Abstract
Background and Objectives
Although a clear advantage in mortality has been documented among older Hispanic subgroups, particularly the foreign-born, research examining health selectivity in morbidity life expectancies among older Hispanics are scarce. Differences in sociocultural characteristics among Hispanic subgroups may influence racial/ethnic and nativity disparities in morbidity. Research examining the heterogeneity among older Hispanic subgroups may further our understanding of why some Hispanics are able to preserve good health in old age, while others experience a health disadvantage. Thus, the primary goal of this analysis is to examine racial/ethnic, nativity, and country of origin differences in morbidity life expectancies among older adults in the United States.
Research Design and Methods
We used individual-level data (1999–2015) from the National Health Interview Survey to estimate Sullivan-based life tables of life expectancies with morbidity and without morbidity by gender for U.S.-born Mexicans, foreign-born Mexicans, U.S.-born Puerto Ricans, island-born Puerto Ricans, foreign-born Cubans, and whites in mid-life (age 50), and late-life (age 65).
Results
Hispanics are heterogeneous in morbidity life expectancies. Among females, U.S.-born Mexicans, foreign-born Mexicans, and island-born Puerto Ricans spent more late-life years with morbidity than whites. For men, U.S.-born Puerto Ricans were the only Hispanic subgroup disadvantaged in the number of years lived with morbidity. Conversely, foreign-born Cubans exhibited the healthiest outcomes of all groups, regardless of gender.
Discussion and Implications
Reducing the risk for late-life morbidity must be informed by a comprehensive understanding of a wide range of factors that shape health among older adults. Research should avoid pan-ethnic groupings that overlook important differences in chronic disease risk profiles among Hispanic subgroups. Recognizing the various sociocultural and environmental processes that underlie Hispanic subpopulations is important for development and implementation of social and public health policies aimed at ameliorating negative health outcomes of late-life morbidity among minority and immigrant groups.
Keywords: Chronic disease, Health Disparities, Hispanics, Morbidity
Translational Significance
Recognizing the various sociocultural processes that underlie the health of older Hispanic subgroups is important for development and implementation of data-driven culture-appropriate interventions and targeted policies aimed at ameliorating the risks and negative health outcomes of late-life multi-morbidity among minority and immigrant groups.
As the composition of the U.S. population becomes increasingly older and more diverse, the need to understand health differences by race/ethnicity, nativity, and country of origin in late life becomes increasingly important for our society, especially with respect to public health policy and social services. Immigration from Mexico and other areas of Latin America and the aging of the Hispanic population play a significant role in the demographic shift in the age structure of the older U.S. population (West, Cole, Goodkind, & He, 2014). For example, the proportion of Hispanics aged 65 and older is projected to increase from 8% in 2014 to 22% in 2060 (Mather, Jacobsen, & Pollard, 2015). These trends make clear that the future health patterns of older adults in the United States will increasingly reflect those of the Hispanic population (Hummer & Hayward, 2015). Such trends have implications for public health planning and health care resources allocations.
Despite a disadvantaged socioeconomic profile, older Hispanics, particularly the foreign-born, have been found to have longer life expectancies than non-Hispanic whites (hereafter, “whites”) (Arias, Heron, & Xu, 2017; Garcia, Downer, et al., 2017). However, greater longevity accompanied by unfavorable socioeconomic characteristics raises important questions regarding health patterns of the older Hispanic population (Garcia, Valderrama-Hinds, et al., 2017; Hummer & Hayward, 2015). Declines in mortality without subsequent improvements in the incidence and prevalence of morbidity can lead to an increase in the proportion of the population living with potentially disabling diseases (Crimmins & Levine, 2016). Thus, for older Hispanics, the individual and social benefits of increased longevity may be undermined if the additional years of life are characterized by a high prevalence of chronic diseases. Indeed, the combination of long life expectancy and increases in the prevalence of disease suggests that, without data-driven health care planning, older Hispanics will require additional health care resources to deal with chronic diseases, functional limitations, and disability in later life.
Morbidity is a common indicator of population health that reflects physiological changes linked to age and other risk factors that may lead to physiologic dysregulation, which precedes disability and functioning loss (Crimmins, Kim, & Vasunilashorn, 2010). Studies on trends in morbidity have shown an increase in the proportion of older individuals living with major diseases such as diabetes, cancer, stroke, and heart disease (Crimmins & Beltrán-Sánchez, 2011; Martin & Schoeni, 2014), resulting in a growth of the population living longer with disease (Crimmins & Levine, 2016). Research has documented racial/ethnic and nativity differences among older Hispanics (Cantu, Hayward, Hummer, & Chiu, 2013) and elder Mexican Americans (Garcia, Valderrama-Hinds, et al., 2017) in life expectancy with morbidity, life expectancy without morbidity, and the proportion of late life spent with morbidity. However, older Hispanics in the United States are heterogeneous in their nativity and country of origin composition. In 2015, 34.4% of Hispanics were foreign-born, and 56.6% were born in the United States (Flores, 2017). Moreover, the U.S. Census Bureau defines Hispanic as any person of Cuban, Mexican, Puerto Rican, South or Central American, or other Spanish origin, regardless of race (Humes, Jones, & Ramirez, 2011). These individuals have origins in more than 20 countries, each with distinctive sociocultural characteristics that contribute to unique health experiences (Fenelon, Chinn, & Anderson, 2017). For consistency, the term “Hispanic” will be used throughout the article to identify any of the subgroups mentioned above regardless of nativity or country of origin.
Recent findings highlight two key patterns in mortality and morbidity outcomes among older Hispanic subgroups by nativity, and country of origin: (a) older Hispanics (with the exception of U.S.-born Puerto Ricans) exhibit lower mortality rates than whites, regardless of gender (Fenelon et al., 2017); and (b) foreign-born Cubans and foreign-born Mexicans exhibit a lower overall disease burden relative to whites, regardless of gender (Garcia, Garcia, & Ailshire, 2018; Zsembik & Fennell, 2005). However, it remains unclear whether the lower risk of mortality observed among Hispanic subgroups relative to whites contributes to a longer healthier life expectancy or a longer life expectancy with chronic morbidity.
Consequently, this study aims to contribute to the current literature on older Hispanic health in three important ways. The first is to propose theoretical considerations for assessing the heterogeneity among older Hispanics. Second, we provide an overview of sociocultural characteristics that are important to understand morbidity and longevity differences among older Hispanics by nativity, country of origin, and gender. Finally, we combine national data on morbidity and mortality to document differences in life expectancies with morbidity, without morbidity, and the proportion of life without morbidity between older white and Hispanic subgroups. For our third aim, we focus on two distinct stages that encompass mid-life (50 and older), and late-life (65 and older) to assess whether increasing life expectancy among older Hispanic subgroups relative to whites is accompanied by better health and quality of life.
