Abstract
Chemotherapy is an important adjuvant therapy for epithelial ovarian cancer (EOC). The main cause of chemotherapy failure in EOC is paclitaxel resistance. The present study aimed to identify novel biomarkers to predict chemosensitivity to paclitaxel and improve our understanding of the molecular mechanisms underlying paclitaxel resistance in EOC. In the present study, the heterogeneity of EOC was evaluated by adenosine triphosphate-tumor chemosensitivity assay (ATP-TCA) in vitro. Fresh samples were collected from 54 EOC cases during cytoreductive surgery. Tumor cells were isolated, cultured, and tested for sensitivity to paclitaxel. Proteins that were differentially expressed between paclitaxel-resistant tissues and paclitaxel-sensitive tissues were identified via isobaric tags for relative and absolute quantitation (iTRAQ)-based proteomic analysis. Two upregulated proteins, plexin domain containing 2 (Plxdc2) and cytokeratin 7 (CK7), were selected to verify the iTRAQ method using western blot analysis in EOC tissues with different chemosensitivities (sensitive, weakly sensitive and resistant). There was notable heterogeneity of chemosensitivity in the EOC specimens. Highly to mildly-differentiated or early-stage (I/II) EOC specimens had decreased sensitivity to paclitaxel compared with specimens with low differentiation (P<0.05) or an advanced stage (III; P<0.05), respectively. A total of 496 significantly differentially expressed proteins, including 263 that were downregulated (P<0.05) and 233 that were upregulated (P<0.05) in paclitaxel-resistant tissues compared with paclitaxel-sensitive tissues, were identified using iTRAQ in combination with LC-MS/MS. The expression levels of two proteins associated with paclitaxel resistance, Plxdc2 and CK7, were further validated by western blotting, which revealed that they were upregulated in the paclitaxel-resistant tissues. The present study determined candidate proteins associated with paclitaxel resistance in EOC. Plxdc2 and CK7 may be potential makers for distinguishing patients with paclitaxel-resistant EOC from those with paclitaxel-sensitive EOC.
Keywords: ovarian cancer, paclitaxel resistance, plexin domain containing 2, cytokeratin 7, isobaric tags for relative and absolute quantitation
Introduction
Ovarian cancer is the most lethal gynecological malignancy in the world (1). Due to the limited number of specific symptoms, women usually only seek medical help once the disease is at an advanced stage, with distant metastases (2). Overall, 90% of ovarian cancer cases are epithelial ovarian cancer (EOC) (3). Standard therapy for advanced EOC involves a combination of cytoreductive surgery and platinum-based chemotherapy, with the combination of paclitaxel and platinum being the standard adjuvant chemotherapy regimen for EOC (4). Paclitaxel is an important agent for EOC treatment, and is an effective first-line therapy for advanced ovarian cancer. However, recurrence still affects the majority of patients a short period following chemotherapeutic intervention (5). The main cause for the failure of chemotherapy is chemoresistance of the tumor tissues, which adversely affects the prognosis of patients with ovarian cancer. Furthermore, patients with ovarian carcinoma may have variable responses to the standard chemotherapeutic regimen, even when they have the same histologic type. Heterogeneity of the tumor tissue, one of the primary features of malignancies, is thought to be the main factor causing this difference (6). With the incidence of paclitaxel resistance increasing, it is necessary to identify novel, specific biomarkers that predict chemosensitivity to paclitaxel to improve outcomes for patients with ovarian cancer (7,8).
The chemosensitivity test is an in vitro, predictive assay for used to assess cancer cell sensitivity to a range of chemotherapeutic agents. Adenosine triphosphate-tumor chemosensitivity assays (ATP-TCA) are sensitive assays that have been widely used to determine the drug sensitivity of solid tumors in the past few years (9). ATP-TCA measures the intracellular ATP levels of drug-exposed cells and untreated controls to assess tumor cell viability. This method has notable advantages for guiding the design of chemotherapy protocols and individualized treatments, and assessing novel chemotherapeutic drugs. Since its introduction, a number of studies have reported that ATP-TCA have a high sensitivity and a positive predictive value, and accurately predict the response to chemotherapy in ovarian cancer (10,11).
In the present study, ATP-TCA was used to assess the chemosensitivity of EOC to paclitaxel. Parameters determined by analyzing the correlation between the inhibition rate and paclitaxel doses were measured as follows: Inhibitory concentration (IC)90 and IC50, (90 or 50% growth inhibition in vitro, respectively), and sensitivity index (SI), which was calculated by summation of the percentage of tumor growth inhibition (TGI) at each concentration detected (12). SI >250 was suggested to be the optimal standard for predicting chemoresistance. Therefore, 250 were selected as the cut-off point for SI in the present study (13).
Paclitaxel is known to induce cytotoxicity by triggering apoptosis via regulation of the expression of apoptosis-associated proteins in the caspase-independent and caspase-dependent pathways, or by preventing tubulin depolymerization during the metaphase to anaphase transition of mitosis (14). However, paclitaxel resistance limits its use in the long-term management of EOC, and the molecular mechanisms underlying this resistance remain to be fully elucidated. Therefore, the identification of specific markers for ovarian cancer with paclitaxel resistance is a long-term goal of the medical community. The present study aimed to identify proteins associated with paclitaxel resistance in ovarian cancer, in order to investigate the molecular mechanisms underlying paclitaxel resistance and discover potential novel drug targets for paclitaxel-resistant ovarian cancer (15).
In the present study, two approaches for quantitative proteomic analysis were selected for identifying the differentially expressed proteins between paclitaxel-resistant and paclitaxel-sensitive groups of ovarian cancer tissues: iTRAQ analysis and two-dimensional electrophoresis coupled to liquid chromatography tandem mass spectrometry (LC-MS/MS). iTRAQ is a gel free mass spectrometry technique, applying isobaric amine specific tags to compare peptide intensities between samples, then inferring quantitative values for the corresponding proteins. LC-MS/MS is based on the differential two-dimensional gel electrophoresis pattern between protein samples and provides additional biological information, including molecular weight alterations or isoelectric point drift, based on which protein functions are implicated (16). The present study aimed to identify biomarkers, which were associated with paclitaxel-resistant ovarian cancer, providing information to aid our understanding of the underlying molecular mechanisms and to predict treatment responses to therapeutic agents. The ovarian cancer-specific proteins identified were further confirmed by western blot analysis (17).
