Abstract
Objectives:
The objective of this study was to report causes, management options, and complications of facial fractures among children.
Materials and Methods:
The groups were defined on the basis of age, gender, cause of injuries, location, and type of injuries. The treatment modalities ranged from no intervention, closed reduction alone or with open reduction internal fixation (ORIF).
Statistical Analysis:
Descriptive statistics were generated by using SPSS software for the entire range of the variables under study.
Results:
Records of 240 pediatric patients were obtained and a total of 322 fractures were found among a study sample. Among these, one-thirds were due to road traffic accidents (RTAs) (37.26%) and fall injuries (36.64%), making them the leading causes of facial fractures. Mandibular fractures were the most common and they accounted for 46% (n = 148) of all fractures. The highest number of RTA (n = 27) was found in adolescents and fall injuries were more prevalent in preschool children (n = 34). Forty-two percent of the fractures (n = 101) were treated with close treatment using arch bars and splints, followed by ORIF (n = 68). The rest, 29.6% (n = 71), received conservative treatments. Postoperative complications were observed in 18.33% (n = 44) of cases, of which jaw deviation, growth disturbance, and trismus were more frequently encountered.
Conclusion:
Pediatric facial fractures if not managed properly can cause severe issues; therefore, injury prevention strategies should be strictly followed to reduce pediatric injuries in low socioeconomic countries.
Key words: Complications, facial fractures, fall injuries, road traffic accident, surgical fixation
INTRODUCTION
External causes of injuries (trauma) account for significant morbidity and mortality among children and adolescents worldwide. It is estimated that each year more than 950,000 children under the age of 18 dies of an injury.[1,2] According to a recent report, injury is the 28th leading cause of deaths globally.[3] It is reported that the prevalence rates for traumatic dental injuries among different populations are between 4.9% and 37%.[4] Various studies have identified the young population as the most vulnerable group to be affected by fall-related injuries, with males being affected twice as much as females. Fall from height has also been recognized as one of the most common modes of injuries in low-income nations.
A recently published study [5] reported 3335 fall-related injuries, and it was observed that a majority of the falls were due to slipping (n = 671, 56.6%), followed by falls from heights (n = 338, 28.5%). About two-thirds (n = 675, 66.6%) of fall injuries involved extremities, followed by head/neck injuries (n = 257, 25.4%) and facial injuries (n = 99, 9.8%). The study also concluded that falls are a major cause of injury-related visits to emergency departments (EDs). Pediatric trauma differs from adult trauma because of various anatomical factors and continued growth in children. Furthermore, according to the study, patterns of pediatric trauma vary depending on the levels of modernization. However, the authors have found very limited studies on this.[6,7] The quality of treatment for pediatric facial fractures has improved during the past few years due to advances in imaging modalities, bone fixation technology, microsurgical techniques, and distraction osteogenesis.[8] The management of these injuries continues to evolve at a rapid pace. However, specific issues related to pediatric patients have not received much attention compared to adult patients with facial injuries. Many developing countries have witnessed several challenges related to the management of pediatric trauma. These include insufficient trauma centers, shortages of adequately trained staff, and personnel training programs and finally, lack of public awareness programs.[9]
The aim of this study was to present the demographics, mechanisms, nature, anatomical location, age-related variations, treatment trends, and their outcomes for maxillofacial injuries among pediatric populations. It is important to mention that the study was conducted at the largest tertiary care oral and maxillofacial surgery (OMFS) center, Mayo Hospital, King Edward Medical University (KEMU), Lahore, Pakistan. To the best our knowledge, no recent clinical research on pediatric maxillofacial injuries from this region has been presented so far. Therefore, this study is particularly useful as it serves as a source of the most current and updated information on the magnitude, nature, causes, and management of pediatric maxillofacial trauma among existing communities. This article may consequently facilitate a better perception of childhood maxillofacial injuries and will help to develop evidence-based interventions.
MATERIALS AND METHODS
A study of 240 cases (male: female; 1.8:1) presented at the Department of OMFS, Mayo Hospital/KEMU, Lahore, Pakistan. This was after obtaining ethical permission from the Institutional Ethical Review Committee. This study followed the Declaration of Helsinki on medical protocols and ethics. Children (neonates up to 14 years) were included in this study.
