Abstract
Background
The incidence of gastric cancer, while declining in many places worldwide, is characterized by considerable geographical variability. The USA has large racial, ethnic and regional variation; we collected data from all 50 states to better characterize recent changes in gastric cancer incidence nationwide.
Methods
Annual gastric cancer incidence rates from 1999 to 2013 were extracted from the United States Cancer Statistics (USCS) registry. Secular trends of gastric cancer incidence were examined overall and by sociodemographic factors and states. We used Joinpoint regression to compute annual percent change (APC) and average annual percent change (AAPC) and corresponding 95% confidence intervals (CIs). SEER 13 registries data were extracted to examine the secular trends by cardia and non-cardia gastric cancers.
Results
Overall gastric cancer incidence decreased until 2007 (APC = −1.55, 95% CI: −1.88, −1.21), and remained stable thereafter (APC = −0.32, 95% CI: −0.84, 0.20). However, rates increased among persons <50 years of age (AAPC = 0.89, 95% CI: 0.61, 1.16), especially among non-Hispanic white females and Hispanic females. Incidence of non-cardia gastric cancer increased among persons <50 years of age (AAPC = 0.69, 95% CI: −0.06, 1.44), whereas rates of gastric cardia cancer remained unchanged. States with rapid increases in high-risk population groups (e.g. Hispanic females aged <50), including California and Texas, had highest annual increases in gastric cancer incidence.
Conclusions
Divergent trends for gastric cancer incidence were observed in the USA. Incidence rates, particularly for non-cardia gastric cancer, were stable or increasing among persons aged <50 years.
Keywords: Gastric cancer incidence, USA, state analysis
Key Messages
The rate of decline in overall gastric cancer incidence rates has slowed in the USA since 2007.
Although gastric cancer incidence rates have declined among persons aged ≥50 years, rates are increasing among persons aged <50 years, particularly among females.
Texas and California, states with rapid growth of Hispanic populations, had the highest annual increases in gastric cancer incidence.
States with high and increasing non-cardia gastric cancer incidence rates should address provisions for the detection and treatment of underlying risk factors, including H. pylori screening and treatment.
Introduction
Worldwide, gastric cancer is the fifth most common malignancy and the third leading cause of cancer-related death.1 In the USA, approximately 28 000 new cases of gastric cancer and 10 960 deaths from gastric cancer are expected to occur in 2017. Consistent with global trends, overall incidence and mortality rates for gastric cancer (primarily non-cardia) in the USA have declined during the past four decades.2Helicobacter pylori is the major established risk factor for non-cardia gastric cancer, accounting for >75% of cases worldwide,3 but there is increasing evidence that tobacco smoking,4 heavy alcohol consumption,5 obesity,6 high intake of red meat7 and low intake of fruits8 and high sodium intake9 also increase the risk of gastric cancer. Differences in the prevalence of exposure to H. pylori infection and lifestyle factors likely contribute to the geographical variations in gastric cancer incidence, as well as to the differences in incidence among racial and ethnic subgroups within a country.10
Previous studies examining incidence rates and secular trends for gastric cancer in the USA have relied on data from the National Cancer Institute’s (NCI) Surveillance, Epidemiology and End Results (SEER) programme.11,12 Though the sampling of SEER is intended to capture a broadly representative sample of the overall US population,13 certain racial/ethnic groups and geographical regions are under-represented, and the generalizability of its findings may be limited. Therefore, an analysis of overall incidence trends in SEER could potentially mask the changing patterns of gastric cancer incidence among certain population subgroups. For example, a study using SEER data from 1978 to 2005 found a decreasing trend of gastric cancer incidence overall, and as well as in all subgroups defined by race/ethnicity, sex, histology and anatomical site.11 Notably, SEER expanded to include more racial minority groups from 1992.13 A more recent study using the 13 SEER registries found a rising trend of gastric cancer among Hispanic men aged <50 years between 1992 and 2011.12 Among Hispanics in the state of California, there is some evidence for divergent trends by histology, anatomical site and place of birth.14 Therefore investigating secular trends using data from all 50 states both individually and collectively would provide a more comprehensive description of recent gastric cancer trends in the USA.
A better understanding of gastric cancer trends is crucial in implementing preventive strategies, such as H. pylori eradication, and early detection of gastric cancer at targeted populations and geographical regions.10,15 Therefore, we performed a comprehensive examination of the overall burden as well as secular trends in gastric cancer incidence rates at both national and state levels in all 50 US states between 1999 and 2013. This included a novel evaluation of racial/ethnic differences in gastric cancer rates across states and time periods, as well as identification of states with the greatest burden and most rapidly changing incidence rates.
