Abstract
Background
Non-adherence to medications is common and leads to suboptimal outcomes. Non-adherence can be intentional (e.g., deciding to skip dosages) or unintentional (e.g., forgetting), yet few studies have distinguished these reasons. An improved understanding of the reasons for non-adherence could inform the development of effective interventions.
Methods and Results
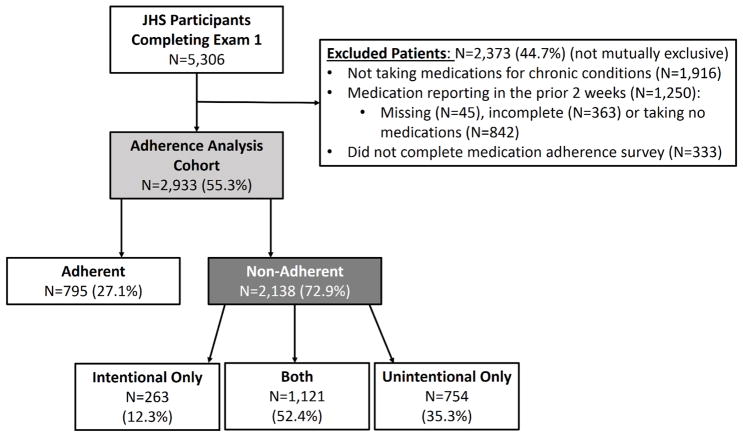
We analyzed data from African Americans in the Jackson Heart Study who were prescribed medications for one or more chronic conditions. Participants were grouped by patient-reported adherence with non-adherence categorized as being intentional, unintentional or both. We used modified Poisson regression models to examine the factors associated with types of non-adherence. Of 2,933 participants taking medication, 2138 (72.9%) reported non-adherence with 754 (35.3%) reporting only unintentional non-adherence, 263 (12.3%) only intentional non-adherence, and 1121 (52.4%) both. Factors independently associated with intentional non-adherence included female sex and depressive symptoms while factors associated with unintentional non-adherence included younger age and separated relationship status. Unintentional and intentional non-adherence was more common among participants taking anti-arrhythmic and anti-asthmatic medications, respectively. Higher levels of global perceived stress was associated with both types of non-adherence. The adjusted models for intentional and unintentional non-adherence had c-statistics of 0.65 and 0.66, respectively, indicating modest discrimination.
Conclusion
Specific patient factors and individual medication classes were associated with distinct patterns of intentional and unintentional non-adherence, yet the overall modest discrimination of the models suggests contributions from other unmeasured factors. These findings provide a construct for understanding reasons for non-adherence and provide rationale to assess whether personalized interventions can improve adherence.
Keywords: medication adherence, intentional, unintentional, African Americans
INTRODUCTION
Medication non-adherence for individuals with chronic conditions may contribute to suboptimal outcomes and increased healthcare costs.1, 2 Medication-taking behaviors are complex and affected by multiple factors at the patient, physician and system level.3 Existing evidence suggests that patient-level factors associated with non-adherence may include increased disease burden, older age, and minority race/ethnicity.4, 5 In a recent analysis evaluating racial differences in medication adherence in a sample of Medicare patients, elderly African Americans reported lower adherence levels than elderly whites with differences persisting after adjustment for sociodemographic variables.6 While racial disparities in medication adherence may be due, in part, to patient-level factors such as comorbidity burden7 and health literacy8, other potential contributing factors to these health disparities have not been fully explored.
Reasons for suboptimal medication adherence can be broadly grouped into intentional and unintentional reasons.9 Intentional non-adherence is an active process where a person chooses to deviate from the prescribed treatment regimen, often as a result of weighing of the perceived risks and benefits associated with treatment.10 Unintentional non-adherence is a result of passive processes including forgetfulness or not taking medication as prescribed due to misunderstanding of instructions. Despite efforts to characterize the prevalence of reasons for non-adherence to medications for chronic conditions, data are limited on reasons for non-adherence particularly among minority populations. Furthermore, few studies have examined whether reasons for non-adherence change over time. Better understanding of intentional and unintentional reasons for non-adherence and whether these reasons vary over time can help inform targeted interventions to promote medication adherence in populations with chronic disease.
We examined the prevalence of non-adherence to medications by type of non-adherence (i.e., only intentional reasons, only non-intentional reasons, both intentional and non-intentional reasons), and reasons for non-adherence in the Jackson Heart Study, a well-characterized, longitudinal cohort of African Americans. In addition, we examined patient-level factors associated with unique medication-taking patterns.
METHODS
Data Sources
The JHS is a prospective community-based observational study of 5,306 African Americans designed to investigate risk factors for cardiovascular disease11. Initiated in 2000, all study participants provided written informed consent, and study protocols were approved by local institutional review boards. Participants were recruited from the Jackson, Mississippi cohort of the Atherosclerosis Risk in Communities study and the overall tricounty population12. Participants completed 3 study visits: exam 1 between 9/2000–3/2004, exam 2 between 10/2005–12/2008, and exam 3 between 2/2009–1/2013. Data collected include demographic characteristics, comorbid conditions, medications, anthropometry and laboratory values13. Of the questionnaires used in JHS, the global perceived stress score is an eight-item questionnaire that measures the perception of the severity of chronic stress over the prior 12 months with scores ranging from 0 to 24 where higher scores indicate increased perceived stress. The social support score ranges from 0 to 5 and is determined from 8 questions related to relationships with family members, a significant other, friends and the community where higher scores indicate greater perceived support. Ongoing surveillance for health outcomes (e.g., myocardial infarction) includes annual telephone follow-up interviews, review of medical records and review of death certificates. The details of visit procedures including medication adherence assessment have been previously described13. The definitions of co-morbidities as well as medication collection and coding have also been reported14, 15.
Study Population
For the present analysis, we included 2,933 JHS participants who completed exam 1, were prescribed medications for one or more chronic conditions and had documentation of medication adherence status. We focused on non-adherence in medication classes for management of common chronic conditions that represent substantial health burden in the JHS population: hypertension, hyperlipidemia, heart failure (HF), coronary artery disease (CAD), stroke, diabetes, chronic obstructive pulmonary disease (COPD) and depressive symptoms. We excluded participants who did not complete the exam 1 medication survey and those with incomplete recording of medication use during the two weeks preceding the exam 1 visit. Baseline characteristics of participants taking medications for chronic conditions who did not complete the medication adherence survey are provided in Supplemental Table 1. The follow-up evaluations included participants with data collected at exams 2 and 3 with similar exclusion criteria as at the baseline assessment.