All the patients referred from the ED were initially resuscitated and subsequently examined. Relevant radiographs were taken, followed by definitive management after gaining the patient's consent. Information retrieved included age, gender, cause of injuries, location, and type of injuries (soft tissue and hard tissue). The causes were grouped into road traffic accidents (RTAs), fall injuries, sports injuries, firearm injuries (FAIs), animal-related injuries, interpersonal violence, stab injuries, and others. Fractures were grouped as mandibular fractures, maxillary fractures, zygomatic bone, nasoorbitoethmoidal (NOE), and nasal bone fractures. The treatment modalities ranged from no intervention (simple undisplaced fractures with normal occlusion), closed reduction by only maxillomandibular fixation alone or with open reduction internal fixation (ORIF). Follow-ups for duration of 2 years and 9 months were done for all patients.
From each patient, informed consent was obtained before inclusion of their information in this study/treatment and permission was also sought and granted to publish their records and pictures. Data were statistically analyzed using the SPSS software (version 15, IBM, Armonk, New York, USA) to study the characteristics of the subjects. Descriptive statistics were generated for the entire range of the variables under study. Most variables were categorical for which proportions were reported, and the means and standard deviations were calculated for continuous variables. Data analysis involved a descriptive analysis which was made for each variable.
RESULTS
Among 240 patients, total fractures were 322, where, one-third were RTAs (37.26%) and fall injuries (36.64%), making them the leading causes of facial fractures. Mandibular fractures being the most common accounted for 46% (n = 148) of all fractures, followed by maxillary fractures (20%), the zygomatic bone fractures (13.04%), and dentoalveolar fractures (14%) as shown in Table 1. The least common were isolated orbital fractures (4.34%) and NOE (3.1%).
Table 1.
Causes of facial fractures in pediatric patients

The cases were categorized into six age groups as tabulated in Table 2, and the results showed that fall injuries were the most common cases, i.e., 38.3% (n = 92). A majority of these were preschool children (n = 34), whereas the highest frequency of RTAs was found in the adolescent group (n = 27). Figure 1a shows the bilateral periorbital ecchymosis, subconjunctival hemorrhage, depressed nasal bridge, telecanthus, and chin laceration. Furthermore, in Figure 1b, the X-ray paranasal sinus view exhibits bilateral Lefort II fracture lines, mandibular symphysis, and NOE fractures. Figure 2 shows massive periorbital and facial edema, skin abrasions, and lacerations. Sports-related injuries were n = 26 patients, whereas firearm victims were n = 18. Forty-two percent of fractures (n = 101) were treated with closed treatment using arch bars [Figure 3] and splints, followed by ORIF (n = 68). The rest 29.6% (n = 71) received conservative treatments, i.e., soft diets and were kept under observation.
Table 2.
Distribution of fractures according to the age of patients and etiology

Figure 1.
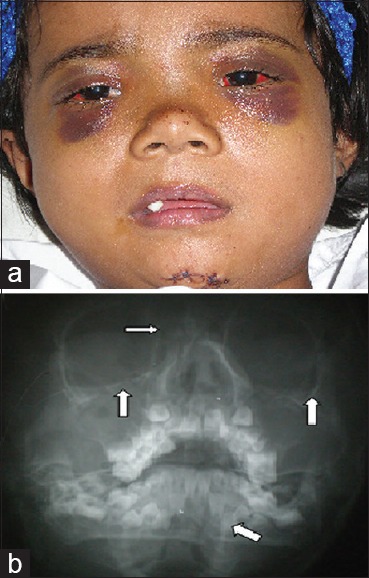
(a) Bilateral periorbital ecchymosis and subconjunctival hemorrhage, depressed nasal bridge, telecanthus, and chin laceration, (b) X-ray paranasal sinus view showing bilateral Lefort fracture lines, mandible symphysis, and nasoorbitoethmoidal fractures
Figure 2.

Massive periorbital and facial edema with bilateral periorbital ecchymosis, stitched nasal bridge, and left upper lid
Figure 3.
