Abstract
PURPOSE
To analyze stress distribution in premolars restored with inlays or onlays using various materials.
MATERIALS AND METHODS
Three-dimensional maxillary premolar models of abutments were designed to include the following: 1) inlay with O cavity (O group), 2) inlay with MO cavity (MO group), 3) inlay with MOD cavity (MOD group), and 4) onlay (ONLAY group). A restoration of each inlay or onlay cavity was simulated using gold alloy, e.max ceramic, or composite resin for restoration. To simulate masticatory forces, a total of 140 N static axial force was applied onto the tooth at the occlusal contact areas. A finite element analysis was performed to predict the magnitude and pattern of stresses generated by occlusal loading.
RESULTS
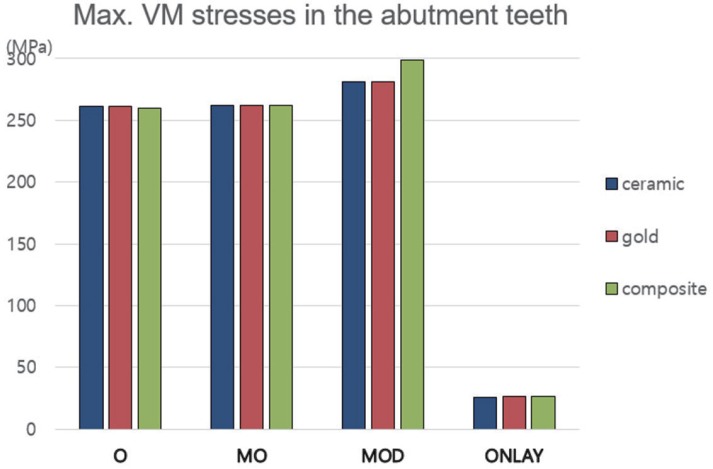
Maximum von Mises stress values generated in the abutment teeth of the ONLAY group were ranged from 26.1 to 26.8 MPa, which were significantly lower than those of inlay groups (O group: 260.3–260.7 MPa; MO group: 252.1–262.4 MPa; MOD group: 281.4–298.8 MPa). Maximum von Mises stresses generated with ceramic, gold, and composite restorations were 280.1, 269.9, and 286.6 MPa, respectively, in the MOD group. They were 252.2, 248.0, 255.1 MPa, respectively, in the ONLAY group.
CONCLUSION
The onlay design (ONLAY group) protected tooth structures more effectively than inlay designs (O, MO, and MOD groups). However, stress magnitudes in restorations with various dental materials exhibited no significant difference among groups (O, MO, MOD, ONLAY).
Keywords: Inlay, Onlay, Finite element analysis, Restorative material
INTRODUCTION
In restorative dentistry, inlays and onlays are frequently used as treatment options to restore missing tooth structure after removal of caries. Inlays can restore cavities inside the teeth. However, onlays can restore one or more cusps. It may completely cover the occlusal surface to obtain good stress distribution of the teeth. Compared to inlay, preparation of onlay requires additional tooth reduction. Vital teeth with conservative restorations are less susceptible to fracture than large restorations regardless of restorative material used.1,2
Reports on the strength of teeth after restoration using different designs are ambiguous. Stappert et al.3 have reported that tooth-inlay complex has higher fracture resistance than tooth-onlay complex. However, Arnelund et al.4 has reported that inlay restorations have higher failures rate than onlay restorations after a 5-year clinical evaluation. Controversy exists on the type of restoration that should be used to restore large defects to avoid fractures and improve survival rate.5,6
Gold alloy, composite resins, and dental ceramics are commonly used to restore inlay/onlay cavities of posterior teeth. When selecting materials for posterior restorations, clinicians need to take increasing patient expectations of aesthetic restorations and functionality into consideration. Gold restoration has been successfully used in dentistry for a long time.7 However, ceramic and composite restorations in posterior teeth have substituted gold restorations under various dental situations. For restorative dental material, a prerequisite is its ability to withstand chewing forces in the oral environment.8
Many dental researches have been conducted to find responses of restoration and restored tooth using various factors applied from outside, such as occlusal loading. Most studies on fracture mechanism in restored teeth are based on “in vivo” or “in vitro” experimental analyses.4,8,9,10,11 Recently, finite element analysis (FEA) has been used in biomechanical researches of clinical situations and various areas of dentistry.12,13,14,15,16 In fact, some dental and medical studies have been conducted on living subjects. They are costly and ethically skeptical. Using virtual models and simulations can help improve research results and reduce the cost of in vitro and in vivo experiments.17
Up to date, inconsistent and conflicting results have been reported from studies investigating the effect of inlay or onlay cavity design and restorative materials on stress distribution in the tooth-restoration complex.4,5,6,10,11,18 The objective of this study was to compare stress distribution and maximum stress observed in various restorations and in tooth structures of maxillary second premolars using three-dimensional FEA method. Various restorative materials with different mechanical properties (gold alloy, composite resins, and dental ceramics) were also compared in this study with each cavity design of inlay and onlay.
