Abstract
Introduction
Information exchange is critical to high-quality care transitions from hospitals to post-acute care (PAC) facilities. We conducted a survey to evaluate the completeness and timeliness of information transfer and communication between a tertiary care academic hospital and its related PAC facilities.
Methods
This was a cross-sectional web-based 36-question survey of 110 PAC clinicians and staff representing 31 PAC facilities conducted between October and December 2013.
Results
We received responses from 71 of 110 individuals representing 29 of 31 facilities (65% and 94% response rates). We collapsed 4-point Likert responses into dichotomous variables to reflect completeness (sufficient vs. insufficient) and timeliness (timely vs. not timely) for information transfer and communication. Among respondents, 32% reported insufficient information about discharge medical conditions and management plan, and 83% reported at least occasionally encountering problems directly related to inadequate information from the hospital. Hospital clinician contact information was the most common insufficient domain. With respect to timeliness, 86% of respondents desired receipt of a discharge summary on or before the day of discharge, but only 58% reported receiving the summary within this timeframe. Through free text responses, several participants expressed the need for paper prescriptions for controlled pain medications to be sent with patients at the time of transfer.
Discussion
Staff and clinicians at PAC facilities perceive substantial deficits in content and timeliness of information exchange between the hospital and facilities. Such deficits are particularly relevant in the context of the increasing prevalence of bundled payments for care across settings as well as forthcoming readmissions penalties for PAC facilities. Targets identified for quality improvement include: structuring discharge summary information to include information identified as deficient by respondents, completion of discharge summaries prior to discharge to PAC facilities, and provision of hard-copy opioid prescriptions at discharge.
Introduction
Information exchange is critical to high-quality care transitions between care settings. Insufficient or untimely information exchange between hospitals and other settings can lead to medication discrepancies, missed test results, and even rehospitalization.1–6 Optimizing information exchange between hospitals and post-acute care (PAC) facilities accepting patients after hospital discharge is of particular importance because clinicians often need to provide treatments (e.g., antibiotics, pain medications) to patients immediately upon arrival at the PAC facility. In a prior study, 22% of transfers from PAC facilities back to an acute care hospital occurred within six days of admission to the facility, and 11% occurred within 2 days of admission, suggesting failure of care transitions from hospitals to PAC facilities.7 As Medicare increasingly prioritizes reducing preventable readmissions to the hospital from all care settings, improving communication across the care continuum has become a priority for hospitals and PAC facilities.8 To inform future quality improvement initiatives, we sought perspectives of PAC clinicians and staff about the sufficiency and timeliness of information transfer from a tertiary-care academic medical center to PAC facilities accepting referrals from this hospital.
Methods
We completed a cross-sectional survey of 110 post-acute care clinicians and staff at 31 PAC facilities between October 2013 and December 2013. A purposeful recruitment strategy was used to identify and recruit PAC facilities. First, organizations or PAC facilities with both a high volume of discharges and close proximity to our hospital were identified. Five were organizations that owned and managed multiple facilities in Colorado, and four were single facilities. Among the nine organizations/facilities identified, only one, a government-owned facility, did not express interest in an online EHR portal. Each managing organization was encouraged to identify facilities within their network that would like to acquire an EHR portal for our hospital. Clinical leadership within each facility identified clinicians and staff who wished to acquire access to the EHR portal, who then comprised the survey sample. Participants were sent a web-based, 36-question survey to evaluate the completeness and timeliness of information provided from UCH to the facility; sample questions are available in Appendix 1. Several of the survey questions were modified from a previously-validated publically available instrument, the PREPARED survey, which was designed to measure the quality of information transfer from the hospital to community providers.9
A majority of survey questions requested responses on a 4-point Likert scale, and additional questions assessed challenges to receiving complete and timely information encountered by respondents through questions about specific discharge information (e.g., hospitalist contact information, code status), in categorical and free text responses. We collapsed 4-point Likert responses into dichotomous variables (e.g., sufficient vs. insufficient; timely vs. not timely). Survey responses were de-identified by individual and by facility for analysis. Analysis of the survey responses was descriptive and performed using Microsoft Excel (Redmond, WA). This study was reviewed by the Colorado Institutional Review Board and deemed not human subjects research.
