Abstract
Background and Objectives
Arts in medicine programs have emerged as a patient-centered approach that aims to improve health-related quality of life for patients in U.S. hospitals. Storytelling and poetry/monologue recitation are forms of arts-based experiences designed to enhance healing and are delivered by an artist-in-residence. We evaluated the effect of a storytelling/poetry experience on delirium screening scores and patient satisfaction in hospitalized older adults.
Research Design and Methods:
We conducted an observational pre–post study with a control group in the Acute Care for the Elders (ACE) unit at an academic medical center. A convenience sample of 50 participants was recruited to participate and complete two questionnaires measuring pain, anxiety, general well-being, and distress at hospital admission and at hospital discharge. Multivariable regression models were used to compare delirium screening score (primary outcome) between the control and intervention groups and to adjust for the differences in baseline characteristics between groups.
Results
At baseline participants in the intervention group were younger and had significantly lower cognitive impairment compared with those in the control group. Participants exposed to the storytelling/poetry intervention had a lower delirium screening score at hospital discharge compared with those in the control group. The result remained significant after adjusting for age, baseline cognitive impairment, and general well-being. Participants in the intervention group reported a high level of satisfaction with the interaction with the artist delivering the intervention.
Discussion and Implications
An artist in residence-delivered storytelling/poetry experience was associated with a lower delirium score at discharge in this pilot study. Further larger studies in diverse inpatient settings are needed to examine whether storytelling/poetry interventions or other types of arts in medicine programs can prevent or reduce delirium in hospitalized older adults.
Keywords: Alternative and complementary medicine/care/therapy, Quality of care, Delirium
Translational Significance
The results suggest that performing arts programs that include storytelling/poetry may be beneficial in the inpatient setting among certain geriatric populations.
Background and Objectives
Although advances have been made in the management of delirium (Ely et al., 2004), pain (Puntillo et al., 2001), anxiety, distress, and depression (Wilkinson et al., 2007) in hospitalized older patients, addressing these clinical issues, in older adults remains a challenge (Ahlers et al., 2008; Misra, & Ganzini, 2003; Puntillo et al., 2001; Rincon et al., 2001; Rotondi et al., 2002; Stolic & Mitchell, 2010). Arts in medicine programs have emerged as an adjunct form of support for patients that promotes a healing environment, facilitates the physical, mental, and emotional recovery of patients, and aims to improve patients’ quality of life through the management of pain, stress, anxiety, and depression (Lane & Graham-Pole, 1994; Rollins, Sonke, Cohen, Boles, & Li, 2009). According to a 2007 Joint Commission survey, nearly half of the 1,807 respondent healthcare institutions reported having arts programming (Rollins et al., 2009). Common types of bedside art programming include music, visual arts, drama, dance, literature, creative writing, and storytelling (Lane & Graham-Pole, 1994; Rollins et al., 2009). For example, music therapy has been recognized as a simple and inexpensive adjunct to pharmacologic treatment regimens in managing postoperative pain and anxiety (Allred, Byers, & Sole, 2010; Bonny, 1983) and can inhibit stress by reducing anxiety and pain (Almerud & Petersson, 2003; Chlan, Engeland, Anthony, & Guttormson, 2007; Nilsson, 2008; Twiss, Seaver, & McCaffrey, 2006) in intensive care units.
Arts-based interactions represent creative approaches to healing that can be categorized as either active (involving patient participation) or receptive (patient listens and observes) sessions that provide creative experiences and positive distractions (Warth et al., 2014). Storytelling is a form of arts experience designed to be delivered in both active and receptive sessions by artists in residence. Poetry/monologue recitations have also been included in performing arts programs. The artist in residence can tailor the type of session according to the individual patient’s physical and mental state. Despite anecdotal evidence of patients benefiting from storytelling/poetry sessions, few studies have examined whether exposure to this form of art programming influences patient outcomes. For example, in a study involving children with leukemia, a hypnotic trance through use of a child’s favorite story was found to be significantly more effective than a behavioral distraction and standard medical practice in alleviating distress, pain, and anxiety during bone marrow aspirations (Kuttner, 1988).
Delirium is common in hospitalized older adults (Ehlenbach et al., 2010) and is associated with poor outcomes including prolonged hospitalization, decreased cognitive and physical functioning, increased placement in long-term health care facilities and increased mortality (Campbell et al., 2009). Cognitive impairment is a major risk factor for delirium, and cognitively stimulating activities have been found efficacious in preventing delirium in hospitalized older patients (Inouye et al., 1999). In hospitalized patients, storytelling and/or poem/monologue recitations could reduce stress levels, increase pain tolerance, improve mood, and hasten recovery times (Rollins et al., 2009). Based on the need for an improved understanding of the effectiveness of performing arts programming in health care settings, the goals of our study was to evaluate the feasibility of a storytelling/poetry intervention among hospitalized older adults and to provide preliminary data on its effect on delirium and patient satisfaction in an inpatient setting. We hypothesized that exposure to our storytelling/poetry intervention will be associated with fewer cases and fewer symptoms of delirium.