Methods
Study population
We obtained gastric cancer incidence data between 1999 and 2013 from the United States Cancer Statistics (USCS) registry. The USCS registry provides the official federal statistics on cancer incidence from registries with high quality data for all 50 states and the District of Columbia. Each of the cancer registries capture more than 90% of all cases; less than 5% of cases are solely identified from death certificates; less than 5% of cases have missing data on age, sex or race/ethnicity; and more than 97% of cases pass computerized validity and logic checks. The primary sources of data for the USCS registry are from: (i) the National Program of Cancer Registries (NPCR) held by the Center for Disease Control and Prevention (CDC), covering 96% of the US population and with 27 million invasive cancer cases diagnosed between 1995 and 2014; and (ii) the 14 population-based cancer registries and three supplemental registries from the SEER programme held by the NCI, covering approximately 28% of the US population.16
Incident case identification and annual incidence rate computation
Gastric cancer is identified within USCS registries by the International Classification of Diseases for Oncology, third edition: site codes C160-C169; and ICD-O-3 histology type excluding 9050–9055, 9140 and 9590–9992. Overall annual incidence rates for gastric cancer (cardia and non-cardia combined) were accessed through the CDC Wide-ranging Online Data for Epidemiologic Research (WONDER) platform, an online query-based system allowing access to CDC public health information. Annual incidence rates for gastric cancer were obtained using standard formula implemented within WONDER, which uses the number of cases as the numerator and the corresponding population size based on US Census Bureau data as the denominator. The corresponding 95% confidence intervals (CIs) were computed using the Tiwari et al. method.17
Statistical analysis
Annual age-adjusted incidence rates (standardized to the 2000 US population using the direct method) for gastric cancer were computed. The trends in gastric cancer incidence rates over time were evaluated using the NCI’s Joinpoint program (version 4.5.0.1; available at: http://surveillance.cancer.gov/joinpoint), which tests whether or not an apparent change in trend is statistically significant using a Monte Carlo Permutation method. The model was tested starting from a single line model (i.e. no joinpoints) and examined whether more joinpoints should be added to the model based on their statistical significance.18 We allowed a maximum of three joinpoints with a minimum of four observations per segment. The annual percent change (APC) for each single linear segment and average annual percent change (AAPC) for the entire study period were computed for each joinpoint model. The temporal trend of gastric cancer incidence was examined overall and by 5-year age groups, sex, race/ethnicity (non-Hispanic White, Black, Hispanic, Asian or Pacific Islander, and American Indian/Alaska Native) and geographical regions (Northeast, Midwest, South and West). In our preliminary analysis, the secular trend differed between persons aged <50 years and those aged ≥50 years. Therefore, we further stratified the Joinpoint model by age at 50 years.
Secular trends at the state level were examined in two ways: (i) the top five states with highest incidence of gastric cancer (over the entire study period: 1999–2013); and (ii) the top five states with highest increases in gastric cancer incidence rates (measured by AAPC) within the most recent 5 years (2009–13). Both were examined by sex and age group (<50 and ≥50 years).
We created state heat maps for both overall and age-stratified (<50 and ≥50 years) incidence rates, highlighting the secular trend in age-adjusted incidence rates in each state over three 5-year periods: 1999–2003; 2004–08; and 2009–13. Age-adjusted rates for each state were categorized using quartile midpoints determined based on overall national gastric cancer incidence rates in the first time period (1999–2003).
Since USCS data do not provide information on anatomical site (i.e. cardia vs. non-cardia), we further examined incidence rates, APC and AAPC of cardia and non-cardia gastric cancer separately using data from SEER 13 registries for gastric cancer cases from 1999 to 2013. In the SEER 13 dataset, cardia gastric cancer was defined as primary site of C160. Non-cardia gastric cancer was defined as primary site of C161-C168. All analyses were conducted using SEER*stat (version 8.3.4, NCI, Bethesda, USA) and SAS 9.4 (SAS Inc., Cary, NC, USA).
Results
There were 317 706 new cases of gastric cancer diagnosed between 1999 and 2013 in the USCS registry. Over the entire study period, joinpoint regression identified one inflection point (in 2007) and thus two linear segments (1997 to 2007; and 2007 to 2013). The overall age-adjusted incidence rates for gastric cancer decreased by 1.55% per year between 1999 and 2007 (APC = −1.55%, 95% CI: −1.88, −1.21), and then remained unchanged between 2007 and 2013 (APC = −0.32, 95% CI: −0.84, 0.20) (Table 1). Based on the age group analysis by 5-year increment, trends in gastric cancer incidence were consistently increasing for individuals aged <50 years, whereas decreasing trends were observed for individuals aged ≥50 years (Table 1). Furthermore, using data from SEER 13, examination of trends by anatomical site showed that non-cardia gastric cancer incidence decreased among individuals aged >60 years whereas incidence of cardia gastric cancer remained unchanged across all age groups (Supplementary Table 1, available as Supplementary data at IJE online).
Table 1.