MATERIALS AND METHODS
Maxillary second premolar tooth model (D51DP-TRM, Nissan dental product Inc., Kyoto, Japan) was scanned using 3-D scanner (Freedom HD, DOF Inc., Seoul, Korea). Obtained surface contours and meshes were then imported into SolidWorks 2015 software (Dassault Systems Solid-Works Corp., Waltham, MA, USA). Three-dimensional solid model of the scanned tooth was generated by using a “SCANto3D” add-in module.
Interfacial surface between pulp chamber and dentin and interfacial surface between dentin and enamel were made by lofting technique of CAD program according to the anatomy of natural tooth (eHuman 3D Tooth Atlas 7.6, eHuman Inc., Fremont, CA, USA). After generating 3D volumes of enamel, dentin and pulp, Boolean operations were used to ensure congruence between relevant interfaces. For example, the dentin volume was generated by subtracting the pulp cavity volume. Next, the volume of dentin was subtracted to obtain a three-dimensional volume of enamel. All three-dimensional solid models of this study were derived from the three-dimensional solid model of intact maxillary second premolar.17
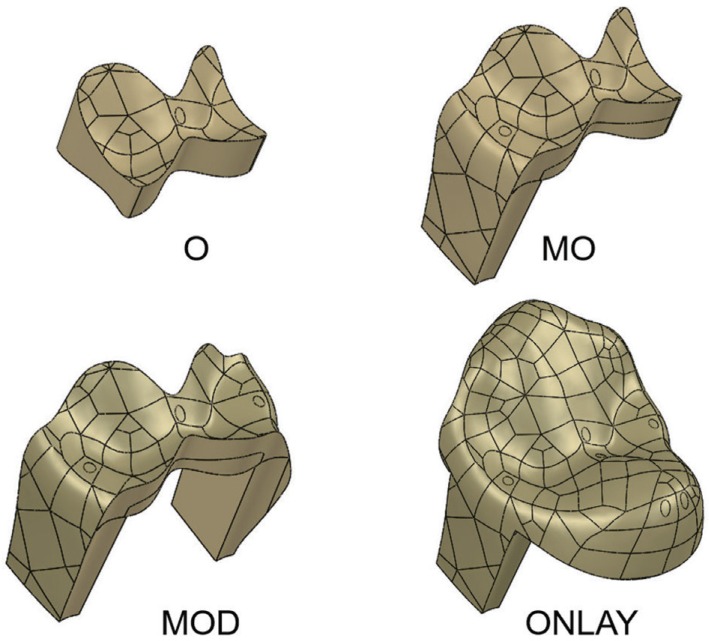
Inlay and onlay models were made based on the three-dimensional CAD model of intact maxillary premolar tooth. The following four 3D experimental models were designed and created: (1) O group (inlay with O cavity restored); (2) MO group (inlay with MO cavity restored); (3) MOD group (inlay with MOD cavity restored), and (4) ONLAY group (onlay restored). Shapes and dimensions of inlays and onlays were taken from the literature.20
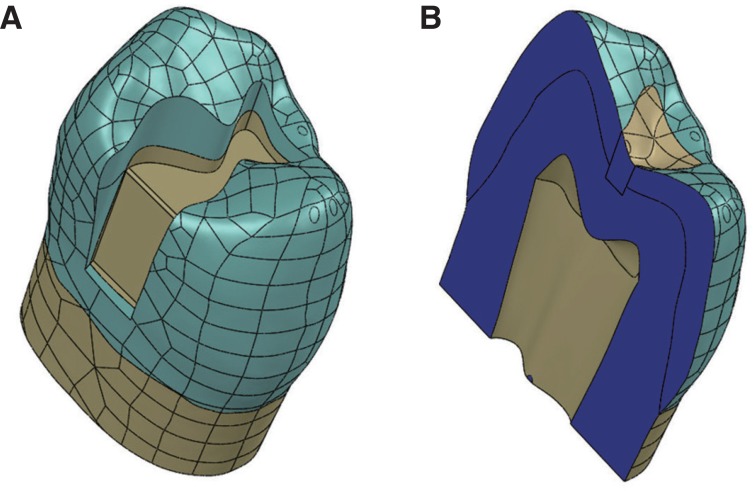
All inlay and onlay cavities had pulpal and axial walls with dentin thickness over the pulp for at least 1.0 mm while cervical walls of proximal boxes were located 1.0 mm above the cemento-enamel junction. Occlusal view of inlay cavity resembled a butterfly. The narrowest portion of the preparation was 0.9 mm faciolingually. It was located between buccal and lingual cusp tips. The cavity extended the full length of the occlusal groove, including mesial and distal pits with their radiating grooves. The pulpal wall was flat horizontally. The occlusocervical thickness of inlay was between 0.8 mm and 2.6 mm in the O group. In MO and MOD inlay cavity groups, cavity preparation was the same as that used for inlay with O cavity except that proximal boxes were extended proximally from the occlusal inlay cavity of the O group. The shape of the proximal box was on straight lines or planes with thickness of at least 0.6 mm. Onlay abutment was modified from the MOD inlay preparation. Occlusal surface was fully covered by onlay restoration with a thickness of approximately 1.0 mm in the ONLAY group (Fig. 1, Fig. 2).