Research Design and Methods
Study Design
This pilot study was conducted in the Acute Care for Elders (ACE) unit at the University of Alabama at Birmingham (UAB) between June and August 2016 and was approved by the local institutional review board. We used a pre–post design in which an intervention phase (storytelling intervention in addition to usual inpatient care) was followed by a control phase (usual inpatient care). The intervention phase was conducted between June and mid-July followed by the control phase between mid-July and August. During the study period, no other type of arts experience (e.g., music therapy, dance, textile therapy) was offered in the unit where the participants were hospitalized and recruited for this study. In addition, for the duration of the study, visits by hospital volunteers and pet therapy were not offered in the hospital unit where the study was performed.
Study Participants
Potential study participants were patients admitted to the ACE unit. Patients aged 65 years or older were recruited to be part of the intervention or control group using the same process that had been previously established in the ACE unit for utilization of storytelling by artists in residence as an adjunct modality for usual clinical care. Specifically, the ACE interdisciplinary clinical care team comprised of hospitalists, nurses, geriatrician/geriatrics nurse practitioners, chaplain, a social worker, a clinical pharmacist, and therapists considered if the patients might benefit from interacting with artists in residence during their daily interdisciplinary rounds. As per the predefined exclusion criteria, the interdisciplinary ACE team excluded patients admitted to the ACE unit who had severe agitation or delirium (i.e., anyone who required restraints, needed medications for their behaviors, or were so inattentive that they could not participate in the intervention or respond to questionnaires), those who refused to participate, or whose families declined participation. Each participant was given an information sheet describing the study and were asked to give a verbal agreement before receiving the study surveys and intervention. The unit clinical nurse coordinator obtained informed consent for participation verbally. Participation in the study was voluntary.
Storytelling/Poetry Intervention
Two artists in residence, who were part of UAB Hospital’s Institute for Arts in Medicine (AIM), delivered the bedside storytelling/poetry intervention. The AIM program, initiated in 2013, is a partnership between UAB Medicine and the UAB-affiliated performing arts center and aims to transform the health care environment and enhance healing and wellness for patients, visitors, and staff through creative arts experiences. Both artists in residence have more than 15 years of acting experience and have been trained to facilitate arts experiences in the health care environment. The artists visited the patients at the bedside for 15 minutes once during the hospital stay. At the beginning of their interaction with the patient, the artists in residence introduced themselves and asked if the patient would like to hear a story or poem. If the patient responded positively, the artist in residence asked the patient preference regarding the type of story or poem (e.g., religious, humorous, folktale, legend, myths, fairy tale) they would like to hear. Upon completion of the story/poem, the artist in residence asked the patient for feedback. The session was designed to be interactive, with the patient having the opportunity to reflect on the story or poem and share stories from his or her own life. An example of the intervention can be found at http://www.uab.edu/news/arts/item/6304-creative-approaches-to-healing-at-uab-s-institute-for-arts-in-medicine-inspire-patients-and-clinicians.
Baseline Data Collection
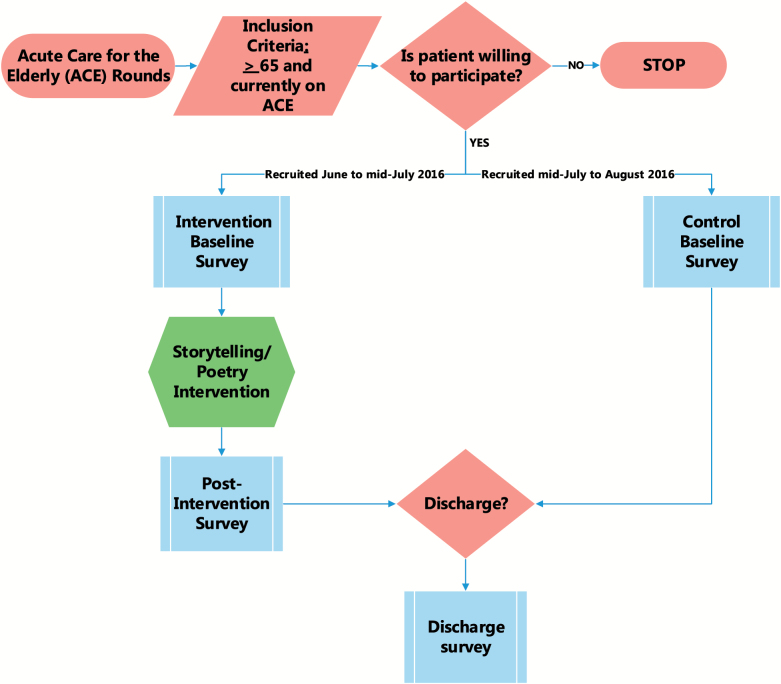
Demographic characteristics (age, sex, race/ethnicity), comorbidities, and insurance coverage were collected from the electronic health record for all participating patients. A baseline paper-based questionnaire (Figure 1) evaluated pain, anxiety, general well-being, and distress and was conducted on average 1–3 days after the admission and before the participants in the intervention group were exposed to storytelling/poem recitation. Pain (Gallagher, Bijur, Latimer, & Silver, 2002), anxiety (Facco et al., 2011), and general well-being (Warth, Keßler, Hillecke, & Bardenheuer, 2015) were assessed using visual analog scales (range 0–10, lower values are better). The level of distress/anxiety was assessed using the one-item subjective units of disturbance scale (SUDS) scored from 0 (no distress/totally relaxed) to 10 (highest distress/fear/anxiety/discomfort ever; Kim, Hwallip, & Yong, 2008; Wolpe, 1969). Nursing