Annual and average annual percent change in gastric cancer incidence rates by demographic characteristics: United States Cancer Statistics Registry Data 1999–2013
| Characteristics | Year | APC (95% CI) | P-value | AAPC (95% CI) | P-value |
|---|---|---|---|---|---|
| Overall | 1999 to 2007 | −1.55 (−1.88, −1.21) | <0.001 | −1.02 (−1.28, −0.76) | <0.001 |
| 2007 to 2013 | −0.32 (−0.84, 0.20) | 0.197 | |||
| Sex | |||||
| Male | 1999 to 2003 | −2.01 (−3.00, −1.01) | 0.001 | −3.27 (−3.56, −2.98) | <0.001 |
| 2003 to 2013 | −3.77 (−4.01, −3.52) | <0.001 | |||
| Female | 1999 to 2002 | −1.22 (−2.47, 0.05) | 0.057 | −2.76 (−3.11, −2.40) | <0.001 |
| 2002 to 2007 | −2.66 (−3.44, −1.88) | <0.001 | |||
| 2007 to 2013 | −3.60 (−4.04, −3.15) | <0.001 | |||
| Age in years | |||||
| 20 to 24 | 1999 to 2013 | 3.61 (2.24, 5.01) | <0.001 | 3.61 (2.24, 5.01) | <0.001 |
| 25 to 29 | 1999 to 2013 | 2.05 (1.44, 2.66) | <0.001 | 2.05 (1.44, 2.66) | <0.001 |
| 30 to 34 | 1999 to 2013 | 1.60 (0.85, 2.36) | <0.001 | 1.60 (0.85, 2.36) | <0.001 |
| 35 to 39 | 1999 to 2013 | 1.73 (1.35-2.10) | <0.001 | 1.73 (1.35-2.10) | <0.001 |
| 40 to 44 | 1999 to 2006 | 2.22 (1.23, 3.22) | 0.001 | 1.35 (0.76, 1.95) | <0.001 |
| 2006 to 2013 | 0.50 (−0.43, 1.43) | 0.261 | |||
| 45 to 49 | 1999 to 2013 | 0.24 (0.05, 0.42) | 0.017 | 0.24 (0.05, 0.42) | 0.017 |
| 50 to 54 | 1999 to 2003 | 1.68 (−0.02, 3.42) | 0.052 | −0.01 (−0.50, 0.47) | 0.959 |
| 2003 to 2013 | −0.68 (−1.05, −0.32) | 0.002 | |||
| 55 to 59 | 1999 to 2005 | −1.24 (−2.03, −0.45) | 0.008 | −2.22 (−2.84, −1.59) | <0.001 |
| 2005 to 2010 | −3.74 (−5.07, −2.40) | <0.001 | |||
| 2010 to 2013 | −1.59 (−3.76, 0.63) | 0.133 | |||
| 60 to 64 | 1999 to 2002 | −2.00 (−4.60, 0.67) | 0.124 | −3.56 (−4.10, −3.02) | <0.001 |
| 2002 to 2013 | −3.98 (−4.31, −3.65) | <0.001 | |||
| 65 to 69 | 1999 to 2004 | −2.16 (−3.20, −1.12) | 0.001 | −3.89 (−4.29, −3.49) | <0.001 |
| 2004 to 2013 | −4.84 (−5.26, −4.41) | <0.001 | |||
| 70 to 74 | 1999 to 2002 | −1.18 (−3.13, 0.82) | 0.216 | −3.60 (−4.01, −3.19) | <0.001 |
| 2002 to 2013 | −4.25 (−4.53, −4.00) | <0.001 | |||
| 75 to 79 | 1999 to 2002 | −1.80 (−3.05, −0.54) | 0.012 | −3.65 (−4.01, −3.29) | <0.001 |
| 2002 to 2008 | −3.62 (−4.19, −3.04) | <0.001 | |||
| 2008 to 2013 | −4.78 (−5.43, −4.13) | <0.001 | |||
| 80 to 84 | 1999 to 2004 | −2.56 (−3.50, −1.62) | <0.001 | −3.56 (−3.94, −3.19) | <0.001 |
| 2004 to 2013 | −4.12 (−4.52, −3.71) | <0.001 | |||
| 85+ | 1999 to 2008 | −3.10 (−3.46, −2.74) | <0.001 | −3.91 (−4.26, −3.56) | <0.001 |
| 2008 to 2013 | −5.36 (−6.25, −4.46) | <0.001 | |||
| Race/ethnicity | |||||
| Non-Hispanic White | 1999 to 2002 | −1.61 (−3.00, −0.23) | 0.029 | −3.12 (−3.51, −2.74) | <0.001 |
| 2002 to 2007 | −3.13 (−3.98, −2.28) | <0.001 | |||
| 2007 to 2013 | −3.87 (−4.35, −3.38) | <0.001 | |||
| Black | 1999 to 2013 | −1.70 (−1.88, −1.53) | <0.001 | −1.70 (−1.88, −1.53) | <0.001 |
| Hispanic | 1999 to 2013 | −2.08 (−2.36, −1.80) | <0.001 | −2.08 (−2.36, −1.80) | <0.001 |
| American Indian Native/Alaska Native | 1999 to 2013 | −2.18 (−3.47, −0.86) | 0.003 | −2.18 (−3.47, −0.86) | 0.003 |
| Asian or Pacific Islander | 1999 to 2013 | −2.88 (−3.26, −2.50) | <0.001 | −2.88 (−3.26, −2.50) | <0.001 |
| Region | |||||
| Northeast | 1999 to 2013 | −1.37 (−1.60, −1.14) | <0.001 | −1.37 (−1.60, −1.14) | <0.001 |
| Midwest | 1999 to 2008 | −1.15 (−1.69, −0.61) | 0.001 | −0.51 (−1.02, 0.10) | 0.054 |
| 2008 to 2013 | 0.66 (−0.67, 2.01) | 0.296 | |||
| South | 1999 to 2006 | −1.52 (−2.20, −0.85) | 0.001 | −0.93 (−1.33, −0.53) | <0.001 |
| 2006 to 2013 | −0.33 (−0.94, 0.29) | 0.262 | |||
| West | 1999 to 2013 | −1.13 (−1.43, −0.84) | <0.001 | −1.13 (−1.43, −0.84) | <0.001 |
APC, annual percent change; AAPC, average annual percent change; CI, confidence interval.
For individuals aged ≥50 years, the joinpoint regression identified one inflection point (in 2008) and thus two linear segments (Table 2). Incidence decreased at a rate of 1.75% per year between 1999 and 2008 (APC = −1.75, 95% CI: −2.02, −1.47), but remained unchanged between 2008 and 2013 (APC = −0.24, 95% CI: −0.89, 0.42). The temporal pattern was no different when we examined gastric cancer incidence rates by sex, race/ethnicity and geographical region; AAPC ranged from −0.77% to −2.98% across these subgroups (Table 2). When we examined the secular trends in persons aged ≥50 years by anatomical sites in the SEER 13 dataset, we found that the decreasing trend was mainly due to decreasing incidence of non-cardia gastric cancer (AAPC = −2.20, 95% CI: −2.51, −1.90), whereas incidence of cardia gastric cancer remain unchanged in persons aged ≥50 years (AAPC = −0.30, 95% CI: −0.85, 0.25) (Supplementary Table 2, available as Supplementary data at IJE online).
