Abstract
Purpose
The aetiology of femoral trochlear dysplasia is unknown. The aim of this prospective cohort study was to describe trochlear development in a newborn population during the first six years of life.
Methods
In an earlier study, the femoral trochlea was examined by ultrasound in 174 newborns. A dysplastic trochlea was defined with a sulcus angle (SA) above 159°. Two groups were defined, one group of 15 knees with SA > 159° (dysplastic group), and one group of 101 knees with SA < 159° (non-dysplastic group). In the present follow-up study, the children were further examined at six, 18 and 72 months.
Results
There was a statistically significant difference in the SA between the dysplastic and the non-dysplastic group at all follow-ups (p < 0.001). A small but statistically significant change in the SA between 0 to 72 months was detected for the dysplastic knees (p = 0.032) and for the controls (p < 0.001).
Conclusion
Only minor changes in the anatomy of the femoral trochlea from newborn to age six years were found. A dysplastic trochlea at birth remains shallow and the anatomy does not change from normal to dysplastic during the same time span.
Level of Evidence
II
Keywords: Trochlear dysplasia, patellar instability, patellar dislocation, trochlear development
Introduction
Trochlear dysplasia is a major cause of patellar instability,1,2 reported in up to 96% of patients operated on for recurrent patellar dislocations.3 Although the different predisposing anatomical factors behind patellar instability are defined,4 the aetiology remains unclear. Instability of the patellofemoral joint usually presents with discomfort or anterior knee pain, most frequently in the second decade of life. A patellar dislocation may be the initiating event, followed by recurrent patellar instability in up to 48% of patients.5 Ailments from patellar instability among children and adolescents are common.6
Significant efforts are made to diagnose and treat developmental dysplasia of the hip early in life. Correct positioning of the femoral head in the acetabulum is crucial for normal development of the joint. We raise the question: does our knowledge of the potential for re-modulation of the hip during infancy also apply to the newborn patellofemoral joint?7 Is the position and the tracking of the patella during knee-movement vital for the development of the joint as is true for the hip joint? If so, is there any opportunity for early non-surgical treatment of trochlear dysplasia? Knowledge of the natural history of trochlear development during early childhood seems important in order to understand the potential of re-modulation of the femoral trochlea.
The formation of the patellofemoral joint in early embryonal life between four and ten weeks8 and later embryonal development9,10 has been described. All three studies found the trochlear sulcus shaped at an early embryonal stage and postulated a theory of a genetic determinant to the initial shape of the trochlea. The geometry of the neonatal trochlea has been described11 and ultrasonography has proven to be a reliable and safe method for examination of the patellofemoral joint.11,12 Nietosvaara13 performed ultrasonographic examinations of the femoral trochlea in 50 children. The femoral trochlear shape in newborns seems to be comparable with the anatomy later in life9 but data of its development during the first years of life is sparse.
A high sulcus angle (SA) indicating a flat, dysplastic trochlea has been found in newborns.14 Breech presentation with extended knees appears to be a major risk factor of trochlear dysplasia, particularly frank breech with the knees locked in extension.14 There is uncertainty as to whether this dysplasia will be permanent with the potential to cause patellar instability later in life, or if it modulates to a normal trochlea during infancy.
The aim of this study was, therefore, to describe the femoral trochlear development in a population to determine whether SA measurements changed during the first six years of life.
Patients and methods
The basis for the present prospective cohort study was the population of our former explorative cohort study in which both knees of 174 newborns had been examined by ultrasonography within three days of birth.11 The study population was newborns admitted to one of three neonatal wards at the University Hospital of Trondheim over a period of two months. Different parameters to describe the trochlear anatomy and to detect trochlear dysplasia were investigated.11 The SA seemed to be the best parameter, owing to its ease of recording and interpretation. Based on the findings in the explorative cohort study, we defined the threshold of a pathologically high SA by adding two SDs to our population mean SA of 148°, resulting in a dysplastic threshold value of 159°. This defined 17 as dysplastic- and 331 as non-dysplastic knees. However, there are no uniform limits defining trochlear dysplasia in newborns found in the literature.