Medication non-adherence
The study outcome of interest was patient-reported adherence. At each exam, patients were asked about their “usual medication taking behaviors” without a specific time period of assessment (i.e., during the past 2 or 4 weeks). Eleven different medication adherence questions were grouped into intentional vs. unintentional reasons per discussion with coauthors and external subject matter experts (Table 1). In brief, intentional reasons included not wanting to take medications, perceptions of inconvenience, ineffectiveness, and concern of addiction, as well as side effects related to feeling bad or limiting normal daily activities. Unintentional reasons were not having the medication available, not having money to purchase medications and “being in a hurry” or forgetting.
Table 1.
Medication questions used to characterize adherence status stratified by intentional and unintentional reasons.
| Baseline Medication Adherence Status | Definition/Assessment |
|---|---|
| Intentional Non-adherence | Answered ‘yes’ to any of the following on the exam 1 medication survey:
|
| Unintentional Non-adherence | Answered ‘yes’ to any of the following on the exam 1 medication survey:
|
| Both Intentional and Unintentional Non-adherent | Answered ‘yes’ to at least one intentional and unintentional non-adherence question above. |
| Adherent | Answered ‘no’ to all medication adherence questions |
Covariates
Variables of interest from the baseline clinical exam included demographics (age, sex, marital and insurance status), socioeconomic factors (education, family income), psychosocial factors (stress, social support, depression), health behaviors (tobacco use, alcohol use, physical activity), comorbidities (hypertension, diabetes, chronic kidney disease [CKD], myocardial infarction [MI], stroke, heart failure), anthropometry (height, weight, waist circumference), medication class (cardiovascular, pulmonary, diabetes, depression medications) and total number of prescribed medications. Covariates were selected for inclusion based on review of prior studies and clinical judgment.
Statistical Analysis
We calculated baseline (exam 1) characteristics of the study population by medication adherence status at baseline (adherent and non-adherent, separately) using frequencies with percentages for categorical variables and means with standard deviations or medians with interquartile range (IQR) for continuous variables. We tested for differences in baseline characteristics by adherence status using chi-square tests for categorical variables and Kruskal-Wallis tests for continuous variables.
Among non-adherent participants, we calculated the distribution of baseline characteristics by reasons for non-adherence (intentional only, unintentional only, and both intentional and unintentional reasons) at baseline and determined the statistical significance of differences across reasons for non-adherence using chi-square tests for categorical variables and Kruskal-Wallis tests for continuous variables. Within the non-adherent cohort, we calculated the frequency of reasons for non-adherence by medication class (non-mutually exclusive classes: cardiovascular, pulmonary, diabetes, anti-depression, multiple classes [taking medications for management of more than one of the chronic disease types of interest (pulmonary, CVD, diabetes, depression)]). Since we evaluated data on chronic disease groups that are not mutually exclusive, we did not compare reasons for non-adherence across classes with a formal statistical test (which assumes independence between groups). However, in a secondary analysis we separated participants into non-overlapping groups and compared reasons for non-adherence using chi-square tests (Supplemental Table 2).
To identify the factors associated with intentional and unintentional non-adherence at baseline, we used separate modified Poisson regression models16. Due to high rates of intentional and unintentional non-adherence (>40%), we used modified Poisson regression to approximate risk ratios in lieu of logistic regression. Log-binomial regression models were tested but did not converge. We estimated up to 187 degrees of freedom (df) allowed based on 1875 intentional events and up to 138 df based on 1384 unintentional events. Candidate variables associated with unintentional and intentional medication non-adherence included age, sex, marital status, insurance, BMI, waist circumference, current smoking, prior smoking, alcoholic drinks/week, physical activity hours/week, CKD, COPD, diabetes or HbA1c, heart failure, hypertension or systolic/diastolic blood pressure, MI, stroke, education, family income, stress, social support, depression, ACE/ARB, anti-arrhythmic, anti-asthmatic, anti-cholinergic, anti-coagulant, anti-depressant, anti-hyperlipidemic, anti-hypertensive, anti-platelet, beta-blocker, calcium channel blocker, digoxin, diuretic, insulin, nitrates, oral anti-diabetic, and taking multiple chronic medications [more than one of the 16 chronic medications examined]. We tested for multicollinearity and eliminated candidate variables where variance inflation factor was > 3. To examine unadjusted associations, each candidate variable was included as the sole independent variable in separate models. To examine multivariable adjusted associations and address potential confounding, all variables were included as covariates in a single model.
In addition, to explore whether underlying diseases may be modifying these associations, we performed a sensitivity analysis stratified by the presence of depressive symptoms at baseline. Furthermore, in order to explore whether the variables associated with non-adherence vary based on the specific reason for non-adherence, we performed an additional exploratory analysis examining the factors associated with the 2 most common intentional non-adherence reasons: (1) “Makes me feel bad” and (2) “Trying to do without” as well as the 2 most common unintentional reasons: (1) “In a hurry, too busy, forgot to take” and (2) “Did not have medication available”.
We calculated the proportion of non-adherent participants at exam 1 who reported intentional only, unintentional only or both intentional and unintentional reasons for medication non-adherence and the mean number of reported reasons for non-adherence overall and in each group. Among non-adherent participants at exam 1, we compared the proportion reporting intentional only, unintentional only or both unintentional and intentional reasons for non-adherence at the baseline examination with the proportions at visits 2 and 3. We also examined adherence status among all participants across exams to evaluate stability in this classification over time.
Most variables had very low missing rates (<5%). For variables that had low rates of missingness (i.e., < 5% of records), we imputed continuous variables to the overall median value, dichotomous variables to ‘no’ and multichotomous variables to the most frequent categorical value. For variables with >5% missing (e.g, family income ~15% missing, depression ~30% missing) we treated the missing values as a separate category. We used a 2-tailed α = .05 to establish statistical significance and will report 95% confidence intervals. All analyses were performed with SAS version 9.4 (SAS Institute Inc, Cary, NC). The institutional review board of the Duke University Health System approved the study.
Results
Figure 1 presents the details for the analysis cohort using self-reported adherence data from the baseline exam. Of 2,933 participants routinely taking medications at baseline, 2138 (72.9%) reported non-adherence. Of these participants, 754 (35.3%) reported only unintentional non-adherence, 263 (12.3%) reported only intentional non-adherence, and 1121 (52.4%) both intentional and unintentional non-adherence.
Figure 1.
Study cohort from the Jackson Heart Study (JHS). Note that of the 333 participants not completing the adherence survey, there were only 47 with complete medication and documented chronic medications who then did not complete the adherence survey.