Materials and methods
Ethics statement
The study protocol received approval from the Ethics Committee of the Beijing Shijitan Hospital, Capital Medical University (Beijing, China). Written, signed informed consent was obtained from all patients and their family members prior to surgery. All procedures were carried out in agreement with the Code of Ethics of the World Medical Association (Declaration of Helsinki, 1964; as revised in 2004).
Tumor samples
A total of 54 fresh specimens were obtained from patients with EOC who underwent staging surgery at the Beijing Shijitan Hospital, Beijing University People's Hospital (Beijing, China), People's Liberation Army General Hospital (Beijing, China) and Beijing Obstetrics and Gynecology Hospital (Beijing, China), between March 2013 and December 2014. Routine histopathology was conducted on formalin-fixed and paraffin-embedded samples, which were obtained from the same tissues, by at least two experienced gynecological pathologists (the Beijing Shijitan Hospital) in order to determine the malignancy and the stage of the tumor samples. Each fresh collected sample was divided into two fractions: One was prepared for ATP-TCA, and the other was stored at −80°C for subsequent tests. The ATP-TCA was conducted as a routine procedure immediately following surgery using residual primary tumor samples which were not required for histopathology. The sensitivity of viable ovarian cancer cells harvested from malignant tissues to paclitaxel (Corden Pharma Latina S.P.A., Sermoneta Italy) was then detected as follows.
In vitro ATP-TCA
An ATP-TCA kit, containing serum-free complete assay medium, digestive enzyme and luciferin-luciferase reagent (Huzhou Haichuang Biotech Co., Ltd., Huzhou, China) was used for the assessment of chemosensitivity. The ATP-TCA was performed as previously described (12,18). Briefly, samples (1–2 cm3) were harvested from solid tumors during surgical resection and cut into smaller fragments (1 mm3). The fragments were then incubated with 5–10 ml sterile digestive enzyme reagent for 2–3 h at 37°C in a 5% CO2 incubator, and dissociated to form a single cell suspension. Once the concentration of the cell suspension was adjusted to 2–4×105/ml, 100 µl cell suspension was seeded into a 96-well polypropylene microplate. Cells were incubated with 5% CO2 at 37°C for 5 days, and treated with five different doses (12.5, 25, 50, 100 and 200%) of the test drug concentration (TDC) derived from the plasma peak concentrations, which were in turn determined by pharmacokinetic and clinical information (19). The standard 100% TDC value of paclitaxel was 13.8 g/ml. The assay was performed in duplicate wells, with positive and negative controls. For each dose, two controls were included in each plate: A drug free control comprised of media only (M0) and a maximum inhibitor (MI) control which kills all cells present. At the end of the 5 day-incubation, the cells were lysed with 50 µl ATP extraction reagent, and 50 µl luciferin-luciferase reagent was added to each well. A luminometer (Orion II; Berthold Technologies GmbH & Co. KG, Bad Wildbad, Germany) was used to assess the level of ATP present, and an inhibition curve was plotted.
iTRAQ combined with LC-MS/MS
According to the results of the ATP-TCA, tumor specimens were divided into three main types: Sensitive, weakly sensitive and resistant. In order to screen the altered proteins associated with paclitaxel resistance more effectively, sensitive specimens (S group, n=8) and resistant specimens (R group, n=8) were selected for iTRAQ analysis. Frozen tissues were homogenized and sonicated (20 kHz) using 0.5% sodium dodecyl sulfate (SDS) with a cell disperser, followed by centrifugation at 20,000 × g for 30 min at 4°C to eliminate the cell debris. Following this, the supernatant was collected, and the Bradford assay was used to determine protein concentration. Next, 100 µg protein per condition were treated with dithiothreitol (10 mM) and iodoacetamide (55 mM) for reduction and alkylation. Following this, the proteins were digested with trypsin (Promega Corporation, Madison, WI, USA), and the resultant peptides mixture was further labeled using chemicals from the iTRAQ reagent kit (Applied Biosystems; Thermo Fisher Scientific, Inc., Waltham, MA, USA) according to the manufacturer's protocols. The samples were marked with iTRAQ tags as follows: iTRAQ115 for the S group and iTRAQ116 for the R group.
Next, the iTRAQ-labeled peptides were pooled and fractionated by strong cation exchange (SCX) chromatography on a SCX column (5 µm, 100A; Phenomenex, Torrance, CA, USA) with a linear gradient from 0% B to 100% B in 90 min at a flow rate of 1 ml/min (solution A: 10 mM KH2PO4, pH 3.0, 25% acetonitrile; solution B: 2 M KCl, 10 mM KH2PO4, pH 3.0, 25% acetonitrile). According to the chromatography results, the collected fractions were recombined into 16 fractions and then freeze-dried (−10°C). Following this, each freeze-dried fraction from the SCX column was re-dissolved in 100 µl 0.1% formic acid aqueous solution, and then desalted using a strata-X C18 column (Phenomenex). The sample was then extracted and analyzed using nano-LC-MS/MS with a quadrupole-Orbitrap mass spectrometer (Q-Exactive; Thermo Fisher Scientific, Inc.) as previously described (20).
