Abstract
Optimal use of goal-setting strategies in self-management efforts with high-risk individuals with asthma is not well understood. This study aimed to describe factors associated with goal attainment in an asthma self-management intervention for African American women with asthma and determine whether goal attainment methods proved beneficial to goal achievement and improved asthma outcomes. Data came from 212 African American women in the intervention arm of a randomized clinical trial evaluating a telephone-based asthma self-management program. Telephone interview data were collected to assess goals and goal attainment methods identified, asthma symptoms, asthma control, and asthma-related quality of life at baseline and 2-year follow-up. Generalized estimating equations were used to assess the long-term impact of goal setting and goal attainment methods on outcomes. The average age of the sample was 42.1 years (SD = 14.8). Factors associated with goal attainment included higher education (p < .01) and fewer depressive symptoms (p < .01). Using a goal attainment method also resulted in more goals being achieved over the course of the intervention (Estimate [SE] = 1.25 [0.18]; p < .001) when adjusted for clinical and demographic factors. Use of and types of goal attainment methods and goals were not found to significantly affect asthma control, quality of life, or frequency of nighttime asthma symptoms at follow-up. Using a method to achieve goals led to greater goal attainment. Goal attainment alone did not translate into improved asthma outcomes in our study sample. Further studies are warranted to assess the challenges of self-management in chronic disease patients with complex health needs and how goal setting and goal attainment methods can be strategically integrated into self-management efforts to improve health endpoints.
Keywords: asthma, behavior change, goals, intervention, outcomes, self-management
Asthma is a serious health and economic concern in the United States, affecting 8% of adults, and responsible for a large proportion of health care utilization, especially among women and communities of color (Centers for Disease Control and Prevention, 2011). Asthma self-management interventions are an important resource for developing effective disease management skills between office visits and for the prevention of frequent asthma symptoms and exacerbations (National Asthma Education and Prevention Program, 2007). Clinical guidelines for the successful management of asthma include increased patient involvement in self-education programs to improve asthma management techniques (National Asthma Education and Prevention Program, 2007). Systematic reviews have consistently shown that self-management programs can improve asthma outcomes, including improved quality of life and reduced urgent health care utilization (Denford, Taylor, Campbell, & Greaves, 2014; Press et al., 2012).
Self-management interventions differ greatly in their strategies to increase participants’ knowledge and self-care efforts (Denford et al., 2014; Newman, Steed, & Mulligan, 2004). Goal setting is one method that has been incorporated into many chronic disease self-management interventions (Locke & Latham, 2012). Goal setting works to increase behavior by enhancing the direction, self-regulation (use of tactics), and persistence of task-directed effort (Locke & Latham, 2012). In general, goal setting is thought to result in higher performance for prolonged periods of time in behaviors of interest (Latham & Locke, 1991; Locke & Latham, 1990). In controlled trials, collaborative goal setting with a coach or professional has been shown to improve total cholesterol, blood pressure, body mass index, physical activity levels, and smoking rates among cardiac patients (Butler, Furber, Phongsavan, Mark, & Bauman, 2009; Redfern, Briffa, Ellis, & Freedman, 2008), and glycemic control, blood pressure, low-density lipoprotein levels, physical activity levels, and fruit and vegetable intake among diabetes patients (Estabrooks et al., 2005; West, Lagua, Trief, Izquierdo, & Weinstock, 2010). Future research to inform the effective practice of goal setting suggests further investigations of which audiences and health behaviors are best suited for goal setting interventions and expanding our understanding of key moderators of goal attainment (Locke & Latham, 2012).
We could only locate one study that examined goal specificity and goal achievement with relation to asthma outcomes (Smith et al., 2013). In an Australian community pharmacy setting with pharmacists and patients developing collaborative goals, goal specificity was found to be strongly related to the achievement of goals and asthma control (Smith et al., 2013). In practice, some studies have found that methods of goal setting paired with clinician collaboration have improved asthma-related strategies of care during scheduled physician visits (monitoring peak flow, writing asthma action plan, and collaborative goal setting; Mangione-Smith et al., 2005; Schonlau et al., 2005). Although collaborative goal setting has been studied extensively, its utility in asthma self-management interventions across diverse populations is less well known. We could not locate any studies that have examined dispositional factors (via demographic and potential clinical characteristics) that may lead to goal attainment, and the use and type of actual strategies enacted (e.g., method of achieving goal) as a potential moderator to achieve goals and health outcomes. Such information would better inform for whom goal setting is most effective, and how and where other behavioral strategies may need to be considered for improving self-management in the context of asthma.
African American women with asthma provide a unique population to examine goal setting, goal attainment methods, and relationships to outcomes in a high-risk population. Women have a higher asthma prevalence than men, and the highest asthma burden is evident among African American women compared with all other subgroups (Centers for Disease Control and Prevention, 2012). They experience more hospitalizations and emergency department visits compared with other subgroups (Centers for Disease Control and Prevention, 2012). African American women also face the greatest challenge with self-management and are more likely to perceive treatment costs as a barrier to obtaining the resources they need to effectively self-manage their asthma (Centers for Disease Control and Prevention, 2012).