We argue that differences in social and cultural characteristics based on nativity, and immigration experiences between older Mexican, Puerto Rican, and Cuban Hispanics influence racial/ethnic and nativity disparities in chronic disease. Research examining the heterogeneity among older Hispanics may further our understanding of Hispanic health and shed light on whether any advantages/disadvantages exist among older men and women by nativity and country of origin. Recognizing the various sociocultural processes that underlie the health of older Hispanic subgroups is important for development and implementation of data-driven culture-appropriate interventions and targeted policies aimed at ameliorating the risks and negative health outcomes of late-life multi-morbidity among minority and immigrant groups. The findings from this study will be one of the first attempts in documenting the heterogeneity among older Hispanics by nativity, country of origin, and gender in life expectancies with morbidity and without morbidity.
Background
Most Hispanics in the United States have been found to have comparable or better health and mortality outcomes than whites despite low levels of education and income (Fenelon et al., 2017; Markides & Eschbach, 2005, 2011). This contradiction between the relative socioeconomic disadvantage and health of Hispanics vis-a-vis whites has been labeled the Hispanic paradox (Markides & Eschbach, 2011). Potential explanations for the observed health advantage among older Hispanics have been attributed to (a) selective migration: in-migration of healthy individuals and return migration of older Hispanics in poor health to their country of origin, which results in a healthier Hispanic population residing in the United States (Bostean, 2013; Markides & Eschbach, 2005); and (b) social and cultural factors among Hispanic immigrants associated with positive health behaviors (e.g., lower levels of smoking, and healthier diet) that promote health and longevity (Bostean, Ro, & Fleischer, 2017; Fenelon, 2013; Lariscy, Hummer, & Hayward, 2015; Riosmena, Kuhn, & Jochem, 2017). Though, research shows foreign-born Hispanics are more likely to engage in negative health behaviors such as smoking with increased duration in the United States which leads to the weakening of any immigrant health advantage (Fenelon, 2013; Lariscy et al., 2015). The role of migration selectivity, cultural factors, and health behaviors are important mechanisms in describing health and mortality outcomes among older Hispanics. However, the definitions and conceptual formations of these hypotheses are hard to test and rarely well specified (Treas & Gubernskaya, 2016). Moreover, these selection and protective mechanisms may not operate the same for different Hispanic subgroups or by gender.
For example, grouping the various social, demographic, economic, migratory, and health characteristics of U.S.-born Hispanic subgroups (i.e., U.S.-born Mexicans and U.S.-born Puerto Ricans) and foreign-born Hispanic subgroups (i.e., foreign-born Mexicans, island-born Puerto Ricans, and foreign-born Cubans) downplays important health differentials given the substantial heterogeneity that exists within the Hispanic population. Mounting evidence examining health among older Hispanics by nativity and country of origin indicates substantial variation in morbidity, disability, and mortality outcomes (Fenelon et al., 2017; Markides, Eschbach, Ray, & Peek, 2007; Melvin, Hummer, Elo, & Mehta, 2014; Garcia, Garcia, & Ailshire 2018; Sheftel, 2017; Zsembik & Fennell, 2005). Generally, it has been found that foreign-born Cubans and foreign-born Mexicans have better health profiles than whites (Markides et al., 2007; Palloni & Arias, 2004; Garcia, Garcia, & Ailshire, 2018). In contrast, island-born Puerto Ricans consistently report poorer health outcomes relative to whites (Garcia, Garcia, & Ailshire, 2018; Zsembik & Fennell, 2005). Although numerous studies document important health differences by nativity and country of origin, it is unclear whether lower mortality among certain Hispanic subgroups coincides with an increase in the length of life without morbidity.
While a clear advantage in mortality has been documented among older Hispanic subgroups, particularly the foreign-born (Fenelon et al., 2017), research examining health selectivity in morbidity life expectancies among older Hispanic subgroups are scarce. For example, Cantu and colleagues (2013) were the first to document morbidity life expectancies among older whites, blacks, U.S.-born Hispanics, and foreign-born Hispanics in the United States. Using NHIS data for 1997–2006, they found foreign-born Hispanics had the longest life expectancies at age 50 and spent more of their later years without a chronic condition compared with whites, regardless of gender. In addition, this study documented that U.S.-born Hispanics do not share the same health advantages of their foreign-born counterparts. While U.S.-born Hispanics’ life expectancy is comparable to that of whites, they spend more years with a chronic condition than foreign-born Hispanics and whites. Furthermore, this study showed the relationship between nativity and morbidity life expectancies varied by gender. Specifically, foreign-born Hispanic women were found to be the most advantaged in the number of years lived without morbidity, whereas U.S.-born Hispanic women were the most disadvantaged in the number of years lived with morbidity (Cantu et al., 2013). Although Cantu and colleagues differentiated between foreign-born and U.S.-born Hispanics, this study was limited to analyzing Hispanics as a pan-ethnic group.
More recent research by Garcia, Valderrama-Hinds, et al. (2017) assessed morbidity life expectancies among Mexican-origin adults aged 65 and older in the Southwestern United States. Consistent with Cantu and colleagues (2013), they found foreign-born respondents spend significantly more of their later years without a chronic condition compared with their U.S.-born counterparts, regardless of gender. In addition, this study established that the overall advantage among the foreign-born in life expectancies after age 65 without a chronic condition was stronger among women than men. Importantly, this association was found to vary by age of migration; mid-life migrant men (age 20–49) and late-life migrant women (those who migrated after age 50) were found to be the most advantaged among the foreign-born. The authors attributed these advantages to mid-life migrant men being selected in health characteristics, and late-life migrant women lacking health care access and underreporting chronic health conditions (Garcia, Valderrama-Hinds, et al., 2017).
Although these studies shed light on the importance of nativity in morbidity life expectancies, less is known on whether these findings extend to other Hispanic subgroups. For instance, an important limitation of these studies is that they were unable to assess the sociocultural heterogeneity among older Hispanic subgroups by nativity and country of origin. Researchers have argued that political and social acculturation and economic incorporation among immigrants play an important role in differential health outcomes in later life (Gubernskaya, Bean, & Van Hook, 2013; Treas & Gubernskaya, 2016). Research that focuses on health disparities by nativity neglects the diversity among older immigrant subgroups and paints an incomplete portrait of immigrant health (Fenelon et al., 2017; Treas & Gubernskaya, 2016). Brown, Donato, Laske, and Duncan (2013) emphasize the importance of identities as intersections of race/ethnicity, nativity, and other sociocultural factors that do not operate as independent stratification mechanisms, which shape an individuals’ lived experiences and health. Simultaneously considering race/ethnicity, nativity, and sociocultural influences, according to these authors, would result in a more theoretically informed, reliable, and valid understanding of health and a more targeted and culturally relevant approach to public health policy (Brown et al., 2013). By considering this form of intersectionality, an individual’s lived experience would be more accurately described (Brown, 2018; Moodley, 2000; Nadeem et al., 2007). Substantial differences in migratory experiences, poverty, education, health coverage, and health behaviors may contribute to racial/ethnic, nativity, and country of origin differentials in morbidity life expectancies among older Hispanic adults.
Drawing on this background, we developed the following hypotheses to guide our analyses: (a) foreign-born Mexicans (health selectivity) and foreign-born Cubans (higher socioeconomic status) will have a longer total life expectancy reflected by a lower burden of disease and island-born Puerto Ricans (no selectivity/poor socioeconomic status) will exhibit a longer total life expectancy reflected by a higher burden of late-life years with disease than their U.S.-born counterparts and whites; and (b) U.S.-born Mexicans and U.S.-born Puerto Ricans will have comparable total life expectancies as whites; reflected in a higher burden of late-life years with disease indicative of their minority status.