Western blot analysis
Based on the proteomic results, two proteins of interest, plexin domain containing 2 (Plxdc2) and cytokeratin 7 (CK7), were expressed at higher levels in paclitaxel-resistant tissues than paclitaxel-sensitive tissues. Western blot analysis was used to examine the expression of CK7 and Plxdc2 in EOC tissues with different chemosensitivities (sensitive, weakly sensitive and resistant). The protein selections were based on a high fold change (FC) and high significance (Plxdc2, P<0.05; FC=1.539; CK7, P<0.05; FC=1.724). The extracted proteins (20 µg) were separated by 12% SDS-PAGE and transferred onto nitrocellulose membranes. Following blocking with 5% non-fat milk in Tris-buffered saline with 0.1% Tween-20 at room temperature for 1 h, the membranes were probed with the following primary antibodies: Rabbit anti-human polyclonal Plxdc2 (dilution, 1:5,000; cat. no. NBP1-76858; Novus Biologicals, LLC, Littleton, CO, USA) and rabbit anti-human polyclonal CK7 (dilution, 1:10,000; cat. no. ab154334; Abcam, Cambridge, MA, USA) at 4°C overnight. Following washing with Tris-buffered saline with Tween-20 three times, the membranes were incubated with a horseradish peroxidase-conjugated goat anti-rabbit immunoglobulin G antibody (dilution, 1:5,000; cat. no. ab97051; Abcam, Cambridge, MA, USA) at room temperature for 1–2 h. Membranes were washed as aforementioned and analyzed using a two-color infrared imaging system (Odyssey; Li-COR Biosciences, Lincoln, NE, USA). The gray level of each band was calculated using image processing ImageJ software (version 1.48; National Institutes of Health, Bethesda, MA, USA). Densitometric analysis of the bands was conducted three times and normalized to GAPDH (dilution, 1:5,000; cat. no. ab9485; Abcam, Cambridge, MA, USA).
Data analysis
ATP-TCA
ATP-TCA data were exported to a Microsoft Excel 2010 spreadsheet (Microsoft Corporation, Redmond, WA, USA), and the parameters SI (SI=500 - sum of % TGI at 200, 100, 50, 25 and 12.5% TDC), IC90 and IC50 were compared. The three types of in vitro sensitivity were defined below: Sensitive (S), IC50 <25% TDC and IC90 ≤100% TDC; weakly sensitive (WS), IC50 <25% TDC and IC90 ≤100% TDC or SI ≤250; and resistant (R), SI >250. Quality control for each assay was conducted as follows: Two measurements of every drug-treated sample were used for controlling the variability of individual ATP values. Samples with coefficient of variation (CV) >0.15 were rejected and retested. For the present study, the mean CV was 0.048 (range, 0.023–0.114).
iTRAQ assay
LC-MS/MS analysis of iTRAQ-labeled peptides was performed using Mascot (version 2.3.0) and Proteome Discoverer Version 1.3 software (Thermo Fisher Scientific, Inc.) and identification of the proteins was conducted by utilizing the raw MS data (21). For quantitative iTRAQ analysis, the peptide was automatically selected by Protein Discoverer with the Pro Group™ algorithm, and the error factor, P-value and the reporter peak area were calculated. If the iTRAQ ratio (sensitive tissues/resistant tissues) was <0.83 or >1.2 (P<0.05), the protein was considered to be differentially expressed (22). Next, Gene Ontology enrichment analysis was conducted to analyze functions of the differentially expressed proteins using Bioconductor 3.0 software (https://www.bioconductor.org), and biological process, molecular function and cellular component were included. For significant enrichment of the protein sets, a false discovery rate of <0.05 was considered as a threshold (23–25).
Statistical analysis
All results are expressed as the mean ± standard deviation. Statistical analysis between groups was performed using SPSS 18.0 software (SPSS, Inc., Chicago, IL, USA), and comparisons were made using an unpaired Student's t-test, χ2 test and one-way analysis of variance (ANOVA). Fishers least significant difference test was performed on ANOVA data in order to determine statistical significance. P<0.05 was considered to indicate a statistically significant difference.
Results
In vitro ATP-TCA
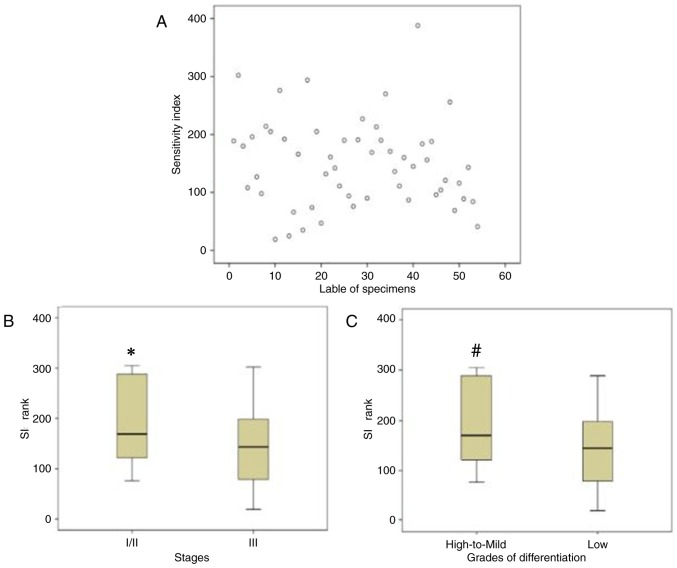
The patients were aged between 20–76 years, with a median age of 51 years. The tumor characteristics of the samples are listed in Table I. Notable heterogeneity in chemosensitivity was observed among the tumor samples examined (Fig. 1A). There was a significant association between clinical indicators of the tumor samples and the ATP-TCA results. The associations between the stage or differentiation grade of the tumor samples and the ATP-TCA results were assessed using χ2 tests. It was demonstrated that specimens with high to mild differentiation or an early stage (I/II) had lower chemosensitivity to paclitaxel when compared with low-differentiated or advanced stage (III) specimens, respectively (Table II). Furthermore, the SIs of different tumor stages and differentiation grades were also significantly different (Fig. 1B and C).
Table I.