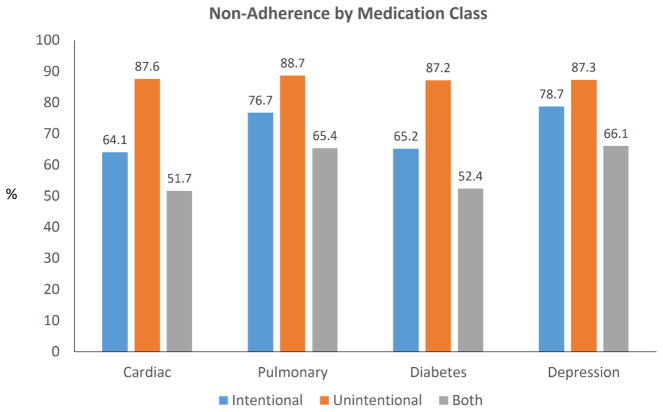
Table 2 presents the baseline characteristics by adherence status. Compared with those reporting complete adherence, participants reporting non-adherence were younger, more often women, uninsured and had more comorbidities including hypertension, depression, and heart failure. The number and classes of medication being taken was similar between groups. Participants reporting intentional non-adherence were on average older, more often women and had lower global perceived stress scores compared with those reporting unintentional non-adherence. Depression was more common in those with intentional non-adherence compared to those reporting unintentional non-adherence. Intentional non-adherence was higher in participants taking pulmonary and antidepressive therapies compared with cardiac and diabetes medications (~77% vs. 65%) (Figure 2 and Table 3) Unintentional non-adherence was high across the different medication classes including those used for the treatment of cardiovascular and pulmonary disease as well as diabetes and depression (~88% of non-adherent patients).
Table 2.
Baseline characteristics of the study population by adherence status.
| Adherent | Non-Adherent | Adherent vs. Non-adherent p-value |
Type of Non-Adherence | Comparison of 3 non-adherence groups p-value |
|||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Intentional Only | Unintentional Only | Both intentional and unintentional | |||||
| N | 795 | 2,138 | 263 | 754 | 1,121 | ||
| Demographics | |||||||
| Age, median (IQR), y | 62.8 (53.9, 69.4) | 59.8 (51.1, 66.9) | < .001 | 62.7 (56.0, 70.1) | 60.3 (51.8, 67.4) | 58.8 (50.2, 66.1) | < .001 |
| Male sex, No. (%) | 291 (36.6) | 639 (29.9) | < .001 | 72 (27.4) | 265 (35.1) | 302 (26.9) | < .001 |
| Marital status, No. (%) | .33 | .002 | |||||
| Divorced | 120 (15.1) | 317 (14.8) | 33 (12.5) | 103 (13.7) | 181 (16.1) | ||
| Married | 433 (54.5) | 1,135 (53.1) | 147 (55.9) | 414 (54.9) | 574 (51.2) | ||
| Never been married | 75 (9.4) | 208 (9.7) | 15 (5.7) | 60 (8.0) | 133 (11.9) | ||
| Separated | 22 (2.8) | 96 (4.5) | 8 (3.0) | 34 (4.5) | 54 (4.8) | ||
| Widowed | 145 (18.2) | 382 (17.9) | 60 (22.8) | 143 (19.0) | 179 (16.0) | ||
| Insurance status, No. (%) | .047 | .11 | |||||
| Uninsured | 72 (9.1) | 252 (11.8) | 24 (9.1) | 89 (11.8) | 139 (12.4) | ||
| Any Medicaid reported | 136 (17.1) | 314 (14.7) | 39 (14.8) | 94 (12.5) | 181 (16.1) | ||
| Other | 587 (73.8) | 1,572 (73.5) | 200 (76.0) | 571 (75.7) | 801 (71.5) | ||
| Socioeconomic, No. (%) | |||||||
| Education | .31 | .30 | |||||
| Less than high school | 176 (22.1) | 490 (22.9) | .65 | 71 (27.0) | 179 (23.7) | 240 (21.4) | |
| High school graduate | 319 (40.1) | 860 (40.2) | .96 | 95 (36.1) | 291 (38.6) | 474 (42.3) | |
| College degree | 146 (18.4) | 432 (20.2) | .27 | 54 (20.5) | 149 (19.8) | 229 (20.4) | |
| Graduate or professional degree | 154 (19.4) | 356 (16.7) | .08 | 43 (16.3) | 135 (17.9) | 178 (15.9) | |
| Family income | .29 | .14 | |||||
| <$20,000 | 227 (28.6) | 590 (27.6) | 69 (26.2) | 203 (26.9) | 318 (28.4) | ||
| $20,000–$50,000 | 240 (30.2) | 656 (30.7) | 90 (34.2) | 215 (28.5) | 351 (31.3) | ||
| $50,000–$75,000 | 116 (14.6) | 287 (13.4) | 29 (11.0) | 121 (16.0) | 137 (12.2) | ||
| >$75,000 | 103 (13.0) | 248 (11.6) | 26 (9.9) | 97 (12.9) | 125 (11.2) | ||
| Missing | 109 (13.7) | 357 (16.7) | 49 (18.6) | 118 (15.6) | 190 (16.9) | ||
| Psychosocial | |||||||
| Global Perceived Stress Score [0–24], median (25th,75th) | 3.0 (0.0, 5.0) | 4.0 (2.0, 8.0) | < .001 | 3.0 (1.0, 6.0) | 4.0 (1.0, 7.0) | 5.0 (2.0, 9.0) | < .001 |
| Social support [0–5], median (25th,75th) | 4.0 (4.0, 5.0) | 4.0 (4.0, 5.0) | .91 | 4.0 (4.0, 5.0) | 4.0 (4.0, 5.0) | 4.0 (4.0, 5.0) | .78 |
| Depression, No. (%) | < .001 | < .001 | |||||
| None | 423 (53.2) | 995 (46.5) | 132 (50.2) | 380 (50.4) | 483 (43.1) | ||
| Minor depression | 51 (6.4) | 158 (7.4) | 21 (8.0) | 37 (4.9) | 100 (8.9) | ||
| Major depression | 35 (4.4) | 195 (9.1) | 25 (9.5) | 42 (5.6) | 128 (11.4) | ||
| Missing | 286 (36.0) | 790 (37.0) | 85 (32.3) | 295 (39.1) | 410 (36.6) | ||
| Health Behaviors | |||||||
| Alcoholic drinks per week, median (25th,75th) | 0.0 (0.0, 0.1) | 0.0 (0.0, 0.1) | .05 | 0.0 (0.0, 0.1) | 0.0 (0.0, 0.2) | 0.0 (0.0, 0.1) | .34 |
| Physical activity, hours/week, No. (%) | .13 | .84 | |||||
| None | 397 (49.9) | 1,103 (51.6) | 129 (49.0) | 380 (50.4) | 594 (53.0) | ||
| <1 hour | 90 (11.3) | 212 (9.9) | 25 (9.5) | 72 (9.5) | 115 (10.3) | ||
| 1– <2 hours | 128 (16.1) | 317 (14.8) | 44 (16.7) | 111 (14.7) | 162 (14.5) | ||
