Abstract
Brain metastases and/or leptomeningeal disease (LMD) with associated central nervous system (CNS) metastases are known complications of advanced epidermal growth factor receptor (EGFR) mutation-positive non-small cell lung cancer (NSCLC). It is important, therefore, to assess the activity of EGFR tyrosine kinase inhibitors (TKIs) versus such CNS complications. This review explores the literature reporting the intracranial activity of EGFR TKIs, and finds that there is evidence for varying efficacy of the approved agents, erlotinib, gefitinib, afatinib, and osimertinib in patients with CNS metastases. Other EGFR TKIs in development, such as AZD3759, may have a future role as therapeutic options in this setting. Emerging evidence indicates that the second- and third-generation EGFR TKIs, afatinib and osimertinib, effectively penetrate the blood-brain barrier, and therefore represent viable treatment options for CNS lesions, and can reduce the risk of CNS progression. These agents should therefore be considered as first-line treatment options in patients with EGFR mutation-positive NSCLC who have brain metastases and/or LMD. While there are currently no prospective data comparing the intracranial efficacy of second- and third-generation EGFR TKIs in this setting, CNS activity and protection offered by different EGFR TKIs should be an additional consideration when making decisions about the optimal sequence of treatment with EGFR TKIs in order to maximize survival benefit in individual patients.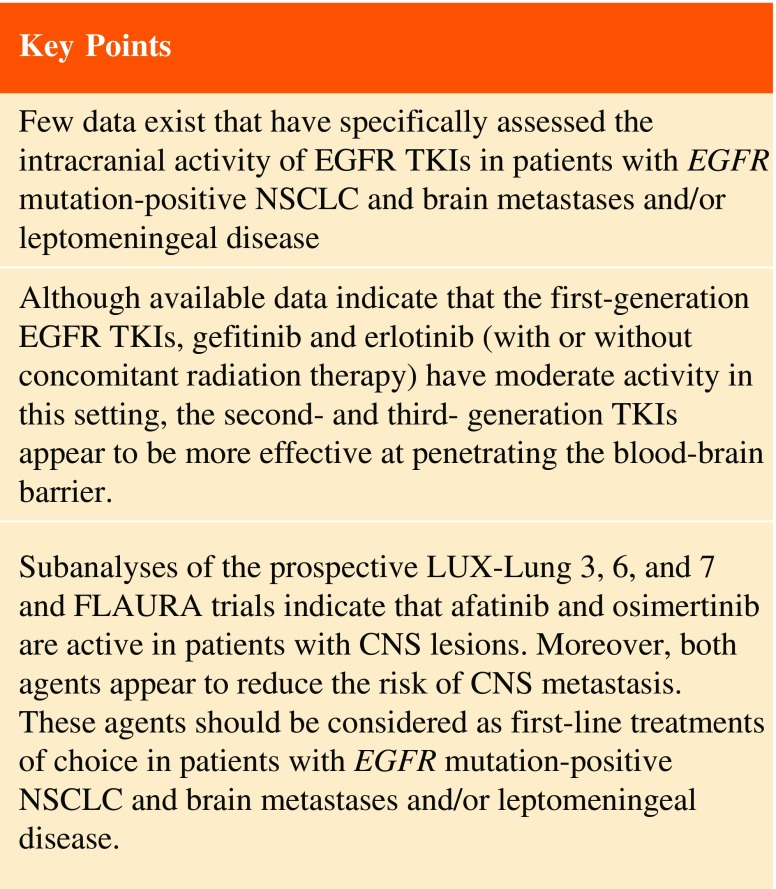
Introduction
The brain is a common site of metastatic spread in patients with advanced non-small cell lung cancer (NSCLC), with brain metastases affecting more than 25% of patients during the course of their disease [1]. NSCLC brain metastases can cause neurological symptoms and an associated deterioration in quality of life, while prognosis is poor for these patients, with a median survival after diagnosis ranging between 1 and 5 months [1–7]. The most common approaches to the treatment of brain metastases are radiation therapy (RT), including whole-brain radiation therapy (WBRT) and stereotactic radiosurgery (SRS), and surgical resection. However, recent evidence has shown that WBRT does not improve overall survival (OS) or overall quality of life compared with supportive care [8]. In practice, the specific therapeutic approach adopted tends to depend on the site and number of lesions [9–12]; for example, SRS is only recommended in the event of a small number of isolated lesions of maximum diameter 4 cm [9].
A small proportion (1–10%) of NSCLC patients develop leptomeningeal disease (LMD), also known as leptomeningeal carcinomatosis (LMC) or neoplastic meningitis, which results from the spread of tumor cells to the leptomeninges, subarachnoid space, and cerebrospinal fluid (CSF) [13–15]. As with brain metastases, prognosis for patients with LMD is poor. Suggested treatment options for patients with LMD include RT, surgery, and intrathecal chemotherapy, but the efficacy of these treatments is limited and no consensus has been reached regarding the best therapeutic strategy [16–19]. In general, traditional chemotherapeutic agents used to treat NSCLC do not cross the blood-brain barrier (BBB), so their role in the treatment of central nervous system (CNS) metastases is limited [20, 21]. However, in some cases, tumor neoangiogenesis and damage of the BBB due to tumor growth may allow chemotherapy drugs to penetrate the CNS, supporting their use in certain patients [22, 23].
A higher incidence of brain metastases has been reported in patients with NSCLC harboring epidermal growth factor receptor (EGFR) mutations compared with EGFR wild-type (WT) tumors, both at the time of diagnosis and during the course of the disease [24–30]. Interestingly, in general, median OS after diagnosis of brain metastases is significantly longer in patients with EGFR mutation-positive versus EGFR WT tumors [24–30]. Consequently, EGFR-targeted agents, in particular EGFR tyrosine kinase inhibitors (TKIs)—which are an established systemic treatment options for patients with EGFR mutation-positive NSCLC—are of interest in the treatment of brain or CNS metastases in this setting.
This review will explore clinical and preclinical evidence for the activity of EGFR TKIs in the treatment of patients with EGFR mutation-positive NSCLC and brain metastases and/or LMD, including their ability to penetrate the BBB, and efficacy outcomes reported in clinical trials, Compassionate Use Program (CUP) settings, and case series/studies.
First-Generation EGFR TKIs
Activity of Erlotinib and Gefitinib in Patients with NSCLC and CNS Metastases
The first-generation, reversible EGFR TKIs erlotinib and gefitinib are able to cross the BBB, although, after administration of standard doses, their concentrations in the CSF are limited compared with those in plasma [31–35]. Both drugs have shown some evidence of intracranial activity in patients with NSCLC. Numerous small trials, retrospective analyses, and case studies assessing the efficacy and safety of gefitinib and erlotinib in patients with brain metastases have been described; these studies are detailed in Table 1 and some of these results are described below.
Table 1.
Summary of studies reporting the efficacy of first-generation EGFR TKIs in patients with NSCLC and CNS metastases
| EGFR TKI | Publication | Study description | Treatments | Patient characteristics | Results | |
|---|---|---|---|---|---|---|
| Name/type | Phase | |||||
| Gefitinib | Iuchi et al. [39] | II | Gefitinib (250 mg QD) | N = 41; EGFR mutation-positive, TKI-naïve patients with brain metastases; surgical resection of the brain did not preclude participation | • ORR: 87.8% • Median PFS: 14.5 months; Del19 was associated with improved PFS vs. L858R (17.5 vs. 10.2 months, respectively; P = 0.003) • Median OS: 21.9 months; Del19 was associated with improved survival vs. L858R (30.3 vs. 19.8, respectively; P = 0.025) |
|
| Ceresoli et al. [50] | Prospective trial | Gefitinib (250 mg QD) with or without prior WBRT | N = 41 (18 with prior WBRT, 37 with prior chemotherapy); patients with NSCLC and brain metastases | • ORR: PR, 10%; SD, 17% • DCR: 27%; higher DCR in patients with prior WBRT • Median PFS: 3 months |
||
| Erlotinib | Deng et al. [32] | Erlotinib (150 mg QD), following first- or second-line chemotherapy | N = 6 (n = 4 with EGFR mutations); patients with NSCLC and brain metastases | • ORR: WT EGFR, 33.3%; mutant EGFR, 50% • Brain metastases response: PR, 33.3%; SD, 33.3% • Median PFS: overall, 2.8 months; mutant EGFR, 5.6 months |
||
| Porta et al. [103] | Retrospective analysis of patients from the Spanish Lung Adenocarcinoma Data Base (SLADB) study | First- and second-line erlotinib (150 mg QD) | N = 69 (n = 17 with EGFR mutations); patients with NSCLC and brain metastases | • OR: 14 patients, all of whom had EGFR mutations (14/17; 82.4%) • In patients with EGFR mutations: PR, 35.3%; CR, 47.1%; SD, 17.6% • In patients with EGFR mutations, median PFS: 11.7 months |
||
| Ohara et al. [104] | Case report | Fourth-line erlotinib (150 mg QD), following progression after gefitinib, chemotherapy, and RT | Female, Japanese patient with T790M-positive NSCLC and brain metastasis | • Neurological symptoms (disorientation) resolved • Brain metastases disappeared, but extracranial (lung) primary lesion progressed, resulting in treatment discontinuation |
||
| Ruppert et al. [105] | Case report | Third-line erlotinib (150 mg QD), following gefitinib and chemotherapy | Male with del19 mutant NSCLC with brain metastasis; secondary T790M mutation was identified after stopping EGFR TKI, consistent with development of resistance | • Prolonged disease control (4 months), until liver metastases were detected | ||
| Katayama et al. [106] | Retrospective analysis | Erlotinib (150 mg QD), following prior gefitinib therapy | N = 7; 6 patients with EGFR mutation-positive NSCLC (1 patient EGFR mutational status not available) with brain metastases or LMD; 6 patients had prior WBRT or radiosurgery | • ORR: PR, 3 patients; SD, 3 patients • ECOG PS score improved in 3 patients • Neurological symptoms improved in 5 patients |
||
| Gefitinib or erlotinib | Park et al. [36] | Prospective study of first-line EGFR TKI | II | First-line gefitinib (250 mg QD) or erlotinib (150 mg QD) | 28; patients with common EGFR mutations and metastatic brain tumors | • ORR: PR, 83%; SD, 11% • Median PFS: 6.6 months • Median OS: 15.9 months; no differences in survival between gefitinib and erlotinib |
| Kim et al. [37] | II | First-line gefitinib (250 mg QD) or erlotinib (150 mg QD) | N = 23; Korean, never-smoking patients with brain metastases | • ORR: PR, 70%; SD, 13% • Median PFS: 7.1 months • Median OS: 18.8 months |
||
| Zhang et al. [38] | Retrospective analysis | First-line gefitinib (250 mg QD) or erlotinib (150 mg QD) | N = 81; patients with EGFR mutant NSCLC and brain metastases | • Median PFS: gefitinib, 9.5 months; erlotinib, 9.0 months • Median PFS (overall treatments): Del19, 10.4 months; L858R, 8.6 months (P = 0.408) |
||
| Gefitinib or erlotinib + RT | Zhu et al. [58] | Retrospective analysis | Gefitinib (250 mg QD) or erlotinib (150 mg QD) WBRT (30–40 Gy in 10–20 fractions, 5 days/week) or SRS (15–24 Gy) |
N = 133 (EGFR TKI alone, n = 66; EGFR TKI + WBRT, n = 63; EGFR TKI + SRS, n = 4); patients with EGFR mutations and brain metastases | • Median intracranial PFS: TKI + RT, 16.0 months; TKI, 11.5 months (P = 0.017) • Median OS: TKI + RT, 22 months; TKI, 15 months (P = 0.015) • Exon 21 mutations: Median PFS and OS were longer with TKI + RT than TKI alone (PFS: 14 vs. 9.5 months, P = 0.001; OS: 22 vs. 13.5 months, P = 0.004) |