Characteristics of tumor samples (n=54).
| Characteristics | N | (%) |
|---|---|---|
| Histology | ||
| Serous | 41 | 75.9 |
| Mucinous | 2 | 3.7 |
| Clear cell | 5 | 9.3 |
| Endometrioid | 4 | 7.4 |
| Transitional cell | 2 | 3.7 |
| FIGO stage | ||
| I | 8 | 14.8 |
| II | 7 | 13.0 |
| III | 39 | 72.2 |
| Grade of differentiation | ||
| High | 5 | 9.3 |
| Mild | 7 | 13.0 |
| Low | 42 | 77.8 |
| Primary | 48 | 88.9 |
| Recurrent | 6 | 11.1 |
FIGO, International Federation of Gynecology and Obstetrics.
Figure 1.
Results of in vitro adenosine triphosphate-tumor chemosensitivity assays. (A) Scatter plots demonstrating heterogeneity of paclitaxel in various tumor samples. Box-and-whisker plots of the SI rank of paclitaxel in specimens with different (B) stages or (C) grades of differentiation. The bottom and top edges of the boxes represent the 25th and 75th percentiles, respectively, whereas the horizontal line corresponds to the median value. The vertical lines show the range of values. *P<0.05 vs. advanced-stage (III) specimens, #P<0.05 vs. low differentiation. SI, sensitivity index.
Table II.
Associations between the adenosine triphosphate-tumor chemosensitivity assay results for paclitaxel resistance and the stage or grade of differentiation of tumor samples.
| FIGO stage | Differentiation | |||||
|---|---|---|---|---|---|---|
| Sensitivity to paclitaxel | I/II | III | P-value | High-mild | Low | P-value |
| S+WS | 8 | 34 | 0.021 | 5 | 37 | 0.003 |
| R | 7 | 5 | 7 | 5 | ||
FIGO, International Federation of Gynecology and Obstetrics; S, sensitive; WS, weak sensitive; R, resistant.
iTRAQ assay
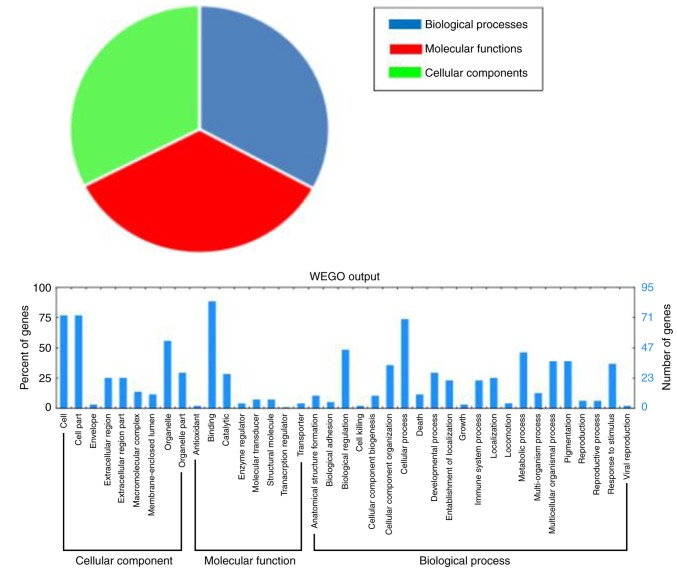
Proteins from paclitaxel-sensitive tissues and paclitaxel-resistant tissues were quantified by LC-MS/MS and iTRAQ analysis. In the present study, a total of 496 significantly differentially-expressed proteins were identified between paclitaxel-sensitive and paclitaxel-resistant tissues. The threshold of the iTRAQ ratio (sensitive tissue/resistant tissue) was <0.83 or >1.2, which implied lower or higher expression of proteins in sensitive tissues compared with resistant tissues. Among them, 233 proteins were upregulated in the paclitaxel-resistant tissues and 263 proteins were downregulated. Certain proteins with important biological functions are listed in Table III. In order to investigate the functions of the differentially expressed proteins, Gene Ontology enrichment analysis was performed to analyze the functions of those proteins. A total of 96 differentially expressed proteins were divided into three categories: ‘Molecular functions’ (92.7%), ‘cellular components’ (87.5%), and ‘biological processes’ (88.5%; Fig. 2).
Table III.
Differentially expressed proteins in S tissues compared with R tissues.
| Serial no. | Protein | Fold-change for S/R |
|---|---|---|
| Upregulated in R tissues | ||
| P02765 | α-2-HS-glycoprotein | 0.346 |
| Q9BW30 | Tubulin polymerization-promoting protein family member 3 | 0.359 |
| Q92954 | Proteoglycan 4 | 0.463 |
| P00734 | Prothrombin | 0.467 |
| P07602 | Proactivator polypeptide | 0.485 |
| P35080 | Profilin-2 | 0.517 |
| Q9UNP9 | Peptidyl-prolyl cis-trans isomerase E | 0.524 |
| Q14508 | WAP four-disulfide core domain protein 2 | 0.525 |
| Q6ZU11 | Uncharacterized protein C9orf142 | 0.539 |
| Q9H6Y7 | E3 ubiquitin-protein ligase RNF167 | 0.547 |
| P09758 | Tumor-associated calcium signal transducer 2 | 0.552 |
| P84157 | Matrix-remodeling-associated protein 7 | 0.565 |
| Q9H4G0 | Band 4.1-like protein 1 | 0.567 |
| P08729 | Cytokeratin 7, type II cytoskeletal 7 | 0.580 |
| P42330 | Aldo-keto reductase family 1 member C3 | 0.587 |
| O75882 | Attractin | 0.592 |
| Q969E4 | Transcription elongation factor A protein-like 3 | 0.595 |
| Q9Y240 | C-type lectin domain family 11, member A | 0.604 |
| P05783 | Cytokeratin 7, type I cytoskeletal 18 | 0.623 |
| P81605 | Dermcidin | 0.644 |
| P09455 | Retinol-binding protein 1 | 0.649 |
| Q6UX71 | Plexin domain-containing protein 2 | 0.650 |
| O43175 | D-3-phosphoglycerate dehydrogenase | 0.651 |
| P55809 | Succinyl-CoA:3-ketoacid-coenzyme A transferase 1, mitochondrial | 0.653 |
| Q7L2H7 | Eukaryotic translation initiation factor 3 subunit M | 0.688 |