Further investigation of the use of goal setting methods in asthma self-management interventions may better equip patients and health care providers to use more specified strategies that lead to improvements in outcomes including asthma control and urgent health care utilization. The purpose of this study was to (a) describe demographic and clinical factors associated with goal attainment in an asthma self-management intervention within a high-risk group, particularly African American women; (b) determine whether utilizing a particular method was beneficial in goal attainment; and (c) examine the relationship between the types of goals set and methods used to achieve goals and asthma outcomes. We explored these questions from the evaluation of a telephone counseling asthma self-management intervention that incorporated collaborative goal setting.
Method
Data Source and Sample
This study used data from 212 African American women in the intervention arm of a randomized control trial evaluating a telephone-based asthma self-management program that utilized goal setting as part of its intervention approach. Details of the trial are described elsewhere (Janevic et al., 2012). The program used a highly tailored telephone counseling approach to address both specific cultural factors affecting asthma and female sex and gender factors on asthma control, evaluated over a 2-year period. The intervention is based on principles of self-regulation in chronic disease management (Clark, Gong, & Kaciroti, 2014), which required participants to identify a problem, observe their behaviors, set an asthma management goal, identify steps to achieve their goal, track their progress, and identify appropriate rewards. Participants completed five sessions via telephone communication with a health educator over the course of 3 months. The first five sessions were conducted approximately 2 weeks apart. A final sixth session (“booster session”) was conducted 6 months after Session 5. Previous trials utilizing a similar intervention approach have shown that participants become self-regulating in their chronic disease management over the course of this Time Frame 5 contact sessions (Clark et al., 2009). All study procedures were approved by an institutional review board (IRB Study HUM00033784).
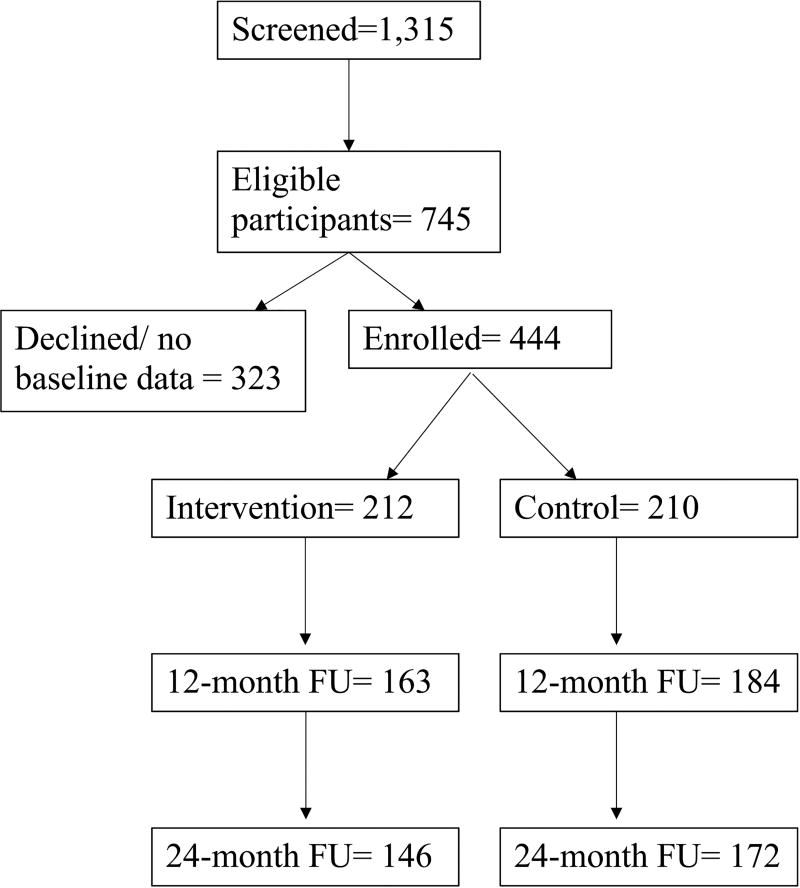
Primary recruitment took place through the university health system. Eligible participants: (a) self-identified as African American, (b) were 18 years or older, (c) had telephone access, (d) were not pregnant, and (e) were listed on the asthma patient registry, within the registry of Blue Cross Blue Shield, or cared for by health system provider. Figure 1 shows the randomization diagram. All participants provided written informed consent for participation.
Figure 1.
Participant flow diagram.
Measures
Data related to goals and methods used to achieve goals were collected by the health educators on standardized forms during telephone counseling sessions. Clinical, demographic, and outcome data were collected through surveys via standardized telephone interviews by trained interviewers at three time points: baseline and 12 and 24 months postbaseline.
Primary outcomes included goal attainment, asthma control, quality of life, and frequency of nighttime asthma symptoms. Independent variables included demographic and clinical variables, methods used to achieve goals, and goal type.
Goal and Goal Attainment Methods
Throughout the intervention, participants identified one short-term goal in Sessions 3 and 4, followed by one long-term goal in Session 5 with the guidance of a trained, health educator. Goal attainment strategies perceived as most helpful in goal attainment were identified retroactively during Session 6. In this final session, participants were also queried whether they applied their goal attainment method to other issues in their life, whether they believed the goal attainment method may have utility in managing other chronic conditions, and if so, in what ways.
Goal Achievement
In the final session of the intervention, participants were asked if they met the final goal that they set (yes/no).
Asthma Control
Asthma control was measured using the five-item, validated Asthma Control Test (Schatz et al., 2006).