| 2– <3 hours | 53 (6.7) | 169 (7.9) | 23 (8.7) | 65 (8.6) | 81 (7.2) | ||
| 3– <4 hours | 37 (4.7) | 137 (6.4) | 20 (7.6) | 47 (6.2) | 70 (6.2) | ||
| 4+ hours | 90 (11.3) | 200 (9.4) | 22 (8.4) | 79 (10.5) | 99 (8.8) | ||
| Current smoker | 77 (9.7) | 246 (11.5) | .16 | 32 (12.2) | 87 (11.5) | 127 (11.3) | .93 |
| Prior smoker | 179 (22.5) | 486 (22.7) | .90 | 57 (21.7) | 179 (23.7) | 250 (22.3) | .70 |
| Medical History, No. (%) | |||||||
| Chronic kidney disease | 35 (4.4) | 144 (6.7) | .02 | 16 (6.1) | 49 (6.5) | 79 (7.0) | .81 |
| Chronic lung disease | 59 (7.4) | 182 (8.5) | .34 | 17 (6.5) | 45 (6.0) | 120 (10.7) | < .001 |
| Diabetes | 257 (32.3) | 692 (32.4) | .98 | 96 (36.5) | 245 (32.5) | 351 (31.3) | .27 |
| Heart failure | 72 (9.1) | 304 (14.2) | < .001 | 38 (14.4) | 86 (11.4) | 180 (16.1) | .02 |
| Hypertension | 635 (79.9) | 1,814 (84.8) | .001 | 215 (81.7) | 649 (86.1) | 950 (84.7) | .24 |
| Myocardial infarction | 64 (8.1) | 170 (8.0) | .93 | 21 (8.0) | 62 (8.2) | 87 (7.8) | .94 |
| Stroke | 56 (7.0) | 126 (5.9) | .25 | 18 (6.8) | 41 (5.4) | 67 (6.0) | .70 |
| Anthropometry, median, (25th,75th) | |||||||
| Height, cm | 168.0 (162.0, 175.0) | 167.0 (161.0, 174.0) | .07 | 166.0 (160.0, 173.0) | 168.0 (161.0, 175.0) | 167.0 (161.0, 174.0) | .01 |
| Weight, kg | 87.0 (76.0, 99.2) | 89.7 (77.7, 104.7) | .001 | 87.6 (76.0, 100.3) | 88.9 (78.0, 104.0) | 91.0 (78.0, 105.6) | .06 |
| Waist circumference, cm | 100.0 (92.0, 110.0) | 102.0 (93.0, 114.0) | < .001 | 102.0 (94.0, 111.0) | 102.0 (92.0, 113.0) | 103.0 (93.0, 114.0) | .34 |
| BMI, kg/m2 | 30.5 (27.1, 34.9) | 31.6 (27.8, 36.8) | < .001 | 30.8 (27.9, 35.5) | 31.1 (27.5, 36.3) | 32.2 (28.0, 37.4) | .01 |
| Labs/physical exam, median, (25th,75th) | |||||||
| Systolic blood pressure, mmHg | 127.5 (117.4, 138.5) | 128.4 (119.2, 139.4) | .01 | 129.3 (120.2, 139.4) | 128.4 (119.2, 139.4) | 128.4 (119.2, 140.3) | .73 |
| Diastolic blood pressure, mmHg | 75.0 (68.4, 80.9) | 75.9 (70.1, 81.7) | .006 | 74.2 (68.4, 80.0) | 75.9 (70.1, 81.7) | 75.9 (70.1, 81.7) | .03 |
| HbA1c, % | 5.8 (5.5, 6.4) | 5.8 (5.5, 6.5) | .79 | 5.9 (5.5, 6.7) | 5.8 (5.5, 6.5) | 5.8 (5.5, 6.4) | .73 |
| Medications, No. (%) | |||||||
| Cardiovascular medications | 758 (95.3) | 2,038 (95.3) | .98 | 252 (95.8) | 732 (97.1) | 1,054 (94.0) | .008 |
| ACE-inhibitor/ARB | 219 (27.5) | 603 (28.2) | .72 | 65 (24.7) | 239 (31.7) | 299 (26.7) | .02 |
| Anti-arrhythmic | 2 (0.3) | 17 (0.8) | .10 | 2 (0.8) | 10 (1.3) | 5 (0.4) | .11 |
| Anti-coagulant | 17 (2.1) | 58 (2.7) | .38 | 8 (3.0) | 20 (2.7) | 30 (2.7) | .94 |
| Anti-hyperlipidemic | 168 (21.1) | 437 (20.4) | .68 | 64 (24.3) | 161 (21.4) | 212 (18.9) | .11 |
| Anti-hypertensive | 419 (52.7) | 1,156 (54.1) | .51 | 133 (50.6) | 433 (57.4) | 590 (52.6) | .06 |
| Anti-platelet (any) | 349 (43.9) | 752 (35.2) | < .001 | 91 (34.6) | 284 (37.7) | 377 (33.6) | .20 |
| Beta-blocker | 129 (16.2) | 374 (17.5) | .42 | 44 (16.7) | 163 (21.6) | 167 (14.9) | < .001 |
| Calcium channel blocker | 211 (26.5) | 603 (28.2) | .37 | 85 (32.3) | 218 (28.9) | 300 (26.8) | .17 |
| Digoxin | 22 (2.8) | 51 (2.4) | .56 | 3 (1.1) | 20 (2.7) | 28 (2.5) | .36 |
| Diuretic | 296 (37.2) | 857 (40.1) | .16 | 116 (44.1) | 289 (38.3) | 452 (40.3) | .25 |
| Nitrate | 29 (3.6) | 86 (4.0) | .64 | 9 (3.4) | 31 (4.1) | 46 (4.1) | .87 |
| Pulmonary medications | 38 (4.8) | 133 (6.2) | .14 | 15 (5.7) | 31 (4.1) | 87 (7.8) | .005 |
| Anti-asthmatic | 38 (4.8) | 133 (6.2) | .14 | 15 (5.7) | 31 (4.1) | 87 (7.8) | .005 |
| Anti-cholinergic | 2 (0.3) | 12 (0.6) | .28 | 0 (0.0) | 6 (0.8) | 6 (0.5) | .33 |
| Diabetes medications | 209 (26.3) | 531 (24.8) | .42 | 68 (25.9) | 185 (24.5) | 278 (24.8) | .91 |
| Oral anti-diabetic | 150 (18.9) | 382 (17.9) | .53 | 53 (20.2) | 140 (18.6) | 189 (16.9) | .37 |
| Insulin | 92 (11.6) | 212 (9.9) | .19 | 21 (8.0) | 62 (8.2) | 129 (11.5) | .04 |
| Anti-depressant medications | 73 (9.2) | 221 (10.3) | .35 | 28 (10.6) | 47 (6.2) | 146 (13.0) | < .001 |
| Chronic medication count, median (25th,75th) | 2.0 (1.0, 4.0) | 2.0 (1.0, 4.0) | .57 | 2.0 (1.0, 4.0) | 2.0 (1.0, 4.0) | 2.0 (1.0, 4.0) | .52 |
| Taking multiple chronic medications*, No. (%) | 540 (67.9) | 1,531 (71.6) | .05 | 187 (71.1) | 546 (72.4) | 798 (71.2) | .83 |
| Multiple medication classes**, No. (%) | 250 (31.4) | 685 (32.0) | .76 | 88 (33.5) | 218 (28.9) | 379 (33.8) | .07 |
| Number of reported non-adherence reasons, mean (SD), median (25th,75th) | - - |
3.0 (2.1) 2.0 (1.0, 4.0) |
1.7 (0.9) 1.0 (1.0, 2.0) |
1.4 (0.7) 1.0 (1.0, 2.0) |
4.3 (2.0) 4.0 (3.0, 5.0) |
< .001 | |
Values presented as median (IQR), mean (SD) or No. (%).