Results
We received responses from 71 of 110 individuals (65% response rate) representing 29 of 31 PAC facilities (94% response rate for facilities). Four of the individual respondents represented one quality partnership group for an organization that owned and managed multiple facilities – of these respondents two were clinical liaisons and two were in sales/marketing positions. Five of 71 surveys were partially completed. Among the 29 PAC facilities with respondents, all offered skilled services; the number of responses ranged from 1 to 6 respondents per facility (average of 2.3 respondents per facility) and respondents reported between 40 and 242 patient beds at the facilities. In addition, 45% (n=31 of 69) of respondents reported having at least half of the beds at their facility dedicated to subacute care; 41% (n=28 of 69) and 70% (48 of 69) reported admitting patients from UCH at least weekly and at least monthly, respectively. Respondents reported a variety of roles: 32% (n=23) worked in admissions, 17% (n=12) were clinical liaisons, 13% (n=9) worked in health information or medical records, 10% (n=7) were physicians, 10% (n=7) worked in administration, 6% (n=4) worked in business or marketing, 6% (n=4) were directors of nursing. The remaining 7% (n=5) of respondents had other roles, including physician assistant, social services, and community relations.
Completeness
When asked about the completeness of information provided from the hospital, 32% (n=23) of respondents reported insufficient discharge medical condition and management plan information. Among the subset of eight physician or physician assistant respondents, 63% reported having insufficient discharge medical condition and management plan information. In addition, 83% (n=58 of 70) of respondents reported that they occasionally, often, or almost always encounter problems directly related to not having adequate information about a patient they receive from the hospital. The six most frequent insufficient discharge domains are shown in Figure 1. The most commonly-identified insufficient domain was hospital clinician contact information, followed by the plan for tests that are pending at discharge (e.g., blood cultures), indication and planned duration for lines and catheters, code status, contact isolation for infections (e.g., Clostridium difficile), and medications and medication management.
Figure 1.
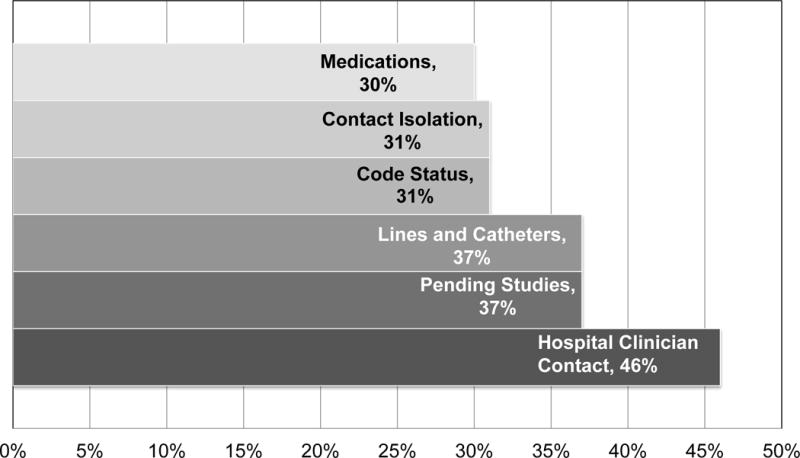
Most Frequently-Identified Insufficient Discharge Domains
Proportion of Respondents Identifying Domains as Insufficient
Timeliness
When asked about the average timeliness of discharge information receipt, although 86% (n=61) of respondents desired receipt of discharge summaries on or before the day of discharge, only 58% (n=41) reported receiving summaries within this timeframe. In addition, 10% (n=7) reported never receiving discharge paperwork from the discharging hospital.
Additional Suggestions for Improvement
Respondents submitted additional areas for improvement in PAC transfers through free text responses. A recurring theme was the desire for hard-copy paper prescriptions for controlled pain medications to be sent with patients at the time of transfer to avoid delay in filling and administration of these medications, as in the following response: “Not certain if hard scripts are sent with the patient at (discharge). DEA regulations make pain management difficult for patients with acute needs arriving late in the day. Hard copies would mitigate any wait time for pain medication administration.”
Discussion
Clinicians and staff at PAC facilities receiving hospital transfers reported substantial deficits in completeness and timeliness of information received upon hospital discharge. Of note, how to contact the appropriate hospital clinician was the most frequently deficient piece of information, which has implications for patient safety during care transitions to PAC facilities. In addition, the difference between desired and actual receipt of discharge summary was substantial, which suggests an opportunity to improve the timeliness of information provided to PAC facilities during this critical time.