Fig. 1. (A) MO cavity was created on the 3-D CAD model of the maxillary premolar tooth. (B) Cross-sectional view of premolar tooth showing the enamel, dentin and pulp chamber.
Fig. 2. Models of 3 inlays and 1 onlay bodies restored on the maxillary second premolars. (O), Class I inlay with butt joint and 0.9 mm-wide isthmus. (MO), Class II MO inlay with a mesial proximal box. (MOD), Class II inlay with both mesial and distal proximal boxes. (ONLAY), Onlay completely covers the occlusal surface with proximal boxes.
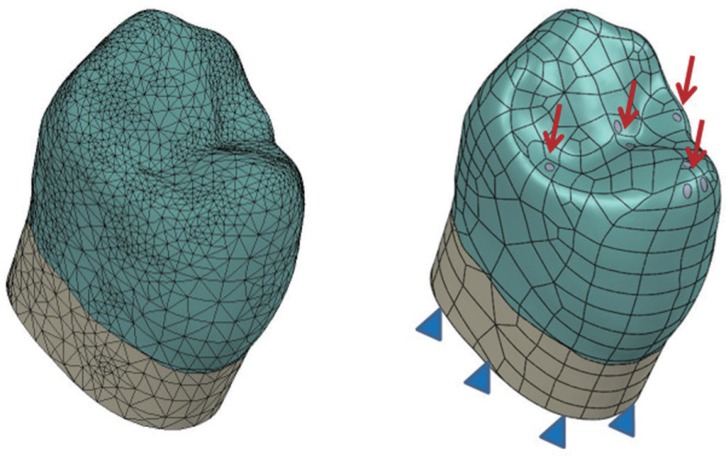
In each group, the following three types of restorative materials were used: (1) gold alloy, (2) e.max ceramic, and (3) composite resin. Young's modulus of elasticity and the Poisson's ratio for the materials used in this study were obtained from previous studies. They are summarized in Table 1.10,11,12,13,14 All materials were assumed to be linear, elastic, homogeneous and isotropic. Three-dimensional solid models were meshed with tetrahedral elements. The number of elements and nodes varies depending on the model (36,372 to 40,148 elements and 53,620 to 59,284 nodes). Fixed zerodisplacement and zero-rotation boundary conditions in all directions (X, Y, and Z) were assigned to nodes at the bottom of the tooth, preventing rigid body displacement for all models. To simulate biting forces, a total amount of 140 N load was applied vertically onto the tooth at 7 occlusal contact points (3 palatal cusp points, 2 central fossa points, and each point on both marginal ridges) (Fig. 3). A static FEA was performed to predict stress concentration produced by occlusal loading. Outputs of maximum von Misses stress, minimum principal (compressive), and maximum principal (tensile) stress values in the enamel, dentin, and restoration were evaluated separately.
Table 1. Materials used in models of premolars with inlays or onlay.
Fig. 3. 3-D solid models meshed with tetrahedral elements. All nodes on the lower surface of the tooth were constrained in all directions (X, Y, and Z), as a boundary condition. The static axial force was applied vertically onto the tooth at occlusal contact points (palatal cusp, central fossa, and marginal ridges).
RESULTS
The results of all structures were separated from the rest of the model to analyze the distribution and magnitude of stress in each component. For each group, maximum stresses on restorative material, enamel, and dentin were evaluated separately.