Abbreviations:
Multiple chronic medications = taking >1 of the 16 types of chronic medications of interest
Multiple medication classes = taking medications for management of more than one of the chronic disease types of interest (pulmonary, CVD, diabetes, depression)
Figure 2.
Non-adherence reasons by medication class.
Sample sizes for each medication class: cardiovascular, n=2038; pulmonary, n=133; diabetes, n=221; depression, n=685.
Table 3.
Frequency of non-adherence reasons by medication class.
| Medication class | |||||
|---|---|---|---|---|---|
|
| |||||
| Cardiovascular | Pulmonary | Diabetes | Anti-depression | Multiple | |
| N | 2,038 | 133 | 531 | 221 | 685 |
| Intentional non-adherence | 1,306 (64.1) | 102 (76.7) | 346 (65.2) | 174 (78.7) | 467 (68.2) |
| Inconvenient to take | 434 (21.3) | 44 (33.1) | 139 (26.2) | 70 (31.7) | 183 (26.7) |
| Would not do any good-did not take | 304 (14.9) | 30 (22.6) | 77 (14.5) | 47 (21.3) | 107 (15.6) |
| Medication made you feel bad-did not take | 550 (27.0) | 54 (40.6) | 139 (26.2) | 86 (38.9) | 203 (29.6) |
| Cannot carry out normal activities | 481 (23.6) | 37 (27.8) | 127 (23.9) | 79 (35.7) | 182 (26.6) |
| Thought you might become addicted | 295 (14.5) | 30 (22.6) | 73 (13.7) | 56 (25.3) | 120 (17.5) |
| Do not like to take medicine | 251 (12.3) | 21 (15.8) | 38 (7.2) | 33 (14.9) | 67 (9.8) |
| Trying to do without taking medications | 681 (33.4) | 63 (47.4) | 154 (29.0) | 107 (48.4) | 232 (33.9) |
| Other reasons for not taking medications | 118 (5.8) | 7 (5.3) | 28 (5.3) | 14 (6.3) | 39 (5.7) |
| Unintentional non-adherence | 1,786 (87.6) | 118 (88.7) | 463 (87.2) | 193 (87.3) | 597 (87.2) |
| In a hurry, too busy, forgot to take | 1,509 (74.0) | 99 (74.4) | 376 (70.8) | 154 (69.7) | 483 (70.5) |
| No money to purchase medication | 608 (29.8) | 51 (38.3) | 194 (36.5) | 91 (41.2) | 264 (38.5) |
| Did not have medication available | 756 (37.1) | 56 (42.1) | 213 (40.1) | 91 (41.2) | 284 (41.5) |
| Intentional + Unintentional non-adherence | 1,054 (51.7) | 87 (65.4) | 278 (52.4) | 146 (66.1) | 379 (55.3) |
Participants could be in more than one medication class.
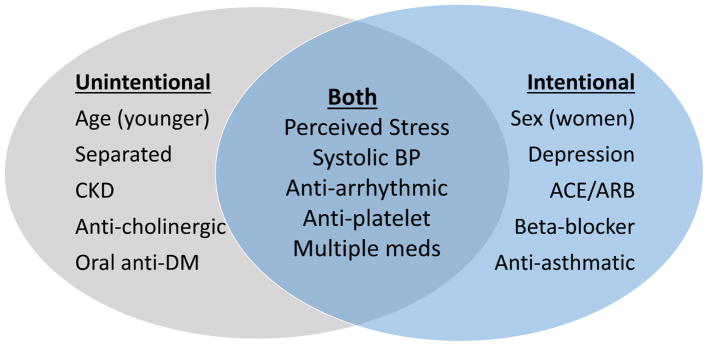
Table 4 summarizes the overall results of unadjusted and adjusted models examining factors associated with intentional and unintentional non-adherence (see Supplemental Table 3 for full details). Female sex and depression were associated with intentional non-adherence, while younger age and separated relationship status were associated with unintentional non-adherence. Oral anti-diabetes medications and beta-blockers were associated with lower unintentional and intentional non-adherence, respectively. Anti-arrhythmics and anti-asthmatics were associated with higher unintentional and intentional non-adherence, respectively. Global perceived stress and taking multiple chronic medications was associated with both types of non-adherence. Figure 3 lists the factors associated with the different forms of non-adherence. The adjusted models for intentional and non-intentional non-adherence had c-statistics of 0.65 and 0.66, respectively.
Table 4.