Method
Data
This study used data from the National Health Interview Survey (NHIS), an annual household interview survey of the noninstitutionalized civilian population conducted by the National Center for Health Statistics. Data are pooled across 17 years (1999–2015) to obtain a large sample of Hispanic subgroups by nativity and country of origin. The annual response rate of the NHIS is approximately 80% of eligible households. The data were downloaded from the Integrated Health Interview Series (IHIS). The IHIS contains harmonized variables from the NHIS from 1963 to the present, as well as provides appropriate weights for the complex survey design. In addition, data from the public use National Health Interview Survey Linked Mortality Files (NHIS-LMF) are used to estimate mortality. The NHIS-LMF provides mortality follow-up from the National Death Index through December 31, 2011.
The difference in observation periods for the prevalence of morbidity and incidence of mortality stems from the need to draw on the most complete information available to obtain reliable estimates. We do not have mortality estimates from 2012 to 2015 as the NHIS-LMF only provides mortality information up to 2011. Although estimates of prevalence can be obtained for the same year range (i.e., 1999–2011) of available mortality information, we adopt an approach used in previous research examining older Hispanic adult life expectancies with NHIS-LMF data and use all available prevalence information (up to 2015) to provide robust estimates for refined subgroups of the population (Cantu et al., 2013; Hayward, Hummer, Chiu, González-González, & Wong, 2014). Therefore, we use the maximum information for mortality (1999–2011) and prevalence (1999–2015). The final analytic sample includes 170,949 unique individuals that contribute 1,546,813 person-years.
Measures
In this study, we focused on the occurrence of at least one of four self-reported chronic conditions: heart disease, diabetes, cancer (excluding skin cancer), and stroke—that are among the leading causes of mortality in the United States (Murphy, Xu, Kochanek, Curtin, & Arias, 2017). Respondents were asked, “Has a doctor ever told you that you have (had a) [condition].” Respondents who reported having any of the four chronic conditions were classified as having morbidity (1 = has morbidity, 0 = has no morbidity). Hypertension and arthritis are excluded from our summary measure due to its high prevalence among older U.S. adults (Chiu, Hayward, & Saito, 2016; Helmick et al., 2008; Ong, Cheung, Man, Lau, & Lam, 2007), and also so that we can compare our findings to previous research on morbidity life expectancies among older Hispanic populations (Cantu et al., 2013; Garcia, Valderrama-Hinds, et al., 2017).
Sociodemographic Characteristics
National-level data allows us to examine the three largest Hispanic subgroups in the United States: Mexicans, Puerto Ricans, and Cubans. Respondents are classified based on self-reported race/ethnicity, birthplace information, and country of origin, which include: U.S.-born Mexicans, foreign-born Mexicans, U.S.-born Puerto Ricans, island-born Puerto Ricans, foreign-born Cubans, and whites. Respondents were categorized as being U.S.-born if they were born in one of the 50 states in the United States, and foreign-born if born outside the United States, including its territories (i.e., Puerto Rico). U.S.-born Cubans, Dominicans, and Central/South Americans are excluded due to small cell sizes. Gender is coded 1 = female and 0 = male. Age is a continuous variable.
In addition, we include several sociocultural variables for our descriptive analysis that may contribute to differentials in morbidity and mortality outcomes among older Hispanic subgroups: Marital status, coded 1 = married and 0 = not married. Language of interview was assessed by whether the interview was conducted in English or Spanish. Education is measured by years of formal school completed. Poverty is determined using the income-to-poverty ratio that represents the ratio of total household income to the official poverty thresholds established by the U.S. Census Bureau (2014). Respondents with ratios less than 1.00 were coded as living below poverty. Health insurance status is determined by respondent reports of health care coverage (Medicare, Medicaid, private, military). Smoking status is determined by whether the respondent reported they ever smoked or are currently smoking. Drinking status is determined by whether the respondent reported they ever drank or are currently drinking, and obesity is measured as having a body mass index (BMI) equal to 30 kg/m2 or above.
Statistical Analyses
In the descriptive analysis, we provide an overview of sociodemographic characteristics by race/ethnicity, nativity, country of origin, and gender. F-tests for continuous variables and chi-squared tests for categorical variables were used to compare differences across groups. Statistical significance was assessed at α = 0.05. Although these measures are not included in our life expectancy analyses, we include them to highlight sociocultural differences that have been shown to contribute to morbidity and mortality differentials among older Hispanic subgroups by nativity, country of origin, and gender (Fenelon et al., 2017; Lariscy et al., 2015; Zsembik & Fennell, 2005).
The construct of Sullivan Health Expectancy refers to the number of years an individual can expect to live in good health or absent of a particular health condition (Jagger, Van Oyen, & Robine, 2014), in this case, morbidity. Sullivan health expectancies are increasingly used as a policy tool and have provided results for populations in more than 50 countries worldwide (Jagger & Robine, 2011; Jagger et al., 2013). This method is particularly appealing to compare across population groups at the same point of time despite any differences in age distributions as this approach takes into account age-specific prevalence of health conditions and age-specific mortality risks (Jagger et al., 2014). Thus, the interpretation for morbidity life expectancies calculated by this method is the average number of years (at ages 50 and 65) a population can expect to live with morbidity and without morbidity, if they were to experience the observed disease and mortality risks of the current cohorts in the group throughout the life course.
For our life expectancy analysis, we integrated information on age-specific morbidity prevalence from the NHIS with age-specific mortality information from the NHIS-LMF to calculate Sullivan life table models of life expectancy with morbidity and without morbidity, for each race/ethnic, nativity, and country of origin group by gender (Sullivan, 1971). The prevalence is estimated with multinomial logistic regression models and sampling weights provided by NHIS. We estimate mortality rates with Gompertz hazard models and sampling weights from the NHIS-LMF. A weighted bootstrapping technique was used to obtain standard errors which allowed us to estimate sampling variability for the life expectancies. Confidence intervals were obtained for the life expectancy functions based on 300 bootstrap samples for each group.
Results
Descriptive Statistics
Sample characteristics are shown in Table 1 by race/ethnicity, nativity, country of origin, and gender. Among the Hispanic subgroups in the analysis, U.S.-born Mexicans comprise 36% of the sample. Foreign-born Mexicans are the next largest (35%), followed by island-born Puerto Ricans (13%), foreign-born Cubans (12%), and U.S.-born Puerto Ricans (4%). For both men and women, all Hispanic subgroups (except for foreign-born Cubans) tended to be younger and were less likely to be married (apart from foreign-born Mexicans) than whites. Foreign-born Hispanic subgroups were more likely to have taken the interview in Spanish compared with their U.S.-born co-ethnics, with foreign-born Cubans (68.5%–75.5%) and U.S.-born Mexicans and foreign-born Mexicans (64.9%–67.9%) having the highest proportions. All Hispanic subgroups reported less education and greater poverty than whites. However, education and poverty levels varied significantly by nativity and country of origin. For instance, foreign-born Mexicans and island-born Puerto Ricans reported lower levels of education and higher poverty compared with other Hispanic subgroups, whereas foreign-born Cubans exhibited more favorable socioeconomic conditions. Although most respondents reported health insurance coverage, foreign-born Mexicans reported lower rates compared with other groups. Except for foreign-born Cubans, all Hispanic subgroups were more obese than whites. Moreover, all Hispanic subgroups (apart from U.S.-born Puerto Ricans) reported lower rates of smoking and drinking than whites.