personnel, who were unaware of the patient’s participation in the study, assessed patients’ level of cognitive impairment and whether delirium was present, and recorded these data in the patient’s EHR during the first day of hospitalization and the day of discharge. Cognitive impairment was measured as part of the routine clinical using the Six-Item Screener (SIS; Callahan, Unverzagt, Hui, Perkins, & Hendrie, 2002). The participants were asked to recall three random words and to state the year, the month, and the day. The number of errors is added together for a score ranging from 0 (no cognitive impairment) to 6 (severe cognitive deficit; Callahan et al., 2002). The presence of delirium was assessed by clinical nurses according to the usual clinical protocol at our institution once per hospital shift using the Nurses Delirium Screening Scale (Nu-DESC, range 0–10; score ≥ 2 indicates delirium; Gaudreau, Gagnon, Harel, Tremblay, & Roy, 2005), which includes five symptom domains (scored from 0 to 2): disorientation, inappropriate behavior, inappropriate communication, illusions/hallucinations, and psychomotor retardation. Each domain was scored either 0 (no signs of item present), 1 (mild to moderate, barely expressed), or 2 (moderate to severe). The total score from the five domains was added together and a total score ≥2 represents positive screening for the presence of delirium. The first assessment of delirium occurred at admission to the ACE unit. Psychometric properties of SUDS, SIS, and Nu-DESC have been previously published (Callahan et al., 2002; Kim et al., 2008; van Velthuijsen et al., 2016). Of note, a validation study including hospitalized patients found that while Nu-DESC is a specific delirium detection tool, has lower sensitivity at the usually proposed cut-off point of ≥2 (Hargrave et al., 2017).
Figure 1.
Recruitment and study procedures for the evaluation of a storytelling/poetry intervention in hospitalized older adults study.
Outcomes and Follow-Up
We collected study outcomes for both intervention and control phase at the hospital discharge using paper-based questionnaires (Figure 1). The primary outcome of this study was delirium score as measured by the Nu-DESC scale (Gaudreau et al., 2005; Neufeld et al., 2013). Secondary outcomes were patient satisfaction with the physician, satisfaction with the nonclinical team and satisfaction with the artist in residence administering bedside story or poetry. Patient satisfaction outcomes were assessed using a 5-point Likert scale scored from 1 (strongly disagree) to 5 (strongly agree).
Similar to the baseline questionnaire, the follow-up questionnaires also included the same items evaluating the patient’s level of pain, anxiety, general well-being, and distress.
Statistical Analysis
We used descriptive statistics to compare participant characteristics between the intervention and control group. Means and standard deviations (SDs) were calculated for continuous variables, and frequencies and proportions were calculated for categorical variables. Differences in sociodemographic and clinical characteristics of between control and intervention group were examined using t-tests, chi-square tests, or Fisher’s exact tests, as appropriate.
In preliminary analyses, logistic regression models were used to compare the proportion of participants screening positive for delirium at discharge between the control and the intervention groups. The small sample size limited power to detect differences between the intervention and control groups in the proportion of participants that met Nu-DESC criteria ≥2. Thus for this pilot study, we decided to evaluate at the Nu-DESC score as a continuous variable to see if we could identify an effect of the intervention that might warrant further study after controlling for important confounders. Multivariable regression models were used to compare delirium screening score (primary outcome) between the control and intervention groups to adjust for the differences in baseline characteristics between groups. We used generalized linear models to evaluate the association between the exposure to the storytelling intervention and discharge Nu-DESC score or change in Nu-DESC score, respectively. In multivariable regression models, we included as covariates those baseline variables which were found at p <.10 to be associated with both the intervention and the primary outcome. We assessed for the presence of multicollinearity between cognitive impairment and Nu-DESC score at discharge. Paired t-tests were used to compare the pre–post measures of patient satisfaction. A p <.05 was the criterion for statistical significance. No adjustments for multiple comparisons were performed. All analyses were conducted in SAS (v9.3, Enterprise Guide v4.3, Cary, NC).