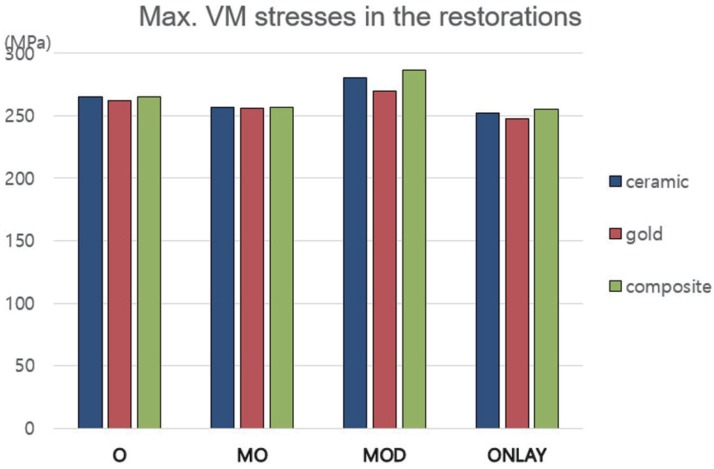
Regarding the effect of dental material, different restorative materials generated similar stress distribution patterns for all inlay groups when a total occlusal load of 140 N was applied onto functional cusp, marginal ridges, and central fossa. Composite resin generated the highest maximum von Mises stress, followed by ceramic and gold alloy, which showed the lowest value of maximum von Mises stress in restorations tested in this experiment. However, difference in maximum von Mises stress in the restorations with various restorative materials observed for the same cavity designs were small (1.4%, 0.2%, 5.8%, and 2.8% in the O, MO, MOD, and ONLAY groups, respectively).
Regarding the effect of cavity design, similar maximum von Mises stress values were found for restorations among experimental inlay and onlay groups. In general, stress intensity for both inlay and onlay cavity designs had the following order: MOD > O > MO > ONLAY. Maximum von Mises stresses generated in ceramic, gold, and composite restorations in the MOD group were 280.1, 269.9, and 286.6 Mpa, respectively. They were the highest. Maximum von Mises stresses generated in ceramic, gold, and composite restorations in the ONLAY group were 252.2, 248.0, 255.1 MPa, respectively. They were the lowest. The composite MOD group generated the highest stress in the restoration whereas the gold ONLAY group generated the lowest stress in the restoration (Fig. 4).
Fig. 4. Maximum von Mises stresses generated in restorations with various dental materials. Stress magnitudes in restorations restored with various dental materials showed relatively little differences among groups of O, MO, MOD and ONLAY.
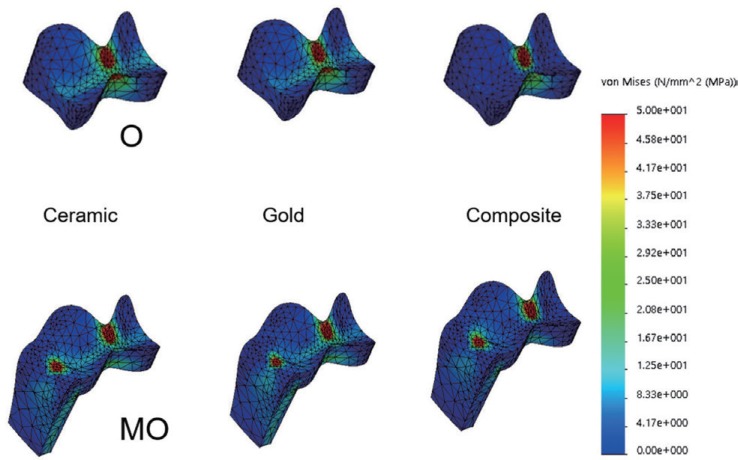
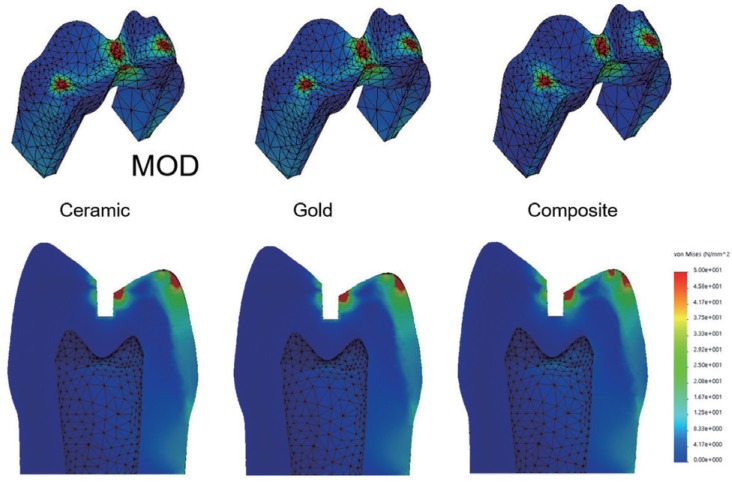
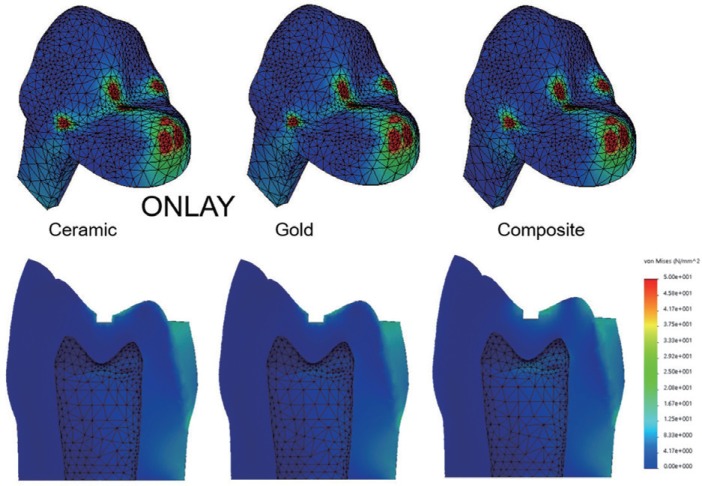
When all restorative materials and cavity designs of inlays or onlays were compared, the maximum stress values generated in restorations were close to each other between inlay/onlay designs or among the three tested dental materials with the same cavity design. In terms of stress location, high concentrations of von Mises stress on surfaces of restorations were found in the vicinity of occlusal contact surfaces where biting forces were applied (Fig. 5, Fig. 6, Fig. 7).
