Abstract
Introduction
A cholecystocolonic fistula (CCF) is a late complication following repeated episodes of chronic inflammation of the gallbladder in contact with the hepatic flexure, and it might cause a biliary ileus in the colon, causing an intestinal obstruction, and if left untreated, a life threatening disease.
Presentation of case
a 49-year-old female patient presented with abdominal pain and bowel obstruction due to a gallstone impaction on the sigmoid colon as consequence of a cholecystocolonic fistula. An enterolithotomy was performed, and the patient evolved favorably. She was discharged without complications on the 5th Postoperative day (POD).
Discussion
Clinical signs of CCF are usually minimal, and a preoperative diagnostic of CCF is rare, and it often presents with abdominal pain, nausea, vomiting, diarrhea, weight loss, and malabsorption. In the vast majority of patients presenting with CCF and biliary ileus, the stone is located within the sigmoid colon, accompanied with a concomitant disease at this point, with diverticulosis being the most common occurrence.
Conclusion
A cholecystocolonic fistula with a gallstone colonic ileus must be suspected in an elderly, and female, patient presenting with cholelithiasis and with intestinal obstruction. Treatment should not be delayed, and correction of the intestinal obstruction ought to be the basis of the treatment.
Keywords: Cholecystocolonic fistula, Gallstone ileus, Colonic ileus, Bilioenteric fistula
Highlights
-
•
We present a case report of a 49-year-old female patient presented with abdominal pain and bowel obstruction due to a gallstone impaction on the sigmoid colon.
-
•
Little over 250 cases have been reported in medical literature.
-
•
Correction of the intestinal obstruction with enterolithotomy ought to be the basis of the treatment.
1. Introduction
A gallstone ileus is a mechanical intestinal obstruction caused by a gallstone impaction within the gastrointestinal tract [1]. It mainly occurs following the formation of a cholecystoenteric fistula, most commonly in the duodenum and secondly in the colon. A cholecystocolonic fistula (CCF) is a late complication of repeated episodes of chronic inflammation of the gallbladder in contact with the hepatic flexure, occurring in 0.06%-0. 14% of patients with biliary disease, and it represent around 6.3%–26.5% of all cholecystoenteric fistulas [[2], [3], [4], [5], [6]]. A gallstone ileus is a rare complication of cholelithiasis, accounting for 1–4% of all cases of intestinal obstruction with a predominance in the female population [1,[5], [6], [7], [8]]. The most common place of presentation is within the small intestine, then the stomach and less frequently inside the colon [7]. Impaction of a gallstone in the sigmoid colon causing a large bowel obstruction is rare and it's usually at the sites of previous inflammation or colonic disease [4].
Here we present a case of a 49-year-old female patient presenting with abdominal pain and bowel obstruction due to a gallstone impaction on the sigmoid colon due to a CCF. No more than 250 cases have been reported; a review of the literature of this rare condition is also revised. The work has been reported in line with the SCARE criteria [9].
2. Presentation of case
A 49 year-old female patient was admitted to the hospital with severe abdominal pain, nausea, vomiting, and constipation following a 3-day history of colicky middle abdominal pain. The patient had no relevant medical history, reporting only arterial hypertension being treated with telmisartan.
On examination the patient was hemodynamically stable and afebrile. Physical examination revealed abdominal distension with decreased bowel movements to auscultation accompanied by diffuse tenderness to superficial and deep palpation and a tympanic colonic margin to percussion. After a thorough abdominal exploration, no positive signs for peritonism were detected. Digital rectal examination revealed an empty rectum, without abnormalities.
Laboratories showed a normal hemoglobin of 13.7 g/dl, a WBC of 6.7 × 10ˆ10 and no alterations in liver enzymes, except for an elevation in GGT, with a value of 226UL.