Results
A total of 50 patients, mostly women (64%) with a mean (SD) age of 81.2 (9.5) participated in the study. Compared with the control group, participants in the intervention group were slightly younger, 77 (8.7) years versus 85.4 (8.6) and had less cognitive impairment: SIS score of 1.05 (1.9) versus 2.6 (2.2). There was no significant difference between groups (intervention vs control group) in terms of sex, race, anxiety, pain, general well-being, distress, Charlson comorbidity index, and Nu-DESC score at baseline (Table 1). A total of seven (28%) participants in the control group and four (16%) in the intervention group had a Nu-DESC score ≥2 at hospital admission. At hospital discharge, five (20%) participants in the control group and one (4%) participant in the intervention group had a Nu-DESC score ≥2 and thus met criteria for delirium according to the Nu-DESC assessment (p = .18). On the day of discharge, the delirium screening score was significantly lower (less cognitive dysfunction) in the intervention group compared with the control group in univariable analysis (Table 2). However, there were no differences in the length of stay and measurements of anxiety, pain, general wellbeing, and distress at hospital discharge between the intervention and control group (Table 3). After adjustment for level of cognitive impairment, age, general wellbeing, and admission delirium score, exposure to the intervention remained independently associated with a significantly lower discharge delirium screening score (beta = 0.7 [0.17, 1.24], p = .01; Table 4, Model A). Since the duration of hospital stay was longer among those in the intervention group compared with the control group, we further adjusted for length of stay. However, the storytelling/poetry intervention remained independently associated with significantly lower delirium screening score at discharge (beta = 0.7 [0.15, 1.24], p = .01; Table 4, Model B). Similarly, after adjustment for level of cognition, age, and well-being, there was a borderline significant association between exposure to the intervention and decrease in delirium score between hospital admission and discharge (beta = 0.8 [−0.01, 1.6], p = .05).
Table 1.
Baseline Study Participant Characteristics by Treatment Group
| Characteristic | Intervention (N = 25) | Control (N = 25) | p Value |
|---|---|---|---|
| Age, mean (SD), years | 77 (8.7) | 85.4 (8.6) | .001 |
| Female, N (%) | 16 (64) | 16 (64) | 1.0 |
| White race, N (%) | 15 (60) | 12 (48) | .4 |
| Comorbidity index, mean (SD) | 6 (2.0) | 6.5 (1.7) | .4 |
| Insurance, N (%) | .1 | ||
| Medicare (FFS) | 12 (48) | 17 (68) | |
| Commercial | 13 (52) | 6 (24) | |
| Medicare advantage | 0 (0) | 2 (8) | |
| Anxiety,a mean (SD) | 4.1 (2.8) | 3.3 (3.5) | .40 |
| Pain,b mean (SD) | 3.7 (2.9) | 2.1 (2.9) | .06 |
| General well-being,c mean (SD) | 3.5 (2.7) | 3.2 (3.6) | .75 |
| Distress,d mean (SD) | 4.2 (3.0) | 3.0 (3.0) | .2 |
| Cognitive impairment,e mean (SD) | 1.1 (1.9) | 2.6 (2.2) | .01 |
| Nu-DESC score,f mean (SD) | 0.5 (1.0) | 0.9 (1.3) | .3 |
Note: FFS = fee for service; Nu-DESC = Nurses Delirium Screening Scale; SD = standard deviation.
aRange 0–10; 0 (very relaxed); 10 (very tense).
bRange 0–10; 0 (no pain); 10 (worst possible pain).
cRange 0–10; 0 (very good); 10 (very bad).
dRange 0–10; 0 (no distress/totally relaxed); 10 (highest distress/fear/anxiety).
eCognitive impairment measured using the Six-Item Screener (range 0–6).
fNu-DESC Nursing Delirium Screening Scale (range 0–10, score ≧ 2 indicates delirium).
Table 2.
