In the health care professions, the words compassion and empathy are frequently used interchangeably, and the term compassion fatigue is often used to describe a type of post-traumatic stress disorder. According to Dr. Charles Figley (1) of Tulane University, “Compassion fatigue is a state experienced by those helping people or animals in distress; it is an extreme state of tension and preoccupation with the suffering of those being helped to the degree that it can create a secondary traumatic stress for the helper.” But emerging research from the social neuroscience laboratory of Dr. Tania Singer of the Max Planck Institute for Human Cognitive and Brain Sciences in Germany shows that compassion fatigue is a misnomer and that it is empathy that fatigues in care givers, not compassion! (2).
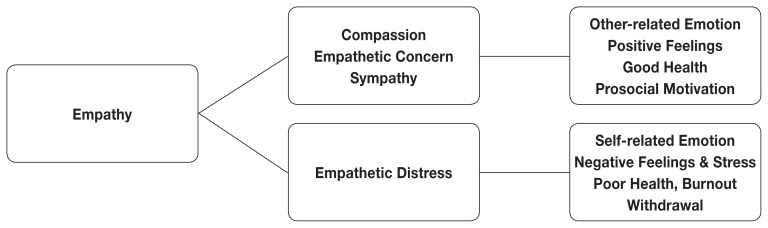
Understanding the neurophysiological differences between empathy and compassion is critical to alleviating the emotional distress frequently experienced by veterinarians and veterinary technologists. To explain the differences, Singer developed a hierarchy model of empathy and compassion (Figure 1).
Figure 1.
Hierarchy model of empathy and compassion.
Empathy
Empathy is a mental construct that allows us to resonate with others’ positive and negative feelings. We can feel happy at the joy of others and we can feel distress when we observe someone in physical or mental pain. While sharing positive emotions with others is certainly pleasant, the sharing of negative emotions can be difficult.
The development of functional magnetic resonance imaging (fMRI) opened the way for neuroscientists to explore the brain circuitry involved when people experience pain in themselves as well as when they observe someone else feeling pain. To investigate pain-related empathy, Dr. Singer studied married couples, with the assumption that couples are likely to feel empathy for each other. Using fMRI scanners, she investigated the brain networks that were activated when a painful stimulus was applied to the hand of one partner and the other partner could see and hear their reaction. Areas of the anterior insula and the anterior middle cingulate cortex were activated when subjects received pain but also when they observed that their partner experienced pain. Other parts of the pain network were activated only in the partner actually receiving the painful stimulus. Singer concluded that the part of the pain network associated with its emotional qualities, but not its sensory qualities, mediates empathy for suffering (3). Thus, both the firsthand experience of pain and the knowledge that a beloved partner is experiencing pain activate the same emotional brain circuits.
In human interactions, feeling empathy is the first step in building social connection. But it is very important that in empathy you feel with the other person, but you don’t confuse yourself with the other; you still know that the emotion you resonate with is the emotion of the other person (4). A good example of appropriate empathy is helping a client through the euthanasia experience. As I have euthanized many of my own animals during my 30-year veterinary career, I can express to the client “I know how you feel” and I feel my own sadness during the euthanasia process. But I can tell that I’m feeling and honoring their grief and not making the grief my own.
After empathy establishes the connection between us, the second step of the hierarchy can diverge into the processes of empathetic distress or compassion and empathetic concern. Whether observation of distress in others leads to empathic concern and altruistic motivation or to personal distress and self-centered emotions depends upon our capacity for “self-other” differentiation (5).
When the “self-other” distinction becomes blurred and we take on the emotional pain of the other person as our own pain, empathetic distress results. In my euthanasia example, if I’m not able to distinguish my client’s grief from my grief over the loss of my own animals, then I move into empathic distress. Empathic distress is the strong aversive and self-oriented response to the suffering of others, accompanied by the desire to withdraw from a situation in order to protect one’s self from excessive negative feelings. As I become overwhelmed by my own euthanasia-associated grief, I may try to avoid the aversive situation by rushing the client through the euthanasia process and withdraw from further interactions with my client as a mechanism to protect myself. The fMRI data show that adopting the self-perspective leads to increased activation in brain areas involved in the processing of threat or pain, such as the amygdala (5). Chronic pain, whether mental or physical, depletes dopamine levels within brain circuits mediating reward and motivation (6). When locked into empathic distress, we have a blunted capacity to experience pleasure along with decreased motivation for natural rewards. Chronic depletion of dopamine from repeated episodes of empathic distress is what leads to burnout, characterized in health care professionals as emotional exhaustion, withdrawal, depersonalization, and a decreased sense of personal accomplishment due to work-related stress (7).