| Q12805 | EGF-containing fibulin-like extracellular matrix protein 1 | 0.689 |
| Q8TEQ8 | GPI ethanolamine phosphate transferase 3 | 0.691 |
| Q9C0H2 | Protein tweety homolog 3 | 0.695 |
| P00751 | Complement factor B | 0.698 |
| Q14676 | Mediator of DNA damage checkpoint protein 1 | 0.701 |
| Q9BUH6 | Uncharacterized protein C9orf142 | 0.702 |
| Q9BX66 | Sorbin and SH3 domain-containing protein 1 | 0.702 |
| P02786 | Transferrin receptor protein 1 | 0.706 |
| P01861 | Ig γ-4 chain C region | 0.706 |
| O15305 | Phosphomannomutase 2 | 0.707 |
| O43752 | Syntaxin-6 | 0.731 |
| Q86SX6 | Glutaredoxin-related protein 5 | 0.732 |
| Q8NFV4 | Abhydrolase domain-containing protein 11 | 0.736 |
| Q14696 | LDLR chaperone MESD | 0.736 |
| P17931 | Galectin-3 | 0.739 |
| Q8WWF6 | DnaJ homolog subfamily B member 3 | 0.741 |
| Downregulated in R tissues | ||
| Q15063 | Periostin | 2.041 |
| P49913 | Cathelicidin antimicrobial peptide | 2.064 |
| P41218 | Myeloid cell nuclear differentiation antigen | 2.111 |
| P01814 | Ig heavy chain V–II region OU | 2.145 |
| Q9HCF4 | Protein ALO17 | 2.231 |
| P59665 | Neutrophil defensin 1 | 2.232 |
| P05164 | Myeloperoxidase | 2.246 |
| P20962 | Parathymosin | 2.283 |
| P61626 | Lysozyme C | 2.284 |
| A8MW06 | Thymosin β-4-like protein 3 | 2.329 |
| Q9NP78 | ATP-binding cassette sub-family B member 9 | 2.337 |
| P02671 | Fibrinogen α chain | 2.554 |
| P08311 | Cathepsin G | 2.763 |
| P02675 | Fibrinogen β chain | 2.784 |
S, paclitaxel-sensitive tissues; R, paclitaxel-resistant tissues.
Figure 2.
Gene Ontology enrichment analysis of the differentially expressed proteins.
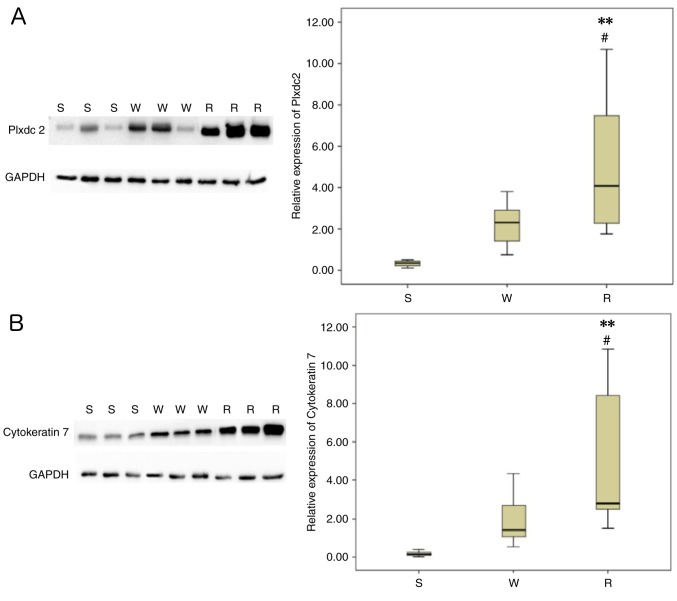
Verification by western blot analysis
To validate the expression of the two selected proteins (Plxdc2 and CK7) identified by iTRAQ in EOC tissues with different chemosensitivities (sensitive, weakly sensitive and resistant), western blotting was performed and normalized densitometry data from the western blotting were used for the determination of relative expression values. Commercially available antibodies were used for probing the proteins, which were extracted from eight individuals with each type of tissues. The results were in concordance with those of the iTRAQ: the protein expression levels of Plxdc2 and CK7 were significantly increased in the paclitaxel-resistant tissues compared with the other two types of tissues (Fig. 3A and B).
Figure 3.
Verification of isobaric tags for relative and absolute quantitation by western blotting. (A) Plxdc2 protein expression in the paclitaxel-resistant tissues was significantly upregulated compared with the other types of tissue. (B) Protein expression of cytokeratin 7 in the paclitaxel-resistant tissues was significantly upregulated compared with the other types of tissue. **P<0.01 vs. S, #P<0.05 vs. W. Plxdc2, plexin domain containing 2; S, sensitive; W, weak sensitive; R, resistant.
Discussion
Ovarian cancer is the most lethal gynecologic malignancy in adult women (26). The standard treatment for EOC is surgical resection of the tumor mass, followed by a combination of paclitaxel and platinum. Although paclitaxel is effective as a first-line drug for advanced ovarian cancer, progression of the disease and mortality remain problems that originate from drug resistance. The main cause of paclitaxel resistance is thought to be the heterogeneity of the tumor tissue (27). EOC is biologically and morphologically heterogeneous, and it is possible to divide cases into several subtypes, which are then prescribed different treatments with different clinical outcomes (28). In the present study, an in vitro ATP-TCA, which has been widely used to determine the drug sensitivity of solid tumors, was used to assess heterogeneity in EOC. There was noticeable heterogeneity in chemosensitivity among the EOC samples examined: Highly- to mildly-differentiated or early-stage (I/II) EOC specimens had lower chemosensitivity to paclitaxel when compared with specimens with low differentiation or an advanced-stage (III), respectively. These results were consistent with those of a previous study, and implied that chemotherapy was not effective at preventing the recurrence of early-stage ovarian cancer (29).