|
| Ma et al. [53] | II | Gefitinib (250 mg QD with WBRT (40 Gy/20f/4w) | N = 21; patients with NSCLC and brain metastases | • ORR: 81% • PR, 62%; CR, 19%; SD, 14% • Median PFS: 10.0 months • Median OS: 13.0 months |
||
| Welsh et al. [54] | II | Erlotinib (150 mg QD) + WBRT | N = 40; patients with NSCLC and brain metastases | • ORR: 86% • Median PFS: overall, 8.0 months; EGFR mutant, 12.3 months; EGFR WT, 5.2 months • Median OS: overall, 11.8 months; EGFR mutant, 19.1 months; EGFR WT, 9.3 months |
||
| Zeng et al. [57] | Retrospective analysis | Gefitinib (250 mg QD) with or without WBRT (40 Gy/20f/4w) | N = 90; patients with NSCLC and brain metastases | • ORR: 64.4% vs. 26.7% (P < 0.001) for gefitinib + WBRT vs. gefitinib • DCR for brain metastases: 71.1% vs. 42.2% (P = 0.006) for gefitinib + WBRT vs. gefitinib • Longer time to progression of brain metastases with gefitinib + WBRT vs. gefitinib (10.6 vs. 6.6 months) • Longer median OS with gefitinib + WBRT vs. gefitinib (23.4 vs. 14.8 months) |
||
| Olmez et al. [56] | Retrospective analysis | Erlotinib (150 mg QD) + WBRT | N = 7; patients with NSCLC and brain metastases | • All patients had intracranial disease control • In extracranial sites: PR, 3 patients; SD, 2 patients |
||
| Lee et al. [51] | II | Erlotinib (100 mg QD) + WBRT (20 Gy/5f), then erlotinib (150 mg QD) | N = 80 (erlotinib, n = 40; placebo, n = 40); patients with NSCLC and brain metastases | • Median neurological PFS: 1.6 months for erlotinib or placebo • Median OS: erlotinib, 3.4 months; placebo, 2.9 months |
||
| Lind et al. [52] | Dose-escalation study | I | Erlotinib (100 mg QD or 150 mg QD) + WBRT (30 Gy/10f) | N = 11; patients with NSCLC and brain metastases | • Only 1 patient had intracranial progression; 6 patients had extracranial progression • Median PFS: 4.6 months • Median OS: 4.4 months • In 7 patients with follow-up neuroimaging: PR, 5 patients; SD, 2 patients |
|
| Zhuang et al. [55] | Prospective cohort study | II | WBRT (30 Gy/10f) with or without second-line erlotinib (150 mg QD) following failure of chemotherapy | N = 54 (WBRT, n = 31; WBRT + erlotinib, n = 23); patients with NSCLC and brain metastases; patients treated with erlotinib had EGFR mutations | • ORR: WBRT, 54.8% (PR, 41.9%; CR, 12.9%; SD, 38.7%; WBRT + erlotinib, 95.7% (PR, 60.9%; CR, 34.8%; SD, 4.4%) • Median intracranial PFS: WBRT, 6.8 months; WBRT + erlotinib, 10.6 months • Median overall PFS: WBRT, 5.2 months; WBRT + erlotinib, 6.8 months • Median OS: WBRT, 8.9 months; WBRT + erlotinib, 10.7 months |
|
| AZD3759 | Ahn et al. [107] | BLOOM | I | Third-line and beyond, AZD3759 (50–500 mg BID) | N = 29 (BM, 21; LM, 5; non-measurable/non-BM or LM, 3); patients with EGFR mutations | Overall: • Among 20 patients with BM: tumor shrinkage, 8; confirmed PR, 3; unconfirmed PR, 3 • Among 5 LM patients, 1 patient had CSF clearance of tumor cells and improvement of brain MRI imaging and CNS symptoms |
| Ahn et al. [64] | BLOOM | I, expansion cohort | AZD3759 (200–300 mg BID) in TKI-naïve patients | N = 20 (BM, 16; LM, 4), TKI-naïve patients with EGFR mutations and CNS metastases | • Confirmed disease control: 90% • Confirmed OR: 65% • Best response: PR, 65%; SD, 25% |
|
| Cho et al. [63] | BLOOM | I, expansion cohort | AZD3759 (200–300 mg BID) in TKI-naïve patients | N = 18, patients with EGFR mutations and LMD | • Best response: PR, 4; SD, 9; CR, 1 • 6/18 patients with extracranial tumors had tumor shrinkage but no confirmed response |
|
CNS central nervous system, DCR disease control rate, ECOG PS Eastern Cooperative Oncology Group performance status, EGFR epidermal growth factor receptor, NSCLC non-small cell lung cancer, ORR overall response rate, OR overall response, OS overall survival, PFS progression-free survival, PR partial response, QD once daily, RT radiation therapy, SD stable disease, SRS stereotactic radiosurgery, TKI tyrosine kinase inhibitor, WBRT whole-brain radiation therapy, WT wild-type
Several studies indicate that the first-generation EGFR TKIs may be active in patients with EGFR mutation-positive NSCLC who present with brain metastases, although there is a paucity of evidence for direct intracranial activity. For example, a prospective phase II study evaluated treatment with either erlotinib or gefitinib in 28 patients with EGFR mutation-positive NSCLC and brain metastases [36]. A systemic partial response (PR) was reported in 83% of patients, and stable disease (SD) in 11%. Median progression-free survival (PFS) was 6.6 months and median OS was 15.9 months, with no difference in survival outcomes between erlotinib and gefitinib. However, no information was provided on intracranial activity. A similar study in Korean patients who had never smoked, which also evaluated the efficacy of erlotinib and gefitinib in patients with NSCLC and brain metastases, showed median PFS of 7.1 months and median OS of 18.8 months, with 70% of patients achieving a PR and 13% achieving SD [37]. In a retrospective analysis of 81 patients with EGFR mutation-positive NSCLC and brain metastases, Zhang et al. reported similar median PFS in patients treated with gefitinib (9.5 months) or erlotinib (9.0 months) [38]. Another Japanese phase II study assessed gefitinib monotherapy in 41 patients with EGFR mutation-positive NSCLC and brain metastases [39]. Surgical resection of brain metastases did not preclude participation; unfortunately, no information was provided on surgical resections. Fifty-six percent of patients had between one and three intracranial lesions, and 44% of patients had four. A response rate of 87.8% was reported, with a median PFS of 14.5 months and a median OS of 21.9 months. As expected, given that it is a known marker of favorable prognosis in patients with EGFR mutation-positive NSCLC treated with EGFR TKIs [40, 41], presence of an EGFR Del19 mutation was associated with improved survival outcomes compared with the presence of an EGFR L858R mutation. In all of the brain metastasis studies, erlotinib and gefitinib were found to be tolerable, with no unexpected adverse events (AEs) reported. Some further retrospective analyses in unselected patients have also been published but are not discussed here, given their limitations. Administration of erlotinib with pulsed dosing has been investigated as a means of increasing CNS penetration. In patients with EGFR mutations, studies have shown that such treatment can delay CNS progression but does not improve PFS versus standard-dose erlotinib [42, 43].
Erlotinib and Gefitinib in Combination with RT
RT is thought to enhance the permeability of the BBB, thereby increasing the concentration of EGFR TKIs in the CSF [44, 45] and reducing the occurrence of the T790M mutation [46, 47]. Consequently, it is possible that EGFR TKI treatment in combination with RT may improve efficacy outcomes in patients with EGFR mutation-positive NSCLC and brain metastases. In preclinical studies, the combination of EGFR TKIs with RT has demonstrated a synergistic effect in human tumor cell lines and xenografts [48, 49]. Several clinical studies (Table 1) have shown that RT with concurrent erlotinib or gefitinib is well tolerated, and although there are few comparisons of EGFR TKI and RT combinations with EGFR TKIs or RT alone, the available studies have shown promising efficacy outcomes [50–57].
A recent retrospective analysis has assessed outcomes in patients with NSCLC and brain metastases who were treated with EGFR TKI treatment alone (n = 66) versus EGFR TKIs combined with RT (n = 67; 63 received WBRT and 4 received SRS) [58]. Median OS and intracranial PFS were significantly longer in the EGFR TKI plus RT group than in the EGFR TKI monotherapy group. Outcomes were also assessed according to EGFR mutation type, showing that, in patients with L858R mutations, the EGFR TKI plus RT group had significantly better median OS and intracranial PFS than the EGFR TKI monotherapy group, while there was no significant difference between treatment groups in patients with Del19 mutations. However, this study did not analyze AEs or changes in neurological symptoms or cognitive function with each treatment. Two other studies showed that combining erlotinib or gefitinib with WBRT resulted in enhanced efficacy, as demonstrated by longer median PFS, median OS, and longer duration of response overall [55–57]. Both of these studies also analyzed the safety profile and toxicity of RT combined with erlotinib/gefitinib; while some AEs were more common with combined therapy, they were mostly mild to moderate in severity. While these are interesting observations, the studies are limited by the retrospective nature of the analyses and the small scale of the studies. Further studies are required to provide additional insights into the efficacy of combined RT and first-generation EGFR TKIs in patients with NSCLC and brain metastases.
BBB-Penetrating First-Generation TKI: AZD3759
The search for drug candidates that are able to effectively penetrate the BBB and achieve effective concentrations in the CSF without unacceptable toxicities has resulted in the development of the selective EGFR inhibitor, AZD3759 [59, 60]. Preclinical and clinical experience with AZD3759 against CNS lesions is summarized below.
Preclinical studies of AZD3759 were performed with erlotinib as a comparator. In murine models of brain metastasis and LM, AZD3759 (15/mg/kg) exhibited excellent CNS penetration, and achieved concentrations above the pEGFR inhibitory concentration (IC50) for longer than 7 h, compared with 6 h or less for erlotinib [61]. AZD3759 was shown to cause tumor regression, and survival rates were significantly higher than those with erlotinib [61].
