submucosal dissection with dental floss clip traction for gastric epithelial neoplasia: a pilot study (with video) Surg Endosc. 2016;30:3100–3106. doi: 10.1007/s00464-015-4580-4. [DOI] [PubMed] [Google Scholar]
- 6.Uraoka T., Saito Y., Matsuda T. Endoscopic indications for endoscopic mucosal resection of laterally spreading tumours in the colorectum. Gut. 2006;55:1592–1597. doi: 10.1136/gut.2005.087452. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Modified dental floss method for recurrent tumor.