Means and Standard Deviations of Nu-DESCa Score, and Participant Satisfaction with Physician, Nonphysician Team and Professional Artist at Hospital Discharge
| Outcomes | Intervention, N = 25 | Control, N = 25 | t test, p Value |
|---|---|---|---|
| Nu-DESC score | 0.2 (0.5) | 1.1 (1.3) | .0041 |
| Satisfied with doctor interaction | 4.1 (1.1) | 4.4 (0.8) | .3924 |
| Satisfied with nonphysician team | 4.5 (0.7) | 4.6 (0.6) | .6651 |
| Satisfied with artist | 4.8 (0.4) | N/A | N/A |
aNurses Delirium Screening Scale (Nu-DESC), range 0–10; score ≥ 2 indicates delirium.
Table 3.
Length of Stay, Anxiety, Pain, General Wellbeing, and Distress at Hospital Discharge
| Outcomes | Intervention, N = 25 | Control, N = 25 | p Value |
|---|---|---|---|
| Length of stay, median (IQR), days | 6 (6) | 4 (3) | .08 |
| Anxiety,a mean (SD) | 3.22 (2.8) | 2.1 (3.2) | .20 |
| Pain,b mean (SD) | 3.1 (2.9) | 2.6 (3.08) | .55 |
| General wellbeing,c mean (SD) | 2.3 (2.0) | 2.2 (2.3) | .88 |
| Distress,d mean (SD) | 2.6 (2.0) | 2.7 (3.0) | .90 |
Note: IQR = interquartile range; SD = standard deviation.
aRange 0–10; 0 (very relaxed); 10 (very tense).
bRange 0–10; 0 (no pain); 10 (worst possible pain).
cRange 0–10; 0 (very good); 10 (very bad).
dRange 0–10; 0 (no distress/totally relaxed); 10 (highest distress/fear/anxiety).
Table 4.
Factors Associated with Nu-DESC Score at Discharge
| Model A | Model B | |||||
|---|---|---|---|---|---|---|
| Characteristic | Estimate | 95% CI | p Value | Estimate | 95% CI | p Value |
| Storytelling/poetry intervention | 0.70 | 0.17 to 1.24 | .01 | 0.70 | 0.15 to 1.24 | .01 |
| Cognitive impairment | 0.13 | −0.02 to 0.28 | .08 | 0.13 | −0.02 to 0.28 | .08 |
| General well-being | 0.15 | 0.07 to 0.22 | .00 | 0.15 | 0.07 to 0.22 | .00 |
| Nu-DESC at hospital admission | 0.09 | −0.16 to 0.34 | .47 | 0.10 | −0.16 to 0.35 | .46 |
| Age | −0.01 | −0.04 to 0.01 | .31 | −0.01 | −0.04 to 0.01 | .31 |
| Length of stay | NA | NA | NA | 0.00 | −0.03 to 0.02 | .90 |
Note: NA = not applicable; Nu-DESC = Nurses Delirium Screening Scale.
Patients in the intervention group reported being satisfied with the artist encounter 4.9 (0.37) (Table 2). Compared with the participants assigned to the control group, there was no significant difference in the patient satisfaction with their physician or nonphysician team (Table 2).
Discussion and Implications
To our knowledge, this is the first study to evaluate the association between a bedside storytelling intervention delivered by artists in residence and changes in measures of cognitive dysfunction in hospitalized older adults. We found that exposure to a storytelling/poetry intervention was associated with improvement in Nu-DESC scores, after controlling for potential confounders including age, baseline cognitive impairment, level of distress, and general well-being. In addition, patient satisfaction with the bedside storytelling/poetry intervention was high.
Many hospitalized patients, especially the older adults, are at risk of developing delirium, a risk that is increased by the presence of cognitive, functional, visual and hearing impairment, depression, and other comorbidities. Delirium is precipitated by hospitalization related factors (e.g., medications, procedures, unfamiliar environment) and is associated with increased morbidity and mortality, longer hospital stays and substantial additional health care costs (Inouye, Westendorp, Saczynski, Kimchi, & Cleinman, 2014). There is a lack of strong evidence for pharmacologic therapies to prevent delirium, thus, nonpharmacologic modalities have the strongest evidence of benefit (Inouye et al., 1999). Such nonpharmacologic interventions have included music therapy, exercise, light, and sensory therapy as well as complementary alternative medicine modalities that have been evaluated with variable success (Inouye et al., 1999, 2014; Levy, Attias, Ben-Arye, Bloch, & Schiff, 2017).