In order to further screen the suitable biomarkers for predicting chemosensitivity to paclitaxel in ovarian cancer, the quantitative proteomic technique iTRAQ was performed to analyze the proteins from paclitaxel-resistant and paclitaxel-sensitive tissues. A total of 496 significantly differentially expressed proteins were identified, including 233 proteins which were upregulated and 263 proteins which were downregulated in paclitaxel-resistant tissues compared with paclitaxel-sensitive tissues. Two proteins of interest (Plxdc2 and CK7) were selected from among the upregulated proteins, which may be associated with paclitaxel resistance in EOC. The expression of Plxdc2 and CK7 in EOC tissues with different chemosensitivities (sensitive, weakly sensitive and resistant) was further detected by western blotting. The two proteins were revealed to be upregulated in the EOC tissues with paclitaxel resistance, consistent with the results from the iTRAQ analysis.
Plxdc2 has the ability to alter normal neurogenesis patterns, and is a novel mitogen for neural progenitors, and is present in the developing neural tube (30). Miller et al (31) were interested in Plxdc2 due to its protein architecture and expression pattern, and described the expression pattern of Plxdc2 in the developing mouse embryo. Notable similarities between the Plxdc2 expression multiple Wnt family members (Wnt1, Wnt3a, Wnt5a and Wnt8b) have been identified (32). In addition, Cheng et al (33) revealed that Plxdc2 is a cell-surface receptor for pigment epithelium derived factor (PEDF). PEDF is a secreted factor with multiple biological functions. It was initially considered to be a neurotrophic factor, but its recognized functions later expanded to include a stem cell niche factor, an inhibitor of cancer cell growth and, notably, the most potent natural antiangiogenic factor (34–36). A number of animal models have demonstrated the therapeutic value of PEDF in the treatment of blinding diseases and multiple types of cancer. Even in the presence of strong proangiogenic factors, PEDF is able to inhibit endothelial cell migration and angiogenesis. Furthermore, PEDF is a non-inhibitory member of the serine protease inhibitors (serpin) superfamily, which possesses potent physiological anti-angiogenic functions. PEDF decreases abnormal neovascularization by exerting anti-angiogenic effects which inhibit pro-angiogenic factors, including vascular endothelial growth factor, and this function has been investigated primarily in the eye and in cancer (37). In the present study, Plxdc2 expression was revealed to be upregulated in paclitaxel-resistant EOC tissues. Therefore, elucidating the associations between Plxdc2 and PEDF may lead to an improved understanding of the mechanisms and the development of novel therapeutic strategies for chemoresistant EOC.
CK7 is a simple, ~55 kDa epithelial cytokeratin which is primarily expressed in single-layered simple epithelia (38). Cytokeratins are intermediate cytoskeletal structural proteins present in the epithelial cells of the majority of organs, and are involved in mechanical support. They are also crucial for epithelial function, as cytokeratins are involved in signal transduction, cell polarity and gene regulation (39). They are maintained during carcinogenesis (40,41). CK7 is expressed by a number of ductal and glandular epithelial cells (mainly gallbladder, hepatic ducts, and pancreatic ducts), by female genital tract tissues (ovary, endometrium, fallopian tube, and cervix) and by breast, lung, and urinary tract tissues (42). Chu et al (43) conducted immunohistochemistry to assess CK7 and cytokeratin 20 expression in 435 epithelial malignancy specimens, and 5% stained cells was considered to be positive. Overall, 100% of lung, ovary, uterine and salivary gland cancers were CK7-positive. In addition, CK7 is a low molecular weight cytokeratin and its expression has been used to assess the differentiation of human primary and metastatic tumors of unknown origin (44,45). In the present study, CK7 was revealed to be upregulated in paclitaxel-resistant EOC tissues, which may be involved in tumor metastasis and chemoresistance.
In conclusion, the mechanisms underlying paclitaxel resistance in ovarian cancer remain to be fully elucidated. Although further studies are required for large-scale validation of the candidate biomarkers identified by the present study, to the best of our knowledge the present study is the first to identify these candidate markers for paclitaxel-resistance in EOC. These results improve our understanding of the mechanisms underlying chemotherapy resistance and may help predict responses to targeted therapeutic agents. Furthermore, the identified proteins may aid further studies of the molecular mechanisms underlying paclitaxel treatment and resistance in EOC.
Acknowledgements
The present study was sponsored by the Capital Health Research and Development Projects of China (grant no. 2011-2008-05).