The present study focuses on the follow-up of 58 of the 174 children. The 17 dysplastic knees were scheduled for further follow-up examinations. In all, 100 knees with a SA nearest the population mean of 148° were selected as normal controls for follow-up. Four patients (eight knees) of these denied further participation in the study. The contralateral knees of nine out of the 17 dysplastic knees were classified as normal and were included in the control group for further follow-up, resulting in 101 normal controls. Three follow-up examinations were scheduled: the first at six months, before the possible influence of weight bearing; the second at 18 months, after the start of weight bearing; and the last examination, just before six years of age to evaluate whether the shape of the femoral trochlea changes during childhood.
Both knees of all newborns had been examined within three days of birth by examiner 1 (CRØ).11 The follow-up examinations were performed by examiner 1 in collaboration with examiner 2 (KJH) using the same procedure. The examiners were blinded with respect to the name, birth presentation and previous clinical findings of the children.
Ultrasonography
The ultrasonographic examination of the knees was conducted with the children in bed or on the examination table in the supine position. The reliability of the method had been evaluated by a separate study. Intraobserver repeatability for the main examiner, and interobserver repeatability between the two examiners, were tested and proved reliable. Details regarding the method and the repeatability are described in detail in a previous study.11 Two ultrasound scanners were used due to the need for parallel examinations by two examiners. A GE Logiq Book XP with linear GE 8L probe and a GE Logiq 7 with linear GE 10L probe (both GE Medical Systems Co., Jiangsu, China) were used. The patella was positioned in the distal part of the trochlea by flexing the knee over 45°. By holding the transducer in a transverse plane perpendicular to the axis of the femoral axis levelled at the most ventral point of the lateral facet, images of the femoral trochlea were obtained. The ossification centre of the distal femur should be visualized, ensuring correct perpendicular angulation of the probe (Fig. 1).
Fig. 1.
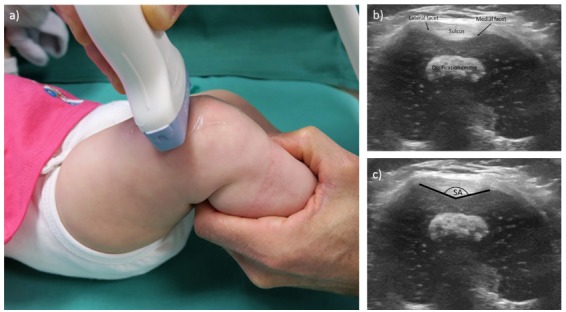
Ultrasonographic examination of the femoral trochlea: (a) the ultrasound probe is held perpendicular to the femoral axis levelled at the most ventral point of the lateral facet, obtaining a transverse image of the femoral trochlea (b); (c) the sulcus angle (SA) is shown. The images are produced for illustration of the technique, the child is four months old and not a participant of the study.
The cartilaginous SA, which is the closed angle defined by the intersection of the lines parallel to the articular cartilage of the medial and lateral femoral facet, was measured.
Statistical analysis
All statistical calculations were made using IBM SPSS Statistics for Windows version 23 (Armonk, New York). Visual inspection of Q-Q plots was used to describe whether data were normally distributed. The SA measurements were normally distributed.
Knees were dichotomized into a dysplastic group (SA ≥ 159°) and a non-dysplastic group (SA < 159°) based on the SA measurements at birth. Generalized mixed linear models were used when analyzing the SA angle to account for data dependency caused by knees nested within children together with repeated measures (four-time points, first-order autoregressive covariance structure). Fixed effects were “group,” “time,” and “group*time”. The residuals in the models were normally distributed. A figure presents plots of the model estimates. Bonferroni-adjusted significant levels are reported. The significance level was set at p < 0.05. Fig. 2 represents model estimates, adjusted for effects caused by data dependency. Consequently, the measurement results presented in Table 1 do not exactly replicate the model estimates.
Fig. 2.
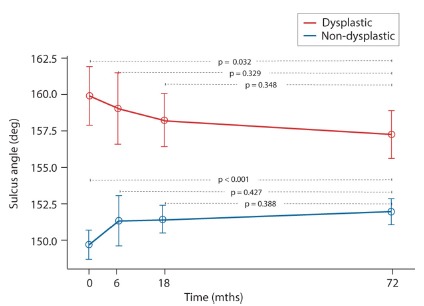
Graphical presentation of the sulcus angle. The threshold for dysplasia ≥ 159°.