Table 1.
Sample Characteristics by Race/Ethnicity, Nativity, Country of Origin, and Gender, NHIS 1999–2015
| White | US Mexican | FB Mexican | US Puerto Rican | IB Puerto Rican | FB Cuban | |
|---|---|---|---|---|---|---|
| Panel A: Females | ||||||
| Age (SD)a | 66.3 (10.9) | 64.2 (10.3) | 62.3 (9.6) | 58.4 (8.2) | 65.0 (9.5) | 68.2 (10.2) |
| Marital statusa | 43.2 | 39.4 | 47.7 | 35.5 | 29.8 | 37.7 |
| Spanish interviewa | — | 11.0 | 67.9 | 10.7 | 39.7 | 75.5 |
| Education (SD) | 13.5 (1.8) | 11.7 (3.4) | 8.2 (4.3) | 13.2 (2.1) | 10.9 (3.8) | 11.6 (3.5) |
| Below povertya | 9.5 | 20.0 | 32.8 | 21.2 | 37.8 | 28.2 |
| Insurancea | 95.1 | 89.5 | 72.0 | 90.9 | 93.5 | 89.3 |
| Obesea | 25.4 | 37.7 | 36.5 | 38.2 | 34.5 | 23.3 |
| Smoking: current/evera | 44.4 | 31.6 | 19.4 | 46.1 | 27.6 | 23.8 |
| Drinking: current/evera | 72.7 | 61.9 | 39.9 | 69.5 | 46.9 | 43.9 |
| Any chronic conditiona | 34.0 | 37.6 | 34.3 | 28.4 | 41.3 | 27.7 |
| N | 86,463 | 3,947 | 3,676 | 391 | 1,474 | 1,362 |
| Panel B: Males | ||||||
| Age (SD)a | 64.4 (10.2) | 62.9 (9.6) | 61.0 (9.1) | 58.6 (8.1) | 64.6 (9.6) | 66.8 (10.4) |
| Marital statusa | 60.1 | 56.2 | 69.2 | 46.5 | 50.1 | 59.9 |
| Spanish interviewa | — | 7.9 | 64.9 | 9.1 | 30.8 | 68.5 |
| Education (SD) | 13.6 (2.0) | 12.2 (3.2) | 8.1 (4.3) | 13.4 (2.2) | 11.0 (3.6) | 12.0 (3.5) |
| Below povertya | 6.9 | 14.0 | 25.8 | 18.5 | 27.0 | 24.0 |
| Insurancea | 93.7 | 91.0 | 68.8 | 89.3 | 92.4 | 86.4 |
| Obesea | 27.5 | 32.5 | 29.1 | 34.9 | 26.4 | 22.5 |
| Smoking: current/evera | 61.8 | 59.4 | 48.0 | 62.7 | 55.3 | 50.4 |
| Drinking: current/evera | 87.6 | 86.5 | 79.8 | 90.2 | 79.3 | 71.7 |
| Any chronic conditiona | 39.0 | 39.7 | 30.4 | 36.3 | 41.4 | 35.3 |
| N | 65,439 | 2,841 | 3,081 | 320 | 940 | 1,015 |
Note: Unweighted Ns; weighted means and percentages.
aSignificantly different across groups at p < .05.
Compared with white females (34.0%), U.S.-born Mexicans (37.6%), foreign-born Mexicans (34.3%), and island-born Puerto Ricans (41.3%) were more likely to report having a chronic condition, whereas U.S.-born Puerto Ricans (28.4%) and foreign-born Cubans (27.7%) were less likely to report a chronic condition. Among males, U.S.-born Mexicans (39.7%) and island-born Puerto Ricans (41.4%) were more likely to report having a chronic condition than whites (39.0%), whereas foreign-born Mexicans (30.4%), U.S.-born Puerto Ricans (36.3%), and foreign-born Cubans (35.3%) were less likely to report having a chronic condition.
Morbidity Life Expectancies
Tables 2 and 3 present morbidity life expectancies for two age groups (50+ and 65+) for men and women by race/ethnicity, nativity, and country of origin. In general, females had longer life expectancies than their male counterparts (with the exception of U.S.-born Puerto Ricans). Note our total life expectancies for white women at age 50 (34.1 years), and age 65 (21.2 years) are slightly higher than 2014 life expectancies reported for the same age groups in the National Vital Statistics Reports (33.4 and 20.6 years, respectively; Arias et al., 2017). Our estimates for white men are within 0.1 years in both age groups. The National Vital Statistics Reports does not differentiate Hispanics by nativity or country of origin, however, our estimates for Hispanic subgroups closely approximate the life expectancies reported for Hispanic men and women. Differences between the current analysis and those using vital statistics data may be due in part to the exclusion of institutionalized adults in the NHIS.
Table 2.
Morbidity Life Expectancies Among Women at Ages 50 and 65 by Race/Ethnicity, Nativity, and Country of Origin, NHIS 1999–2015
| Whites | US Mexican | FB Mexican | US Puerto Rican | IB Puerto Rican | FB Cuban | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Years | (SE) | Years | (SE) | p | Years | (SE) | p | Years | (SE) | p | Years | (SE) | p | Years | (SE) | p | |
| Age 50+ | |||||||||||||||||
| TLE | 34.1 | 0.09 | 34.7 | 0.45 | 36.5 | 0.78 | * | 33.6 | 1.86 | 37.5 | 1.25 | * | 36.7 | 0.61 | * | ||
| LE without morbidity | 21.9 | 0.07 | 20.4 | 0.33 | * | 21.2 | 0.46 | 20.3 | 1.45 | * | 20.6 | 0.81 | 26.1 | 0.56 | * | ||
| LE with morbidity | 12.3 | 0.07 | 14.3 | 0.39 | * | 15.4 | 0.69 | * | 13.3 | 1.64 | 16.9 | 0.95 | * | 10.6 | 0.52 | * | |
| Ratio LE without morbidity | 0.64 | 0.01 | 0.59 | 0.01 | * | 0.58 | 0.01 | * | 0.60 | 0.04 | * | 0.55 | 0.02 | * | 0.71 | 0.02 | * |
| Age 65+ | |||||||||||||||||
| TLE | 21.2 | 0.08 | 21.7 | 0.39 | 23.7 | 0.74 | * | 21.0 | 3.11 | 25.1 | 1.38 | * | 23.0 | 0.60 | * | ||
| LE without morbidity | 11.9 | 0.06 | 11.6 | 0.35 | 12.7 | 0.54 | 10.0 | 1.32 | * | 13.3 | 0.93 | 14.7 | 0.51 | * | |||
| LE with morbidity | 9.3 | 0.06 | 10.1 | 0.38 | * | 11.0 | 0.63 | * | 11.0 | 1.88 | 11.8 | 0.99 | * | 8.3 | 0.49 | * | |
| Ratio LE without morbidity | 0.56 | 0.01 | 0.53 | 0.01 | * | 0.53 | 0.02 | * | 0.48 | 0.06 | * | 0.53 | 0.03 | * | 0.64 | 0.02 | * |
Note: FB = foreign-born; IB = island-born; LE = life expectancy; SE = standard error; TLE = total life expectancy.