Because stories can be used to discuss personal experiences and/or can provide a fantasy escape for the listeners (Rollins et al., 2009) arts programming using storytelling are increasingly encountered in the health care setting (Hanna, Rollins, & Lewis, 2017). However, the evidence supporting the benefits of storytelling/poetry on improving clinical outcomes is sparse, a gap that our study aimed to fill. Storytelling interventions exposing personal experiences with disease management have been shown to decrease blood pressure (Houston et al., 2011), and improve self-efficacy in adults with diabetes and hypertension (Bertera, 2014; Bokhour et al., 2016), while recounting a favorite story has been employed to help children deal with pain (Heiney, 1995; Kuttner, 1988). Storytelling interventions like the one we employed in the present study can provide hospitalized patients with cognitive stimulation and positive distractions from the monotony and stress associated with the hospital stay. Listening to a story provides an emotional experience which may uplift patients’ mood, relieve stress, promote wellness, and assist in the healing process (Buchanan, 2015). However, while storytelling interventions may reduce anxiety and improve pain tolerance in some populations (Hanna et al., 2017; Rollins et al., 2009), we did not replicate these results in our study. This could be due to the different characteristics of the participants enrolled in our study and that acutely sick elders may respond differently to storytelling compared with other groups, or to the small sample size employed by our pilot study.
Our study findings should be interpreted in the light of some limitations. Because our study was a pilot study with small sample size, we were able to adjust only for some potential confounders and the precision of our estimates of the association between our intervention and improved delirium scores upon discharge is limited. Participant recruitment in two phases, first in the intervention phase and then in the control phase, as we implemented in this study, rises the concern for temporal selection bias. However, this approach was chosen to prevent contamination bias, where the participants in the control group were inadvertently exposed to the storytelling/poetry intervention, which could minimize the difference in outcomes between the two groups. In addition, this was an observational study, and we did not employ “attention control” procedures in the control group, and thus we were not able to adequately control for the nonspecific effects of the intervention such as the time spent with the patient. The follow-up period for the study was short, and the long-term effects of exposure to the storytelling intervention were not studied. In addition, the timing of the intervention in regard to the day of discharge may have influenced the effect of our intervention on the delirium screening score at hospital discharge. Because we did not collect data on the timing of the daily Nu-DESC assessment in relation to the intervention, we could not evaluate whether our storytelling/poetry intervention influenced the daily Nu-DESC scores. Given the pilot nature of this study and that we did not record information on the participation rate, the generalizability of our findings is limited and larger studies are needed to confirm our results among hospitalized older individuals (Thabane et al., 2010).
In summary, in this pilot study, we evaluated the use and feasibility of an artist in residence-delivered storytelling/poetry program in older adults admitted to an Acute Care for Elderly unit. We found that the patients participating in the study had positive views about the interaction with the artist. Although our artist in residence-delivered storytelling/poetry experience was associated with lower delirium screening score at hospital discharge, further larger studies in diverse care settings are needed to examine whether storytelling interventions or other types of arts-based experiences in health care can prevent delirium in older adults. In addition, future research should focus evaluating whether it is the art experience itself or the patient–artist interacting about the art form that influences health outcomes.
Funding
This work was supported by an institutional grant. Dr. Danila was supported by NIH/NIAMS K23 AR062100.
Conflict of Interest
None reported.
Acknowledgments
We want to thank the artists in residence, Elizabeth Vander Kamp and David Roby and the Acute Care of Elders nurse coordinator, Terri D. Middlebrooks for their involvement in this study.
References
- Ahlers S. J., van Gulik L., van der Veen A. M., van Dongen H. P., Bruins P., Belitser S. V.,…Knibbe C. A (2008). Comparison of different pain scoring systems in critically ill patients in a general ICU. Critical Care (London, England), 12, R15. doi: 10.1186/cc6789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allred K. D., Byers J. F., & Sole M. L (2010). The effect of music on postoperative pain and anxiety. Pain Management Nursing, 11, 15–25. doi: 10.1016/j.pmn.2008.12.002 [DOI] [PubMed] [Google Scholar]