The results from our study are comparable to those from a qualitative study completed by King and colleagues with focus groups of registered nurses from skilled nursing facilities.5 In this study, nurses reported problems with medications, including frequently lacking signed paper prescriptions for opioid pain medications, which contributed to patient care delays, as noted in our study. Nurses in the King study expressed the desire for improved access to a prescribing provider, ideally from the hospital, to clarify information discrepancies after patient arrival to the facility. An second focus group study with nurses from hospitals and PAC facilities found that a lack of communication between the hospital and PAC can create difficulty when PAC nurses are contemplating whether patients need to be transferred back to the hospital from a PAC facility.10
One factor that may adversely influence discharge information timeliness for PAC facilities is that discharge summaries may not be required to be completed prior to PAC transfer. The requirement of discharge summary completion prior to PAC transfer varies across institutions. A uniform requirement for discharge summary completion by the time of transfer to PAC would address the identified gap between desired and actual state with regard to timely receipt of discharge summaries, and could potentially reduce hospital readmission rates.6 Additional targets for improvement identified in this gap analysis include: improved documentation of hospital clinician contact information, pending studies, indication and duration for lines and catheters, code status, need for contact isolation, and medication management. Many of the elements we identified as insufficient are included in existing tools to improve information exchange between acute hospitals to PAC facilities, which will guide future quality improvements.11 Within free text responses, we also identified a need to provide paper prescriptions for opioids and other controlled substances upon transfer to PAC facilities.
A limitation of this study is that it was completed across multiple PAC facilities to examine the completeness and timeliness of information received from a single tertiary care academic center. The facilities included in this study accept variable volumes of transfers from this single hospital. In addition, even though responses were de-identified by individual and facility, it is possible that the surveyed PAC facility clinicians and staff may have underestimated concerns to avoid jeopardizing their referral relationship with the hospital. Further, the majority of respondents were not clinicians, and the responses of clinicians may differ significantly from non-clinical staff. To mitigate this bias, we completed a sensitivity analysis excluding the four respondents reporting marketing or business positions and found that results were minimally changed compared with the primary analysis with regard to timeliness and insufficient discharge domains. In addition, because sampling was completed in a purposeful manner in which clinical leadership within each facility identified clinicians and staff with interest in an EHR portal, the number of clinicians and staff who were approached and did not express interest in the portal are unknown. We are not aware of the total clinicians and staff that work at all surveyed facilities.
The results of this analysis are not generalizable beyond this context. Yet, the similarity of our results to the study by King and colleagues suggests that fragmented coordination between hospital and PAC facilities is potentially a widespread problem. Strengths of this study include use of questions from a previously-validated survey, which were modified for care transitions from the hospital to PAC facilities.
Our next step to improve this process is providing internet-based portal access to our hospital’s electronic health record (EHR) for PAC facilities with the highest volumes of referrals. After implementation of portal access to our EHR for PAC facilities, we plan to repeat this survey to determine if access to our EHR improves information exchange. Although improved access to our EHR is a step to improve information availability to PAC staff and clinicians, we suspect that an additional multi-faceted intervention will be needed since many of the issues identified by our survey respondents may not be fully addressed by providing PAC facility staff and clinicians with read-only access to our EHR. Such an intervention would likely incorporate formal tools and templates from existing programs, with formal auditing from the PAC perspective to ensure that the tools are consistently completed.11 In addition, an optimal intervention to address identified issues would include bi-directional information exchange and communication between the hospital and PAC setting that is integrated in clinical workflow for users in both the hospital and PAC facility. Finally, a future intervention would help to align data collection and information exchange across settings and provide information that the IMPACT Act will require PAC facilities to report.12
Conclusion
In the context of policy reforms that are increasing accountability for patients across care settings, this study has implications for hospitals and PAC facilities seeking to improve information exchange. Several targets were identified to improve the completeness and timeliness of information transfer and communication at the time of care transitions from the hospital to PAC facilities. Future interventions to improve content and timeliness of communication with PAC facilities could include: 1) structured discharge information to include frequently-insufficient domains reported by respondents, 2) provision of hard-copy opioid prescriptions at discharge, and 3) completion of discharge summaries prior to patient transfer to PAC facilities.