*Significant at p < .05.
Table 3.
Morbidity Life Expectancies among Men at Ages 50 and 65 by Race/Ethnicity, Nativity, and Country of Origin, NHIS 1999–2015.
| Whites | US Mexican | FB Mexican | US Puerto Rican | IB Puerto Rican | FB Cuban | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Years | (SE) | Years | (SE) | p | Years | (SE) | p | Years | (SE) | p | Years | (SE) | p | Years | (SE) | p | |
| Age 50+ | |||||||||||||||||
| TLE | 30.0 | 0.09 | 30.3 | 0.45 | 33.2 | 0.72 | * | 35.2 | 4.43 | * | 28.7 | 0.81 | 30.7 | 0.63 | |||
| LE without morbidity | 17.4 | 0.07 | 16.8 | 0.34 | 19.8 | 0.48 | * | 15.6 | 1.34 | * | 15.9 | 0.56 | * | 19.8 | 0.55 | * | |
| LE with morbidity | 12.7 | 0.08 | 13.5 | 0.41 | 13.4 | 0.63 | 19.6 | 4.15 | * | 12.8 | 0.68 | 10.9 | 0.58 | * | |||
| Ratio LE without morbidity | 0.58 | 0.01 | 0.55 | 0.01 | 0.60 | 0.02 | 0.45 | 0.05 | * | 0.55 | 0.02 | 0.65 | 0.02 | * | |||
| Age 65+ | |||||||||||||||||
| TLE | 17.9 | 0.07 | 19.0 | 0.46 | * | 21.7 | 0.83 | * | 21.6 | 3.33 | * | 17.7 | 0.99 | 18.4 | 0.55 | ||
| LE without morbidity | 8.1 | 0.06 | 9.2 | 0.38 | * | 11.1 | 0.52 | * | 6.9 | 1.64 | * | 7.7 | 0.54 | 10.0 | 0.45 | * | |
| LE with morbidity | 9.8 | 0.07 | 9.8 | 0.38 | 10.6 | 0.72 | 14.7 | 3.19 | * | 10.0 | 0.82 | 8.4 | 0.50 | * | |||
| Ratio LE without morbidity | 0.45 | 0.01 | 0.48 | 0.02 | * | 0.51 | 0.02 | * | 0.32 | 0.07 | * | 0.44 | 0.03 | 0.55 | 0.02 | * | |
Note: Significant at p < .05. TLE = Total life expectancy. LE = Life expectancy. SE = Standard error. FB = Foreign-born. IB = Island-born.
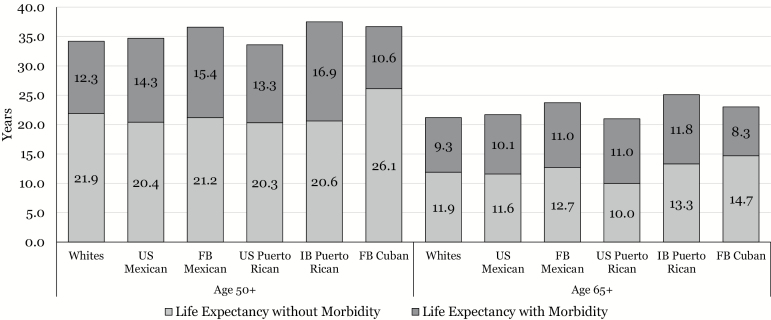
Among women (Table 2), foreign-born Mexicans (36.5 years), island-born Puerto Ricans (37.5 years), and foreign-born Cubans (36.7 years) had longer total life expectancies at age 50 than whites (34.1 years); whereas U.S.-born Mexican (34.7 years) and U.S.-born Puerto Rican (33.6 years) women had comparable total life expectancies at age 50 to white women. A similar pattern is observed for total life expectancies among women 65 years and older. In addition, results indicate that older female Hispanic subgroups are heterogeneous in morbidity life expectancies (Figure 1). At age 50, U.S.-born Mexicans and U.S.-born Puerto Ricans spend significantly fewer years without morbidity than whites (20.4 years, and 20.3 years vs 21.9 years). Conversely, foreign-born Cuban women can expect to live an additional 4.2 years without morbidity compared with white women. Furthermore, U.S.-born Mexicans, foreign-born Mexicans, and island-born Puerto Ricans spent more years after age 50 with morbidity (14.3, 15.4, and 16.9 years), compared with white women (12.3 years), whereas foreign-born Cuban women (10.6 years) spend significantly less years with a chronic condition. Island-born Puerto Rican women were the most disadvantaged among Hispanic subgroups in the total years with morbidity. In contrast, foreign-born Cuban women exhibit more favorable morbidity life expectancies among all race/ethnic, nativity, and country of origin groups. The above morbidity life expectancy patterns largely remain the same for women 65 years and older with the exception of U.S.-born Mexican women no longer significantly differing from white women in years lived without morbidity.
Figure 1.
Estimated years of life expectancy at ages 50 and 65 with and without morbidity among women by race/ethnicity, nativity, and country of origin, NHIS 1999–2015.
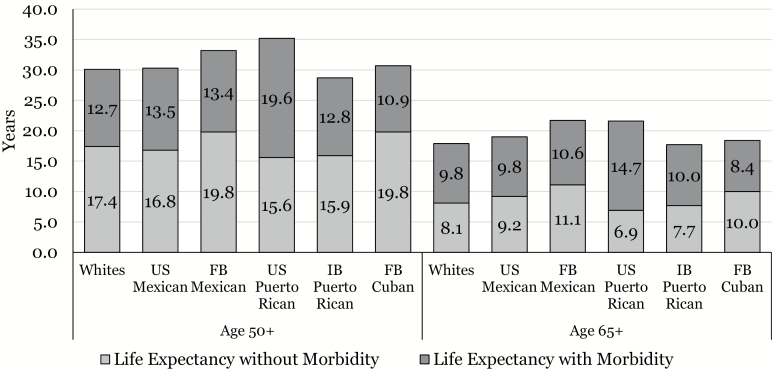
Among men (Table 3), foreign-born Mexicans (33.2 years) and U.S.-born Puerto Ricans (35.2 years) had longer total life expectancies than whites (30.0 years). U.S.-born Mexican (30.3 years), island-born Puerto Rican (28.7 years), and foreign-born Cuban (30.7 years) men did not differ from white men in total life expectancy. A similar pattern is observed for total life expectancies at ages 65 and older with the exception of U.S.-born Mexicans exhibiting a slight longevity advantage relative to whites (19.0 years vs 17.9 years).