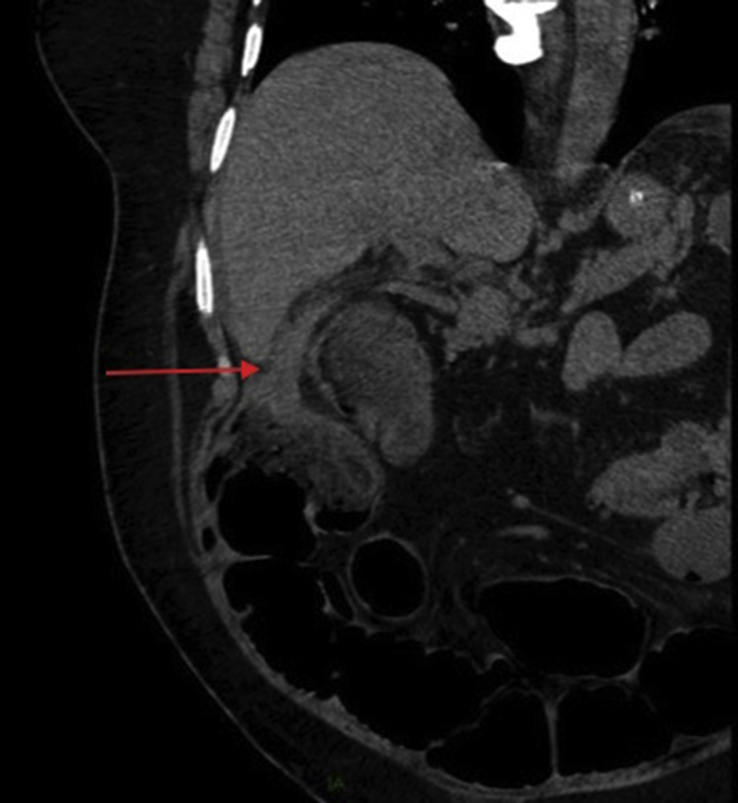
Simple abdominal radiographs were performed, observing dilated loops of the small bowel, and no signs of gas in the rectum. A CT was ordered, revealing a 3 × 2 cm calcified mass in the sigmoid colon, suggestive of a gallstone, with associated enlargement of the surrounding intestinal wall, with stranding pericolonic fat and signs of diverticular disease (Fig. 1). A collapsed gallbladder was observed with no dilation of the biliary tree, along with a fistulous connection between the gallbladder and the hepatic flexure (Fig. 2).
Fig. 1.
Red arrow showing a 3 × 2 cm calcified mass in the sigmoid colon, compatible with a gallstone, with pericolonic fat stranding and diverticular disease. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
Fistulous connection between the gallbladder and the hepatic flexure, showed with a red arrow. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
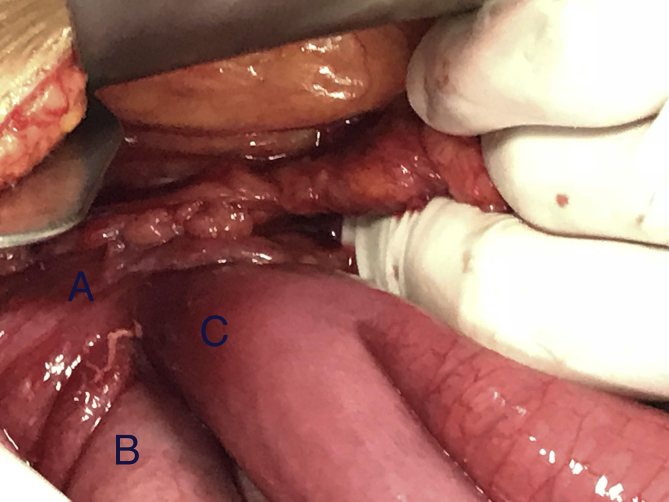
The patient underwent an exploratory laparotomy, and after the abdominal cavity was exposed, signs of dilation of the small intestinal loops became evident. An intraluminal, solid, non-mobile mass was found in the sigmoid colon (Fig. 3). An enterolithotomy was performed, and a 4 × 4 cm gallstone was extracted without complications, performing a primary transverse closure of the colon. A fistulous track was observed between the gallbladder and the hepatic flexure of the colon, the small intestine was also adhered to the gallbladder without any anomalous communications (Fig. 4).
Fig. 3.