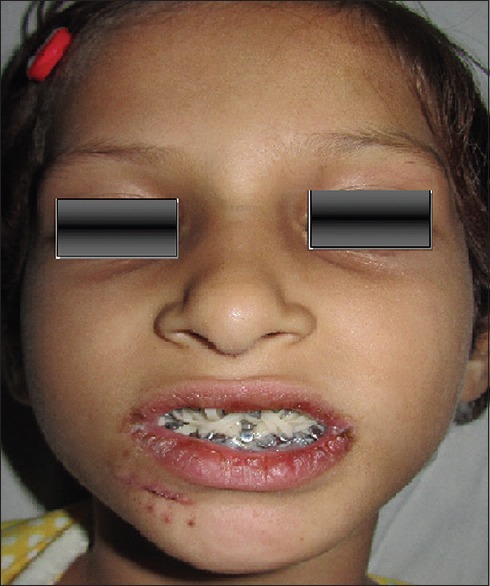
Arch bar and elastics, healing scar at right chin
Postoperative complications [Table 3] were observed in 18.33% (n = 44) of cases. From the results, jaw deviations (n = 10), growth disturbances (n = 9), and trismus (n = 7) were more frequently encountered than infections, temporomandibular joint (TMJ) ankyloses, and deranged occlusion. Jaw deviation and restricted facial growth/growth disturbance were observed in cases where hardware was not removed within 6 months of treatment.
Table 3.
Complication with various treatment modalities

Trismus and deranged occlusion were also seen in cases where occlusal splinting or only arch bars were done. The displacement or dislocation of tooth bud and TMJ ankylosis was mostly seen in cases where closed treatment (with prolonged immobilization was instituted). However, postoperative infections were the least common complications observed as was seen in cases where ORIF was done. The reason could be poor compliance to oral hygiene maintenance that led to suture dehiscence and plate exposures. Patients who developed infections posttreatment had undergone plate removal, which increased their duration of stay in the hospital.
DISCUSSION
Maxillofacial injuries can be life threatening because they pose risks of airway blockage and substantial hemorrhage. The management is tricky to make progress esthetically acceptable, and a suitable administration is important to recreate and reproduce the structure, profile, form, and function of uninjured status.[10]
In this study, it was observed that incidences of maxillofacial fractures in pediatric patients were much higher as compared to populations in other countries. A total of 88% patients had single or multiple facial fractures and 11.2% had isolated soft-tissue injuries.
The statistics regarding the causes of injuries in our series differ as compared to most of the other series reported in relevant literatures. In our study, falls were the most common cause (38.3%), whereas RTAs (31.2%) remained the second most common cause of injury. Among the RTAs, bicycle accidents were the most common. Fall injuries were common in preschool children (age: 3–5 years) whereas RTAs were more common among children of 11–14 years.
Among children, a vast majority of vehicular accidents can be attributed to bicycle accidents. Discrepancies in the reported cases exist because some authors categorized injuries resulting from bicycles as falls while others classified this as vehicle accidents. This is in contrast to our series, in that, sports-related injuries are less common (11%) because a lower number of children participate in outdoor sports in the region.
There is a strong relationship between social class and childhood falls both between geographical regions and within countries. Various factors have been known to influence such injuries. These factors include exposure to hazardous environments, overcrowding, sole parenthood, unemployment, young maternal age, low maternal education, caregiver stress, mental health problems, and inequities in access to health care. In low-income countries, children in the labor force are at a higher risk of fall injuries because the work demands more than what their age, strength, and skills can offer.[1,11,12] Other risk factors for falling include animal riding, inadequate supervision of younger children, and inappropriate heights and surfaces in playgrounds.