Table 2.
Annual and average annual percent change in gastric cancer incidence rates among persons ≥50 years by demographic characteristics: USCS Registry Data 1999–2013
| Characteristics | Year | APC (95% CI) | P-value | AAPC (95% CI) | P-value |
|---|---|---|---|---|---|
| Overall | 1999 to 2008 | −1.75 (−2.02, −1.47) | <0.001 | −1.21 (−1.47, −0.95) | <0.001 |
| 2008 to 2013 | −0.24 (−0.89, 0.42) | 0.440 | |||
| Sex | |||||
| Male | 1999 to 2007 | −2.12 (−2.47, −1.76) | <0.001 | −1.48 (−1.74, −1.21) | <0.001 |
| 2007 to 2013 | −0.62 (−1.14, −0.10) | 0.024 | |||
| Female | 1999 to 2008 | −1.66 (−2.06, −1.27) | <0.001 | −1.19 (−1.57, −0.81) | <0.001 |
| 2008 to 2013 | −0.33 (−1.30, −0.65) | 0.463 | |||
| Race/ethnicity | |||||
| Non-Hispanic White | 1999 to 2007 | −2.20 (−2.81, −1.59) | <0.001 | −1.45 (−1.93, −0.98) | <0.001 |
| 2007 to 2013 | −0.45 (−1.41, 0.53) | 0.332 | |||
| Black | 1999 to 2013 | −1.78 (−1.96, −1.59) | <0.001 | −1.78 (−1.96, −1.59) | <0.001 |
| Hispanic | 1999 to 2013 | −2.38 (−2.68, −2.08) | <0.001 | −2.38 (−2.68, −2.08) | <0.001 |
| American Indian/Alaska Native | 1999 to 2013 | −2.50 (−3.79, −1.20) | 0.001 | −2.50 (−3.79, −1.20) | 0.001 |
| Asian or Pacific Islander | 1999 to 2013 | −2.98 (−3.37, −2.59) | <0.001 | −2.98 (−3.37, −2.59) | <0.001 |
| Region | |||||
| Northeast | 1999 to 2013 | −1.60 (−1.82, −1.38) | <0.001 | −1.60 (−1.82, −1.38) | <0.001 |
| Midwest | 1999 to 2008 | −1.47 (−1.97, −0.96) | <0.001 | −0.77 (−1.25, −0.29) | 0.002 |
| 2008 to 2013 | 0.50 (−0.73, 1.74) | 0.386 | |||
| South | 1999 to 2007 | −1.67 (−2.19, −1.14) | <0.001 | −1.08 (−1.47, −0.70) | <0.001 |
| 2007 to 2013 | −0.30 (−1.05, 0.46) | 0.393 | |||
| West | 1999 to 2013 | −1.40 (−1.74, −1.07) | <0.001 | −1.40 (−1.74, −1.07) | <0.001 |
APC, annual percent change; AAPC, average annual percent change; CI, confidence interval; USCS, United States Cancer Statistics.
Among individuals aged <50 years, gastric cancer incidence showed linear increases in age-standardized incidence rates between 1999 and 2013 (APC = 0.89, 95% CI: 0.61, 1.16) (Table 3). Greatest increases were observed among females (AAPC = 1.81, 95% CI: 1.40, 2.22) and non-Hispanic whites (AAPC = 0.50, 95% CI: 0.08, 0.91) (Table 3). A further examination by anatomical site suggested an increase in incidence for both cardia and non-cardia gastric cancers in persons aged <50 years in SEER 13 (Supplementary Table 3, available as Supplementary data at IJE online). The increasing trend among non-Hispanic Whites based on USCS data could be due to rising incidence of cardia gastric cancer (AAPC = 1.56, 95% CI: −0.20, 3.36) (Supplementary Table 3, available as Supplementary data at IJE online).
Table 3.
Annual and average annual percent change in gastric cancer incidence rates among persons <50 years by demographic characteristics: USCS Registry Data 1999–2013
| Characteristics | Year | APC (95% CI) | P-value | AAPC (95% CI) | P-value |
|---|---|---|---|---|---|
| Overall | 1999 to 2013 | 0.89 (0.61-1.16) | <0.001 | 0.89 (0.61-1.16) | <0.001 |
| Sex | |||||
| Male | 1999 to 2013 | 0.14 (−0.23, 0.52) | 0.421 | 0.14 (−0.23, 0.52) | 0.421 |
| Female | 1999 to 2013 | 1.81 (1.40, 2.22) | <0.001 | 1.81 (1.40, 2.22) | <0.001 |
| Race/ethnicity | |||||
| Non-Hispanic White | 1999 to 2013 | 0.50 (0.08, 0.91) | 0.023 | 0.50 (0.08, 0.91) | 0.023 |
| Black | 1999 to 2013 | −1.03 (−1.63, −0.43) | 0.003 | −1.03 (−1.63, −0.43) | 0.003 |
| Hispanic | 1999 to 2013 | 0.16 (−0.27, 0.58) | 0.442 | 0.16 (−0.27, 0.58) | 0.442 |
| American Indian/Alaska Native | 1999 to 2013 | −0.09 (−2.78, 2.68) | 0.946 | −0.09 (−2.78, 2.68) | 0.946 |
| Asian or Pacific Islander | 1999 to 2013 | −1.92 (−2.86, −0.96) | 0.001 | −1.92 (−2.86, −0.96) | 0.001 |
| Region | |||||
| Northeast | 1999 to 2013 | 0.63 (0.13, 1.12) | 0.017 | 0.63 (0.13, 1.12) | 0.017 |
| Midwest | 1999 to 2013 | 1.59 (0.78, 2.40) | 0.001 | 1.59 (0.78, 2.40) | 0.001 |
| South | 1999 to 2013 | 0.47 (−0.03, 0.97) | 0.061 | 0.47 (−0.03, 0.97) | 0.061 |
| West | 1999 to 2013 | 0.96 (0.61, 1.32) | <0.001 | 0.96 (0.61, 1.32) | <0.001 |
APC, annual percent change; AAPC, average annual percent change; CI, confidence interval; USCS, United States Cancer Statistics.