Furthermore, the results indicate at age 50, foreign-born Mexicans and foreign-born Cubans can expect to spend 2.4 years more than whites without a chronic condition (19.8 years vs 17.4 years), whereas U.S.-born Puerto Ricans (15.6 years) and island-born Puerto Ricans (15.9 years) spend significantly less years without morbidity than whites (Figure 2). In contrast, U.S.-born Mexicans do not differ from whites in the number of years after age 50 without morbidity. However, island-born Puerto Rican men spend significantly more years with morbidity than whites (19.6 years vs 12.7 years), and foreign-born Cubans (10.9 years) spend significantly less years with morbidity than whites. In addition, U.S.-born Mexicans, foreign-born Mexicans, and island-born Puerto Ricans had comparable life expectancies with morbidity as whites. Similar to women, foreign-born Cuban men spend the largest proportion of their remaining late-life years without a morbidity relative to whites and other Hispanic subgroups. In contrast, U.S. Puerto Rican men are the most disadvantaged among all race/ethnic, nativity, and country of origin groups in the proportion of late life spent with morbidity. Finally, the above patterns in morbidity life expectancy largely remain the same for men aged 65 years and older with the exception of U.S.-born Mexican men exhibiting a significant advantage in years lived without morbidity relative to white men (9.2 years vs 8.1 years), and the proportion of late-life years without morbidity.
Figure 2.
Estimated years of life expectancy at ages 50 and 65 with and without morbidity among men by race/ethnicity, nativity, and country of origin, NHIS 1999–2015.
Discussion
Race/ethnicity, nativity, and country of origin differences in morbidity life expectancies among older adults are crucial as they highlight the effects of inequalities in social status, economic opportunity, and process of achieving U.S. citizenship, which are shaped by intersections of various aspects of identity and migratory experiences (Brown et al., 2013, 2018). The rationale underlying the current analysis is that variation in sociocultural characteristics within the Hispanic population by nativity, and country of origin is often overlooked in health research and public health discourse. Mexican-origin individuals account for nearly two thirds of Hispanics residing in the United States, and as a result, many inferences on the Hispanic population are disproportionately impacted by their numbers. When viewed as a monolithic group, conclusions about longevity and health outcomes for older Hispanics can lead to an inaccurate depiction of the Hispanic paradox by disregarding important nativity and country of origin differences that may help explain differential chronic disease risk profiles among Hispanic subgroups.
Consistent with previous research, we find foreign-born Hispanic women have longer total life expectancies compared with white and U.S.-born Hispanic women (Cantu et al., 2013; Garcia, Downer, et al., 2017). For men, we found the foreign-born Hispanic advantage that has been documented in longevity is largely driven by immigrants from Mexico. Contrary to the healthy immigrant effect, neither island-born Puerto Rican nor foreign-born Cuban men exhibited longer total life expectancies relative to white men.
However, extended longevity among foreign-born Hispanic subgroups does not necessarily coincide with better health in late life. In fact, our first hypothesis received mixed support. Among women, we find that foreign-born Mexicans and island-born Puerto Ricans exhibit no health selectivity in morbidity life expectancies. Foreign-born Mexican and island-born Puerto Rican women not only spend a greater number of years, but also a larger proportion of their remaining life with the disease than white women. Thus, their additional years of longevity relative to whites are accompanied with an increased burden of disease. Conversely, foreign-born Cuban women exhibited an advantage in life expectancies with morbidity, without morbidity, and the proportion of life without morbidity relative to whites. While Cuban women do not experience a longevity advantage relative to whites, they are clearly selected in healthier morbidity life expectancies reflected by a lower burden of disease.
Among men, older foreign-born Mexicans exhibited an immigrant advantage in the number of late-life years without morbidity. Thus, extended longevity for foreign-born Mexican men relative to whites is accompanied with a lower burden of disease, which is consistent with the Hispanic paradox. Researchers have proposed that the health advantage in morbidly life expectancy among foreign-born Mexican men may be attributed to health selection at time of migration (Garcia, Valderrama-Hinds, et al., 2017). Similar to women, foreign-born Cuban men experience comparable longevity profiles to white men and exhibit healthier morbidity life expectancies reflected in a lower burden of disease. Conversely, island-born Puerto Rican men did not substantially differ from white men in morbidity life expectancies, with the exception of a lower number of years spent without morbidity in midlife.
We also find partial support for our second hypothesis. U.S.-born Mexican and U.S.-born Puerto Rican women have morbidity life expectancies more indicative of their minority status and spend a larger proportion of their remaining years with chronic morbidity compared with whites. For men, U.S.-born Puerto Ricans exhibit a longevity advantage relative to whites, however, they spend significantly less years without morbidity, more years with morbidity, and a larger proportion of later life with the disease than other groups. This finding is consistent with research showing U.S.-born Puerto Ricans exhibit a higher prevalence of disease than whites and other Hispanic subgroups (Garcia, Garcia, & Ailshire, 2018). Conversely, our results indicate U.S.-born Mexican men have comparable morbidity life expectancies as white men. This finding is consistent with previous research (Cantu et al., 2013), and may be partially attributed to lower levels of poverty relative to other Hispanic subgroups.
Differing socioeconomic, migratory, cultural, and behavioral experiences have lasting effects that accumulate across the life course, which may contribute to health disparities and poor quality of life among aging Hispanics (Brown, 2018; Ferraro, Kemp, & Williams, 2017). Particularly, differences in nativity and country of origin among older immigrants have been found to be an important factor that affects morbidity and mortality outcomes of Hispanics (Fenelon et al., 2017; Garcia, Garcia, & Ailshire, 2018; Zsembik & Fennell, 2005). Older immigrants from less economically developed countries have lower levels of education that lead to conspicuous disadvantages in gaining employment in occupations with higher earnings, access to health insurance, and other benefits that promote better health in late life (Burr, Gerst, Kwan, & Mutchler, 2008). Furthermore, structural circumstances that influence the migratory process play a key role in the health of older immigrants. For instance, island-born Puerto Ricans are U.S. citizens, which allow them to travel freely from the island to the U.S. mainland (Duany, 2011). Similarly, foreign-born Cubans have benefited from political status as refugees that grant them U.S. citizenship (Van Hook, Glick, & Bean, 1999). As such, these immigrants may be less selected on longevity compared with other Hispanic groups.
The current study’s findings should be viewed in light of several limitations. This analysis pooled 17 years of data to obtain a large sample of Hispanic subgroups by nativity and country of origin. The benefit of a pooled sample is to use all the available data to increase the reliability and precision of estimates. However, in pooling data, an assumption is made that population differences are stable across survey years. Although individual-level characteristics may vary across cohorts, the amount of variation is likely small over the study period. In addition, this study used linked NHIS-NDI records to obtain information on deaths, which may be less accurate for foreign-born Hispanics since data is based on Social Security numbers.