Sigmoid non-mobile gallstone of 4 × 4 cm.
Fig. 4.
Fistulous connection between the gallbladder (A) and the hepatic flexure of the colon (B). A portion of the small intestine was in contact with the anomalous communication (C).
The patient had an adequate postoperative outcome, referring only moderate pain during the first day. Oral intake was reintroduced on the fourth day, without further complications. On the fifth POD the patient was discharged home, with good oral intake and with normal evacuations. On a 8 month-follow up, the patient is doing well with no biliary symptoms.
3. Discussion
The exact etiology of CCF secondary to gallstone disease may vary. Glenn et al. [10] in their study of a few more than a hundred bilioenteric fistulas, stated that acute inflammation of the gallbladder with obstruction of the cystic duct allows adhesion of the gallbladder to the contiguous organs. This promotes ulceration and ischaemia of the wall of the gallbladder and the adjacent organs, creating an anomalous communication between them. Costi et al. [6] in their CCF systematic review of 231 cases, support this theory, but also stated that other etiologies are associated with this particular fistula, such as a previous gastric surgery, cholecystostomy and traumatic or iatrogenic abdominal wounds.
Clinical signs of CCF are usually minimal, and preoperative diagnosis of CCF is rare and only considered in 7.9% of all CCF, therefore the diagnosis is often made intraoperatively [6,11]. Signs and symptoms of a CCF may vary, as it often presents with abdominal pain, nausea, vomit, diarrhea, weight loss, and malabsorption. The later may be present, because the enterohepatic circulation may also be affected; increasing the secretion of water and electrolytes from the colon [2,3,6,12]. This last symptom along with right hypochondrium pain and cholangitis, form a clinical triad described in patients with this entity [6].
Gallstone ileus develops in 0.3%-0. 5% of patients with cholelithiasis. It constitutes the etiologic factor in less than 5% of cases of intestinal obstruction, but up to 25% of nonstrangulated small bowel obstructions in elderly patients [1,[13], [14], [15], [16], [17]] Gallstone impaction occurs most frequently in the small intestine, followed by the colon in 8% of the cases [1,[18], [19], [20]].
In the vast majority of patients presenting with CCF and biliary ileus, the stone is located at the sigmoid colon. The size of the gallstone is presumed to determine whether and where a migrated stone will impact. Small and mid-sized stones are thought to pass through the entire colon, thus being easily expelled through stools; whereas gallstones over 2.5 cm in diameter may cause colonic obstruction at the sigmoid colon [2,6,16,20,21]. They usually occur secondary to a concomitant pathologic narrowing at that level, with diverticular disease being the most common cause [1,4,16,20,22]. Our patient had diverticular disease and a gallstone of 4 cm, predisposing it to impact at this point.
Misdiagnosis is common and it also carries a significant rate of complications with a mortality rate ranging from 12% to 27% in most series reported [13,14,23]. Preoperatively diagnosis is therefore critical to improve morbidity, mortality and post-operative complications. In 1941, Rigler et al. [24] described four radiographic signs in gallstone ileus: intestinal obstruction; pneumobilia; aberrant gallstone; and change of the position of such gallstone on serial films. The presence of two of the three first signs has been considered pathognomonic. While diagnosing a gallstone ileus, the sensitivity of plain film varied from 40% to 70% and in combination with ultrasonography it increased to 74%, compared to the 93% of sensitivity of the CT scan, making it the gold standard for diagnosis [1,4,13,25].