Compassion
In contrast to empathy, compassion is characterized by feelings of warmth, concern, and care for the other, as well as a strong motivation to improve the other’s wellbeing. Compassion goes beyond feeling with the other to feeling for the other. Unlike empathy, compassion increases activity in the areas of the brain involved in dopaminergic reward and oxytocin-related affiliative processes, and enhances positive emotions in response to adverse situations (8). While empathizing with my client making a euthanasia decision invokes my own feelings of sadness, moving to compassion for my client’s situation results in sympathy, empathic concern, and positive emotional feelings that counterbalance my sadness and cause me to take action to help my client. Instead of withdrawing and rushing through the procedure in self-defence, compassion enables me to slow down and be present with my client without experiencing distress.
This is the critical property of compassion that differentiates it from empathy. Because compassion generates positive emotions, it counteracts negative effects of empathy elicited by experiencing others’ suffering. Unlike the dopamine depletion that occurs from activation of the pain networks, the neural networks activated when people feel compassion towards others activate brain areas linked to reward processing that are full of receptors for oxytocin and vasopressin, the neuropeptides that are crucial in attachment and bonding (2). Compassion does not fatigue — it is neurologically rejuvenating!
Cultivating compassion
Interventions to deal with burnout in health care professionals typically focus on stress management and other self-care strategies, but have little evidence of efficacy (7). While self-care is always a good thing, Singer and other neuroscientists have proven that compassion is a skill that can be cultivated, and that empathic distress can be reversed, by learning how to turn empathy into compassion.
The most well-studied techniques for compassion skills are found in mindfulness meditation programs. Even with short periods of compassion training, participants continue to feel empathy for the suffering of others, but gain the capacity to feel positive emotions without feeling distress (8).
With the understanding that empathic distress is self-centered while compassion is other-centered, it should come as no surprise that wellness is a social phenomenon and the techniques for cultivating compassion are taught in groups with interactive exercises. In fact, many studies now demonstrate that compassion training leads to long-lasting changes in attitudes and behaviors toward other people that transcend the specific situation in which compassionate feelings were evoked, and moreover that these prosocial behaviors transfer to a broad range of people and situations (9,10).
Footnotes
First published in the February 2018 issue of the Saskatchewan Veterinary Medical Association.
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Figley C. The Compassion Fatigue Awareness Project. [Last accessed May 1, 2018]. Available from: http://www.compassionfatigue.org/
- 2.Klimecki O, Singer T. Empathic distress fatigue rather than compassion fatigue? Integrating findings from empathy research in psychology and social neuroscience. In: Oakley B, Knafo A, Madhavan G, et al., editors. Pathological Altruism. New York, New York: Oxford University Press; 2011. pp. 1–23. [Google Scholar]
- 3.Singer T, Seymour B, O’Doherty J, Kaube H, Dolan RJ, Frith CD. Empathy for pain involves the affective but not sensory components of pain. Science. 2004;303:1157–1162. doi: 10.1126/science.1093535. [DOI] [PubMed] [Google Scholar]
- 4.Singer T, Klimecki OM. Empathy and compassion. Curr Biol. 2014;24:R875–R878. doi: 10.1016/j.cub.2014.06.054. [DOI] [PubMed] [Google Scholar]
- 5.Lamm C, Batson CD, Decety J. The neural substrate of human empathy: Effects of perspective-taking and cognitive appraisal. J Cogn Neurosci. 2007;19:42–58. doi: 10.1162/jocn.2007.19.1.42. [DOI] [PubMed] [Google Scholar]
- 6.Borsook D, Linnman C, Faria V, Strassman AM, Becerra L, Elman I. Reward deficiency and anti-reward in pain chronification. Neurosci Biobehav Rev. 2016;68:282–297. doi: 10.1016/j.neubiorev.2016.05.033. [DOI] [PubMed] [Google Scholar]
- 7.McCray LW, Cronholm PF, Bogner HR, Gallo JJ, Neill RA. Resident physician burnout: Is there hope? Fam Med. 2008;40:626–632. [PMC free article] [PubMed] [Google Scholar]
- 8.Klimecki OM, Leiberg S, Lamm C, Singer T. Functional neural plasticity and associated changes in positive affect after compassion training. Cereb Cortex. 2013;23:1552–1561. doi: 10.1093/cercor/bhs142. [DOI] [PubMed] [Google Scholar]
- 9.Leiberg S, Klimecki O, Singer T. Short-term compassion training increases prosocial behavior in a newly developed prosocial game. PLoS One. 2011;6:e17798. doi: 10.1371/journal.pone.0017798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weng HY, Fox AS, Shackman AJ, et al. Compassion training alters altruism and neural responses to suffering. Psychol Sci. 2013;24:1171–1180. doi: 10.1177/0956797612469537. [DOI] [PMC free article] [PubMed] [Google Scholar]