References
- 1.Cornelison R, Llaneza DC, Landen CN. Emerging Therapeutics to overcome chemoresistance in epithelial ovarian cancer: A mini-review. Int J Mol Sci. 2017;18:E2171. doi: 10.3390/ijms18102171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duda K, Cholewa H, Łabuzek K, Boratyn-Nowicka A, Okopień B. Novel strategies of ovarian cancer treatment. Pol Merku Lekarski. 2015;39:337–342. [PubMed] [Google Scholar]
- 3.Ramalingam P. Morphologic, immunophenotypic, and molecular features of epithelial ovarian cancer. Oncology (Williston Park) 2016;30:166–176. [PubMed] [Google Scholar]
- 4.Bookman MA. Optimal primary therapy of ovarian cancer. Ann Oncol. 2016;27(Suppl 1):i158–i162. doi: 10.1093/annonc/mdw088. [DOI] [PubMed] [Google Scholar]
- 5.Matsumoto K, Onda T, Yaegashi N. Pharmacotherapy for recurrent ovarian cancer: Current status and future perspectives. Jpn J Clin Oncol. 2015;45:408–410. doi: 10.1093/jjco/hyv014. [DOI] [PubMed] [Google Scholar]
- 6.O'Donnell RL, Kaufmann A, Woodhouse L, McCormick A, Cross PA, Edmondson RJ, Curtin NJ. Advanced ovarian cancerdisplays functional intratumor heterogeneity that correlates to ex vivo drug sensitivity. Int J Gynecol Cancer. 2016;26:1004–1011. doi: 10.1097/IGC.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 7.Tatar B, Boyraz G, Selçuk İ, Doğan AK, Usubütün A, Tuncer ZS. In vitro chemosensitivity in ovarian carcinoma: Comparison of three leading assays. J Turk Ger Gynecol Assoc. 2016;17:35–40. doi: 10.5152/jtgga.2016.16017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang H, Zhang L, Wei L, Gao X, Tang LI, Gong W, Min NA, Zhang LI, Yuan Y. Knockdown of cathepsin L sensitizes ovarian cancer cells to chemotherapy. Oncol Lett. 2016;11:4235–4239. doi: 10.3892/ol.2016.4494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee M, Kim SW, Nam EJ, Cho H, Kim JH, Kim YT, Kim S. ATP-based chemotherapy response assay in primary or recurrent ovarian and peritoneal cancer. Yonsei Med J. 2014;55:1664–1671. doi: 10.3349/ymj.2014.55.6.1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Han SS, Choi SH, Lee YK, Kim JW, Park NH, Song YS, Lee HP, Kang SB. Predictive value of individualized tumor response testing by ATP based chemotherapy response assay in ovarian cancer. Cancer Invest. 2008;26:426–430. doi: 10.1080/07357900701813250. [DOI] [PubMed] [Google Scholar]
- 11.Zhao D, Zhang W, Li XG, Wang XB, Zhang LF, Li M, Li YF, Tian HM, Song PP, Liu J, et al. Predicting clinical chemo-sensitivity of primary ovarian cancer using adenosine triphosphate-tumor chemo-sensitivity assay combined with detection of drug resistance genes. Zhonghua Fu Chan Ke Za Zhi. 2011;46:193–198. (In Chinese) [PubMed] [Google Scholar]
- 12.Fehm T, Zwirner M, Wallwiener D, Seeger H, Neubauer H. Antitumor activity of zoledronic acid in primary breast cancer cells determined by the ATP tumor chemosensitivity assay. BMC Cancer. 2012;12:308. doi: 10.1186/1471-2407-12-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neubauer H, Stefanova M, Solomayer E, Meisner C, Zwirner M, Wallwiener D, Fehm T. Predicting resistance to platinum-containing chemotherapy with the ATP tumor chemosensitivity assay in primary ovarian cancer. Anticancer Res. 2008;28:949–955. [PubMed] [Google Scholar]
- 14.Safinya CR, Chung PJ, Song C, Li Y, Ewert KK, Choi MC. The effect of multivalent cations and Tau on paclitaxel-stabilized microtubule assembly, disassembly, and structure. Adv Colloid Interface Sci. 2016;232:9–16. doi: 10.1016/j.cis.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tian Y, Tan AC, Sun X, Olson MT, Xie Z, Jinawath N, Chan DW, Shih IeM, Zhang Z, Zhang H. Quantitative proteomic analysis of ovarian cancer cells identified mitochondrial proteins associated with paclitaxel resistance. Proteomics Clin Appl. 2009;3:1288–1295. doi: 10.1002/prca.200900005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gagné JP, Ethier C, Gagné P, Mercier G, Bonicalzi ME, Mes-Masson AM, Droit A, Winstall E, Isabelle M, Poirier GG. Comparative proteome analysis of human epithelial ovarian cancer. Proteome Sci. 2007;5:16. doi: 10.1186/1477-5956-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tian Y, Yao Z, Roden RB, Zhang H. Identification of glycoproteins associated with different histological subtypes of ovarian tumors using quantitative glycoproteomics. Proteomics. 2011;11:4677–4687. doi: 10.1002/pmic.201000811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ling ZQ, Qi CJ, Lu XX, Qian LJ, Gu LH, Zheng ZG, Zhao Q, Wang S, Fang XH, Yang ZX, et al. Heterogeneity of chemosensitivity in esophageal cancer using ATP-tumor chemosensitivity assay. Acta Pharmacol Sin. 2012;33:401–406. doi: 10.1038/aps.2011.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Konecny G, Crohns C, Pelgram M, Felber M, Lude S, Kurbacher C, Cree IA, Hepp H, Untch M. Correlation of drug response with the ATP tumorchemosensitivity assay in primary FIGO stage III ovarian cancer. Gynecol Oncol. 2000;77:258–263. doi: 10.1006/gyno.2000.5728. [DOI] [PubMed] [Google Scholar]