Asthma-Related Quality of Life
The validated, 15-item Mini Asthma Quality of Life questionnaire assessed activity limitations, symptom frequency and intensity, and emotional functioning to provide an asthma-related quality of life score (Juniper, Guyatt, Cox, Ferrie, & King, 1999). Higher scores indicated a higher quality of life.
Symptom Frequency
Participants were asked the average nights over the past month they experienced asthma symptoms.
Demographic and clinical data were also collected including age, educational attainment, household income, marital status, insurance type, social support, asthma-related financial burden, and employment status. Clinical variables included asthma control, frequency of symptoms, quality of life, social support ratings, specialty of care, number of chronic conditions, medication type and number, and a depression score reflecting depressive symptoms measured on the CES-D 8 (Radloff, 1977).
Analysis
A sample size calculation was done at the design stage to determine 420 participants needed at baseline (210 women in each treatment arms) using the primary study outcomes of emergency department visits and hospitalizations in a period of 12 months. This calculation took the issue of missing data into account at a 30% attrition rate over 24 months and a loss of five women per group due to pregnancy. This sample size would allow testing of other study outcomes with a similar or higher level of confidence.
A total of 1,315 women were initially approached. Of those, 843 women were successfully reached via telephone and mail, and a total of 444 (53%) women consented to participate. At the end of recruitment, 422 of those who consented to participate provided baseline data and were subsequently randomized to intervention and control arms of the trial. The analysis of this study comprised data collected at three time points from the 212 women randomized to the intervention arm of the study (76% retention rate).
Goal setting data were numerically coded into categories. All short-term and long-term goals attained were summed to calculate a variable representing the total number of goals achieved over the course of the intervention. Asthma control scores were summed and classified into three categories: well controlled, not well controlled, and poorly controlled based on the National Asthma Education Prevention Program (NAEPP) guidelines and analyzed as a continuous variable as an outcome in regression models. Self-reported responses of symptom frequency were classified based on NAEPP guidelines (National Asthma Education and Prevention Program, 2007).
Means and frequencies were computed for all categorical clinical and demographic variables and to describe the goal setting and goal attainment methods used by participants in the intervention. Frequencies for the short-term and long-term goal themes sum to numbers larger than the number of women in the intervention arm of this study for several reasons. First, participants often set more than one long-term or short-term goal at each goal setting session. Second, over the course of the intervention, participants made two separate short-term goals. For analysis purposes, goal themes for these two separate short-term goal setting sessions were collapsed into one category.
Student’s t tests for continuous variables and contingency tables with chi-square and Fisher’s exact tests for categorical variables were used to examine differences in demographic and clinical factors among women who attained their long-term goal compared with women who did not.
Multiple variable linear regression analysis was also used to examine whether the use of a goal attainment method was predictive of the number of goals achieved over the course of the intervention. Models were adjusted for age, social support, employment status, educational attainment, depressive symptoms, and frequency of asthma symptoms.
To examine whether using a goal attainment method resulted in greater improvement in outcomes at 2-year follow-up among intervention women, mixed model regression analyses were used for continuous asthma outcomes (asthma control, asthma-related quality of life), and a generalized estimating equation (GEE) assuming a cumulative logit model was used for categorical outcomes (frequency of nighttime asthma symptoms). Models were adjusted for age, education, number of chronic conditions, depressive symptoms, and intervention completion.
Last, to examine which goal and goal attainment methods identified by women in the intervention resulted in greater improvements in outcomes at 2-year follow-up, mixed model regression analyses were used for continuous asthma outcomes (asthma control, asthma-related quality of life), and GEE assuming a cumulative logit model was used for categorical outcomes (frequency of nighttime asthma symptoms). Since several factors were found to be associated with the chance of dropout, as well as the presence of intermittent missing data, the assumption of data missing at random was used in the analysis. The method of inverse probability weighting was adopted to incorporate the chance of missingness in all GEE analyses. Goal types with frequencies greater than or equal to 10% were included in the mixed models. Models were adjusted for age, education, number of chronic conditions, depressive symptoms, and intervention completion. An interaction term of each goal type or goal attainment method by time was included in models to examine the effect of goal type and goal attainment method on asthma outcomes over time. Alpha values of .05 or less were considered statistically significant for all analyses. All analyses were computed in SAS (Version 9.4).
Results
Sample
The average age was 42.1 years (SD = 14.8). Of the 212 women who participated in the intervention, 20% (n = 42) obtained a high school diploma or equivalent, 51% (n = 107) had some college, 68% (n = 144) were employed. Forty-seven percent (n = 100) reported having private insurance. More than 67% (n = 143) of the women reported being head of their household, only 29% (n = 61) were married, and they reported a moderate level of social support (3.0 [SD = 1.1]). Fifty-three percent (n = 112) of participants perceived financial burden with their asthma care, which is undoubtedly related to the low annual household income reported by the women.
Clinically, 31% (n = 67) of participants were classified as having well-controlled asthma. Thirty-five percent (n = 74) of women saw both a primary care physician and an asthma specialist and 58% (n = 122) of participants saw only a primary care physician. On average, participants were on 2.7 (SD = 1.4) medications and reported 3.95 (SD = 2.69) other chronic conditions in addition to their asthma. Average quality of life rating was moderate (4.7 [SD = 1.3]), and the mean depression score was 7.47 (SD = 5.53), suggesting a clinically significant level of depressive symptoms that would suggest psychological distress (Huba, Melchior, The Measurement Group, & HRSA/HAB’s SPNS Cooperative Agreement Steering Committee, 1995). The mean body mass index of participants was 33.4 (SD = 8.2).