Fig. 5. Similar distribution and concentration pattern of von Mises stresses in restoration of the O group and the MO group during mastication. High stress concentration areas were generated at the loading site near central fossa in the O group. Marginal ridge and central fossa area generated maximum values in the MO group.
Fig. 6. Stress concentration localized around the central fossa and marginal ridges of MOD group regardless of various restorative materials.
Fig. 7. High von Mises stress concentration areas were observed at the loading site near the lingual cusp tip, marginal ridges and central fossa in onlay body regardless of various restorative materials. The ONLAY group showed a favorable distribution of stresses in the abutment tooth. Only a small value of von Mises stresses and slight difference in stress gradient were found in tooth structures.
Similar stress distribution patterns in enamel and dentin were observed in all inlay models. High stress concentrations were found at the enamel surface near the lingual cusp tip and marginal ridges where axial occlusal forces were applied. Abutment teeth of the ONLAY group with occlusal surface completely covered by restorative material generated 10 times lower value of maximum von Mises stress than the teeth with inlay groups (O, MO, and MOD). Reduced gradient of stress concentration was also found in the abutment tooth (Fig. 6, Fig. 7).
In terms of the highest stress values, differences in von Mises stress in the enamel with various restorative materials but the same cavity design were 0.2%, 0.1%, 5.9%, and 2.6% in the O, MO, MOD, and ONLAY groups, respectively. The gold MO group produced the highest von Mises stress (53.8 MPa) in the dentin, while the composite MOD group generated the highest von Mises stress (298.8 MPa) in the enamel when occlusal load was applied (Fig. 8).
Fig. 8. Maximum von Mises stresses generated in the abutment teeth with various dental materials. Stress values in ONLAY group were significantly lower than those of inlay groups (O, MO, MOD).
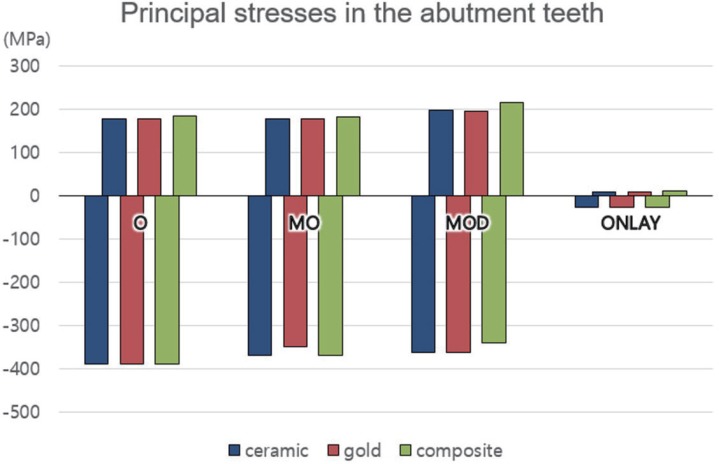
The maximum values of von Mises stress in abutment teeth in the ONLAY group were 26.1 to 26.8 MPa, which were significantly lower than those in inlay groups (O: 260.3-260.7; MO: 252.1-262.4; and MOD: 281.4-298.8 MPa). The maximum compressive stress values in abutment teeth of the ONLAY group were between 21.1 and 26.1 MPa, while those of inlay groups (O, MO, and MOD) were between 341.0 and 388.8 MPa. The maximum tensile stress values in abutment teeth of the ONLAY group were between 4.5 and 12.1 MPa, while those of inlay groups (O, MO, and MOD) were between 176.9 and 216.7 MPa. The compressive and tensile stress values of the ONLAY group were significantly lower than those of inlay groups (O, MO, MOD). However, magnitude tendencies of principal stress were similar to values of von Mises stress shown in Fig. 8 (Fig. 9).