Undocumented Hispanics in the United States do not have Social Security numbers, which may lead to more foreign-born Hispanic deaths being unmatched. However, death matches for Hispanics using the linked NHIS-NDI data have been found to be highly accurate (Lariscy, 2011; Lariscy et al., 2015). Thus, any bias due to this type of missing information is less likely among the cohort of adults aged 50 and older in the NHIS. Furthermore, information on the prevalence of morbidity was based on self-reports of diagnosis by health professionals. Evaluating morbidity using self-reports relies on an individual’s interaction with the health care system that may result in underestimates or undiagnosed diseases in Hispanic subgroups due to lower insurance rates, reduced health care access, differences in utilization/source of care, language, and cultural barriers (Morales, Lara, Kington, Valdez, & Escarce, 2002).
Despite these limitations, the current study represents an important contribution to knowledge on the complex patterns of race/ethnicity, nativity, and older adult health in the United States. By including a broad range of Hispanic subgroups, we document morbidity life expectancy profiles that are less apparent in research that focuses on Hispanics as a monolithic group. With a rapidly changing demographic profile, which includes a large number of aging Hispanics, it is essential that U.S. society implement social and health policies aimed at ameliorating the risks and negative health outcomes among the disadvantaged groups that we have documented. Researchers interested in Hispanic health should disaggregate pan-ethnic groupings to explicitly acknowledge differing migration experiences, sociopolitical histories, and cultural factors that may contribute to differences in late-life morbidity.
To better understand the causes and consequences of morbidity life expectancies among older Hispanics, we should consider intersectional race/ethnic, nativity, and country of origin identities to assess exposures to chronic disease throughout the life course (Brown, 2018; Ferraro et al., 2017). Reducing the health impact of late-life morbidity must be informed by a comprehensive understanding of the wide range of factors that shape health status. Not all community environments are created equal when it comes to opportunities for healthy living and interventions should be targeted toward specific Hispanic subgroups to address health disparities. An example informed by our findings and those of others is the need for implementing community-based lifestyle interventions and public health initiatives that promote and facilitate opportunities for walking and other physical activities and discourage food deserts in Hispanic-dense neighborhoods. Also, informed by our findings is the need to develop culturally appropriate community-based programs to help older Hispanics (particularly older Mexican Americans) to acquire education to effectively navigate the complex U.S. health care systems. Culture-appropriate interventions are considerate of and sensitive to unique cultural, social, historical, language, and experiential drivers of health in diverse populations (U.S. Department of Health and Human Services, 2008). Such programs might promote activities to improve health literacy, screening, prevention, and access to care for disadvantaged Hispanic subgroups.
Funding
This research work was supported by the Sealy Center on Aging at the University of Texas Medical Branch in Galveston and by the Health of Older Minorities (T32AG00270) training grant from the National Institute on Aging, the support of the Davis School of Gerontology at the University of Southern California, the Multidisciplinary Research Training in Gerontology Training Grant (T32AG000037) from the National Institutes of Health/National Institute on Aging, and the National Institute on Aging/National Institutes of Health (R36AG057949).
Conflict of Interest
The authors declare no conflict of interest.
References
- Arias E., Heron M., & Xu J (2017). United States life tables, 2014. National Vital Statistics Reports, 66, 1–64. [PubMed] [Google Scholar]
- Bostean G. (2013). Does selective migration explain the Hispanic paradox? A comparative analysis of Mexicans in the U.S. and Mexico. Journal of Immigrant and Minority Health, 15, 624–635. doi: 10.1007/s10903-012-9646-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostean G., Ro A., & Fleischer N. L (2017). Smoking trends among US Latinos, 1998–2013: The impact of immigrant arrival cohort. International Journal of Environmental Research and Public Health, 14, 255. doi:10.3390/ijerph14030255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T. N., Donato K. M., Laske M. T., & Duncan E. M (2013). Race, nativity, ethnicity, and cultural influences in the sociology of mental health. In Handbook of the sociology of mental health (pp. 255–276). Springer. [Google Scholar]
- Brown T. H. (2018). Racial stratification, immigration, and health inequality: A life course-intersectional approach. Social Forces. [Google Scholar]
- Burr J., Gerst K., Kwan N., & Mutchler J (2008). Economic well-being and welfare program participation among older immigrants in the United States. Generations, 32, 53–60. [Google Scholar]
- Cantu P. A., Hayward M. D., Hummer R. A., & Chiu C. T (2013). New estimates of racial/ethnic differences in life expectancy with chronic morbidity and functional loss: Evidence from the National Health Interview Survey. Journal of Cross-Cultural Gerontology, 28, 283–297. doi: 10.1007/s10823-013-9206-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu C. T., Hayward M., & Saito Y (2016). a comparison of educational differences on physical health, mortality, and healthy life expectancy in Japan and the United States. Journal of Aging and Health, 28, 1256–1278. doi: 10.1177/0898264316656505 [DOI] [PubMed] [Google Scholar]
- Crimmins E. M., & Beltrán-Sánchez H (2011). Mortality and morbidity trends: Is there compression of morbidity?The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66, 75–86. doi: 10.1093/geronb/gbq088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins E., Kim J. K., & Vasunilashorn S (2010). Biodemography: New approaches to understanding trends and differences in population health and mortality. Demography, 47, S41–S64. doi:10.1353/dem.2010.0005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins E. M., & Levine M. E (2016). Current status of research on trends in morbidity, healthy life expectancy, and the compression of morbidity. In Kaeberlein M, Martin G, eds.. Handbook of the biology of aging (8th ed, pp. 495–505). San Diego: Academic Press. [Google Scholar]
- Duany J. (2011). Blurred borders: Transnational migration between the Hispanic Caribbean and the United States. Chapel Hill: University of North Carolina Press. [Google Scholar]
- Fenelon A. (2013). Revisiting the Hispanic mortality advantage in the United States: The role of smoking. Social Science & Medicine (1982), 82, 1–9. doi: 10.1016/j.socscimed.2012.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon A., Chinn J. J., & Anderson R. N (2017). a comprehensive analysis of the mortality experience of Hispanic subgroups in the United States: Variation by age, country of origin, and nativity. SSM—Population Health, 3, 245–254. doi: 10.1016/j.ssmph.2017.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro K. F., Kemp B. R., & Williams M. M (2017). Diverse aging and health inequality by race and ethnicity. Innovation in Aging, 1(1), 1–11. doi:10.1093/geroni/igx002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores A. (2017). How the US Hispanic population is changing. Washington, DC: Pew Research Center. [Google Scholar]