Currently, AZD3759 is undergoing clinical evaluation in the phase I BLOOM study, which is assessing both AZD3759 and the third-generation EGFR TKI osimertinib treatment in heavily pretreated patients with EGFR mutation-positive NSCLC who had progressed on prior EGFR TKI therapy and had a confirmed diagnosis of LMD [62]. Patients had mostly good ECOG PS (57% ECOG 0/1) and 48% had neurological symptoms. AZD3759 has been found to be well tolerated in patients with LMD previously treated with at least one line of EGFR TKI therapy and chemotherapy. One patient (6%) discontinued treatment due to an AE (skin disorder), and some antitumor activity has been observed at an AZD3759 dose of 200–300 mg twice daily [63]. In this study, 5 out of 18 patients (28%) had a confirmed PR or CR in the brain, and 9 (50%) had a SD (Table 1). Only 6 of 18 patients (33%) with extracranial lesions had tumor shrinkage, with no confirmed PR. Two case studies reported similar AZD3759 trough plasma and CSF concentrations 1 week after the start of treatment, indicating full penetration of the BBB [61]. BLOOM is also assessing AZD3759 in patients with treatment-naïve CNS manifestation. Twenty EGFR mutation-positive NSCLC patients, with either brain metastases (n = 16) or leptomeningeal metastasis (n = 4; three pretreated with WBRT) were treated with AZD3759 (200 or 300 mg twice daily). Fifty-five percent experienced grade ≥ 3 AEs (30% skin-related, 20% gastrointestinal), and the treatment discontinuation rate was 10%. Efficacy data were encouraging, with 15 (83%) patients with measurable brain metastases achieving an objective response (1 complete response); 3 (75%) patients with LMD also achieved an objective response, as did 13 (72%) patients with extracranial manifestations (2 complete responses) [64].
Second-Generation TKIs
The ErbB family blocker, afatinib, is the most extensively studied of the second-generation EGFR TKIs; afatinib irreversibly inhibits signaling from homo- and heterodimers of all ErbB family members (EGFR, human epidermal growth factor receptor 2 [HER2, ErbB2], ErbB3 [HER3], and ErbB4 [HER4]). Other second-generation TKIs are also in development in NSCLC [59]. Of note, results were recently reported from the phase III ARCHER 1050 study, which compared dacomitinib, an irreversible inhibitor of three ErbB family members (EGFR, HER2, and ErbB4, versus gefitinib in treatment-naïve patients with advanced NSCLC [65]. However, no data are currently available describing the effect of dacomitinib in patients with CNS metastases, as these patients were specifically excluded from the ARCHER 1050 study [65]. Another study of dacomitinib in patients with progressive brain metastases (NCT02047747) was recently terminated early [66]. Accordingly, and due to the lack of data for other second-generation EGFR TKIs, here we will focus on the preclinical and clinical evidence which demonstrates that afatinib can penetrate the BBB and is active in patients with advanced NSCLC and brain metastases and/or LMD.
Preclinical Evidence for Afatinib Activity in NSCLC Brain Metastases
Preclinical studies have shown that afatinib potently inhibits the kinase activity of EGFR, HER2, and ErbB4, with lower IC50 than those of erlotinib or gefitinib [67–70]. This potency at relatively low concentrations suggests that afatinib has the potential to provide effective treatment of CNS metastases despite incomplete penetration of the BBB [71, 72]; in addition, afatinib may also remain effective in the CSF after resistance to erlotinib or gefitinib has developed [4]. In a murine model of EGFR mutation-positive NSCLC, afatinib dose-dependently inhibited the growth of brain lesions and reduced phosphorylated EGFR (pEGFR) levels, indicating target engagement in the CNS. Moreover, there was a strong positive correlation between plasma and CSF concentrations of afatinib, demonstrating that it can effectively penetrate the BBB at sufficient concentrations to inhibit tumor growth in mice. These findings supported the evaluation of afatinib in patients with NSCLC and brain metastases [73].
Clinical Evidence for First-Line Afatinib in Patients with Advanced NSCLC with Brain Metastases and/or LMD
The approval of afatinib for the first-line treatment of EGFR mutation-positive NSCLC was based on two phase III trials comparing afatinib with platinum-based chemotherapy in this setting; LUX-Lung 3 (conducted globally), and LUX-Lung 6 (conducted in China, the Republic of Korea, and Thailand) [74–76]. More recently, the phase IIb LUX-Lung 7 study compared afatinib with gefitinib in the first-line treatment of EGFR mutation-positive NSCLC [77]. All three of these trials permitted enrollment of patients with clinically asymptomatic and controlled brain metastases, and included prespecified subgroup analyses in patients with brain metastases at enrollment [71, 77]. Baseline brain metastases were present in 12% of patients in LUX-Lung 3, 13% in LUX-Lung 6, and 16% in LUX-Lung 7.
In a combined analysis of LUX-Lung 3 and 6 (Table 2), PFS was significantly improved with afatinib versus chemotherapy in patients with brain metastases and common (Del19/L858R) EGFR mutations (median 8.2 vs. 5.4 months; hazard ratio [HR] 0.50 [95% confidence interval [CI] 0.27–0.95]; P = 0.0297) [78]. In both trials, assessed independently, there was a trend toward improved PFS with afatinib versus chemotherapy in patients with brain metastases and common EGFR mutations, and the magnitude of PFS improvement with afatinib was similar to that observed in patients without brain metastases. Furthermore, in LUX-Lung 7 (Table 2), the magnitude of PFS improvement versus gefitinib was similar in patients without, and with, brain metastases (HR 0.74 and 0.76, respectively). PFS difference for afatinib versus gefitinib was not significant for patients with brain metastases given the small sample size (n = 51) [77].
Table 2.
Summary of studies reporting the efficacy of second-generation EGFR TKIs in patients with NSCLC and CNS metastases
| EGFR TKI | Publication | Study description | Treatments | Patient characteristics | Results | |
|---|---|---|---|---|---|---|
| Name/type | Phase | |||||
| Afatinib | Schuler et al. [71] | LUX-Lung 3 | III | First-line afatinib (40 mg QD) vs. cisplatin/pemetrexed (75 mg/m2 and 500 mg/m2 once every 21 days, up to a maximum of 6 cycles) | N = 345 (n = 42 with brain metastases [afatinib, n = 27; cisplatin/pemetrexed, n = 15], of which n = 35 also harbor common EGFR mutations [afatinib, n = 20; cisplatin/pemetrexed, n = 15]); patients with EGFR mutation-positive NSCLC and brain metastases | In patients with common EGFR mutations: • Median PFS: afatinib, 11.1 months; cisplatin/pemetrexed, 5.4 months • Median OS: afatinib, 19.8 months; cisplatin/pemetrexed, 33.2 months • Rate of CNS progression: afatinib, 45.0%; cisplatin/pemetrexed, 33.3% • Time to CNS progression: afatinib, 15.2 months; cisplatin/pemetrexed, 5.7 months • ORR: afatinib, 70.0%; cisplatin/pemetrexed, 20.0% (P = 0.0058) • DCR: afatinib, 95.0%; cisplatin/pemetrexed, 80.0% |
| Schuler et al. [71] | LUX-Lung 6 | III | First-line afatinib (40 mg QD) vs. cisplatin (75 mg/m2 every 21 days, up to 6 cycles) and gemcitabine (1000 mg/m2 on day 1 and day 8) | N = 364 (n = 49 with brain metastases [afatinib, n = 30; cisplatin/gemcitabine, n = 19], of which n = 46 harbor common EGFR mutations [afatinib, n = 28; cisplatin/gemcitabine, n = 18]); patients with EGFR mutation-positive NSCLC and brain metastases | In patients with common EGFR mutations: • Median PFS: afatinib, 8.2 months; cisplatin/gemcitabine, 4.7 months • Median OS: afatinib, 22.4 months; cisplatin/gemcitabine, 24.7 months • Rate of CNS progression: afatinib, 21.4%; cisplatin/gemcitabine, 27.8% • Time to CNS progression: afatinib, 15.2 months; cisplatin/gemcitabine, 7.3 months • ORR: afatinib, 75.0%; cisplatin/gemcitabine, 27.8% (P = 0.0027) • DCR: afatinib, 89.3%; cisplatin/gemcitabine, 72.2% |
|
| Schuler et al. [71] | Combined analysis of LUX-Lung 3 and LUX-Lung 6 | III | LUX-Lung 3: First-line afatinib (40 mg QD) vs. cisplatin/pemetrexed (75 mg/m2 and 500 mg/m2 once every 21 days, up to a maximum of 6 cycles) LUX-Lung 6: First-line afatinib (40 mg QD) vs. cisplatin (75 mg/m2 every 21 days, up to 6 cycles) and gemcitabine (1000 mg/m2 on day 1 and day 8) |
N = 91 (n = 81 harbor common EGFR mutations); patients with EGFR mutation-positive NSCLC and brain metastases | In patients with common EGFR mutations: • Median PFS: afatinib, 8.2 months; chemotherapy, 5.4 months (P = 0.0297) • Median PFS was higher with afatinib vs. chemotherapy in patients with Del19 mutation (9.5 vs. 4.7 months, respectively; P = 0.0012); there were no significant differences between treatments in patients with L858R (afatinib, 6.9 months; chemotherapy, 9.7 months) • PFS benefit was higher with afatinib compared to chemotherapy in patients who received prior WBRT (13.8 vs. 4.7 months) than in those who did not (6.9 vs. 5.4 months) • Median OS: afatinib, 22.4 months; chemotherapy, 25.0 months; no significant differences were seen between treatments among patients harboring Del19 or L8585R mutations |
|
| Park et al. [77] | LUX-Lung 7 | IIb | First-line afatinib (40 mg QD) vs. gefitinib (250 mg QD) | N = 319 (n = 50 with brain metastases: afatinib, n = 26; gefitinib, n = 24); patients with common EGFR mutation-positive NSCLC and brain metastases | • Median PFS: afatinib, 7.2 months; gefitinib, 7.4 months • Median TTF: afatinib, 8.4 months; gefitinib, 9.3 months |
|
| Hoffknecht et al. [4] | CUP and case report | Afatinib (50 mg/day); all patients pretreated with chemotherapy and erlotinib/gefitinib Case report: fourth-line afatinib (50 mg/day) |
N = 100 patients with brain metastases or LMD; 74% had EGFR mutations (77% of which were Del19 or L858R) Case report: Female patient; age: 59 years; ECOG PS: 3/4; L858R-positive NSCLC with LMD |
• ORR: PR, 42%; SD, 39% • TTF: overall, 3.6 months; EGFR-mutation-positive vs. WT, 4.0 vs. 1.3 months • Median OS: 9.8 months Case report: • Neurological symptoms diminished • ECOG PS improved to 1/2 |
||
| Tamiya et al. [80] | Multicenter trial | Third-line or later afatinib (40 mg/day) | N = 11; patients with EGFR-mutations and LMD | • ORR 27.3% • Median PFS 2.0 months • Median OS 3.8 months • Survival outcomes superior in patients with G719X mutation-positive tumors (median PFS 5.6 months; median OS 7.0 months) |
||
| Saijo et al. [89] | Case series | Third-line afatinib (40 mg/day) or afatinib (40 mg/day) following RT | N = 3; Japanese female patients with EGFR common mutations and LMD | Third-line afatinib, n = 2 patients with Del19: • Reduction in LMD-associated symptoms after 2 weeks • Improvement in ECOG PS to 1; disappearance of evidence of LMD/brain metastases Afatinib after RT, n = 1 patient with L858R: • No improvement in ECOG PS, but levels of consciousness improved • LMD under control after 11 months |