Treatment of CCF has changed through the years; traditional treatment during the early 80s suggested a ‘‘two-stage’’ procedure, performing a diverting colostomy. Nowadays, a ‘‘one-step’’ management has been considered the treatment of choice without significant complications being reported, versus doing only the enterolithotomy alone [6,26]. When a colonic ileus is present, the preferred treatment is to resolve the obstruction by performing an enterolithotomy by itself; where a longitudinal enterotomy incision is performed extracting the stone and closing it in a transverse fashion [1,15,16,27]. Reisner et al. [14] in their review of 1001 cases, determined a lower mortality rate when performing an enterolithotomy by itself against a definitive biliary surgery during the same procedure. Also, an exploratory search for other stones in both the small and large bowel is mandatory to prevent reobstruction [15]. The need to repair the bilioenteric fistula and perform the cholecystectomy in the same procedure is still a matter of debate, and it must be weighed against performing the enterolithotomy alone. We opted to perform solely the enterolithotomy because the patient never experienced biliary colic or any other symptoms associated with gallbladder disease. We decided to correct only the occlusion during the laparotomy, as the surgical approach was less complicated, and it had a lower mortality rate. Simple enterolithotomy enthusiasts state the infrequency of recurrent gallstone ileus, and the rarity of complications directly related to a persistent gallbladder fistula, such as cholecystitis, cholangitis, malabsorption and carcinoma of the gallbladder [14,17,26,28,29]. Also, when the occlusion is resolved, the possibility of spontaneous closure of the fistulous track is higher, leaving behind only a fibrous remnant [26,28].
Less common management options for a gallstone ileus include; oesophagogastroduodenoscopy in gastric outlet obstruction or Bouveret's syndrome [30], removal of a colonic stone with colonoscopy [31], extracorporeal shock wave lithotripsy, endoscopic laser lithotripsy, electrohydraulic lithotripsy, or mechanical lithotripsy [1,15,18,32]. A limitation for endoscopic management of a gallstone is a location out of endoscopic reach, however, whenever possible endoscopic treatment should be attempted, especially in elderly patients with associated comorbidities. We didn't attempt the latter because the hospital didn't have the necessary resources.
Laparoscopy treatment is also a feasible option in uncomplicated cases, if it's managed by experienced laparoscopic surgeons, although increased operating time and conversion rate are to probably be expected [6].
4. Conclusion
A Cholecystocolonic fistula must be suspected when the patient is elderly, female, affected by gallbladder lithiasis and presenting a distal colon obstruction. Surgical relief of obstruction by performing an enterolithotomy is the cornerstone of the treatment, and a one-stage cholecystectomy and repair of the bilioenteric fistula is justified only in selected patients in good general condition and who are adequately stabilized preoperatively. Whenever possible, utilizing less invasive measures with an endoscopic approach avoids the potential morbidity of surgery.
Ethical approval
NA.
Sources of funding
None funding.
Author contribution
Mauricio Gonzalez- Urquijo: He is a second year general surgery resident. He was the leader of the work, he design the case report. He recollected data, and wrote the manuscript.
Enrique Quevedo-Fernandez: He is a first year surgical resident. He helped recollected the patient data, and helped wrote the manuscript.
David Eugenio Hinojosa Gonzalez: He is a senior year medical student. He recollected the patient data, and wrote the presentation of the case.
Conflicts of interest
None.
Research registration number
NA.
Guarantor
Mauricio Gonzalez-Urquijo.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
González-Urquijo Mauricio, Email: mauriciogzzu@gmail.com.
Hinojosa-Gonzalez David Eugenio, Email: d.hinojosa94@gmail.com.
Quevedo-Fernandez Enrique, Email: enriquequevedo@live.com.mx.