Demographic and clinical characteristics associated with goal attainment included education (p < .01) and depressive symptoms (p < .01), with those with higher education and fewer depressive symptoms more likely to achieve goals (Table 1).
Table 1.
Demographic and Clinical Characteristics Among Women Randomized to the Intervention Arm Who Did and Did Not Attain Goal Set (N = 212).
| Characteristics | Total sample % (N = 212) |
Goal attained % (N = 110) |
Goal not attained % (N = 102) |
χ2/t test statistica (p value) |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, M (SD) | 42 (14.8) | 43.25 (14.26) | 40.68 (15.25) | t = 1.27 |
| BMI, M (SD) | 33 (8.2) | 33.61 (8.36) | 33.08 (7.99) | t = 0.46 |
| Annual household income | — | |||
| <$20,000 | 100 (199) | 100 (107) | 100 (92) | |
| $20,001–$40,000 | 0 | 0 | 0 | |
| $40,001–$60,000 | 0 | 0 | 0 | |
| >$60,001 | 0 | 0 | 0 | |
| Educational attainment | χ2(2) = 9.46** | |||
| High school/GED or less | 20 (42) | 12 (13) | 29 (29) | |
| Some college or vocational school | 51 (107) | 56 (62) | 44 (45) | |
| College or above | 29 (62) | 32 (35) | 27 (27) | |
| Employed (% yes) | 68 (144) | 68 (75) | 68 (69) | χ2(1) = 0 |
| Health insurance | χ2(3) = 3.67a | |||
| Private | 47 (100) | 52 (57) | 42 (43) | |
| Medicare | 18 (38) | 21 (23) | 17 (17) | |
| Medicaid | 25 (52) | 20 (22) | 29 (30) | |
| Other | 6 (11) | 5 (5) | 4 (4) | |
| No insurance | 4 (8) | 2 (2) | 6 (6) | |
| Marital status (% married) | 29 (61) | 32 (35) | 26 (26) | χ2(1) = 0.94 |
| Head of household (% yes) | 67 (143) | 69 (76) | 66 (67) | χ2(1) = 0.18 |
| Perceived financial burden (% yes) | 53 (112) | 53 (58) | 54 (54) | χ2(1) = 0.03 |
| Level of social support, M (SD) | 3 (1.1) | 2.7 (1.0) | 2.7 (1.1) | t = 0.19 |
| Clinical characteristics | ||||
| Asthma-related quality of life, M (SE) | 4.7 (1.3) | 5.0 (1.29) | 4.7 (1.26) | t = 1.64 |
| Frequency of asthma symptoms | χ2(2) = 4.02 | |||
| <2 days per week | 63 (133) | 69 (76) | 56 (57) | |
| ≥3 days per week | 27 (57) | 22 (24) | 32 (33) | |
| Throughout the day | 10 (22) | 9 (10) | 12 (12) | |
| Specialty of care | χ2(1) = 1.13b | |||
| Primary care and specialist | 35 (74) | 38 (41) | 33 (33) | |
| Primary care only | 58 (122) | 53 (58) | 63 (64) | |
| Specialist only | 4 (9) | 5 (6) | 3 (3) | |
| No doctor | 3 (5) | 4 (4) | 1 (1) | |
| Asthma control | χ2(2) = 0.02 | |||
| Well controlled | 31 (67) | 32 (35) | 32 (32) | |
| Not well controlled | 31 (65) | 31 (34) | 30 (31) | |
| Very poorly controlled | 38 (80) | 37 (41) | 38 (39) | |
| Asthma medications | χ2(1) = 0.11c | |||
| Controller and rescue | 69 (146) | 72 (79) | 66 (67) | |
| Controller only | 2 (4) | 1 (1) | 3 (3) | |
| Rescue only | 20 (43) | 20 (22) | 21 (21) | |
| Other | 10 (19) | 5 (5) | 11 (11) | |
| Number of medications, M (SD) | 2.7 (1.4) | 2.7 (1.42) | 2.8 (1.39) | t = 0.38 |
| Number of chronic conditions, M (SD) | 3.95 (2.69) | 4.10 (2.86) | 3.79 (2.51) | t = 0.38 |
| χ2(3) = 3.74 | ||||
| Asthma only | 4 (8) | 5 (6) | 2 (2) | |
| 1 other condition | 15 (32) | 12 (13) | 19 (19) | |
| 2 other conditions | 16 (35) | 16 (17) | 17 (18) | |
| 3+ other conditions | 65 (137) | 67 (74) | 62 (63) | |
| Depressive symptoms, M (SD) | 7.47 (5.53) | 6.5 (5.28) | 8.51 (5.63) | t = 2.64** |
Note. BMI = body mass index; SE = standard error; SD = standard deviation; M = mean.
Due to low cell count, chi-square test ran for the following categories: private, Medicare, and Medicaid.
Due to low cell count, chi-square test ran for the following categories: primary care and specialist, primary care only.
Due to low cell count, chi-square test ran for the following categories: controller and rescue and rescue only.
Level of significance reported as (p value): *p < .05,
p < .01,
p < .001.