||
| Kuiper et al. [14] | Retrospective cohort analysis | Afatinib with/without cetuximab | N = 3; male patients with Del19 mutation and LMD | • Survival following LMD diagnosis was variable: 4.6, 8.7, and 0.2 months in the 3 patients | ||
| Lin et al. [87] | Case report | Afatinib (40 mg/day) plus cetuximab (250 mg/m2 biweekly) | Female patient with Del19 and LMD | • Regression of brain lesions on MRI and reduction of LMD-associated symptoms after 1 month • PD of the lung after 4 months, but no suggestion of relapse of LMD |
||
| Kawaguchi et al. [86] | Case report | Eight-line afatinib (40 mg/day) | Female patient with L858R and LMD | • Regression of neurological symptoms after 1 week of afatinib treatment • Symptom free after 1 month with ECOG PS improved to 1 • Progression free at 7 months |
||
| Ghosn et al. [85] | Case report | Third-line afatinib (50 mg/day) | Male patient with Del19 and LMD | • Disappearance of meningeal enhancement on brain MRI 10 months after the start of afatinib therapy • Patient alive with no evidence of neurological relapse at 35 months |
||
| Afatinib + RT | Baird et al. [81] | Cambridge Brain Mets Trial 1 (CamBMT1); Phase 2 of study is currently ongoing (NCT02768337) | Ib | Afatinib (20 mg QD, escalated to 30 mg and 40 mg) + 2 Gy or 4 Gy targeted RT | N = 10; patients with NSCLC (n = 6) or breast tumors (n = 4) with operable brain metastases | • Phase I (dose defining) of study completed: afatinib 40 mg QD will be used in phase II which compares efficacy • Afatinib dose in resected brain metastases was not correlated with RT dose • No dose-limiting toxicities were identified |
| Li et al. [84] | Retrospective analysis | Afatinib (30 or 40 mg/day initial or maintenance dose) + WBRT (mean dose of 2805.9 ± 405.4 cGy) | N = 28; EGFR mutation-positive, treatment-naive NSCLC patients receiving afatinib monotherapy (n = 11) or afatinib with WBRT (n = 17) | • ORR: afatinib monotherapy, 81.8%; afatinib + WBRT, 88.2% • Intracranial CR: afatinib monotherapy, 63.6%; afatinib + WBRT, 17.6% (p = 0.02) • No significant differences in OS between treatments |
||
| Dacomitinib | NCT02047747 [66] | II | Dacomitinib (45 mg/day) | Patients with lung cancer, melanoma, HER2-amplified breast cancer, or HER2-amplified gastric cancer with brain metastases or LMD | Study terminated after 4 patients | |
CNS central nervous system, DCR disease control rate, ECOG PS Eastern Cooperative Oncology Group performance status, EGFR epidermal growth factor receptor, HER2 human epidermal growth factor receptor 2, LMD leptomeningeal disease, MRI magnetic resonance imaging, NSCLC non-small cell lung cancer, ORR overall response rate, OS overall survival, PD progressive disease, PFS progression-free survival, PR partial response, QD once daily, RT radiation therapy, SD stable disease, TKI tyrosine kinase inhibitor, TTF time to failure, WBRT whole-brain radiation therapy, WT wild-type
In both LUX-Lung 3 and 6, overall response rate (ORR) was significantly improved with afatinib versus chemotherapy in patients with brain metastases and common EGFR mutations (LUX-Lung 3 70% vs. 20%, P = 0.0058; LUX-Lung 6 75% vs. 28%, P = 0.0027), and these response rates were similar to those in patients without baseline brain metastases [71]. No statistically significant OS benefit was observed in patients with brain metastases treated with afatinib versus chemotherapy either in the individual LUX-Lung 3 or 6 trials, or in a combined analysis. It should be noted, however, that afatinib was associated with quality of life benefits versus chemotherapy in both trials [74, 75]. Evidence of the activity of afatinib against brain metastases is further confirmed by a recent competing risk analyses of the LUX-Lung 3 and 6 studies. In patients with a target brain lesion at the start of afatinib treatment, the risk of CNS progression (34%) was lower than the risk of non-CNS progression (48%). De novo CNS progression was observed in only 5% of patients after 24 months. In patients without brain metastases at baseline, the non-CNS progression rate after 24 months was 71% [79]. These data demonstrate that afatinib may delay the development of metastatic disease in the brain. In addition, the brain was not the site of first disease progression in the majority of patients with baseline brain metastases who experienced progressive disease (PD) on afatinib, indicating control of existing brain metastases by afatinib. In both LUX-Lung 3 and 6, the safety profile of afatinib in patients with brain metastases was similar to that in those without brain metastases, with no unexpected AEs reported in both treatment groups [71].
CSF concentrations of afatinib were not assessed in LUX-Lung 3 or 6, but a recent prospective multicenter study evaluated the rate of penetration of afatinib into the CSF, in patients with EGFR mutation-positive NSCLC with LMC [80]. Eleven patients with confirmed LMC, mostly heavily pretreated and with 8 patients having common [Del19/L858R] EGFR mutations, were treated with afatinib 40 mg/day; blood and CSF levels of afatinib were assessed on day 8. The level of afatinib in the CSF (median) was 2.9 nM, which is greater than the IC50 of afatinib for EGFR [80]. In contrast with the LUX-Lung 3, 6, and 7 studies, which permitted the inclusion of patients with asymptomatic brain metastases only, a case series has also been reported describing five patients from one center who had NSCLC with multiple symptomatic brain metastases [78]. These patients declined WBRT and were treated with afatinib only as first-line treatment. In all five patients, afatinib treatment induced complete remission of brain metastases, which lasted for at least 6 months according to magnetic resonance imaging (MRI) analysis, thus representing a clear clinical benefit.
Afatinib in Combination with RT
Several studies have assessed the feasibility of combining afatinib with RT. The ongoing CamBMT1 phase Ib study is investigating afatinib penetration into cerebral metastases for patients undergoing neurosurgical resection, directly following low-dose targeted RT. Patients with operable brain metastases from breast or lung origin were treated with afatinib for 11 days prior to surgery on day 12. Patients also received a single fraction of targeted RT on day 10 (2 Gy or 4 Gy). Preliminary results from 10 treated patients showed no dose-limiting toxicities and identified a recommended phase II dose for afatinib of 40 mg/day for monotherapy in both the 2-Gy and 4-Gy arms. Importantly, afatinib concentrations in resected brain metastases were, on average, more than 15-fold higher than those in plasma, independent of the applied dose of radiation [81]. Two recent case reports also indicate that combination of 40 mg afatinib with WBRT (30–35 Gy) is feasible, with no signs of acute or late toxicities [82, 83]. A recent retrospective analysis of 28 treatment-naïve NSCLC patients with brain metastases compared the efficacy of afatinib monotherapy with that of afatinib plus WBRT (afatinib, n = 11; afatinib + WBRT, n = 17). The ORR was 81.8% and 88.2%, respectively. However, the afatinib monotherapy group had a significantly higher complete response rate for intracranial lesions compared with the combination with WBRT (63.6% vs. 17.6%, respectively; P = 0.02), and there were no significant differences between the two treatment groups in OS or time to treatment failure with median time to treatment failure of 14.5 months for afatinib plus WBRT and 18.5 months for patients treated with afatinib monotherapy. These data support the therapeutic benefit of afatinib in treatment-naïve, EGFR mutation-positive NSCLC patients with brain metastases, regardless of concomitant radiotherapy [84].
Clinical Evidence for Afatinib in EGFR TKI-Pretreated Patients with Advanced NSCLC
In an afatinib CUP, patients, some of whom had EGFR mutations, were treated with afatinib following progression after at least one line of chemotherapy and one line of EGFR TKI therapy [4]. Among 31 evaluable patients with CNS metastases (brain metastases or LMD), the overall rate of cerebral response to afatinib was 35%, and the median duration of response was 120 days (range, 21–395). The CNS disease control rate (DCR) was 66%.
Clinical Evidence for Afatinib in Patients with Advanced NSCLC and LMD
Data on afatinib use in patients with LMD are limited, but one prospective trial and several case reports have presented results in pretreated patients (Table 2). In total, data from 21 patients with LMD who received afatinib treatment (including two patients treated with afatinib in combination with cetuximab) have been reported [4, 14, 85–89]. The median age of these 21 patients was 61 years (range, mid 20s–79), 14 were female, and the majority had an Eastern Cooperative Oncology Group performance status (ECOG PS) of 3 or 4 at the start of afatinib treatment. Nineteen patients were pretreated, and 18 had received previous treatment with an EGFR TKI. The most common EGFR mutation was Del19 (12 cases), while 6 cases were reported with L858R mutations, and 3 cases with G719X. Across these studies, afatinib treatment resulted in regression of neurological symptoms, often accompanied by a dramatic improvement in ECOG PS. Cerebral remissions were also reported and, in some cases, were long-lasting. The median PFS was approximately 4.6 months, ranging from 0.6 months to 35 months with treatment still ongoing. Of note, most of these studies assessed afatinib levels in the CSF, and showed overall CSF levels ranging from 0.14–2.85 ng/mL, which corresponds to 0.1–9.3 nM. To put this into context, the EC50 of afatinib for EGFR is 0.5 nM, and the IC50 is 1 nM [68, 69], indicating that afatinib reached sufficient CSF concentrations in these studies to achieve effective inhibition of EGFR in the CNS.
Third-Generation EGFR TKIs
Several third-generation EGFR TKIs have been developed. Osimertinib was originally developed to target the gatekeeper EGFR T790 M mutation, the predominant mechanism of acquired resistance to first- and second-generation EGFR TKIs (50–70%) of cases [90, 91]. It has demonstrated striking clinical activity in patients with T790M-positive tumors following failure of erlotinib, gefitinib, or afatinib [92, 93]. Osimertinib is also active against activating EGFR mutations (Del19, L858R) but is wild-type sparing and has demonstrated superior PFS versus first-generation EGFR TKIs in a first-line setting, with a favorable tolerability profile [94]. Preclinical and clinical experience with osimertinib against CNS lesions is summarized below.