References
- 1.Nuño-Guzmán C.M. Gallstone ileus, clinical presentation, diagnostic and treatment approach. World J Gastrointest Surg [Internet] 2016;8(1):65. doi: 10.4240/wjgs.v8.i1.65. Available from: http://www.wjgnet.com/1948-9366/full/v8/i1/65.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alqunai M.S., Daif-allah M.A., Alhammad L. vol. 4. 2017. pp. 2823–2825. (Acute Cholecystitis with Cholecystocolic Fistula: a Case Report and Pertinent Literature Review). 8. [Google Scholar]
- 3.Antonacci N., Taffurelli G., Casadei R., Ricci C., Monari F., Minni F. Asymptomatic cholecystocolonic fistula: a diagnostic and therapeutic dilemma, asymptomatic cholecystocolonic fistula: a diagnostic and therapeutic dilemma. Case Reports Surgery, Case Reports Surg [Internet] 2013;2013:2013. doi: 10.1155/2013/754354. http://www.hindawi.com/journals/cris/2013/754354/abs/%5Cnhttp://downloads.hindawi.com/journals/cris/2013/754354.pdf%5Cnhttp://www.hindawi.com/journals/cris/2013/754354/%5Cnhttp://www.ncbi.nlm.nih.gov/ e754354. Available from: http://www.hindawi.com/journals/cris/2013/754354/abs/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Brien J.W., Webb L.A., Evans L., Speakman C., Shaikh I. Gallstone ileus caused by cholecystocolonic fistula and gallstone impaction in the sigmoid colon: review of the literature and novel surgical treatment with trephine loop colostomy. Case Rep Gastroenterol. 2017;11(1):95–102. doi: 10.1159/000456656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gibreel W., Greiten L.L., Alsayed A., Schiller H.J. Management dilemma of cholecysto-colonic fistula: case report. Int J Surg Case Rep [Internet] 2018;42:233–236. doi: 10.1016/j.ijscr.2017.12.017. Available from: https://doi.org/10.1016/j.ijscr.2017.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costi R., Randone B., Violi V., Scatton O., Sarli L., Soubrane O. Cholecystocolonic fistula: facts and myths. A review of the 231 published cases. J Hepatobiliary Pancreat Surg. 2009;16(1):8–18. doi: 10.1007/s00534-008-0014-1. [DOI] [PubMed] [Google Scholar]
- 7.Halleran D.R., Halleran D.R. Colonic perforation by a large gallstone: a rare case report. Int J Surg Case Rep [Internet] 2014;5(12):1295–1298. doi: 10.1016/j.ijscr.2014.11.058. Available from: https://doi.org/10.1016/j.ijscr.2014.11.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heaney R.M. Colonic gallstone ileus: the rolling stones. BMJ Case Rep. 2014;2014:2–5. doi: 10.1136/bcr-2014-204402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Glenn J.F. Analysis of 51 patients with horseshow kidney. NEJM. 1959;261(14):684–687. doi: 10.1056/NEJM195910012611402. [DOI] [PubMed] [Google Scholar]
- 11.Chowbey Pradeep k., Bandyopadhyay S.K., Anil S., Rajesh K., Vandana S., Manish B. Laparoscopic management of cholecystoenteric fistulas. J Laparoendosc Adv Surg Tech [Internet] 2006;16(5):453–456. doi: 10.1089/lap.2006.16.467. Available from: https://doi.org/10.1016/S0976-0016(11)60090-2. [DOI] [PubMed] [Google Scholar]
- 12.Elsas L.J., Gilat T. Cholecystocolonic fistula with malabsorption. Ann. Intern. Med. 1965 Sep;63:481–486. doi: 10.7326/0003-4819-63-3-481. [DOI] [PubMed] [Google Scholar]
- 13.Yu C.-Y., Lin C.-C., Shyu R.-Y., Hsieh C.-B., Wu H.-S., Tyan Y.-S. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol World J Gastroenterol ISSN. 2005;11(14):2142–2147. doi: 10.3748/wjg.v11.i14.2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reisner R.M., Cohen J.R. Gallstone ileus: a review of 1001 reported cases. Am. Surg. 1994 Jun;60(6):441–446. [PubMed] [Google Scholar]
- 15.Abou-Saif A., Al-Kawas F.H. Complications of gallstone disease: mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am. J. Gastroenterol. 2002;97(2):249–254. doi: 10.1111/j.1572-0241.2002.05451.x. [DOI] [PubMed] [Google Scholar]