Goal and Steps Identified to Manage Asthma
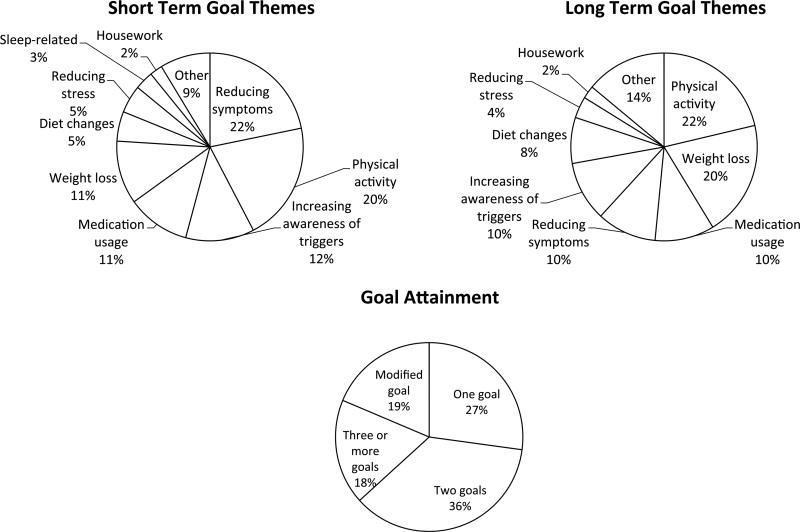
When considering the long-term goals among the 212 participants, 22% set a goal to increase physical activity, 20% set a weight loss goal, and 10% set a goal to either increase awareness of asthma triggers, to reduce symptoms while performing other activities, or to take medication regularly. A similar breakdown was evident for short-term goals. Twenty-seven percent of participants achieved one goal that was set, 36% achieved two goals, and 18% achieved three or more goals (Figure 2).
Figure 2.
Frequencies of long-term and short-term goal types identified and achieved by women randomized to the intervention arm (N = 212).
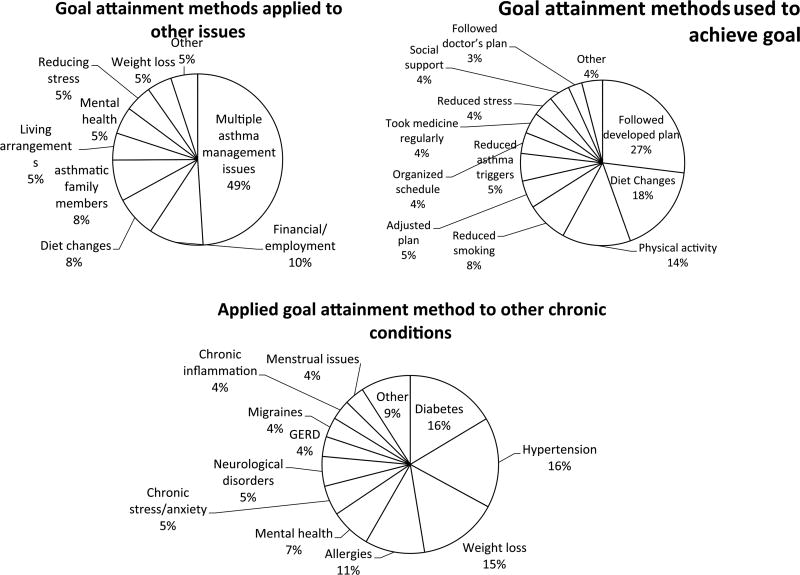
Sixty percent of participants used a goal attainment method to achieve their goals. Twenty-seven percent reported following the plan developed with their health educator, 8.1% reported reducing smoking behavior, 14% reported increasing physical activity, and 18% reported making appropriate dietary changes. Sixty-nine percent applied their goal attainment method to other issues, including multiple asthma management issues (49%), financial and employment (10%), and other dietary changes (8%). Application of the goal attainment methods to other chronic conditions was reported by 89% of the participants, and was most frequently applied to the management of diabetes (16%), hypertension (16%), and weight loss (15%; Figure 3).
Figure 3.
Use of goal attainment methods identified by women randomized to the intervention arm (N = 212).
All individuals who reached their goal used a goal attainment method. Method utilization also resulted in more goals being achieved over the course of the intervention (Estimate [SE] = 1.25 [0.18]; p < .001) when adjusted for age, social support, employment status, educational attainment, depressive symptoms, and frequency of asthma symptoms.
Asthma Outcomes
After adjusting for age, education, number of chronic conditions, depressive symptoms, and intervention completion, use of a goal attainment method was not found to significantly affect asthma control, quality of life, or frequency of nighttime asthma symptoms at follow-up (Table 2).
Table 2.
Adjusted Linear Mixed Models of Goal Attainment Methods Associated With Asthma Control, Asthma-Related Quality of Life, and Nighttime Symptom Frequency at 12- and 24-Month Follow-Up Among Women Randomized to the Intervention (N = 212).a
| Factor | Asthma control | Asthma-related quality of life | Nighttime symptom frequency |
|---|---|---|---|
| Used goal attainment method | |||
| Estimate | 0.14 | −0.05 | −0.63 |
| 95% confidence intervalb | [−1.70, 1.98] | [−0.52, 0.41] | [−1.75, 0.47] |
| Time * Used goal attainment method | |||
| p value | .60 | .75 | .85 |
Models adjusted for age, education, number of chronic conditions, depressive symptoms, intervention completion.