Preclinical Evidence for Osimertinib Activity in NSCLC Brain Metastases
Preclinical data indicate that osimertinib penetrates the BBB and has antitumor activity [95]. Studies in cynomolgus monkeys using radiolabeled osimertinib and gefitinib also showed much higher brain exposure to osimertinib versus gefitinib. Investigations in a mouse model of EGFR mutation-positive brain metastases showed that osimertinib induced dose-dependent tumor regression [95]. These data suggest the potential for clinical application of osimertinib.
Clinical Evidence for Osimertinib in Patients with Advanced NSCLC with Brain Metastases
The efficacy of osimertinib in EGFR TKI-pretreated patients with brain metastases was reported in some early clinical cases. In the phase I/II study AURA trial, two case studies were described of patients with EGFR mutation-positive NSCLC and baseline brain metastases [95]. PR was achieved in both these cases, indicating the ability of osimertinib to control the growth of intracranial tumors in humans. In the phase I BLOOM study described earlier, osimertinib demonstrated encouraging activity in these patients, with an overall leptomeningeal metastasis (LM) response of 43%, as well as improvement of neurological symptoms. However, it should be noted that the osimertinib dose used in this study (160 mg/day) was double the approved dose. Nevertheless, the increased dose appeared to be well tolerated; only two patients had grade ≥ 3 AEs; one case of grade 3 diarrhea and one case of grade 3 nausea.
Two phase II trials, the AURA extension and AURA2 studies, aimed to evaluate the efficacy and safety of osimertinib (80 mg/day) in patients with T790M mutation-positive NSCLC, with PD following prior EGFR TKI therapy. Pooled data from these two trials were used in a pre-planned subgroup analysis of CNS response [96]. Of 192 patients with baseline brain scans, 50 were evaluable for CNS response. Baseline demographics were generally consistent with the overall populations; 66% had Del19 mutations, 76% had WHO PS 2, and 74% had received prior brain irradiation. The confirmed CNS ORR was 54% (95% CI 39–68%), and 12% of patients had a complete CNS response. Eighty-two percent of patients responded by the time of the first assessment (within 6 weeks), and CNS responses were observed regardless of prior brain radiation. The CNS DCR was 92%, and the median maximum percentage change from baseline in CNS target lesion size was −53% (range, −100% to +80%). The 6- and 12-month PFS rates were 72% and 56%, respectively.
These findings have been substantiated by recent results from the phase III studies, AURA3 and FLAURA (Table 3). In the AURA3 study, the efficacy of osimertinib (80 mg/day) was compared with chemotherapy in patients with T790 M-positive NSCLC with disease progression following first-line EGFR TKI therapy [92]. In patients who were evaluable for CNS response (n = 46), CNS ORR was 70% with osimertinib and 31% with chemotherapy (OR, 5.1; 95% CI 1.4–20.6) [97]. Median CNS duration of response was 8.9 and 5.7 months, respectively, and CNS PFS was significantly improved with osimertinib versus chemotherapy (median 11.7 vs. 5.6 months; HR 0.32 [95% CI 0.15–0.69]) [97].
Table 3.
Summary of studies reporting the efficacy of the third-generation EGFR TKI osimertinib in patients with NSCLC and CNS metastases
| EGFR TKI | Publication | Study description | Treatments | Patient characteristics | Results | |
|---|---|---|---|---|---|---|
| Name/type | Phase | |||||
| Osimertinib | Yang et al. [62] | BLOOM | I | Osimertinib (160 mg/day) | N = 32; patients with EGFR mutations and LMD (n = 11 with T790M mutation) | • 23 patients reached radiological assessment: 10 had improvements, 13 had SD • Same 23 patients reached 12-week neurological assessment: 8 symptomatic patients, 7 improved and 1 had SD; of 15 asymptomatic patients, 2 worsened and 13 remained asymptomatic |
| Goss et al. [96] | Pooled analysis of AURA and AURA2 | II | Osimertinib (80 mg/day) following prior EGFR TKI therapy | N = 50; patients with T790M mutation and brain metastases | • CNS ORR: 54%; CNS CR: 12% • CNS responses observed in 82% of patients within 6 weeks, regardless of prior RT • Median CNS PFS not reached |
|
| Mok et al. [92] | AURA3 | III | Osimertinib (80 mg/day) following prior first-line EGFR TKI therapy vs. chemotherapy (IV pemetrexed 500 mg/m2 plus either carboplatin or cisplatin) | N = 419 (osimertinib, n = 279; platinum-pemetrexed, n = 140); patients with T790M mutation and CNS metastases (osimertinib in patients with CNS metastases, n = 93; platinum-pemetrexed, n = 51) | • Median PFS: osimertinib, 8.5; chemotherapy, 4.2 months • ORR: osimertinib, 71%; chemotherapy, 31% |
|
| Soria et al. [94] | FLAURA | III | First-line osimertinib (80 mg QD) vs. standard of care (erlotinib [150 mg QD] or gefitinib [250 mg QD]) | N = 116 (osimertinib, n = 53; erlotinib/gefitinib, n = 63); patients with Del19 or L858R EGFR mutations and brain metastases | • Median PFS, osimertinib, 15.2 months; erlotinib/gefitinib, 9.6 months • CNS progression: osimertinib, 6%; erlotinib/gefitinib, 15% (all patients, N = 556) |
|
BID twice daily, BM brain metastases, CNS central nervous system, CR complete response, CSF cerebrospinal fluid, EGFR epidermal growth factor receptor, IV intravenous, LM leptomeningeal metastases, LMD leptomeningeal disease, MRI magnetic resonance imaging, NSCLC non-small cell lung cancer, ORR overall response rate, OR overall response, PFS progression-free survival, PR partial response, QD once daily, RT radiation therapy, SD stable disease, TKI tyrosine kinase inhibitor
The FLAURA trial examined the benefit of osimertinib in the first-line setting, in patients with NSCLC harboring common EGFR mutations, including patients with brain metastases [94]. Improved PFS, response rate, and duration of response were reported with osimertinib compared with the first-generation EGFR TKIs, erlotinib and gefitinib. A subset of 116 patients with brain metastases were included (osimertinib, n = 53; erlotinib/gefitinib, n = 63), 25% of whom were pre-treated with RT. The improvement in PFS with osimertinib versus erlotinib/gefitinib was the same in patients with brain metastases (HR = 0.47) as those without (HR = 0.46). In the overall population, CNS progression was markedly less frequent with osimertinib (6%) than with erlotinib or gefitinib (15%) [94]. Based on competing risk analysis, the probability of experiencing a CNS progression event (in the absence of non-CNS progression or death) was 5% vs. 18% at 6 months, and 8% vs. 24% at 12 months [98]. The CNS ORR was 66% vs. 43%; duration of response was 15.2 vs. 18.7 months with osimertinib and erlotinib/gefitinib, respectively [98].
Conclusions/Key Points
The high rate of CNS progression in patients with EGFR mutation-positive NSCLC means that there is a need to identify and characterize treatment strategies which are active against existing brain lesions and also reduce the risk of metastatic spread to the CNS. While EGFR TKIs have been studied extensively in patients with advanced NSCLC, relatively few studies included patients with brain metastases and/or LMD. A number of studies described herein indicate that first-generation EGFR TKIs may have some activity in patients with EGFR mutation-positive NSCLC and CNS metastases. However, emerging evidence suggests that second- and third-generation TKIs may be better treatment options. The ability of different TKIs to target existing brain metastases and to mitigate the risk of CNS progression are important considerations when contemplating treatment decisions, especially with regard to how best to utilize different EGFR TKIs in sequence. Higher BBB penetrance with afatinib and osimertinib, compared with the first-generation agents erlotinib and gefitinib, may lead to greater CNS efficacy; this is supported by evidence from the LUX-Lung 3, 6, and 7, and FLAURA studies [77, 94]. These studies provide supportive evidence for osimertinib and afatinib as first-line treatments of choice (in preference to first-generation TKIs) in patients with CNS involvement; both drugs have clinical CNS benefit, and appear to delay the onset of metastatic disease in the brain. In the absence of studies directly comparing second- and third-generation EGFR TKIs in this setting, there is no clear first-choice EGFR TKI, and treatment decisions must be based on indirect comparisons of safety and efficacy data from across the published studies; other factors likely to influence treatment decisions may include clinical experience, patient preference, cost, and reimbursement. Another consideration is the likely availability of targeted treatment options for second-line and later lines of therapy. More information is required on the development of acquired resistance mechanisms, both generally and in CNS lesions. Currently, resistance mechanisms to osimertinib are not well defined and appear heterogeneous [99–102]. In contrast, the main mechanism of acquired resistance to afatinib in primary tumors is the emergence of T790M mutations (50–70% of cases). If the emergence of T790M is identified as the predominant mechanism of afatinib resistance for CNS lesions, then most patients with brain metastases could benefit from sequential therapy with afatinib followed by osimertinib. On the other hand, given that some patients will progress on afatinib via T790M-independent mechanisms and that other patients will not survive beyond first-line therapy, reserving osimertinib for second-line use will preclude its use in some patients. Prospective comparison of sequential EGFR-TKI regimens is required to define the optimal treatment strategy in patients with EGFR mutation-positive NSCLC, including those with CNS lesions.
In summary, while erlotinib and gefitinib have shown some efficacy in patients with EGFR mutation-positive NSCLC and CNS metastases, and other EGFR TKIs such as AZD3759 may prove promising as future therapeutic options in this setting, at present, the strongest data support afatinib and osimertinib treatment in this patient population. Additional large-scale studies conducted specifically in patients with EGFR mutation-positive NSCLC and CNS metastases should shed more light on the differences between EGFR TKIs, and may reveal the treatment strategies that yield the greatest benefits and improvements in OS for most patients.
Compliance with Ethical Standards
Funding
Open Access publication of this article was funded by Boehringer Ingelheim. This work was supported by Boehringer Ingelheim. Medical writing assistance, supported financially by Boehringer Ingelheim, was provided by Helen Kitchen and Hashem Dbouk of GeoMed, an Ashfield company, part of UDG Healthcare plc, during the preparation of this article. Boehringer Ingelheim was involved in the preparation of the manuscript.
Conflict of Interest
MJH has received speaker fees from MSD, BMS, AstraZeneca, Roche, Lilly, and Boehringer Ingelheim.