A consistent decreasing trend of gastric cancer incidence was observed among the top five states (or districts) with historically high gastric cancer incidence rates (Table 4). However, there was some suggestion that the rate of decline has slowed in more recent years, and may even be increasing in some states or districts such as New York and Washington DC. This was particularly evident among female populations in New York, where a rising trend of gastric cancer after 2009 was observed (APC = 2.69, 95% CI: −0.65, 6.14) (Table 4). However for persons aged <50 years (especially females), gastric cancer incidence either increased or remained stable (Supplementary Table 4, available as Supplementary data at IJE online). A similar pattern was found among persons aged ≥50 years in the top five states/districts with high rates (Supplementary Table 5, available as Supplementary data at IJE online).
Table 4.
Annual and average annual percent change in gastric cancer incidence rates among top five states with highest incidence rates during 1999–2013: USCS Registry Data 1999–2013
| Statesa | IR (95% CI)b | Year | APC (95% CI) | P-value | AAPC (95% CI) | P-value |
|---|---|---|---|---|---|---|
| Overall | ||||||
| Hawaii | 11.52 (11.08−11.98) | 1999 to 2013 | −4.11 (−4.78, −3.44) | <0.001 | −4.11 (−4.78, −3.44) | <0.001 |
| Washington DC | 9.25 (8.59, 9.95) | 1999 to 2004 | −7.54 (−13.63, −1.01) | 0.029 | −2.26 (−4.72, 0.26) | 0.078 |
| 2004 to 2013 | 0.80 (−1.74, 3.41) | 0.498 | ||||
| New York | 9.19 (9.08−9.30) | 1999 to 2009 | −1.73 (−2.34, −1.11) | <0.001 | −0.95 (−1.69, −0.20) | 0.013 |
| 2009 to 2013 | 1.02 (−1.52, 3.63) | 0.397 | ||||
| New Jersey | 8.66 (8.51, 8.81) | 1999 to 2013 | −1.61 (−2.03, −1.19) | <0.001 | −1.61 (−2.03, −1.19) | <0.001 |
| Connecticut | 8.49 (8.26, 8.73) | 1999 to 2013 | −0.69 (−1.18, −0.20) | <0.001 | −0.69 (−1.18, −0.20) | <0.001 |
| Male | ||||||
| Hawaii | 15.23 (14.46, 16.03) | 1999 to 2013 | −4.48 (−5.39, −3.56) | <0.001 | −4.48 (−5.39, −3.56) | <0.001 |
| New York | 12.89 (12.69, 13.09) | 1999 to 2010 | −1.90 (−2.45, −1.36) | <0.001 | −1.17 (−2.00, −0.33) | 0.006 |
| 2010 to 2013 | 1.57 (−2.41, 5.71) | 0.405 | ||||
| Connecticut | 12.32 (11.89, 12.77) | 1999 to 2013 | −1.06 (−1.73, −0.38) | 0.005 | −1.06 (−1.73, −0.38) | 0.005 |
| Washington DC | 12.29 (11.10, 13.57) | 1999 to 2013 | −2.89 (−4.89, −0.86) | 0.009 | −2.89 (−4.89, −0.86) | 0.009 |
| New Jersey | 12.21 (11.93, 12.50) | 1999 to 2013 | −2.19 (−2.81, −1.57) | <0.001 | −2.19 (−2.81, −1.57) | <0.001 |
| Female | ||||||
| Hawaii | 8.56 (8.04, 9.10) | 1999 to 2013 | −3.75 (−5.47, −2.00) | 0.001 | −3.75 (−5.47, −2.00) | 0.001 |
| Washington DC | 7.08 (6.34, 7.90) | 1999 to 2013 | −1.53 (−3.84, 0.85) | 0.183 | −1.53 (−3.84, 0.85) | 0.183 |
| New York | 6.46 (6.34, 6.58) | 1999 to 2004 | 0.24 (−2.02, 2.55) | 0.812 | −0.40 (−1.82, 1.03) | 0.579 |
| 2004 to 2009 | −3.43 (−6.60, −0.16) | 0.043 | ||||
| 2009 to 2013 | 2.69 (−0.65, 6.14) | 0.100 | ||||
| New Jersey | 6.03 (5.86, 6.20) | 1999 to 2013 | −0.96 (−1.66, −0.25) | 0.012 | −0.96 (−1.66, −0.25) | 0.012 |
| California | 5.85 (5.76, 5.94) | 1999 to 2013 | −0.62 (−1.04, −0.20) | 0.008 | −0.62 (−1.04, −0.20) | 0.008 |
APC, annual percent change; AAPC, average annual percent change; CI, confidence interval; IR, incidence rate; USCS, United States Cancer Statistics.