- 20.Wang H, Wu K, Liu Y, Wu Y, Wang X. Integrative proteomics to understand the transmission mechanism of Barley yellow dwarf virus-GPV by its insect vector Rhopalosiphum padi. Sci Rep. 2015;5:10971. doi: 10.1038/srep10971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perkins DN, Pappin DJ, Creasy DM, Cottrell JS. Probability-based protein identification by searching sequence databases using mass spectrometry data. Electrophoresis. 1999;20:3551–3567. doi: 10.1002/(SICI)1522-2683(19991201)20:18<3551::AID-ELPS3551>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 22.Zhong XW, Zou Y, Liu SP, Yi QY, Hu CM, Wang C, Xia QY, Zhao P. Proteomic-based insight into Malpighian tubules of silkworm Bombyx mori. PLoS One. 2013;8:e75731. doi: 10.1371/journal.pone.0075731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shan N, Zhou W, Zhang S, Zhang Y. Identification of HSPA8 as a candidate biomarker for endometrial carcinoma by using iTRAQ-based proteomic analysis. Onco Targets Ther. 2016;9:2169–2179. doi: 10.2147/OTT.S97983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, Davis AP, Dolinski K, Dwight SS, Eppig JT, et al. Gene ontology: Tool for the unification of biology. Nat Genet. 2000;25:25–29. doi: 10.1038/75556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The Gene Ontology Consortium: Expansion of the Gene Ontology knowledgebase and resources. Nucleic Acids Res. 2017;45:D331–D338. doi: 10.1093/nar/gkw1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Christie M, Oehler MK. Molecular pathology of epithelial ovarian cancer. J Br Menopause Soc. 2006;12:57–63. doi: 10.1258/136218006777525794. [DOI] [PubMed] [Google Scholar]
- 27.Giordano S, Zucchetti M, Decio A, Cesca M, Nerini Fuso I, Maiezza M, Ferrari M, Licandro SA, Frapolli R, Giavazzi R, et al. Heterogeneity of paclitaxel distribution in different tumor models assessed by MALDI mass spectrometry imaging. Sci Rep. 2016;6:39284. doi: 10.1038/srep39284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Symeonides S, Gourley C. Ovarian cancer molecular stratification and tumor heterogeneity: A necessity and a challenge. Front Oncol. 2015;5:229. doi: 10.3389/fonc.2015.00229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang J, Li H. Heterogeneity of tumor chemosensitivity in ovarian epithelial cancer revealed using theadenosine triphosphate-tumor chemosensitivity assay. Oncol Lett. 2015;9:2374–2380. doi: 10.3892/ol.2015.3056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miller-Delaney SF, Lieberam I, Murphy P, Mitchell KJ. Plxdc2 is a mitogen for neural progenitors. PLoS One. 2011;6:e14565. doi: 10.1371/journal.pone.0014565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller SF, Summerhurst K, Rünker AE, Kerjan G, Friedel RH, Chédotal A, Murphy P, Mitchell KJ. Expression of Plxdc2/TEM7R in the developing nervous system of the mouse. Gene Expr Patterns. 2007;7:635–644. doi: 10.1016/j.modgep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 32.Qi W, Yang C, Dai Z, Che D, Feng J, Mao Y, Cheng R, Wang Z, He X, Zhou T, et al. High levels of pigment epithelium-derived factor in diabetes impair wound healing through suppression of Wnt signaling. Diabetes. 2015;64:1407–1419. doi: 10.2337/db14-1111. [DOI] [PubMed] [Google Scholar]
- 33.Cheng G, Zhong M, Kawaguchi R, Kassai M, Al-Ubaidi M, Deng J, Ter-Stepanian M, Sun H. Identification of PLXDC1 and PLXDC2 as the transmembrane receptors for the multifunctional factor PEDF. Elife. 2014;3:e05401. doi: 10.7554/eLife.05401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sagheer U, Gong J, Chung C. Pigment Epithelium-Derived Factor (PEDF) is a determinant of stem cell fate: Lessons from an Ultra-Rare disease. J Dev Biol. 2015;3:112–128. doi: 10.3390/jdb3040112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang S, Zhai G, Shi W, Wang Y, Zhu L, Dai Y, Chen C. Pigment Epithelium-Derived factor inhibits oxygen-induced retinal neovascularization in a murine model. Fetal Pediatr Pathol. 2016;35:173–185. doi: 10.3109/15513815.2016.1147626. [DOI] [PubMed] [Google Scholar]
- 36.Belkacemi L, Zhang SX. Anti-tumor effects of Pigment Epithelium-Derived Factor (PEDF): Implication for cancer therapy. A mini-review. J Exp Clin Cancer Res. 2016;35:4. doi: 10.1186/s13046-015-0278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chuderland D, Ben-Ami I, Bar-Joseph H, Shalgi R. Role of pigment epithelium-derived factor in the reproductive system. Reproduction. 2014;148:R53–R61. doi: 10.1530/REP-14-0251. [DOI] [PubMed] [Google Scholar]
- 38.Sandilands A, Smith FJ, Lunny DP, Campbell LE, Davidson KM, MacCallum SF, Corden LD, Christie L, Fleming S, Lane EB, McLean WH. Generation and characterisation of Keratin 7 (K7) knockout mice. PLoS One. 2013:e64404. doi: 10.1371/journal.pone.0064404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Windoffer R, Beil M, Magin TM, Leube RE. Cytoskeleton in motion: The dynamics of keratin intermediate filaments in epithelia. J Cell Biol. 2011;194:669–678. doi: 10.1083/jcb.201008095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bayrak R, Yenidunya S, Haltes H. Cytokeratin 7 and Cytokeratin 20 expression in colorectal adenocarcinoma. Pathol Res Pract. 2011;207:156–160. doi: 10.1016/j.prp.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 41.Gurzu S, Jung I. Aberrant pattern of the cytokeratin 7/cytokeratin 20 immunophenotype in colorectal adenocarcinomas with BRAF mutation. Pathol Res Pract. 2012;208:163–166. doi: 10.1016/j.prp.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 42.Toyoshima M, Momono Y, Makino H, Kudo T, Oka N, Sakurada J, Suzuki H, Kodama H, Yoshinaga K. Cytokeratin 7-positive/cytokeratin 20-negative cecal adenocarcinoma metastaticto the uterine cervix: A case report. World J Surg Oncol. 2016;14:22. doi: 10.1186/s12957-016-0774-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chu P, Wu E, Weiss LM. Cytokeratin 7 and cytokeratin 20 expression in epithelial neoplasms: A survey of 435 cases. Mod Pathol. 2000;13:962–972. doi: 10.1038/modpathol.3880175. [DOI] [PubMed] [Google Scholar]
- 44.Shin JH, Bae JH, Lee A, Jung CK, Yim HW, Park JS, Lee KY. CK7, CK20, CDX2 and MUC2 Immunohisto-chemical staining used to distinguish metastatic colorectal carcinoma involving ovary from primary ovarian mucinous adenocarcinoma. Jpn J Clin Oncol. 2010;40:208–213. doi: 10.1093/jjco/hyp150. [DOI] [PubMed] [Google Scholar]
- 45.Moll R, Divo M, Langbein L. The human keratins: Biology and pathology. Histochem Cell Biol. 2008;129:705–733. doi: 10.1007/s00418-008-0435-6. [DOI] [PMC free article] [PubMed] [Google Scholar]