References
- 1.Langer CJ, Mehta MP. Current management of brain metastases, with a focus on systemic options. J Clin Oncol. 2005;23(25):6207–19. [DOI] [PubMed]
- 2.Eichler AF, Loeffler JS. Multidisciplinary management of brain metastases. Oncologist. 2007;12(7):884–98. [DOI] [PubMed]
- 3.Fan Y, Huang Z, Fang L, Miu L, Lin N, Gong L, et al. Chemotherapy and EGFR tyrosine kinase inhibitors for treatment of brain metastases from non-small-cell lung cancer: survival analysis in 210 patients. Onco Targets Ther. 2013;6:1789–1803. doi: 10.2147/OTT.S52172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoffknecht P, Tufman A, Wehler T, Pelzer T, Wiewrodt R, Schutz M, et al. Efficacy of the irreversible ErbB family blocker afatinib in epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI)-pretreated non-small-cell lung cancer patients with brain metastases or leptomeningeal disease. J Thorac Oncol. 2015;10(1):156–63. [DOI] [PMC free article] [PubMed]
- 5.Khuntia D, Brown P, Li J, Mehta MP. Whole-brain radiotherapy in the management of brain metastasis. J Clin Oncol. 2006;24(8):1295–304. [DOI] [PubMed]
- 6.Ruderman N, Hall R. Use of glucocorticoids in the palliative treatment of metastatic brain tumors. Cancer. 1965;18:298–306. [DOI] [PubMed]
- 7.Zimm S, Wampler GL, Stablein D, Hazra T, Young HF. Intracerebral metastases in solid-tumor patients: natural history and results of treatment. Cancer. 1981;48(2):384–94. [DOI] [PubMed]
- 8.Mulvenna P, Nankivell M, Barton R, Faivre-Finn C, Wilson P, McColl E, et al. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiority, randomised trial. Lancet. 2016;388(10055):2004–2014. doi: 10.1016/S0140-6736(16)30825-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet. 2004;363(9422):1665–1672. doi: 10.1016/S0140-6736(04)16250-8. [DOI] [PubMed] [Google Scholar]
- 10.Kocher M, Soffietti R, Abacioglu U, Villa S, Fauchon F, Baumert BG, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol. 2011;29(2):134–141. doi: 10.1200/JCO.2010.30.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990;322(8):494–500. doi: 10.1056/NEJM199002223220802. [DOI] [PubMed] [Google Scholar]
- 12.Tsao MN, Rades D, Wirth A, Lo SS, Danielson BL, Gaspar LE, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): an American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol. 2012;2(3):210–225. doi: 10.1016/j.prro.2011.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gleissner B, Chamberlain MC. Neoplastic meningitis. Lancet Neurol. 2006;5(5):443–452. doi: 10.1016/S1474-4422(06)70443-4. [DOI] [PubMed] [Google Scholar]
- 14.Kuiper JL, Hendriks LE, van der Wekken AJ, de Langen AJ, Bahce I, Thunnissen E, et al. Treatment and survival of patients with EGFR-mutated non-small cell lung cancer and leptomeningeal metastasis: a retrospective cohort analysis. Lung Cancer. 2015;89(3):255–261. doi: 10.1016/j.lungcan.2015.05.023. [DOI] [PubMed] [Google Scholar]
- 15.Nagpal S, Riess J, Wakelee H. Treatment of leptomeningeal spread of NSCLC: a continuing challenge. Curr Treat Options in Oncol. 2012;13(4):491–504. doi: 10.1007/s11864-012-0206-4. [DOI] [PubMed] [Google Scholar]
- 16.Clarke JL, Perez HR, Jacks LM, Panageas KS, Deangelis LM. Leptomeningeal metastases in the MRI era. Neurology. 2010;74(18):1449–1454. doi: 10.1212/WNL.0b013e3181dc1a69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gwak HS, Joo J, Kim S, Yoo H, Shin SH, Han JY, et al. Analysis of treatment outcomes of intraventricular chemotherapy in 105 patients for leptomeningeal carcinomatosis from non-small-cell lung cancer. J Thorac Oncol. 2013;8(5):599–605. doi: 10.1097/JTO.0b013e318287c943. [DOI] [PubMed] [Google Scholar]
- 18.Morris PG, Reiner AS, Szenberg OR, Clarke JL, Panageas KS, Perez HR, et al. Leptomeningeal metastasis from non-small cell lung cancer: survival and the impact of whole brain radiotherapy. J Thorac Oncol. 2012;7(2):382–385. doi: 10.1097/JTO.0b013e3182398e4f. [DOI] [PubMed] [Google Scholar]
- 19.O’Meara WP, Borkar SA, Stambuk HE, Lymberis SC. Leptomeningeal metastasis. Curr Probl Cancer. 2007;31(6):367–424. doi: 10.1016/S0147-0272(07)00067-0. [DOI] [PubMed] [Google Scholar]
- 20.Moscetti L, Nelli F, Felici A, Rinaldi M, De Santis S, D’Auria G, et al. Up-front chemotherapy and radiation treatment in newly diagnosed nonsmall cell lung cancer with brain metastases: survey by outcome research network for evaluation of treatment results in oncology. Cancer. 2007;109(2):274–281. doi: 10.1002/cncr.22399. [DOI] [PubMed] [Google Scholar]
- 21.Postmus PE, Smit EF. Chemotherapy for brain metastases of lung cancer: a review. Ann Oncol. 1999;10(7):753–759. doi: 10.1023/A:1008318515795. [DOI] [PubMed] [Google Scholar]
- 22.Fidler IJ, Yano S, Zhang RD, Fujimaki T, Bucana CD. The seed and soil hypothesis: vascularisation and brain metastases. Lancet Oncol. 2002;3(1):53–57. doi: 10.1016/S1470-2045(01)00622-2. [DOI] [PubMed] [Google Scholar]
- 23.Holash J, Maisonpierre PC, Compton D, Boland P, Alexander CR, Zagzag D, et al. Vessel cooption, regression, and growth in tumors mediated by angiopoietins and VEGF. Science. 1999;284(5422):1994–1998. doi: 10.1126/science.284.5422.1994. [DOI] [PubMed] [Google Scholar]
- 24.Bhatt VR, Kedia S, Kessinger A, Ganti AK. Brain metastasis in patients with non-small-cell lung cancer and epidermal growth factor receptor mutations. J Clin Oncol. 2013;31(25):3162–4. [DOI] [PubMed]
- 25.Eichler AF, Kahle KT, Wang DL, Joshi VA, Willers H, Engelman JA, et al. EGFR mutation status and survival after diagnosis of brain metastasis in nonsmall cell lung cancer. Neuro Oncol. 2010;12(11):1193–9. [DOI] [PMC free article] [PubMed]
- 26.Han G, Bi J, Tan W, Wei X, Wang X, Ying X, et al. A retrospective analysis in patients with EGFR-mutant lung adenocarcinoma: is EGFR mutation associated with a higher incidence of brain metastasis? Oncotarget. 2016;7(35):56998–57010. doi: 10.18632/oncotarget.10933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hendriks LE, Smit EF, Vosse BA, Mellema WW, Heideman DA, Bootsma GP, et al. EGFR mutated non-small cell lung cancer patients: more prone to development of bone and brain metastases? Lung Cancer. 2014;84(1):86–91. [DOI] [PubMed]
- 28.Iuchi T, Shingyoji M, Itakura M, Yokoi S, Moriya Y, Tamura H, et al. Frequency of brain metastases in non-small-cell lung cancer, and their association with epidermal growth factor receptor mutations. Int J Clin Oncol. 2015;20(4):674–679. doi: 10.1007/s10147-014-0760-9. [DOI] [PubMed] [Google Scholar]
- 29.Shin DY, Na II, Kim CH, Park S, Baek H, Yang SH. EGFR mutation and brain metastasis in pulmonary adenocarcinomas. J Thorac Oncol. 2014;9(2):195–199. doi: 10.1097/JTO.0000000000000069. [DOI] [PubMed] [Google Scholar]
- 30.Stanic K, Zwitter M, Hitij NT, Kern I, Sadikov A, Cufer T. Brain metastases in lung adenocarcinoma: impact of EGFR mutation status on incidence and survival. Radiol Oncol. 2014;48(2):173–183. doi: 10.2478/raon-2014-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clarke JL, Pao W, Wu N, Miller VA, Lassman AB. High dose weekly erlotinib achieves therapeutic concentrations in CSF and is effective in leptomeningeal metastases from epidermal growth factor receptor mutant lung cancer. J Neuro-Oncol. 2010;99(2):283–286. doi: 10.1007/s11060-010-0128-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Deng Y, Feng W, Wu J, Chen Z, Tang Y, Zhang H, et al. The concentration of erlotinib in the cerebrospinal fluid of patients with brain metastasis from non-small-cell lung cancer. Mol Clin Oncol. 2014;2(1):116–120. doi: 10.3892/mco.2013.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hata A, Kaji R, Fujita S, Katakami N. High-dose erlotinib for refractory brain metastases in a patient with relapsed non-small cell lung cancer. J Thorac Oncol. 2011;6(3):653–654. doi: 10.1097/JTO.0b013e3181d899bb. [DOI] [PubMed] [Google Scholar]
- 34.Lee E, Keam B, Kim DW, Kim TM, Lee SH, Chung DH, et al. Erlotinib versus gefitinib for control of leptomeningeal carcinomatosis in non-small-cell lung cancer. J Thorac Oncol. 2013;8(8):1069–1074. doi: 10.1097/JTO.0b013e318294c8e8. [DOI] [PubMed] [Google Scholar]
- 35.Togashi Y, Masago K, Masuda S, Mizuno T, Fukudo M, Ikemi Y, et al. Cerebrospinal fluid concentration of gefitinib and erlotinib in patients with non-small cell lung cancer. Cancer Chemother Pharmacol. 2012;70(3):399–405. doi: 10.1007/s00280-012-1929-4. [DOI] [PubMed] [Google Scholar]
- 36.Park SJ, Kim HT, Lee DH, Kim KP, Kim SW, Suh C, et al. Efficacy of epidermal growth factor receptor tyrosine kinase inhibitors for brain metastasis in non-small cell lung cancer patients harboring either exon 19 or 21 mutation. Lung Cancer. 2012;77(3):556–60. [DOI] [PubMed]
- 37.Kim JE, Lee DH, Choi Y, Yoon DH, Kim SW, Suh C, et al. Epidermal growth factor receptor tyrosine kinase inhibitors as a first-line therapy for never-smokers with adenocarcinoma of the lung having asymptomatic synchronous brain metastasis. Lung Cancer. 2009;65(3):351–4. [DOI] [PubMed]
- 38.Zhang JX, Cai D, Li SY, Zhou CZ, Qin YY, Ouyang M. Clinical comparison of erlotinib and gefitinib in non-small cell lung cancer with brain metastases. Chin J Cancer Prevent Treat. 2015;22:285–8.