Fig. 9. Maximum and minimum principal stresses generated in the abutment teeth with various dental materials. Bars with minus direction denote the minimum principal (compressive) stresses. Bars with plus direction show the maximum principal (tensile) stress. Magnitude tendencies of principal stress are similar to the values of von Mises stress shown in Fig. 8. Stress values in ONLAY group are significantly lower than those of inlay groups (O, MO, and MOD).
DISCUSSION
Masticatory loads in the posterior area are much higher than those in the anterior area of dentition. Among posterior teeth, maxillary premolars suffer the most from vertical fractures, leading to loss of dental element.19 This is why we choose maxillary second premolar as an abutment tooth for inlay/onlay restoration in this study. Concentration of stress can be associated with various forms of clinical failures such as tooth fracture, rupture of cement seal, and fracture of restorative body. The primary goal of this study was to evaluate maximum stress values and stress distribution after occlusal loading in order to identify the possibility of failure under different restoration conditions.
Conservation of healthy tooth structure is an important objective of restorative dentistry. However, from a mechanical point of view, protecting the remaining tooth structure from undesirable occlusal loading should be considered even if removal of additional dental tissue is necessary. Due to their unfavorable anatomical structure, maxillary premolars with extensive MOD cavities have a large risk of fracture if they are restored without obeying the principle of protection.6 Tooth preparation designs proposed for posterior inlay restorations are based on GV Black's recommendations for cast metal and amalgam, resulting in considerable tooth structure removal, parallel opposing walls, and steep internal line angles.20 The preparation design for an indirect restoration must satisfy a balance between preserving tooth structure and maximizing the strength of restoration. Removal of marginal ridges, increased depth and width of the inlay cavity, and increased preparation in proximal box formation are main reasons for decreased resistance to fracture.
St-Georges et al.18 have reported that MOD preparations can weaken their abutment teeth by about 59% and concluded that bonded MOD inlay restorations cannot restore the original strength of teeth. However, others have reported conflicting results on the effect of inlay cavity.3,5 Our FEA study results showed that the MOD group generated higher values of stresses to both inlay body and tooth structures than other groups (O, MO, ONLAY) when occlusal load was applied (Fig. 4, Fig. 8, Fig. 9). Mondelli et al.9 have suspected that the reason for the high risk of fracture in class II inlay cavity might be wedge effect. It can produce additional horizontal stresses on cavity walls.
According to a clinical long term study21 of IPS Empress inlays and onlays, cavity preparation mode (inlay vs. onlay) has no influence on the longevity of ceramic restorations over a clinical period of 12 years. However, other reports10,11 have suggested that onlay design is more effective in protecting tooth structures than inlay design. In our study, onlay with complete occlusal coverage exhibited the most favorable pattern of stress distribution in abutment teeth. The ONLAY group reduced the value of maximum von Mises stresses drastically in the abutment tooth (26.1–26.8 MPa), which was 10 times smaller in value than inlay groups. In our current study, as the restorative material covered the functional cusp in the ONLAY group, forces were absorbed by the restorative material and partially transferred to the abutment tooth. On the contrary, in groups with inlay design (O, MO, MOD), all loads on the functional cusp were directly transferred to tooth structures. Onlay covered buccal and lingual cusps of the tooth, resulting in a good distribution of stresses in teeth along with reduced fracture risk of maxillary premolar tooth (Fig. 5, Fig. 6, Fig. 7). FEA calculations obtained in this study were consistent with those of Dejak et al.10 that recommended ceramic onlay for wide inlay preparations in molars. Our results are also consistent with those of Yamanel et al.11 that advocated onlay design for protecting tooth structures.
In our study, stress distribution patterns in abutment teeth were similar to each other among all inlay groups (O, MO, and MOD). There were high stress concentration areas at loading points near the lingual cusp tip, marginal ridges, and central fossa. The composite MOD group generated the highest von Mises stress (286.5 MPa), while the gold ONLAY group exhibited the lowest von Mises stress (248.0 MPa) in the restoration. The composite MOD group generated the highest von Mises stress (298.8 MPa) in the abutment tooth when occlusal load was applied. Consequently, mechanical failure is most likely to occur in composite resin with MOD inlay during masticatory cycle (Fig. 8, Fig. 9).