- Garcia C., Garcia M. A., & Ailshire J. A (2018). Sociocultural variability in the Latino population: Age-patterns and differences in morbidity among older U.S. adults. Demographic Research, 38, 1605–1618. doi:10.4054/demres.2018.38.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M. A., Downer B., Chiu C.-T., Saenz J. L., Rote S., & Wong R (2017). Racial/ethnic and nativity differences in cognitive life expectancies among older adults in the United States. The Gerontologist. doi: 10.1093/geront/gnx142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M. A., Valderrama-Hinds L. M., Chiu C. T., Mutambudzi M. S., Chen N. W., & Raji M (2017). Age of migration life expectancy with functional limitations and morbidity in Mexican Americans. Journal of the American Geriatrics Society, 65, 1591–1596. doi: 10.1111/jgs.14875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubernskaya Z., Bean F. D., & Van Hook J (2013). (Un)healthy immigrant citizens: Naturalization and activity limitations in older age. Journal of Health and Social Behavior, 54, 427–443. doi: 10.1177/0022146513504760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward M. D., Hummer R. A., Chiu C. T., González-González C., & Wong R (2014). Does the Hispanic paradox in U.S. adult mortality extend to disability?Population Research and Policy Review, 33, 81–96. doi: 10.1007/s11113-013-9312-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmick C. G., Felson D. T., Lawrence R. C., Gabriel S., Hirsch R., Kwoh C. K.,…Stone J. H; National Arthritis Data Workgroup (2008). Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part i. Arthritis and Rheumatism, 58, 15–25. doi: 10.1002/art.23177 [DOI] [PubMed] [Google Scholar]
- Humes K., Jones N. A., & Ramirez R. R (2011). Overview of race and Hispanic origin, 2010. Washington, DC: U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau. [Google Scholar]
- Hummer R. A., & Hayward M. D (2015). Hispanic older adult health & longevity in the United States: Current patterns & concerns for the future. Daedalus, 144, 20–30. doi: 10.1162/DAED_a_00327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagger C., McKee M., Christensen K., Lagiewka K., Nusselder W., Van Oyen H.,…Robine J. M (2013). Mind the gap—Reaching the European target of a 2-year increase in healthy life years in the next decade. European Journal of Public Health, 23, 829–833. doi: 10.1093/eurpub/ckt030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagger C., & Robine J.-M (2011). Healthy life expectancy. In Rogers RG, Crimmins EM, eds. International handbook of adult mortality (pp. 551–568). Dordrecht: Springer. [Google Scholar]
- Jagger C., Van Oyen H., & Robine J.-M (2014). Health expectancy calculation by the Sullivan method: A practical guide. Newcastle upon Tyne, UK: Institute for Ageing, Newcastle University. [Google Scholar]
- Lariscy J. T. (2011). Differential record linkage by Hispanic ethnicity and age in linked mortality studies: Implications for the epidemiologic paradox. Journal of Aging and Health, 23, 1263–1284. doi: 10.1177/0898264311421369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lariscy J. T., Hummer R. A., & Hayward M. D (2015). Hispanic older adult mortality in the United States: New estimates and an assessment of factors shaping the Hispanic paradox. Demography, 52, 1–14. doi: 10.1007/s13524-014-0357-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides K. S., & Eschbach K (2005). Aging, migration, and mortality: Current status of research on the Hispanic paradox. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, 68–75. doi:10.1093/geronb/60.special_issue_2.s68 [DOI] [PubMed] [Google Scholar]
- Markides K. S., & Eschbach K (2011). Hispanic paradox in adult mortality in the United States. In Rogers RG, Crimmins EM, eds. International handbook of adult mortality (pp. 227–240). Dordrecht: Springer. [Google Scholar]
- Markides K. S., Eschbach K., Ray L. A., & Peek M. K (2007). Census disability rates among older people by race/ethnicity and type of Hispanic origin. In The health of aging Hispanics (pp. 26–39). Springer. [Google Scholar]
- Martin L. G., & Schoeni R. F (2014). Trends in disability and related chronic conditions among the forty-and-over population: 1997–2010. Disability and Health Journal, 7, S4–S14. doi: 10.1016/j.dhjo.2013.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mather M., Jacobsen L. A., & Pollard K. M (2015). Aging in the United States. Population Bulletin, 70(2), 1–18. [Google Scholar]
- Melvin J., Hummer R., Elo I., & Mehta N (2014). Age patterns of racial/ethnic/nativity differences in disability and physical functioning in the United States. Demographic Research, 31, 497–510. doi: 10.4054/DemRes.2014.31.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moodley R. (2000). Representation of subjective distress in black and ethnic minority patients: Constructing a research agenda. Counselling Psychology Quarterly, 13, 159–174. doi:10.1080/713658486 [Google Scholar]
- Morales L. S., Lara M., Kington R. S., Valdez R. O., & Escarce J. J (2002). Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. Journal of Health Care for the Poor and Underserved, 13, 477–503. doi:10.1353/hpu.2010.0630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy S. L., Xu J., Kochanek K. D., Curtin S. C., & Arias E (2017). Deaths: Final data for 2015. National Vital Statistics Reports, 66, 1–75. [PubMed] [Google Scholar]
- Nadeem E., Lange J. M., Edge D., Fongwa M., Belin T., & Miranda J (2007). Does stigma keep poor young immigrant and u.s.-born black and Latina women from seeking mental health care?Psychiatric Services (Washington, D.C.), 58, 1547–1554. doi: 10.1176/ps.2007.58.12.1547 [DOI] [PubMed] [Google Scholar]
- Ong K. L., Cheung B. M., Man Y. B., Lau C. P., & Lam K. S (2007). Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension (Dallas, Tex.: 1979), 49, 69–75. doi: 10.1161/01.HYP.0000252676.46043.18 [DOI] [PubMed] [Google Scholar]
- Palloni A., & Arias E (2004). Paradox lost: Explaining the Hispanic adult mortality advantage. Demography, 41, 385–415. doi:10.1353/dem.2004.0024 [DOI] [PubMed] [Google Scholar]
- Riosmena F., Kuhn R., & Jochem W. C (2017). Explaining the immigrant health advantage: Self-selection and protection in health-related factors among five major national-origin immigrant groups in the United States. Demography, 54, 175–200. doi: 10.1007/s13524-016-0542-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheftel M. G. (2017). Prevalence of disability among Hispanic immigrant populations: New evidence from the American community survey. Population Review, 56(1), 1–30. doi:10.1353/prv.2017.0000 [Google Scholar]
- Sullivan D. F. (1971). A single index of mortality and morbidity. HSMHA Health Reports, 86, 347–354. [PMC free article] [PubMed] [Google Scholar]
- Treas J., & Gubernskaya Z (2016). Immigration, aging, and the life course. In George L, Ferraro KF, eds. Handbook of Aging and the Social Sciences (8th ed, pp. 143–161). Amsterdam: Elsevier. [Google Scholar]
- U.S. Census Bureau (2014). Current population survey—Definitions and explanations. Retrieved on December 8, 2017, from http://www.census.gov/population/www/cps/cpsdef.html. [Google Scholar]
- U.S. Department of Health and Human Services (2008). The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: Recommendations for the framework and format of Healthy People 2020. Section IV. Advisory Committee findings and recommendations. Retrieved on April 8, 2018, from https://www.healthypeople.gov/sites/default/files/PhaseI_0.pdf. [Google Scholar]
- Van Hook J., Glick J. E., & Bean F. D (1999). Public assistance receipt among immigrants and natives: How the unit of analysis affects research findings. Demography, 36, 111–120. doi:10.2307/2648137 [PubMed] [Google Scholar]
- West L. A., Cole S., Goodkind D., & He W (2014). 65+ in the United States: 2010. Washington, DC: U.S. Census Bureau. [Google Scholar]
- Zsembik B. A., & Fennell D (2005). Ethnic variation in health and the determinants of health among Latinos. Social Science & Medicine (1982), 61, 53–63. doi: 10.1016/j.socscimed.2004.11.040 [DOI] [PubMed] [Google Scholar]