- 39.Iuchi T, Shingyoji M, Sakaida T, Hatano K, Nagano O, Itakura M, et al. Phase II trial of gefitinib alone without radiation therapy for Japanese patients with brain metastases from EGFR-mutant lung adenocarcinoma. Lung Cancer. 2013;82(2):282–7. [DOI] [PubMed]
- 40.Riely GJ, Pao W, Pham D, Li AR, Rizvi N, Venkatraman ES, et al. Clinical course of patients with non-small cell lung cancer and epidermal growth factor receptor exon 19 and exon 21 mutations treated with gefitinib or erlotinib. Clin Cancer Res. 2006;12(3 Pt 1):839–44. [DOI] [PubMed]
- 41.Jackman DM, Yeap BY, Sequist LV, Lindeman N, Holmes AJ, Joshi VA, et al. Exon 19 deletion mutations of epidermal growth factor receptor are associated with prolonged survival in non-small cell lung cancer patients treated with gefitinib or erlotinib. Clin Cancer Res. 2006;12(13):3908–3914. doi: 10.1158/1078-0432.CCR-06-0462. [DOI] [PubMed] [Google Scholar]
- 42.Arbour KC, Kris MG, Riely GJ, Ni A, Beal K, Daras M, et al. Twice weekly pulse and daily continuous-dose erlotinib as initial treatment for patients with epidermal growth factor receptor-mutant lung cancers and brain metastases. Cancer. 2018;124(1):105–109. doi: 10.1002/cncr.30990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yu HA, Sima C, Feldman D, Liu LL, Vaitheesvaran B, Cross J, et al. Phase 1 study of twice weekly pulse dose and daily low-dose erlotinib as initial treatment for patients with EGFR-mutant lung cancers. Ann Oncol. 2017;28(2):278–284. doi: 10.1093/annonc/mdw556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.d’Avella D, Cicciarello R, Angileri FF, Lucerna S, La Torre D, Tomasello F. Radiation-induced blood-brain barrier changes: pathophysiological mechanisms and clinical implications. Acta Neurochir Suppl. 1998;71:282–284. doi: 10.1007/978-3-7091-6475-4_82. [DOI] [PubMed] [Google Scholar]
- 45.van Vulpen M, Kal HB, Taphoorn MJ, El-Sharouni SY. Changes in blood-brain barrier permeability induced by radiotherapy: implications for timing of chemotherapy? (Review). Oncol Rep. 2002;9(4):683–8. [PubMed]
- 46.Ahsan A. Mechanisms of resistance to EGFR tyrosine kinase inhibitors and therapeutic approaches: an update. Adv Exp Med Biol. 2016;893:137–153. doi: 10.1007/978-3-319-24223-1_7. [DOI] [PubMed] [Google Scholar]
- 47.Li J, Wu X, Wang Z, Shen Z, Sun N, Zhu X. Ionizing radiation reduces TKI resistance caused by T790M mutation in NSCLC cell lines. Zhongguo Fei Ai Za Zhi. 2015;18(8):475–480. doi: 10.3779/j.issn.1009-3419.2015.08.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akimoto T, Hunter NR, Buchmiller L, Mason K, Ang KK, Milas L. Inverse relationship between epidermal growth factor receptor expression and radiocurability of murine carcinomas. Clin Cancer Res. 1999;5(10):2884–2890. [PubMed] [Google Scholar]
- 49.Chinnaiyan P, Huang S, Vallabhaneni G, Armstrong E, Varambally S, Tomlins SA, et al. Mechanisms of enhanced radiation response following epidermal growth factor receptor signaling inhibition by erlotinib (Tarceva) Cancer Res. 2005;65(8):3328–3335. doi: 10.1158/0008-5472.CAN-04-3547. [DOI] [PubMed] [Google Scholar]
- 50.Ceresoli GL, Cappuzzo F, Gregorc V, Bartolini S, Crino L, Villa E. Gefitinib in patients with brain metastases from non-small-cell lung cancer: a prospective trial. Ann Oncol. 2004;15(7):1042–1047. doi: 10.1093/annonc/mdh276. [DOI] [PubMed] [Google Scholar]
- 51.Lee SM, Lewanski CR, Counsell N, Ottensmeier C, Bates A, Patel N, et al. Randomized trial of erlotinib plus whole-brain radiotherapy for NSCLC patients with multiple brain metastases. J Natl Cancer Inst. 2014;106(7):ii. [DOI] [PMC free article] [PubMed]
- 52.Lind JS, Lagerwaard FJ, Smit EF, Senan S. Phase I study of concurrent whole brain radiotherapy and erlotinib for multiple brain metastases from non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2009;74(5):1391–1396. doi: 10.1016/j.ijrobp.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 53.Ma S, Xu Y, Deng Q, Yu X. Treatment of brain metastasis from non-small cell lung cancer with whole brain radiotherapy and Gefitinib in a Chinese population. Lung Cancer. 2009;65(2):198–203. doi: 10.1016/j.lungcan.2008.10.028. [DOI] [PubMed] [Google Scholar]
- 54.Welsh JW, Komaki R, Amini A, Munsell MF, Unger W, Allen PK, et al. Phase II trial of erlotinib plus concurrent whole-brain radiation therapy for patients with brain metastases from non-small-cell lung cancer. J Clin Oncol. 2013;31(7):895–902. doi: 10.1200/JCO.2011.40.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhuang H, Yuan Z, Wang J, Zhao L, Pang Q, Wang P. Phase II study of whole brain radiotherapy with or without erlotinib in patients with multiple brain metastases from lung adenocarcinoma. Drug Des Devel Ther. 2013;7:1179–1186. doi: 10.2147/DDDT.S53011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Olmez I, Donahue BR, Butler JS, Huang Y, Rubin P, Xu Y. Clinical outcomes in extracranial tumor sites and unusual toxicities with concurrent whole brain radiation (WBRT) and Erlotinib treatment in patients with non-small cell lung cancer (NSCLC) with brain metastasis. Lung Cancer. 2010;70(2):174–179. doi: 10.1016/j.lungcan.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 57.Zeng YD, Zhang L, Liao H, Liang Y, Xu F, Liu JL, et al. Gefitinib alone or with concomitant whole brain radiotherapy for patients with brain metastasis from non-small-cell lung cancer: a retrospective study. Asian Pac J Cancer Prev. 2012;13(3):909–914. doi: 10.7314/APJCP.2012.13.3.909. [DOI] [PubMed] [Google Scholar]
- 58.Zhu Q, Sun Y, Cui Y, Ye K, Yang C, Yang D, et al. Clinical outcome of tyrosine kinase inhibitors alone or combined with radiotherapy for brain metastases from epidermal growth factor receptor (EGFR) mutant non small cell lung cancer (NSCLC) Oncotarget. 2017;8(8):13304–13311. doi: 10.18632/oncotarget.14515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sullivan I, Planchard D. Next-generation EGFR tyrosine kinase inhibitors for treating EGFR-mutant lung cancer beyond first line. Front Med (Lausanne) 2016;3:76. doi: 10.3389/fmed.2016.00076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zeng Q, Wang J, Cheng Z, Chen K, Johnstrom P, Varnas K, et al. Discovery and evaluation of clinical candidate AZD3759, a potent, oral active, central nervous system-penetrant, epidermal growth factor receptor tyrosine kinase inhibitor. J Med Chem. 2015;58(20):8200–8215. doi: 10.1021/acs.jmedchem.5b01073. [DOI] [PubMed] [Google Scholar]
- 61.Yang Z, Guo Q, Wang Y, Chen K, Zhang L, Cheng Z, et al. AZD3759, a BBB-penetrating EGFR inhibitor for the treatment of EGFR mutant NSCLC with CNS metastases. Sci Transl Med. 2016;8(368):368ra172. doi: 10.1126/scitranslmed.aag0976. [DOI] [PubMed] [Google Scholar]
- 62.Yang JC-H, Cho BC, Kim D-W, Kim S-W, Lee J-S, Su W-C, et al. Osimertinib for patients (pts) with leptomeningeal metastases (LM) from EGFR-mutant non-small cell lung cancer (NSCLC): Updated results from the BLOOM study. J Clin Oncol. 2017;35(suppl 18):abst 2020.
- 63.Cho BC, Ahn M-J, Lee J-S, Kim D-W, Kim S-W, John T, et al. Phase I study (BLOOM) of AXD3759, a BBB penetrable EGFR inhibitor, in EGFRm NSCLC patients with leptomeningeal metastasis (LM) who progressed after other anti-cancer therapy. J Clin Oncol. 2017;35(suppl 18):abst 2069.
- 64.Ahn M-J, Kim D-W, Cho BC, Kim S-W, Lee J-S, Ahn JS, et al. Phase I study (BLOOM) of AXD3759, a BBB penetrable EGFR inhibitor, in TKI naïve EGFRm NSCLC patients in CNS metastases. J Clin Oncol. 2017;35(suppl 18):abst 2006.
- 65.Wu YL, Cheng Y, Zhou X, Lee KH, Nakagawa K, Niho S, et al. Dacomitinib versus gefitinib as first-line treatment for patients with EGFR-mutation-positive non-small-cell lung cancer (ARCHER 1050): a randomised, open-label, phase 3 trial. Lancet Oncol. 2017;18(11):1454–1466 [DOI] [PubMed]
- 66.Piccioni D. A Phase II Study of Dacomitinib in Progressive Brain Metastases. https://www.clinicaltrialsgov/ct2/show/study/NCT02047747?view=record, 2016.