Table 1.
The mean sulcus angle (SA) displayed with SD and range for both the dysplastic and non-dysplastic group. The number of the knees at 0, six, 18 and 72 months follow-up are presented; n represents the number of knees examined at the different follow-ups
| Follow-up (mths) | SA | SA | ||||||
|---|---|---|---|---|---|---|---|---|
| Dysplastic group | Non-dysplastic group | |||||||
| n | Mean | SD | Range | n | Mean | SD | Range | |
| 0 | 15 | 161.0 | 2.4 | 159.2 to 168.6 | 101 | 149.5 | 4.6 | 140.2 to 158.8 |
| 6 | 14 | 160.0 | 3.9 | 154.0 to 168.1 | 56 | 150.0 | 5.5 | 131.0 to 165.1 |
| 18 | 10 | 158.5 | 2.4 | 154.2 to 161.2 | 86 | 151.2 | 3.8 | 145.6 to 159.9 |
| 72 | 12 | 158.3 | 3.3 | 153.0 to 164.0 | 80 | 151.6 | 3.8 | 144.0 to 161.0 |
Results
Details of the number of participants during follow-up are given in Table 1. One participant with dysplasia of both knees was lost for all follow-ups. At 72 months, approximately 20% of the knees were lost to follow-up in both groups. Being settled far away was the prime reason to decline follow-up. All the participants that were originally chosen to follow were invited to all the follow-up examinations.
The number of knees at the follow-ups together with descriptive statistics are presented in Table 1.
The overall SA across all follow-ups was 158.6° in the dysplastic and 151.1° in the non-dysplastic group holding a statistical significant difference of 7.5° (p < 0.001).
The difference between the two groups was statistically significant at all follow-ups (p < 0.001).
The SA differences within the groups, between follow-ups, are presented in Fig. 2.
For both the dysplastic and the non-dysplastic group, a small but statistically significant change in the SA between 0 to 72 months was detected. The main part of this change happened within the first 18 months for the dysplastic group, the SA dropping from 160° to 158°. For the non-dysplastic group this change occurred mainly within the first six months, rising from 149° to 151°. After 18 months the graphs representing the SAs are almost parallel.
Discussion
The main finding of this study was that there was minor change in the trochlear SA during the first six years of growth. A shallow trochlea at birth, with SA measurements consistent with adult dysplasia, remained shallow.
The anatomy of the femoral trochlea is a vital determinant of patellofemoral joint stability. Even so, there is no agreement regarding factors that influence the shaping of the joint surface. The development of the joint in utero was described by Doskocil in 19858 and Glard et al9,10 in 2005. Doskocil8 studied the femoral trochlea in 14 joints of embryos aged four to ten weeks and described an asymmetric trochlea where the lateral facet was larger than the medial. He postulated that the shape of the joint was genetically determined early in utero, but influences of mechanical forces later in the intrauterine environment could cause remodelling. Glard et al9,10 performed a biometric study of the femoral trochlea in 44 foetuses aged 13 to 38 weeks and compared their findings with similar studies on adults. No significant differences were determined, which implied a genetically determined anatomy of the femoral trochlea. Nietosvaara13 conducted ultrasonographic examinations of 50 normal children from birth to 18 years and measured the SA between 134° and 155° at all ages. He found the femoral sulcus to be well developed early in life, and the SA stayed virtually constant during the growth phase. By assessment of the plots, it seems that only a few individuals were under one year of age, consequently, congenital dysplasia is probably missed and the trochlear development through infancy still unknown.
On the contrary, anthropological studies of human development show that the femur undergoes morphological changes during infantile and adolescent growth.15,16 A shift from a vertical to an oblique femur relative to the knee joint line takes place during infantile and early growth. Later, with adolescent growth, a remodelling of the distal femur epiphysis takes place with deepening of the trochlea and increased protuberance of the lateral facet. These morphological changes to the femur and knee were predicted to be acquired owing to transition to an upright posture, rather than being genetically determined.