It has also been observed that the etiology of pediatric facial fractures varies with age. Children under 5 years tend to suffer fewer injuries because they are usually under direct supervision of their guardians and are, therefore, more monitored in their movements and activities. As children become older, however, the incidences as well as the causes of injury increase due to more independence involved in their outdoor activities. The lack of play areas results to children playing on streets and roads which consequently lead to more RTAs. These results raise questions regarding the adequacy of safety measures inside homes, which are considered the safest places for children. The need of full-time supervision by adults, especially for younger children in addition to safe environments is, therefore, a key factor in reducing childhood injuries.[1]
Incidence rates of mandibular fractures in children have been fairly consistent in various literatures over the years. The results of our study show mandibular fractures (46%) as the most common fractures, either isolated or in combination with other facial injuries. The study also reveals that mandibular fractures are more common in fall injuries and RTAs. The prevalence of this injury is due to the position of the mandible, which makes it more susceptible to fractures than the mid-face.[13] Furthermore, it was found that the condyle was more commonly involved in the fractures as compared to parasymphysis. Dentoalveolar fractures were mostly observed in the anterior parts of maxilla and mandible since the upper incisor region is more prone to injuries and fractures. The total complication rate in the study remained at 18.33%, which was less than the results of studies conducted by Motamedi [14] (44%) and Abiose [15] (61.5%).
Furthermore, according to the study, it was concluded that the rate of complications varies depending on the treatment modalities. The total complication rate in conservative treatment was 29.5%, whereas the complication rate in closed treatment was 27.3%. Jaw deviation was found to be the most common complication in both of these treatment modalities. The rate was, however, higher in patients treated with closed treatment in which the mouth remained closed for more than 10–21 days postoperation. This might be due to unaddressed fracture of condylar segments which later resulted in decreased joint function, jaw deviation, deranged occlusion, and TMJ ankylosis. With relation to 18 FAI cases, 90% resulted from stray bullets. This could be due to security issues or lack of strict implementation of legislations regarding gun usage.
In the present study, ORIF was employed in only 28.33% of cases. This was a lower number when compared to other studies done by Motamedi [14] (40% ORIF cases) and Vetter et al.[16] (60% ORIF cases). The complications with ORIF were 43.2%, which remained the highest in all treatment options. The authors of the aforementioned studies preferred closed treatment or more conservative approaches to open the fracture segments. This helped them take advantage of more greenstick and nondisplaced fractures among children seen in our study. Damage to tooth bud and growth restriction at the point of hardware fixation resulted in delayed or unerupted tooth and facial asymmetries. With the future morphological and anatomical changes in mind, the management of these facial injury victims becomes a more complicated and arduous task for a surgeon. However, rapid wound healing among children is a promising sign.
The lowest complication rate of nonunion in all categories of treatment could be justified with increased growth potential in children. It is worth mentioning that TMJ ankylosis was prevalent in patients with closed treatment which might be due to the restricted functional joint movement for a longer period of time. However, with strict monitoring of suspicious cases and physiotherapy exercises, better results were observed, and this resulted in a further change to data. It was thus observed that, in such cases, the management utilizing the closed approach needs an early mobilization of TMJ and vigilant follow-ups.
Among developing countries, maxillofacial trauma has various etiologies, and the predominance of one or other factors is due to age, gender, social status, or urban/residential areas.[17,18,19] From our study, we have also observed that fall injuries in urban areas, especially during construction of residential houses, are quite common. On the other hand, most trauma incidents in rural areas are due to falls from trees. Further follow-ups of these patients till adulthood are, however, required for further data collection.