- 67.Cross DA, Ashton SE, Ghiorghiu S, Eberlein C, Nebhan CA, Spitzler PJ, et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov. 2014;4(9):1046–1061. doi: 10.1158/2159-8290.CD-14-0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li D, Ambrogio L, Shimamura T, Kubo S, Takahashi M, Chirieac LR, et al. BIBW2992, an irreversible EGFR/HER2 inhibitor highly effective in preclinical lung cancer models. Oncogene. 2008;27(34):4702–11. [DOI] [PMC free article] [PubMed]
- 69.Solca F, Dahl G, Zoephel A, Bader G, Sanderson M, Klein C, et al. Target binding properties and cellular activity of afatinib (BIBW 2992), an irreversible ErbB family blocker. J Pharmacol Exp Ther. 2012;343(2):342–50. [DOI] [PubMed]
- 70.Wind S, Schmid M, Erhardt J, Goeldner RG, Stopfer P. Pharmacokinetics of afatinib, a selective irreversible ErbB family blocker, in patients with advanced solid tumours. Clin Pharmacokinet. 2013;52(12):1101–9. [DOI] [PubMed]
- 71.Schuler M, Wu YL, Hirsh V, O’Byrne K, Yamamoto N, Mok T, et al. First-line afatinib versus chemotherapy in patients with non-small cell lung cancer and common epidermal growth factor receptor gene mutations and brain metastases. J Thorac Oncol. 2016;11(3):380–390. doi: 10.1016/j.jtho.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 72.Yufen X, Binbin S, Wenyu C, Jialiang L, Xinmei Y. The role of EGFR-TKI for leptomeningeal metastases from non-small cell lung cancer. Springerplus. 2016;5(1):1244. [DOI] [PMC free article] [PubMed]
- 73.Zhang SR, Zhu LC, Jiang YP, Zhang J, Xu RJ, Xu YS, et al. Efficacy of afatinib, an irreversible ErbB family blocker, in the treatment of intracerebral metastases of non-small cell lung cancer in mice. Acta Pharmacol Sin. 2017;38(2):233–240. doi: 10.1038/aps.2016.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sequist LV, Yang JC, Yamamoto N, O’Byrne K, Hirsh V, Mok T, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol. 2013;31(27):3327–34. [DOI] [PubMed]
- 75.Wu YL, Zhou C, Hu CP, Feng J, Lu S, Huang Y, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(2):213–22. [DOI] [PubMed]
- 76.Yang JC, Wu YL, Schuler M, Sebastian M, Popat S, Yamamoto N, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015;16(2):141–51. [DOI] [PubMed]
- 77.Park K, Tan EH, O’Byrne K, Zhang L, Boyer M, Mok T, et al. Afatinib versus gefitinib as first-line treatment of patients with EGFR mutation-positive non-small-cell lung cancer (LUX-lung 7): a phase 2B, open-label, randomised controlled trial. Lancet Oncol. 2016;17(5):577–589. doi: 10.1016/S1470-2045(16)30033-X. [DOI] [PubMed] [Google Scholar]
- 78.Hochmair M, Holzer S, Burghuber OC. Complete remissions in afatinib-treated non-small-cell lung cancer patients with symptomatic brain metastases. Anti-Cancer Drugs. 2016;27(9):914–915. doi: 10.1097/CAD.0000000000000410. [DOI] [PubMed] [Google Scholar]
- 79.Girard N. Optimizing outcomes in EGFR mutation-positive NSCLC: which tyrosine kinase inhibitor and when? Future Oncol. 2018: 10.2217/fon-2017-0636. [DOI] [PubMed]
- 80.Tamiya A, Tamiya M, Nishihara T, Shiroyama T, Nakao K, Tsuji T, et al. Cerebrospinal fluid penetration rate and efficacy of Afatinib in patients with EGFR mutation-positive non-small cell lung Cancer with leptomeningeal Carcinomatosis: a multicenter prospective study. Anticancer Res. 2017;37(8):4177–4182. doi: 10.21873/anticanres.11806. [DOI] [PubMed] [Google Scholar]
- 81.Baird RD, Garcia-Corbacho J, Linossi C, Kumar SS, Smith D, Williams M, et al. Cambridge Brain Mets Trial 1 (CamBMT1). A proof of principle study of afatinib penetration into cerebral metastases (mets) for patients (pts) undergoing neurosurgical resection, combined with prior low-dose, targeted radiotherapy (RT). Phase 1b results. J Clin Oncol. 2017;35(18_suppl):abst 2008.
- 82.Eze C, Hegemann NS, Roengvoraphoj O, Dantes M, Manapov F. Concurrent Afatinib and whole-brain radiotherapy in exon 19-del-EGFR mutant lung adenocarcinoma: a case report and mini review of the literature. Front Oncol. 2017;7:88. doi: 10.3389/fonc.2017.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Li SH, Hsieh MH, Fang YF. Afatinib in treatment-naive patients with EGFR-mutated lung adenocarcinoma with brain metastasis: a case series. Medicine (Baltimore) 2015;94(41):e1739. doi: 10.1097/MD.0000000000001739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li SH, Liu CY, Hsu PC, Fang YF, Wang CC, Kao KC, et al. Response to afatinib in treatment-naive patients with advanced mutant epidermal growth factor receptor lung adenocarcinoma with brain metastases. Expert Rev Anticancer Ther. 2018;18(1):81–89. doi: 10.1080/14737140.2018.1409623. [DOI] [PubMed] [Google Scholar]
- 85.Ghosn M, Assi T, El Rassy E, Moussa T, Kattan J. An unexpected response to second line EGFR inhibitor in relapsing leptomeningeal carcinomatosis from lung adenocarcinoma raises questions on differential mechanisms of action of these agents. Bull Cancer. 2017;104(4):385–387. doi: 10.1016/j.bulcan.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 86.Kawaguchi Y, Hanaoka J, Hayashi H, Mizusaki N, Iihara H, Itoh Y, et al. Clinical efficacy of afatinib treatment for a patient with leptomeningeal carcinomatosis. Chemotherapy. 2017;62(3):147–150. doi: 10.1159/000454727. [DOI] [PubMed] [Google Scholar]
- 87.Lin CH, Lin MT, Kuo YW, Ho CC. Afatinib combined with cetuximab for lung adenocarcinoma with leptomeningeal carcinomatosis. Lung Cancer. 2014;85(3):479–480. doi: 10.1016/j.lungcan.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 88.Tamiya A, Tamiya M, Nishihara T, Shiroyama T, Nakao K, Tsuji T, et al. Afatinib efficacy and cerebrospinal fluid concentration in NSCLC patients with EGFR mutation developing leptomeningeal carcinomatosis. Ann Oncol. 2016;27(suppl 6):abst 1241P.
- 89.Saijo T, Ito T, Ikeda N. Three cases of EGFR mutation-positive lung adenocarcinoma with leptomeningeal Carcinomatosis successfully treated with Afatinib. Haigan. 2016;56(4):290–6.
- 90.Sequist LV, Waltman BA, Dias-Santagata D, Digumarthy S, Turke AB, Fidias P, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3(75):75ra26. [DOI] [PMC free article] [PubMed]
- 91.Yang JC-H, Ahn M-J, Kim D-W, Ramalingam SS, Sequist LV, Su W-C, et al. Osimertinib in pretreated T790M-positive advanced non–small-cell lung Cancer: AURA study phase II extension component. J Clin Oncol. 2017;35(12):1288–1296. doi: 10.1200/JCO.2016.70.3223. [DOI] [PubMed] [Google Scholar]
- 92.Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim HR, Ramalingam SS, et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N Engl J Med. 2017;376(7):629–640. doi: 10.1056/NEJMoa1612674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Janne PA, Yang JC, Kim DW, Planchard D, Ohe Y, Ramalingam SS, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med. 2015;372(18):1689–1699. doi: 10.1056/NEJMoa1411817. [DOI] [PubMed] [Google Scholar]
- 94.Soria JC, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2017;378(2):113–125. doi: 10.1056/NEJMoa1713137. [DOI] [PubMed] [Google Scholar]
- 95.Ballard P, Yates JW, Yang Z, Kim DW, Yang JC, Cantarini M, et al. Preclinical comparison of osimertinib with other EGFR-TKIs in EGFR-mutant NSCLC brain metastases models, and early evidence of clinical brain metastases activity. Clin Cancer Res. 2016;22(20):5130–5140. doi: 10.1158/1078-0432.CCR-16-0399. [DOI] [PubMed] [Google Scholar]
- 96.Goss G, Tsai C-M, Shepherd F, Ahn M-J, Bazhenova L, Crinò L, et al. CNS response to osimertinib in patients with T790M-positive advanced NSCLC: Pooled data from two Phase II trials. J Thorac Oncol. 2017;12(1):S440–S1;abst MA16.11. [DOI] [PubMed]
- 97.Mok T, Ahn M, Han J. CNS response to osimertinib in patients (pts) with T790M-positive advanced NSCLC: data from a randomized phase III trial (AURA3). J Clin Oncol. 2017;35(suppl 15):9005.
- 98.Vansteenkiste J, Reungwetwattana T, Nakagawa K, Cho BC, Cobo Dols MA, Cho EK, et al. CNS response to osimertinib vs standard of care (SoC) EGFR-TKI as first-line therapy in patients (pts) with EGFR-TKI sensitising mutation (EGFRm)-positive advanced non-small cell lung cancer (NSCLC): Data from the FLAURA study. Ann Oncol. 2017;28(suppl 10):abstract LBA5.
- 99.Planchard D, Loriot Y, Andre F, Gobert A, Auger N, Lacroix L, et al. EGFR-independent mechanisms of acquired resistance to AZD9291 in EGFR T790M-positive NSCLC patients. Ann Oncol. 2015;26(10):2073–2078. doi: 10.1093/annonc/mdv319. [DOI] [PubMed] [Google Scholar]
- 100.Song HN, Jung KS, Yoo KH, Cho J, Lee JY, Lim SH, et al. Acquired C797S mutation upon treatment with a T790M-specific third-generation EGFR inhibitor (HM61713) in non-small cell lung Cancer. J Thorac Oncol. 2016;11(4):e45–e47. doi: 10.1016/j.jtho.2015.12.093. [DOI] [PubMed] [Google Scholar]
- 101.Thress KS, Paweletz CP, Felip E, Cho BC, Stetson D, Dougherty B, et al. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non-small cell lung cancer harboring EGFR T790M. Nat Med. 2015;21(6):560–562. doi: 10.1038/nm.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ramalingam SS, Yang JC, Lee CK, Kurata T, Kim DW, John T, et al. Osimertinib as first-line treatment of EGFR mutation-positive advanced non-small-cell lung Cancer. J Clin Oncol. 2017;25:JCO2017747576. doi: 10.1200/JCO.2017.74.7576. [DOI] [PubMed] [Google Scholar]
- 103.Porta R, Sanchez-Torres JM, Paz-Ares L, Massuti B, Reguart N, Mayo C, et al. Brain metastases from lung cancer responding to erlotinib: the importance of EGFR mutation. Eur Respir J. 2011;37(3):624–31. [DOI] [PubMed]
- 104.Ohara S, Ushijima T, Gunji M, Tanai C, Tanaka Y, Noda H, et al. Brain metastasis effectively treated with erlotinib following the acquisition of resistance to gefitinib: a case report. J Med Case Rep. 2014;8:64. doi: 10.1186/1752-1947-8-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ruppert AM, Beau-Faller M, Neuville A, Guerin E, Voegeli AC, Mennecier B, et al. EGFR-TKI and lung adenocarcinoma with CNS relapse: interest of molecular follow-up. Eur Respir J. 2009;33(2):436–440. doi: 10.1183/09031936.00162307. [DOI] [PubMed] [Google Scholar]
- 106.Katayama T, Shimizu J, Suda K, Onozato R, Fukui T, Ito S, et al. Efficacy of erlotinib for brain and leptomeningeal metastases in patients with lung adenocarcinoma who showed initial good response to gefitinib. J Thorac Oncol. 2009;4(11):1415–1419. doi: 10.1097/JTO.0b013e3181b62572. [DOI] [PubMed] [Google Scholar]
- 107.Ahn MJ, Kim DW, Cho BC, Kim SW, Lee JS, Ahn JS, et al. Activity and safety of AZD3759 in EGFR-mutant non-small-cell lung cancer with CNS metastases (BLOOM): a phase 1, open-label, dose-escalation and dose-expansion study. Lancet Respir Med. 2017;5(11):891–902. doi: 10.1016/S2213-2600(17)30378-8. [DOI] [PubMed] [Google Scholar]