- 16.Milsom J.W., Mackeigan J.M. 1985. Gallstone Obstruction of the Colon Report of Two Cases and Review of Management; pp. 367–368. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez-Sanjuán J.C., Casado F., Fernández M.J., Morales D.J., Naranjo A. Cholecystectomy and fistula closureversus enterolithotomy alone in gallstone ileus. Br J Surg [Internet] 1997;84(5):634–637. Available from: http://doi.wiley.com/10.1002/bjs.1800840514. [PubMed] [Google Scholar]
- 18.Pracki M., Regula J., Pachlewski J., Rupinski M., Cwik M. 2006. Sigmoid Laser Lithotripsy for Gallstone Ileus; pp. 30–32. [Google Scholar]
- 19.Clavien P a, Richon J., Burgan S., Rohner a. Gallstone ileus. Br J Surg [Internet] 1990;77(7):737–742. doi: 10.1002/bjs.1800770707. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2200556. [DOI] [PubMed] [Google Scholar]
- 20.Anseline P. 1981. Colonic Gallstone Ileus; pp. 62–65. 0(January) [Google Scholar]
- 21.Glenn F., Reed C., Grafe W.R. Biliary enteric fistula. Surg. Gynecol. Obstet. 1981 Oct;153(4):527–531. [PubMed] [Google Scholar]
- 22.Farkas N., Karthigan R., Lewis T., Read J., Farhat S., Zaidi A. A single centre case series of gallstone sigmoid ileus management. Int J Surg Case Rep [Internet] 2017;40:58–62. doi: 10.1016/j.ijscr.2017.09.009. Available from: https://doi.org/10.1016/j.ijscr.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dowse J.L. Cholecysto-duodenocolic fistulae due to gall-stones. Br. J. Surg. 1963;50:776–778. doi: 10.1002/bjs.18005022520. [DOI] [PubMed] [Google Scholar]
- 24.Lg R., Cn B., Jf N. Gallstone obstruction: pathogenesis and roentgen manifestations. J Am Med Assoc [Internet] 1941 Nov 22;117(21):1753–1759. Available from: https://doi.org/10.1001/jama.1941.02820470001001. [Google Scholar]
- 25.Ripolles T., Miguel-Dasit A., Errando J., Morote V., Gomez-Abril S.A., Richart J. Gallstone ileus: increased diagnostic sensitivity by combining plain film and ultrasound. Abdom. Imag. 2001;26(4):401–405. doi: 10.1007/s002610000190. [DOI] [PubMed] [Google Scholar]
- 26.Costantini R., Massimini F., Fiordaliso M., Cotroneo A.R., Innocenti P., Giamberardino M.A. Gallstone ileus of the sigmoid colon: a rare complication of gallbladder calculosis typical of advanced age. Report of a Case. 2016;5(3) [Google Scholar]
- 27.Doogue M.P., Choong C.K., Frizelle F a. Recurrent gallstone ileus: underestimated. Aust. N. Z. J. Surg. 1998;68(11):755–756. doi: 10.1111/j.1445-2197.1998.tb04669.x. [DOI] [PubMed] [Google Scholar]
- 28.DECKOFF S.L. Gallstone ileus; a report of 12 cases. Ann. Surg. 1955;142(1):52–65. doi: 10.1097/00000658-195507000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bossart Peter A., Andrew H., Patterson H.A.Z. Carcinoma of the gallbladder. Am. J. Surg. 1962;103:366–369. doi: 10.1016/0002-9610(62)90227-1. [DOI] [PubMed] [Google Scholar]
- 30.Bedogni G., Contini MM S., Pedrazzoli GCP C. Pyloroduodenal obstruction due to a biliary stone (Bouveret's syndrome) managed by endoscopic extraction G. Gastrointest Endosc [Internet] 1985;31:36–38. doi: 10.1016/s0016-5107(85)71965-7. Available from: https://doi.org/10.1016/S0016-5107(85)71965-7. [DOI] [PubMed] [Google Scholar]
- 31.Roberts S.R., Chang C., Chapman T., Koontz P.G.J., Early G.L. Colonoscopic removal of a gallstone obstructing the sigmoid colon. J. Tenn. Med. Assoc. 1990 Jan;83(1):18–19. [PubMed] [Google Scholar]
- 32.Sackmann M., Holl J., Haerlin M., Sauerbruch T., Hoermann R., Heinkelein J. Gallstone ileus successfully treated by shock-wave lithotripsy. Dig. Dis. Sci. 1991 Dec;36(12):1794–1795. doi: 10.1007/BF01296628. [DOI] [PubMed] [Google Scholar]