CONCLUSION
Pediatric facial fractures can result in significant morbidity if not managed properly. Mandible fractures are the most common type of facial bone fractures, and falls remain the highest cause of injury, especially among preschool age groups. With the increase in age, however, RTAs notably become a major contributing factor for injuries. Although the principles of the management remained the same as that, of adult patients, a majority of these fractures could be managed conservatively with acceptable outcomes. If surgery is required, care must be taken to avoid further morbidity. Public education efforts regarding child safety should involve different dedicated teams and the media. Injury prevention strategies should be strictly followed in the hope of reducing such preventable pediatric injuries in low socioeconomic countries.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Peden M. World Report on Child Injury Prevention. Switzerland: World Health Organization; 2008. [PubMed] [Google Scholar]
- 2.Fraga AM, Bustorff-Silva JM, Fernandez TM, Fraga GP, Reis MC, Baracat EC, et al. Children and adolescents deaths from trauma-related causes in a Brazilian city. World J Emerg Surg. 2013;8:52. doi: 10.1186/1749-7922-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2013 Mortality and Causes of Death Collaborators. Naghavi M, Wang H, Lozano R, Davis A, Liang X, Zhou M. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ozer S, Yilmaz EI, Bayrak S, Tunc ES. Parental knowledge and attitudes regarding the emergency treatment of avulsed permanent teeth. Eur J Dent. 2012;6:370–5. [PMC free article] [PubMed] [Google Scholar]
- 5.Mir M, Bachani AM, Khawaja H, Afridi S, Ali S, Khan M, et al. The Pakistan National Emergency Department Surveillance Study (Pak-NEDS): Introducing a pilot surveillance. BMC Emerg Med. 2015;15(Suppl 2):S1. doi: 10.1186/1471-227X-15-S2-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iida S, Matsuya T. Paediatric maxillofacial fractures: Their aetiological characters and fracture patterns. J Craniomaxillofac Surg. 2002;30:237–41. doi: 10.1054/jcms.2002.0295. [DOI] [PubMed] [Google Scholar]
- 7.Muñante-Cárdenas JL, Olate S, Asprino L, de Albergaria Barbosa JR, de Moraes M, Moreira RW, et al. Pattern and treatment of facial trauma in pediatric and adolescent patients. J Craniofac Surg. 2011;22:1251–5. doi: 10.1097/SCS.0b013e31821c696c. [DOI] [PubMed] [Google Scholar]
- 8.Cole P, Kaufman Y, Hollier LH., Jr Managing the pediatric facial fracture. Craniomaxillofac Trauma Reconstr. 2009;2:77–83. doi: 10.1055/s-0029-1202592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ademuyiwa AO, Usang UE, Oluwadiya KS, Ogunlana DI, Glover-Addy H, Bode CO, et al. Pediatric trauma in Sub-Saharan Africa: Challenges in overcoming the scourge. J Emerg Trauma Shock. 2012;5:55–61. doi: 10.4103/0974-2700.93114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gazal G. Evaluation of the effectiveness of early or delayed treatment upon healing of mandibular fractures: A retrospective study. Eur J Dent. 2015;9:87–91. doi: 10.4103/1305-7456.149650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bartlett SN. The problem of children's injuries in low-income countries: A review. Health Policy Plan. 2002;17:1–3. doi: 10.1093/heapol/17.1.1. [DOI] [PubMed] [Google Scholar]
- 12.Ghaffar A, Hyder AA, Mastoor MI, Shaikh I. Injuries in Pakistan: Directions for future health policy. Health Policy Plan. 1999;14:11–7. doi: 10.1093/heapol/14.1.11. [DOI] [PubMed] [Google Scholar]
- 13.Kaban LB, Mulliken JB, Murray JE. Facial fractures in children: An analysis of 122 fractures in 109 patients. Plast Reconstr Surg. 1977;59:15–20. doi: 10.1097/00006534-197701000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Motamedi MH. An assessment of maxillofacial fractures: A 5-year study of 237 patients. J Oral Maxillofac Surg. 2003;61:61–4. doi: 10.1053/joms.2003.50049. [DOI] [PubMed] [Google Scholar]
- 15.Abiose BO. The incidence and management of middle third facial fractures at the University College Hospital, Ibadan. East Afr Med J. 1991;68:164–73. [PubMed] [Google Scholar]
- 16.Vetter JD, Topazian RG, Goldberg MH, Smith DG. Facial fractures occurring in a medium-sized metropolitan area: Recent trends. Int J Oral Maxillofac Surg. 1991;20:214–6. doi: 10.1016/s0901-5027(05)80177-8. [DOI] [PubMed] [Google Scholar]
- 17.Ellis E, 3rd, Moos KF, el-Attar A. Ten years of mandibular fractures: An analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985;59:120–9. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- 18.Zargar M, Khaji A, Karbakhsh M, Zarei MR. Epidemiology study of facial injuries during a 13 month of trauma registry in Tehran. Indian J Med Sci. 2004;58:109–14. [PubMed] [Google Scholar]
- 19.Ortakoğlu K, Günaydin Y, Aydintuğ YS, Bayar GR. An analysis of maxillofacial fractures: A 5-year survey of 157 patients. Mil Med. 2004;169:723–7. doi: 10.7205/milmed.169.9.723. [DOI] [PubMed] [Google Scholar]