Values in brackets are 95% confidence intervals.
Level of significance reported as (p value): *p < .05,
p < .01,
p < .001.
After adjusting for age, education, number of chronic conditions, depressive symptoms, and intervention completion, no particular goal (related or unrelated to asthma management) or goal attainment method was found to significantly affect asthma control, quality of life, or frequency of night-time asthma symptoms at follow-up (Table 3).
Table 3.
Adjusted Linear Mixed Models of Goal-Type and Goal Attainment Method Associated With Asthma Control, Quality of Life, and Nighttime Symptom Frequency at 12- and 24-Month Follow-Up Among Women Randomized to Intervention (N = 212).a
| Factor | Asthma control | Asthma-related quality of life | Nighttime symptom frequency |
|---|---|---|---|
| Goal type | |||
| Weight loss (yes/no) | |||
| Estimate | −0.59 | −0.02 | −0.22 |
| 95% CIb | [−2.33, 1.14] | [−0.451, 0.48] | [−1.32, 0.88] |
| Time * Weight loss | |||
| p value | .27 | .35 | .86 |
| Exercise (yes/no) | |||
| Estimate | −0.45 | −0.05 | −0.20 |
| 95% CI | [−2.1, 1.22] | [−0.49, 0.38] | [−1.16, 0.76] |
| Time * Exercise | |||
| p value | .18 | .09 | .17 |
| Increasing awareness of triggers (yes/no) | |||
| Estimate | 1.05 | 0.35 | −0.14 |
| 95% CI | [−1.27, 3.38] | [−0.26, 0.96] | [−1.45, 1.16] |
| Time * Increasing awareness of triggers | |||
| p value | .16 | .18 | .53 |
| Reducing symptoms (yes/no) | |||
| Estimate | −0.75 | −0.04 | 0.67 |
| 95% CI | [−3.08, 1.57] | [−0.65, 0.57] | [−0.73, 2.08] |
| Time * Reducing symptoms | |||
| p value | .70 | .67 | .17 |
| Taking medication as prescribed (yes/no) | |||
| Estimate | 1.47 | 0.42 | 1.18 |
| 95% CI | [−1.11, 4.06] | [−0.25, 1.11] | [−1.10, 3.46] |
| Time * Taking medication as prescribed | |||
| p value | .09 | .28 | .47 |
| Goal attainment method | |||
| Followed plan (yes/no) | |||
| Estimate | 0.63 | 0.13 | −0.22 |
| 95% CI | [−1.37, 2.63] | [−0.38, 0.66] | [−1.38, 0.94] |
| Time * Followed plan | |||
| p value | .63 | .63 | .64 |
| Dieting (yes/no) | |||
| Estimate | −0.27 | −0.14 | −0.29 |
| 95% CI | [−2.59, 2.04] | [−0.74, 0.46] | [−1.53, 0.94] |
| Time * Dieting | |||
| p value | .82 | .33 | .89 |
| Increasing physical activity (yes/no) | |||
| Estimate | 1.29 | −0.08 | 0.01 |
| 95% CI | [−1.30, 3.89] | [−0.76, 0.60] | [−1.60, 1.64] |
| Time * Increasing physical activity | |||
| p value | .15 | .15 | .34 |
| Reducing smoking (yes/no) | |||
| Estimate | 2.30 | 0.64 | 0.72 |
| 95% CI | [−0.97, 5.58] | [−0.22, 1.50] | [−1.24, 2.69] |
| Time * Reducing smoking | |||
| p value | .35 | .56 | .97 |
Note. CI = confidence interval.
Models adjusted for age, education, number of chronic conditions, depressive symptoms, intervention completion.
Values in brackets are 95% confidence intervals.
Level of significance reported as (p value): *p < .05,
p < .01,
p < .001.
Discussion
This is the first study we are aware of to examine the utility of goal setting in a high-risk population with asthma, specifically African American women, and whether certain types of goals and goal attainment methods led to goal achievement and improved outcomes. We found that those with more education and fewer depressive symptoms were more likely to achieve goals, and all individuals who utilized a method to reach their goal actually achieved their goal. Utilizing a goal attainment method also led to more goals being achieved, regardless of education and the presence of depressive symptoms. Given the extensive use of goal setting efforts in self-management education, the findings from this study suggest that their strategic use provides important mechanisms for enacting behavior change.
Contrary to our expectation, no associations were observed between self-identified goal types and goal attainment methods and asthma control, quality of life, and frequency of asthma symptoms at follow-up; in other words, successful goal attainment did not translate into improved outcomes. Several factors may explain these findings. First, goals identified in the intervention by participants tended to be general and, in some cases, less obvious to the management of asthma. Other work has shown that goal specificity is a stronger predictor of asthma control than goal achievement, whereby specific goals were positively associated with better asthma control (Smith et al., 2013). Second, goal attainment methods were queried retroactively at later sessions of the intervention; thus, their active formation was not part of the collaborative process between the participant and health educator when goals were set. This may have resulted in potential misalignment between goal set and methods used, or missed opportunities to provide more structured methods. It may be that longer follow-up time is needed to show changes in outcomes, or there may be other mechanisms that demonstrate the association between the goal set or goal attainment method used and outcomes rather than the goal or method itself.