Factors associated with intentional and unintentional non-adherence.*
| Intentional Non-Adherence Risk Ratio (95% CI) | Adjusted p-value |
Unintentional Non-Adherence Risk Ratio (95% CI) | Adjusted p-value |
|||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||
| Age, per 5 years | 0.96 (0.95,0.98) | 0.99 (0.97,1.01) | .36 | 0.96 (0.95,0.97) | 0.97 (0.95,0.98) | < .001 |
| Male sex | 0.80 (0.73,0.87) | 0.87 (0.79,0.96) | .005 | 0.93 (0.88,0.99) | 0.96 (0.90,1.03) | .23 |
| Marital status - Married (reference) | ||||||
| Divorced | 1.06 (0.95,1.19) | 1.04 (0.91,1.18) | .57 | 1.03 (0.95,1.12) | 1.03 (0.94,1.12) | .58 |
| Never been married | 1.14 (1.01,1.29) | 1.04 (0.90,1.20) | .58 | 1.08 (0.99,1.18) | 1.00 (0.90,1.11) | .93 |
| Separated | 1.14 (0.95,1.37) | 1.04 (0.85,1.27) | .72 | 1.18 (1.06,1.32) | 1.13 (1.00,1.28) | .048 |
| Widowed | 0.99 (0.89,1.10) | 1.00 (0.87,1.14) | .97 | 0.97 (0.90,1.05) | 1.05 (0.95,1.15) | .37 |
| Global Perceived Stress Score, per 1 point | 1.04 (1.04,1.05) | 1.03 (1.02,1.04) | < .001 | 1.03 (1.03,1.04) | 1.03 (1.02,1.03) | < .001 |
| Social support, per 1 point | 1.00 (0.96,1.05) | 1.06 (1.00,1.13) | .05 | 0.99 (0.96,1.02) | 1.02 (0.98,1.06) | .36 |
| Depression – None (reference) | ||||||
| Minor depression | 1.33 (1.17,1.52) | 1.24 (1.09,1.41) | .001 | 1.08 (0.97,1.20) | 1.02 (0.91,1.13) | .77 |
| Major depression | 1.53 (1.38,1.71) | 1.26 (1.11,1.43) | < .001 | 1.21 (1.11,1.33) | 1.06 (0.96,1.16) | .27 |
| Chronic kidney disease | 1.13 (0.98,1.31) | 1.05 (0.91,1.20) | .50 | 1.13 (1.02,1.24) | 1.10 (1.00,1.21) | .047 |
| Heart failure | 1.27 (1.16,1.40) | 1.13 (1.00,1.28) | .05 | 1.12 (1.05,1.21) | 1.08 (0.98,1.18) | .12 |
| Systolic blood pressure, mmHg | 1.02 (1.00,1.04) | 1.04 (1.01,1.06) | .01 | 1.02 (1.00,1.03) | 1.03 (1.01,1.05) | .006 |
| BMI, kg/m2 | 1.01 (1.01,1.02) | 1.00 (1.00,1.01) | .09 | 1.01 (1.00,1.01) | 1.00 (1.00,1.01) | .07 |
| ACE-inhibitor/ARB | 0.92 (0.84,1.00) | 0.88 (0.79,0.98) | .02 | 1.03 (0.97,1.10) | 0.99 (0.92,1.06) | .74 |
| Anti-arrhythmic | 0.78 (0.43,1.41) | 0.85 (0.49,1.49) | .57 | 1.24 (0.98,1.56) | 1.31 (1.03,1.66) | .03 |
| Anti-platelet (any) | 0.85 (0.78,0.92) | 0.87 (0.79,0.95) | .001 | 0.91 (0.85,0.96) | 0.90 (0.85,0.96) | < .001 |
| Beta-blocker | 0.87 (0.78,0.97) | 0.86 (0.76,0.96) | .01 | 1.03 (0.96,1.11) | 1.03 (0.95,1.10) | .50 |
| Anti-asthmatic | 1.29 (1.13,1.46) | 1.18 (1.03,1.36) | .02 | 1.08 (0.98,1.20) | 0.99 (0.89,1.12) | .92 |
| Anti-cholinergic | 0.91 (0.50,1.66) | 0.66 (0.38,1.16) | .15 | 1.34 (1.08,1.67) | 1.33 (1.04,1.70) | .02 |
| Oral anti-diabetic | 0.96 (0.86,1.06) | 0.93 (0.83,1.05) | .24 | 0.96 (0.89,1.03) | 0.92 (0.84,0.99) | .03 |
| Anti-depressant medications | 1.29 (1.16,1.43) | 1.07 (0.96,1.19) | .24 | 1.03 (0.94,1.12) | 0.92 (0.84,1.01) | .09 |
| Taking multiple chronic medications** | 1.03 (0.94,1.12) | 1.13 (1.01,1.26) | .03 | 1.05 (0.99,1.12) | 1.13 (1.04,1.22) | .003 |
For unadjusted models, each candidate variable was included as the sole independent variable in separate models. For multivariable models, all variables listed above were included as covariates in the model.
Multiple chronic medications = taking >1 of the 16 types of chronic medications of interest
Figure 3.
Comparison of factors associated with an increased probability for intentional and unintentional non-adherence (P<0.05). CKD indicates chronic kidney disease; DM, diabetes mellitus; BP, blood pressure; ACE, angiotensin converting enzyme; ARB, angiotensin receptor blocker.
*Multiple medications = taking >1 of the 16 types of chronic medications of interest
In sensitivity analyses, differential associations between clinical factors and non-adherence were present in those with vs. without depressive symptoms (Supplemental Tables 4–7). For instance, in participants without depressive symptoms, underlying heart failure was associated with a higher prevalence of intentional non-adherence while this association was not present in those with depressive symptoms. Similarly, chronic kidney disease was associated with intentional non-adherence in those with depressive symptoms but not those without depressive symptoms. In a sensitivity analysis, we found that in general the clinical factors associated with the most common reasons for both intentional and unintentional non-adherence were fairly consistent across these different patient-reported reasons (Supplemental Tables 8–11).
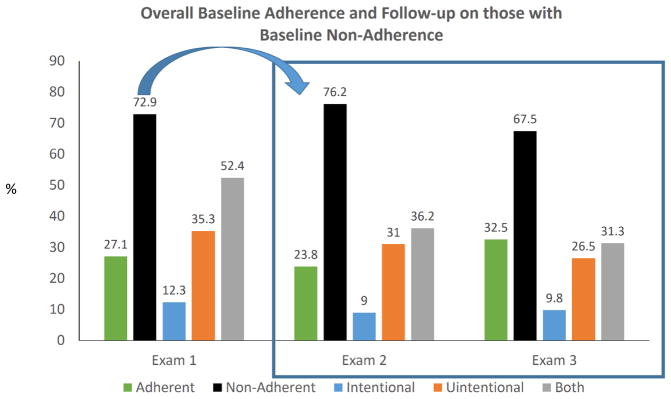
The prevalence of non-adherence was lower among those completing follow-up exams; 72.9% at baseline, 69.6% (1,872/2,688) at exam 2 and 61.6% (1,361/2,211) at exam 3. Among participants who reported non-adherence at baseline, 23.8% and 32.5% reported complete adherence at exams 2 and 3, respectively (Figure 4). There was a similar breakdown between the different types of non-adherence at the 2 follow-up exams. Of the 795 participants who reported complete adherence at baseline, approximately half of those with follow-up data at exam 2 and 3 reported complete adherence (46.9% at exam 2 and 51.1% at exam 3).