Mechanical defects can be manifested by fractures in the restoration itself and the tooth fractures. If the maximum stress generated by the occlusal force exceeds the range of yield stress of compressive, tensile, and von Mises that the material can withstand, fracture occurs due to permanent deformation. The von Mises stress is calculated by the square root of the sum of the squares of the principle stress values. The von Mises stress provide a realistic value for predicting fracture in almost all cases when considering compression or warping, especially for materials with ductility. The maximum principal stress is useful as a basis for fracture to brittle materials.22 In this experiment, both principal stresses (compressive and tensile) and von Mises stresses were calculated and compared, but the tendency of results were similar regardless of the type of materials. Therefore, the results are mainly analyzed by the values of von Mises stress.
Although cast gold restoration remains the standard of care for inlays and onlays, tooth-colored restorative materials such as ceramic and filled polymer are acceptable at moderate level for long-term indirect restorative service. To date, several studies have been conducted to compare results and effects of various restorative materials for restoring inlay or onlay cavities. Based on a randomized clinical evaluation, Molin and Karlsson23 have reported that 92% of the 60 ceramic inlays and 100% of the 20 gold inlays are satisfactory after 5 years. All patients with fractured inlays have exhibited moderate to severe occlusal wear, which could be a contributory factor to fracture. Restorative material is considered as a factor that can affect the biomechanics during occlusal loading. Ceramic restorative material tends to concentrate more stress inside the inlay, resulting in lower cusp deflection than the resin, while resin tends to transfer more stress to the tooth structure and promote lower fracture resistance than the ceramic.8 Overall, the descending order of von Mises stress intensity in inlay/onlay restorations for each dental materials in our finite element stress analysis was as follows: composite resin > ceramic > gold alloy. This trend corresponds to the rank order of the elastic modulus used for each material, indicating that materials with lower elastic modulus can increase the stress observed in the restoration. If patient does not demand an aesthetic alternative, cast gold restoration is a reliable and effective treatment option. Interestingly, in contrast to cavity design for inlay and onlay, slight differences in maximum stresses were found for three different restorative materials in each experimental group (Fig. 4, Fig. 5, Fig. 6, Fig. 7). Therefore, using a proper cavity design might be more important than using certain restorative material.
Resistance to breakage of restored teeth with inlay or onlay is very complicated. It is not possible to incorporate all variables found in the oral environment into computer simulation.10 In this study, simplified three-dimensional models of maxillary second premolars with inlay/onlay were subjected to loading condition that might be generated in the last clenching stage of the chewing cycle. Stress concentration cannot predict failure pattern by a static computer simulation. However, higher von Mises stress concentration should be related to fracture of restoration or abutment tooth. In the oral cavity, complex and variable forces are applied to the teeth during function. Several limitations and weaknesses of computer simulation should be addressed in future studies. Furthermore, experimental and clinical validations are needed to draw firm conclusions.
CONCLUSION
Finite element stress analysis was performed in this study to determine the effect of inlay and onlay designs with various restorative materials on premolars under a masticatory force.
The highest value of von Mises stress was observed not only in the restoration but also in the enamel of the composite resin MOD group. Stress concentration areas were found at the loading site near the lingual cusp tip, marginal ridges, and central fossa. The stress distribution patterns in abutment teeth were similar to each other among all inlay groups.
Regarding the effect of restorative material, differences in maximum von Mises stress with the same cavity design were as small as 0.2% – 5.8% and 1.1% – 5.9% for restorations and abutment teeth, respectively. Regarding the effect of cavity design, onlay design (ONLAY) protected tooth structures more effectively than inlay designs (O, MO, MOD).