States with missing incidence rate for consecutive or more than 3 intermittent years were excluded.
Age-adjusted incidence rate per 100 000; direct adjustment performed using the 2000 US Standard population.
A rapidly increasing trend within the past 5 years (2009–13) was mostly observed in Midwestern states including Ohio, Kentucky and Minnesota (Table 5). Among males, gastric cancer incidence increased by 3.92% (95% CI: 0.59, 7.35) per year in Oregon, and by 3.08% (95% CI: −0.28, 6.55) per year in Ohio. The recent increasing trend was less pronounced among females and ranged from 0.82% to 2.69% among the top five states (Table 5). States with the highest increasing trend in the past 5 years among persons aged ≥50 years also came from the Midwestern region (Supplementary Table 6, available as Supplementary data at IJE online). For females aged <50 years, California and Texas are states with both historically high gastric cancer incidence rates and high AAPC over the past 5 years (Supplementary Tables 5 and 7, available as Supplementary data at IJE online).
Table 5.
Annual and average annual percent change in gastric cancer incidence rates among top five states with 5-year largest average annual percent increase (2009-13): USCS Registry Data 1999–2013
| Statesa | Incident cases in 2013 | Population in 2013 | 2013 age-adjusted IR/100 000 (95% CI)b | AAPC (95% CI) | P-value |
|---|---|---|---|---|---|
| Overall | |||||
| Ohio | 942 | 11 572 005 | 6.77 (6.33, 7.22) | 2.73 (−0.02, 5.57) | 0.052 |
| Kentucky | 342 | 4 399 583 | 6.66 (5.96, 7.43) | 2.21 (0.28, 4.18) | 0.029 |
| Minnesota | 361 | 5 422 060 | 5.92 (5.31, 6.58) | 1.79 (−0.02, 3.64) | 0.052 |
| New York | 2 058 | 19 695 680 | 9.08 (8.68, 9.48) | 0.99 (−1.67, 3.72) | 0.470 |
| West Virginia | 151 | 1 853 595 | 6.10 (5.15, 7.20) | 0.77 (−0.50, 2.06) | 0.215 |
| Male | |||||
| Oregon | 190 | 1 942 495 | 8.72 (7.50, 10.10) | 3.92 (0.59, 7.35) | 0.025 |
| Ohio | 611 | 5 660 612 | 9.85 (9.07, 10.69) | 3.08 (−0.28, 6.55) | 0.073 |
| Minnesota | 238 | 2 693 165 | 8.54 (7.46, 9.73) | 1.86 (−0.61, 4.40) | 0.126 |
| New York | 1243 | 9 550 834 | 12.56 (11.86, 13.30) | 0.69 (−1.93, 3.38) | 0.609 |
| Tennesseans | 280 | 3 166 370 | 8.34 (7.36, 9.41) | 0.60 (−0.74, 1.94) | 0.339 |
| Female | |||||
| New York | 815 | 10 144 846 | 6.40 (5.96, 6.87) | 2.69 (−0.65, 6.14) | 0.100 |
| Minnesota | 123 | 2 728 895 | 3.85 (3.18, 4.62) | 1.51 (−0.30, 3.36) | 0.094 |
| New Hampshire | 35 | 669 630 | 4.14 (2.85, 5.87) | 1.03 (−0.99, 3.08) | 0.293 |
| West Virginia | 58 | 938 460 | 4.37 (3.29, 5.73) | 1.02 (−1.43, 3.52) | 0.389 |
| North Carolina | 278 | 5 049 628 | 4.48 (3.96, 5.05) | 0.82 (−0.13, 1.78) | 0.084 |
AAPC, average annual percent change; CI, confidence interval; IR, incidence rate; USCS, United States Cancer Statistics.
States with missing incidence rate for: (i) any single year between 2009 and 2013; (ii) consecutive years; or (iii) more than 3 intermittent years between 1999 and 2008 were excluded.
Direct adjustment performed using the 2000 US Standard population.
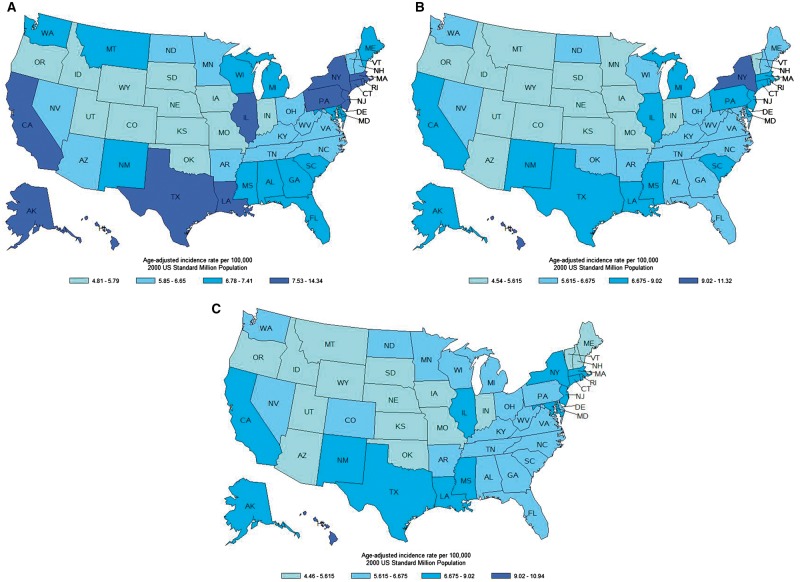
As shown in the state-level heat maps, overall gastric cancer incidence rates decreased between 1999 and 2003 and 2009 and 2013 (Figure 1). For the period 1999 to 2003, only 11 states had an incidence rate <5.8 per 100 000 (the lowest category of the heat map). The number of states in this lowest category increased to 15 for the period 2004 to 2008 and to 16 for the period 2009 to 2013 (Figure 1). Similarly for persons aged ≥50 years, there were 12 states in this lowest incidence category for the period from 1999 to 2003, increasing to 21 states in the lowest category for the period from 2009 to 2013 (Supplementary Figure 1, available as Supplementary data at IJE online). Conversely, gastric cancer incidence rates among persons aged <50 years increased (Supplementary Figure 2, available as Supplementary data at IJE online). There were 12 states classified into the lowest category in the heat map in 1999–2003, and the number decreased to nine states in 2009–13 (Supplementary Figure 2, available as Supplementary data at IJE online).