The null findings may be attributed, at least in part, to the high morbidity evident within the study population. While the sample population was identified as one with asthma, it turned out that this population is potentially better characterized by one with multiple chronic conditions (MCCs). More than half of adults with asthma manage MCCs (Patel, Janevic, Heeringa, Baptist, & Clark, 2013). On average, women in the sample were self-managing approximately four additional chronic conditions with asthma. Other qualitative work suggests the presence of comorbid conditions in African American women negatively affects perception of the importance of asthma self-management activities (Janevic, Ellis, Sanders, Nelson, & Clark, 2014). Other work in the goal setting literature has suggested that goal setting may be undesirable for the manger performing complex decision making unless accompanied by some method of task strategy shaping and development (Locke & Latham, 2012).
The majority of goals set by women in the intervention were related to weight loss and physical activity. In addition, the majority of women applied their goal attainment methods to both other areas of their life (e.g., financial management) and other chronic conditions they were managing such as diabetes and hypertension. Common concerns with self-management that individuals with MCCs identify are often linked to functional challenges and are not disease specific (Liddy, Blazkho, & Mill, 2014). Goal setting has been shown to be a feasible tool to facilitate patient-centered care among individuals with MCCs (Toto, Skidmore, Terhorst, Rosen, & Weiner, 2015) and may have implications for self-management support as a common unifying framework for the growing population with MCCs. How goal setting can be strategically incorporated into self-management support with MCCs to improve outcomes for the case condition and other conditions is a ripe area for further investigation.
Several limitations were evident in this study. Data were self-reported; therefore, it is probable that some responses do not reflect actual circumstance for variables where comparison data were not available. This was a secondary analysis of data from an evaluation of a telephone-based self-management intervention. As a result, the data used to analyze the questions of interest in this study were limited to what was available and how it was collected, although intent-to-treat analyses were employed. Participants developed goals in collaboration with trained health educators, and possible turnover of study personnel or fidelity of intervention delivery may have affected the types and specificity of the goals set. As previously mentioned, goal attainment methods were queried retroactively at later sessions of the intervention and was not a more prominent component of the original intervention. Lack of face-to-face contact could potentially have some influence on goal achievement, as other work has shown that some individuals benefit more from in-person intervention (Clark et al., 2009). Finally, as this study population consisted of low-income African American women in Southeast Michigan with high comorbidity, findings are not generalizable to all African American women with asthma or all individuals with asthma.
This study also has several strengths. First, it describes characteristics that are more conducive to goal attainment in an asthma self-management intervention targeted to a population at high risk for poor asthma outcomes, specifically African American women. Second, this study further highlights that using goal attainment methods can facilitate greater attainment of goals. Last, this study revealed that effective goal setting strategies in self-management interventions require further inquiry when the population has complex health needs beyond a single disease.
These findings have several implications for future practice and research. Our findings suggest that health educators and clinicians may consider more targeted and specified efforts when incorporating goal setting into self-management support for individuals with asthma with complex health care needs. Goal attainment methods may be critical and beneficial to establish when establishing goals given their high correlation with goal attainment. Future research may consider prospective study designs to further explore what goals and methods are most helpful to complex patients. Future research might also explore the mechanisms through which goal achievement and goal attainment methods can lead to improved health outcomes in order to further facilitate targeted efforts at using these strategies in behavioral interventions and clinical practice.
In conclusion, we found that using goal attainment methods led to greater goal attainment. Goal attainment alone did not translate into improved asthma outcomes in our study sample. Further studies are warranted to assess the complex challenges of self-management in chronic disease patients, especially those with MCCs and how goal setting and particular goal attainment methods can be strategically integrated into self-management efforts to improve health endpoints.
Acknowledgments
The authors would like to thank the study team and all the participants for their contributions to this work. This work is dedicated to the loving memory of Dr. Noreen M. Clark, Director of the Center for Managing Chronic Disease at the University of Michigan School of Public Health.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Lung Division of the National Heart, Lung, and Blood Institute of the National Institutes of Health (1R18HL094272 01).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Butler L, Furber S, Phongsavan P, Mark A, Bauman A. Effects of a pedometer-based intervention on physical activity levels after cardiac rehabilitation: A randomized controlled trial. Journal of Cardiopulmonary Rehabilitation and Prevention. 2009;29:105–114. doi: 10.1097/HCR.0b013e31819a01ff. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: Asthma prevalence, disease characteristics, and self-management education: United states, 2001–2009. Morbidity and Mortality Weekly Report. 2011;60:547–552. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Asthma’s impact on the nation. 2012 Retrieved from http://www.cdc.gov/asthma/impacts_nation/asthmafactsheet.pdf.
- Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Education & Behavior. 2014;41:499–508. doi: 10.1177/1090198114547701. [DOI] [PubMed] [Google Scholar]
- Clark NM, Janz NK, Dodge JA, Lin X, Trabert BL, Kaciroti N, Keteyian S. Heart disease management by women: Does intervention format matter? Health Education & Behavior. 2009;36:394–409. doi: 10.1177/1090198107309458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denford S, Taylor RS, Campbell JL, Greaves CJ. Effective behavior change techniques in asthma self-care interventions: Systematic review and meta-regression. Health Psychology. 2014;33:577–587. doi: 10.1037/a0033080. [DOI] [PubMed] [Google Scholar]
- Estabrooks PA, Nelson CC, Xu S, King D, Bayliss EA, Gaglio B, Glasgow RE. The frequency and behavioral outcomes of goal choices in the self-management of diabetes. Diabetes Educator. 2005;31:391–400. doi: 10.1177/0145721705276578. [DOI] [PubMed] [Google Scholar]
- Huba GJ, Melchior LA The Measurement Group, & HRSA/ HAB’s SPNS Cooperative Agreement Steering Committee. Module 26A: CES-D Form (Interview) Culver City, CA: Measurement Group; 1995. Retrieved from http://themeasurementgroup.com/ [Google Scholar]
- Janevic MR, Ellis KR, Sanders GM, Nelson BW, Clark NM. Self-management of multiple chronic conditions among African American women with asthma: A qualitative study. Journal of Asthma. 2014;51:243–252. doi: 10.3109/02770903.2013.860166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janevic MR, Sanders GM, Thomas LJ, Williams DM, Nelson B, Gilchrist E, Clark NM. Study protocol for women of color and asthma control: A randomized controlled trial of an asthma-management intervention for African American women. BMC Public Health. 2012;12:76. doi: 10.1186/1471-2458-12-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juniper EF, Guyatt GH, Cox FM, Ferrie PJ, King DR. Development and validation of the mini asthma quality of life questionnaire. European Respiratory Journal. 1999;14(1):32–38. doi: 10.1034/j.1399-3003.1999.14a08.x. [DOI] [PubMed] [Google Scholar]
- Latham GP, Locke EA. Self-regulation through goal-setting. Organizational Behavior and Human Decision. 1991;50:212–247. [Google Scholar]
- Liddy C, Blazkho V, Mill K. Challenges of self-management when living with multiple chronic conditions: Systematic review of the qualitative literature. Canadian Family Physician Medecin De Famille Canadien. 2014;60:1123–1133. [PMC free article] [PubMed] [Google Scholar]
- Locke EA, Latham GP. A theory of goal-setting and performance. Englewood Cliffs, NJ: Prentice-Hall; 1990. [Google Scholar]
- Locke EA, Latham GP. New developments in goal setting and task performance. London, England: Routledge; 2012. [Google Scholar]
- Mangione-Smith R, Schonlau M, Chan K, Keesey J, Rosen M, Louis T, Keeler E. Measuring the effectiveness of a collaborative for quality improvement in pediatric asthma care: Does implementing the chronic care model improve processes and outcomes of care? Ambulatory Pediatrics. 2005;5:75–82. doi: 10.1367/A04-106R.1. [DOI] [PubMed] [Google Scholar]
- National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the diagnosis and management of asthma. 2007 Retrieved from http://www.nhlbi.nih.gov/files/docs/guidelines/asthgdln.pdf.
- Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364:1523–1537. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- Patel MR, Janevic MR, Heeringa SG, Baptist AP, Clark NM. An examination of adverse asthma outcomes in U.S. adults with multiple morbidities. Annals of the American Thoracic Society. 2013;10:426–431. doi: 10.1513/AnnalsATS.201302-032OC. [DOI] [PubMed] [Google Scholar]
- Press VG, Pappalardo AA, Conwell WD, Pincavage AT, Prochaska MH, Arora VM. Interventions to improve outcomes for minority adults with asthma: A systematic review. Journal of General Internal Medicine. 2012;27:1001–1015. doi: 10.1007/s11606-012-2058-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Redfern J, Briffa T, Ellis E, Freedman SB. Patient-centered modular secondary prevention following acute coronary syndrome: A randomized controlled trial. Journal of Cardiopulmonary Rehabilitation and Prevention. 2008;28:107–115. doi: 10.1097/01.HCR.0000314204.86805.13. [DOI] [PubMed] [Google Scholar]
- Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, Jhingran P. Asthma control test: Reliability, validity, and responsiveness in patients not previously followed by asthma specialists. Journal of Allergy and Clinical Immunology. 2006;117:549–556. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Schonlau M, Mangione-Smith R, Chan KS, Keesey J, Rosen M, Louis TA, Keeler E. Evaluation of a quality improvement collaborative in asthma care: Does it improve processes and outcomes of care? Annals of Family Medicine. 2005;3:200–208. doi: 10.1370/afm.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L, Alles C, Lemay K, Reddel H, Saini B, Bosnic-Anticevich S, Armour C. The contribution of goal specificity to goal achievement in collaborative goal setting for the management of asthma. Research in Social & Administrative Pharmacy. 2013;9:918–929. doi: 10.1016/j.sapharm.2013.02.002. [DOI] [PubMed] [Google Scholar]
- Toto PE, Skidmore ER, Terhorst L, Rosen J, Weiner DK. Goal attainment scaling (GAS) in geriatric primary care: A feasibility study. Archives of Gerontology and Geriatrics. 2015;60(1):16–21. doi: 10.1016/j.archger.2014.10.022. [DOI] [PubMed] [Google Scholar]
- West SP, Lagua C, Trief PM, Izquierdo R, Weinstock RS. Goal setting using telemedicine in rural underserved older adults with diabetes: Experiences from the informatics for diabetes education and telemedicine project. Telemedicine Journal and e-Health. 2010;16:405–416. doi: 10.1089/tmj.2009.0136. [DOI] [PubMed] [Google Scholar]