References
- 1.Shillingburg HT, Sather DA, Wilson EL, Cain JR, Mitchell DL, Blanco LJ, Kessler JC. Fundamentals of fixed prosthodontics. 4th ed. Chicago: Quintessence; 2012. pp. 193–227. [Google Scholar]
- 2.Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. 1989;15:512–516. doi: 10.1016/S0099-2399(89)80191-8. [DOI] [PubMed] [Google Scholar]
- 3.Stappert CF, Guess PC, Gerds T, Strub JR. All-ceramic partial coverage premolar restorations. Cavity preparation design, reliability and fracture resistance after fatigue. Am J Dent. 2005;18:275–280. [PubMed] [Google Scholar]
- 4.Arnelund CF, Johansson A, Ericson M, Häger P, Fyrberg KA. Five-year evaluation of two resin-retained ceramic systems: a retrospective study in a general practice setting. Int J Prosthodont. 2004;17:302–306. [PubMed] [Google Scholar]
- 5.Cubas GB, Habekost L, Camacho GB, Pereira-Cenci T. Fracture resistance of premolars restored with inlay and onlay ceramic restorations and luted with two different agents. J Prosthodont Res. 2011;55:53–59. doi: 10.1016/j.jpor.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Kantardzić I, Vasiljević D, Blazić L, Luzanin O. Influence of cavity design preparation on stress values in maxillary premolar: a finite element analysis. Croat Med J. 2012;53:568–576. doi: 10.3325/cmj.2012.53.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christensen GJ. The coming demise of the cast gold restoration? J Am Dent Assoc. 1996;127:1233–1236. doi: 10.14219/jada.archive.1996.0417. [DOI] [PubMed] [Google Scholar]
- 8.Costa A, Xavier T, Noritomi P, Saavedra G, Borges A. The influence of elastic modulus of inlay materials on stress distribution and fracture of premolars. Oper Dent. 2014;39:E160–E170. doi: 10.2341/13-092-L. [DOI] [PubMed] [Google Scholar]
- 9.Mondelli J, Steagall L, Ishikiriama A, de Lima Navarro MF, Soares FB. Fracture strength of human teeth with cavity preparations. J Prosthet Dent. 1980;43:419–422. doi: 10.1016/0022-3913(80)90213-9. [DOI] [PubMed] [Google Scholar]
- 10.Dejak B, Mlotkowski A, Romanowicz M. Strength estimation of different designs of ceramic inlays and onlays in molars based on the Tsai-Wu failure criterion. J Prosthet Dent. 2007;98:89–100. doi: 10.1016/S0022-3913(07)60042-0. [DOI] [PubMed] [Google Scholar]
- 11.Yamanel K, Caglar A, Gülsahi K, Ozden UA. Effects of different ceramic and composite materials on stress distribution in inlay and onlay cavities: 3-D finite element analysis. Dent Mater J. 2009;28:661–670. doi: 10.4012/dmj.28.661. [DOI] [PubMed] [Google Scholar]
- 12.Jiang W, Bo H, Yongchun G, LongXing N. Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: a three-dimensional finite element analysis. J Prosthet Dent. 2010;103:6–12. doi: 10.1016/S0022-3913(09)60206-7. [DOI] [PubMed] [Google Scholar]
- 13.Zarone F, Sorrentino R, Apicella D, Valentino B, Ferrari M, Aversa R, Apicella A. Evaluation of the biomechanical behavior of maxillary central incisors restored by means of endocrowns compared to a natural tooth: a 3D static linear finite elements analysis. Dent Mater. 2006;22:1035–1044. doi: 10.1016/j.dental.2005.11.034. [DOI] [PubMed] [Google Scholar]
- 14.Ereifej N, Rodrigues FP, Silikas N, Watts DC. Experimental and FE shear-bonding strength at core/veneer interfaces in bilayered ceramics. Dent Mater. 2011;27:590–597. doi: 10.1016/j.dental.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Moon SY, Lim YJ, Kim MJ, Kwon HB. Three-dimensional finite element analysis of platform switched implant. J Adv Prosthodont. 2017;9:31–37. doi: 10.4047/jap.2017.9.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Song HY, Huh YH, Park CJ, Cho LR. A two-short-implantsupported molar restoration in atrophic posterior maxilla: A finite element analysis. J Adv Prosthodont. 2016;8:304–312. doi: 10.4047/jap.2016.8.4.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ausiello P, Franciosa P, Martorelli M, Watts DC. Numerical fatigue 3D-FE modeling of indirect composite-restored posterior teeth. Dent Mater. 2011;27:423–430. doi: 10.1016/j.dental.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 18.St-Georges AJ, Sturdevant JR, Swift EJ, Jr, Thompson JY. Fracture resistance of prepared teeth restored with bonded inlay restorations. J Prosthet Dent. 2003;89:551–557. doi: 10.1016/s0022-3913(03)00173-2. [DOI] [PubMed] [Google Scholar]
- 19.Cohen S, Berman LH, Blanco L, Bakland L, Kim JS. A demographic analysis of vertical root fractures. J Endod. 2006;32:1160–1163. doi: 10.1016/j.joen.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Thompson MC, Thompson KM, Swain M. The all-ceramic, inlay supported fixed partial denture. Part 1. Ceramic inlay preparation design: a literature review. Aust Dent J. 2010;55:120–127. doi: 10.1111/j.1834-7819.2010.01214.x. [DOI] [PubMed] [Google Scholar]
- 21.Frankenberger R, Taschner M, Garcia-Godoy F, Petschelt A, Krämer N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J Adhes Dent. 2008;10:393–398. [PubMed] [Google Scholar]
- 22.Tang CB, Liul SY, Zhou GX, Yu JH, Zhang GD, Bao YD, Wang QJ. Nonlinear finite element analysis of three implantabutment interface designs. Int J Oral Sci. 2012;4:101–108. doi: 10.1038/ijos.2012.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Molin MK, Karlsson SL. A randomized 5-year clinical evaluation of 3 ceramic inlay systems. Int J Prosthodont. 2000;13:194–200. [PubMed] [Google Scholar]