The effects of the patella on shaping the femoral trochlea has been investigated in rabbits, showing flattening of the groove during growth with an inadequate position of the patella.17 Early reduction seems to prevent dysplasia development.18 These studies indicate that the immature skeleton is influenced and molded by the forces acting upon it. Expectantly, the possible molding effects that growth and increasing activity might afflict on the trochlear anatomy should result in gradual equalization of the SA. The overall difference of the SA through all follow-ups was 7.5°. A general agreement to the definition of trochlear dysplasia by ultrasonographical measurements does not exist. Measurements of the SA in children with patellar dislocation found SAs ranging from 154° to 195°.19 Corresponding MRI studies have found a mean SA of 156.7° in children with first-time patellar dislocation.20 With the knowledge that trochlear dysplasia is found in 96% of children treated for patellar instability,3 a threshold of pathological SA seems to be 155°. The difference between a normal SA and a SA indicating dysplasia seems to be under 10°. Our findings indicate that after six years, there is still a significant difference in the SAs between those being born with a high SA and the normal controls. A small shift towards equalization of the SA between the groups does seem to occur, taking place during the first 18 months of life.
Today, we have knowledge of the hip joint and its potential for re-modulation during infancy.7 Correct positioning of the femoral head in the acetabulum is crucial for normal development of the joint, and treatment when hip instability has been detected is based on achieving and maintaining this correct position. Correspondingly, a correct position and tracking of the patella might be essential for developing a normal trochlear groove. Intuitively, there might be an opportunity for conservative treatment of trochlear dysplasia during the first months of life. The detected early changes of the SA support this theory. There are different screening programmes for children with risk factors for hip dysplasia today, including breeches which are examined clinically and by ultrasonography of the hips. Inclusion of the knees should not cause much effort, given the existence of such an opportunity. If no initiative is taken to correct a maltracking patella, a child born with a tendency towards trochlear dysplasia may have the condition persisting at least for the first six years of life and possibly result in instability of the patellofemoral joint later in life.
In the literature, others have defined 155° as the dysplastic threshold value.3,13,20 As our threshold of 159° was higher, we performed an additional analysis using 155° as the threshold value. The changes in SA were similar to those found using 159° as the threshold. The difference between the groups was statistically significant at all follow-ups (p < 0.001).
Our methodology using ultrasonography for examining the femoral trochlea in infants has been evaluated in an intraobserver and interobserver repeatability study.11 Ultrasonographic imaging is reliable and is the only method that is ethically accepted for use in infants and children. Our measurements are comparable with other studies using the same examination technique.12,13
A child born in the frank breech position has a significantly higher risk of a shallow or flat trochlea.14 Breech positions seem to be a common risk factor for trochlear and hip dysplasia, and both conditions can be detected by ultrasonography. Since the dysplastic appearance does not change during the first six years of childhood, the dysplasia found at birth might cause instability of the patellofemoral joint. Consequently, one should consider efforts to detect and treat trochlear dysplasia early in life, comparable with existing procedures to treat developmental dysplasia of the hip. Soft, elastic braces might be used to keep the knees flexed while relaxed, with the opportunity to kick and extend the knees while awaken. Intuitively, swaddling infants in leg extension might prevent a dysplastic trochlea being transformed into one with sufficient depth to provide support for the patella during the first months of life. This topic should be further studied. Naturally, as breech presentation appears to be a risk factor for congenital dysplasia, a connection between breech presentation and patellofemoral instability should be explored.
The strength of this study is in the prospective cohort design. This study seems to be the first prospective study published covering the development of the femoral trochlea. The limitations include our definition of trochlear dysplasia in newborns which has not been evaluated by others. The limits defining dysplasia should be regarded as estimates. Also, the number of knees included in the follow-ups are small. To make the dysplasia definition and description of changes in SA more robust, further studies including larger population are needed.
Future perspectives
We believe that at least one type of trochlear dysplasia is congenital; the dysplasia found at birth might cause instability of the patellofemoral joint later in life. As breech presentation appears to be a risk factor for congenital dysplasia, a connection between breech presentation and patellofemoral instability should be explored. A last follow-up examination of the dysplastic and non-dysplastic group after growth-arrest is required to assess if the SA differences are still significant.
COMPLIANCE WITH ETHICAL STANDARDS
FUNDING STATEMENT
The study received grants from The Norwegian Orthopaedic Association in 2010 and from The Research Foundation of Unimed (#97191) in 2011.