Figure 4.
Baseline adherence and follow-up details among participants reporting non-adherence at baseline.
Exam 1 adherence status included 2,138 participants (72.9%) with non-adherence out of 2,933 eligible participants on chronic medications with adherence survey data; exam 2, 1638 participants who were non-adherent at baseline with follow-up data (76.6% of baseline non-adherent cohort) and exam 3, 1315 participants who were non-adherent at baseline with follow-up data (61.5% of baseline non-adherent cohort).
Discussion
Among African Americans in the JHS, more than 70% of participants taking medications for chronic conditions reported non-adherence at baseline, with more than half of those reporting non-adherence having some degree of both intentional and unintentional non-adherence. The number of medications being taken and medication classes were was similar between those reporting and not reporting non-adherence. Factors independently associated with unintentional non-adherence included younger age and separated relationship status, while factors associated with intentional non-adherence included female sex and depressive symptoms. Specific medication classes including anti-arrhythmics and anti-asthmatics were associated with higher unintentional and intentional non-adherence, respectively. Global perceived stress was associated with both types of non-adherence. These findings provide a construct for understanding reasons for non-adherence and a rationale to assess whether personalized behavioral interventions can improve adherence.
The prevalence of participant-reported non-adherence was high in the JHS. While definitions of adherence have varied markedly in previous analyses, the results from the current analyses are consistent with prior work demonstrating that ~50% of adults with known cardiovascular disease have poor adherence17. Moreover, medication adherence rates have been shown to be lower in African-American compared with white patients18. One analysis in the Veterans Administration system where access to medications is generally equal regardless of race and income found that 63% of African Americans had inadequate blood pressure control compared with 50% of whites; African Americans were also approximately 80% more likely to be non-adherent to antihypertensive medication19. It is notable that adherence improved in the JHS cohort over time. While this may be related in part due to attrition of less adherent participants, nearly a third of participants who reported non-adherence at the baseline exam reported being adherent at the third exam visit approximately 10 years later. Moreover, there was a reduction in both intentional and unintentional non-adherence. Since there was no specific adherence intervention in the JHS, further work is needed to better understand the reasons for this improvement.
There are limited data available on intentional and unintentional non-adherence to medications20. In the JHS, approximately half of participants who were non-adherent reported both intentional and unintentional reasons for non-adherence and only 12% reported only intentional reasons for non-adherence. Intentional non-adherence was more common in women and participants with depressive symptoms as well as with specific drug classes such as anti-asthmatic medications. Previous work exploring intentional non-adherence was conducted in relatively small populations and did not consistently identify differences between variables associated with intentional vs. unintentional non-adherence20, 21. Further, data on reasons for non-adherence within specific medication classes are sparse. Therefore, the present findings may offer important insights regarding the individual phenotype of adults more likely to have intentional non-adherence. Even though the absolute percentage of participants with intentional-only non-adherence was modest at 12% among those with non-adherence (9% of overall study cohort), women and those with depressive symptoms and pulmonary disease may represent an important subset to identify and employ shared-decision making approaches to support medication adherence given the deliberate nature of their medication non-use.
We identified several variables associated with unintentional non-adherence. Specifically, participants reporting unintentional non-adherence were younger, more likely to have separated marital status and more likely to have chronic kidney disease. These observations are supported by prior work demonstrating an association between younger age and unintentional non-adherence 22. The present findings extend prior research by demonstrating that specific medication classes including anti-cholinergics and anti-arrhythmics are associated with higher unintentional non-adherence. The apparent non-deliberate nature of this non-adherence may allow for opportunities to discuss strategies to improve medication taking behaviors. For instance, strategies to address unintentional non-adherence could include pill boxes and daily reminders for medication taking as well as identification of lowest cost options and foundational support to address root causes related to forgetting and financial constraints. In addition, individuals who are non-adherent could also benefit from assessment of medication beliefs related to perceived need and overall medication concerns. In summary, unintentional non-adherence may benefit from interventions employing reminders and targeting affordability but also identifying root causes for forgetting related to perceived importance, need and benefit of medication use which could support making adherence a priority. Given that the majority of non-adherence was due to a combination of both intentional and non-intentional reasons, it is likely that successful interventions will need to take a multi-faceted approach that targets the multitude of reasons for non-adherence and also individualizes the intervention23.
Limitations
This was a retrospective analysis from a community-based cohort of African Americans in the Southern United States; results may not generalize to other communities with different medication-taking patterns. There may be unmeasured variables that influence these results, including potential additional barriers to optimal adherence that were not explicitly measured (interactions with food/beverage or other medications, lapses in insurance coverage, need for monitoring, etc.) The sample size in the group with intentional-only non-adherence was modest. Participants were grouped by self-reported adherence (“usual medication taking behaviors”) rather than by an objective assessment of adherence during a pre-specified time period (e.g., in the prior 2–4 weeks) or a specific threshold of percentage of pills taken (e.g., >80% of pills taken to categorize adherence)17. These observations are therefore dependent upon self-report and may differ from analyses that focus on pharmacy fills, pill counts, or objective adherence questionnaires. While not formally validated, the adherence questionnaire used in the JHS provides an expedient, low-burden method for describing specific reasons for non-adherence. Moreover, the optimal cut-point or definitions of adherence remain poorly understood such that the present data offer important insights into the longitudinal medication-taking behaviors of a large cohort of African Americans. Development of standardized assessment tools is needed. Further, we restricted the analysis to medications for management of a pre-defined subset of chronic diseases. Further investigation of these patterns in additional chronic conditions is warranted. Finally, the differential association between baseline factors and non-adherence based on underlying comorbidities such as depressive symptoms highlights how these data should be interpreted with caution when applied to an individual patient.
CONCLUSION
More than 70% of participants taking medications for chronic conditions in the current study reported non-adherence. Approximately half of these participants reported both intentional and unintentional reasons for non-adherence. Specific participant factors and individual medication classes were associated with distinct patterns of intentional and unintentional non-adherence, yet the overall modest discrimination of the models suggests contributions from other factors. These findings provide a construct for understanding variation in the reasons for non-adherence and provide rationale to assess whether personalized interventions can improve adherence.