Appendix 1: Survey Question Examples: Completeness and Timeliness
| Completeness | Sufficient Responses | Insufficient Responses | |
|---|---|---|---|
| Overall | In general, how often do you have access to sufficient information from the [hospital name] about a patient’s discharge medical conditions and management plan? | -Almost Always -Frequently |
-Occasionally -Rarely |
| Medications | How often do you generally have access to sufficient information from the [hospital name] about a patient’s medicines and medication management? | -Almost Always -Frequently |
-Occasionally -Rarely |
| Contact Isolation | In general, how sufficient is information from [hospital name] about whether patients have been diagnosed with infections that require contact isolation, such as multi-drug resistant organisms (e.g. MRSA) and clostridium difficile? | - More than sufficient - Sufficient |
- Less than sufficient - Not at all |
| Code Status | Are you generally made aware by [hospital name] of advanced directives and code status of a patient? | - Yes | - No |
| Lines and Catheters | In general, how sufficient is information from [hospital name] about indication and planned duration for devices such as PICC lines and Foley catheters? | - More than sufficient - Sufficient |
- Less than sufficient - Not at all |
| Pending Tests | In general, how adequate are instructions from [hospital name] about the follow up plan for tests that are pending at discharge (e.g., blood culture results)? | - More than adequate - Adequate |
- Less than adequate - No information is provided |
| Clinician Contact | In general, how sufficient is information from [hospital name] about how to contact the appropriate clinician at UCH with questions about a patient’s management? | - More than sufficient - Sufficient |
- Less than sufficient - Not at all |
| Timeliness | Timely | Not Timely | |
| Desired | On average, when do you have access to a discharge summary for a patient admitted to your facility from [hospital name]? | - While patient is in hospital - On the day of discharge |
- 1-3 days following discharge - >3 days following discharge - Discharge paperwork is never received |
| Actual | In your opinion, when do you feel that you should have access to a discharge summary for a patient that is admitted to your facility from [hospital name]? | - While patient is in hospital - On the day of discharge |
- 1-3 days following discharge - >3 days following discharge - Discharge summary is not necessary |
Footnotes
Disclosures: No conflicts of interest
References
- 1.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831–41. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 2.Callen J, Georgiou A, Li J, Westbrook JI. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf. 2011;20:194–9. doi: 10.1136/bmjqs.2010.044339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18:646–51. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tjia J, Bonner A, Briesacher BA, McGee S, Terrill E, Miller K. Medication discrepancies upon hospital to skilled nursing facility transitions. J Gen Intern Med. 2009;24:630–5. doi: 10.1007/s11606-009-0948-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.King BJ, Gilmore-Bykovskyi AL, Roiland RA, Polnaszek BE, Bowers BJ, Kind AJ. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc. 2013;61:1095–102. doi: 10.1111/jgs.12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoyer EH, Odonkor CA, Bhatia SN, Leung C, Deutschendorf A, Brotman DJ. Association between days to complete inpatient discharge summaries with all-payer hospital readmissions in Maryland. J Hosp Med. 2016;11:393–400. doi: 10.1002/jhm.2556. [DOI] [PubMed] [Google Scholar]
- 7.Ouslander JG, Naharci I, Engstrom G, Shutes J, Wolf DG, Alpert G, Rojido C, Tappen R, Newman D. Root Cause Analyses of Transfers of Skilled Nursing Facility Patients to Acute Hospitals: Lessons Learned for Reducing Unnecessary Hospitalizations. J Am Med Dir Assoc. 2016;17:256–62. doi: 10.1016/j.jamda.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 8.MedPAC. Medicare Payment Advisory Commission Report to the Congress: Medicare Payment Policy. 2016 [Google Scholar]
- 9.Grimmer K, Moss J. The development, validity and application of a new instrument to assess the quality of discharge planning activities from the community perspective. Int J Qual Health Care. 2001;13:109–16. doi: 10.1093/intqhc/13.2.109. [DOI] [PubMed] [Google Scholar]
- 10.Kirsebom M, Wadensten B, Hedstrom M. Communication and coordination during transition of older persons between nursing homes and hospital still in need of improvement. J Adv Nurs. 2013;69:886–95. doi: 10.1111/j.1365-2648.2012.06077.x. [DOI] [PubMed] [Google Scholar]
- 11.Ouslander JG, Bonner A, Herndon L, Shutes J. The Interventions to Reduce Acute Care Transfers (INTERACT) quality improvement program: an overview for medical directors and primary care clinicians in long term care. J Am Med Dir Assoc. 2014;15:162–70. doi: 10.1016/j.jamda.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.cms.gov. IMPACT Act of 2014 & Cross Setting Measures. 2015 accessed May 20, 2016. [Google Scholar]