- Almerud S., & Petersson K (2003). Music therapy—A complementary treatment for mechanically ventilated intensive care patients. Intensive & Critical Care Nursing, 19, 21–30. doi:10.1016/S0964-3397(02)00118-0 [DOI] [PubMed] [Google Scholar]
- Bertera E. M. (2014). Storytelling slide shows to improve diabetes and high blood pressure knowledge and self-efficacy: Three-year results among community dwelling older African Americans. Educational Gerontology, 40, 785–800. doi:10.1080/03601277.2014.894381 [Google Scholar]
- Bokhour B. G., Fix G. M., Gordon H. S., Long J. A., DeLaughter K., Orner M. B.,…Houston T. K (2016). Can stories influence African-American patients’ intentions to change hypertension management behaviors? A randomized control trial. Patient Education and Counseling, 99, 1482–1488. doi: 10.1016/j.pec.2016.06.024 [DOI] [PubMed] [Google Scholar]
- Bonny H. (1983). Music listening for intensive coronary care units: A pilot project. Music Therapy, 3, 4–16. doi:10.1093/mt/3.1.4 [Google Scholar]
- Buchanan C. (2015 April). Creative approaches to healing inspire patients and clinicians. UAB Magazine. Retrieved on June 1, 2018, from http://www.uab.edu/uabmagazine/features/art-soul. [Google Scholar]
- Callahan C. M., Unverzagt F. W., Hui S. L., Perkins A. J., & Hendrie H. C (2002). Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care, 40, 771–781. doi: 10.1097/01.MLR.0000024610.33213.C8 [DOI] [PubMed] [Google Scholar]
- Campbell N., Boustani M. A., Ayub A., Fox G. C., Munger S. L., Ott C.,…Singh R (2009). Pharmacological management of delirium in hospitalized adults—A systematic evidence review. Journal of General Internal Medicine, 24, 848–853. doi: 10.1007/s11606-009-0996-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chlan L. L., Engeland W. C., Anthony A., & Guttormson J (2007). Influence of music on the stress response in patients receiving mechanical ventilatory support: A pilot study. American Journal of Critical Care, 16, 141–145. [PubMed] [Google Scholar]
- Ehlenbach W. J., Hough C. L., Crane P. K., Haneuse S. J., Carson S. S., Curtis J. R., & Larson E. B (2010). Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA, 303, 763–770. doi: 10.1001/jama.2010.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely E. W., Stephens R. K., Jackson J. C., Thomason J. W., Truman B., Gordon S.,…Bernard G. R (2004). Current opinions regarding the importance, diagnosis, and management of delirium in the intensive care unit: A survey of 912 healthcare professionals. Critical Care Medicine, 32, 106–112. doi: 10.1097/01.CCM.0000098033.94737.84 [DOI] [PubMed] [Google Scholar]
- Facco E., Zanette G., Favero L., Bacci C., Sivolella S., Cavallin F., & Manani G (2011). Toward the validation of visual analogue scale for anxiety. Anesthesia Progress, 58, 8–13. doi: 10.2344/0003-3006-58.1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher E. J., Bijur P. E., Latimer C., & Silver W (2002). Reliability and validity of a visual analog scale for acute abdominal pain in the ED. Am J Emerg Med 20, 287–290. doi:10.1053/ajem.2002.33778 [DOI] [PubMed] [Google Scholar]
- Gaudreau J. D., Gagnon P., Harel F., Tremblay A., & Roy M. A (2005). Fast, systematic, and continuous delirium assessment in hospitalized patients: The nursing delirium screening scale. Journal of Pain and Symptom Management, 29, 368–375. doi: 10.1016/j.jpainsymman.2004.07.009 [DOI] [PubMed] [Google Scholar]
- Hanna G., Rollins J., & Lewis L (2017). Arts in medicine literature review. Orlando, FL: Grantmakers in the Arts. [Google Scholar]
- Hargrave A., Bastiaens J., Bourgeois J. A., Neuhaus J., Josephson S. A., Chinn J.,…Douglas V (2017). Validation of a nurse-based delirium-screening tool for hospitalized patients. Psychosomatics, 58, 594–603. doi: 10.1016/j.psym.2017.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiney S. P. (1995). The healing power of story. Oncology Nursing Forum, 22, 899–904. [PubMed] [Google Scholar]
- Houston T. K., Allison J. J., Sussman M., Horn W., Holt C. L., Trobaugh J.,…Hullett S (2011). Culturally appropriate storytelling to improve blood pressure: A randomized trial. Annals of Internal Medicine, 154, 77–84. doi: 10.7326/0003-4819-154-2-201101180-00004 [DOI] [PubMed] [Google Scholar]
- Inouye S. K., Bogardus S. T. Jr., Charpentier P. A., Leo-Summers L., Acampora D., Holford T. R., & Cooney L. M. Jr (1999). A multicomponent intervention to prevent delirium in hospitalized older patients. The New England Journal of Medicine, 340, 669–676. doi: 10.1056/NEJM199903043400901 [DOI] [PubMed] [Google Scholar]