Supplementary Material
Acknowledgments
Funding: This work was supported by grant R01HL117305, K24 HL125704 and R01HL117323 from the National Heart, Lung, And Blood Institute. The Jackson Heart Study is supported by contracts HHSN268201300046C, HHSN268201300047C, HHSN268201300048C, HHSN268201300049C, HHSN268201300050C from the National Heart, Lung, and Blood Institute and the National Institute on Minority Health and Health Disparities. The authors thank the participants and data collection staff of the Jackson Heart Study. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services.
The Jackson Heart Study (JHS) is supported and conducted in collaboration with Jackson State University (HHSN268201300049C and HHSN268201300050C), Tougaloo College (HHSN268201300048C), and the University of Mississippi Medical Center (HHSN268201300046C and HHSN268201300047C) contracts from the National Heart, Lung, and Blood Institute (NHLBI) and the National Institute for Minority Health and Health Disparities (NIMHD). The authors also wish to thank the staffs and participants of the JHS.
Abbreviations
- JHS
Jackson Heart Study
- HF
heart failure
- CAD
coronary artery disease
- COPD
chronic obstructive pulmonary disease
Footnotes
DISCLOSURES: RJM receives research support from the National Institutes of Health (U10HL110312 and R01AG045551-01A1), Amgen, AstraZeneca, Bayer, GlaxoSmithKline, Gilead, Luitpold, Merck, Novartis, and Otsuka. Dr. Daichi Shimbo is a consultant for Abbott Vascular and Novartis Pharmaceuticals Corporation. The remaining authors reports no relevant conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006;296(21):2563–71. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]
- 2.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 3.Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–14. doi: 10.4065/mcp.2010.0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rolnick SJ, Pawloski PA, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11(2):54–65. doi: 10.3121/cmr.2013.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balkrishnan R. Predictors of medication adherence in the elderly. Clin Ther. 1998;20(4):764–71. doi: 10.1016/s0149-2918(98)80139-2. [DOI] [PubMed] [Google Scholar]
- 6.Gerber BS, Cho YI, Arozullah AM, Lee SY. Racial differences in medication adherence: A cross-sectional study of Medicare enrollees. Am J Geriatr Pharmacother. 2010;8(2):136–45. doi: 10.1016/j.amjopharm.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charles H, Good CB, Hanusa BH, Chang CC, Whittle J. Racial differences in adherence to cardiac medications. J Natl Med Assoc. 2003;95(1):17–27. [PMC free article] [PubMed] [Google Scholar]
- 8.Osborn CY, Cavanaugh K, Wallston KA, Kripalani S, Elasy TA, Rothman RL, et al. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16(Suppl 3):268–78. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lehane E, McCarthy G. Intentional and unintentional medication non-adherence: a comprehensive framework for clinical research and practice? A discussion paper. Int J Nurs Stud. 2007;44(8):1468–77. doi: 10.1016/j.ijnurstu.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Lowry KP, Dudley TK, Oddone EZ, Bosworth HB. Intentional and unintentional nonadherence to antihypertensive medication. Ann Pharmacother. 2005;39(7–8):1198–203. doi: 10.1345/aph.1E594. [DOI] [PubMed] [Google Scholar]
- 11.Taylor HA., Jr The Jackson Heart Study: an overview. Ethnicity & disease. 2005;15(4 Suppl 6):S6-1-3. [PubMed] [Google Scholar]
- 12.Fox ER, Musani SK, Bidulescu A, Nagarajarao HS, Samdarshi TE, Gebreab SY, et al. Relation of Obesity to Circulating B-Type Natriuretic Peptide Concentrations in Blacks: The Jackson Heart Study. Circulation. 2011;124(9):1021–1027. doi: 10.1161/CIRCULATIONAHA.110.991943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carpenter MA, Crow R, Steffes M, Rock W, Heilbraun J, Evans G, et al. Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. The American journal of the medical sciences. 2004;328(3):131–44. doi: 10.1097/00000441-200409000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Wyatt SB, Akylbekova EL, Wofford MR, Coady SA, Walker ER, Andrew ME, et al. Prevalence, Awareness, Treatment, and Control of Hypertension in the Jackson Heart Study. Hypertension. 2008;51(3):650–656. doi: 10.1161/HYPERTENSIONAHA.107.100081. [DOI] [PubMed] [Google Scholar]
- 15.Akylbekova EL, Crow RS, Johnson WD, Buxbaum SG, Njemanze S, Fox E, et al. Clinical Correlates and Heritability of QT Interval Duration in Blacks: The Jackson Heart Study. Circulation: Arrhythmia and Electrophysiology. 2009;2(4):427–432. doi: 10.1161/CIRCEP.109.858894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zou G. A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 17.Kronish IM, Ye S. Adherence to cardiovascular medications: lessons learned and future directions. Progress in cardiovascular diseases. 2013;55(6):590–600. doi: 10.1016/j.pcad.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holmes HM, Luo R, Hanlon JT, Elting LS, Suarez-Almazor M, Goodwin JS. Ethnic disparities in adherence to antihypertensive medications of medicare part D beneficiaries. Journal of the American Geriatrics Society. 2012;60(7):1298–303. doi: 10.1111/j.1532-5415.2012.04037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bosworth HB, Dudley T, Olsen MK, Voils CI, Powers B, Goldstein MK, et al. Racial differences in blood pressure control: potential explanatory factors. The American journal of medicine. 2006;119(1):70e9–15. doi: 10.1016/j.amjmed.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 20.Nafradi L, Galimberti E, Nakamoto K, Schulz PJ. Intentional and Unintentional Medication Non-Adherence in Hypertension: The Role of Health Literacy, Empowerment and Medication Beliefs. Journal of public health research. 2016;5(3):762. doi: 10.4081/jphr.2016.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mukhtar O, Weinman J, Jackson SH. Intentional non-adherence to medications by older adults. Drugs & aging. 2014;31(3):149–57. doi: 10.1007/s40266-014-0153-9. [DOI] [PubMed] [Google Scholar]
- 22.Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: how unintentional is it really? BMC health services research. 2012;12:98. doi: 10.1186/1472-6963-12-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferdinand KC, Senatore FF, Clayton-Jeter H, Cryer DR, Lewin JC, Nasser SA, et al. Improving Medication Adherence in Cardiometabolic Disease: Practical and Regulatory Implications. Journal of the American College of Cardiology. 2017;69(4):437–451. doi: 10.1016/j.jacc.2016.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.