Figure 1.
State-level age-adjusted gastric cancer incidence rates per 100 000 among all persons by 5-year intervals: A, 1999–2003; B, 2004–08; C, 2009–13.
Discussion
In this large population-based study using cancer incidence data from all 50 US states, we showed that the overall age-adjusted incidence rates for gastric cancer decreased in the USA between 1999 and 2013 from 7.64 per 100 000 to 6.55 per 100 000. However, most of the decrease had occurred by 2007, and the incidence rates remained essentially unchanged between 2007 and 2013. Furthermore, whereas incidence rates among persons aged ≥50 years decreased, incidence rates have increased among persons aged <50 years. The fastest increases in gastric cancer incidence rates were seen among females and non-Hispanic Whites. Among persons aged <50 years, incidence increased in all regions of the USA, with the highest annual change observed in the Midwest (1.59% per year from 1999 to 2013). At the state level, California and Texas were among the top five states with both historically high gastric cancer burden and rapidly increasing incidence rates during past 5 years.
A previous study using SEER registries data found increasing gastric cancer incidence rates between 1992 and 2011 among young Hispanic males (APC = 1.55, 95% CI: 0.26, 2.86), but not among the overall population aged 20–49 years (AAPC = 0.33, 95% CI: −0.12, 0.78).12 In our study using both SEER and NPCR data, we detected an overall increasing trend among persons aged <50 years. Instead of Hispanic males, we found the increasing trend among non-Hispanic White and Hispanic females. Consistent with previous findings that gastric cancer incidence increased among Hispanic females in California (AAPC = 3.0, 95% CI: 0.7, 5.3),14 we also found evidence for increasing incidence of gastric cancer among females in California (AAPC = 1.77%). This increasing trend among females was observed for both cardia and non-cardia gastric cancers, as shown from the SEER data. For cardia gastric cancer, the increasing obesity epidemic is one of the possible explanations for the increasing trend among females. Based on data from the National Health and Nutrition Examination Survey, the prevalence of obesity is 26.9% in non-Hispanic White females and is 34.4% among Hispanic females aged 20–39 years in the USA. Higher prevalence of H. pylori infection among Hispanics than among other ethnicities could also explain the increasing rates of overall19 and especially non-cardia gastric cancer.20,21
Among states and districts with historically high burdens of gastric cancer among males, incidence rates for gastric cancer may have plateaued. On the other hand, incidence rates continue to increase for states and districts with historically high incidence rates among females, including California, New Jersey and Texas. One of the possible explanations is the sharp rise in the Hispanic female population, who have increasing rates, in these particular states. From 1999 to 2013, the Hispanic female population increased by 30.1% and 50.9% in California and Texas, respectively. The rapid increase in this high-risk population group likely plays a role in making California and Texas among the top five states with highest AAPC within the past 5 years.
A rapid increase in gastric cancer incidence was observed in states with historically low to moderate gastric cancer incidence rates, such as Kentucky, Minnesota, Ohio, Tennessee (in males) and Oregon (in males). These are Midwestern and northern plain regions, where cardia gastric cancer rates are also increasing (AAPC = 2.52, 95% CI: −0.01, 5.21). There is a high proportion of non-Hispanic Whites in these states and there is some evidence that the incidence of cardia gastric cancer is also increasing (AAPC = 1.56, 95% CI: −0.20, 3.36).
A major strength of our study was that the data used are representative of the entire US population. The larger sample size and greater representation of younger and racial minority cancer cases as well as geographical regions enabled us to more comprehensively describe recent gastric cancer trends in the USA in all subgroups. This is vital, as we focused on the population aged <50 years where gastric cancer developed less frequently than among their elderly counterparts. Although no age-related trend was found using SEER data, we found an increasing trend of gastric cancer among population aged <50 years from USCS data. Another advantage of USCS data is the availability of state-level information on annual incidence. This allowed for in-depth examination of geographical variation of disease burden over time periods.
One of the limitations of our study is the unavailability of anatomical site or histology type information from the USCS registry. Thus, we could not directly assess the secular trend and burden of gastric cancer by further breaking down into more refined disease categories. However we also used SEER data, which had histology and site information, to conduct secondary analysis, and our findings were verified by the results using this approach. Neither USCS nor SEER provided information on established risk factors for gastric cancer such as H. pylori infection, smoking, obesity, heavy alcohol consumption and physical inactivity. Therefore, we could not directly assess or attribute the variation in gastric cancer incidence and trends between gender, race/ethnicities and geographical regions to these risk factors.
