Walled-off necrosis (WON) develops as a sequel to acute pancreatitis. Approximately 15% of patients with acute pancreatitis can experience WON. EUS-guided transmural drainage of WON has been a safe, efficacious, and widely used therapeutic modality in recent times. The lumen-apposing metal stent (LAMS) is a novel self-expanding covered metal stent designed for enteric drainage of large pseudocysts and necrosectomy of WON. Adverse events associated with LAMS placement include bleeding, infection, migration, and dislodgement during necrosectomy. Dislodgement of the LAMS can happen during the performance of necrosectomy despite its anchoring design. We present such a case of accidental LAMS migration that occurred during a necrosectomy procedure.
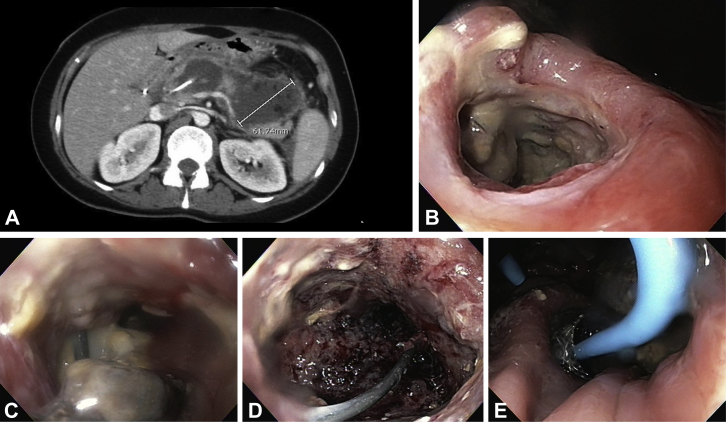
A 48-year-old woman presented with 1 day of epigastric pain, nausea, and vomiting. The initial CT of the abdomen revealed necrotizing pancreatitis involving 33% of the pancreas (Fig. 1A). An EGD was performed after 4 weeks for placement of a 15 mm × 10 mm LAMS under EUS guidance. A 7F × 5 cm double-pigtail stent was placed within the LAMS to maintain patency. Five days after the initial cystogastrostomy, an EGD was performed for necrosectomy. During the necrosectomy, the LAMS was dislodged accidentally (Fig. 1B). After the stent was dislodged, the cystogastrostomy site was dilated, and further necrosectomy was performed with ease because of the larger open cystogastrostomy site (Figs. 1C and D). The stent was removed, and the end of the stent was engaged with the snare and pulled into the therapeutic endoscope channel. Next, the stent was deployed under direct visualization with the distal end in the WON through the cystogastrostomy and the proximal end into the stomach (Video 1, available online at www.VideoGIE.org). We also placed a 10F × 5 cm double-pigtail stent through the LAMS to secure its position and prevent food impaction (Fig. 1E). This technique provides a cost-effective solution to accidental LAMS migration during necrosectomy. Removal of the LAMS to facilitate necrosectomy can be done routinely with replacement after the procedure if necessary.
Figure 1.
A, CT scan after 17 days of the acute event showing necrotizing pancreatitis with extensive parenchymal necrosis. B, Cystogastrostomy site showing dislodged lumen-apposing metal stent. C, Wall of walled-off necrosis showing necrotic tissue. D, Healthy granulation tissue around the wall of the walled-off necrosis site after necrosectomy. E, Redeployed lumen-apposing metal stent with double-pigtail stent through it to maintain its position and prevent food impacting.
The patient’s abdominal pain and sepsis improved a few days after necrosectomy with the redeployment of a LAMS. A repeated CT scan showed improvement of the necrosis and peripancreatic fluid collections. The patient’s symptoms resolved, and she was discharged without antibiotics.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Retrieval and redeployment of migrated lumen-apposing metal stent to facilitate endoscopic necrosectomy of walled-off necrosis.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Retrieval and redeployment of migrated lumen-apposing metal stent to facilitate endoscopic necrosectomy of walled-off necrosis.