- Inouye S. K., Westendorp R. G., Saczynski J. S., Kimchi E. Y., & Cleinman A. A (2014). Delirium in elderly people—Authors’ reply. Lancet (London, England), 383, 2045. doi: 10.1016/S0140-6736(14)60994-6 [DOI] [PubMed] [Google Scholar]
- Kim D., Hwallip B., & Yong C. P (2008). Validity of the subjective units of disturbance scale in EMDR. Journal of EMDR Practice and Research, 2, 57–62. doi:10.1891/1933-3196.2.1.57 [Google Scholar]
- Kuttner L. (1988). Favorite stories: A hypnotic pain-reduction technique for children in acute pain. The American Journal of Clinical Hypnosis, 30, 289–295. doi: 10.1080/00029157.1988.10402752 [DOI] [PubMed] [Google Scholar]
- Lane M. T., & Graham-Pole J (1994). Development of an art program on a bone marrow transplant unit. Cancer Nursing, 17, 185–192. doi:10.1097/00002820-199406000-00002 [PubMed] [Google Scholar]
- Levy I., Attias S., Ben-Arye E., Bloch B., & Schiff E (2017). Complementary medicine for treatment of agitation and delirium in older persons: A systematic review and narrative synthesis. International Journal of Geriatric Psychiatry, 32, 492–508. doi: 10.1002/gps.4685 [DOI] [PubMed] [Google Scholar]
- Misra S., & Ganzini L (2003). Delirium, depression, and anxiety. Critical Care Clinics, 19, 771–787. doi:10.1016/S0749-0704(03)00048-4 [DOI] [PubMed] [Google Scholar]
- Neufeld K. J., Leoutsakos J. S., Sieber F. E., Joshi D., Wanamaker B. L., Rios-Robles J., & Needham D. M (2013). Evaluation of two delirium screening tools for detecting post-operative delirium in the elderly. British Journal of Anaesthesia, 111, 612–618. doi: 10.1093/bja/aet167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson U. (2008). The anxiety- and pain-reducing effects of music interventions: A systematic review. AORN Journal, 87, 780–807. doi: 10.1016/j.aorn.2007.09.013 [DOI] [PubMed] [Google Scholar]
- Puntillo K. A., White C., Morris A. B., Perdue S. T., Stanik-Hutt J., Thompson C. L., & Wild L. R (2001). Patients’ perceptions and responses to procedural pain: Results from thunder project II. American Journal of Critical Care, 10, 238–251. [PubMed] [Google Scholar]
- Rincon H. G., Granados M., Unutzer J., Gomez M., Duran R., Badiel M.,…Echeverri P (2001). Prevalence, detection and treatment of anxiety, depression, and delirium in the adult critical care unit. Psychosomatics, 42, 391–396. doi: 10.1176/appi.psy.42.5.391 [DOI] [PubMed] [Google Scholar]
- Rollins J., Sonke J., Cohen R., Boles A., & Li J (2009). State of the field report: Arts in Healthcare 2009. Washington, DC: Society for the Arts in Healthcare. [Google Scholar]
- Rotondi A. J., Chelluri L., Sirio C., Mendelsohn A., Schulz R., Belle S.,…Pinsky M. R (2002). Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Critical Care Medicine, 30, 746–752. doi:10.1097/00003246-200204000-00004 [DOI] [PubMed] [Google Scholar]
- Stolic S., & Mitchell M. L (2010). Pain management for patients in cardiac surgical intensive care units has not improved over time. Australian Critical Care, 23, 157–159. doi: 10.1016/j.aucc.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Thabane L., Ma J., Chu R., Cheng J., Ismaila A., Rios L. P.,…Goldsmith C. H (2010). A tutorial on pilot studies: The what, why and how. BMC Medical Research Methodology, 10, 1. doi: 10.1186/1471-2288-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twiss E., Seaver J., & McCaffrey R (2006). The effect of music listening on older adults undergoing cardiovascular surgery. Nursing in Critical Care, 11, 224–231. doi:10.1111/j.1478-5153.2006.00174 [DOI] [PubMed] [Google Scholar]
- van Velthuijsen E. L., Zwakhalen S. M., Warnier R. M., Mulder W. J., Verhey F. R., & Kempen G. I (2016). Psychometric properties and feasibility of instruments for the detection of delirium in older hospitalized patients: A systematic review. International Journal of Geriatric Psychiatry, 31, 974–989. doi: 10.1002/gps.4441 [DOI] [PubMed] [Google Scholar]
- Warth M., Keßler J., Hillecke T. K., & Bardenheuer H. J (2015). Music therapy in palliative care. Deutsches Arzteblatt International, 112, 788–794. doi: 10.3238/arztebl.2015.0788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warth M., Kessler J., Koenig J., Wormit A. F., Hillecke T. K., & Bardenheuer H. J (2014). Music therapy to promote psychological and physiological relaxation in palliative care patients: Protocol of a randomized controlled trial. BMC Palliative Care, 13, 60. doi: 10.1186/1472-684X-13-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson S. M., Love S. B., Westcombe A. M., Gambles M. A., Burgess C. C., Cargill A.,…Ramirez A. J (2007). Effectiveness of aromatherapy massage in the management of anxiety and depression in patients with cancer: A multicenter randomized controlled trial. Journal of Clinical Oncology, 25, 532–539. doi: 10.1200/JCO.2006.08.9987 [DOI] [PubMed] [Google Scholar]
- Wolpe J. (1969). The practice of behavior therapy (1st ed). New York: Pergamon Press. [Google Scholar]