In summary, this population-based, 50-state descriptive study has confirmed the overall decrease in gastric cancer incidence rates in the USA. However, the rate of decline in incidence rates has slowed in more recent years. Furthermore, non-cardia gastric cancer incidence rates are increasing among persons aged <50 years, especially among females. Likely reflecting the rapidly expanding young Hispanic population in certain regions in the USA, the largest overall increases in rates were seen in Texas and California. States with high and increasing non-cardia gastric cancer incidence rates should address provisions for the detection and treatment of underlying risk factors, including H. pylori screening and treatment.
Supplementary Data
Supplementary data are available at IJE online.
Funding
Z.W. is supported by a Research Training Grant from the Cancer Prevention and Research Institute of Texas (CPRIT; RP160097). H.B.E-S. is supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK K24–04-107).
Conflict of interest: None declared.
Supplementary Material
References
- 1. Ferlay J, Soerjomataram I, Ervik M. et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 Lyon, France: International Agency for Research on Cancer, 2013.
- 2.Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence—SEER 9 Regs Research Data, Nov 2016 Sub (1973–2014) <Katrina/Rita Population Adjustment>—Linked To County Attributes—Total U.S., 1969–2015 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2017, based on the November 2016 submission. http://www.seer.cancer.gov.
- 3. Conteduca V, Sansonno D, Lauletta G, Russi S, Ingravallo G, Dammacco F.. H. pylori infection and gastric cancer: state of the art (review). Int J Oncol 2013;42:5–18. [DOI] [PubMed] [Google Scholar]
- 4. Ladeiras-Lopes R, Pereira AK, Nogueira A. et al. Smoking and gastric cancer: systematic review and meta-analysis of cohort studies. Cancer Causes Control 2008;19:689–701. [DOI] [PubMed] [Google Scholar]
- 5. Tramacere I, Negri E, Pelucchi C. et al. A meta-analysis on alcohol drinking and gastric cancer risk. Ann Oncol 2012;23:28–36. [DOI] [PubMed] [Google Scholar]
- 6. Yang P, Zhou Y, Chen B. et al. Overweight, obesity and gastric cancer risk: results from a meta-analysis of cohort studies. Eur J Cancer 2009;45:2867–73. [DOI] [PubMed] [Google Scholar]
- 7. Zhu H, Yang X, Zhang C. et al. Red and processed meat intake is associated with higher gastric cancer risk: a meta-analysis of epidemiological observational studies. PLoS One 2013;8:e70955.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang Q, Chen Y, Wang X, Gong G, Li G, Li C.. Consumption of fruit, but not vegetables, may reduce risk of gastric cancer: results from a meta-analysis of cohort studies. Eur J Cancer 2014;50:1498–509. [DOI] [PubMed] [Google Scholar]
- 9. D’Elia L, Rossi G, Ippolito R, Cappuccio FP, Strazzullo P.. Habitual salt intake and risk of gastric cancer: a meta-analysis of prospective studies. Clin Nutr 2012;31:489–98. [DOI] [PubMed] [Google Scholar]
- 10. Rugge M, Genta RM, Di Mario F. et al. Gastric cancer as preventable disease. Clin Gastroenterol Hepatol 2017;15:1833–43. [DOI] [PubMed] [Google Scholar]
- 11. Wu H, Rusiecki JA, Zhu K, Potter J, Devesa SS.. Stomach carcinoma incidence patterns in the United States by histologic type and anatomic site. Cancer Epidemiol Biomarkers Prev 2009;18:1945–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Merchant SJ, Kim J, Choi AH, Sun V, Chao J, Nelson R.. A rising trend in the incidence of advanced gastric cancer in young Hispanic men. Gastric Cancer 2017;20:226–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.SEER. Population Characteristics of Surveillance , Epidemiology, End Results (SEER) Program https://seer.cancer.gov/registries/data (2 October 2017, date last accessed).
- 14. Chang ET, Gomez SL, Fish K. et al. Gastric cancer incidence among Hispanics in California: patterns by time, nativity, and neighborhood characteristics. Cancer Epidemiol Biomarkers Prev 2012;21:709–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reddy KM, Chang JI, Shi JM, Wu BU.. Risk of gastric cancer among patients with intestinal metaplasia of the stomach in a US Integrated Health Care System. Clin Gastroenterol Hepatol 2016;14:1420–25. [DOI] [PubMed] [Google Scholar]
- 16. U.S. Cancer Statistics Working Group. United States Cancer Statistics 1999–2012 Incidence and Mortality Web-Based Report Washington, DC: US Department of Health and Human Services, 2015.
- 17. Tiwari RC, Clegg LX, Zou Z.. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res 2006;15:547–69. [DOI] [PubMed] [Google Scholar]
- 18. Kim HJ, Fay MP, Feuer EJ, Midthune DN.. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000;19:335–51. [DOI] [PubMed] [Google Scholar]
- 19. Dong E, Duan L, Wu BU.. Racial and ethnic minorities at increased risk for gastric cancer in a regional US population study. Clin Gastroenterol Hepatol 2017;15:511–17. [DOI] [PubMed] [Google Scholar]
- 20. Long Parma D, Muñoz E, Ogden SM. et al. Helicobacter pylori infection in Texas Hispanic and Non-Hispanic White men: implications for gastric cancer risk disparities. Am J Mens Health 2017;11:1039–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sonnenberg A, Turner KO, Spechler SJ, Genta RM.. The influence of Helicobacter pylori on the ethnic distribution of Barrett’s metaplasia. Aliment Pharmacol Ther 2017;45:283–90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.