OA LICENCE TEXT
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) License (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
ETHICAL STATEMENT
Ethical approval: The study was approved by the Regional Committees for Medical and Health Research Ethics (REC) 2010/160-1 and 2010/160-4 (doc-id: 689468). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
ICMJE CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
Special thanks to Elin M T Ljungstrôm for assisting in the correspondence with and drafting of participants.
REFERENCES
- 1.Jaquith BP, Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthop 2017;37:484–490. [DOI] [PubMed] [Google Scholar]
- 2.Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 2013;41:575–581. [DOI] [PubMed] [Google Scholar]
- 3.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994;2:19–26. [DOI] [PubMed] [Google Scholar]
- 4.Steensen RN, Bentley JC, Trinh TQ, Backes JR, Wiltfong RE. The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: a magnetic resonance imaging study. Am J Sports Med 2015;43:921–927. [DOI] [PubMed] [Google Scholar]
- 5.Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res 2007;455:93–101. [DOI] [PubMed] [Google Scholar]
- 6.Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114–1121. [DOI] [PubMed] [Google Scholar]
- 7.Holen KJ, Tegnander A, Terjesen T, Johansen OJ, Eik-Nes SH. Ultrasonographic evaluation of breech presentation as a risk factor for hip dysplasia. Acta Paediatr 1996;85:225–229. [DOI] [PubMed] [Google Scholar]
- 8.Doskocil M. Formation of the femoropatellar part of the human knee joint. Folia Morphol (Praha) 1985;33:38–47. [PubMed] [Google Scholar]
- 9.Glard Y, Jouve JL, Garron E, et al. Anatomic study of femoral patellar groove in fetus. J Pediatr Orthop 2005;25:305–308. [PubMed] [Google Scholar]
- 10.Glard Y, Jouve JL, Panuel M, et al. An anatomical and biometrical study of the femoral trochlear groove in the human fetus. J Anat 2005;206:411–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Øye CR, Holen KJ, Foss OA. Mapping of the femoral trochlea in a newborn population: an ultrasonographic study. Acta Radiol 2015;56:234–243. [DOI] [PubMed] [Google Scholar]
- 12.Kohlhof H, Heidt C, Bähler A, et al. Can 3D ultrasound identify trochlea dysplasia in newborns? Evaluation and applicability of a technique. Eur J Radiol 2015;84:1159–1164. [DOI] [PubMed] [Google Scholar]
- 13.Nietosvaara Y. The femoral sulcus in children. An ultrasonographic study. J Bone Joint Surg [Br] 1994;76-B:807–809. [PubMed] [Google Scholar]
- 14.Øye CR, Foss OA, Holen KJ. Breech presentation is a risk factor for dysplasia of the femoral trochlea. Acta Orthop 2016;87:17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tardieu C, Damsin JP. Evolution of the angle of obliquity of the femoral diaphysis during growth--correlations. Surg Radiol Anat 1997;19:91–97. [PubMed] [Google Scholar]
- 16.Tardieu C. Short adolescence in early hominids: infantile and adolescent growth of the human femur. Am J Phys Anthropol 1998;107:163–178. [DOI] [PubMed] [Google Scholar]
- 17.Huri G, Atay OA, Ergen B, et al. Development of femoral trochlear groove in growing rabbit after patellar instability. Knee Surg Sports Traumatol Arthrosc 2012;20:232–238. [DOI] [PubMed] [Google Scholar]
- 18.Wang S, Ji G, Yang X, et al. Femoral trochlear groove development after patellar subluxation and early reduction in growing rabbits. Knee Surg Sports Traumatol Arthrosc 2016;24:247–253. [DOI] [PubMed] [Google Scholar]
- 19.Nietosvaara Y, Aalto K. The cartilaginous femoral sulcus in children with patellar dislocation: an ultrasonographic study. J Pediatr Orthop 1997;17:50–53. [PubMed] [Google Scholar]
- 20.Askenberger M, Janarv PM, Finnbogason T, Arendt EA. Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations: a prospective magnetic resonance imaging study in skeletally immature children. Am J Sports Med 2017;45:50–58. [DOI] [PubMed] [Google Scholar]


